Abstract
Inflammatory bowel disease (IBD) is a term for two autoimmune diseases encompassing Crohn’s disease (CD) and ulcerative colitis (UC) which are lifelong diseases affecting more than 3 million adults (1.3%) in the United States. IBD is characterized by chronic inflammation of the whole digestive system which results in damage to the gastrointestinal (GI) tract. IBD often emerges during adolescence and young adulthood. Maternal morbidity includes physical and psychological conditions that result from or are aggravated by pregnancy and have an adverse effect on a woman’s health, the baby’s health or both. Some women have health challenges that arise before or during pregnancy that could lead to complications. It is recommended for women to receive health care counseling before and during pregnancy. Compared to other developed countries, the United States has the highest rate of women dying of pregnancy related complications. During the past 25 years maternal mortality has been getting worse. African American women (AAW) with and/or without IBD are dying at significantly higher rates than other groups. This is linked to several factors, i.e., systemic, institutionalized, and structural racism in health-care delivery and subsequent toxic stress from people’s lived experiences of racism, limited knowledge about healthcare system function, lack of access to healthcare, (inclusiveness and insurance policies) all of which negatively impact these patients. African Americans (AAs) are also up to three times as likely to experience severe maternal morbidity: unexpected outcomes of labor and delivery, deficient or lacking prenatal care and social determinants of health like lack of transportation, adequate employment, limited literacy, and limited healthcare access contribute to poor health outcomes. Studies on IBD patients indicate Medicaid expansion is associated with reduced rates of maternal morbidity, particularly for African American Women (AAW) and increased access to preconception and prenatal services that make pregnancy and childbirth safer for parent and baby. Herein we examine the physiological changes of pregnancy in patients diagnosed with inflammatory bowel disease and their relationship perinatal outcomes and parenthood.
Keywords: Pregnancy, inflammatory bowel disease, Healthcare system inclusiveness, insurance policies, systemic-institutionalized-structural-racism
1. Introduction
Inflammatory Bowel Disease (IBD) encompasses two medically unsolved gastrointestinal disorders i.e., ulcerative colitis (UC) and Crohn’s disease (CD) and it presents with prolonged chronic relapsing and remitting inflammation of the digestive tract system.[1–5] The aetiopathogenesis of IBD remains enigmatic but is believed to be due to multifactorial interplay between Western lifestyle, genetically susceptible individuals, the immune system, the intestinal change in microbiome symbiotic relationship (dysbiosis/dysbacteriosis), pollution, changing hygiene status, socioeconomic status and several other environmental exposure factors.[6,7] The key differences between UC and CD is in tissue inflammation, damage, and prognosis, which suggest distinctive enteropathogenic processes responsible for their respective features, which at times may be challenging to interpret clinically and/or histologically.[8]. Typically, intestinal wall thickening is segmental in CD but continuous in UC.[9,10] UC causes inflammation and ulceration of the mucosal and, to a lesser degree, the submucosal lining of the colon and rectum.[9] Furthermore, CD differs from UC in that it may cause inflammation deeper within all layers of GI tract (transmural inflammation and skip lesions) and also may affect other non-GI organs through fistulation.[11,12] Unfortunately, these features are obscure during the prodromal stages of the disease, confounding the treatment regimens.[9,13].
The incidence of IBD is alarmingly evolving in young adults worldwide.[6,7] IBD incidence and prevalence is now contemplated to be an emergent global disease with health-care costs rising exponentially.[6,14–16] The burden of IBD varies in different countries and locations, especially when compared between resource-limited,[16–31] and rich countries.[32,33] Estimated data suggest that 25% - 30% of cases with CD and 20% of patients with UC present early in life during adolescence and young adulthood.[2,34–42] The magnitude of racial/ethnic and regional differences in the prevalence of IBD in the United States remains largely obscure warranting additional research.[43,44] Until recently, IBD has predominantly affected whites, particularly Ashkenazi Jews but over the last three decades, IBD has “emerged” in minority communities.[44–49]
IBD patients may have questions about their fertility especially related to the effects of their medications and disease itself. Even more concerns are raised about the pregnancy course and their baby’s safety while having this chronic intestinal condition. The risks associated with IBD in pregnancy are significant numerous, including miscarriage, small-for-gestational-age infant, premature delivery, poor maternal weight gain, insomnia, and preeclampsia. Further, complications of labor and delivery include, placental abruption, and increased probability of cesarean delivery.[50–58] During preconception counseling is paramount, potential for parents to get best maternal and infant health picture prediction which provides an opportunity to focus on the benefits of controlling disease activity. This preconception counseling is lacking for minority populations, especially AAW. A recent survey of adult gastrointestional (GI) program directors and trainees in the United States, reported that only one third of the trainees were satisfied with their level of IBD exposure, while more than half were uncomfortable dealing with IBD special situations including the management of pouch, stoma, pregnancy or postoperative patients.[29,30] Involving a maternal-fetal medicine specialist early in the conversation provides more confidence for the patients as they make decisions about IBD management. The challenge of improving care to the AAW with IBD is best met with the power of online information, collaboration, and shared decision-making.[31] Web-based resources were the first choice, more than any other, as an information aid for IBD clinical care and were selected by almost half of the trainees.[29,30]
Understanding the perinatal health care patterns of AAW with IBD patients will prepare us to manage the burden of IBD over time in this population. This review highlights a comprehensive, updated overview of the literature, the relative safety of medications used to treat IBD before, during and after pregnancy and breastfeeding, and summarizes the updated recommendations for immunosuppressant and biologics/ biosimilars to establish the current available perinatal IBD care in the AAW, contrast it with the increase in IBD and forecast the effects of IBD substantial costs for health care. The majority of patients are diagnosed early in life and the incidence continues to rise; therefore, the effect of IBD on health-care systems will rise exponentially. We also provide action tips to help safety guide the patients and clinicians during pre-, peri- and post pregnancy, and breastfeeding. Finally, we address identified neighborhood factors, education, healthcare access and quality, economic stability, and other personal and societal contexts that can help health care institutions work towards a common goal of achieving health equity, regardless of racial/ethnic background.
2. Core tip
Pregnant women in the health insurance coverage gap are eligible for Medicaid, but necessary preconception care is likely unavailable.[6] Being uninsured prior to pregnancy is associated with a higher prevalence of risk factors that contribute to poor pregnancy outcomes, especially for AAW.[58] AAW experience unacceptably high rates of poor maternal health outcomes, and a maternal mortality rate of three times that of their White counterparts.[50–58] In fact, AAW with or without IBD are three times more likely to die from pregnancy or parturition than women of any other race in the United States.[29–31] Both societal and healthcare related factors contribute to high rates of poor health outcomes and AAW maternal mortality. The profound risk that AAW face from conception, to birth, and into motherhood is structural racism.[107–111] Throughout the course of a pregnancy, AAW face a variety of healthcare related disadvantages compared to non-Hispanic or white women.[75–78] The reasons for this may not be immediately obvious because AAW’s heightened risk of pregnancy-related death spans income and education levels. While AAW are at a higher risk for developing high blood pressure and fibroids during pregnancy, the predominant issue comes down to medical inequity and access to quality care. [59–67] AAW also face medical racism and clinical research that historically has excluded AAW.[107,108] These risks and subsequent complications extend from pregnancy to childbirth and motherhood. In additional to IBD, these include postpartum cardiomyopathy, preeclampsia and eclampsia, causing AAW maternal mortality rates to be five times those of non-Hispanic women.[66,78,134,135] AAW also are over two times more likely than non-Hispanic women to die of hemorrhage or embolism. The African American (AA) infant mortality rate in 2018 was 10.8 deaths per 1,000 live births, compared to 4.6 deaths per 1,000 live births for white babies. The infant mortality rate among AA families is still significantly higher than non-Hispanic families across income and education levels. Issues involving health equity and improving access to reliable and unbiased healthcare is of the utmost importance when it comes to decreasing the AA maternal morbidity and mortality rates.[114].
Moreover, uninsured AA is likely to delay prenatal care until they apply to enroll in Medicaid.[58] Medicaid pays 40 percent of U.S. births and 65 percent of births to AA mothers as part of a comprehensive strategy to address the AA maternal health crisis. Medicaid under the Affordable Care Act have significant health coverage among AAW of reproductive age but does not cover preconception counseling and prenatal services that make pregnancy and parturition safer for parent and baby.[112] Robust research evidence shows Medicaid expansion is associated with reduced rates of maternal death, particularly for AA.[112] Closing the coverage gap would significantly improve Black maternal health.[75] Overall, IBD affects people during their reproductive years and has emerged globally with rising prevalence and has become an emergent disease with healthcare costs rising at an exponential rate.[6]
The management of IBD in pregnancy, maternal and infant health is complex, demanding and challenging, especially to AAW.[59–67] Poorly controlled IBD during pregnancy increases the risk of prematurity, low weight for gestation, and fetal loss.[68] The default is to cease interventions during pregnancy and lactation, despite the known risk of fulminant disease, the commonest to pregnancy outcome.[68–72]
3. African American Women versus White American Women with Inflammatory Bowel Disease and Pregnancy
There are physiological changes during pregnancy including uterine expansion, increase in progesterone hormone level (that may delay gastric emptying) and anatomic compression and lower esophageal sphincter pressures, thereby increasing risk for reflux, nausea, early satiety, and constipation.[73] A study evaluating infant outcome in women with IBD at an urban university, and tertiary-referral center, reviewed medical records with single births who received all of their gastroenterology and obstetrical care at the medical center over a 9-year period.[74] In summary, this study reveal that IBD is not associated with a higher pre-term delivery, neonatal intensive care unit requirements or congenital abnormalities when compared to the general population. The study observed however that AAW had more infants with low birth weights than CAW (P = 0.0459). Coordinated gastroenterology and obstetrical care in women with IBD is critical to optimize infant clinical outcome.
Considerable number of AA experience higher rates of maternal morbidity and mortality compared to US women of other racial/ ethnic groups. Lack of knowledge among both patients and physicians regarding reproductive health, especially in patients diagnosed with IBD is significant.[75–78] The management of IBD during pregnancy is widely ascertained to all pregnant women but there is lack of knowledge among AAW regarding healthcare system inclusiveness and lack of health insurance negatively impacts these patients. They lack good control of disease and clinical remission at the time of conception which decreases the likelihood of quiescent disease during pregnancy necessary for having successful pregnancy outcomes. Closing the coverage gap would significantly improve black maternal health. Overall, IBD affects people during their reproductive years and has emerged globally with rising prevalence and has become an emergent disease with healthcare costs rising at an exponential rate.[6] Remarkable progress has been made in the treatment of IBD in recent years resulting in successive launching of new pharmaceuticals (biologics / biosimilars), though understanding of safety use of each newly developed medication during pregnancy and their in utero effects have not been maintained. Studies have demonstrated increased concentrations of biological agents in infant’s blood stream multifold more than mother’s trough when administered in late gestation period. Relatively high concentrations of biological agents do not seem to cause adverse birth outcomes nor future developmental defects but may affect baby’s immune function. Therefore, special consideration should be given to vaccination schedule of the newborn babies whose mothers were treated with biologics / biosimilars in the late gestation period. A summarized overview of IBD in pregnancy clinical care pathways is depicted in Fig. 1.[31,84,85] Importantly, good prenatal supplementing nutrition is advised to handle the extra body demands as the pregnancy progresses.[79,80] The goal is to balance getting enough nutrients to support the growth of the fetus and maintaining a healthy weight.[81] While all women need to increase intake of certain essential vitamin and nutrients (folic acid, Vitamin D & iron) to ensure a healthy pregnancy, the woman with IBD is at greater risk for these kind of deficits.[81–83] This is especially true with fulminant IBD since bowel inflammation and diarrhea prevent proper absorption or the loss of nutrients. Fulminant IBD also reduce appetite and make food harder to digest. Prenatal dietary supplement guidelines are depicted in Fig. 3.
Figure 1.
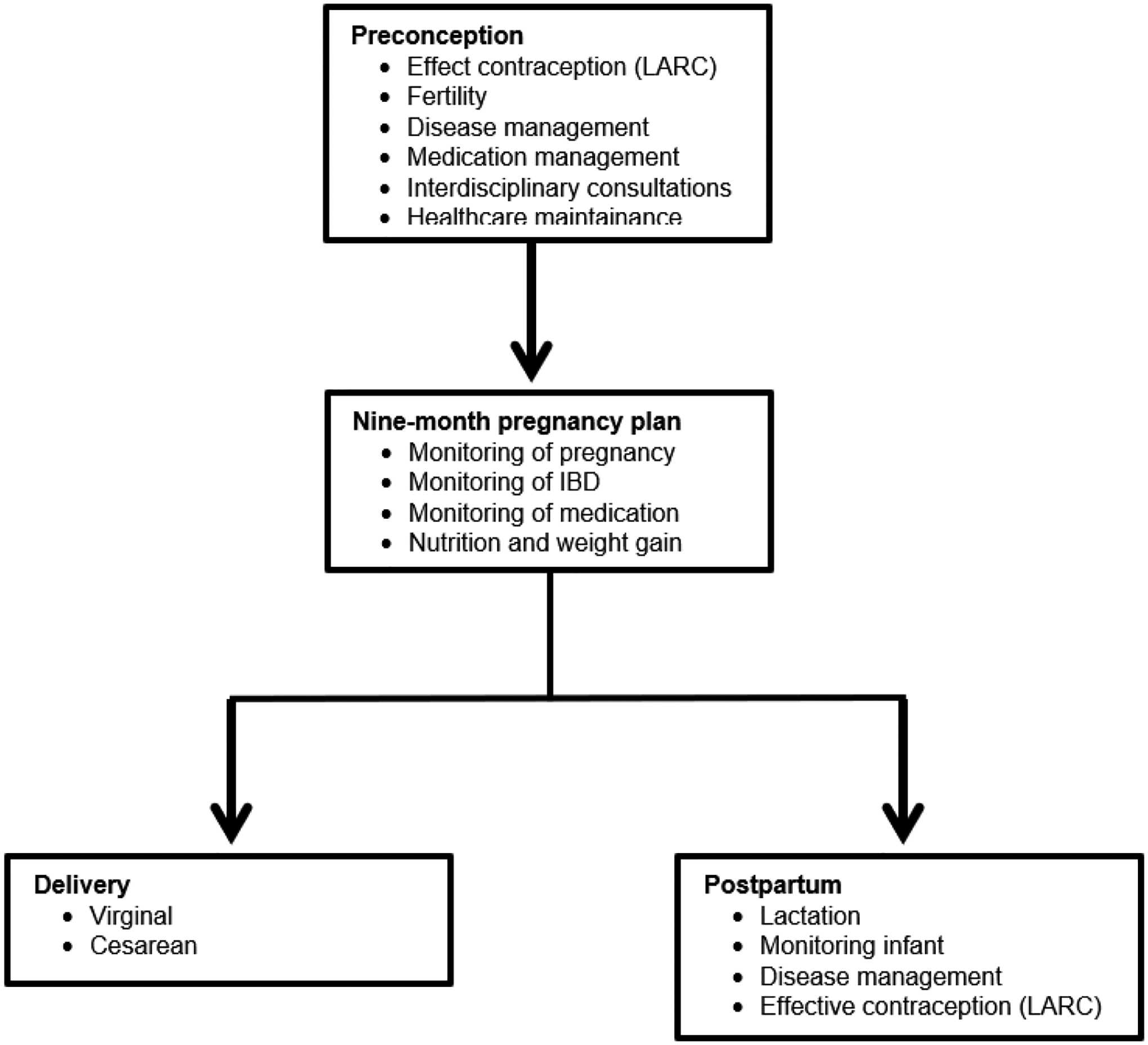
Overview of Inflammatory bowel disease in pregnancy clinical care pathway [32,89,90]
Abbreviations: LARC, long-acting, reversible contraception; IBD, inflammatory bowel disease.
Figure 3.
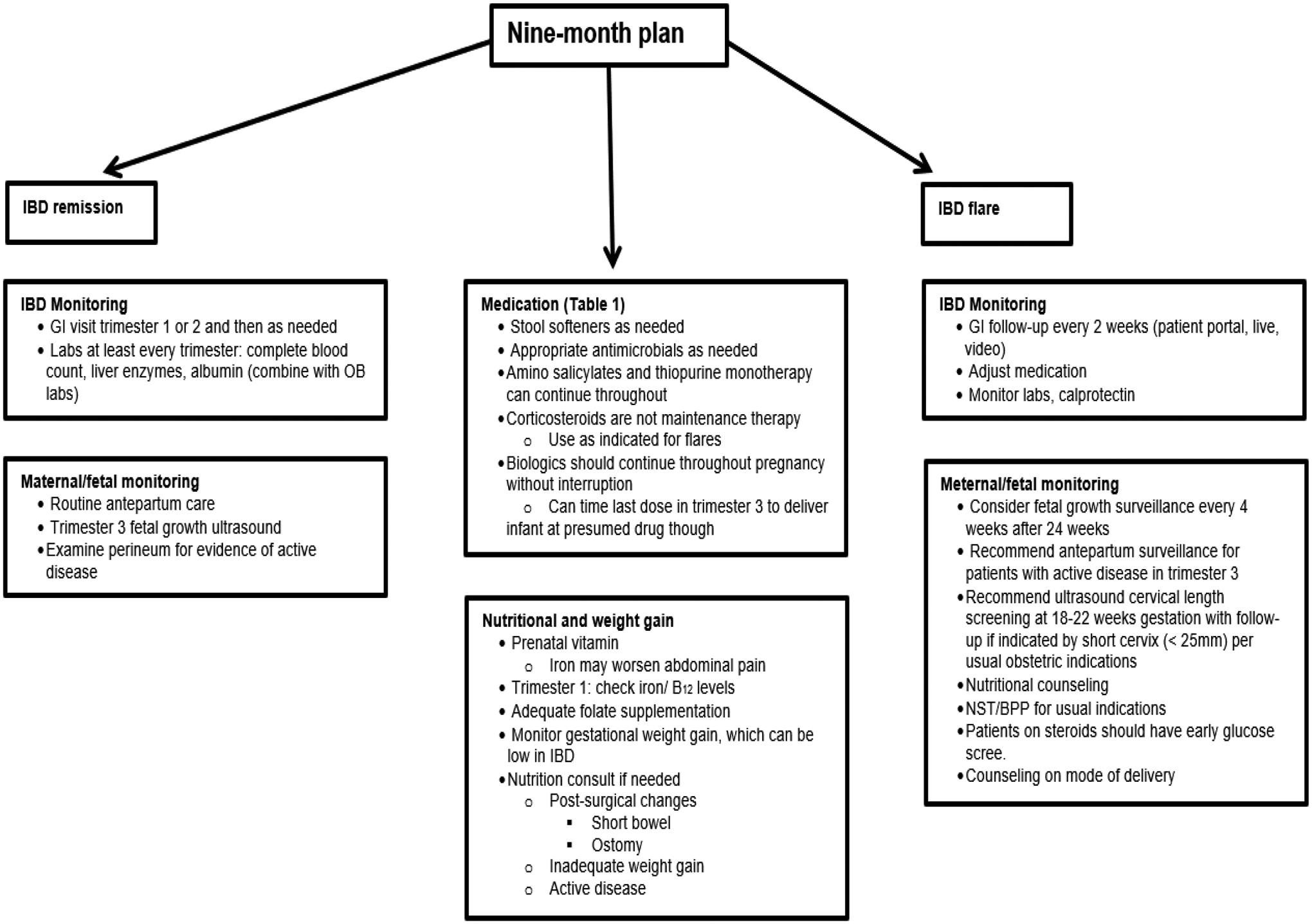
Abbreviations: NST, Nonstress test; BPP, Biophysical profile; IBD, inflammatory bowel disease; NST/BPP; non-stress test/biophysical profile scan.
4. Conception - Fertility: Chances of becoming pregnant in African American Women patients with Inflammatory Bowel Disease
Women suffering from IBD have been shown to have similar fertility as the general population,[84–92] although some studies report that they have reduced fertility, especially when their disease is active, fulminant colitis.[93,94] Clinically, fulminant colitis occurs in patients with severe UC who have more than 10 bowel movement per day, continuous mucosal bleeding, abdominal pain, distention, and acute, severe toxic symptoms including fever and anorexia.[92,93,95] IBD patients can have normal fertility, however once UC patients have had a pouch surgery (restorative proctocolectomy with ileal pouch-anal anastomosis (RPC-IPAA)), they have an increased risk of infertility up to 3–4 fold.[93–100] This increased infertility rate after RPC-IPAA is due to partial or total obstruction of fallopian tubes from the adhesions and scarring.[45,99,100] Patients who have had laparoscopic RPC-IPAA have been shown to have less adhesions,101] and lower infertility rates.[102,103] There are varying reports on the infertility rates among women with CD and UC. These differences are attributed to voluntary childlessness (VC), i.e., voluntary choice to not have children. In a meta-analysis of eleven studies, they found that in women with CD, fertility was decreased up to 44% vs. controls, however, further analyses divulged association to VC; they did not find any reduction in fertility in women with UC.[49,104]
The fact that knowledge on gastroenterological and obstetrical management of IBD has improved over the years, many patients still actively avoid pregnancy for fear of adverse maternal or neonatal outcomes. There is fear of adverse effects of pregnancy on the disease activity, of eventual IBD inheritance, or of an increased risk of congenital malformations. Indeed, though data indicate that fertility is hardly affected by the disease, there is conflicting knowledge about the impact of IBD on fertility, pregnancy and sexual function health and health care professionals (HCPs) do not sufficiently inform their patients about reproductive outcomes often associated with a higher risk of adverse pregnancy outcomes such as low birth weight, preterm birth, and spontaneous abortion. More research information on these topics is indisputably needed for IBD patients, especially AAW.[105,106] Because of these uncertainty, many women with IBD may choose to remain childless due to a lack of IBD-specific reproductive knowledge.[106] Another serious misconception challenges in planning pregnancy among AAW with or even without IBD is the maternal mortality crisis in the United States which emphasizes the validity behind this notion of systemic institutionalized structural racism.[107,108] Racism is the relegation of people of color to inferior status and treatment based on unfounded myths, taboo and beliefs about innate inferiority, as well as unjust treatment and oppression, whether intended or not.[109,110] Racism is not always conscious, explicit, or readily visible, often it is systemic and structural that is the systems’ platform/ scaffolding.[111] Systemic and structural racism are forms of racism that are pervasively and deeply embedded in systems, laws, written or unwritten policies, and entrenched practices and beliefs that produce, condone, and perpetuate widespread unfair treatment and oppression of people of color, with adverse health consequences.[112–115] Unfortunately causal pathways for health damages can take decades, even generations, may pass between exposure to systemic racism and evidence of its health damages, obscuring the connection experiences of racism contribute to racial or ethnic disparities in health by setting in motion various sequential causal pathways often difficult to detect their origins underlying unseen causes.[113] There are several other examples of systemic institutional structural racism visible in policy discourse e.g. in political disempowerment, segregation, financial practices, environmental injustice, criminal justice system, historical examples, data aggregation etc. Strategies to dismantle systemic racism should be prioritized to addressing inequities in the key determinants of policy discourse such as health care.116].
5. Sleep quality and pregnancy in African American Women patients with Inflammatory Bowel Disease
It has been long recognized that IBD patients suffer from poor sleep quality, only a handful of studies have evaluated the prevalence and risk factors associated with sleep disturbance and severity in IBD.[118–122] Further, discrimination/racism is reported to be associated with poor sleep quality in pregnant AAW.[123–125] Another study of patients who completed the Pittsburgh Sleep Quality Index (PSQI), the IBD questionnaire (IBDQ), the IBD-Disability Index (IBD-DI) questionnaire, and the Hospital Anxiety and Depression Scale (9-HADS) were analyzed using a multivariate regression model applied to assess independent risk factors of sleep disturbance among IBD-related variables, disability, quality of life, anxiety, and depression. The study investigated the sleep quality of 166 patients, finding 67.5% of them suffering from sleep disturbance. In particular, low quality of life, presence of disability and extraintestinal manifestations were identified as independent risk factors of sleep disturbance. The study discovered that all depressed patients were also affected by sleep disturbance, while found no difference in sleep disturbance between patients with or without anxiety state. However, a positive correlation was reported between both anxiety and depression scores and PSQI score (Spearman correlation: r = 0.31 and r = 0.38 respectively). The study showed that sleep quality is not directly associated with an active or inactive IBD state or with the ongoing treatment, but it is mostly correlated with the patients’ mood state, disability, and quality of life.[126] Advisably, Gastroenterologists and Psychologists should join forces during clinical outpatients’ visits to evaluate emotional states for a better IBD management.
6. Pregnant African American Women Patients with Inflammatory Bowel Disease
There are significant racial and ethnic differences in the incidence and temporal trends of IBD over the last few decades in the US population-based cohort.[166] Studies suggest that migration and race influence the risk of developing IBD may be due to different inherent responses upon exposure to an environmental trigger in the adopted country.[167] The prevalence of IBD is 96 cases per 100,000 person-years in African Americans.[43] In the 1980s, a study from southern California, USA using the Kaiser Permanente Medical Care Program reported that African Americans had IBD prevalence approximately two-thirds of that of whites 29.8 cases per incidence of IBD among racial and ethnic groups in the US.[166,168] In AAW with IBD face poor access to outpatient IBD specialist care which contributes to IBD-related emergency department (ED) visits.[169] Strategies to increase specialist access may reduce the utilization of emergency services.[170,171] IBD affects mainly young people who are often in the process of family planning.[2,38,172] The patients with IBD commonly experience unexpected relapses of the disease and not a few IBD patients have disease flare during their pregnancy, childbirth, and nursing most likely due to endogenous cortisol levels which is more than double during pregnancy.[173.174] Options for flare management and maintenance therapies during pregnancy planning and conception, pregnancy and lactation are depicted in Tables 1 & 2 [175–185] and Figure 1 and Figure 2.[31,72,84,85,193,194] Detailed nine-months plan is shown in Figure 3.[71,175,176,186,187] During pregnancy, many physiological changes occur in order to allow implantation and fetal growth. This is the reason why pregnancy represents a period of intense endocrine fluctuation and immune modulation.[188] In previous years, it was thought that during pregnancy there was a rise in maternal immune tolerance; however, it is now emerging that immunological states fluctuate during these months on demand to meet various requirements.[189] Insecurity of patients and their primary physicians concerning the disease course, successful pregnancy and the appropriate medication is to date still a challenge often followed by a decision against the pregnancy.[190,191] A recent study comparing IBD and non-IBD pregnant women[192] showed an improvement in the modulation of cytokine patterns during pregnancy in the first group. Indeed, IL-6, IL-8, IL-12, IL-17, and TNF-a proinflammatory cytokines significantly decreased after conception. During pregnancy itself, serum cytokine levels in patients with IBD subsequently remain relatively stable over the 40 weeks of gestation. On the other hand, Kim et al. and coworkers showed that a surrogate marker of bowel inflammation (i.e., Fecal Calprotectin (FC)), had higher levels in pregnant patients affected by IBD compared with controls, but it gradually decreased in the case-group.[193] The opposite trend was observed in the control-group, demonstrating a slight gradual increase in their FC inflammation marker levels during gestation. As for babies born to mothers with IBD, the same study showed significantly higher FC levels compared with control babies from 2 to 36 months of age. The authors speculated that those babies may have been less able to achieve a balanced mucosal immunity or to establish an optimal intestinal barrier function. This fact is probably explained by a lower immune tolerance to commensal bacteria in babies born to IBD mothers, potentially leading to chronic mild intestinal inflammation due to a modification in the intestinal microbiota.
Table 1.
| Medical Treatment | Safety and Recommendations in Pregnancy | Safety and Recommendations in Breastfeeding |
|---|---|---|
| Aminosalicylates (mesalazine, sulfasalazine, balsalazide, olsalazide) | No increased obstetrical risk. Always recommended (formulation without dibutylphthalate are preferable and, if sulfasalazine is used, suggestion to supplement with folate) | Safe and must be discontinued only in case of neonatal severe bloody diarrhea. |
| Corticosteroids | Concerns about teratogenic effects, such as cleft lip or palate. Recommended only in case of active flares | Recommended to breastfeed babies 4 h after taking corticosteroids |
| Antibiotics (metronidazole and ciprofloxacin) | Concerns about teratogenic effects, such as cleft lip or plate.Recommended only after the first trimester of gestation. | Recommended to breastfeed babies 12–24 h after metronidazole and 48 h after ciprofloxacin intake. A short-term antibiotic regimen must be preferred |
| Thiopurines (azathioprine or 6-mercaptopurine) | Slight increase in preterm deliveries. Recommended as monotherapy | Advisable, no a higher risk of physical or developmental anomalies in newborns |
| Methotrexate | Strong teratogenicity and abortive effects. Never recommended in pregnancy | Contraindicated |
| Cyclosporine | No data on pregnant women available, only recommended as rescue therapy for acute severe steroid-refractory ulcerative colitis | Contraindicated |
| Antibiotics (metronidazole and ciprofloxacin) | Concerns about teratogenic effects, such as cleft lip or plate.Recommended only after the first trimester of gestation. | Recommended to breastfeed babies 12–24 h after metronidazole and 48 h after ciprofloxacin intake A short-term antibiotic regimen must be preferred |
| Thiopurines (azathioprine or 6-mercaptopurine) | Slight increase in preterm deliveries. Recommended as monotherapy. | Advisable, no a higher risk of physical or developmental anomalies in newborns. |
| Anti-TNFα agents (infliximab, adalimumab, golimumab and certolizumab) | Evidence of crossing the placenta, except of certolizumab Recommended stopping around the 24th week of gestation, if the case permits. | Safe due to their transmission in breast milk only in small amounts and deactivation by neonatal digestion enzymes |
| Vedolizumab and ustekinumab | Should be avoided due to their transmission across the placenta and partial lack of data in pregnancy. Can eventually be prescribed only as an ultimate alternative | Safety data are still missing, so their use is not recommended |
| Tofacitinib, filgotinib and upadacitinib | Contraindicated due to the complete lack of data in pregnancy. | Safety data are still missing, so their use is not recommended. |
Abbreviations: CRP, C-reactive protein; CT, computed tomography; ESR, erythrocyte sedimentation rate; MRI, magnetic resonance imaging, IBD, inflammatory bowel disease.
Table 2.
| Laboratory Values | Endoscopy | Radiology imaging | Surgery | Medication |
|---|---|---|---|---|
| Standard IBD laboratory values chacked | Perform for strong indications: | MRI and CT have similar diagnostics accuracy for assessing IBD | Surgery intervention may be needed: | Mange similar to nonpregnant IBD Patients |
|
-Determining IBD disease activity | Gadolinium should be avoided in pregnancy | - Acute refractory colitis - Perforation |
Exceptions: -Thiopurine-naïve patients avoid first start in pregnancy due to concerns for distinctive rare adverse reactions |
|
-When results will change management | The cumulative radiation exposure of a single CT scan (about 50 mGy) is below the level of concern | -Abscess -Severe hemorrhage |
Methotrexate contraindicated |
|
Flexible sigmoidoscopy is preferred oner pancolonoscopy when possible; can be performed unsedated, and in any trimester | Ultrasound, where available is appropriate for terminal ileal disease | -Bowel obstruction | Tofacitinib: avoid due to limited human data |
|
||||
|
||||
|
Abbreviation: Anti-TNFα, tumor-necrosis factor-α
Figure 2.
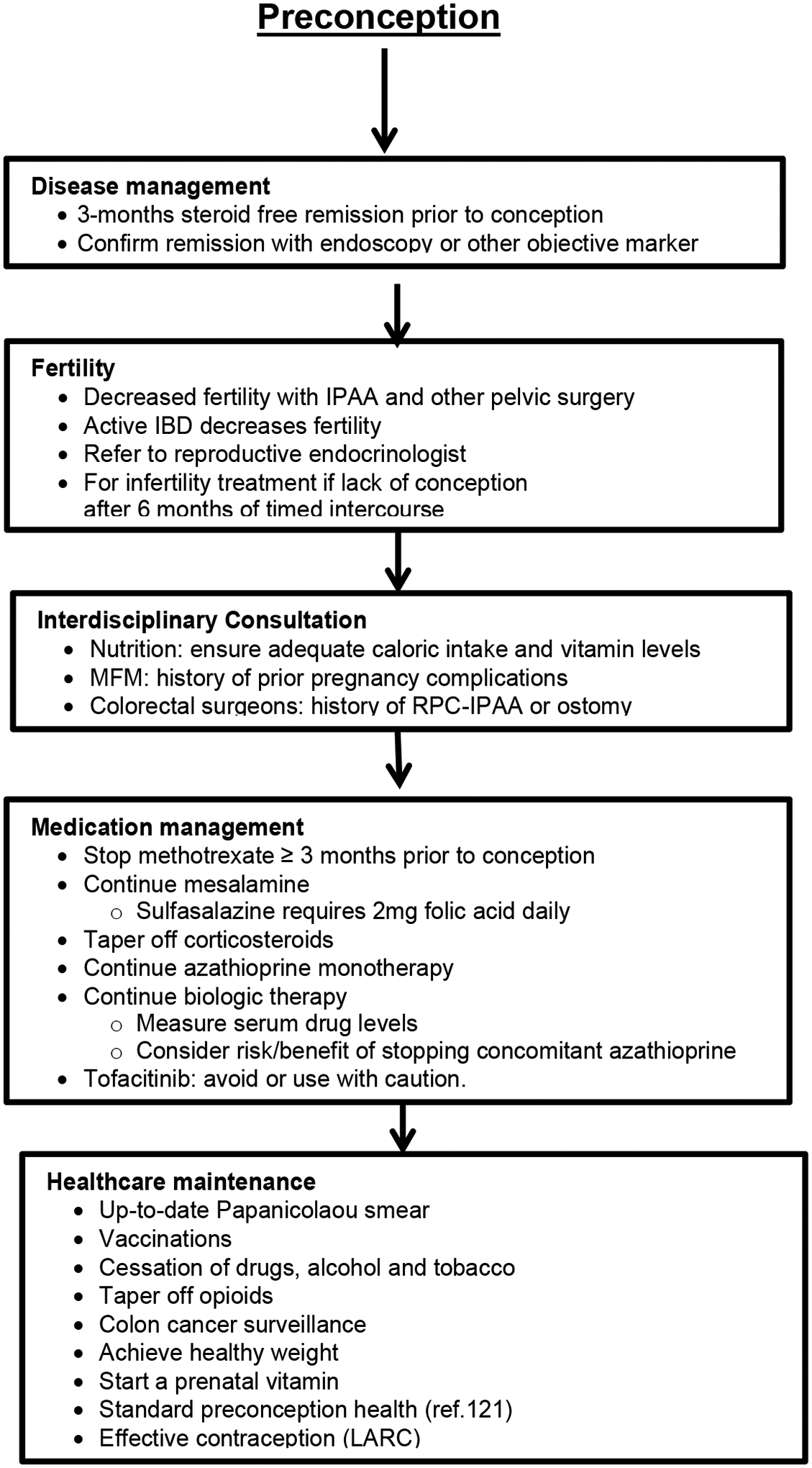
Pregnancy planning and conception [71,73,221]
Abbreviations: ACOG, American College of Obstetricians and Gynecologists; LARC, long-acting, reversible contraception; IBD, inflammatory bowel disease; IPAA, ileal pouch-anal anastomosis; RPC-IPAA, restorative proctocolectomy with ileal pouch-anal anastomosis.
7. Pregnancy and Inflammatory Bowel Disease Care Coordination Team and Disparities
It is important to educate the young patients with IBD during family planning counseling.[194–200] Low health literacy is present in IBD populations and more common among older AAs[201–203] Opportunities exist for providing more health literacy-sensitive care in IBD to address disparities and to benefit those with low health literacy.[203] Unfortunately, to date, racial disparities and racism severely impacts AAW during pregnancies in health and diseases while attending care coordination services.[125,204,205] Fulminant colitis disease during conception and pregnancy in women with IBD increases the risk of pregnancy complications and adverse neonatal outcomes.[185,206–208] Preferably, a pregnant patient with IBD should be monitored by both a gastroenterologist specialized in IBD and a maternal–fetal medicine (MFM) specialist, OB/GYN with assistance from nutritionists, lactation counselors, colorectal surgeons, and care coordinator as needed. Pregnancy planning and conception is depicted in Figure 2 [71,209,210] However, due to variations in access, availability, and preference, patients may receive their IBD care from a general gastroenterologist, nurse practitioner, physician’s assistant, surgeon, primary care provider, or even the emergency department. Similarly, obstetric care may be provided by a maternal fetal medicine (MFM) general obstetrician, midwife, and family practitioner. Painstakingly, many nulligravida and/ or nulliparous AAW have no one at all for much of the pregnancy.[68,211] It is realizable that sizable number of patients and providers do not have access to IBD experts and MFM specialists, particularly outside of urban centers. However, any gastroenterologist, OB/GYN, or specialized physician’s assistant, nurse practitioner, or midwife can follow the Care Pathway to optimize outcomes in this population. Some patients are newly diagnosed with IBD during pregnancy and may be directed to a gastroenterologist after an emergency department visit, hospital admission, or visit with their primary care provider or obstetrician/ gynecologist (OB/GYN). Importantly, efforts to decrease institutional and interpersonal experiences of racial/ethnic discrimination and gendered structural racism would tremendously benefit the healthcare service and sleep quality of pregnant AAW,[205,212–215] particularly during early pregnancy.[124]
8. The Inflammatory Bowel Disease Parenthood project and persistent barriers
Parenting mothers with IBD who are breastfeeding should follow standard nutritional recommendations.[216–219] American Gastroenterological Association (AGA) runs an IBD parenthood project which provides information to women with IBD and how they can stay healthy and have healthy babies.[71,186,220] The long-term safety of exposure to biologic/ biosimilar drugs in IBD patients during pregnancy has received attention. Recently, multicenter retrospective studies have been reporting on fertility health and pregnancy in these patients diagnosed with IBD.[39,189,221–224] Further, there is shared information focused on disease characteristics, medication use, lifestyle, inadequate gestational weight gain, pregnancy outcomes and long-term health outcomes of children breastfed by women receiving biologic/ biosimilar therapies and effects of breastfeeding and development retrieved from mothers and medical charts.[225–235] Assessment of adverse reactions to vaccinations, growth, infections, autoimmune diseases and malignancies are reported.[236–242] Furthermore, the IBD Parenthood project further helps gastroenterologists provide care during all stages of family planning such as: groundbreaking medical research in IBD - a family affair, supporting IBD patients in family planning and pregnancy, how to care for IBD patients in pregnancy and, what is the IBD in Pregnancy Clinical Care Pathway? Overview of IBD in Pregnancy Clinical Care Pathway is herein depicted in Figure 1.[31,84,85] Further, recommendation/ decision algorithm for mode of delivery – cesarean vs. vaginal is detailed illustrated in Figure 4.[31,243–245] Post-delivery care for mother and baby is summarized in Figure 5.[246–348]
Figure 4.

Decision algorithm for mode of delivery[31,255–257]
Abbreviations: GBS, group B streptococcus; VTE, venous thromboembolism; GBS, Group B streptococcus; VTE, Venous thromboembolic disease.
Figure 5.
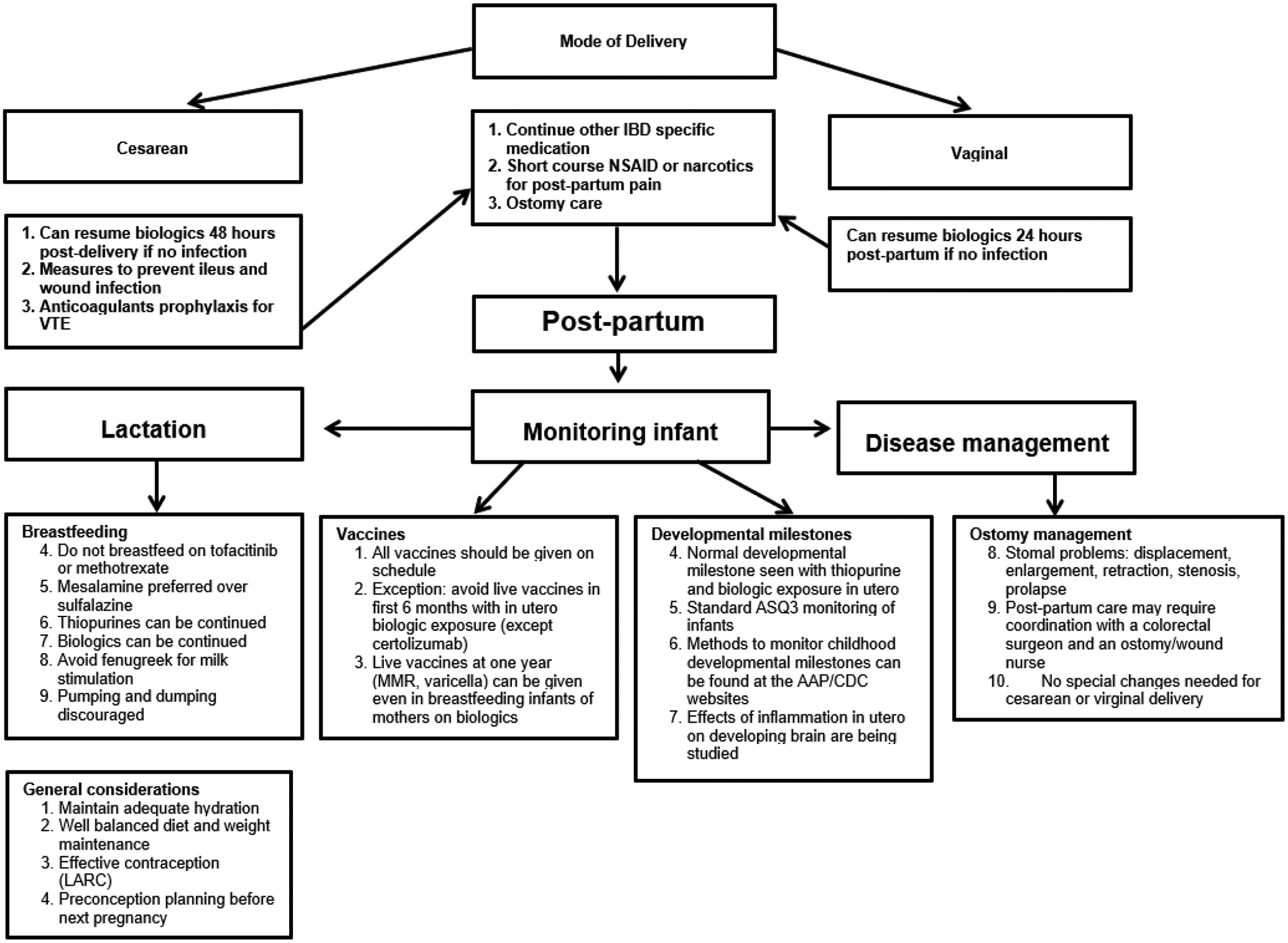
Post-delivery care for mother and baby[258–260]
Abbreviations: IBD, inflammatory bowel disease; LARC, long-acting, reversible contraception; MMR, measles, mumps, rubella; NSAID, nonsteroidal anti-inflammatory drug; VTE, venous thromboembolism; NSAID, nonsteroidal anti-inflammatory drugs; MMR, measles, mumps, rubella; AAP, American Academy of Pediatrics; CDC, Centers for Disease Control and Prevention.
9. Pharmaceutics Strategies for Management of patients with Inflammatory Bowel Disease
To date, there is no definite curative pharmacological drug(s) exists for IBD, which may result in significant long-term comorbidity.[249] The scientific evidence warrants assessing and providing expert opinion related to nutritional, psychological, and supportive care of women and their infants throughout the prenatal, antenatal, and infant periods.[250,251] In recent years, the IBD community has witnessed the marketing of novel therapies involving orally administrated drugs that target key inflammatory signaling pathways.[71,186,187,225,252,253] However, these carefully designed drugs do not cure IBD but manages symptomatology temporarily; moreover, the active pharmaceutical ingredients have serious side effects, and a sub-group of patients are not responsive to them. Thus, given the personal and societal impact of this disease, this unmet need justifies the continued development of novel therapeutic strategies for the treatment of IBD.[254,255] There are established clinical recommendation option guidelines for the flare management efficacy and safety for use of medical pharmaceuticals of IBD patients during pregnancy and lactation as summarized herein in Table 1 and Table 2.[159–169].
10. Surgical therapy for Inflammatory Bowel Disease on Female Fertility
The standard curative surgical procedure for treating UC is pouch surgery, RPC-IPAA.[256,–258] Women with refractory UC may require RPC-IPAA surgery which may increase risk of infertility.[50,258–260] Colonic Crohn’s disease (CD) called Crohn’s colitis (CC) is a relative contraindication to RPC-IPAA intervention because of higher rate of complications and pouch failure even in highly selected patient.[82] Therefore, it is important to accurately categorize indeterminate colitis (IC) into authentic either UC or CD prior to surgery.[261–264] We identified 16 observational studies of which ten studies were included in meta-analyses, of which nine compared women with and without a previous IBD-related surgery and the other compared women with open and laparoscopic RPC-IPAA. Of the ten studies included in meta-analyses, four evaluated infertility, one evaluated assisted reproductive technology (ART), and seven reported on pregnancy-related outcomes. Seven studies in which women were compared before and after colectomy and/or RPC-IPAA were summarized qualitatively, of which five included a comparison of infertility, three included the use of ART, and three included other pregnancy-related outcomes. One study included a comparison of women with and without RPC-IPAA, as well as before and after RPC-IPAA, and was therefore included in both the meta-analysis and the qualitative summary. All studies were at high risk of bias for at least two of Chochran risk-of-bias tool domains. The Chochran risk of bias tool covers six domains of bias i.e., selection bias, performance bias, detection bias, attrition bias, reporting bias, and other bias.[265–269] According to the latest AGA, American Society of colon and Rectal Surgeons (ASCRS) and European Crohn’s and Colitis Organization (ECCO) guidelines on reproduction, UC without previous pelvic surgery and inactive CD do not impair fertility.[178,270] Conversely, active CD may impair fertility via multiple factors such as pelvic inflammatory disease (PID) which includes fallopian tube inflammation (salpingitis) and/or ovaries (oophoritis) or Inflammation of the fallopian tubes and ovaries simultaneously (salpingoophoritis).[271] Different considerations should be made in UC patients who underwent RPC-IPAA, which seems to increase the risk of infertility by approximately threefold mainly due to tubal dysfunction caused by adhesions.[97,99] Women with RPC-IPAA mostly suffer a reduction in the probability of conception rather than complete infertility.[272,273] Because complications during pregnancy and delivery are rare, caesarean section should be based mainly on obstetric indications.[274,275] Considering all the above possible factors lead to infertility, patients with IBD may be referred to ART earlier than the general population, even after only six months of attempts.[271] It is still not clear to date if the ART success rate in IBD patients differs from the general population.
11. Concluding remarks
In spite of the fact that knowledge on gastroenterological and obstetrical management of IBD has greatly improved over the years, many patients still actively avoid pregnancy for fear of adverse maternal or neonatal outcomes, of adverse effects of pregnancy on the disease activity, of eventual IBD inheritance, or of an increased risk of congenital malformations. Although data hints that fertility is hardly affected by the disease, a reduced birth rate is nevertheless observed in patients with IBD. Moreover, physicians often showed concerns about starting IBD medications before and during pregnancy and did not feel adequately trained on the safety of IBD therapies. IBD-expert gastroenterologists and gynecologists should discuss pregnancy and breastfeeding issues with patients in order to provide appropriate information; therefore, pre-conception counseling on an individualized basis should be mandatory for all patients of reproductive age to reassure them that maintaining disease remission and balancing the eventual obstetrical risks is possible. A healthcare system that is not inclusive is problematic in certain countries including the United States and a substantial number of women are not counseled in a timely manner and those with IBD are as well ineffectively counseled of immunosuppressive therapy on fertility health and pregnancy.[276] This largely impacts AAW linked to structural racism in health care delivery and subsequent toxic stress of racism, knowledge about healthcare system function, inclusiveness and insurance policies negatively impacts these patients. IBD control prior to conception and throughout pregnancy is the cornerstone to successful pregnancy management in these patients. Although the woman with IBD possesses a greater potential for a complicated pregnancy, the majority of these patients will experience an uneventful normal pregnancy. It is important to educate the young patient with or without IBD during family planning counseling. Conception at a time when IBD is quiescent offers the greatest likelihood of an uncomplicated pregnancy. Physicians must recognize and inform their patients that most medications that are necessary to suppress the disease should be continued throughout pregnancy, Table 2. Although generalities can be made regarding the management of pregnant women with IBD, the individual patient may need specifically tailored therapy for her individual case. There is no evidence to suggest that babies born to mothers with IBD regardless of medication exposure have any developmental delays. Recommendations on monitoring childhood developmental milestones can be found at the American Academy of Pediatrics and Centers for Disease Control and Prevention websites.[228,277] The PIANO data on developmental milestones support the lack of negative effect of IBD medications on development.
Practice Point Areas.
Profound hormonal changes may impact onset of prodromal IBD and/or worsen active IBD in pregnant women particularly in AAW.
Pregnant women with IBD are more likely than the general pregnant population to experience adverse maternofetal outcomes, especially at the time of conception and during pregnancy.
Pregnant women with IBD are more likely than the general pregnant population to experience adverse maternofetal outcomes, especially at the time of conception and during pregnancy.
Salivary cortisol and alpha-amylaseare novel biomarkers of stress tied to triggering of latent IBD, reflecting the hypothalamic-pituitary-adrenal axis and sympathetic nervous system, respectively.[278]
Our literature reviews show that sleep quality is not directly associated with an active or inactive IBD state or with the ongoing treatment, but rather it is mostly correlate with the patients’ mood state, disability, and quality of life.[118,126,279]
Gastroenterologists, obstetricians, and psychologists should join forces during clinical outpatients’ visits to evaluate emotional states for a better IBD management.
Research Agenda/Plan.
Consequences of racism before, during and after pregnancy complicating IBD.
Action is needed to have unfettered access to healthcare and facilitate early detection of IBD, especially in AA.
The effect of chronic disease need to be evaluated in future studies by including a comparative group of pregnant women with active IBD.[278]
Funding
This study is supported by NIH Grant U54 MD007586
Footnotes
Conflict of interest
None
Author Contributions
Conceptualization: Amosy E. M’Koma, Jamie N. Ware, Rosemary K. Nabaweesi, Sanika S. Chirwa.
Data curation: Amosy E. M’Koma, Jamie N. Ware, Rosemary K. Nabaweesi, Sanika S. Chirwa.
Formal Analysis of the Literature: Conceptualization: Amosy E. M’Koma, Jamie N. Ware, Rosemary K. Nabaweesi, Sanika S. Chirwa.
Funding Acquisition: Sanika S. Chirwa.
Investigation: Amosy E. M’Koma, Jamie N. Ware, Rosemary K. Nabaweesi, Sanika S. Chirwa.
Performed literature searches, reviewed the article for inclusion, and revised, edited and approval the final manuscript: Amosy E. M’Koma, Jamie N. Ware, Rosemary K. Nabaweesi, Sanika S. Chirwa.
Project administration and supervision: Sanika S. Chirwa.
Resources: Sanika S. Chirwa.
Software: Amosy E. M’Koma
Validation: Amosy E. M’Koma, Jamie N. Ware, Rosemary K. Nabaweesi, Sanika S. Chirwa.
Visualization: Amosy E. M’Koma, Jamie N. Ware, Rosemary K. Nabaweesi, Sanika S. Chirwa.
Writing original draft: Amosy M’Koma.
Intellectual critics, comments, and suggestions: Jamie N. Ware, Rosemary K. Nabaweesi, Sanika S. Chirwa
Clinical guidelines: Jamie N. Ware, Amosy E. M’Koma
Reference
- 1.M’Koma AE. The Multifactorial Etiopathogeneses Interplay of Inflammatory Bowel Disease: An Overview. Gastrointest Disord. 2018;1(1):75–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Siegmund B, Zeitz M. [Inflammatory bowel disease and pregnancy]. Z Gastroenterol. 2009;47(10):1069–74. [DOI] [PubMed] [Google Scholar]
- 3.Podolsky DK. Inflammatory bowel disease. N Engl J Med. 2002;347(6):417–29. [DOI] [PubMed] [Google Scholar]
- 4.Love JR, Irvine EJ, Fedorak RN. Quality of life in inflammatory bowel disease. J Clin Gastroenterol. 1992;14(1):15–9. [DOI] [PubMed] [Google Scholar]
- 5.Sands BE. Therapy of inflammatory bowel disease. Gastroenterology. 2000;118(2 Suppl 1):S68–82. [DOI] [PubMed] [Google Scholar]
- 6.M’Koma AE. Inflammatory Bowel Disease: An Expanding Global Health Problem. Clinical Medicine Insights Gastroenterology. 2013(6):33–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ventham NT, Kennedy NA, Nimmo ER, Satsangi J. Beyond gene discovery in inflammatory bowel disease: the emerging role of epigenetics. Gastroenterology. 2013;145(2):293–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tremaine WJ. Review article: Indeterminate colitis--definition, diagnosis and management. Aliment Pharmacol Ther. 2007;25(1):13–7. [DOI] [PubMed] [Google Scholar]
- 9.Conrad K, Roggenbuck D, Laass MW. Diagnosis and classification of ulcerative colitis. Autoimmun Rev. 2014;13(4–5):463–6. [DOI] [PubMed] [Google Scholar]
- 10.Jevon GP, Madhur R. Endoscopic and histologic findings in pediatric inflammatory bowel disease. Gastroenterol Hepatol (N Y). 2010;6(3):174–80. [PMC free article] [PubMed] [Google Scholar]
- 11.Nosti PA, Stahl TJ, Sokol AI. Surgical repair of rectovaginal fistulas in patients with Crohn’s disease. European journal of obstetrics, gynecology, and reproductive biology. 2013. [DOI] [PubMed] [Google Scholar]
- 12.Nielsen OH, Rogler G, Hahnloser D, Thomsen OO. Diagnosis and management of fistulizing Crohn’s disease. Nat Clin Pract Gastroenterol Hepatol. 2009;6(2):92–106. [DOI] [PubMed] [Google Scholar]
- 13.Laass MW, Roggenbuck D, Conrad K. Diagnosis and classification of Crohn’s disease. Autoimmun Rev. 2014;13(4–5):467–71. [DOI] [PubMed] [Google Scholar]
- 14.Kaplan GG. The global burden of IBD: from 2015 to 2025. Nat Rev Gastroenterol Hepatol. 2015;12(12):720–7. [DOI] [PubMed] [Google Scholar]
- 15.Everhov AH, Halfvarson J, Myrelid P, Sachs MC, Nordenvall C, Soderling J, et al. Incidence and Treatment of Patients Diagnosed With Inflammatory Bowel Diseases at 60 Years or Older in Sweden. Gastroenterology. 2018;154(3):518–28 e15. [DOI] [PubMed] [Google Scholar]
- 16.Archampong TN, Nkrumah KN. Inflammatory bowel disease in Accra: what new trends. West Afr J Med. 2013;32(1):40–4. [PubMed] [Google Scholar]
- 17.Ukwenya AY, Ahmed A, Odigie VI, Mohammed A. Inflammatory bowel disease in Nigerians: still a rare diagnosis? Ann Afr Med. 2011;10(2):175–9. [DOI] [PubMed] [Google Scholar]
- 18.Agoda-Koussema LK, Anoukoum T, Djibril AM, Balaka A, Folligan K, Adjenou V, et al. [Ulcerative colitis: a case in Togo]. Med Sante Trop. 2012;22(1):79–81. [DOI] [PubMed] [Google Scholar]
- 19.Mebazaa A, Aounallah A, Naija N, Cheikh Rouhou R, Kallel L, El Euch D, et al. Dermatologic manifestations in inflammatory bowel disease in Tunisia. Tunis Med. 2012;90(3):252–7. [PubMed] [Google Scholar]
- 20.Senbanjo IO, Oshikoya KA, Onyekwere CA, Abdulkareem FB, Njokanma OF. Ulcerative colitis in a Nigerian girl: a case report. BMC Res Notes. 2012;5:564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bouzid D, Fourati H, Amouri A, Marques I, Abida O, Haddouk S, et al. The CREM gene is involved in genetic predisposition to inflammatory bowel disease in the Tunisian population. Human immunology. 2011;72(12):1204–9. [DOI] [PubMed] [Google Scholar]
- 22.O’Keefe EA, Wright JP, Froggatt J, Cuming L, Elliot M. Medium-term follow-up of ulcerative colitis in Cape Town. S Afr Med J. 1989;76(4):142–5. [PubMed] [Google Scholar]
- 23.O’Keefe EA, Wright JP, Froggatt J, Zabow D. Medium-term follow-up of Crohn’s disease in Cape Town. S Afr Med J. 1989;76(4):139–41. [PubMed] [Google Scholar]
- 24.Segal I Ulcerative colitis in a developing country of Africa: the Baragwanath experience of the first 46 patients. Int J Colorectal Dis. 1988;3(4):222–5. [DOI] [PubMed] [Google Scholar]
- 25.Segal I, Tim LO, Hamilton DG, Walker AR. The rarity of ulcerative colitis in South African blacks. Am J Gastroenterol. 1980;74(4):332–6. [PubMed] [Google Scholar]
- 26.Wright JP, Marks IN, Jameson C, Garisch JA, Burns DG, Kottler RE. Inflammatory bowel disease in Cape Town, 1975–1980. Part II. Crohn’s disease. S Afr Med J. 1983;63(7):226–9. [PubMed] [Google Scholar]
- 27.Wright JP, Marks IN, Jameson C, Garisch JA, Burns DG, Kottler RE. Inflammatory bowel disease in Cape Town, 1975–1980. Part I. Ulcerative colitis. S Afr Med J. 1983;63(7):223–6. [PubMed] [Google Scholar]
- 28.Brom B, Bank S, Marks IN, Barbezat GO, Raynham B. Crohn’s disease in the Cape: a follow-up study of 24 cases and a review of the diagnosis and management. S Afr Med J. 1968;42(41):1099–107. [PubMed] [Google Scholar]
- 29.Novis BH, Marks IN, Bank S, Louw JH. Incidence of Crohn’s disease at Groote Schuur Hospital during 1970–1974. S Afr Med J. 1975;49(17):693–7. [PubMed] [Google Scholar]
- 30.Sobel JD, Schamroth L. Ulcerative colitis in the South African Bantu. Gut. 1970;11(9):760–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Giraud RM, Luke I, Schmaman A. Crohn’s disease in the Transvaal Bantu: a report of 5 cases. S Afr Med J. 1969;43(21):610–3. [PubMed] [Google Scholar]
- 32.Ananthakrishnan AN, Kwon J, Raffals L, Sands B, Stenson WF, McGovern D, et al. Variation in treatment of patients with inflammatory bowel diseases at major referral centers in the United States. Clin Gastroenterol Hepatol. 2015;13(6):1197–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kappelman MD, Rifas-Shiman SL, Porter CQ, Ollendorf DA, Sandler RS, Galanko JA, et al. Direct health care costs of Crohn’s disease and ulcerative colitis in US children and adults. Gastroenterology. 2008;135(6):1907–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Molodecky NA, Soon IS, Rabi DM, Ghali WA, Ferris M, Chernoff G, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142(1):46–54 e42; quiz e30. [DOI] [PubMed] [Google Scholar]
- 35.Chouraki V, Savoye G, Dauchet L, Vernier-Massouille G, Dupas JL, Merle V, et al. The changing pattern of Crohn’s disease incidence in northern France: a continuing increase in the 10- to 19-year-old age bracket (1988–2007). Aliment Pharmacol Ther. 2011;33(10):1133–42. [DOI] [PubMed] [Google Scholar]
- 36.Shmidt E, Dubinsky MC. Inflammatory Bowel Disease and Pregnancy. Am J Gastroenterol. 2022;117(10s):60–8. [DOI] [PubMed] [Google Scholar]
- 37.Baiocco PJ, Korelitz BI. The influence of inflammatory bowel disease and its treatment on pregnancy and fetal outcome. J Clin Gastroenterol. 1984;6(3):211–6. [PubMed] [Google Scholar]
- 38.Heetun ZS, Byrnes C, Neary P, O’Morain C. Review article: Reproduction in the patient with inflammatory bowel disease. Aliment Pharmacol Ther. 2007;26(4):513–33. [DOI] [PubMed] [Google Scholar]
- 39.Vermeire S, Carbonnel F, Coulie PG, Geenen V, Hazes JM, Masson PL, et al. Management of inflammatory bowel disease in pregnancy. J Crohns Colitis. 2012;6(8):811–23. [DOI] [PubMed] [Google Scholar]
- 40.Jakobsen C, Paerregaard A, Munkholm P, Faerk J, Lange A, Andersen J, et al. Pediatric inflammatory bowel disease: increasing incidence, decreasing surgery rate, and compromised nutritional status: A prospective population-based cohort study 2007–2009. Inflammatory bowel diseases. 2011;17(12):2541–50. [DOI] [PubMed] [Google Scholar]
- 41.North American Society for Pediatric Gastroenterology H, Nutrition, Colitis Foundation of A, Bousvaros A, Antonioli DA, Colletti RB, et al. Differentiating ulcerative colitis from Crohn disease in children and young adults: report of a working group of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition and the Crohn’s and Colitis Foundation of America. J Pediatr Gastroenterol Nutr. 2007;44(5):653–74. [DOI] [PubMed] [Google Scholar]
- 42.Griffiths AM. Specificities of inflammatory bowel disease in childhood. Best Pract Res Clin Gastroenterol. 2004;18(3):509–23. [DOI] [PubMed] [Google Scholar]
- 43.Wang YR, Loftus EV Jr., Cangemi JR, Picco MF. Racial/Ethnic and regional differences in the prevalence of inflammatory bowel disease in the United States. Digestion. 2013;88(1):20–5. [DOI] [PubMed] [Google Scholar]
- 44.Afzali A, Cross RK. Racial and Ethnic Minorities with Inflammatory Bowel Disease in the United States: A Systematic Review of Disease Characteristics and Differences. Inflammatory bowel diseases. 2016;22(8):2023–40. [DOI] [PubMed] [Google Scholar]
- 45.Li D, Collins B, Velayos FS, Liu L, Lewis JD, Allison JE, et al. Racial and ethnic differences in health care utilization and outcomes among ulcerative colitis patients in an integrated health-care organization. Dig Dis Sci. 2014;59(2):287–94. [DOI] [PubMed] [Google Scholar]
- 46.Castaneda G, Liu B, Torres S, Bhuket T, Wong RJ. Race/Ethnicity-Specific Disparities in the Severity of Disease at Presentation in Adults with Ulcerative Colitis: A Cross-Sectional Study. Dig Dis Sci. 2017;62(10):2876–81. [DOI] [PubMed] [Google Scholar]
- 47.Avalos DJ, Mendoza-Ladd A, Zuckerman MJ, Bashashati M, Alvarado A, Dwivedi A, et al. Hispanic Americans and Non-Hispanic White Americans Have a Similar Inflammatory Bowel Disease Phenotype: A Systematic Review with Meta-Analysis. Dig Dis Sci. 2018;63(6):1558–71. [DOI] [PubMed] [Google Scholar]
- 48.Hou JK, El-Serag H, Thirumurthi S. Distribution and manifestations of inflammatory bowel disease in Asians, Hispanics, and African Americans: a systematic review. Am J Gastroenterol. 2009;104(8):2100–9. [DOI] [PubMed] [Google Scholar]
- 49.Huang VW, Habal FM. From conception to delivery: managing the pregnant inflammatory bowel disease patient. World J Gastroenterol. 2014;20(13):3495–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Malhame I, Bublitz MH, Bourjeily G. The Challenge of Screening for Obstructive Sleep Apnea in Pregnancy. Ann Am Thorac Soc. 2019;16(10):1242–4. [DOI] [PubMed] [Google Scholar]
- 51.Balserak BI, Zhu B, Grandner MA, Jackson N, Pien GW. Obstructive sleep apnea in pregnancy: performance of a rapid screening tool. Sleep Breath. 2019;23(2):425–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lomakova YD, Chen X, Stein TP, Steer RA. Decreased Adiponectin Levels in Early Pregnancy Are Associated with High Risk of Prematurity for African American Women. Journal of clinical medicine. 2022;11(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chen X, Scholl TO, Stein TP, Steer RA, Williams KP. Maternal Circulating Lipid Profile during Early Pregnancy: Racial/Ethnic Differences and Association with Spontaneous Preterm Delivery. Nutrients. 2017;9(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Manuck TA. Racial and ethnic differences in preterm birth: A complex, multifactorial problem. Semin Perinatol. 2017;41(8):511–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Huesch M, Doctor JN. Factors associated with increased cesarean risk among African American women: evidence from California, 2010. Am J Public Health. 2015;105(5):956–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Aron DC, Gordon HS, DiGiuseppe DL, Harper DL, Rosenthal GE. Variations in risk-adjusted cesarean delivery rates according to race and health insurance. Med Care. 2000;38(1):35–44. [DOI] [PubMed] [Google Scholar]
- 57.Sakala C, Belanoff C, Declercq ER. Factors Associated with Unplanned Primary Cesarean Birth: Secondary Analysis of the Listening to Mothers in California Survey. BMC Pregnancy Childbirth. 2020;20(1):462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hoxha I, Braha M, Syrogiannouli L, Goodman DC, Juni P. Caesarean section in uninsured women in the USA: systematic review and meta-analysis. BMJ Open. 2019;9(3):e025356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Julsgaard M, Norgaard M, Hvas CL, Buck D, Christensen LA. Self-reported adherence to medical treatment prior to and during pregnancy among women with ulcerative colitis. Inflammatory bowel diseases. 2011;17(7):1573–80. [DOI] [PubMed] [Google Scholar]
- 60.Selinger CP, Ghorayeb J, Madill A. What Factors Might Drive Voluntary Childlessness (VC) in Women with IBD? Does IBD-specific Pregnancy-related Knowledge Matter? J Crohns Colitis. 2016;10(10):1151–8. [DOI] [PubMed] [Google Scholar]
- 61.Mountifield R, Bampton P, Prosser R, Muller K, Andrews JM. Fear and fertility in inflammatory bowel disease: a mismatch of perception and reality affects family planning decisions. Inflammatory bowel diseases. 2009;15(5):720–5. [DOI] [PubMed] [Google Scholar]
- 62.Elkafrawi D, Sisti G, Araji S, Khoury A, Miller J, Rodriguez Echevarria B. Risk Factors for Neonatal/Maternal Morbidity and Mortality in African American Women with Placental Abruption. Medicina (Kaunas). 2020;56(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kinser PA, Jallo N, Amstadter AB, Thacker LR, Jones E, Moyer S, et al. Depression, Anxiety, Resilience, and Coping: The Experience of Pregnant and New Mothers During the First Few Months of the COVID-19 Pandemic. Journal of women’s health. 2021;30(5):654–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lee S, Metcalfe A, Raman M, Leung Y, Aghajafari F, Letourneau N, et al. Pregnant Women with Inflammatory Bowel Disease Are at Increased Risk of Vitamin D Insufficiency: A Cross-Sectional Study. J Crohns Colitis. 2018;12(6):702–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dove-Medows E, Deriemacker A, Dailey R, Nolan TS, Walker DS, Misra DP, et al. Pregnant African American Women’s Perceptions of Neighborhood, Racial Discrimination, and Psychological Distress as Influences on Birth Outcomes. MCN Am J Matern Child Nurs. 2020;45(1):49–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zhang M, Wan P, Ng K, Singh K, Cheng TH, Velickovic I, et al. Preeclampsia Among African American Pregnant Women: An Update on Prevalence, Complications, Etiology, and Biomarkers. Obstet Gynecol Surv. 2020;75(2):111–20. [DOI] [PubMed] [Google Scholar]
- 67.Mileski MR, Shirey MR, Patrician PA, Childs G. Perceived Racial Discrimination in the Pregnant African American Population: A Concept Analysis. ANS Adv Nurs Sci. 2021;44(4):306–16. [DOI] [PubMed] [Google Scholar]
- 68.Pinder M, Lummis K, Selinger CP. Managing inflammatory bowel disease in pregnancy: current perspectives. Clinical and experimental gastroenterology. 2016;9:325–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cohen BL, Ha C, Ananthakrishnan AN, Rieder F, Bewtra M. State of Adult Trainee Inflammatory Bowel Disease Education in the United States: A National Survey. Inflammatory bowel diseases. 2016;22(7):1609–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mahadevan U How to Get an Education in Inflammatory Bowel Disease During Fellowship: Expectations and Realities. Gastroenterology. 2017;152(8):1813–6. [DOI] [PubMed] [Google Scholar]
- 71.Mahadevan U, Robinson C, Bernasko N, Boland B, Chambers C, Dubinsky M, et al. Inflammatory Bowel Disease in Pregnancy Clinical Care Pathway: A Report From the American Gastroenterological Association IBD Parenthood Project Working Group. Gastroenterology. 2019;156(5):1508–24. [DOI] [PubMed] [Google Scholar]
- 72.Herman AM HA, James SD 3, Ballard BR, M’Koma AE. Inflammatory Bowel Disease On-Line Web-Based Guide to Health Professionals and Patients in Developing and African Nations. Japanise Journal of Gastroenterology and Hepatology. 2020;3(2):1–11. [PMC free article] [PubMed] [Google Scholar]
- 73.Body C, Christie JA. Gastrointestinal Diseases in Pregnancy: Nausea, Vomiting, Hyperemesis Gravidarum, Gastroesophageal Reflux Disease, Constipation, and Diarrhea. Gastroenterol Clin North Am. 2016;45(2):267–83. [DOI] [PubMed] [Google Scholar]
- 74.Passi MMC, Marie B. P-090 African-American Women with Inflammatory Bowel Disease Deliver More Low Birth Weight Infants than White Women. Inflammatory Bowel Diseases 2014(1):S63–S4. [Google Scholar]
- 75.Johnson JE, Roman L, Key KD, Meulen MV, Raffo JE, Luo Z, et al. Study protocol: The Maternal Health Multilevel Intervention for Racial Equity (Maternal Health MIRACLE) Project. Contemp Clin Trials. 2022;120:106894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Alio AP, Dillion T, Hartman S, Johnson T, Turner S, Bullock S, et al. A Community Collaborative for the Exploration of Local Factors Affecting Black Mothers’ Experiences with Perinatal Care. Matern Child Health J. 2022;26(4):751–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gillespie SL, Christian LM, Mackos AR, Nolan TS, Gondwe KW, Anderson CM, et al. Lifetime stressor exposure, systemic inflammation during pregnancy, and preterm birth among Black American women. Brain Behav Immun. 2022;101:266–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Suresh S, Amegashie C, Patel E, Nieman KM, Rana S. Racial Disparities in Diagnosis, Management, and Outcomes in Preeclampsia. Curr Hypertens Rep. 2022;24(4):87–93. [DOI] [PubMed] [Google Scholar]
- 79.Cochrane KM, Hutcheon JA, Karakochuk CD. Iron-Deficiency Prevalence and Supplementation Practices Among Pregnant Women: A Secondary Data Analysis From a Clinical Trial in Vancouver, Canada. J Nutr. 2022;152(10):2238–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Jun S, Gahche JJ, Potischman N, Dwyer JT, Guenther PM, Sauder KA, et al. Dietary Supplement Use and Its Micronutrient Contribution During Pregnancy and Lactation in the United States. Obstet Gynecol. 2020;135(3):623–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lamb CA, Kennedy NA, Raine T, Hendy PA, Smith PJ, Limdi JK, et al. British Society of Gastroenterology consensus guidelines on the management of inflammatory bowel disease in adults. Gut. 2019;68(Suppl 3):s1–s106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Herfarth HH, Kappelman MD, Long MD, Isaacs KL. Use of Methotrexate in the Treatment of Inflammatory Bowel Diseases. Inflammatory bowel diseases. 2016;22(1):224–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Dignass AU, Gasche C, Bettenworth D, Birgegard G, Danese S, Gisbert JP, et al. European consensus on the diagnosis and management of iron deficiency and anaemia in inflammatory bowel diseases. J Crohns Colitis. 2015;9(3):211–22. [DOI] [PubMed] [Google Scholar]
- 84.Hudson M, Flett G, Sinclair TS, Brunt PW, Templeton A, Mowat NA. Fertility and pregnancy in inflammatory bowel disease. Int J Gynaecol Obstet. 1997;58(2):229–37. [DOI] [PubMed] [Google Scholar]
- 85.Sahyoun LC, Gaidos JKJ. A Practical Approach to IBD Care in the Pregnant Patient. Curr Gastroenterol Rep. 2022. [DOI] [PubMed] [Google Scholar]
- 86.Vieujean S, De Vos M, Paridaens K, Daftary GS, Danese S, Peyrin-Biroulet L. Fertility and assisted reproductive technologies outcomes of women with non-surgically managed inflammatory bowel diseases: a systematic review. J Crohns Colitis. 2022. [DOI] [PubMed] [Google Scholar]
- 87.Torres J, Chaparro M, Julsgaard M, Katsanos K, Zelinkova Z, Agrawal M, et al. European Crohn’s and Colitis Guidelines on Sexuality, Fertility, Pregnancy, and Lactation. J Crohns Colitis. 2022. [DOI] [PubMed] [Google Scholar]
- 88.Manosa M, Navarro-Llavat M, Marin L, Zabana Y, Cabre E, Domenech E. Fecundity, pregnancy outcomes, and breastfeeding in patients with inflammatory bowel disease: a large cohort survey. Scand J Gastroenterol. 2013;48(4):427–32. [DOI] [PubMed] [Google Scholar]
- 89.Khosla R, Willoughby CP, Jewell DP. Crohn’s disease and pregnancy. Gut. 1984;25(1):52–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Willoughby CP, Truelove SC. Ulcerative colitis and pregnancy. Gut. 1980;21(6):469–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Lindhagen T, Bohe M, Ekelund G, Valentin L. Fertility and outcome of pregnancy in patients operated on for Crohn’s disease. Int J Colorectal Dis. 1986;1(1):25–7. [DOI] [PubMed] [Google Scholar]
- 92.De Dombal FT, Burton IL, Goligher JC. Crohn’s disease and pregnancy. Br Med J. 1972;3(5826):550–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mayberry JF, Weterman IT. European survey of fertility and pregnancy in women with Crohn’s disease: a case control study by European collaborative group. Gut. 1986;27(7):821–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Moody GA, Probert C, Jayanthi V, Mayberry JF. The effects of chronic ill health and treatment with sulphasalazine on fertility amongst men and women with inflammatory bowel disease in Leicestershire. Int J Colorectal Dis. 1997;12(4):220–4. [DOI] [PubMed] [Google Scholar]
- 95.Arkuran C, McComb P. Crohn’s disease and tubal infertility: the effect of adhesion formation. Clin Exp Obstet Gynecol. 2000;27(1):12–3. [PubMed] [Google Scholar]
- 96.M’Koma AE. Observation on essential biochemical data profile in connection with restorative proctocolectomy in humans. Vitamin B12 and fat absorption cited. Dissertation Thesis. 2001:1–126. [Google Scholar]
- 97.Waljee A, Waljee J, Morris AM, Higgins PD. Threefold increased risk of infertility: a meta-analysis of infertility after ileal pouch anal anastomosis in ulcerative colitis. Gut. 2006;55(11):1575–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Cornish J, Tan E, Teare J, Teoh TG, Rai R, Clark SK, et al. A meta-analysis on the influence of inflammatory bowel disease on pregnancy. Gut. 2007;56(6):830–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Rajaratnam SG, Eglinton TW, Hider P, Fearnhead NS. Impact of ileal pouch-anal anastomosis on female fertility: meta-analysis and systematic review. Int J Colorectal Dis. 2011;26(11):1365–74. [DOI] [PubMed] [Google Scholar]
- 100.Tulchinsky H, Averboukh F, Horowitz N, Rabau M, Klausner JM, Halpern Z, et al. Restorative proctocolectomy impairs fertility and pregnancy outcomes in women with ulcerative colitis. Colorectal Dis. 2013;15(7):842–7. [DOI] [PubMed] [Google Scholar]
- 101.Hull TL, Joyce MR, Geisler DP, Coffey JC. Adhesions after laparoscopic and open ileal pouch-anal anastomosis surgery for ulcerative colitis. Br J Surg. 2012;99(2):270–5. [DOI] [PubMed] [Google Scholar]
- 102.Beyer-Berjot L, Maggiori L, Birnbaum D, Lefevre JH, Berdah S, Panis Y. A total laparoscopic approach reduces the infertility rate after ileal pouch-anal anastomosis: a 2-center study. Ann Surg. 2013;258(2):275–82. [DOI] [PubMed] [Google Scholar]
- 103.Bartels SA, D’Hoore A, Cuesta MA, Bensdorp AJ, Lucas C, Bemelman WA. Significantly increased pregnancy rates after laparoscopic restorative proctocolectomy: a cross-sectional study. Ann Surg. 2012;256(6):1045–8. [DOI] [PubMed] [Google Scholar]
- 104.Tavernier N, Fumery M, Peyrin-Biroulet L, Colombel JF, Gower-Rousseau C. Systematic review: fertility in non-surgically treated inflammatory bowel disease. Aliment Pharmacol Ther. 2013;38(8):847–53. [DOI] [PubMed] [Google Scholar]
- 105.Vieujean S, De Vos M, D’Amico F, Paridaens K, Daftary G, Dudkowiak R, et al. Inflammatory bowel disease meets fertility: A physician and patient survey. Dig Liver Dis. 2023. [DOI] [PubMed] [Google Scholar]
- 106.Huang VW, Chang HJ, Kroeker KI, Goodman KJ, Hegadoren KM, Dieleman LA, et al. Does the level of reproductive knowledge specific to inflammatory bowel disease predict childlessness among women with inflammatory bowel disease? Can J Gastroenterol Hepatol. 2015;29(2):95–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Hardeman RR, Karbeah J, Kozhimannil KB. Applying a critical race lens to relationship-centered care in pregnancy and childbirth: An antidote to structural racism. Birth. 2020;47(1):3–7. [DOI] [PubMed] [Google Scholar]
- 108.Hardeman RR, Karbeah J. Examining racism in health services research: A disciplinary self-critique. Health Serv Res. 2020;55 Suppl 2(Suppl 2):777–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health. 2000;90(8):1212–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Williams DR, Sternthal M. Understanding racial-ethnic disparities in health: sociological contributions. J Health Soc Behav. 2010;51 Suppl(Suppl):S15–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Cushing L, Faust J, August LM, Cendak R, Wieland W, Alexeeff G. Racial/Ethnic Disparities in Cumulative Environmental Health Impacts in California: Evidence From a Statewide Environmental Justice Screening Tool (CalEnviroScreen 1.1). Am J Public Health. 2015;105(11):2341–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Moriya AS, Chakravarty S. Racial And Ethnic Disparities In Preventable Hospitalizations And ED Visits Five Years After ACA Medicaid Expansions. Health affairs. 2023;42(1):26–34. [DOI] [PubMed] [Google Scholar]
- 113.Braveman PA AE, Proctor D, Kauh T, Holm N. Systemic And Structural Racism:Definitions, Examples, HealthDamages, and Approaches To Dismantling. Health affairs. 2022;41(2):171–8. [DOI] [PubMed] [Google Scholar]
- 114.Kauh TJ, Read JG, Scheitler AJ. The Critical Role of Racial/Ethnic Data Disaggregation for Health Equity. Popul Res Policy Rev. 2021;40(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Bailey ZD, Krieger N, Agenor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453–63. [DOI] [PubMed] [Google Scholar]
- 116.Camara P, Jones. Confronting Institutionalized Racism: Clark Atlanta University; 2002. [Google Scholar]
- 117.Chirwa S, Nwabuisi CR, Ladson GM, Korley L, Whitty JE, Atkinson R, et al. Poor Sleep Quality Is Associated with Higher Hemoglobin A1c in Pregnant Women: A Pilot Observational Study. International journal of environmental research and public health. 2018;15(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ananthakrishnan AN, Long MD, Martin CF, Sandler RS, Kappelman MD. Sleep disturbance and risk of active disease in patients with Crohn’s disease and ulcerative colitis. Clin Gastroenterol Hepatol. 2013;11(8):965–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Sobolewska-Wlodarczyk A, Wlodarczyk M, Banasik J, Gasiorowska A, Wisniewska-Jarosinska M, Fichna J. Sleep disturbance and disease activity in adult patients with inflammatory bowel diseases. J Physiol Pharmacol. 2018;69(3). [DOI] [PubMed] [Google Scholar]
- 120.Ranjbaran Z, Keefer L, Farhadi A, Stepanski E, Sedghi S, Keshavarzian A. Impact of sleep disturbances in inflammatory bowel disease. J Gastroenterol Hepatol. 2007;22(11):1748–53. [DOI] [PubMed] [Google Scholar]
- 121.Vedamurthy A, Ananthakrishnan AN. Influence of Environmental Factors in the Development and Outcomes of Inflammatory Bowel Disease. Gastroenterol Hepatol (N Y). 2019;15(2):72–82. [PMC free article] [PubMed] [Google Scholar]
- 122.Qazi T, Farraye FA. Sleep and Inflammatory Bowel Disease: An Important Bi-Directional Relationship. Inflammatory bowel diseases. 2019;25(5):843–52. [DOI] [PubMed] [Google Scholar]
- 123.Francis B, Klebanoff M, Oza-Frank R. Racial discrimination and perinatal sleep quality. Sleep Health. 2017;3(4):300–5. [DOI] [PubMed] [Google Scholar]
- 124.Cohen MF, Corwin EJ, Johnson DA, Amore AD, Brown AL, Barbee NR, et al. Discrimination is associated with poor sleep quality in pregnant Black American women. Sleep Med. 2022;100:39–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Alhalel J, Patterson L, Francone NO, Danner S, Osei C, O’Brian CA, et al. Addressing racial disparities in perinatal care for African American/Black individuals in the Chicago community health setting: a qualitative study. BMC Pregnancy Childbirth. 2022;22(1):771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Marinelli C, Savarino EV, Marsilio I, Lorenzon G, Gavaruzzi T, D’Inca R, et al. Sleep disturbance in Inflammatory Bowel Disease: prevalence and risk factors - A cross-sectional study. Sci Rep. 2020;10(1):507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Nassikas N, Malhame I, Miller M, Bourjeily G. Pulmonary Considerations for Pregnant Women. Clin Chest Med. 2021;42(3):483–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Holdcroft A, Bevan DR, O’Sullivan JC, Sykes MK. Airway closure and pregnancy. Anaesthesia. 1977;32(6):517–23. [DOI] [PubMed] [Google Scholar]
- 129.Middleton PG. Obstructive sleep apnoea and sleep disorders in pregnancy. Best Pract Res Clin Obstet Gynaecol. 2022;85(Pt A):107–13. [DOI] [PubMed] [Google Scholar]
- 130.Brown NT, Turner JM, Kumar S. The intrapartum and perinatal risks of sleep-disordered breathing in pregnancy: a systematic review and metaanalysis. Am J Obstet Gynecol. 2018;219(2):147–61 e1. [DOI] [PubMed] [Google Scholar]
- 131.Oyiengo D, Louis M, Hott B, Bourjeily G. Sleep disorders in pregnancy. Clin Chest Med. 2014;35(3):571–87. [DOI] [PubMed] [Google Scholar]
- 132.Franklin KA, Holmgren PA, Jonsson F, Poromaa N, Stenlund H, Svanborg E. Snoring, pregnancy-induced hypertension, and growth retardation of the fetus. Chest. 2000;117(1):137–41. [DOI] [PubMed] [Google Scholar]
- 133.O’Brien LM, Bullough AS, Chames MC, Shelgikar AV, Armitage R, Guilleminualt C, et al. Hypertension, snoring, and obstructive sleep apnoea during pregnancy: a cohort study. BJOG : an international journal of obstetrics and gynaecology. 2014;121(13):1685–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Edwards N, Blyton DM, Kirjavainen T, Kesby GJ, Sullivan CE. Nasal continuous positive airway pressure reduces sleep-induced blood pressure increments in preeclampsia. Am J Respir Crit Care Med. 2000;162(1):252–7. [DOI] [PubMed] [Google Scholar]
- 135.Blyton DM, Sullivan CE, Edwards N. Reduced nocturnal cardiac output associated with preeclampsia is minimized with the use of nocturnal nasal CPAP. Sleep. 2004;27(1):79–84. [DOI] [PubMed] [Google Scholar]
- 136.Pilkington S, Carli F, Dakin MJ, Romney M, De Witt KA, Dore CJ, et al. Increase in Mallampati score during pregnancy. Br J Anaesth. 1995;74(6):638–42. [DOI] [PubMed] [Google Scholar]
- 137.Sedov ID, Cameron EE, Madigan S, Tomfohr-Madsen LM. Sleep quality during pregnancy: A meta-analysis. Sleep Med Rev. 2018;38:168–76. [DOI] [PubMed] [Google Scholar]
- 138.Sullivan CE, Issa FG, Berthon-Jones M, Eves L. Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet. 1981;1(8225):862–5. [DOI] [PubMed] [Google Scholar]
- 139.Blyton DM, Skilton MR, Edwards N, Hennessy A, Celermajer DS, Sullivan CE. Treatment of sleep disordered breathing reverses low fetal activity levels in preeclampsia. Sleep. 2013;36(1):15–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Garbazza C, Hackethal S, Riccardi S, Cajochen C, Cicolin A, D’Agostino A, et al. Polysomnographic features of pregnancy: A systematic review. Sleep Med Rev. 2020;50:101249. [DOI] [PubMed] [Google Scholar]
- 141.Carvalho KM, Figueiredo M, Galindo Neto NM, Sa GGM, Silva C, Mendes PN. Comparison of the effectiveness of two educational interventions on sleep quality in older adults: a randomized clinical trial. Rev Esc Enferm USP. 2022;56:e20220326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Singh AH, Bathla M, Gupta P, Bhusri L. Quality of sleep and disability associated with headache: migraine versus tension-type headache: A comparative study. Ann Afr Med. 2023;22(1):11–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Sweeney BM, Signal TL, Babbage DR. Effect of a behavioral-educational sleep intervention for first-time mothers and their infants: pilot of a controlled trial. J Clin Sleep Med. 2020;16(8):1265–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Ladyman C, Gander P, Huthwaite M, Sweeney B, Signal TL. Sleep HAPi: A Feasibility and Descriptive Analysis of an Early and Longitudinal Sleep Education Intervention for Pregnant Women. Behav Sleep Med. 2021;19(4):427–44. [DOI] [PubMed] [Google Scholar]
- 145.Gessesse DN, Tsega NT, Aklil MB, Temesgan WZ, Abegaz MY, Anteneh TA, et al. Prevalence and associated factors of poor sleep quality among postpartum women in North West Ethiopia: a community-based study. BMC Psychiatry. 2022;22(1):538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Lucchini M, O’Brien LM, Kahn LG, Brennan PA, Glazer Baron K, Knapp EA, et al. Racial/ethnic disparities in subjective sleep duration, sleep quality, and sleep disturbances during pregnancy: an ECHO study. Sleep. 2022;45(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Felix NAR, Ceolim MF. Sleep in pregnancy quarters: a longitudinal study. Rev Gaucha Enferm. 2022;44:e20210278. [DOI] [PubMed] [Google Scholar]
- 148.Cai YM, Zheng XL, Shen ZM, Zhou BF, Liu YM, Yang JY, et al. Study on the sleep quality of women pregnant with a second child and the influencing factors. Eur J Med Res. 2022;27(1):207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Wirth MD, Liu J, Wallace MK, McLain AC, Turner-McGrievy GM, Davis JE, et al. Dietary Inflammatory Index and sleep quality and duration among pregnant women with overweight or obesity. Sleep. 2022;45(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Lau Y, Cheng LJ, Chee DGH, Zhao M, Wong SH, Wong SN, et al. High body mass index and sleep problems during pregnancy: A meta-analysis and meta-regression of observational studies. J Sleep Res. 2022;31(1):e13443. [DOI] [PubMed] [Google Scholar]
- 151.Ghante A, Raj JP, Krishna B, Thomas A. Prevalence and predictors of sleep deprivation and poor sleep quality and their associated perinatal outcomes during the third trimester of pregnancy. J Taibah Univ Med Sci. 2021;16(3):359–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Cao V, Makarem N, Maguire M, Samayoa I, Xi H, Liang C, et al. History of Weight Cycling Is Prospectively Associated With Shorter and Poorer-Quality Sleep and Higher Sleep Apnea Risk in Diverse US Women. J Cardiovasc Nurs. 2021;36(6):573–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Papadopoulou SK, Mantzorou M, Voulgaridou G, Pavlidou E, Vadikolias K, Antasouras G, et al. Nutritional Status Is Associated with Health-Related Quality of Life, Physical Activity, and Sleep Quality: A Cross-Sectional Study in an Elderly Greek Population. Nutrients. 2023;15(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Bei B, Pinnington DM, Shen L, Blumfield M, Drummond SPA, Newman LK, et al. A scalable cognitive behavioural program to promote healthy sleep during pregnancy and postpartum periods: protocol of a randomised controlled trial (the SEED project). BMC Pregnancy Childbirth. 2019;19(1):254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Rezaei E, Moghadam ZB, Nejat S, Dehghannayeri N. The impact of sleep healthy behavior education on the quality of life in the pregnant women with sleep disorder: A randomized control trial in the year 2012. Iran J Nurs Midwifery Res. 2014;19(5):508–16. [PMC free article] [PubMed] [Google Scholar]
- 156.Hayase M, Shimada M, Seki H. Sleep quality and stress in women with pregnancy-induced hypertension and gestational diabetes mellitus. Women Birth. 2014;27(3):190–5. [DOI] [PubMed] [Google Scholar]
- 157.Umeno S, Kato C, Nagaura Y, Kondo H, Eto H. Characteristics of sleep/wake problems and delivery outcomes among pregnant Japanese women without gestational complications. BMC Pregnancy Childbirth. 2020;20(1):179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Felder JN, Roubinov D, Zhang L, Gray M, Beck A. Endorsement of a single-item measure of sleep disturbance during pregnancy and risk for postpartum depression: a retrospective cohort study. Arch Womens Ment Health. 2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Baattaiah BA, Alharbi MD, Babteen NM, Al-Maqbool HM, Babgi FA, Albatati AA. The relationship between fatigue, sleep quality, resilience, and the risk of postpartum depression: an emphasis on maternal mental health. BMC Psychol. 2023;11(1):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Brekke M, Amro A, Smastuen MC, Glavin K, Solberg B, Oygarden AU, et al. Quality of life in Norwegian pregnant women and men with pregnant partners, and association with perception of sleep and depressive symptoms: a cross-sectional study. BMC Pregnancy Childbirth. 2023;23(1):37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Vanderlinden J, Boen F, van Uffelen JGZ. Effects of physical activity programs on sleep outcomes in older adults: a systematic review. Int J Behav Nutr Phys Act. 2020;17(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Das S, Roy RN, Das DK, Chakraborty A, Mondal R. Sleep Quality and its various correlates: A community-based study among geriatric population in a community development block of Purba Bardhaman district, West Bengal. J Family Med Prim Care. 2020;9(3):1510–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Ngui EM, Warner TD, Roberts LW. Perceptions of African-American health professionals and community members on the participation of children and pregnant women in genetic research. Public Health Genomics. 2014;17(1):23–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Thomas SB, Fine MJ, Ibrahim SA. Health disparities: the importance of culture and health communication. Am J Public Health. 2004;94(12):2050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Boutron I, Moher D, Altman DG, Schulz KF, Ravaud P, Group C. Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: explanation and elaboration. Ann Intern Med. 2008;148(4):295–309. [DOI] [PubMed] [Google Scholar]
- 166.Aniwan S, Harmsen WS, Tremaine WJ, Loftus EV Jr. Incidence of inflammatory bowel disease by race and ethnicity in a population-based inception cohort from 1970 through 2010. Therap Adv Gastroenterol. 2019;12:1756284819827692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Misra R, Faiz O, Munkholm P, Burisch J, Arebi N. Epidemiology of inflammatory bowel disease in racial and ethnic migrant groups. World J Gastroenterol. 2018;24(3):424–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Nguyen GC, Torres EA, Regueiro M, Bromfield G, Bitton A, Stempak J, et al. Inflammatory bowel disease characteristics among African Americans, Hispanics, and non-Hispanic Whites: characterization of a large North American cohort. Am J Gastroenterol. 2006;101(5):1012–23. [DOI] [PubMed] [Google Scholar]
- 169.Nguyen GC, Tuskey A, Dassopoulos T, Harris ML, Brant SR. Rising hospitalization rates for inflammatory bowel disease in the United States between 1998 and 2004. Inflammatory bowel diseases. 2007;13(12):1529–35. [DOI] [PubMed] [Google Scholar]
- 170.Nguyen GC, LaVeist TA, Harris ML, Wang MH, Datta LW, Brant SR. Racial disparities in utilization of specialist care and medications in inflammatory bowel disease. Am J Gastroenterol. 2010;105(10):2202–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Nguyen GC, Bouchard S, Diong C, Promoting A, Care through Centres of Excellence N. Access to Specialists and Emergency Department Visits in Inflammatory Bowel Disease: A Population-Based Study. J Crohns Colitis. 2019;13(3):330–6. [DOI] [PubMed] [Google Scholar]
- 172.Habal FM, Huang VW. Review article: a decision-making algorithm for the management of pregnancy in the inflammatory bowel disease patient. Aliment Pharmacol Ther. 2012;35(5):501–15. [DOI] [PubMed] [Google Scholar]
- 173.Pofi R, Tomlinson JW. Glucocorticoids in pregnancy. Obstet Med. 2020;13(2):62–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Evans LM, Myers MM, Monk C. Pregnant women’s cortisol is elevated with anxiety and depression - but only when comorbid. Arch Womens Ment Health. 2008;11(3):239–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Bortoli A, Pedersen N, Duricova D, D’Inca R, Gionchetti P, Panelli MR, et al. Pregnancy outcome in inflammatory bowel disease: prospective European case-control ECCO-EpiCom study, 2003–2006. Aliment Pharmacol Ther. 2011;34(7):724–34. [DOI] [PubMed] [Google Scholar]
- 176.Norgard B, Hundborg HH, Jacobsen BA, Nielsen GL, Fonager K. Disease activity in pregnant women with Crohn’s disease and birth outcomes: a regional Danish cohort study. Am J Gastroenterol. 2007;102(9):1947–54. [DOI] [PubMed] [Google Scholar]
- 177.Hatch Q, Champagne BJ, Maykel JA, Davis BR, Johnson EK, Bleier JS, et al. Crohn’s disease and pregnancy: the impact of perianal disease on delivery methods and complications. Dis Colon Rectum. 2014;57(2):174–8. [DOI] [PubMed] [Google Scholar]
- 178.van der Woude CJ, Ardizzone S, Bengtson MB, Fiorino G, Fraser G, Katsanos K, et al. The second European evidenced-based consensus on reproduction and pregnancy in inflammatory bowel disease. J Crohns Colitis. 2015;9(2):107–24. [DOI] [PubMed] [Google Scholar]
- 179.Panes J, Bouzas R, Chaparro M, Garcia-Sanchez V, Gisbert JP, Martinez de Guerenu B, et al. Systematic review: the use of ultrasonography, computed tomography and magnetic resonance imaging for the diagnosis, assessment of activity and abdominal complications of Crohn’s disease. Aliment Pharmacol Ther. 2011;34(2):125–45. [DOI] [PubMed] [Google Scholar]
- 180.Schulze H, Esters P, Dignass A. Review article: the management of Crohn’s disease and ulcerative colitis during pregnancy and lactation. Aliment Pharmacol Ther. 2014;40(9):991–1008. [DOI] [PubMed] [Google Scholar]
- 181.Tremblay E, Therasse E, Thomassin-Naggara I, Trop I. Quality initiatives: guidelines for use of medical imaging during pregnancy and lactation. Radiographics. 2012;32(3):897–911. [DOI] [PubMed] [Google Scholar]
- 182.Haq AI, Sahai A, Hallwoth S, Rampton DS, Dorudi S. Synchronous colectomy and caesarean section for fulminant ulcerative colitis: case report and review of the literature. Int J Colorectal Dis. 2006;21(5):465–9. [DOI] [PubMed] [Google Scholar]
- 183.Overbey D, Govekar H, Gajdos C. Surgical management of colonic perforation due to ulcerative colitis during pregnancy: Report of a case. World journal of gastrointestinal surgery. 2014;6(10):201–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Naganuma M, Kunisaki R, Yoshimura N, Nagahori M, Yamamoto H, Kimura H, et al. Conception and pregnancy outcome in women with inflammatory bowel disease: A multicentre study from Japan. J Crohns Colitis. 2011;5(4):317–23. [DOI] [PubMed] [Google Scholar]
- 185.Nielsen OH, Gubatan JM, Juhl CB, Streett SE, Maxwell C. Biologics for Inflammatory Bowel Disease and Their Safety in Pregnancy: A Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol. 2022;20(1):74–87 e3. [DOI] [PubMed] [Google Scholar]
- 186.Mahadevan U, Robinson C, Bernasko N, Boland B, Chambers C, Dubinsky M, et al. Inflammatory Bowel Disease in Pregnancy Clinical Care Pathway: A Report From the American Gastroenterological Association IBD Parenthood Project Working Group. Am J Obstet Gynecol. 2019;220(4):308–23. [DOI] [PubMed] [Google Scholar]
- 187.Abhyankar A, Ham M, Moss AC. Meta-analysis: the impact of disease activity at conception on disease activity during pregnancy in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2013;38(5):460–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Erlebacher A Immunology of the maternal-fetal interface. Annu Rev Immunol. 2013;31:387–411. [DOI] [PubMed] [Google Scholar]
- 189.Ronchetti C, Cirillo F, Di Segni N, Cristodoro M, Busnelli A, Levi-Setti PE. Inflammatory Bowel Disease and Reproductive Health: From Fertility to Pregnancy-A Narrative Review. Nutrients. 2022;14(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Seifarth C, Ritz JP, Pohlen U, Kroesen AJ, Siegmund B, Frericks B, et al. Therapy of complicated Crohn’s disease during pregnancy--an interdisciplinary challenge. Int J Colorectal Dis. 2014;29(6):645–51. [DOI] [PubMed] [Google Scholar]
- 191.Walldorf J, Zwirnmann K, Seufferlein T. [Pregnancy and inflammatory bowel disease]. Internist (Berl). 2011;52(1):76, 8–80. [DOI] [PubMed] [Google Scholar]
- 192.van der Giessen J, Binyamin D, Belogolovski A, Frishman S, Tenenbaum-Gavish K, Hadar E, et al. Modulation of cytokine patterns and microbiome during pregnancy in IBD. Gut. 2020;69(3):473–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Kim ES, Tarassishin L, Eisele C, Barre A, Nair N, Rendon A, et al. Longitudinal Changes in Fecal Calprotectin Levels Among Pregnant Women With and Without Inflammatory Bowel Disease and Their Babies. Gastroenterology. 2021;160(4):1118–30e3. [DOI] [PubMed] [Google Scholar]
- 194.Toomey D, Waldron B. Family planning and inflammatory bowel disease: the patient and the practitioner. Fam Pract. 2013;30(1):64–8. [DOI] [PubMed] [Google Scholar]
- 195.Walldorf J, Pijan E, Greinert R, Riesner-Wehner A, Michl P. Family planning with inflammatory bowel disease: the challenge of childlessness and parent concerns. Z Gastroenterol. 2021;59(8):841–50. [DOI] [PubMed] [Google Scholar]
- 196.Flanagan E, Wright EK, Sparrow MP, Moore GT, Connell WR, De Cruz P, et al. A Single Educational Intervention Improves Pregnancy-Related Knowledge and Emotional Health Among Women With IBD Who Are Pregnant or Wish to Conceive. Inflammatory bowel diseases. 2021;27(12):1909–18. [DOI] [PubMed] [Google Scholar]
- 197.Tsuda S, Sameshima A, Sekine M, Kawaguchi H, Fujita D, Makino S, et al. Pre-conception status, obstetric outcome and use of medications during pregnancy of systemic lupus erythematosus (SLE), rheumatoid arthritis (RA) and inflammatory bowel disease (IBD) in Japan: Multi-center retrospective descriptive study. Mod Rheumatol. 2020;30(5):852–61. [DOI] [PubMed] [Google Scholar]
- 198.Gawron LM, Goldberger AR, Gawron AJ, Hammond C, Keefer L. Disease-related pregnancy concerns and reproductive planning in women with inflammatory bowel diseases. J Fam Plann Reprod Health Care. 2015;41(4):272–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Gawron LM, Hammond C, Keefer L. Documentation of reproductive health counseling and contraception in women with inflammatory bowel diseases. Patient Educ Couns. 2014;94(1):134–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Steinlauf AF, Present DH. Medical management of the pregnant patient with inflammatory bowel disease. Gastroenterol Clin North Am. 2004;33(2):361–85, xi. [DOI] [PubMed] [Google Scholar]
- 201.Dos Santos Marques IC, Theiss LM, Baker SJ, Liwo A, Wood LN, Cannon JA, et al. Low Health Literacy Exists in the Inflammatory Bowel Disease (IBD) Population and Is Disproportionately Prevalent in Older African Americans. Crohns Colitis 360. 2020;2(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Dos Santos Marques IC, Herbey II, Theiss LM, Shao CC, Fouad MN, Scarinci IC, et al. Understanding the surgical experience for Black and White patients with inflammatory bowel disease (IBD): The importance of health literacy. Am J Surg. 2022;223(2):303–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Kaps L, Omogbehin L, Hildebrand K, Gairing SJ, Schleicher EM, Moehler M, et al. Health literacy in gastrointestinal diseases: a comparative analysis between patients with liver cirrhosis, inflammatory bowel disease and gastrointestinal cancer. Sci Rep. 2022;12(1):21072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Mehra R, Alspaugh A, Dunn JT, Franck LS, McLemore MR, Keene DE, et al. “‘Oh gosh, why go?’ cause they are going to look at me and not hire”: intersectional experiences of black women navigating employment during pregnancy and parenting. BMC Pregnancy Childbirth. 2023;23(1):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Liese K, Stewart K, Pearson P, Lofton S, Mbande T, Patil C, et al. Melanated Group Midwifery Care: Centering the Voices of the Black Birthing Community. J Midwifery Womens Health. 2022;67(6):696–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Chaparro M, Donday MG, Abad-Santos F, Martin de Carpi FJ, Macia-Martinez MA, Montero D, et al. The safety of drugs for inflammatory bowel disease during pregnancy and breastfeeding: the DUMBO registry study protocol of GETECCU. Therap Adv Gastroenterol. 2021;14:17562848211018097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Laube R, Paramsothy S, Leong RW. Use of medications during pregnancy and breastfeeding for Crohn’s disease and ulcerative colitis. Expert Opin Drug Saf. 2021;20(3):275–92. [DOI] [PubMed] [Google Scholar]
- 208.Gubatan J, Nielsen OH, Levitte S, Juhl CB, Maxwell C, Streett SE, et al. Biologics During Pregnancy in Women With Inflammatory Bowel Disease and Risk of Infantile Infections: A Systematic Review and Meta-Analysis. Am J Gastroenterol. 2021;116(2):243–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Pedersen N, Bortoli A, Duricova D, R DI, Panelli MR, Gisbert JP, et al. The course of inflammatory bowel disease during pregnancy and postpartum: a prospective European ECCO-EpiCom Study of 209 pregnant women. Aliment Pharmacol Ther. 2013;38(5):501–12. [DOI] [PubMed] [Google Scholar]
- 210.de Lima A, Zelinkova Z, Mulders AG, van der Woude CJ. Preconception Care Reduces Relapse of Inflammatory Bowel Disease During Pregnancy. Clin Gastroenterol Hepatol. 2016;14(9):1285–92 e1. [DOI] [PubMed] [Google Scholar]
- 211.Friedman SH, Heneghan A, Rosenthal M. Characteristics of women who do not seek prenatal care and implications for prevention. J Obstet Gynecol Neonatal Nurs. 2009;38(2):174–81. [DOI] [PubMed] [Google Scholar]
- 212.Clark EC, Cranston E, Polin T, Ndumbe-Eyoh S, MacDonald D, Betker C, et al. Structural interventions that affect racial inequities and their impact on population health outcomes: a systematic review. BMC Public Health. 2022;22(1):2162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Jeffers NK, Berger BO, Marea CX, Gemmill A. Investigating the impact of structural racism on black birthing people - associations between racialized economic segregation, incarceration inequality, and severe maternal morbidity. Soc Sci Med. 2023;317:115622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.OjiNjideka Hemphill N, Crooks N, Zhang W, Fitter F, Erbe K, Rutherford JN, et al. Obstetric experiences of young black mothers: An intersectional perspective. Soc Sci Med. 2023;317:115604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Gao X, Snowden JM, Tucker CM, Allen A, Morello-Frosch R, Abrams B, et al. Remapping racial and ethnic inequities in severe maternal morbidity: The legacy of redlining in California. Paediatr Perinat Epidemiol. 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Maternal, Child Nutrition Study G, Group m, Black RE, Alderman H, Bhutta ZA, et al. Maternal and child nutrition: building momentum for impact. Lancet. 2013;382(9890):372–5. [DOI] [PubMed] [Google Scholar]
- 217.Plaza-Diaz J, Ruiz-Ojeda FJ, Morales J, de la Torre AIC, Garcia-Garcia A, de Prado CN, et al. Effects of a Novel Infant Formula on Weight Gain, Body Composition, Safety and Tolerability to Infants: The INNOVA 2020 Study. Nutrients. 2022;15(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Auestad N, Scott DT, Janowsky JS, Jacobsen C, Carroll RE, Montalto MB, et al. Visual, cognitive, and language assessments at 39 months: a follow-up study of children fed formulas containing long-chain polyunsaturated fatty acids to 1 year of age. Pediatrics. 2003;112(3 Pt 1):e177–83. [DOI] [PubMed] [Google Scholar]
- 219.Ip S, Chung M, Raman G, Trikalinos TA, Lau J. A summary of the Agency for Healthcare Research and Quality’s evidence report on breastfeeding in developed countries. Breastfeed Med. 2009;4 Suppl 1:S17–30. [DOI] [PubMed] [Google Scholar]
- 220.Mahadevan U, Robinson C, Bernasko N, Boland B, Chambers C, Dubinsky M, et al. Inflammatory Bowel Disease in Pregnancy Clinical Care Pathway: A Report From the American Gastroenterological Association IBD Parenthood Project Working Group. Inflammatory bowel diseases. 2019;25(4):627–41. [DOI] [PubMed] [Google Scholar]
- 221.Kokoszko-Bilska A, Sobkiewicz S, Fichna J. Inflammatory bowel diseases and reproductive health. Pharmacol Rep. 2016;68(4):859–64. [DOI] [PubMed] [Google Scholar]
- 222.Selinger CP, Leong RW, Lal S. Pregnancy related issues in inflammatory bowel disease: evidence base and patients’ perspective. World J Gastroenterol. 2012;18(21):2600–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Maliszewska AM, Warska A, Cendrowski K, Sawicki W. Inflammatory bowel disease and pregnancy. Ginekol Pol. 2017;88(7):398–403. [DOI] [PubMed] [Google Scholar]
- 224.Ellul P, Zammita SC, Katsanos KH, Cesarini M, Allocca M, Danese S, et al. Perception of Reproductive Health in Women with Inflammatory Bowel Disease. J Crohns Colitis. 2016;10(8):886–91. [DOI] [PubMed] [Google Scholar]
- 225.Kushner T, Fairchild A, Johnson FR, Sands BE, Mahadevan U, Subramanian S, et al. Women’s Willingness to Accept Risks of Medication for Inflammatory Bowel Disease During Pregnancy. Patient. 2022;15(3):353–65. [DOI] [PubMed] [Google Scholar]
- 226.Long MD, Siegel CA, Abraham BP, Chiorean M, Mahadevan U. Day Care Attendance and Infectious Complications in Children Born to Mothers With Inflammatory Bowel Disease. Clin Gastroenterol Hepatol. 2022;20(3):706–8 e1. [DOI] [PubMed] [Google Scholar]
- 227.Mahadevan U, Long MD, Kane SV, Roy A, Dubinsky MC, Sands BE, et al. Pregnancy and Neonatal Outcomes After Fetal Exposure to Biologics and Thiopurines Among Women With Inflammatory Bowel Disease. Gastroenterology. 2021;160(4):1131–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Bengtson MB, Aamodt G, Mahadevan U, Vatn MH. Inadequate Gestational Weight Gain, the Hidden Link Between Maternal IBD and Adverse Pregnancy Outcomes: Results from the Norwegian Mother and Child Cohort Study. Inflammatory bowel diseases. 2017;23(7):1225–33. [DOI] [PubMed] [Google Scholar]
- 229.Bengtson MB, Haugen M, Brantsaeter AL, Aamodt G, Vatn MH. Intake of dairy protein during pregnancy in IBD and risk of SGA in a Norwegian population-based mother and child cohort. BMC Gastroenterol. 2020;20(1):28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Myklebust-Hansen T, Aamodt G, Haugen M, Brantsaeter AL, Vatn MH, Bengtson MB. Dietary Patterns in women with Inflammatory Bowel Disease and Risk of Adverse Pregnancy Outcomes: Results from The Norwegian Mother and Child Cohort Study (MoBa). Inflammatory bowel diseases. 2017;24(1):12–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Picardo S, Seow CH. A Pharmacological Approach to Managing Inflammatory Bowel Disease During Conception, Pregnancy and Breastfeeding: Biologic and Oral Small Molecule Therapy. Drugs. 2019;79(10):1053–63. [DOI] [PubMed] [Google Scholar]
- 232.Horst S, Kane S. The use of biologic agents in pregnancy and breastfeeding. Gastroenterol Clin North Am. 2014;43(3):495–508. [DOI] [PubMed] [Google Scholar]
- 233.Wang H, Hu Y, Chen F, Shen M. Comparative safety of infliximab and adalimumab on pregnancy outcomes of women with inflammatory bowel diseases: a systematic review & meta-analysis. BMC Pregnancy Childbirth. 2022;22(1):854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Clowse M, Fischer-Betz R, Nelson-Piercy C, Scheuerle AE, Stephan B, Dubinsky M, et al. Pharmacovigilance pregnancy data in a large population of patients with chronic inflammatory disease exposed to certolizumab pegol. Ther Adv Musculoskelet Dis. 2022;14:1759720X221087650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Wiersma TK, Visschedijk MC, de Boer NK, Lub-de Hooge MN, Prins JR, Touw DJ, et al. The Effect of Pregnancy and Inflammatory Bowel Disease on the Pharmacokinetics of Drugs Related to Inflammatory Bowel Disease-A Systematic Literature Review. Pharmaceutics. 2022;14(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Wieringa JW, Driessen GJ, Van Der Woude CJ. Pregnant women with inflammatory bowel disease: the effects of biologicals on pregnancy, outcome of infants, and the developing immune system. Expert Rev Gastroenterol Hepatol. 2018;12(8):811–8. [DOI] [PubMed] [Google Scholar]
- 237.Matro R, Martin CF, Wolf D, Shah SA, Mahadevan U. Exposure Concentrations of Infants Breastfed by Women Receiving Biologic Therapies for Inflammatory Bowel Diseases and Effects of Breastfeeding on Infections and Development. Gastroenterology. 2018;155(3):696–704. [DOI] [PubMed] [Google Scholar]
- 238.Beaulieu DB, Ananthakrishnan AN, Martin C, Cohen RD, Kane SV, Mahadevan U. Use of Biologic Therapy by Pregnant Women With Inflammatory Bowel Disease Does Not Affect Infant Response to Vaccines. Clin Gastroenterol Hepatol. 2018;16(1):99–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Julsgaard M, Christensen LA, Gibson PR, Gearry RB, Fallingborg J, Hvas CL, et al. Concentrations of Adalimumab and Infliximab in Mothers and Newborns, and Effects on Infection. Gastroenterology. 2016;151(1):110–9. [DOI] [PubMed] [Google Scholar]
- 240.Weiss B, Ben-Horin S, Lev A, Broide E, Yavzori M, Lahat A, et al. Immune function in newborns with in-utero exposure to anti-TNFalpha therapy. Front Pediatr. 2022;10:935034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.de Aragao MC, Beraldo RF, Marcondes MB, de Barros JR, Herrerias GSP, Saad-Hossne R, et al. Management of inflammatory bowel disease and serum level of infliximab in newborn exposed to anti-TNF therapy during pregnancy: Case report and literature review. Medicine (Baltimore). 2021;100(51):e28274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Sako M, Yoshimura N, Sonoda A, Okano S, Ueda M, Tezuka M, et al. Safety Prediction of Infants Born to Mothers with Crohn’s Disease Treated with Biological Agents in the Late Gestation Period. J Anus Rectum Colon. 2021;5(4):426–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Nguyen GC, Seow CH, Maxwell C, Huang V, Leung Y, Jones J, et al. The Toronto Consensus Statements for the Management of Inflammatory Bowel Disease in Pregnancy. Gastroenterology. 2016;150(3):734–57 e1. [DOI] [PubMed] [Google Scholar]
- 244.Burke KE, Haviland MJ, Hacker MR, Shainker SA, Cheifetz AS. Indications for Mode of Delivery in Pregnant Women with Inflammatory Bowel Disease. Inflammatory bowel diseases. 2017;23(5):721–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Foulon A, Dupas JL, Sabbagh C, Chevreau J, Rebibo L, Brazier F, et al. Defining the Most Appropriate Delivery Mode in Women with Inflammatory Bowel Disease: A Systematic Review. Inflammatory bowel diseases. 2017;23(5):712–20. [DOI] [PubMed] [Google Scholar]
- 246.Brestfeeding So. Breast feeding anf thevuse of human milk. Pediatrics. 2012;129:e827–e41.22371471 [Google Scholar]
- 247.Brodribb W. ABM Clinical Protocol #9: Use of Galactogogues in Initiating or Augmenting Maternal Milk Production, Second Revision 2018. Breastfeed Med. 2018;13(5):307–14. [DOI] [PubMed] [Google Scholar]
- 248.Anderson PO. Drugs that Suppress Lactation, Part 2. Breastfeed Med. 2017;12:199–201. [DOI] [PubMed] [Google Scholar]
- 249.Sezgin E, Terlemez G, Bozkurt B, Bengi G, Akpinar H, Buyuktorun I. Quantitative real-time PCR analysis of bacterial biomarkers enable fast and accurate monitoring in inflammatory bowel disease. PeerJ. 2022;10:e14217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Godny L, Svolos V, Williams AJ, Czuber-Dochan W, Aloi M, Ibarra A, et al. Multidisciplinary Perinatal Care in IBD. J Crohns Colitis. 2022. [DOI] [PubMed] [Google Scholar]
- 251.Selinger CP, Nelson-Piercy C, Fraser A, Hall V, Limdi J, Smith L, et al. IBD in pregnancy: recent advances, practical management. Frontline Gastroenterol. 2021;12(3):214–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Feng Z, Kang G, Wang J, Gao X, Wang X, Ye Y, et al. Breaking through the therapeutic ceiling of inflammatory bowel disease: Dual-targeted therapies. Biomedicine & pharmacotherapy = Biomedecine & pharmacotherapie. 2023;158:114174. [DOI] [PubMed] [Google Scholar]
- 253.AE MK. Inflammatory Bowel Disease: Clinical Diagnosis and Pharmaceutical Management. Medical Research Archives. 2023;11(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Louis E, Resche-Rigon M, Laharie D, Satsangi J, Ding N, Siegmund B, et al. Withdrawal of infliximab or concomitant immunosuppressant therapy in patients with Crohn’s disease on combination therapy (SPARE): a multicentre, open-label, randomised controlled trial. Lancet Gastroenterol Hepatol. 2023;8(3):215–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Danese S, Vermeire S, D’Haens G, Panes J, Dignass A, Magro F, et al. Treat to target versus standard of care for patients with Crohn’s disease treated with ustekinumab (STARDUST): an open-label, multicentre, randomised phase 3b trial. Lancet Gastroenterol Hepatol. 2022;7(4):294–306. [DOI] [PubMed] [Google Scholar]
- 256.M’Koma AE. Inflammatory Bowel Disease: Clinical Diagnosis and Surgical Treatment-Overview. Medicina (Kaunas). 2022;58(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.M’Koma AE. Serum biochemical evaluation of patients with functional pouches ten to 20 years after restorative proctocolectomy. Int J Colorectal Dis. 2006;21(7):711–20. [DOI] [PubMed] [Google Scholar]
- 258.M’Koma AE, Wise PE, Muldoon RL, Schwartz DA, Washington MK, Herline AJ. Evolution of the restorative proctocolectomy and its effects on gastrointestinal hormones. Int J Colorectal Dis. 2007;22(10):1143–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.M’Koma AE, Lindquist K, Liljeqvist L. Biochemical laboratory data in patients before and after restorative proctocolectomy. A study on 83 patients with a follow-up of 36 months. Ann Chir. 1994;48(6):525–34. [PubMed] [Google Scholar]
- 260.M’Koma AE, Lindquist K, Liljeqvist L. Effect of restorative proctocolectomy on gastric acid secretion and serum gastrin levels: a prospective study. Dis Colon Rectum. 1999;42(3):398–402. [DOI] [PubMed] [Google Scholar]
- 261.Ballard BR, M’Koma AE. Gastrointestinal endoscopy biopsy derived proteomic patterns predict indeterminate colitis into ulcerative colitis and Crohn’s colitis. World journal of gastrointestinal endoscopy. 2015;7(7):670–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Williams AD, Korolkova OY, Sakwe AM, Geiger TM, James SD, Muldoon RL, et al. Human alpha defensin 5 is a candidate biomarker to delineate inflammatory bowel disease. PloS one. 2017;12(8):e0179710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.M’Koma AE. Diagnosis of inflammatory bowel disease: Potential role of molecular biometrics. World journal of gastrointestinal surgery. 2014;6(11):208–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Rana T, Korolkova OY, Rachakonda G, Williams AD, Hawkins AT, James SD, et al. Linking bacterial enterotoxins and alpha defensin 5 expansion in the Crohn’s colitis: A new insight into the etiopathogenetic and differentiation triggers driving colonic inflammatory bowel disease. PloS one. 2021;16(3):e0246393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Greenland S, O’Rourke K. On the bias produced by quality scores in meta-analysis, and a hierarchical view of proposed solutions. Biostatistics. 2001;2(4):463–71. [DOI] [PubMed] [Google Scholar]
- 266.Juni P, Witschi A, Bloch R, Egger M. The hazards of scoring the quality of clinical trials for meta-analysis. Jama. 1999;282(11):1054–60. [DOI] [PubMed] [Google Scholar]
- 267.Tandon P, Natt N, Malhi G, Wong EC, Matthews P, Reinisch W, et al. Clinical remission in paired phase two and three studies in inflammatory bowel disease: a systematic review with meta-analysis. Eur J Gastroenterol Hepatol. 2023;35(3):231–40. [DOI] [PubMed] [Google Scholar]
- 268.Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. Bmj. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Darie AM, Sinopoulou V, Ajay V, Bel Kok K, Patel KV, Limdi J, et al. BSG 2024 IBD guidelines protocol (standard operating procedures). BMJ Open Gastroenterol. 2023;10(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Magro F, Gionchetti P, Eliakim R, Ardizzone S, Armuzzi A, Barreiro-de Acosta M, et al. Third European Evidence-based Consensus on Diagnosis and Management of Ulcerative Colitis. Part 1: Definitions, Diagnosis, Extra-intestinal Manifestations, Pregnancy, Cancer Surveillance, Surgery, and Ileo-anal Pouch Disorders. J Crohns Colitis. 2017;11(6):649–70. [DOI] [PubMed] [Google Scholar]
- 271.Leenhardt R, Riviere P, Papazian P, Nion-Larmurier I, Girard G, Laharie D, et al. Sexual health and fertility for individuals with inflammatory bowel disease. World J Gastroenterol. 2019;25(36):5423–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Lee S, Crowe M, Seow CH, Kotze PG, Kaplan GG, Metcalfe A, et al. The impact of surgical therapies for inflammatory bowel disease on female fertility. Cochrane Database Syst Rev. 2019;7(7):CD012711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Goto Y, Uchino M, Horio Y, Kusunoki K, Minagawa T, Kuwahara R, et al. Delivery Mode after Ileal Pouch-Anal Anastomosis among Pregnant Women with Ulcerative Colitis. J Anus Rectum Colon. 2021;5(4):419–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Lepisto A, Sarna S, Tiitinen A, Jarvinen HJ. Female fertility and childbirth after ileal pouch-anal anastomosis for ulcerative colitis. Br J Surg. 2007;94(4):478–82. [DOI] [PubMed] [Google Scholar]
- 275.Hahnloser D, Pemberton JH, Wolff BG, Larson D, Harrington J, Farouk R, et al. Pregnancy and delivery before and after ileal pouch-anal anastomosis for inflammatory bowel disease: immediate and long-term consequences and outcomes. Dis Colon Rectum. 2004;47(7):1127–35. [DOI] [PubMed] [Google Scholar]
- 276.Anderson BT, Ertle JT, Borum ML. Men with inflammatory bowel disease are rarely counseled regarding effects of immunosuppressive therapy on fertility and pregnancy. J Crohns Colitis. 2013;7(12):e716. [DOI] [PubMed] [Google Scholar]
- 277.Roy ACC, Martin C, Kane SV, Dubinsky M, Sandborn WJ, Sands BE, Mahdevan U. Exposure to Biologic Therapy and Childhood Development among Offspring of Women with Inflammatory Bowel Disease: Results from the Piano Registry. Gastroenterology. 2017;152(5):S85–S6. [Google Scholar]
- 278.Khil J, Picardo S, Seow CH, Leung Y, Metcalfe A, Afshar EE, et al. Physiological and psychological stress in pregnant women with quiescent inflammatory bowel disease: A pilot study using salivary biomarkers. JGH Open. 2020;4(4):692–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Mikocka-Walus A, Pittet V, Rossel JB, von Kanel R, Swiss IBDCSG. Symptoms of Depression and Anxiety Are Independently Associated With Clinical Recurrence of Inflammatory Bowel Disease. Clin Gastroenterol Hepatol. 2016;14(6):829–35 e1. [DOI] [PubMed] [Google Scholar]


