Abstract
Background
Taurodontism is an anomalous developmental condition where the coronal portion of the tooth is enlarged while the radicular portion is compromised. This may have important clinical implications while considering endodontic or exodontic procedures which may affect the technique of the treatment or its prognosis.
Case Report
This article describes the case of a 4-year-old female girl with molars exhibiting taurodontism with its clinical management and a review of this unique clinical condition.
Conclusion
This case report and review summarizes the diagnosis, classification, clinical management challenges and comprehensive rehabilitation of taurodontism in primary teeth.
How to cite this article
Gupte MP, Mistry LN, Jawdekar A. Challenges and Treatment Considerations with Comprehensive Rehabilitation of a Case of Taurodontism in Primary Dentition: A Case Report and Review. Int J Clin Pediatr Dent 2023;16(3):510-514.
Keywords: Case Report, Endodontic Management, Molars, Primary Teeth, Review, Taurodontism
Introduction
Taurodontism is a combination of two Latin words; tauro meaning bull and dentis meaning tooth.1 Taurodontism is a developmental anomaly of the tooth which features morphoanatomical changes in which the body of the tooth is enlarged at the expense of roots.2
Taurodontism is caused due to the inability of Hertwig's epithelial root sheath to move inward, leading to the failure of the epithelial diaphragm to form a bridge prior to dentin deposition resulting in large pulp chambers. Taurodontism has been associated with certain syndromes such as Down's syndrome, Klinefelter's syndrome, and tricho–dento–osseous syndrome, but is most often seen as an independent anomaly.2
Based on our literature search, there are few reported cases of taurodontism in the primary dentition. There are six reported cases of taurodontism in the primary dentition of which two papers have reported the prevalence and four papers have discussed the management of teeth having taurodontism.3–8 This paper reports a case of bilateral taurodontism in primary first and second molars. Thus, the aim of this paper is to describe the condition, classification, and treatment considerations of taurodontism in the primary dentition.
CASE DESCRIPTION
A 4-year-old girl reported to the Department of Pediatric and Preventive Dentistry at Bharati Vidyapeeth Dental College and Hospital, Navi Mumbai, India with a chief complaint of pain in the lower left and right back tooth region of the jaw for 1 week. The pain was intermittent, aggravated during meals, and gave a positive history of nocturnal pain suggestive of irreversible pulpitis. Medical history was noncontributory.
The patient was uncooperative on the first visit and was rated definitely negative according to Frankl's behavior rating scale. The parent gave a history of past negative dental experiences 1 week back in relation to treatment for the same chief complaint.
Intraoral examination revealed a complete set of deciduous dentitions with no soft tissue abnormality and a flush terminal molar relation. Superficial carious lesions were observed with respect to 51 and 61 (Fig. 1A); 73, 74, 75, 84, and 85 (Fig. 1C) showed deep carious lesions (Fédération Dentaire Internationale system of teeth nomenclature) (Fig. 1).
Figs 1A to C.
(A) Clinical frontal view showing proximal caries with 51 and 61 (Preoperative); (B) Maxillary occlusal view; (C) Mandibular occlusal view; arrows displaying molars affected by taurodontism in 74,75,84 and 85 (Preoperative)
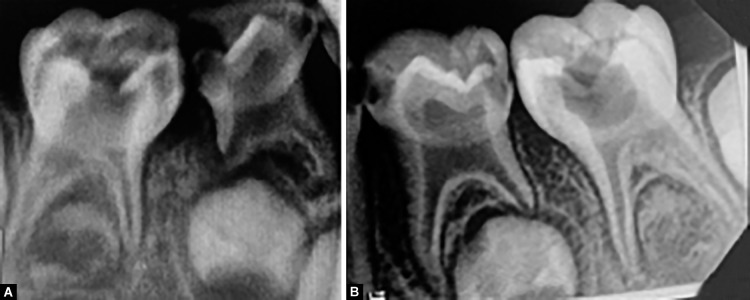
Intraoral periapical radiographs revealed caries involving the pulp in relation to 74, 75, 84, and 85 (Fig. 2). Resorption was observed on the distal root of 84 (Fig. 2A). Interestingly, there were large pulp chambers and small roots in relation to 74, 75, 84, and 85, suggestive of taurodontism. Based on Shifman and Chanannel's classification of taurodontism, three variables are measured, variable 1 is the height of the pulp chamber, variable 2 is the distance between the roof of the pulp chamber and the root's apex and variable 3 is the distance between the cementoenamel junction to the floor of the pulp chamber.9 After obtaining the values of all the variables, the degree of taurodontism is calculated using the following formula9:
Figs 2A and B.
(A) Intra-oral periapical radiograph showing taurodontism in 84 and 85 (Preoperative); (B) Intra-oral periapical radiograph showing taurodontism with 74 and 75 (Preoperative)
T1 = Variable 1 × 100/Variable 2
Taurodontism is diagnosed when T1 is greater than 20 and variable 3 exceeds 2.5 mm. Based on the calculations according to Shifman and Chanannel, 74, 75, 84, and 85 were classified as hypertaurodontism.9 Extraoral and general examination did not reveal any significant findings that could point to any syndrome and was associated as an independent anomaly (Figs 2 and 3).
Fig. 3.
Radiograph explaining the classification of taurodontism
Based on the clinical and radiographic diagnosis a tentative treatment plan was made. Restoration of 51 and 61; pulp therapy with respect to 73, 74, 74, and 85; extraction with respect to 84 followed by space maintainer was decided, in accordance with parents and after obtaining consent.
On the second visit, behavior modification and restoration of 51 and 61 were carried out. Modeling and Tell, Show, and Do was used for behavior modification. Caries was excavated using small round bur BR-45 (Mani, Inc., Utsunomiya, Japan) and was restored using composite (3M ESPE Filtek™ Z350 XT, United States of America) using a standard protocol.
On the third visit, a pulpectomy with 75 was done. Rubber dam isolation could not be achieved since the patient was not cooperative. Local anesthesia [2% lignocaine hydrochloride with 1:2,00,000 adrenaline (Lignocad Adr Cadilla Pharmaceuticals Ltd., India)] was administered using the inferior alveolar nerve block technique. Access opening was done using a large round bur BR-31 (Mani, Inc., Utsunomiya, Japan), on gaining access to the pulp chamber, the hyperemic pulp was observed. Pulp tissue was extirpated using a barbed broach. The working length was determined using the radiographic method. Biomechanical preparation was done using 21 mm K-files (Mani, Inc., Utsunomiya, Japan) up to #30 K-file. H-files (Mani, Inc., Utsunomiya, Japan) were used for circumferential filing. Copious irrigation with normal saline was done. After drying the canals, canals were obturated using calcium hydroxide and iodoform (Metapex, Meta Biomed, Korea). Postobturation restoration was done using glass ionomer cement (3M Ketac™ Molar, India).
On the fourth visit, after administration of local anesthesia using the inferior alveolar nerve block technique, pulpectomy was done with 85 similar to 75. On the same day, extraction with 84 was performed. After the reflection of the flap, the tooth was luxated with the help of a straight elevator thus minimizing the use of forceps. After achieving sufficient mobility, forceps were introduced for completing the procedure.
On the next visit, the patient showed acceptance towards the operator and dental procedures. Rubber dam application was achieved and pulpectomy with 73 and 74 were performed under local anesthesia using the inferior alveolar nerve block technique. A temporary restoration was placed with respect to 73 until the cementation of a preformed stainless steel crown with 74.
Preformed stainless steel crown (3M ESPE™ Stainless Steel Primary Molar Crowns, United States of America) with 85 was cemented using type I glass ionomer cement (GC Gold label Type 1 Luting and Lining Cement, Japan). Tooth preparation for 74 and 75 was done simultaneously and preformed stainless steel crowns were cemented. Postobturation restoration with 73 was done after obtaining a distal contact with 74 using composite (Fig. 4).
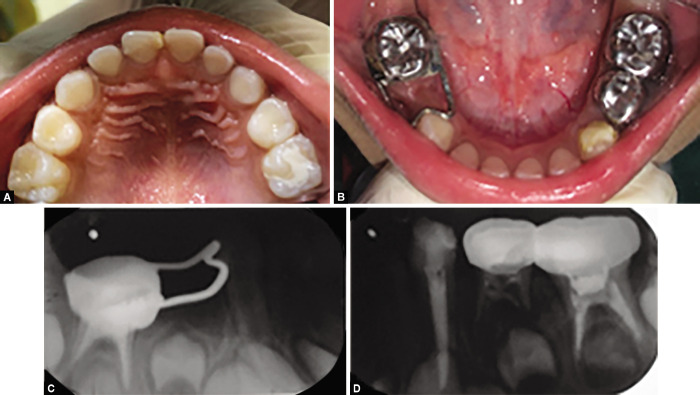
Figs 4A to C.
Postoperative radiographs (A) Intra-oral periapical radiograph showing extraction with 84 region and pulpectomy with stainless steel crown with respect to 85 (Postoperative); (B) Intra-oral periapical radiograph showing pulpectomy of 73 (Postoperative); (C) Intra-oral periapical radiograph showing pulpectomy with stainless steel crown with respect to 74 and 75 (Postoperative)
Space management was done using a band and loop space maintainer over a crown with 85. A band was adapted over the crown. A band and loop was fabricated and cemented over the crown (Figs 5 and 6).
Fig. 5.

Postoperative radiograph showing crown band and loop
Figs 6A to E.
Postoperative clinical photographs (A) Frontal view showing restoration with 51 and 61 (Postoperative); (B) Maxillary occlusal view (Postoperative); (C) Mandibular view showing crown band and loop with 85; Stainless steel crown with 74 and 75; Post obturation restoration with 73 (Postoperative). (D) Right lateral view (Postoperative); (E) Left lateral view (Postoperative)
Follow-up was done after 6 months. The patient was asymptomatic and was rated definitely positive according to Frankl's behavior rating scale. Clinically a pit and fissure caries were observed with 65 at follow-up. Caries was excavated and restored using glass ionomer cement. Intraoral periapical radiograph revealed resorption of Metapex with 74. No such resorption was seen with respect to 73, 75, and 85 (Fig. 7).
Figs 7A to D.
Follow-up at 6 months. (A) Maxillary occlusal view (Follow-up); (B) Mandibular occlusal view (Follow-up); (C) Intra-oral periapical radiograph with 84,85 region (Follow-up); (D) Intra-oral periapical radiograph with 73,74 and 75 region (Follow-up)
Discussion
Taurodontism is a morphological developmental anomaly characterized by an enlarged crown structure at the expense of roots. Gorjanovic-Kramberger was the first to describe taurodontism in 1908, and Sir Arthur Keith in 1913 coined the term ”taurodontism.”2 Widdowson defined taurodontism as the “vertical deepening of the pulp cavity at the expense of the roots.”1
Prevalence of taurodontism has been reported to be 0.3% in primary teeth with a male predilection, however, it was diagnosed in a female patient in the present case.10 Within the limitation of our literature search only four cases of taurodontism have been reported.
In 1928, based on the relative displacement of the floor of the pulp chamber, Shaw classified taurodontism as hypotaurodontism, mesotaurodontism, and hypertaurodontism.10 In this present case, the mandibular first and second deciduous molars were classified as hypertaurodont based on Shifman and Chanannel's criteria.9
Diagnosis of this condition is completely based on radiographs as the external morphology often resembles the normal anatomy. The pulp chamber appears enlarged with the bifurcation or trifurcation with only a few millimeters above the root apices.9 In the present case, taurodontism was diagnosed based on the radiographic evaluation. Based on the clinical and radiographical features along with the history of pain it was diagnosed as chronic irreversible pulpitis with 73, 74, 75, and 85.
Taurodontism may often complicate dental procedures due to its altered morphology. The pulp chambers are larger and the apical positioning of the pulp canal orifices makes it difficult for the pulpotomy procedure. Also, there is an increased incidence of bleeding making hemorrhage control difficult.10 Although the prevalence of taurodontism is low, the treatment protocol must be made considering the aforementioned challenges, especially in procedures involving the pulp.
Endodontic treatment often poses certain challenges due to the large pulp chamber, apical position of furcation, access opening, negotiation, and instrumentation of the root canals can often be difficult. Increased hemorrhage can be mistaken for perforation.10 In the present case, single visit pulpectomies with 73, 74, 75, and 85 were done. Ethylenediaminetetraacetic acid was copiously used with every file inserted in the canal to achieve maximum separation of pulp tissue from the radicular dentinal wall, in absence of sodium hypochlorite to facilitate pulp extirpation. Sodium hypochlorite was used minimally as an irrigant as it is difficult to control in the radicular space due to the very short canal size. Metapex was used as an obturating material as materials like zinc oxide eugenol in such bulk may resorb at a slower rate which may delay the normal exfoliation of the teeth.11 Also zinc oxide eugenol becomes difficult to contain in canal space which may cause hypoplasia in succedaneous teeth.
Extraction of teeth with taurodontism may be complicated due to the shift in the furcation in the apical third hence extent of flap reflection is more than normal teeth causing more damage to the periodontium and also difficulty in placing the beaks of the forceps.12 Some authors believe extraction of teeth with taurodontism is less difficult as a large body with a little surface is embedded in the alveolus unless the roots are divergent.12 In the present case, the right mandibular first molar was extracted as resorption with the distal root was noted. The tooth was sufficiently luxated using a straight elevator before the introduction of forceps, thus minimizing the damage.
Preformed stainless steel crowns were cemented for all the pulpectomized molars. For space management with the loss of the right mandibular first molar crown band and loop were preferred over crown and loop. Crown band and loop is a variation of band and loop appliance. For the crown and loop appliance, it requires preparation of the abutment tooth followed by soldering of the loop directly to the crown. In case of a solder joint failure with a crown and loop appliance, it is required to cut off the crown, a new crown to be fitted and the wire resoldered. Thus it is convenient to restore the abutment tooth with a stainless steel crown and then fabricate a band and loop appliance that fits the crown.13
At 6 month follow-up, resorption of Metapex was seen from the canals of 74, clinically the tooth had no sign of mobility and was asymptomatic. Radiographically some radiolucency can be seen, hence the tooth is kept under observation till further follow-up, and subsequently, SOS extraction may be done followed by appropriate space management, depending on the age of the patient. The resorption of Metapex could be attributed to persistent inflammation in the periradicular region.
Conclusion
Taurodontism offers its share of complexities in its management, such as large pulp chambers, and altered root size, making root canal-related therapy or extraction challenging. Emphasis should be made on preventive care so as to avoid the difficulties encountered in the management of teeth with taurodontism. For the management of such conditions, diagnosis is very important, preoperatively, following which guidelines as mentioned in this article can be followed to minimize difficulty and complications.
Clinical Significance
Taurodontism is a rare developmental anomaly in primary dentition which affects the morphological features. Taurodontism features an enlarged crown structure at the expense of the root size. The deviation from the normal anatomical structure may offer different challenges in clinical case management, especially during endodontic therapy. This case report describes the diagnosis, classification, different challenges which can be encountered, and comprehensive rehabilitation of a case of taurodontism in the primary dentition.
Footnotes
Source of support: Nil
Conflict of interest: None
Patient consent statement: The author(s) have obtained written informed consent from the patient's parents/legal guardians for publication of the case report details and related images.
References
- 1.Mena CA. Taurodontism. Oral Surg Oral Med Oral Pathol. 1971;32(5):812–823. doi: 10.1016/0030-4220(71)90308-2. [DOI] [PubMed] [Google Scholar]
- 2.Dineshshankar J, Sivakumar M, Balasubramanium AM, et al. Taurodontism. J Pharm Bioallied Sci. 2014;6(Suppl 1):S13–S15. doi: 10.4103/0975-7406.137252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhat SS, Sargod S, Mohammed SV. Taurodontism in deciduous molars: a case report. J Indian Soc Pedod Prev Dent. 2004;22(4):193–196. [PubMed] [Google Scholar]
- 4.Jogendra Sai Sankar A, Sreedevi E, Satya Gopal A, et al. A rare condition of bimaxillary primary molar taurodontism. J Dent. 2017;18(2):153–156. [PMC free article] [PubMed] [Google Scholar]
- 5.Vashisth P, Dwivedi S, Arora S, et al. Multiple bilateral taurodontic teeth in primary dentition: a case report. Int J Clin Pediatr Dent. 2013;6(2):132–133. doi: 10.5005/jp-journals-10005-1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Srivathsa SH. Taurodontism of deciduous molars: report of two cases. SRM J Res Dent Sci. 2014;5(2):111–113. doi: 10.4103/0976-433X.132084. [DOI] [Google Scholar]
- 7.Birajee G, Dali M, Shrestha S, et al. Taurodontism in deciduous molars: a report of a rare case. J Interdiscip Dent. 2017;7(2):69–71. doi: 10.4103/jid.jid_54_16. [DOI] [Google Scholar]
- 8.Matondkar SP, Yavagal C, Anegundi R. Taming the bull by its horns: a case report on bilateral primary tooth taurodontism. J Ad Clin Res Insights. 2018;5(6):200–202. doi: 10.15713/ins.jcri.244. [DOI] [Google Scholar]
- 9.Shifman A, Chanannel I. Prevalence of taurodontism found in radiographic dental examination of 1,200 young adult Israeli patients. Community Dent Oral Epidemiol. 1978;6(4):200–203. doi: 10.1111/j.1600-0528.1978.tb01150.x. [DOI] [PubMed] [Google Scholar]
- 10.Manjunatha BS, Kovvuru SK. Taurodontism-a review on its etiology, prevalence and clinical considerations. J Clin Exp Dent. 2010;2(4):e187–e190. doi: 10.4317/jced.2.e187. [DOI] [Google Scholar]
- 11.Yeh SC, Hsu TY. Endodontic treatment in taurodontism with Klinefelter's syndrome:a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88(5):612–615. doi: 10.1016/s1079-2104(99)70094-6. [DOI] [PubMed] [Google Scholar]
- 12.Durr DP, Campos CA, Ayers CS. Clinical significance of Taurodontism. J Am Dent Assoc. 1980;100(3):378–381. doi: 10.14219/jada.archive.1980.0100. [DOI] [PubMed] [Google Scholar]
- 13.Pinkham JR, Casamassimo PS, Fields HW, McTigue DJ, Nowak A. Pediatric dentistry. Infancy through adolescence. 2005 Sep 20;4. [Google Scholar]