Abstract
The aim of endodontic treatment in immature teeth is to disinfect and regenerate tissues in the apical region for the closure of the root. Stem cells from apical papilla (SCAP) by differentiating into odontogenic and osteogenic tissues create apical closure. Triple antibiotic pastes (TAP) disinfect the root canal without adversely affecting the SCAP. Differentiation of SCAP is promoted by platelet-rich fibrin (PRF). Hence, combining TAP and PRF could have a synergistic effect.
Case description
An 11-year-old girl, a 9-year-old boy, and a 13-year-old boy, symptomatic patients with open apex, are treated with TAP, PRF, and mineral trioxide aggregate (MTA) as an apical barrier sequentially. There was the formation of a calcific barrier at the end of 12, 6, and 3 months, respectively.
Conclusion
Correct diagnosis and protocol of sequential disinfection, regeneration, and finally filling the canal with an apical barrier could yield better results.
How to cite this article
Biradar N, Ragulakollu R, Tej G, et al. Combination Therapy of Antibiotics and Platelet-rich Fibrin for Apical Closure: Case Series. Int J Clin Pediatr Dent 2023;16(3):541-546.
Keywords: Apical closure, Platelet-rich fibrin, Triple antibiotic paste
Introduction
Traumatic injuries sustained in immature teeth result in cessation of root growth, leading to thin dentinal walls and open apex. This allows improper compaction of the root-filling material and lacks a three-dimensional hermetic seal. Hence, the goal of treating should aim formation of an apical barrier to prevent microleakage of toxins and bacteria into the periapical tissues. Various techniques advocated previously include customized cone or blunt-end, rolled cone technique, a short-fill technique, periapical surgery, and apexification or apexogenesis.1
McCormick et al. has hypothesized that debridement of the root canal and removal of the necrotic pulp tissue and microorganisms, along with a decrease in pulp space, are the critical factors in apexification.2 Studies also have proven the inefficiency of the complete removal of microorganisms from root canals by simple mechanical instrumentation.3 Hence a combination of instrumentation and chemical disinfection of the root canal has been suggested for the elimination of microbial organisms from the root canal.4,5
Triple antibiotic paste (TAP) is a combination of ciprofloxacin, metronidazole, and minocycline developed for the elimination of microorganisms from the root canal. Banchs and Trope were the first to report the use of TAP for pulp revascularization procedures, and it showed apical closure as well as thickening of the dentinal walls.6 With a specified dose, it has been able to show antimicrobial activity along with allowing the survival of stem cells from apical papilla (SCAP), which could be detrimental in regenerative and revascularization in endodontics.7,8 An empty space does not support cell growth. A scaffold is a matrix-like system to hold and support these stem cells in an appropriate position and for a considerable time to release growth factors. Platelet-rich plasma (PRP) and platelet-rich fibrin (PRF) are biological scaffolds used for pulpal regeneration and revascularization as they meet ideal scaffold criteria.9
Platelet-rich fibrin contains high-concentration growth factors like transforming growth factor-β (TGF-β), insulin-like growth factors (IGFs), vascular endothelial growth factor (VEGF), and a few others which are required for cell differentiation and proliferation. Hence PRF can be a scaffold for cell-based pulp/dentin regeneration.10
The rationale behind the use of a combination of TAP and PRF is to promote indirectly the proliferation of SCAP by eliminating the bacteria and directly stimulating as well as holding stem cells in a matrix to facilitate the formation of new dentine in the apical region, resulting in the increase in thickness of root canal walls and apical closure. Apical closure creates a hermetic seal by the obturating materials, thereby preventing microleakage.
This case series describes the management of an immature tooth by combining root canal disinfection with TAP, promoting apical closure with PRF over which the canal is filled with an apical barrier.
Case Description
Case 1
An 11-year-old girl presented to the Department of Dentistry with a chief complaint of pain and swelling in the upper front tooth for a few months. The pain was spontaneous, throbbing, localized, radiating pain aggravated on taking hot, cold, and sleeping, relieved after a few hours automatically or on medication. It was not associated with any systemic signs and symptoms. The patient's medical history and family history were noncontributory. There was no significant past dental history. Clinically there was visible discoloration and swelling along with sinus opening with respect to 11 and 12. Intraoral periapical radiograph revealed an improperly done root canal with 11, open apex with 11, and large radiolucency involving periapical area of 11 and 12 (Fig. 1A). There was no response to cold (ice piece), heat (gutta-percha stick), and electric pulp testing (Parkell Electronics Division, Farmingdale, New York) suggestive of the nonvital tooth with 12. With the above-mentioned clinical findings and radiograph findings suggest a diagnosis of chronic periapical abscess in relation to 11 and 12. Hence endodontic therapy is advised in 12 and reendodontic therapy with apical closure in 11.
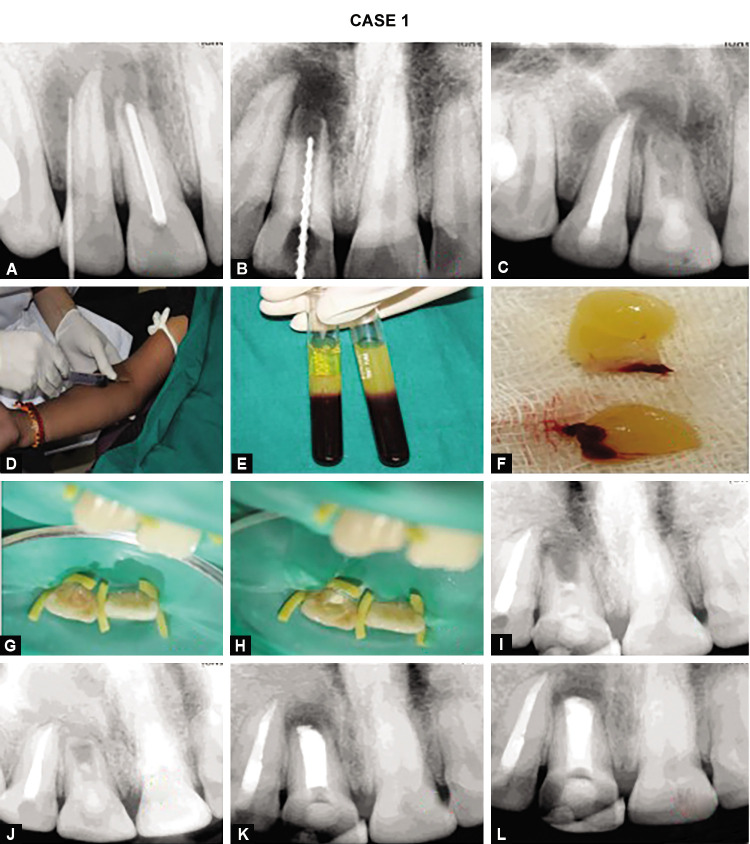
Figs 1A to L.
Preoperative intraoral periapical radiograph; (B) Intraoral periapical radiograph determination of working length; (C) Intraoral periapical radiograph of 11 filled with triple antibiotic paste; (D) Blood from the median cubital vein; (E) Centrifuged blood with three zones; (F) Membrane by compressing in a guaze cloth; (G) Clinical image of PRF membrane being inserted into the root canal; (H) Clinical image of permanent restoration is done; (I) Intraoral periapical radiograph after 6 months; (J) Intraoral periapical radiograph after 12 months; (K) Immediate intraoral periapical radiograph root canal is completely filled with MTA; (L) 36 hrs Intraoral periapical radiograph root canal is completely filled with MTA
Step 1
In the first visit, access cavity preparation is done followed by the determination of working length radiographically by inserting a K-file (80 no.) (Fig. 1B). No instrumentation was attempted, but repeated gentle irrigation was done with 1.5% of sodium hypochlorite and saline alternatively in the root canal. Sterile absorbent points are used to dry the canals. TAP was prepared by taking equal proportions of powdered ciprofloxacin, metronidazole, and minocycline and mixed with propylene glycol. Lentulospirals are inserted into the canal at a slow speed canal and are filled with TAP below the cementoenamel junction to minimize staining (Fig. 1C). Patients were recalled after 6 weeks.
Step 2
Before going to the next, the patient should be asymptomatic. After administration of local anesthetic with infiltration technique, the temporary restoration is removed and irrigated with 17% ethylenediaminetetraacetic acid solution. Bleeding is induced by manipulating periapical tissues with K-file to fill at least apical one-third of the canal and is verified by placing absorbent points. PRF is prepared by drawing 10 mL of blood from the median cubital vein of the patient (Fig. 1D). The sample collected is transferred to a test tube with no anticoagulant and centrifuged at a frequency of 3,600 revolutions per minute for 10 minutes. Three zones consisting of a base of red blood cells at the bottom, PRF clot in the middle, and acellular plasma on the top are formed (Fig. 1E). With the help of nontoothed Adson Forceps, the PRF layer was separated from the other layers and then compressed in a gauze cloth to obtain PRF membrane (Fig. 1F). With the help of an endodontic hand plugger, it is gently inserted into the root canal and pushed apically (Fig. 1G). A permanent restoration is done with glass ionomer cement for a better seal (Fig. 1H). They are scheduled for a visit at 6 or 12 months (Figs 1I and 1J).
Follow-up Examinations
At every follow-up visit, radiographs and pulp testing are done to check the status of the tooth. At the end of 12 months, radiographically there is a presence of calcific bridge formation in the apical region along with the reduction in radiopacity of the periapical lesion, but there was no significant increase in the thickness of the wall of the root. A root canal is accessed gently with a K-file (15 no.) and is used to check the calcific bridge formation. With the help of an MTA carrier, apically 3 mm was filled with MTA and the rest with gutta-percha (Figs 1K and 1L).
Case 2
A 9-year-old boy presented to the Department of Dentistry with a chief complaint of pain in his left upper front tooth for a few months. The pain was spontaneous, throbbing, localized, radiating pain aggravated on taking hot, cold, and sleeping, relieved after a few hours automatically or on medication. It was not associated with any systemic signs and symptoms. The patient's medical history and family history were noncontributory. There was no significant past dental history. Intraoral periapical radiograph presented a fracture of tooth involving pulp and marked periapical radiolucency suggestive of irreversible pulpitis in relation to 21 (Fig. 2A). There was no response to cold (ice piece), heat (gutta-percha stick), and electric pulp testing (Parkell Electronics Division, Farmingdale, New York). Hence, it was diagnosed with acute periapical abscess requiring endodontic therapy with apical closure. A similar procedure is followed as mentioned above, except for PRF was placed at the end of 2 weeks and obturated at the end of 6 months as there was apical closure (Figs 2B to 2F).
Figs 2A to F.
(A) Preoperative intraoral periapical radiograph; (B) Intraoral periapical radiograph determination of working length; (C) Intraoral periapical radiograph of 21 filled with triple antibiotic paste; (D) Permanent restoration is done with glass ionomer cement; (E) Intraoral periapical radiograph after 6 months; (F) Immediate intraoral periapical radiograph root canal is completely filled with MTA
Case 3
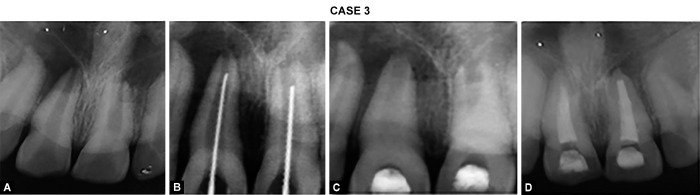
A 13-year-old boy reported to the Department of Dentistry with a chief complaint of pain in his upper front tooth for a few months. The pain was spontaneous, dull, localized pain aggravated on taking hot, cold, and on sleeping, relieved after a few hours automatically or on medication. It was not associated with any systemic signs and symptoms. The patient's medical history and family history were noncontributory. There was no significant past dental history. Intraoral periapical radiograph presented a fracture of tooth involving pulp suggestive of irreversible pulpitis in relation to 11 and 21 (Fig. 3A). There was an exaggerated response to cold (ice piece), heat (gutta-percha stick), and electric pulp testing (Parkell Electronics Division, Farmingdale, New York) suggestive of acute pulpitis. Hence it was diagnosed with irreversible pulpitis requiring endodontic therapy. A similar procedure is followed as mentioned in case description 2, except it is obturated at the end of 3 months with an apical biodentine plug and gutta-percha obturation (Figs 3B to 3D).
Figs 3A to D.
(A) Preoperative intraoral periapical radiograph; (B) Intraoral periapical radiograph determination of working length; (C) Intraoral periapical radiograph of 11, 21 filled with triple antibiotic paste; (D) Immediate intraoral periapical radiograph root canal is completely filled with biodentine
Discussion
Treating immature teeth with open apex is challenging in endodontics. Efforts aimed at disinfecting the canal and preparing the canal for obturation could not produce favorable results as the teeth are prone to fracture because of thin walls.8 Revascularization and regenerative techniques showed considerable success in the treatment of immature teeth.11–13 To achieve this, an environment free of bacteria should be created by the use of irrigation and intracanal medicament; a TAP was recommended.14 This combination is well tolerated by the stem cells’ vital pulp tissue.15 After disinfection, a scaffold should be placed in the canal space to promote the growth of new tissue. To prevent microleakage and proliferation of bacteria in the remaining space, the coronal access is sealed with restorative material. This technique yielded promising results.6
The success of apexification depends on differentiating ability of stem cells in the apical region. SCAPs present in immature permanent teeth have high proliferation potential.16,17 It acts as a great source for osteogenic, dentinogenic, adipogenic, and neurogenic differentiation. Hence it can produce primary odontoblasts, which are required for root dentin formation.18,19
Different scaffolds and their combinations have been tried for the migration and attachment of stem cells, and biologically based scaffolds have been found to be the most successful.16 PRP and PRF have been found to be suitable biological scaffolds.20,21 Self-regulation of inflammation, proliferation ability into various cell types, stimulating cellular differentiation and angiogenesis, and gradual and continuous release makes PRF a better choice for clinicians. It is proved that PRF stimulates the migration and multiplication of SCAP by the extracellular signal-regulated kinase which could be detrimental.21
In this case series, we have used TAP for disinfection of the canal and facilitating the action of PRF by establishing a sterile environment. Case reports published previously the waiting period after placement of TAP was 2 weeks only compared to 6 weeks in the first case.22 The interval is dependent on the symptomatic status of the patient. If the patient is asymptomatic, only PRF can be placed. Most of the case reports published performed placement of PRF as well as apical barrier simultaneously.22–24 Placement of MTA immediately after PRF application can cause dissolution of MTA, leading to microleakage.25 Hence in the case series only after the formation of a calcific bridge or apical closure, obturation is done along with the apical barrier. The purpose of placing an apical barrier is to provide strength and create a better seal.26
The time taken for the formation of the calcific bridge was 12, 6, and 3 months in the current case series. The difference in duration can be explained by the severity of the infection and the width of the apical foramen. Duration of the formation is prolonged if calcium hydroxide and PRF combination are used instead of TAP and PRF.23,27 This can be explained by the better antimicrobial efficacy and stimulation of stem cells by TAP compared to calcium hydroxide.28,29
A randomized control trial with a similar protocol as in a present case series comparing PRF with blood clot concluded that a sterile environment in the root canal is key for the success of the treatment, TAP along with sodium hypochlorite is an effective means of controlling infection, PRF is useful in cases where MTA is placed with minimal or optimal pressure.30 There was apical barrier formation observed in 45.4% of group I while in 63.6% of group II. Therefore, it proves a valid point that PRF could be an additive effect than a solitary effect.30 Identical results were also seen in a similar study comparing PRF, PRP, MTA, and PRP with collagen, where there was no statistically significant apical closure among the groups though the PRF group was better compared to MTA and PRP.31
Conclusion
The role of antibiotics in creating a favorable environment for the growth of pulpal and periapical tissues is once again proved in the present case series. TAP plays a significant role as an intracanal medicament in regenerative and revascularization procedures. The synergistic effect of TAP and PRF is noteworthy in these procedures. Finally, for a successful result in these procedures, a similar protocol as performed in the present case series can be followed although needs further systematic evaluation.
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Morse DR, O’Larnic J, Yesilsoy C. Apexification: review of the literature. Quintessence Int. 1990;21(7):589–598. [PubMed] [Google Scholar]
- 2.McCormick JE, Weine FS, Maggio JD. Tissue pH of developing periapical lesions in dogs. J Endod. 1983;9(2):47–51. doi: 10.1016/S0099-2399(83)80074-0. [DOI] [PubMed] [Google Scholar]
- 3.Bystrom A, Sundqvist G. Bacteriologic evaluation of the efficacy of mechanical root canal instrumentation in endodontic therapy. Scand J Dent Res. 1981;89(4):321–328. doi: 10.1111/j.1600-0722.1981.tb01689.x. [DOI] [PubMed] [Google Scholar]
- 4.Bansal R, Jain A. Overview on the current antibiotic containing agents used in endodontics. N Am J Med Sci. 2014;6(8):351–358. doi: 10.4103/1947-2714.139277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gulabivala K, Patel B, Evans G, Ng YL. Effects of mechanical and chemical procedures on root canal surfaces. Endodontic Topics. 2005;10:103–122. doi: 10.1111/j.1601-1546.2005.00133.x. [DOI] [Google Scholar]
- 6.Banchs F, Trope M. Revascularization of immature permanent teeth with apical periodontitis: new treatment protocol? J Endod. 2004;30(4):196–200. doi: 10.1097/00004770-200404000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Gougousis K, Giannakoulas DG, Taraslia V, et al. Number of dental stem cells on root canal dentin after application of triple antibiotic paste or calcium hydroxide: an in vitro study. Eur J Dent. 2019;13(2):161–165. doi: 10.1055/s-0039-1688733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Windley 3rd W, Teixeira F, Levin L, et al. Disinfection of immature teeth with a triple antibiotic paste. J Endod. 2005;31(6):439–443. doi: 10.1097/01.don.0000148143.80283.ea. [DOI] [PubMed] [Google Scholar]
- 9.Keswani D, Pandey RK. Revascularization of an immature tooth with a necrotic pulp using platelet-rich fibrin: a case report. Int Endod J. 2013;46(11):1096–1104. doi: 10.1111/iej.12107. [DOI] [PubMed] [Google Scholar]
- 10.Huang GTJ. A paradigm shift in endodontic management of immature teeth: conservation of stem cells for regeneration. J Dent. 2008;36(6):379–386. doi: 10.1016/j.jdent.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 11.Kling M, Cvek M, Mejare I. Rate and predictability of pulp revascularization in therapeutically reimplanted permanent incisors. Endod Dent Traumatol. 1986;2(3):83–89. doi: 10.1111/j.1600-9657.1986.tb00132.x. [DOI] [PubMed] [Google Scholar]
- 12.Petrino JA, Boda KK, Shambarger S, et al. Challenges in regenerative endodontics: a case series. J Endod. 2010;36(3):536–541. doi: 10.1016/j.joen.2009.10.006. [DOI] [PubMed] [Google Scholar]
- 13.American Association of Endodontics. American Association of Endodontists; 2016. AAE Clinical considerations for a regenerative procedure. [Google Scholar]
- 14.Ayukawa Y. Pulpal response of human teeth to antibacterial biocompatible pulp-capping agent- improvement of mixed drugs. Japn J Conservative Dent. 1994;37:643–651. [Google Scholar]
- 15.Waya SI, Ikawa M, Kubota M. Revascularization of an immature permanent tooth with apical periodontitis and sinus tract. Dent Traumatol. 2001;17(4):185–187. doi: 10.1034/j.1600-9657.2001.017004185.x. [DOI] [PubMed] [Google Scholar]
- 16.Huang FM, Yang SF, Zhao JH, et al. Platelet-rich fibrin increases proliferation and differentiation of human dental pulp cells. J Endod. 2010;36(10):1628–1632. doi: 10.1016/j.joen.2010.07.004. [DOI] [PubMed] [Google Scholar]
- 17.Sonoyama W, Liu Y, Yamaza T, et al. Characterization of the apical papilla and its residing stem cells from human immature permanent teeth: a pilot study. J Endod. 2008;34(2):166–171. doi: 10.1016/j.joen.2007.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patil, R, Kumar, BM, Lee WJ, et al. Multilineage potential and proteomic profiling of human dental stem cells derived from a single donor. Exp Cell Res. 2014;320(1):92–107. doi: 10.1016/j.yexcr.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 19.Trope M. Treatment of the immature tooth with a non-vital pulp and apical periodontitis. Dent Clin North Am. 2010;54(2):313–324. doi: 10.1016/j.cden.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 20.Jadhav G, Shah N, Logani A. Revascularization with and without platelet-rich plasma in nonvital, immature, anterior teeth: a pilot clinical study. J Endod. 2012;38(12):1581–1587. doi: 10.1016/j.joen.2012.09.010. [DOI] [PubMed] [Google Scholar]
- 21.Bi J, Liu Y, Liu XM, et al. Platelet-rich fibrin improves the osteo-/odontogenic differentiation of stem cells from apical papilla via the extracellular signal-regulated protein kinase signaling pathway. J Endod. 2020;46(5):648–654. doi: 10.1016/j.joen.2020.02.004. [DOI] [PubMed] [Google Scholar]
- 22.Pawar AM, Pawar SM, Pawar MG, et al. Retreatment of endodontically failed tooth with wide-open apex using platelet rich fibrin membrane as matrix and an apical plug of Biodentine™. Eur J Gen Dent. 2015;4(3):50–54. doi: 10.4103/2278-9626.163341. [DOI] [Google Scholar]
- 23.Yadav P, Pruthi PJ, Naval RR, et al. Novel use of platelet-rich fibrin matrix and MTA as an apical barrier in the management of a failed revascularization case. Dent Traumatol. 2015;31(4):328–331. doi: 10.1111/edt.12168. [DOI] [PubMed] [Google Scholar]
- 24.Khetarpal A, Chaudhry S, Talwar S, et al. Endodontic management of open apex using MTA and platelet-rich fibrin membrane barrier: a newer matrix concept. J Clin Exp Dent. 2013;5(5):e291–e294. doi: 10.4317/jced.51178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karan NB, Aricioğlu B. Assessment of bone healing after mineral trioxide aggregate and platelet-rich fibrin application in periapical lesions using cone-beam computed tomographic imaging. Clin Oral Investig. 2020;24(2):1065–1072. doi: 10.1007/s00784-019-03003-x. [DOI] [PubMed] [Google Scholar]
- 26.Matt GD, Thorpe JR, Strother JM, et al. Comparative study of white and gray mineral trioxide aggregate (MTA) simulating a one- or two-step apical barrier technique. J Endod. 2004;30(12):876–879. doi: 10.1097/01.don.0000136213.93171.45. [DOI] [PubMed] [Google Scholar]
- 27.Sakthivel S, Gayathri V, Anirudhan S, et al. Platelet-rich fibrin and collagen matrix for the regeneration of infected necrotic immature teeth. J Clin Transl Res. 2020;6(1):1–5. [PMC free article] [PubMed] [Google Scholar]
- 28.Adl A, Hamedi S, Sedigh Shams M. The ability of triple antibiotic paste and calcium hydroxide in disinfection of dentinal tubules. Iran Endod J. 2014;9(2):123–126. [PMC free article] [PubMed] [Google Scholar]
- 29.Mohammadi Z, Jafarzadeh H, Shalavi S, et al. A review on triple antibiotic paste as a suitable material used in regenerative endodontics. Iran Endod J. 2018;13(1):1–6. doi: 10.22037/iej.v13i1.17941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ragab RA, Lattif AEAE, Dokky NAEWE. Comparative study between revitalization of necrotic immature permanent anterior teeth with and without platelet rich fibrin: a randomized controlled trial. J Clin Pediatr Dent. 2019;43(2):78–85. doi: 10.17796/1053-4625-43.2.2. [DOI] [PubMed] [Google Scholar]
- 31.Narang I, Mittal N, Mishra N. A comparative evaluation of the blood clot, platelet-rich plasma, and platelet-rich fibrin in regeneration of necrotic immature permanent teeth: a clinical study. Contemp Clin Dent. 2015;6(1):63–68. doi: 10.4103/0976-237X.149294. [DOI] [PMC free article] [PubMed] [Google Scholar]