Abstract
Global developmental delay (GDD) is a chronic neurological disturbance that includes defects in one or more developmental domains. Although some diagnosed delays are benign, certain presentations are more worrisome. The developmental domains can be motor, cognitive, daily activities, speech or language, and social or personal development. The etiology of GDD can be prenatal, perinatal, or postnatal. It can be diagnosed early in childhood as the delay or absence of one or more developmental milestones. Hence the role of pediatric dentists and pediatricians becomes more crucial in identifying this condition.
How to cite this article
Thimmegowda U, Chikkanarasaiah N, P A, et al. Global Developmental Delay in Children with Full Mouth Rehabilitation: A Case Series. Int J Clin Pediatr Dent 2023;16(3):522-527.
Keywords: Congenitally missing teeth, Global development delay, Pediatric dentist
Introduction
According to the American Academy of Neurology and Child Neurology Society (CNS), GDD is a subset of developmental disabilities defined as a significant delay in two or more domains of development, including activities of daily living as well as motor, cognitive, speech/language, and personal/social skills.1 It involves a delay in two or more of the following developmental domains—gross and fine motor, speech and language, cognition, personal and social development, and activities of daily living. GDD is classed as—mild (functional age is 33% below the chronological age), moderate (functional age is 34–66% of the chronological age), or severe (functional age is 66% below the chronological age).2–4 GDD is classified as “significant,” if there is an underperformance of at least two standard deviations below the age-appropriate mean on standardized norm-referenced testing. It is estimated that GDD affects 1–3% of children aged 5 years or younger.2,5
Common etiological factors include—prenatal genetic disorders—down syndrome, fragile X syndrome, and chromosomal microdeletion or duplication; cerebral dysgenesis—microcephaly, absent corpus callosum, hydrocephalus, and neuronal migration disorder; vascular—occlusion and hemorrhage; drugs—cytotoxic and antiepileptic; toxins—alcohol and smoking. Early maternal infections—rubella, cytomegalovirus, and toxoplasmosis; late maternal infection—varicella, malaria, and human immunodeficiency viruses.
Perinatal—prematurity, intrauterine growth retardation, intraventricular hemorrhage, and periventricular leukomalacia; perinatal asphyxia—hypoxic-ischemic encephalopathy; metabolic—symptomatic hypoglycemia, and bilirubin-induced neurological dysfunction.
Postnatal—infections—meningitis and encephalitis; metabolic—hypernatremia, hyponatremia, hypoglycemia, and dehydration; anoxia—suffocation, near-drowning, and seizure; trauma—head injury, either accidental or nonaccidental; vascular—stroke.
Others—social—severe understimulation, maltreatment, malnutrition (deficiency of iron, folate, and vitamin D), maternal mental health disorder, and unknown.
Clinical presentation of GDD may not be uniform, as it depends on the domains affected. Clinical features may include one or more of the following dysmorphic features short stature, macrocephaly, generalized hair growth anomalies, facial asymmetry, flat facial profile, and midface hypoplasia. Epilepsy is a common finding in children having GDD. Oral findings include drug-induced gingival hyperplasia if the child is on medication for epilepsy. Due to motor and cognitive developmental delay, children with GDD also display poor oral hygiene and dental caries commensurate to inadequate plaque control.1,6 Hereby, we are presenting cases of GDD and their timely management of the same.
Case Description
Case 1
A 10-year-old male patient came to the Department of Pedodontics and Preventive Dentistry with a chief complaint of pain in the lower right back tooth region for 2 days. The pain was dull, aching, and intermittent in nature, aggravating while having food and relief on its own. The child was a known case of GDD and had undergone heart surgery for patent ductus arteriosus at the age of 3 years and now is not under any medication. There was no familial history of any neurological problem. The mother was 46 years old when she was conceived, and he was a preterm delivery (8 months). All his developmental milestones were delayed and developmental delay in speech and language and hearing impairment were also present. The child's behavior was categorized as positive according to Frankl's behavior rating scale. The profile view of the patient is shown in Figure 1, full body view of the patient with gait is shown in Figure 2.
Fig. 1.

Showing profile view of the patient
Fig. 2.

Showing full body view of the patient with gait
On intraoral examination in the maxillary arch, dental caries was present in relation to 65, retained deciduous teeth in relation to 53 and 63 and lingually erupting teeth in relation to 12 and 22 (Fig. 3), in mandibular arch-radicular abscess was present in relation to 85. Pit and fissure caries in relation to 34, 35, 36, and 46. Preshedding mobility was present in relation to 81 and clinically missing teeth in relation to 32, 41, 42, and 43 (Fig. 4). Occlusal relation was mesial step on both sides and angles class I molar relation on both sides and the crossbite was present in relation to 52 and 62 (Fig. 5). Ankyloglossia was also observed in the patient (Fig. 6). An orthopantomogram (OPG) was taken to see the status of the missing teeth; OPG revealed missing teeth in relation to 32, 41, and 42 (Fig. 7).
Fig. 3.

Showing preop maxillary arch
Fig. 4.

Showing preop mandibular arch
Fig. 5.

Showing both arches in occlusion
Fig. 6.
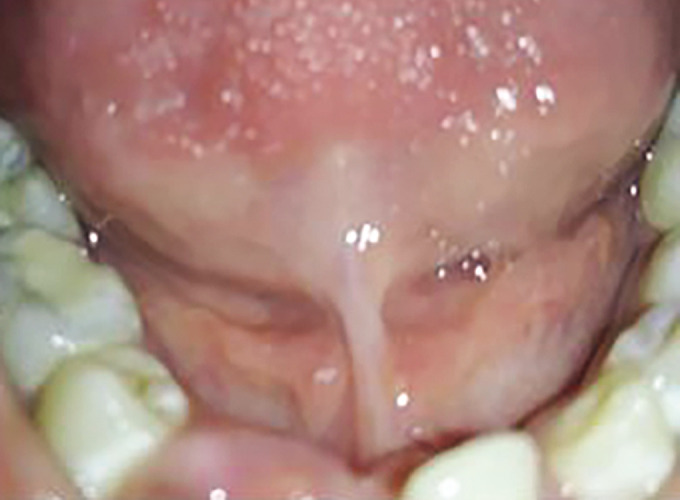
Showing ankyloglossia in the lower arch
Fig. 7.
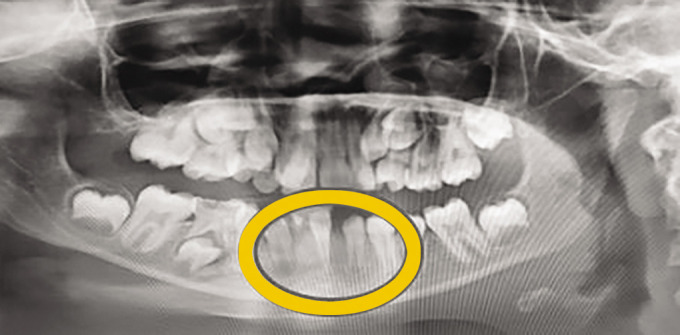
Showing OPG of the patient with congenitally missing teeth in relation to 32, 41, and 42
After obtaining the necessary consent from the Department of Pedodontics and Preventive dentistry, the child was scheduled for dental treatment. Pulp therapy was done in relation to 85, and obturation was done using metapex (Fig. 8). GIC restoration was done in relation to 65 and extraction of 53 and 63 (Fig. 9), pit and fissure sealant was done in relation to 34, 35, 36, and 46, and extraction of 81 was done under topical anesthesia (Fig. 10). Since ankyloglossia was mild and his tongue movements were not restricted, treatment was not required for the same. A removable appliance with a maxillary expansion screw and double cantilever spring was advised for the correction of the crossbite.
Fig. 8.

Showing obturation done in relation to 85 using metapex
Fig. 9.

Showing postop maxilla with GIC restoration in relation to 65, extraction is done in relation to 53 and 63
Fig. 10.

Showing postop mandible with pit and fissure sealant application done in relation to 34, 35, 36, and 46, and extraction done in relation to 81
Case Description 2
An 11-year-old patient came to the department with a chief complaint of pain in the lower right and left back tooth region for 3 days. The pain was dull, aching, and intermittent in nature, aggravating while having food and relief on its own. The child was a known case of GDD. Extraoral examination showing full body view (Fig. 11) and profile view (Fig. 12). On clinical examination, there were deep dental caries in relation to 75 and 85 (Fig. 13), dental caries in relation to 55 and 65 (Fig. 14) and clinically missing tooth in relation to 21. The occlusal view of both arch arches is shown in Figure 15. An OPG was taken to see the status of the missing teeth; OPG revealed erupting tooth in relation to 21, deep dental caries in relation to 75 and 85, and congenitally missing tooth in relation to 32, 35, and 45 (Fig. 16).
Fig. 11.

Showing full body view with the gait of the patient
Fig. 12.

Showing profile view
Fig. 13.

Showing preop maxillary arch
Fig. 14.

Showing preop mandibular arch
Fig. 15.

Showing both arches in occlusion
Fig. 16.

Showing OPG with congenitally missing tooth in relation to 32, 35, and 45
The treatment plan includes pulp therapy in relation to 75 and 85 followed by stainless steel crown, and the same has to be retained in place since the permanent successors are missing. Restoration in relation to 55 and 65 are also planned. Canines in the lower arch are allowed to erupt and orthodontic closure of space is planned. Further, follow-up and maintenance of teeth in good oral hygiene are planned with regular follow-up. Oral hygiene instruction is given for good maintenance of oral health.
Discussion
Global developmental delay (GDD) can be operationally defined as a significant delay in two or more developmental domains. These domains may include gross motor, fine motor, cognition, speech/language, personal/social (including play and recreation), or activities of daily living skills.7,8 As the clinical presentation of GDD may be heterogeneous, the oral findings depend on the developmental domains affected. Hence both the treatment needs and behavior management techniques depend on the individual.1
Functional motor disability can lead to uncontrolled movements of the head and neck and also involuntary movements of the tongue that can interfere with delivering optimal dental treatment. Excessive drooling of saliva and poor manual dexterity due to motor disability can also influence the effectiveness of tooth brushing.9 Delays or deficiencies in the development of speech, language, and cognition definitely act as a hindrance to the appropriate delivery of oral care. If social/personal development is affected, the child may not be attending school or may not want to visit a dentist too. The pedodontist should build a good rapport with such children so as to be familiar with the child.1,9
Global developmental delay (GDD) can have a significant effect on the CNS. The child had profound blindness, sensory, and nonverbal communication disorders, and a learning disability. The traditional “tell-show-do” behavioral management approach was adapted into a multisensory “tell-feel-do” approach. Although the child displayed an absence of cognitive skills and could not comprehend verbal information, instructions, or commands, verbal communication was still important in facilitating voice recognition. The tactile sensation was also important. For instance, when gently pressing the dental mirror against the child's lips, it appeared that he would open his mouth. Furthermore, the child was given ample time to explore his surroundings through touch and sound to encourage familiarity.2,10 In our case, we also adopted the method of tell-feel-do, and it was not the patient's first dental visit, so he was cooperative with the dental treatment.
A universal behavior management protocol cannot be adopted for children with GDD. In extreme cases, of GDD with developmental delay in multiple domains, general anesthesia can be considered the best management option for complete dental rehabilitation. The objective of treatment planning in cases should encompass the assessment of the level of cooperating ability for delivering oral care, a thorough review of the underlying medical conditions, and possible drug therapy for the systemic conditions along with the oral health status of the individual.1 In our case, the patient had undergone surgery for patent ductus arteriosus at the age of 3 years, so consent was obtained from the pediatrician.
Congenital absence of teeth is commonly classified as hypodontia, indicating the absence of only a few teeth; oligodontia meaning the congenital absence of many but not all the teeth and anodontia, implying the total absence of teeth. Oligodontia and anodontia are very rare, but hypodontia is relatively more common.11,12 In our cases, we saw hypodontia.
The treatment option for hypodontia includes maintenance of the primary tooth or teeth, replacement of the missing tooth, prosthetically or by transplantation, extraction of the overlying primary tooth, and then allowing the permanent teeth to drift or extraction of the primary teeth followed by immediate orthodontic treatment.
Multidisciplinary treatment is usually initiated upon the diagnosis of hypodontia, often by the pediatric dentist or general practitioner. The main contribution of these professionals is the prevention of carious lesions and maintenance of the primary teeth in the oral cavity for space maintenance and preservation of alveolar bone for future implant therapy.13 Pediatric dentist's role is for the maintenance of the primary teeth, and it should be considered if root resorption has not affected their stability. When extraction of the primary teeth is indicated, orthodontic treatment should be performed to prevent migration of the adjacent and antagonist teeth and to allow for adequate space for prosthetic rehabilitation.13,14 Prosthetic treatment options include treatment with implants or other conventional partial fixed dentures. The treatment with dental implants may be the best option for patients with hypodontia because this procedure is predictable, stable, and provides excellent aesthetic results.14 Other treatment options, such as conventional partial fixed dentures, may cause biological damage due to the need to reduce the intact tooth structure; in young patients, the risk of pulp damage is high due to the large volume of the pulp chamber. When treatment with dental implants is indicated, the possible postpubertal vertical growth of the facial skeleton should be considered, and consecutive cephalometric analyzes should be performed to establish the period of growth.13,14
Conventional implants are not recommended in growing patients since they interfere with the sagittal and transversal growth of the maxilla. A mini implant is a miniature-sized titanium implant that acts like the root of the tooth. They have a diameter of 1.8–2.7 mm; they are available in multiple tips, threads, bodies, and heads. Thread designs vary from thin to thick and thread spacing is also variable. Square, rectangular, or o-ball heads are common. The height and anatomic structures of the bone determine the length, shape, and thickness of mini implants.14 In this case, removable partial dentures can be given till the patient completes his growing stage and later other treatment options can be considered.
Crossbite correction is routinely undertaken during orthodontic treatment. Maxillary expansion may help to eliminate a mandibular displacement associated with a crossbite and/or be used to create space for the relief of crowding.15 Here, in this case, a maxillary expansion screw with a double cantilever spring was planned for the treatment of the crossbite.
Conclusion
Since pediatricians and pedodontists are the first healthcare providers to examine a child for developmental milestones. A careful history and examination can lead to early detection of GDD. Adequate rehabilitation of these children can enable them to improve their quality of life along with their oral health. Hence, we emphasize the role of pediatric dentists in the early detection of GDD and in helping these children gain better oral and general health.
Orcid
Umapathy Thimmegowda https://orcid.org/0000-0003-2426-5057
Footnotes
Source of support: Nil
Conflict of interest: None
Patient consent statement: The author(s) have obtained written informed consent from the patient's parents/legal guardians for publication of the case report details and related images.
References
- 1.Kumar S, Pai D, Saran R. Oral health characteristics and dental rehabilitation of children with global developmental delay. Case Rep Dent. 2017;2017:5486327. doi: 10.1155/2017/5486327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Modha B. Global developmental delay and its considerations in paediatric dental care—a case report. Oral. 2021;1:181–189. doi: 10.3390/oral1030018. [DOI] [Google Scholar]
- 3.Majnemer A, Shevell MI. Diagnostic yield of the neurologic assessment of the developmentally delayed child. J Pediatr. 1995;127(2):193–199. doi: 10.1016/s0022-3476(95)70294-6. [DOI] [PubMed] [Google Scholar]
- 4.McDonald L, Rennie A, Tolmie J, et al. Investigation of global developmental delay. Arch Dis Child. 2006;91(8):701–715. doi: 10.1136/adc.2005.078147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shevell MI, Majnemer A, Rosenbaum P, et al. Etiologic yield of subspecialists’ evaluation of young children with global developmental delay. J Pediatr. 2000;136(5):593–598. doi: 10.1067/mpd.2000.104817. [DOI] [PubMed] [Google Scholar]
- 6.Patil RB, Urs P, Kiran S, et al. Global developmental delay with sodium valproate-induced gingival hyperplasia. BMJ Case Rep. 2014:1–4. doi: 10.1136/bcr-2013-200672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shevell MI. The evaluation of the child with a global developmental delay. Semin Pediatr Neurol. 1998;5(1):21–26. doi: 10.1016/S1071-9091(98)80014-4. [DOI] [PubMed] [Google Scholar]
- 8.Shevell M, Majnemer A, Platt RW, et al. Developmental and functional outcomes in children with global developmental delay or developmental language impairment. Dev Med Child Neurol. 2005;47(10):678–683. doi: 10.1017/S0012162205001386. [DOI] [PubMed] [Google Scholar]
- 9.Sorsdahl AB, Moe-Nilssen R, Kaale HK, et al. Change in basic motor abilities, quality of movement and everyday activities following intensive, goal-directed, activity-focused physiotherapy in a group setting for children with cerebral palsy. BMC Pediatr. 2010;10 doi: 10.1186/1471-2431-10-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shevell M. Global developmental delay and mental retardation or intellectual disability: conceptualization, evaluation, and etiology. Pediatr Clin North Am. 2008;55(5):1071–1084. doi: 10.1016/j.pcl.2008.07.010. [DOI] [PubMed] [Google Scholar]
- 11.Ng'ang'a RN, Ng'ang'a PM. Hypodontia of permanent teeth in a Kenyan population. East Afr Med J. 2001;78(4):200–203. doi: 10.4314/eamj.v78i4.9063. [DOI] [PubMed] [Google Scholar]
- 12.Goya HA, Tanaka S, Maeda T, et al. An orthopantomographic study of hypodontia in permanent teeth of Japanese pediatric patients. J Oral Sci. 2008;50(2):143–150. doi: 10.2334/josnusd.50.143. [DOI] [PubMed] [Google Scholar]
- 13.Valle AL, Lorenzoni FC, Martins LM, et al. A multidisciplinary approach for the management of hypodontia: case report. J Appl Oral Sci. 2011;19(5):544–548. doi: 10.1590/s1678-77572011000500018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bahrami M, Saleh Saber F, Hendi A. Comprehensive treatments for congenitally missing teeth and generalized diastema. Case Rep Dent. 2017;2017:3254873. doi: 10.1155/2017/3254873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gill D, Naini F, McNally M, et al. The management of transverse maxillary deficiency. Dent Update. 2004;31(9):516–518. 521–523. doi: 10.12968/denu.2004.31.9.516. [DOI] [PubMed] [Google Scholar]


