Abstract
Aim
To analyze the effectiveness of motivational interviewing (MI) compared to traditional health education among mothers in improving children's oral health and behavioral changes.
Review methods
The search strategy was framed using relevant MeSH terms and free text terms in PubMed, Medical Literature Analysis and Retrieval System Online (MEDLINE), Directory of Open Access Journals (DOAJ), Cochrane Library, and Google Scholar for the articles published in the English language between 1st January 2000 and 31st December 2020. Only randomized controlled trials, non-randomized controlled trials, and clinical trials comparing MI with traditional health education were included. Cochrane risk of bias (ROB) tool was used for the quality assessment of the included studies, and Review Manager 5.3 software was used for computing results.
Results
A total of 9 studies were included for qualitative synthesis and 5 for quantitative synthesis from an initial search of 3,708 articles. The cumulative mean difference for dental caries was −1.03 [95% confidence interval (CI)—1.37–0.70] p < 0.00001, for frequency of toothbrushing Pooled odds ratio was 1.69 (95% CI—0.68–4.25) p = 0.26 and for in-between snacking was 0.83 with (95% CI—0.48–1.44) p = 0.51. A significant difference was present in dental caries among children with mothers in the MI group, while no difference was present in in-between snacking and frequency of toothbrushing between both the groups.
Conclusion
Motivational interviewing (MI) prove to be significantly effective in reducing newer dental caries for shorter duration; however, long-term effectiveness could not be assessed.
Clinical significance
Motivational interviewing (MI) can be considered an effective and feasible method for oral health education to mothers, which will, in turn, improve the oral health of their children.
Protocol registration
International prospective register of systematic reviews (PROSPERO) under registration code. CRD42021224278.
How to cite this article
Karande PH, Shetty VB, Vinay V, et al. Comparative Evaluation of Oral Health and Behavior Changes in Children after Motivational Interviewing and Traditional Method of Oral Health Education among Mothers: A Systematic Review and Meta-analysis. Int J Clin Pediatr Dent 2023;16(3):464–473.
Keywords: Dental Caries score, Frequency of toothbrushing, Gingival score, In-between snacking evaluation, Oral health, Plaque score, Randomized controlled trial, Risk of bias, Systematic review and meta-analysis
Introduction
Dental caries has its effects on people of all ages with varying severity synergized with other risk factors.1 Among children, it is considered to be the most common preventable non-communicable disease according to the World Health Organization (WHO). The risk of dental caries begins at the time of eruption of the first tooth in the oral cavity. Erupted teeth stay sound in many children, but a significantly large population in this age-group experiences early childhood caries leading to ravaged teeth with its rapid development and difficulty of control.2 Though the disease is preventable, the condition has not improved over the past 25 years. Around 573 million children worldwide suffer from untreated dental caries in the primary dentition.3 A recent meta-analysis reports 48% as global prevalence among children4 with a range of 25–83% among 5 years old in South-East Asian countries.5
Oral health contributes to general health, thereby enabling us to speak and eat without discomfort, active disease, or embarrassment. Poor oral health, including dental caries, gingival disease, and compromised oral hygiene, has a great impact on the overall quality of life of children as well as their caregivers. Apart from pain and esthetics, it adversely affects their psychology. The pain and agony associated with the diseases force children to miss school, accelerating poor academic performance and decreased working hours for parents due to multiple dental appointment schedules contributing to work loss and financial loss.6 Moreover, the visit to a dentist at the time of advanced disease condition leads to a huge financial burden on the parent as a result of the cost associated with treatment.7
Providing oral prophylaxis and restorative treatment for gingival and dental caries, respectively, has been a traditional method followed for ages. As time advanced, the concept of prevention came into existence. Many paediatric dentists follow an approach for maximizing chances of caries-free permanent dentition while treating children at an early age. The goal of the treatment focuses on minimizing the sepsis and pain to the primary dentition and reducing treatment-related anxiety.8 Apart from this clinical approach towards any oral condition, WHO emphasizes the non-clinical approach that comprises improving awareness among children as well as their caregivers with respect to oral diseases and their prevention at the first go. Literature provides evidence on the impact of oral health education, habit inculcation and constant motivation on improved oral health at all ages.
As it is said, good habits are inculcated best when they are started early in life, and thus childhood is the best time for inculcating healthy oral habits among children. The habits initiated at this age have a high chance of continuing for a lifetime. But unfortunately, unlike adults who can take independent decisions regarding their oral health, children need constant assistance from their caregivers. And thus, the oral health of children is greatly dependent on and influenced by their caregivers. It becomes a necessity to educate mothers regarding their child's oral health and guide them in implementing certain steps from the time the child is born. This includes but is not restricted to cleaning the gum pads and tongue of the child with cloth and lukewarm water, initiating to brush as soon as the first tooth erupts in the oral cavity, visiting a pediatric dentist every 6 months, guiding children in brushing teeth and educating them on oral hygiene with advancing age.
Educating mothers through health education programs encompassing the use of audiovisual aids and health talks has been shown to gain improve the condition to some extent, but these interventions come with certain limitations. Though they educate parents, the traditional health education model proves to be insufficient in changing parents’ behavior towards their high-risk children as parents do not visit the dentist with a readiness to change their patterns that are well established but rather to get an immediate solution to the problem.9
On the contrary, MI, coined by psychologist Miller, an emerging concept that is patient-centered and goal-directed and supports an individual's readiness to change through intrinsic motivation. MI has been adopted in use for quitting adverse habits related to drug addiction, alcoholism, and tobacco, bringing change in lifestyle for preventing health-threatening conditions like obesity, hypertension, diabetes, and eating disorders.10 MI is a purposeful conversation directed towards a specific goal and is a guiding type approach rather than a following or directing type. It elicits a person's own reason for bringing change in the habit by the person enlisting the advantages and disadvantages of continuing with the old habit and incorporating a new healthy habit within the atmosphere of acceptance and compassion. It is like giving people's health in people's hands.11 Considering the importance of this approach, this systematic review and meta-analysis were conducted aiming to evaluate and compare Oral Health and behavior changes in children after educating mothers using MI and traditional methods of oral health education.
Review Methods
Protocol and Registration
This systematic review and meta-analysis were performed in accordance with Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA 2020)12 statement guidelines, the Cochrane Handbook for systematic reviews of interventions,13 version 5.1.0 and is registered at PROSPERO under the registration code, CRD42021224278.
Literature Search
A systematic search was carried out in databases; PubMed, MEDLINE, DOAJ, Cochrane library, and Google scholar for the articles. Relevant MeSH terms and free text terms were used based on Population, Intervention, Comparison, Outcomes and Study (PICOS) (Table 1). The search strategy was framed using Boolean operators (OR, AND) with #1AND #2AND #3AND #4AND #5. Apart from these databases, the articles were also screened by cross reference and citation chasing, along with hand searching from specialty pediatric journals.
Table 1.
Search strategy and PICOS tool
| Search strategy | |
|---|---|
| Focused question | Is there a difference in the effect of MI and the traditional method of oral health education given to mothers on oral health outcomes and behavior changes of their children? |
| Search strategy | |
| Population | Mothers [MeSH] and their children [MeSH] OR Parents [MeSH] OR preschool children [MeSH] OR School children [Text Word] |
| Intervention | MI [MeSH] OR oral health education [Text Word] OR dental counseling [Text Word] |
| Comparisons | Traditional oral health education [Text Word] OR oral health education using videos [Text Word] OR pamphlets [MeSH]. |
| Outcomes | Oral health [MeSH] OR behavior changes [Text Word] OR dental caries outcomes [Text Word] OR caries assessment [Text Word] |
| Study design | Controlled clinical trials, clinical trials [MeSH], randomized controlled trial |
| Search combination | #1AND #2AND #3AND #4 |
| Database search | |
| Language | English language |
| Electronic databases | PubMed, DOAJ, MEDLINE, Cochrane Library, and Google Scholar |
| Journals | International Journal of Paediatric Dentistry, International Journal of Clinical Pediatric Dentistry, European Journal of Paediatric Dentistry, Journal of Indian Society of Pedodontics and Preventive Dentistry, Journal of Indian Association of Paediatric Dentistry. |
Eligibility Criteria
Studies published in the English language between 1st January 2000 and 31st December 2020 were conducted on mothers and their children(irrespective of age) with mothers (irrespective of any age, Socioeconomic status, occupation, education, and the number of children they have) receiving MI (delivered by a dental health care professional or caregiver) as a part of an experimental group and traditional oral health education as a part of control group aimed at assessing primary outcome; dental caries, dental plaque score, and gingival score [using decayed, missing, filled, teeth (dmft), decayed, missing, filled, surface (dmfs) International Caries Detection and Assessment System (ICDAS), WHO criteria for dental caries, modified Radike criteria for dental caries, plaque index, gingival index with a minimum of 2 months follow-up, and mean standard deviation (SD) as an effect measures] and secondary outcome; behavioral changes in children in terms of frequency of toothbrushing and in between snacking (using score of questionnaires with effect measures as number, percentage and mean scores) were included in the study.
The study designs considered for inclusion was randomized controlled trials, non-randomized controlled trials, quasi-experiments, and clinical trials. Only open-access articles freely available in PubMed, MEDLINE, DOAJ, Cochrane Library, and Google Scholar were included, whereas studies with the availability of only abstracts, articles in other languages apart from English, studies reporting outcomes via observational studies or case reports or reviews or expert opinion, studies with single intervention arm and the ones providing data on other educational interviewing techniques in an experimental group along with grey literature were excluded from the present review.
Study Selection
Two reviewers independently (PK and VV) undertook a three-step selection of studies in the databases based on eligibility criteria. In 1st step, the titles of the articles were screened and irrelevant articles were excluded. The second step included the screening of remaining articles based on the abstract, and the third step screened articles after reading the full text to verify the degree of compliance that the studies had with eligibility criteria and make a final decision of their inclusion in this review. Duplicate records were removed using the software. The level of concordance, calculated through Cohen's kappa, between the two reviewers was 0.94 for titles and abstracts and 0.96 for full texts. Discrepancies among authors/reviewers were resolved by the third author (KB) through careful discussion. If needed, authors of the included studies were contacted by e-mail for clarification of any doubts and missing data.
Data Extraction
Before proceeding with data extraction, a standardized data extraction form was prepared in a Microsoft Excel version (2013) spreadsheet assisted by an expert. A pilot form with data extraction of two articles under headings; study ID, place of the study, participant's age (children), the sample size in experimental and control group post follow-up, number of sessions in experimental and control group, duration of sessions in both groups, follow-up period, method and measure of outcome assessment, pre- and post- scores of dental caries and plaque and gingival condition, frequency of change in toothbrush pre- and postintervention, a score of in-between snacking pre- and postintervention and author's conclusion was completed. After the consensus of both authors with the data extracted, further extraction was commenced.
Risk of Bias (ROB) Assessment of Included Studies
Cochrane ROB assessment tool14 was used for categorizing the studies into high, medium, and low risk for further inclusion in quantitative analysis. The ROB tool consisted of critically appraising the studies based on domains; random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, risk of other potential sources of bias, and overall ROB.
Statistical Analysis
Measures of continuous data were assessed as change in mean score before and after intervention for dental caries, plaque index score, and gingival index score, as well as number and percentage of in-between snacking and frequency of toothbrushing (before and after intervention). Mean differences and their standard deviation were analyzed using Review Manager 5.3 software. Chi-square and Tau-square were used to assess whether the observed difference was homogeneous or heterogeneous among the studies. The heterogeneity between the studies was assessed using I2 statistics. A random-effects model for meta-analysis was performed if the heterogeneity was found to be high. Also, the statistical significance was set at p-value (two-tailed) <0.05.
Review Results
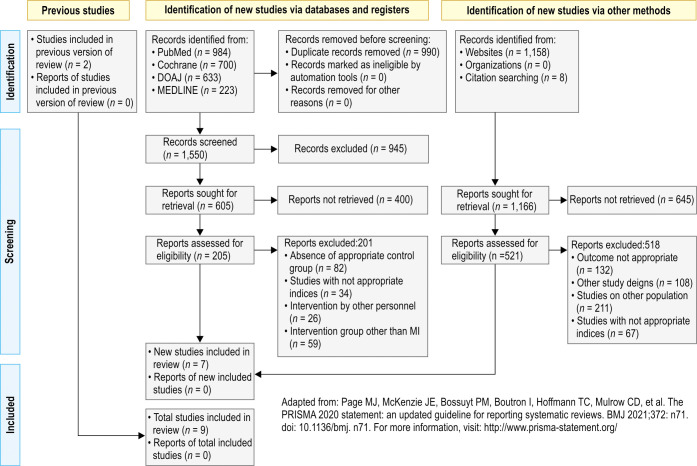
The initial search in PubMed, MEDLINE, DOAJ, and Cochrane library gave a total of 2,540 hits which were subjected to duplicate removal, after which 990 articles were excluded. From the remaining 1,550 articles, 945 were excluded after screening through titles. A total of 400 articles were further removed from the screening process as the abstract gave enough information to decide on their exclusion. The remaining 205 articles were read the full text, from which 201 articles were excluded with reason; absence of appropriate control group in 82, outcomes measured with inappropriate index in 34, intervention conducted by other personnel in 26, and intervention group other than MI in 59 articles. The remaining 04 studies were included for qualitative synthesis. On the other hand, 1,166 studies were identified from other sources like google scholar, which underwent screening phases similar to the ones identified from databases, and a total of 03 studies were further included in the qualitative synthesis. There were two additional studies identified from the previous review, which were directly included in the last phase of screening. Thus, nine studies were included in the present review and were subjected to qualitative synthesis, while 05 studies from these were considered for quantitative synthesis. The screening process is explained in the form of the PRISMA flowchart 2020 (Flowchart 1). The study characteristics of the included studies are presented in Table 2.
Flowchart 1.
PRISMA flow diagram 2020, for selection of studies
Table 2.
Characteristics of the included studies
| Study Id | Authors (year) | Study place | Study design | Participant's age (children) | Sample size (initial/last follow-up) | No. of sessions | Duration of sessions | Follow-up period | Method and outcome assessment measurement | Dental caries | Plaque score | Gingival score | Change in toothbrushing frequency | In-between snacking score | Author's conclusion | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MI | Traditional Education | MI | Traditional Education | MI | Traditional Education | Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | ||||||||
| 1 | Mohammadi et al. (2015)22* | Iran | Community trial | 4–6 years | 111/108 | 111/105 | 7 | 1 | 45 minutes | 45 minutes | 6 months | Mean ± SD of ICDAS score, PI, GI (frequency %) | 4.87 ± 4.1 (MI) | 4.79 ± 4.39 (MI) | 111 (100%) | 108 (97.3%) | 111 (100%) | 108 (97.3%) | Using MI as an oral health education model was significantly more effective than the traditional model. | ||||
| 2 | Gonzalez et al. (2014)17 | Mexico | Randomized clinical trial | 6–10 years | 50/49 | 50/47 | 7 | 1 | 45 minutes | 45 minutes | 6 and 12 months | Mean, SD of ICDAS score, PI (mean SD), questionnaire for in-between snacking (mean) | 9.98 (3.60)–traditional 9.80 (3.91)–MI | 3.15 (0.97)–traditional 2.12 (0.85)–MI | 62.4 (16.5)–traditional 51.4 (17.4)–MI | 41.8 (23.2)–traditional) 17.1 (11.3)—MI | 1.55–traditional 1.61–MI | MI is an effective and promising technique for establishing preventive behaviors | |||||
| 3 | Nomaire et al. (2020)21 * | Egypt | Randomized controlled clinical trial (parallel arms) | 4–6 years | 58/52 | 58/55 | 4 | 1 | 15–30 minutes | 15 minutes | 6 months | The mean and standard deviation of the questionnaire score | 7.64 ± 2.26– conventional, 7.04 ± 1.98– MI | 8.58 ± 2.64–conventional, 9.75 ± 2.05–MI | Using MI as an oral health education tool was significantly more effective in promoting preschool children's oral hygiene | ||||||||
| 4 | Weinstein et al. (2006)9 * | Columbia, USA | Randomized clinical trial | 6–18 months | 220/205 | 220/200 | 7 | 1 | 45 minutes | 11 minutes | 2 years | New caries in % using (modif Radike criteria) | 52.0%–traditional, 35.2%–MI | An MI intervention enhanced the preventive behavior of mothers of young children at high risk of developing caries. | |||||||||
| 5 | Manchanda et al. (2014)18 | Bengaluru | Randomized controlled clinical trial (parallel arms) | 6–18 months | 160/137 | 160/128 | 5 | 1 | Not given | Not given | 8 months | Mean, SD (WHO + Initial lesions), mean ± SD score of questionnaire used for in-between snacking and frequency of toothbrushing. | 0.39 + 0.79–traditional, 0.23 + 0.58– MI | 3.90%– traditional, 2.92%–MI | 21.88%-traditional, 59.12%–MI | 104 (81.25 %)–traditional, 91 (66.42 %)–MI | 106 (82.81%)–traditional, 109 (80.15 %)–MI | The motivational intervention was more effective in reducing dental decay in the children as compared to the other two groups. | |||||
| 6 | Colvara et al. (2018)16 | Brazil | Community trial | Children born in the year 2013 | 245/175 | 224/145 | 1 | 1 | 20–40 minutes | 20–40 minutes | 3 years | Mean (95% CI) of score ICDAS | 1.91, (1.18–2.64) conventional, 0.86, (0.56–1.16)–MI | An intervention based on the principles of MI style was more effective in reducing the number of surfaces affected by early childhood caries compared with conventional oral health education intervention. | |||||||||
| 7 | Naidu et al. (2015)19 | Trinidad | Cluster randomized controlled trial | 5–6 years | 25/21 | 54/20 | 4 | 1 | 30 minutes | 30 minutes | 4 months | Mean and SD of the questionnaire used for in-between snacking and frequency of toothbrushing | 10.55 (4.07)–traditional, 13.09 (1.44)–MI | 25/54 (46.3%)–traditional, 7/25 (28.0 %)–MI | 9/20 (45.0 %)–traditional, 9/21 (42.9 %)–MI | There was evidence that using an MI approach when delivering oral health information had a positive effect on parent/ caregiver, oral health knowledge, toothbrushing behavior, and oral health fatalism compared to traditional DHE. | |||||||
| 8 | Ismail et al. (2011)15 | Michigan, United States of America | Community trial | 0–5 years | 506/299 | 515/300 | 3 | 1 | 40 minutes | 40 minutes | 6 months and 2 years | ICDAS (IRR), questionnaire (OR) | 4.57–MI | 4.07–MI | 168/300 (56%)–traditional 183/299 (61.20%) | This study found that a single MI intervention may change some reported oral health behaviors, it failed to reduce the number of new untreated carious lesions. | |||||||
| 9 | Saengtipbovorn et al. (2017)20 * | Thailand | Randomized controlled trial | 6 months–5 years | 107/98 | 107/98 | 3 | 1 | 15 minutes | 10 minutes | 3 and 6 months | The mean difference between a cavitated and noncavitated, mean difference of plaque score | 0.184 (0.285) | 1.041 (0.383) | 0.160 (0.116) | 0.665 (0.097) | The combination of MI and caries risk assessment in one program decreased early childhood caries in preschool children. | ||||||
Intervention, MI (oral health education, through the specific goal of the importance of child's oral health and toothbrushing, and openly discussing concerns and obstacles in changing behavior and giving reinforcements at particular time intervals through posters, pamphlets, audio-visual aids, telephone, e-mails, letters); traditional oral health education (oral health instruction using posters, pamphlets, or any other aids without any reinforcement); outcomes assessed, PI (plaque index), GI (gingival index), DMFS (decayed, missed, filled permanent tooth surface); dmfs (decayed, missed, filled primary tooth surface); DMFT (decayed, missed, filled permanent tooth), ICDAS, Modified Radike criteria, etc., change in frequency of toothbrushing and in-between snacking using the questionnaire; * excluded from the meta-analysis
Effectiveness of MI
All the studies supported MI in improving children's oral health and mothers’ oral health-related behavior towards their children significantly, except for one study reported by Ismail et al.15 in 2011 that failed to reduce the number of new untreated carious lesions in children.
Dental Caries
Two studies reported by Beatriz et al.16 and Mauricio et al.17 were assessed for dental caries outcome (measuring ICDAS) using a fixed effect model, as the heterogeneity was found to be 0%. The meta-analysis pooled effects from 224 participants in the MI group and 192 in the traditional health education group. A significant difference was observed in dental caries favoring the MI group with a mean difference of −1.03(95% CI—−1.37–0.70) (p < 0.05) (Fig. 1) through a forest plot, thereby indicating that the incidence of Dental caries was less in children whose mothers received MI as compared to traditional health education.
Fig. 1.
Forest plot of dental caries
Frequency of Toothbrushing
There was no difference in the frequency of toothbrushing between the MI group and traditional health education group as obtained from pooled data of Ismail et al.15 and Kavita et al.18 with a total of 436 participants in the MI group and 428 in traditional health education group. A random effect model was used as the heterogeneity was found to be 96%. The pooled odds ratio was 1.69 (95% CI—0.68–4.25). The results indicated that the frequency of toothbrushing was improved in traditional education as compared to MI in oral health education. This result was not statistically significant (p = 0.26) (Fig. 2).
Fig. 2.
Forest plot of the frequency of toothbrushing
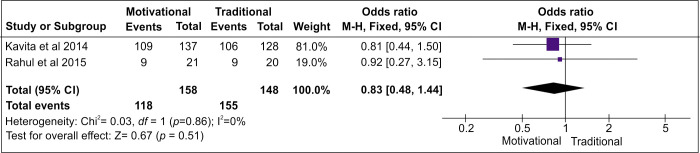
In-between Snacking
Data on in-between snacking from Kavita et al.18 and Rahul et al.,19 with 158 participants in the MI group and 148 in the traditional health education group, gave a pooled odds ratio of 0.83 with 95% CI—0.48–1.44 using fixed effect model (Fig. 3). This data too did not show a statistically significant difference (p = 0.51) between the MI group and traditional health education group thereby demonstrating MI and traditional health education to be comparable in the frequency of in-between snacking among children.
Fig. 3.
Forest plot of in-between snacking
Quality Evidence
Risk of bias (ROB) as assessed by the Cochrane ROB tool revealed that one study by Saengtipbovorn et al.20 was of low risk, two studies reported by Nomaire et al.21, Manchanda et al.18 were of moderate risk, while six studies by Gonzalez et al.,17 Weinstein et al.,9 Naidu et al.,19 Mohammadi et al.,22 Colvara et al.,16 and Ismail et al. 15 were of high risk (Fig. 4). The results obtained were irrespective of the risk involved in the studies.
Fig. 4.
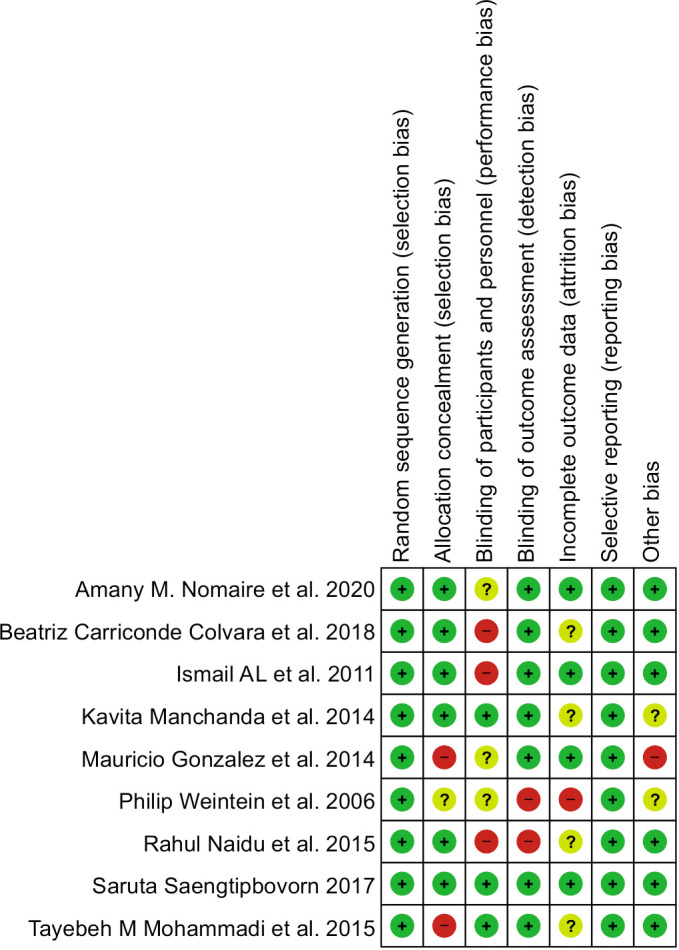
Risk of bias summary graph
Discussion
Motivational interviewing (MI) involves giving patients the autonomy to make their own decisions and change their overall behavior with their own acceptance. This technique has therefore increased the commitment of patients towards a change, unlike other techniques where they tend to cease their commitments as a reason for the forced change.23 The use of MI has been evident in alcohol and tobacco consumption cessation, but its effect on oral health, especially pediatric population, was not clear.24,25
The present systematic review and meta-analysis is one of its kind to represent oral health behavioral changes in children as an effect of MI compared to traditional health education among children's mothers. Overall, the quality of studies included in the review ranged from low to high risk as assessed with the Cochrane ROB tool results in significantly favoring MI, which were reported in five studies by Mohammadi et al.,22 Nomaire et al.,21 Manchanda et al.,18 Colvara et al.,16 Naidu R et al.19 while in one study Gonzalez et al.17 reported that MI is an effective and promising technique for establishing preventive behaviors, another study by Weinstein et al.9 reported that MI enhanced the preventive behavior of mothers of young children at high risk of developing caries, yet another study by Saengtipbovorn et al.20 demonstrated that combination of MI and caries risk assessment in one program, decreased early childhood caries in preschool children. The review reported only one study by Ismail et al.15 that did not favor MI and signified that a single MI intervention might change some reported oral health behaviors, but it failed to reduce the number of new untreated carious lesions among children.
Overall, the sample size in the intervention group at the last follow-up ranged from 21 to 299, while that in the traditional health education group ranged from 20 to 300. All the studies reported a loss of follow-up. It is important to note that the number of sessions for MI and traditional education displayed a great variation across the studies included. Almost all the studies in the present review conducted one session of traditional health education for mothers, while the MI sessions ranged from a minimum of one session in the Colvara et al.16 study to a maximum of seven in Mohammadi et al.22 and Gonzalez et al.17 studies. The only study with an equal session of interventions was Colvara et al.,16 representing that the intervention based on the principles of MI style was more effective in reducing the number of surfaces affected by early childhood caries compared with conventional oral health education. However, the duration of sessions for both MI and traditional education were the same ranging from 10 to 45 minutes across the studies.
Except for one study reported by Naidu et al.,19 all other studies provided outcome analysis at a minimum of 6 months follow-up. But overall, the follow-up period of all the studies was short to assess the actual effect in the long run. From the studies assessing pooled data on dental caries between the two interventions, both the studies used the ICDAS standard for assessment but one of the studies was of high risk. Similarly, one study (Manchanda et al.)18 was of moderate risk in pooled effect obtained on the frequency of toothbrushing, while one study (Naidu et al.)19 with high risk in pooled effect on in-between snacking. Both the parameters of in-between snacking and toothbrushing frequency were assessed by a questionnaire tool in the respective studies.
The results of the present review are comparable with the reviews conducted in the past.26 reported a meta-analysis on the effect of MI for parent involvement in order to improve health behavior and health outcome in the pediatric population. Various parameters considered were diet, reduced screen time, physical activity, and oral health. The improvement in pediatric oral health behavior in terms of reduced dental caries was evident. Another systematic review by Cascaes et al.27 analyzed the effectiveness of MI in improving oral health-related behaviors in terms of sugar consumption, use of fluoride, oral hygiene habits, and dental service utilization but failed to provide a definite conclusion because of an inadequate number of studies assessing outcome with the same standards.
The optimistic thing about MI is that the techniques are calibrated with the patient's level of readiness to change. All the educational approaches provided in MI are initiated only after recognizing that the patient is willing to hear and adapt to the change. Hence, even though the present review did not show a significant difference in the in-between snacking score and toothbrushing frequency between the MI and traditional technique, one can always choose MI considering its long-term advantage of intrinsic change on the patients.28
The review certainly has a few limitations, firstly; no sensitivity analysis was conducted that would provide pooled evidence of studies excluding the high ROB while including only low and moderate ROB studies. One reason for this could be the low number of included studies as per the eligibility criteria of the review that did not allow for further limiting the outcome based on the risk involved in the studies. The studies involved in the present review had small sample sizes and short follow-ups. Thus, the results should be concluded with caution, considering the limitations.
Conclusion
Considering the limitations of the review, MI proves to be an effective method in bringing changes in the attitude of mothers towards their children's oral health and thereby influencing behavioral changes among children towards the positive aspect when compared to the traditional way of health education. Dental caries were found to be significantly less among children of a group of mothers receiving MI, while in-between snacking and frequency of toothbrushing did not show a significant difference by MI over traditional health education method. Further analysis involving more studies of large sample size and low to moderate ROB are recommended.
Clinical Significance
MI can be considered an effective and feasible method for oral health education to mothers, which will, in turn, improve the oral health of their children.
Orcid
Purnima H Karande https://orcid.org/0000-0003-0443-6824
Vineet Vinay https://orcid.org/0000-0002-3354-2186
Ketaki B Bhor https://orcid.org/0000-0003-3847-4319
Kadambari A Ambildhok https://orcid.org/0000-0003-2696-1566
Amar K Shaw https://orcid.org/0000-0002-7785-9644
Footnotes
Source of support: Nil
Conflict of interest: None
Acknowledgments
The study was approved by the Institutional Ethical Committee and Scientific Advisory Committee, Sinhgad Technical Education Society's Sinhgad Dental Collage and Hospital, Pune, bearing Approval Number: SDCH/IEC/2020-21/42.
References
- 1.Frencken JE, Sharma P, Stenhouse L, et al. Global epidemiology of dental caries and severe periodontitis - a comprehensive review. J Clin Periodontol. 2017;44(18):S94–S105. doi: 10.1111/jcpe.12677. [DOI] [PubMed] [Google Scholar]
- 2.Anil S, Anand PS. Early childhood caries: prevalence, risk factors, and prevention. Front Pediatr. 2017;5:157. doi: 10.3389/fped.2017.00157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kassebaum NJ, Bernabé E, Dahiya M, et al. Global burden of untreated caries: a systematic review and metaregression. J Dent Res. 2015;94(5):650–658. doi: 10.1177/0022034515573272. [DOI] [PubMed] [Google Scholar]
- 4.Uribe SE, Innes N, Maldupa I. The global prevalence of early childhood caries: A systematic review with meta-analysis using the WHO diagnostic criteria. Int J Paediatr Dent. 2021;31(6):817–830. doi: 10.1111/ipd.12783. [DOI] [PubMed] [Google Scholar]
- 5.Kale SS, Kakodkar P, Shetiya SH, et al. Dental caries prevalence among 5- to 15-year-old children from SEAR countries of WHO: A systematic review and meta-analysis. Indian J Dent Res. 2019;30(6):937–947. doi: 10.4103/ijdr.IJDR_654_17. [DOI] [PubMed] [Google Scholar]
- 6.Genderson MW, Sischo L, Markowitz K, et al. An overview of children's oral health-related quality of life assessment: from scale development to measuring outcomes. Caries Res. 2013;47(Suppl 1(0 1):13–21. doi: 10.1159/000351693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Academy on Pediatric Dentistry Policy on early childhood caries (ECC): classifications, consequences, and preventive strategies, American Academy of Pediatrics. Pediatr Dent. 2008;30(7 Suppl):40–43. [PubMed] [Google Scholar]
- 8.Innes N, Evans D. Managing dental caries in children: improving acceptability and outcomes through changing priorities and understanding the disease. Br Dent J. 2009;206(10):549–550. doi: 10.1038/sj.bdj.2009.471. [DOI] [PubMed] [Google Scholar]
- 9.Weinstein P, Harrison R, Benton T. Motivating mothers to prevent caries: confirming the beneficial effect of counseling. J Am Dent Assoc. 2006;137(6):789–793. doi: 10.14219/jada.archive.2006.0291. [DOI] [PubMed] [Google Scholar]
- 10.Rollnick S. Behaviour change in practice: targeting individuals. Int J Obes Relat Metab Disord. 1996;20(1suppl):S22–S26. [PubMed] [Google Scholar]
- 11.Miller W, Rollnick S, editors. Motivational Interviewing: Helping People Change. 3rd edn. New York City: Guilford Press; 2013. [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–341. doi: 10.1016/j.ijsu.2010.02.007. 1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 13.Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions, The Cochrane Collaboration; ed., Version 5.1.0 [updated March 2011]. 2011. Available from. [Google Scholar]
- 14.Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane collaboration's tool for assessing risk of bias in randomized trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ismail AI, Ondersma S, Jedele JM, et al. Evaluation of a brief tailored motivational intervention to prevent early childhood caries. Community Dent Oral Epidemiol. 2011;39(5):433–448. doi: 10.1111/j.1600-0528.2011.00613.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Faustino-Silva DD, Colvara BC, Meyer E, et al. Motivational interviewing effects on caries prevention in children differ by income: a randomized cluster trial. Community Dent Oral Epidemiol. 2019;47(6):477–484. doi: 10.1111/cdoe.12488. [DOI] [PubMed] [Google Scholar]
- 17.González-Del-Castillo-McGrath M, Guizar-Mendoza JM, Madrigal-Orozco C, et al. A parent motivational interviewing program for dental care in children of a rural population. J Clin Exp Dent. 2014;6(5):e524–e529. doi: 10.4317/jced.51662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Manchanda K, Sampath N, Sarkar AD. Evaluating the effectiveness of oral health education program among mothers with 6-18 months children in prevention of early childhood caries. Contemp Clin Dent. 2014;5(4):478–483. doi: 10.4103/0976-237X.142815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Naidu R, Nunn J, Irwin JD. The effect of motivational interviewing on oral healthcare knowledge, attitudes and behaviour of parents and caregivers of preschool children: an exploratory cluster randomized controlled study. BMC Oral Health. 2015;15(101) doi: 10.1186/s12903-015-0068-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saengtipbovorn S. Efficacy of motivational interviewing in conjunction with Caries Risk Assessment (MICRA) Programmes in improving the dental health status of preschool children: a randomized controlled trial. Oral Health Prev Dent. 2017;15(2):123–129. doi: 10.3290/j.ohpd.a37924. [DOI] [PubMed] [Google Scholar]
- 21.Nomair AM, Hamza MA, Abdelaziz WE. Effectiveness of motivational interviewing and games on oral hygiene of children and oral health knowledge, attitude and behavior of mothers: a randomized controlled clinical trial. Alex Dent Jour. 2020;46(2):191–196. doi: 10.21608/ADJALEXU.2020.23531.1043. [DOI] [Google Scholar]
- 22.Mohammadi TM, Hajizamani A, Bozorgmehr E. Improving oral health status of preschool children using motivational interviewing method. Dent Res J (Isfahan) 2015;12(5):476–481. doi: 10.4103/1735-3327.166231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Miller WR, Benefield RG, Tonigan JS. Enhancing motivation for change in problem drinking: a controlled comparison of two therapist styles. J Consult Clin Psychol. 1993;61(3):455–461. doi: 10.1037//0022-006x.61.3.455. [DOI] [PubMed] [Google Scholar]
- 24.Riper H, Andersson G, Hunter SB, et al. Treatment of comorbid alcohol use disorders and depression with cognitive-behavioural therapy and motivational interviewing: a meta-analysis. Addiction. 2014;109(3):394–406. doi: 10.1111/add.12441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Heckman CJ, Egleston BL, Hofmann MT. Efficacy of motivational interviewing for smoking cessation: a systematic review and meta-analysis. Tob Control. 2010;19(5):410–416. doi: 10.1136/tc.2009.033175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Borrelli B, Tooley EM, Scott-Sheldon LA. Motivational interviewing for parent-child health interventions: a systematic review and meta-analysis. Pediatr Dent. 2015;37(3):254–265. [PubMed] [Google Scholar]
- 27.Cascaes AM, Bielemann RM, Clark VL, et al. Effectiveness of motivational interviewing at improving oral health: a systematic review. Rev Saude Publica. 2014;48(1):142–153. doi: 10.1590/s0034-8910.2014048004616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boardman T, Catley D, Grobe JE, et al. Using motivational interviewing with smokers: do therapist behaviors relate to engagement and therapeutic alliance? J Subst Abuse Treat. 2006;31(4):329–339. doi: 10.1016/j.jsat.2006.05.006. [DOI] [PubMed] [Google Scholar]