Abstract
Aim
The aim of this case series is to provide a detailed account of pediatric cases with bifid mandibular canal (BMC) along with clinical implications.
Background
The prevalence of BMC on panoramic radiographs has been reported to be 0.03–1.90% in adults. Only one study reported prevalence of BMC in children based on cone-beam computed tomography (CBCT) images. As CBCT images are not routinely prescribed in children, it is important to understand if panoramic radiographs provide a valuable tool to diagnose BMC in children.
Case description
This case series provides a review of three cases of nonsyndromic, bilateral BMC, and associated radiculomegaly affecting mandibular permanent first molars in children during the mixed dentition stage. An overview of clinical implications of BMC in children is also discussed to help clinicians provide appropriate dental care and anticipatory guidance.
Conclusion
Bifid mandibular canal (BMC) has never been reported in children during mixed dentition stage based on panoramic radiographs. This is the first case series reporting BMC and associated dental anomalies in children.
Clinical significance
This case series will help clinicians in diagnosing BMC during mixed dentition stage and understand its clinical implications. Additionally, this case series will help define future cross-sectional studies evaluating BMC and associated dental anomalies in children.
How to cite this article
Puranik CP, Chandki R, Mladenovic R, et al. Bifid Mandibular Canals: A Pediatric Case Series with Clinical Implications. Int J Clin Pediatr Dent 2023;16(3):547-549.
Keywords: Accessory mandibular canal, Bifid mandibular canal, Mandibular canal variations, Panoramic radiography, Retromolar canal, Radiculomegaly
Background
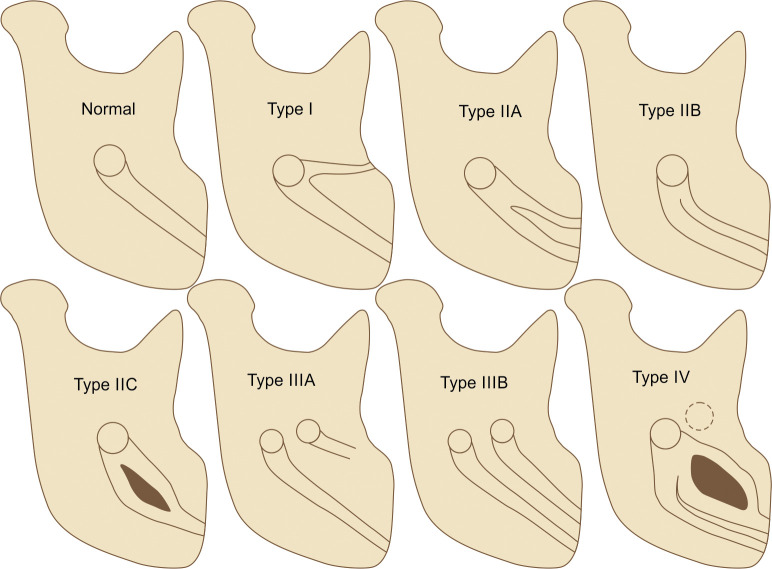
The mandibular canal is a bilateral anatomical structure that traverses the mandible and houses inferior alveolar neurovascular structures.1 Anatomic variations, such as bifid or trifid mandibular canals have been reported in the past.1Figure 1 provides the anatomic variations in the mandibular canal with modified Langlais classification for each side.2 The prevalence of BMC has been reported to be 0.03–65.0% depending on the various populations and radiographs studied.2,3 Majority of the reported cases used panoramic or CBCT images from adults.1–3 Only one group reported prevalence of BMC in children based on CBCT images.4 However, there are no reported cases of BMC during mixed dentition stage in children using panoramic radiographs. Capturing CBCT images is not a standard in pediatric dental care. As panoramic radiographs are routinely captured, it is important to diagnose BMC on panoramic radiographs. This case series provides a review of three cases of nonsyndromic, bilateral BMC in children during mixed dentition stage and associated dental anomalies based on panoramic radiographs. This case series also provides clinical implications of BMC for comprehensive dental care and anticipatory guidance (Fig. 2).
Fig. 1.
Modified Langlais classification of BMC based on panoramic radiographs. Normal—single foramen in ramus and one canal traversing the ramus and body of the mandible. Type I—single foramen and two canals in the ramus with one ending distal to the mandibular molars (retromolar canal) and other traversing the body of the mandible. Type IIA—single foramen and two separate canals in the ramus and two separate canals traversing the body of mandible. Type IIB—single foramen and two fused canals in ramus and traversing the body of mandible. Type IIC—single foramen and two distinct canals in the ramus fusing as a single canal to traverse the body of the mandible. Type IIIA—two foramens and two distinct canals in ramus, but only one canal traverses the body of the mandible while the other ends distal to the mandibular molars (retromolar canal). Type IIIB—two foramens and two distinct canals in the ramus and two distinct canals traversing the body of the mandible. Type IV—one or two foramens and three canals in the ramus traversing as one or multiple canals the body of the mandible.
Fig. 1.
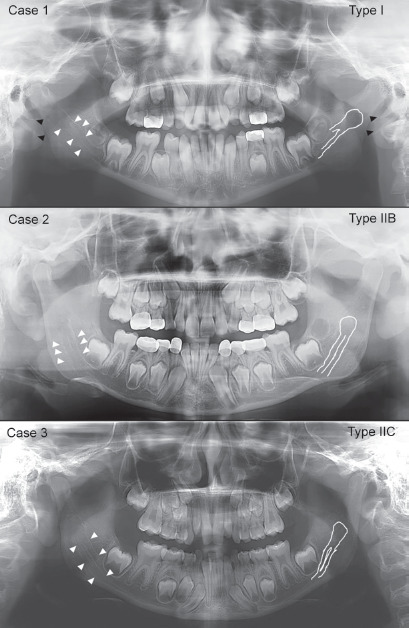
Nonsyndromic, bilateral BMC in three cases. Case 1 with type I canal morphology, case 2 with type IIB canal morphology, and case III with type IIC canal morphology. All three cases demonstrated radiculomegaly of mandibular first permanent molars. Case 3 demonstrated taurodontism of all first permanent molars. (Full white lines demonstrated the BMC on the left side while the white arrows indicated BMC on right side of the mandible. Black arrows point to the bifid styloid processes)
Case Description
All three cases were reported to the Children's Hospital Colorado's dental clinic for routine care. All three cases were healthy with normal height-weight (20–65th percentile) and were designated as high caries risk. The panoramic radiographs were taken at dental age of 8. The Institutional Review Board approved the study evaluating BMC in children (21-2981).
Case I was a 9-year-old Hispanic female with nonsyndromic, bilateral type I BMC associated with radiculomegaly affecting mandibular first permanent molars [root-crown-ratio (RCR) of ≥3)]. Additional dental findings included peg-shaped maxillary lateral incisors, rotated #35, rotated and blocked out #45, and bifid styloid processes. The second case was an 8-year-old Hispanic male with nonsyndromic, bilateral type IIB BMC along with radiculomegaly affecting mandibular first permanent molars (RCR of ≥3). The third case was an 8-year-old African American male demonstrating nonsyndromic, bilateral type IIC BMC. The third case, too, demonstrated radiculomegaly affecting mandibular first permanent molars (RCR of ≥2.7), along with taurodontism affecting all permanent first molars.
Discussion
During embryonic development, the nerves supplying three different types of mandibular teeth fuse to form one single nerve that is housed in one mandibular canal along with the vasculature.1,4 BMC results from the lack of incomplete fusion of these nerves.1 Although anatomic variations in the mandibular canal configuration are common, with BMC, it is highly unpredictable as to which canal houses the neurovascular structures.3,4 While BMC is unique, it has been the least explored entity in pediatric dental practice. This is because the diagnosis of BMC on panoramic radiographs, especially during mixed dentition stage, is challenging.4 Additionally, the developing tooth buds in the mandibular arch may prevent clear visualization of mandibular canal.1
In adults, the prevalence of BMC based on CBCT (10.2–65.0%) is higher than in panoramic radiographs (0.03–1.9%).3 In children, there is only one study that reported a 27% prevalence of BMC based on CBCT from 63 children.4 The buccolingual positioned BMC is difficult to diagnose based on panoramic radiographs. Hence, CBCT may be valuable for such types of BMCs.3 However, the low incidence of buccolingual positioned BMC (1.6–2.8%)3,4 and radiation concerns for CBCT in healthy patients make panoramic radiographs a valuable tool for diagnosing BMC in children.2 Our cases reinforce the value of panoramic radiographs for diagnosing BMC in children, even during the mixed dentition stage.
A recent study reported that the mandibular nerve position could impact the eruption of mandibular molars.5 This case series highlights the association of BMC with idiopathic root malformation (radiculomegaly) for all three cases affecting mandibular first permanent molars. Additionally, one case demonstrated taurodontism of permanent first molars. While ethnic variations are common, no gender differences in BMC are reported.3 Therefore, a comprehensive cross-sectional study is required to evaluate the association between BMC and dental anomalies affecting shape, position, or number of teeth.
Although BMC has not been commonly reported in children, its implications are overreaching in pediatric dental practice. Of particular concern is the high frequency of inferior alveolar nerve (IAN) canal block failure due to BMC, which can impact operative and surgical procedures such as restorations, crowns, pulp therapy, and extractions. In case of IAN block failure, the Gow-Gates or Vazirani–Akinosi technique can be used for effective IAN block.2 Extractions of third molars in BMC cases can lead to paresthesia, excessive bleeding, hematoma, or traumatic neuroma.2,3 In case of trauma, presence of BMC in children can affect stabilization of mandibular fracture.2,4 Similarly, surgical procedures involving mandibular osteotomy and advancement would require special care.2,4 Orthodontic movement of mandibular molars may cause nerve impingement and paresthesia. Although of less concern in pediatric dental practice, implant placement needs diligent planning in cases with BMC.2 Hence, although limited, panoramic radiographs provide an indication of BMC for appropriate case planning and delivery of anticipatory guidance.
Clinical Significance
Bifid mandibular canal (BMC) occurs more frequently in children than commonly perceived.
Panoramic radiographs have a diagnostic value in detecting BMC in children during mixed dentition stage.
The presence of BMC in children can lead to IAN block failure and can impact restorative and surgical care leading to complications, such as paresthesia, excessive bleeding, or traumatic neuroma.
Orcid
Chaitanya P Puranik https://orcid.org/0000-0002-6500-0664
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Valenzuela-Fuenzalida JJ, Cariseo C, Gold M, et al. Anatomical variations of the mandibular canal and their clinical implications in dental practice: a literature review. Surg Radiol Anat. 2021;43(8):1259–1272. doi: 10.1007/s00276-021-02708-7. [DOI] [PubMed] [Google Scholar]
- 2.Langlais RP, Broadus R, Glass BJ. Bifid mandibular canals in panoramic radiographs. J Am Dent Assoc. 1985;110(6):923–926. doi: 10.14219/jada.archive.1985.0033. [DOI] [PubMed] [Google Scholar]
- 3.Zhou X, Gao X, Zhang J. Bifid mandibular canals: CBCT assessment and macroscopic observation. Surg Radiol Anat. 2020;42(9):1073–1079. doi: 10.1007/s00276-020-02489-5. [DOI] [PubMed] [Google Scholar]
- 4.Orhan AI, Orhan K, Aksoy S, et al. Evaluation of perimandibular neurovascularization with accessory mental foramina using cone-beam computed tomography in children. J Craniofac Surg. 2013;24(4):e365–369. doi: 10.1097/SCS.0b013e3182902f49. [DOI] [PubMed] [Google Scholar]
- 5.Lee E, Jeong T, Shin J. Positional differences of the mandibular canal in relation to permanent mandibular first molars with eruption disturbances in children. Children (Basel) 2020;7(11):206. doi: 10.3390/children7110206. [DOI] [PMC free article] [PubMed] [Google Scholar]