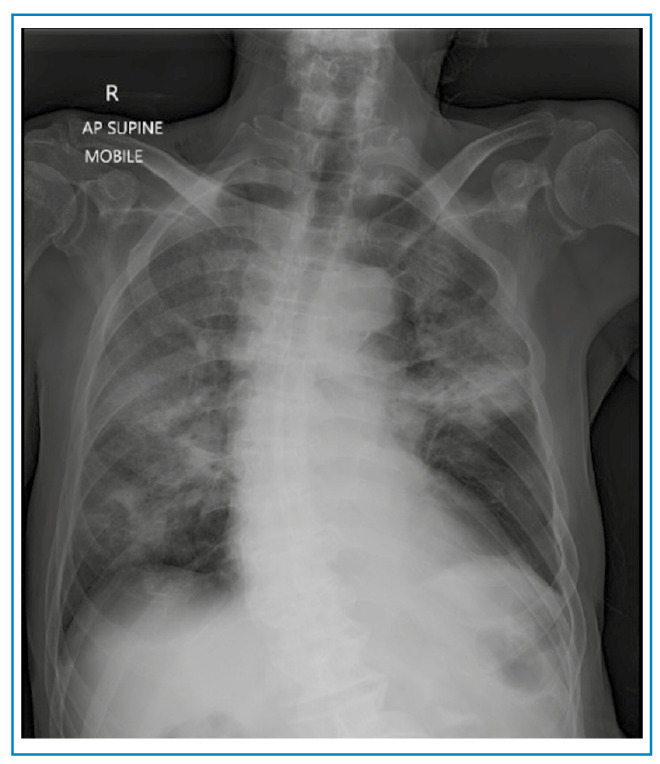
A 78-year-old man presented with a one-week history of worsening shortness of breath and cough. On examination, he had obvious respiratory distress and was profoundly hypoxic, requiring high-flow oxygen. Chest radiography revealed severe consolidation in both lung fields (Figure 1).
FIGURE 1: Chest radiograph on admission showing bilateral diffuse ground-glass opacities.
Covid-19 was confirmed by SARS-CoV-2 detection in nasopharyngeal and oropharyngeal swab samples using RT-PCR. Intravenous corticosteroids, immune modulators, and therapeutic anticoagulants were initiated. However, the patient required ongoing high-flow oxygen to maintain oxygen saturation.
Computed tomography (CT) of the thorax revealed ground-glass opacities in both lung fields with a right pneumothorax, pneumopericardium, and pneumomediastinum, and a bronchopleural fistula (Figures 2 and Figure 3). The patient was treated conservatively owing to his frailty. He was discharged from hospital to palliative care.
FIGURE 2: Computed tomography (CT) of the thorax with pneumomediastinum and pneumopericardium shown by the red arrow.

FIGURE 3: Computed tomography (CT) of the thorax with a small right apical pneumothorax, shown by a yellow arrow. The red arrow shows a bronchopleural fistula.
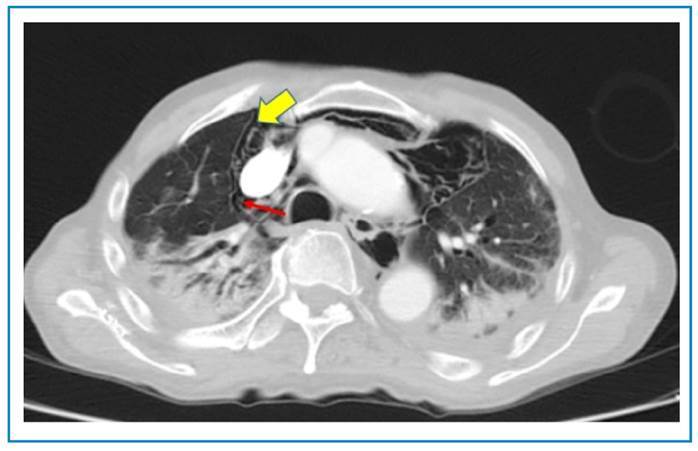
Bronchopleural fistulas, which cause spontaneous pneumothorax, pneumomediastinum, and pneumopericardium, are rare complications of Covid-19. They can occur because of the overwhelming cytokine storm leading to alveolar rupture and air dissects through the peribronchial vascular sheath into the mediastinum and pericardium1.
The patient developed a spontaneous pneumothorax, pneumomediastinum, and pneumopericardium, despite not receiving positive pressure ventilation. To our knowledge this triple combination has not been reported previously in Covid-19. It is important to recognize that they may occur in the absence of positive pressure ventilation.
Currently, there are no official guidelines for managing these complications in the context of Covid-19. Several patients have been treated conservatively with good outcomes2; however some patients require surgical intervention3. Further reports are required to obtain further evidence on the management of these complications.
ACKNOWLEDGMENTS
We express our deepest gratitude to the Radiologists of Taiping Hospital who were involved in the reporting of the CT images. We would also like to thank Dr Chee Yik Chang, Infectious Diseases Fellow from Monash Medical Centre, Melbourne on providing expertise and for the final proof-reading of this article.
Footnotes
Financial Support: None declared.
REFERENCES
- 1.1. Menter T, Haslbauer JD, Nienhold R, Savic S, Hopfer H, Deigendesch N, et al. Postmortem examination of COVID-19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings in lungs and other organs suggesting vascular dysfunction. Histopathology. 2020;77(2):198-209. Available from: http://dx.doi.org/10.1111/his.14134 [DOI] [PMC free article] [PubMed]; Menter T, Haslbauer JD, Nienhold R, Savic S, Hopfer H, Deigendesch N, et al. Postmortem examination of COVID-19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings in lungs and other organs suggesting vascular dysfunction. Histopathology. 2020;77(2):198–209. doi: 10.1111/his.14134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.2. Chang CY. Pneumomediastinum in a patient with severe Covid-19 pneumonia. Rev Soc Bras Med Trop. 2021;54:e03962021. Available from: http://dx.doi.org/10.1590/0037-8682-0396-2021 [DOI] [PMC free article] [PubMed]; Chang CY. Pneumomediastinum in a patient with severe Covid-19 pneumonia. Rev Soc Bras Med Trop. 2021;54:e03962021. doi: 10.1590/0037-8682-0396-2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.3. Talon A, Arif MZ, Mohamed H, Khokar A, Saeed AI. Bronchopleural fistula as a complication in a COVID-19 patient managed with endobronchial valves. J Investig Med High Impact Case Rep. 2021;9:23247096211013215. Available from: http://dx.doi.org/10.1177/23247096211013215 [DOI] [PMC free article] [PubMed]; Talon A, Arif MZ, Mohamed H, Khokar A, Saeed AI. Bronchopleural fistula as a complication in a COVID-19 patient managed with endobronchial valves. J Investig Med High Impact Case Rep. 2021;9:23247096211013215–23247096211013215. doi: 10.1177/23247096211013215. [DOI] [PMC free article] [PubMed] [Google Scholar]


