Abstract
A floating metacarpal is defined as the simultaneous dislocation of the metacarpophalangeal (MCP) and carpometacarpal (CMC) joints. Metacarpal dislocations are rare, and floating metacarpals with double dislocations are extremely rare. In this article, we present a very rare case of floating metacarpal in which the first MCP and CMC dislocations were found simultaneously and successfully treated with closed reduction, open reduction, and Kirschner wire fixation methods.
Keywords: Carpometacarpal dislocation, floating, metacarpal, metacarpophalangeal dislocation.
Introduction
A floating metacarpal is defined as the simultaneous dislocation of the metacarpophalangeal (MCP) and carpometacarpal (CMC) joints, indicating double dislocation of the same metacarpal.[1] It was first described by Moore et al.[2] in 1978 and later named the “floating thumb metacarpal” by Drosos et al.[3] Metacarpal dislocations are rare, and floating metacarpals with double dislocations are extremely rare.[4] In a recent study, there were nine case reports of floating metacarpal in the literature[5] The floating metacarpal is more often described as the thumb.[6] The treatment of these rare injuries can be quite diverse, including closed reduction and casting, percutaneous Kirschner wire (K-wire) fixation, and open repair of ligaments.[7,8]
In this article, we present a very rare case of floating metacarpal in which the first MCP and CMC dislocations were found simultaneously and successfully treated with closed reduction, open reduction, and K-wire fixation methods.
Case Report
A 44-year-old male patient was admitted to the emergency department with complaints of pain, deformity, and limitation of movement in his right hand after falling off a bike. He suffered from pain and swelling in the right thumb and the first metacarpal in his physical examination. In addition, there was a “Z” shaped external deformity and the patient could not move his thumb. The head of the first metacarpal was palpable within the volar muscle group. The distal circulation was good and there was no distal sensation defect. X-ray showed dislocation of the first CMC joint and MCP joint (Figure 1). The reduction was attempted under emergency conditions, the CMC joint could be reduced, but the first MCP joint could not be reduced (Figure 2). After preparations for anesthesia, the patient was taken to surgery for open reduction in the emergency setting.
Figure 1. The first radiographs of the patient showing dislocation of the (a) first carpometacarpal and (b) metacarpophalangeal joint.
Figure 2. First post-reduction radiographs showing that the (a) first carpometacarpal joint is reduced, but the (b) metacarpophalangeal joint is not reduced.
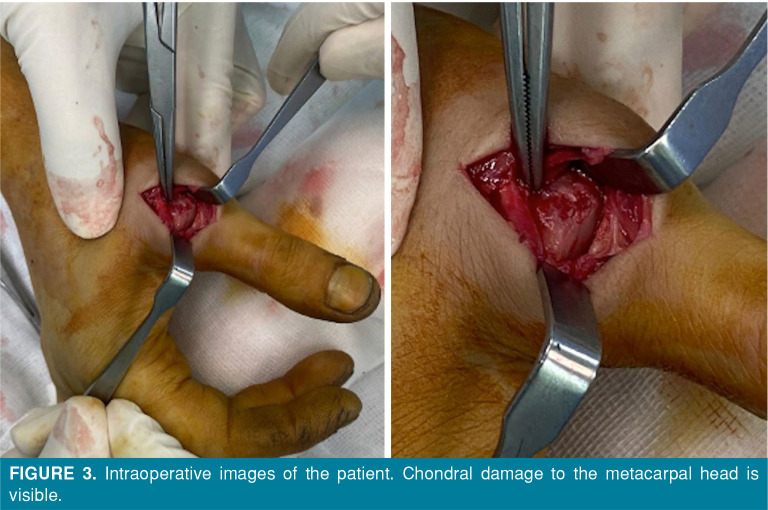
Under fluoroscopy, the first CMC joint was reduced, but there was subluxation in stress tests. Closed reduction of the MCP joint could not be performed under general anesthesia, and open reduction was initiated. A longitudinal incision was made from the dorsal aspect of the MCP joint. The MCP joint was reached. The distal articular surface of the metacarpal bone could not be visualized and was manipulated from within the volar muscle group, and it was seen to be concentrically reduced with the proximal phalanx. Meanwhile, chondral damage was detected in the metacarpal head (Figure 3). The first MCP joint was found to be concentrically reduced and stable. The MCP joint fixation was achieved with two K-wires (1.5 mm). Then, the capsule and all soft tissues were closed appropriately. Fixation of the CMC joint to the trapezium was achieved with a K-wire (1.5 mm) and a short arm splint was applied (Figure 4). The patient, who had no wound site problems or swelling, was discharged the next day and scheduled for outpatient follow-up. The sutures were removed at two weeks of follow-up and all K-wires were removed at five weeks. Control X-ray revealed that the CMC and MCP joints were in a concentric reduced position, and physical therapy was initiated. Afterward, the patient was lost to follow-up and was called several times. Finally, in October 2022, the patient was reached and scheduled for control. On the last visit, the CMC and MCP joints were concentrically reduced, the patient had no pain in both joints, there was no problem in the CMC joint movements, and the MCP joint movements were limited (Figure 5). Total follow-up duration was six months, the Quick Disabilities of Arm, Shoulder and Hand (Q-DASH) score was 11, the Visual Analog Scale (VAS) score was 2, and the Kapandji score was 8/10 (Figure 6).[9] The patient returned to his previous job where he was working using his hand.
Figure 3. Intraoperative images of the patient. Chondral damage to the metacarpal head is visible.
Figure 4. Early postoperative radiographs of the patient.
Figure 5. Six-month follow-up X-rays of the patient.
Figure 6. (a, b, c) Clinical and functional appearance of the patient at the last follow-up. (c) Clinical presentation with a Kapandji score of 8/10.
Discussion
Floating metacarpal injuries of the thumb are very rare injuries caused by high-energy trauma. Conservative treatment is usually not recommended in this type of injury, due to the high risk of instability.[10] In the literature, open reduction and fixation are preferred rather than closed reduction and immobilization.[11] In their case, Messaoudi et al.[10] reported that the dislocated MCP joint was easily reduced and the dorsolateral dislocation of the MCP joint was perfectly stable after reduction. If closed reduction fails, the volar plate, sesamoid bones, or flexor pollicis longus tendon may be interposed.[12,13] In our case, however, MCP joint reduction could not be performed in the emergency setting; therefore, open reduction and fixation with two K-wires were performed. Since no injury was detected in the collateral ligaments, no additional repair was required. During open reduction, the metacarpal head was in the volar muscle group.
Pure CMC joint dislocations are also extremely rare.[14] After stable closed reduction, some authors recommend conservative treatment with cast immobilization; however, there is a risk of longterm instability.[11-13] Khan et al.,[15] in their study in which they presented bilateral CMC joint dislocation, reported that the CMC joint was treated with a cast for six weeks after closed reduction and that functional results were good after a 15-month follow-up. Marcotte and Trzeciak[8] also treated double dislocations of the thumb satisfactorily with closed reduction and plaster cast and achieved a good range of motion. Shih et al.[14] achieved good results in their patients who were followed for 18 months after closed reduction. Some authors prefer stabilization with K-wire, regardless of the reduction method.[3,14] Messaoudi et al.[10] also found mild lateral laxity during the joint test after CMC joint reduction in their patient, and they applied conservative treatment, as the patient did not accept surgical treatment. While Bosmans et al.[16] recommended four to six weeks of plaster treatment if concentric joint compliance was achieved after closed reduction, they recommended fixation with K-wire after closed reduction and even soft tissue repair with the open reduction, if necessary, in the presence of instability or lack of joint compliance. In our case, although the CMC joint was closed-reduced in the emergency setting, a slight subluxation was detected in the CMC joint during the operation; therefore, one K- wire fixation was performed.
In conclusion, dislocations of the CMC and MCP joints of the thumb are very rare in the literature and there are only a few case reports. To date, several methods have been suggested in the treatment, and closed reduction should be attempted first. In cases where closed reduction fails, open reduction is indicated. After reduction, joint stabilization must be checked. We believe that, in cases with joint instability, K-wire fixation and, if necessary, soft tissue repairs should be performed to avoid long-term instability.
Footnotes
Conflict of Interest: The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Author Contributions: Idea/concept, design, literature review, writing the article: B.T., M.U.C.; Control/supervision, critical review: B.T.; Data collection and/or processing, references and fundings, analysis and/or interpretation: M.U.C.
Financial Disclosure: The authors received no financial support for the research and/or authorship of this article.
References
- 1.Stevanovic MV, Stark HH. Dorsal dislocation of the fourth and fifth carpometacarpal joints and simultaneous dislocation of the metacarpophalangeal joint of the small finger: A case report. J Hand Surg Am. 1984;9:714–716. doi: 10.1016/s0363-5023(84)80020-9. [DOI] [PubMed] [Google Scholar]
- 2.Moore JR, Webb CA Jr, Thompson RC. A complete dislocation of the thumb metacarpal. J Hand Surg Am. 1978;3:547–549. doi: 10.1016/s0363-5023(78)80004-5. [DOI] [PubMed] [Google Scholar]
- 3.Drosos GI, Kayias EH, Tsioros K. "Floating thumb metacarpal" or complete dislocation of the thumb metacarpal: A case report and review of the literature. Injury. 2004;35:545–548. doi: 10.1016/S0020-1383(02)00418-7. [DOI] [PubMed] [Google Scholar]
- 4.Atik OŞ. Which articles do the editors prefer to publish. Jt Dis Relat Surg. 2022;33:1–2. doi: 10.52312/jdrs.2022.57903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khan FMY, Guity MR, Arfa A, Bagheri N. A rare case of floating fifth metacarpal and review of literature. Trauma Case Rep. 2019;20:100168–100168. doi: 10.1016/j.tcr.2019.100168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tyagi HR, Kamat N, Wajekar S, Mandalia SH. Traumatic floating 1st metacarpal in a 14-year-old boy managed by close reduction and thumb spica immobilization: A rare case report. J Orthop Case Rep. 2014;4:44–47. doi: 10.13107/jocr.2250-0685.224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang F, Zhang R, Liu S, Ruan H, Xu J, Kang Q. Severe spaghetti wrist injury: Should we expand the terminology from wrist to proximal forearm. Jt Dis Relat Surg. 2022;33:273–284. doi: 10.52312/jdrs.2022.652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marcotte AL, Trzeciak MA. Nonoperative treatment for a double dislocation of the thumb metacarpal: A case report. Arch Orthop Trauma Surg. 2008;128:281–284. doi: 10.1007/s00402-007-0333-8. [DOI] [PubMed] [Google Scholar]
- 9.Kapandji A. Clinical test of apposition and counterapposition of the thumb. Ann Chir Main. 1986;5:67–73. doi: 10.1016/s0753-9053(86)80053-9. [DOI] [PubMed] [Google Scholar]
- 10.Messaoudi T, Errhaimini M, Ghoubach M, Chafik R, Madhar M, Elhaoury H, et al. Floating thumb metacarpal in a motorcyclist: A case report. Chir Main. 2015;34:91–93. doi: 10.1016/j.main.2015.01.007. [DOI] [PubMed] [Google Scholar]
- 11.Dhammi IK, Jain AK, Arora A. Isolated dislocation of the second metacarpal at both ends. J Orthop Trauma. 2001;15:143–145. doi: 10.1097/00005131-200102000-00014. [DOI] [PubMed] [Google Scholar]
- 12.Bohart PG, Gelberman RH, Vandell RF, Salamon PB. Complex dislocations of the metacarpophalangeal joint. Clin Orthop Relat Res. 1982;(164):208–210. [PubMed] [Google Scholar]
- 13.Dutton RO, Meals RA. Complex dorsal dislocation of the thumb metacarpophalangeal joint. Clin Orthop Relat Res. 1982;(164):160–164. [PubMed] [Google Scholar]
- 14.Shih KS, Tsai WF, Wu CJ, Mudgal C. Simultaneous dislocation of the carpometacarpal and metacarpophalangeal joints of the thumb in a motorcyclist. J Formos Med Assoc. 2006;105:670–673. doi: 10.1016/S0929-6646(09)60167-4. [DOI] [PubMed] [Google Scholar]
- 15.Khan AM, Ryan MG, Teplitz GA. Bilateral carpometacarpal dislocations of the thumb. Am J Orthop (Belle Mead NJ) 2003;32:38–41. [PubMed] [Google Scholar]
- 16.Bosmans B, Verhofstad MH, Gosens T. Traumatic thumb carpometacarpal joint dislocations. J Hand Surg Am. 2008;33:438–441. doi: 10.1016/j.jhsa.2007.11.022. [DOI] [PubMed] [Google Scholar]