Abstract
Background
Patients with psoriasis show an increased prevalence of depressive symptoms that worsen disease outcomes. This study investigated the effect of resilience and other sociodemographic/clinical variables on depressive symptoms’ severity in patients with psoriasis.
Methods
This study included 58 psoriasis patients consecutively enrolled during the 14 months of the study. We evaluated psoriasis severity using the Psoriasis Area and Severity Index, Body Surface Area, and Physician Global Assessment. The psychometric assessment included the Resilience Scale and the Beck Depression Inventory-II (BDI-II). We divided participants into two subgroups based on the optimal BDI-II cut-off score (Group A: BDI-II ≤17; Group B: BDI-II >17). A stepwise regression analysis explored whether the variation in the BDI-II score could be predicted by a linear combination of sociodemographic and clinical variables.
Results
Psoriasis patients with more severe depressive symptoms (Group B patients) showed lower resilience levels than Group A patients (p <0.001). Moreover, depressive symptoms correlated only with resilience levels (p <0.001), with a negative correlation. The stepwise regression analysis revealed that resilience explained 37.1 % of the variance in BDI-II scores, whereas resilience, gender, and comorbidity with other physical illnesses combined explained 51.3 % of the variance.
Conclusion
Resilience may alleviate depressive symptoms in psoriasis patients. This study underscores the importance of resilience-building interventions for these patients. HIPPOKRATIA 2022, 26 (4):131-137.
Keywords: Depressive symptoms, psoriasis, psychodermatology, resilience
Introduction
Formerly, the medical term “psoriasis” (from the Greek “psora” meaning “itch”) was used to describe a skin condition regarded as a form of leprosy. It is now well established that psoriasis is a non-contagious, chronic, multifactorial disease. The clinical manifestation varies concerning the degree of skin involvement and lesions’ progression, ranging from minimal to severe. Clinical signs may not be limited to the skin; one out of four patients develops psoriatic arthritis. Furthermore, psoriasis patients show a high prevalence of depressive disorder (10-27.6 %) or experience depressive symptoms (25-68 %)1,2.
Depression is not solely a psychological reaction to the esthetic consequences of psoriasis. Shared immune-inflammatory processes and neurochemical changes may underlie both conditions, maintaining a bidirectional pathophysiological link. Therefore, most studies focus on the association between psoriasis severity and depressive symptoms3,4. Although several psoriasis-related clinical features are associated with depressive symptoms’ severity, improvement in psoriasis signs does not alleviate depressive symptoms in all patients5. Psychological factors, such as the stigma attached to the disease6, feelings of shame5, and low self-esteem7, may be partly responsible for the emergence of depressive symptoms. Furthermore, a study investigating resilience reported that psoriasis patients display lower resilience levels than healthy individuals8.
The term “resilience” encompasses both adaptation and growth despite adversity. Different scales assess resilience by its conceptualization as a trait, a process, or an outcome9. High trait resilience is related to mental health10. Moreover, higher resilience levels are associated with improved outcomes of chronic psychosomatic diseases11. Vice versa, the relation between low resilience levels and vulnerability to depression is well-established12.
Altogether, psoriasis is classified as a psychophysiological skin disorder triggered or exacerbated by emotional stress. Depressive symptoms, a source of emotional stress, may not be associated with psoriasis severity alone. This study conceptualized resilience as a positive personal characteristic promoting adaptation to chronic diseases. The aim was to investigate whether this protective factor may influence depressive symptoms’ severity in psoriasis patients.
Methods
Participants
Study participants were consecutive psoriasis patients recruited from the Psoriasis Outpatient Clinic of the 2nd Department of Dermatology and Venereology of the Aristotle University of Thessaloniki during the 14 months of the study. Inclusion criteria were: i) newly diagnosed (first diagnosis of untreated psoriasis during the study period) or known psoriasis with active lesions; ii) age 18-65 years; iii) Greek as the native language. Exclusion criteria were: i) comorbidity with another skin disorder; ii) diagnosis of overt central nervous system diseases, such as neurocognitive, neurodegenerative, demyelinating disorders, or traumatic brain injury.
This study was approved by the Scientific Committee of “Papageorgiou” General Hospital (decision No 233, dated 1/7/2015) and the Hellenic Personal Data Protection Authority (approval No 1606, GN/EX/6107-3-17/12/2015). All participants provided written informed consent.
Assessments
We recorded patients’ sociodemographic data, medical history and medications, psychiatric history, and positive/adverse life events during the preceding six months based on a semi-structured interview and the patient’s medical records.
Three measures, internationally and routinely used in clinical practice and research, were applied for the reliable evaluation of psoriasis severity: the Psoriasis Area and Severity Index (PASI) [score range: 0 (absent) - 72 (maximum)], the Physician Global Assessment (PGA) [6-point measure: 0 (clear) - 5 (severe)], and the Body Surface Area (BSA) (total BSA =100 %)13,14.
We assessed the depressive symptoms utilizing the Greek version of the Beck Depression Inventory-II (BDI-II)15,16, commonly applied for screening psoriasis patients1. We divided study participants into two subgroups based on the optimal BDI-II cut-off score of 17 in the Greek population15. Group A (BDI-II ≤17) comprised 39, whereas Group B (BDI-II >17) included 19 psoriasis patients.
We evaluated resilience employing the Greek version of the 25-item self-administered Resilience Scale (RS)17,18, which assesses resilience based on five innate characteristics, each explored by five items on a 7-point scale (1 =strongly disagree; 7 =strongly agree; total score range =25-175; higher scores reflect greater resilience levels).
Statistical analyses
We performed all statistical analyses using IBM SPSS Statistics for Windows, Version 21.0 (IBM Corp., Armonk, NY, USA). We utilized Spearman’s rho to calculate correlations and the chi-square test to explore group differences in nominal variables, whereas the Student’s t-test was used for continuous demographic variables. The Kolmogorov-Smirnov test was employed to test scale scores for normality. Since none of the variables tested were normally distributed, non-parametric statistics were used (Mann-Whitney test).
Effect sizes [d and phi (φ)] were estimated and reported accordingly [Cohen’s d statistic: small (d =0.2), medium (d =0.5), large (d =0.8), very large (d ≥1) effect size; phi (φ) statistic: small (φ =0.1), medium (φ =0.3), large (φ =0.5), very large (φ ≥0.7) effect size]. We set the level of statistical significance at p <0.05, two-tailed, adjusted with the Bonferroni correction for multiple comparisons (0.05:8) to a corresponding p <0.00625 level.
We conducted a stepwise regression analysis to explore whether the variation in the BDI-II score could be predicted by a linear combination of sociodemographic and clinical variables. Based on the minimum of ten subjects per independent variable recommendation and according to the correlations between measured variables, we included the following independent variables in the stepwise regression analysis: age, gender, duration of psoriasis, past depressive episodes, comorbidity with other physical illness, presence of psoriasis symptoms on the face or torso, BSA, and RS. The independence of residuals was assessed with the Durbin-Watson statistic at 1.639.
Results
Sixty psoriasis outpatients, in total, agreed to participate and were screened for complying with inclusion/exclusion criteria. Among them, 58 were eligible for the study. The research group comprised 35 men (60.3 %, aged 43.46 ± 12.48 years) and 23 women (39.7 %, aged 47.22 ± 14.66 years). The mean duration of psoriasis was 14.60 ±11.26 years (none of the participants were newly diagnosed). Psoriasis treatment varied significantly (topical treatment in eight patients, various biologics in 22 patients, combination treatment in ten patients, methotrexate in eight patients, cyclosporine in seven patients, acitretin in two patients, and apremilast in one patient).
Concerning psychiatric history, 18 participants (31 %) had a history of depressive episodes; one was diagnosed with obsessive-compulsive disorder, whereas two were occasionally consuming cannabis. At the time of recruitment, none of the patients received psychiatric medication. Several patients (44.8 %) suffered from a comorbid medical condition and were under appropriate treatment.
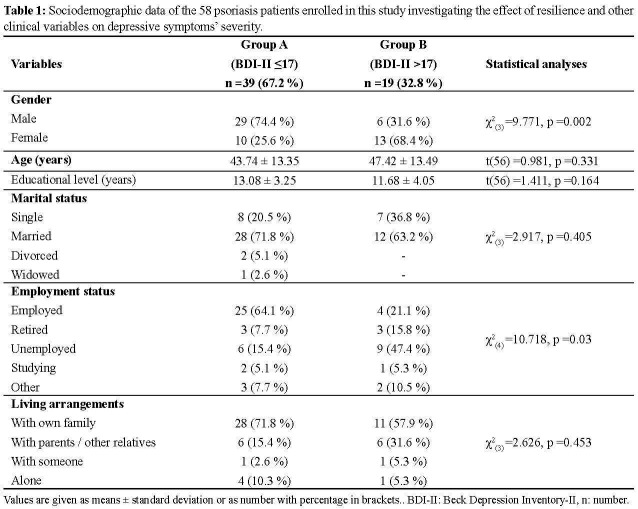
No statistically significant differences were found between Group A (BDI-II ≤17) and Group B (BDI-II >17) regarding age (p =0.331), years of education (p =0.164), marital status (p =0.405), or living arrangements (p =0.453). In contrast, Group B included more female patients (p =0.002) and fewer employed individuals (p =0.03) than Group A (Table 1).
Table 1. Sociodemographic data of the 58 psoriasis patients enrolled in this study investigating the effect of resilience and other clinical variables on depressive symptoms’ severity.
Values are given as means ± standard deviation or as number with percentage in brackets.. BDI-II: Beck Depression Inventory-II, n: number.
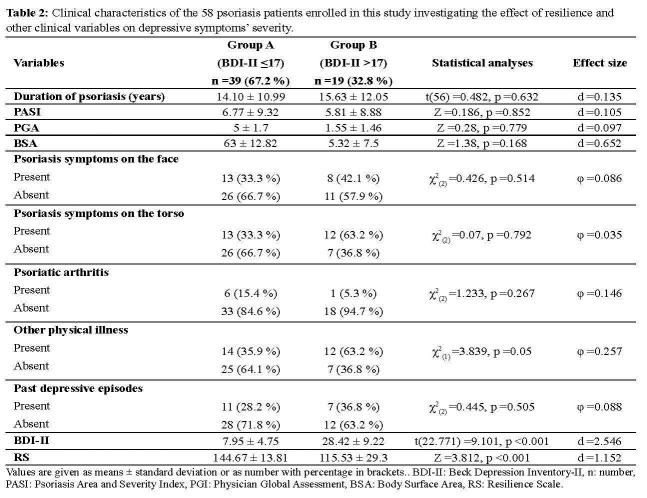
Concerning participants’ clinical characteristics, there were no statistically significant differences in the duration of psoriasis (p =0.632), the presence of psoriatic arthritis (p =0.267), the three psoriasis severity indexes [PASI (p =0.852), PGA (p =0.779), and BSA (p =0.168)], and the presence of psoriasis symptoms on the face (p =0.514) or torso (p =0.792). In addition, there were no differences regarding the prior history of depressive episodes (p =0.505). In contrast, Group B suffered more from other physical illnesses than Group A patients (p =0.05). Lastly, Group A showed significantly higher resilience levels than Group B patients (p <0.001); the mean resilience score was significantly higher in males (142.09 ± 16.67) compared with females (124.52 ± 30.01) [t-test =2.862, df =31.005, p =0.016] (Table 2).
Table 2. Clinical characteristics of the 58 psoriasis patients enrolled in this study investigating the effect of resilience and other clinical variables on depressive symptoms’ severity.
Values are given as means ± standard deviation or as number with percentage in brackets.. BDI-II: Beck Depression Inventory-II, n: number, PASI: Psoriasis Area and Severity Index, PGI: Physician Global Assessment, BSA: Body Surface Area, RS: Resilience Scale.
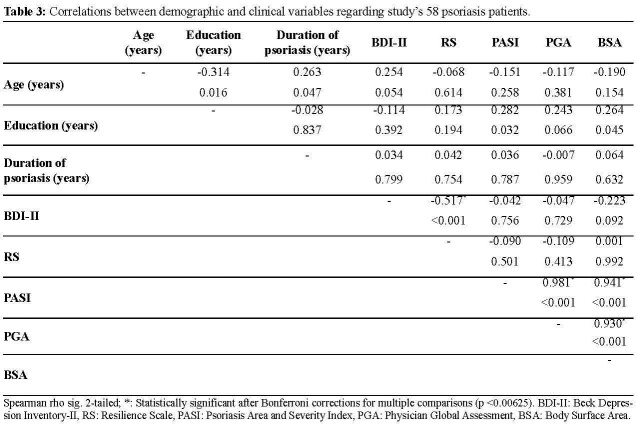
Based on the correlation analysis, depressive symptoms’ severity was only correlated with resilience levels (negative correlation) (Table 3).
Table 3. Correlations between demographic and clinical variables regarding study’s 58 psoriasis patients.
Spearman rho sig. 2-tailed; *: Statistically significant after Bonferroni corrections for multiple comparisons (p <0.00625). BDI-II: Beck Depression Inventory-II, RS: Resilience Scale, PASI: Psoriasis Area and Severity Index, PGA: Physician Global Assessment, BSA: Body Surface Area.
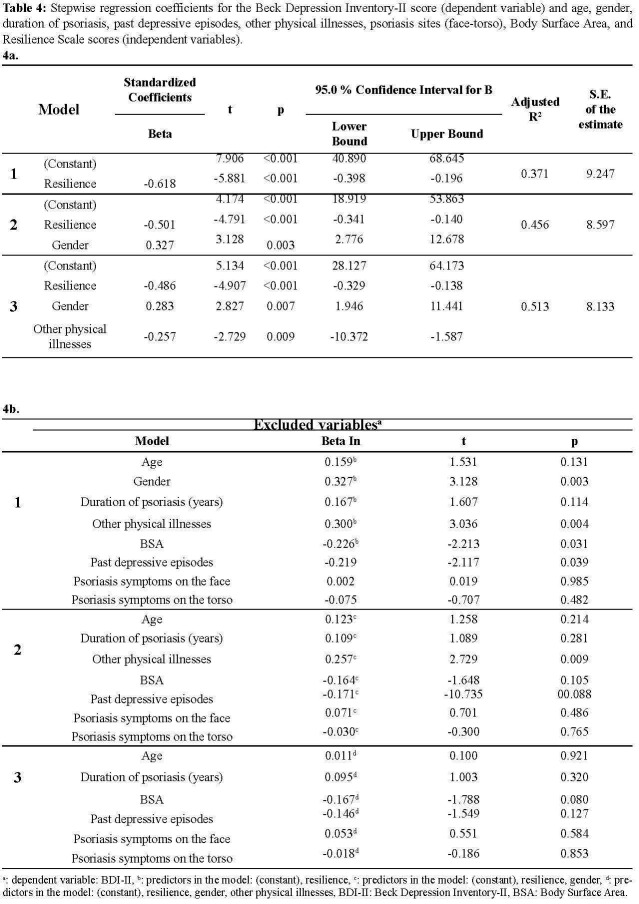
According to the regression analysis, the variables contributing significantly to calculating the BDI-II score were gender, comorbidity with other physical illnesses, and the RS score. In contrast, age, duration of psoriasis, presence of psoriasis symptoms on the face or torso, past depressive episodes, and BSA were dropped from the final third regression step [F(3,54) =21.028, p <0.001]. Resilience displayed a protective role against depressive symptoms (adjusted R2=0.371) that remained statistically significant even after controlling for the effect of gender and comorbidity with other physical illnesses (adjusted R2=0.513) (Table 4).
Table 4. Stepwise regression coefficients for the Beck Depression Inventory-II score (dependent variable) and age, gender, duration of psoriasis, past depressive episodes, other physical illnesses, psoriasis sites (face-torso), Body Surface Area, and Resilience Scale scores (independent variables).
a: dependent variable: BDI-II, b: predictors in the model: (constant), resilience, c: predictors in the model: (constant), resilience, gender, d: predictors in the model: (constant), resilience, gender, other physical illnesses, BDI-II: Beck Depression Inventory-II, BSA: Body Surface Area.
Discussion
Research evidence suggests that skin lesions’ severity and concomitant psoriatic arthritis may be associated with depressive symptoms, though not in all psoriasis patients. The impact of the duration of psoriasis on depressive symptoms is also inconsistent5,19. This study examined the differences between psoriasis patients with clinically non-significant and more severe depressive symptoms. Results revealed a high effect size for the BSA, reflecting psoriasis-affected skin area, but small effect sizes for the PASI and PGA indexes, the presence of psoriasis symptoms on the face or torso, the presence of psoriatic arthritis, and the duration of psoriasis. The effect size for past depressive episodes was again small, with both study groups displaying similar rates. On the contrary, the effect size for the resilience index was significant, indicating that patients with higher resilience levels are less likely to suffer from severe depressive symptoms. Moreover, depressive symptoms were only correlated (inversely) with resilience levels.
Several studies revealed a higher prevalence of depressive symptoms in female psoriasis patients3,19 and an increased risk of depression due to comorbid physical illnesses20. This study’s regression analysis supported the protective effect of resilience against depressive symptoms after controlling for the effects of gender and comorbidity with other physical illnesses. According to the results, resilience explained 37.1 % of the variance in BDI-II scores, whereas resilience, gender, and comorbidity with other physical illnesses combined explained 51.3 % of the variance. Neither psoriasis-related clinical factors nor the history of depressive episodes contributed to depressive symptoms’ severity.
Depressive symptoms worsen psoriasis outcomes, triggering or exacerbating physical symptoms3, which, in turn, affect different aspects of patients’ functioning5. Furthermore, depressive symptoms affect the quality of life21 and adherence to psoriasis treatment22. Moreover, the higher suicide risk in psoriasis patients is a solemn issue23. For all these reasons, treating depressive symptoms in psoriasis patients is essential. Although 32.8 % of this study’s participants scored above the BDI-II cut-off score for clinically significant depressive symptoms, none were under psychiatric medication, an observation hinting at limited screening and treatment of depression in psoriasis patients.
Antidepressants may alleviate psychiatric symptoms, but they may exacerbate psoriasis symptoms5. Biologics may also improve depressive symptoms22,24. Nonetheless, sufficient treatment of psoriasis does not alleviate depressive symptoms in all patients5,25. Therefore, supplementary therapeutic approaches are required since the “recovery” concept involves more than physical symptoms’ improvement; it encompasses overall well-being.
Patients with chronic physical diseases display low resilience levels associated with more severe depressive symptoms11,26. In contrast, high trait resilience contributes significantly to mental health10, protecting against the emergence of depression12,27. This study showed that resilience mitigates depressive symptoms in patients with psoriasis, a chronic psychosomatic disease. Most importantly, resilience is a modifiable characteristic that may be enhanced by psychological interventions, contributing to well-being28. A meta-analysis of psychotherapeutic interventions in dermatological patients revealed encouraging results29, with cognitive behavioral therapy being a promising approach30. However, psychotherapeutic interventions promoting resilience in psoriasis patients require further investigation.
This study had some limitations: i) the cross-sectional design hindered elucidation of causal relationships; ii) the sample size was relatively small; iii) the self-administered tools may suffer from bias related to self-report; iv) although most studies use validated questionnaires to assess depressive symptoms, a practical tool for clinical settings, a definite diagnosis of depression requires diagnostic interviews based on standard diagnostic criteria; v) it was not feasible to investigate the effects of psoriasis medication on depressive symptoms due to divergence in psoriasis treatment.
Conclusively, this was the first study to investigate the effect of resilience and several sociodemographic/clinical variables on depressive symptoms in Greek psoriasis patients. Assessing resilience in different populations is worthwhile due to its social and cultural contributors9. Psoriasis is a psychodermatological disorder requiring a multidimensional therapeutic approach. Evaluating and treating depressive symptoms is essential for improving the disease’s global outcome. This study underscores the implementation of resilience-building interventions since resilience may alleviate depressive symptoms in psoriasis patients. Such interventions could either prevent the emergence of depressive symptoms or complement antidepressant treatment in cases of established depressive symptoms.
Conflict of interest
The authors have no competing interests to report.
References
- 1.Dowlatshahi EA, Wakkee M, Arends LR, Nijsten T. The prevalence and odds of depressive symptoms and clinical depression in psoriasis patients: a systematic review and meta-analysis. J Invest Dermatol. 2014;134:1542–1551. doi: 10.1038/jid.2013.508. [DOI] [PubMed] [Google Scholar]
- 2.Ferreira BR, Pio-Abreu JL, Reis JP, Figueiredo A. Analysis of the Prevalence of Mental Disorders in Psoriasis: The Relevance of Psychiatric Assessment in Dermatology. Psychiatr Danub. 2017;29:401–406. doi: 10.24869/psyd.2017.401. [DOI] [PubMed] [Google Scholar]
- 3.Ferreira BI, Abreu JL, Reis JP, Figueiredo AM. Psoriasis and Associated Psychiatric Disorders: A Systematic Review on Etiopathogenesis and Clinical Correlation. J Clin Aesthet Dermatol. 2016;9:36–43. [PMC free article] [PubMed] [Google Scholar]
- 4.Tohid H, Aleem D, Jackson C. Major Depression and Psoriasis: A Psychodermatological Phenomenon. Skin Pharmacol Physiol. 2016;29:220–230. doi: 10.1159/000448122. [DOI] [PubMed] [Google Scholar]
- 5.Moon HS, Mizara A, McBride SR. Psoriasis and psycho-dermatology. Dermatol Ther (Heidelb) 2013;3:117–130. doi: 10.1007/s13555-013-0031-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hrehorów E, Salomon J, Matusiak L, Reich A, Szepietowski JC. Patients with psoriasis feel stigmatized. Acta Derm Venereol. 2012;92:62–72. doi: 10.2340/00015555-1193. [DOI] [PubMed] [Google Scholar]
- 7.Palijan TZ, Kovacević D, Koić E, Ruzić K, Dervinja F. The impact of psoriasis on the quality of life and psychological characteristics of persons suffering from psoriasis. Coll Antropol. 2011;35 Suppl 2:81–85. [PubMed] [Google Scholar]
- 8.Crosta ML, De Simone C, Di Pietro S, Acanfora M, Caldarola G, Moccia L, et al. Childhood trauma and resilience in psoriatic patients: A preliminary report. J Psychosom Res. 2018;106:25–28. doi: 10.1016/j.jpsychores.2018.01.002. [DOI] [PubMed] [Google Scholar]
- 9.Southwick SM, Bonanno GA, Masten AS, Panter-Brick C, Yehuda R. Resilience definitions, theory, and challenges: interdisciplinary perspectives. Eur J Psychotraumatol. 2014;5 doi: 10.3402/ejpt.v5.25338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hu T, Zhang D, Wang J. A meta-analysis of the trait resilience and mental health. Pers Individ Differ. 2015;76:18–27. [Google Scholar]
- 11.Cal SF, de Sá LR, Glustak ME, Santiago MB. Resilience in chronic diseases: A systematic review. Cogent Psychol. 2015;2:1024928. [Google Scholar]
- 12.Southwick SM, Vythilingam M, Charney DS. The psychobiology of depression and resilience to stress: implications for prevention and treatment. Annu Rev Clin Psychol. 2005;1:255–291. doi: 10.1146/annurev.clinpsy.1.102803.143948. [DOI] [PubMed] [Google Scholar]
- 13.Robinson A, Kardos M, Kimball AB. Physician Global Assessment (PGA) and Psoriasis Area and Severity Index (PASI): why do both? A systematic analysis of randomized controlled trials of biologic agents for moderate to severe plaque psoriasis. J Am Acad Dermatol. 2012;66:369–375. doi: 10.1016/j.jaad.2011.01.022. [DOI] [PubMed] [Google Scholar]
- 14.Bożek A, Reich A. The reliability of three psoriasis assessment tools: Psoriasis area and severity index, body surface area and physician global assessment. Adv Clin Exp Med. 2017;26:851–856. doi: 10.17219/acem/69804. [DOI] [PubMed] [Google Scholar]
- 15.Giannakou M, Roussi P, Kosmides ME, Kiosseoglou G, Adamopoulou A, Garyfallos G. Adaptation of the Beck Depression Inventory-II to Greek population. Hell J Psychol. 2013;10:120–146. [Google Scholar]
- 16.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. Psychological Corporation, San Antonio, TX. 1996 [Google Scholar]
- 17.Pantazi S, Kirla D, Rera I, Bozikas V, Holeva V. The Greek version of the Resilience Scale, the Mindful Attention Awareness Scale and the Satisfaction with Life Scale: translation, adaptation, validation. Abstract Book. 2nd International Conference on Positive Psychology in the Czech Republic (CPPC 2013), Brno, 22-24/5/2013. Masaryk University, Brno. 2013:23–24. [Google Scholar]
- 18.Wagnild GM, Young HM. Development and psychometric evaluation of the Resilience Scale. J Nurs Meas. 1993;1:165–178. [PubMed] [Google Scholar]
- 19.Adesanya EI, Matthewman J, Schonmann Y, Hayes JF, Henderson A, Mathur R, et al. Factors associated with depression, anxiety and severe mental illness among adults with atopic eczema or psoriasis: a systematic review and meta-analysis. Br J Dermatol. 2023;188:460–470. doi: 10.1093/bjd/ljac132. [DOI] [PubMed] [Google Scholar]
- 20.Azevedo-Pinto S, Santos S, von Doellinger O, Barbosa M, Coelho R. The inflammatory perspective of depression in the context of chronic medical conditions. Int J Clin Neurosci Ment Health. 2016;3:S11. [Google Scholar]
- 21.Schmitt JM, Ford DE. Role of depression in quality of life for patients with psoriasis. Dermatology. 2007;215:17–27. doi: 10.1159/000102029. [DOI] [PubMed] [Google Scholar]
- 22.Korman AM, Hill D, Alikhan A, Feldman SR. Impact and management of depression in psoriasis patients. Expert Opin Pharmacother. 2016;17:147–152. doi: 10.1517/14656566.2016.1128894. [DOI] [PubMed] [Google Scholar]
- 23.Wu KK, Armstrong AW. Suicidality among psoriasis patients: a critical evidence synthesis. G Ital Dermatol Venereol. 2019;154:56–63. doi: 10.23736/S0392-0488.18.06112-6. [DOI] [PubMed] [Google Scholar]
- 24.Fleming P, Roubille C, Richer V, Starnino T, McCourt C, McFarlane A, et al. Effect of biologics on depressive symptoms in patients with psoriasis: a systematic review. J Eur Acad Dermatol Venereol. 2015;29:1063–1070. doi: 10.1111/jdv.12909. [DOI] [PubMed] [Google Scholar]
- 25.Fortune DG, Richards HL, Kirby B, McElhone K, Main CJ, Griffiths CE. Successful treatment of psoriasis improves psoriasis-specific but not more general aspects of patients’ well-being. Br J Dermatol. 2004;151:1219–1226. doi: 10.1111/j.1365-2133.2004.06222.x. [DOI] [PubMed] [Google Scholar]
- 26.Ghanei Gheshlagh R, Sayehmiri K, Ebadi A, Dalvandi A, Dalvand S, Nourozi Tabrizi K. Resilience of Patients With Chronic Physical Diseases: A Systematic Review and Meta-Analysis. Iran Red Crescent Med J. 2016;18:e38562. doi: 10.5812/ircmj.38562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Elisei S, Sciarma T, Verdolini N, Anastasi S. Resilience and depressive disorders. Psychiatr Danub. 2013;25 Suppl 2:S263–S267. [PubMed] [Google Scholar]
- 28.Southwick SM, Pietrzak RH, White G. Interventions to enhance resilience and resilience-related constructs in adults. Southwick SM, Litz BT, Charney DS, Friedman MJ (eds). Resilience and Mental Health: Challenges across the lifespan. Cambridge University Press, Cambridge. 2011:289–306. [Google Scholar]
- 29.Lavda AC, Webb TL, Thompson AR. A meta-analysis of the effectiveness of psychological interventions for adults with skin conditions. Br J Dermatol. 2012;167:970–979. doi: 10.1111/j.1365-2133.2012.11183.x. [DOI] [PubMed] [Google Scholar]
- 30.Fortune DG, Richards HL, Kirby B, Bowcock S, Main CJ, Griffiths CE. A cognitive-behavioural symptom management programme as an adjunct in psoriasis therapy. Br J Dermatol. 2002;146:458–465. doi: 10.1046/j.1365-2133.2002.04622.x. [DOI] [PubMed] [Google Scholar]