Abstract
Background
Cardiopulmonary resuscitation (CPR) and early defibrillation are the most common procedures performed by nurses as the first responders to cardiac arrest patients in the hospital setting. Therefore, nurses are demanded to have high skills for effective performance. Self-efficacy and knowledge are considered significant factors affecting early initiation of CPR and automated defibrillation. However, previous studies mostly focused on nursing students instead of frontline nurses.
Objective
This research aimed to assess the relationship between nurses’ knowledge and self-efficacy regarding the early initiation of CPR and automated defibrillation of cardiac arrest patients.
Methods
The study employed a cross-sectional, descriptive, correlational survey. Using convenience sampling, two hundred eighty-seven nurses working in critical areas and inpatient and outpatient departments, King Abdulaziz University Hospital (KAUH), Saudi Arabia, were selected. Resuscitation Knowledge and Self-Efficacy Scales were used for data collection (using Google Form) from November 2020 to January 2021. Descriptive statistics and Pearson correlation were used for data analysis.
Results
Overall, 61.3% of participants had moderate knowledge (13.659 ± 2.175), and 63.8% had high self-efficacy (44.627 ± 58.397). The highest domain of self-efficacy was responding and rescuing, while the lowest domain was debriefing and recording. There was a significant positive relationship between knowledge and self-efficacy (p <0.001; r = 0.207).
Conclusion
The positive relationship explained a high level of self-efficacy if there was a high level of knowledge. Thus, it is recommended that nursing programs apply CPR and automated defibrillation curricula during nurses’ internships, clear policies and procedures about CPR and automated defibrillation, continual updates about CPR and automated defibrillation, and knowledge and continuance training (on-job-training) about CPR and automated defibrillation, which can enhance and improve knowledge and self-efficacy among health care workers, especially for nurses.
Keywords: cardiac arrest, cardiopulmonary resuscitation (CPR), defibrillation, knowledge, nurses, self-efficacy, Saudi Arabia
Sudden cardiac arrest (SCA) is the leading cause of death worldwide, affecting individuals’ health and increasing their mortality risk (Bray et al., 2017). About 70% of out-of-hospital cardiac arrests (OHCAs) occur at home, with approximately 50% unwitnessed. OHCA prognosis is poor, with a relatively low survival-to-discharge rate. Only 11% of adult cases of non-traumatic cardiac arrest are resuscitated by emergency medical services (EMS) (Kleinman et al., 2015; CARES, 2017). In-hospital cardiac arrest (IHCA) prognosis is better, with a survival-to-discharge rate of 22.3%–25.5% in adults (Mozaffarian et al., 2015).
CPR and early defibrillation (CPR-D) are commonly performed by nurses, often first responders in the hospital setting (Jamieson et al., 2002). In addition, early CPR-D is associated with a considerably enhanced survival-to-discharge rate for out-of-hospital cardiac arrest (Bray et al., 2017). Pauses before and after the shock delivered by defibrillators are called preshock pauses. A study by Kleinman et al. (2015) found that the survival-to-discharge rate was higher for those who received preshock pauses of less than ten seconds with total preshock pauses of less than 20 seconds during CPR-D.
Time is one of the factors affecting CPR-D efficacy. The time between cardiac arrest onset to CPR and defibrillator use is associated with increased survival; therefore, even a few minutes of delay are potentially deadly (Koster et al., 2010). In addition, a study by Cartledge et al. (2020) found that most respondents were unsure about how to use the defibrillator. Those with less experience using defibrillators may therefore have a sense of decreased knowledge and self-efficacy.
It is important for nurses not only to have knowledge (know-how) and the right attitude (preparation) but also to believe in their ability (self-efficacy) to handle cardiac cases effectively (Turner et al., 2009). Self-efficacy and knowledge are considered significant factors affecting CPR-D delivery and can predict a nurse’s CPR-D ability; therefore, nurses must be prepared in terms of knowledge and self-efficacy when performing CPR.
Potential damage to the tissues can be minimized by early use of CPR-D and basic life support (BLS) skills, significantly increasing the survival rate in cardiac arrest patients. Specialization in CPR-D is a must, especially for nurses, who are usually the first responders to cardiac arrest patients in the hospital. Increasing nurses’ knowledge is basic to CPR-D performance. Previous studies found a relation between knowledge and self-efficacy. Moon and Hyun (2019) examined the effects of a “blended training program” relying on e-learning materials produced by leading Korean public health establishments with knowledge on CPR-D, attitude, and self-efficacy. They found that the intervention group who received the blended training program had shown significant enhancements in their knowledge, emotional attitude, behavior and attitude, cognitive attitude, and self-efficacy scores after completing the e-learning program.
Partiprajak and Thongpo (2016) measured the participants’ knowledge and self-efficacy in relation to CPR-D three months after training. Although the participants displayed positive chest-compression performance compared to the first results, their knowledge and self-efficacy decreased. Moreover, Kim et al. (2017) found that the participants’ satisfaction showed a significant association between BLS education and CPR self-efficacy.
Previous studies focused on nursing students and other targeted groups instead of on frontline nurses. Little is known about the relationship between nurses’ knowledge and self-efficacy regarding early initiation of CPR and automated defibrillation of cardiac arrest patients in Saudi Arabia. This study resolves a gap in the literature by focusing on nurses’ knowledge base, which might be connected to nurses’ self-efficacy when performing CPR-D. Sharp et al. (2016) stated that one’s sense of efficacy is a powerful human characteristic that affects choices and task effort. It is not based on the ability to do a task but rather on the perceived ability to complete those tasks. Self-efficacy influences the choices individuals make and their time and effort expended on a job. When nurses have a healthy sense of self-efficacy, they will tend toward attitudes and behaviors that support the assistance of cardiac arrest patients.
Methods
Study Design
This study used a cross-sectional, descriptive, and correlational design to describe the relationship between nurses’ knowledge and self-efficacy regarding early initiation of CPR and automated defibrillation of cardiac arrest patients at King Abdulaziz University Hospital (KAUH).
Participants
The study population included nurses working in outpatient clinics, critical care units, emergency departments, medical departments, obstetrics and gynecologic departments, pediatric departments, and surgical departments at KAUH, Jeddah, Saudi Arabia. Convenience sampling was used to assure surveillance of all staff nurses. KUAH has a population of 1123 staff nurses (719 inpatients and 404 outpatient). We calculated the sample size using the online Raosoft calculating program with a confidence level of 95% and a margin of error of 5%; therefore, a minimum sample of 287 respondents was required (Raosoft, 2004). Our inclusion criteria were staff nurses working in inpatient or outpatient wards or critical areas; registered and certified nurses; and nurses who could read, speak, and write English. Our exclusion criterion was nurses who were not working with patients, such as those in administration.
Measures
Three questionnaires were used. First, a general questionnaire was used to measure demographic and individual characteristics: the working department, age, gender, length of experience, and frequency of witnessing or performing CPR-D. Second, the Resuscitation Knowledge Scale of Byun (2014) was used to measure participants’ knowledge about CPR-D. The scale consisted of 20 items: two for checking for breathing, two for checking for consciousness, seven for chest compressions, five for applying the defibrillator, and four for maintaining airway and delivering rescue breaths. The total score ranges from 0 to 20. The score distribution is low (0–9), moderate (10–14), and high (15–20).
Third, the Resuscitation Self-Efficacy Scale (RSES) of Desiani et al. (2017) was used to assess nurses’ self-efficacy. The validity of the RSES was 0.56–0.84 based on Roh et al. (2012) as cited in Desiani et al. (2017). The scale consisted of 17 questions to assess four domains: recognition, debriefing and recording, responding and rescuing, reporting. The participants answer these questions by confirming whether they feel least confident, natural, or very confident. However, self-efficacy is low if the total score is lower than the mean, and self-efficacy is high if the total score is greater than or equal to the mean. Both instruments were administered in the English language. No Arabic translation was necessary since English is one of the inclusion criteria.
We have obtained permission to use the second and third instruments from the original authors.
Data Collection
Data were collected electronically from the target group of nurses through a Google form link and shared data with the head nurses in KAUH. We sent a reminder to the head nurses after two weeks to increase the response rate. The challenge we faced was that participants’ responses were initially weak, necessitating frequent visits to the hospital to motivate participants to answer the survey and extend the survey times so that more nurses could respond (two months). The link to the questionnaires was accessible until enough samples were reached.
Data Analysis
Descriptive statistics (means, SD, frequencies, percentages, and ranges) and Pearson correlation were used for data analysis. The alpha level of significance was set at 0.05. The assumptions of normality were met, with Kolmogorov–Smirnov (p > 0.05).
Ethical Consideration
Official approval was obtained from the Research Ethical Committee of the Faculty of Nursing at King Abdulaziz University (Ref NO 1M.19) and the Unit of Biomedical Ethics Research Committee at KAUH No (HA-02-J-008) (Reference NO 517-20). To meet the ethical consideration of the research process, the participants’ names were encoded for anonymity. There was no potential risk to participants, and it was clear that they had the right to decline to participate. To avoid bias during data gathering, it was ensured that we knew none of the participants.
Results
The total sample was 287 nurses who worked in inpatient and outpatient departments at KAUH. Table 1 shows the demographic characteristics of the nurses, most of whom were female (91.3%). Most were middle-aged (31 to 39) 36.428 ± 7.598. The most represented specialty was pediatrics (30.7%). The participants’ experience was varied.
Table 1.
Demographic characteristics of the participants (N= 287)
| Variables | N | % |
|---|---|---|
| Age | ||
| 20-30 | 65 | 22.6 |
| 31-39 | 116 | 40.4 |
| 40 or above | 106 | 36.9 |
| Mean±SD | 36.428±7.598 | |
| Gender | ||
| Female | 262 | 91.3 |
| Male | 25 | 8.7 |
| Working departments | ||
| Outpatients | 42 | 14.6 |
| Critical care units | 30 | 10.5 |
| Emergency department | 36 | 12.5 |
| Medical department | 44 | 15.3 |
| Obstetrics and gynecology | 16 | 5.6 |
| Pediatric department | 88 | 30.7 |
| Surgical department | 31 | 10.8 |
| Clinical experiences | ||
| Less than one year | 9 | 3.1 |
| 1-less than five years | 52 | 18.1 |
| 5-10 years | 64 | 22.3 |
| More than ten years | 162 | 56.4 |
| Mean±SD | 9.196±4.166 | |
| Frequency of CPR witnessed or performed | ||
| 0 | 15 | 5.2 |
| 1-5 | 93 | 32.4 |
| More than 5 | 179 | 62.4 |
Impressively, most participants had more than ten years of experience (56.4%), with a mean of 9.196 ± 4.166. The frequency of CPR being performed or witnessed differed among participants: the percentage of participants who saw or performed CPR more than five times was 62.4%.
Significantly, as shown in Table 2 and Figure 1, 61.3% of study participants had a moderate knowledge score.
Table 2.
Knowledge level of participants regarding cardiopulmonary resuscitation and automated defibrillation
| Scale Items | Knowledge Scale Score |
|||||||
|---|---|---|---|---|---|---|---|---|
| Low |
Moderate |
High |
Score |
|||||
| N | % | N | % | N | % | Range | Mean±SD | |
| Confirm the reaction | 56 | 19.5% | 0 | 0.0% | 231 | 80.5% | 0-1 | 0.805±0.397 |
| Request help | 152 | 53.0% | 0 | 0.0% | 135 | 47.0% | 0-1 | 0.470±0.500 |
| Circular request | 7 | 2.4% | 82 | 28.6% | 198 | 69.0% | 0-2 | 1.666±0.522 |
| Chest compression | 24 | 8.4% | 122 | 42.5% | 141 | 49.1% | 0-7 | 5.247±1.228 |
| Airway maintenance and artificial respiration | 50 | 17.4% | 152 | 53.0% | 85 | 29.6% | 0-4 | 2.143±0.774 |
| Defibrillation | 54 | 18.8% | 107 | 37.3% | 126 | 43.9% | 0-5 | 3.328±0.952 |
| Total Knowledge | 10 | 3.5% | 176 | 61.3% | 101 | 35.2% | 5-18. | 13.659±2.175 |
Figure 1.
Knowledge level of participants regarding cardiopulmonary resuscitation and automated defibrillation
As shown in Table 3 and Figure 2, 63.8% of participants had a high score on self-efficacy, and the highest domain was the responding and rescuing domain (13.139 ± 61.397). In contrast, the lowest domains of self-efficacy were debriefing and recording (10.244 ± 66.397).
Table 3.
Self-Efficacy level of Participants Regarding Cardiopulmonary Resuscitation and Automated Defibrillation
| Self-Efficacy |
||||||
|---|---|---|---|---|---|---|
| Low |
High |
Score |
||||
| N | % | N | % | Range | Mean±SD | |
| Recognition | 85 | 29.6% | 202 | 70.4% | 4-12. | 10.868±1.755 |
| Debriefing and recording | 128 | 44.6% | 159 | 55.4% | 4-12. | 10.244±66.397 |
| Responding and rescuing | 119 | 41.5% | 168 | 58.5% | 5-15. | 13.139±61.397 |
| Reporting | 120 | 41.8% | 167 | 58.2% | 4-12. | 10.376±1.953 |
| Total Self-Efficacy | 104 | 36.2% | 183 | 63.8% | 17-51 | 44.627±58.397 |
Figure 2.
Self-efficacy score of the studied participants regarding cardiopulmonary resuscitation and automated defibrillation
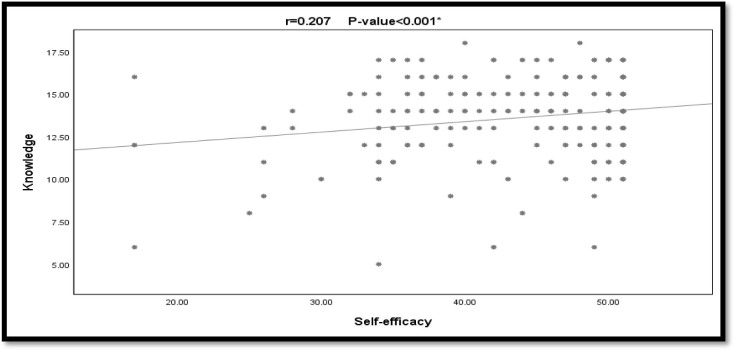
The scattered design was used to describe the correlation between knowledge and self-efficacy, as shown in Figure 3, with a p-value of <0.001* and a r-value of 0.207. Ultimately, the correlation was weak and significantly positive between knowledge and self-efficacy. The positive relationship indicated that there was a high-level self-efficacy if there was a high level of knowledge.
Figure 3.
Correlation between nurses’ knowledge score and nurses’ self-efficacy of cardiopulmonary resuscitation and automated defibrillation
Discussion
This study aimed to assess the relationship between nurses’ knowledge and self-efficacy regarding the early initiation of CPR-D of cardiac arrest patients. Our study found that the mean score for resuscitation knowledge was moderate, a finding that parallels that of Sachdeva (2020) in a tertiary care hospital in India that aimed to assess knowledge and practice of CPR-D among nurses. The similarity in both studies may indicate the need to work on nurses’ CPR-D knowledge. These findings have often been associated with inadequate continuing education programs regarding CPR-D, and most of the participants were working in the pediatrics department and might have answered the questions considering that the patients are children instead of adult patients. In another study, nurses enrolled at Umm Al-Qura University were found to have moderate levels of CPR-D knowledge and practical skills (Shammah et al., 2018).
In addition, our study found that the participants had high overall self-efficacy scores, indicating that they were confident in their CPR-D skills, could stay calm while applying CPR-D, and had little or no problem focusing on the task. The study also observed that the respondents tended to control their anxiety and sense of distress and perform according to their skill levels. Thus, self-efficacy was considered adequate in this regard, and this verified that confidence could encourage nurses to decide to perform CPR-D in instances of cardiac arrest.
Waloyo (2016) reported a self-efficacy rate of 75%, which was higher than the findings of this study. Besides the overall scale scores, the nurses in this research were very confident in terms of scales of self-efficacy subscale scores we have obtained in the present study were 55.4% for debriefing, 65.9% for documentation on quality improvement, 59.6% for remaining calm and focused, 65.9% for performing re-evaluation, 63.4% for reporting, 56.8% for using existing resources and external experts, 65.5% for using appropriate means of communication, and 70% for understanding when to request help.
In comparison to the findings of this study, Desiani et al. (2017) reported lower rates of confidence in terms of the subscales of self-efficacy. According to their data, the rates of nurses who were confident about their skills were 35.5% for debriefing, 46.1% for the correct management of a defibrillator, 38.1% for explaining clinical laboratory findings and critical values and 30.2% for using existing resources and external experts.
Besides, various methods could be used for debriefing to improve CPR-D knowledge and quality: oral debriefing, oral debriefing with voice recording, self-debriefing, debriefing with an instructor, and oral debriefing with video recording (Verkuyl et al., 2018). However, some training facilities or universities may not have easy access to the devices needed for the education of their learners. For instance, when evaluating training for defibrillators’ use, the lack of exposure to a defibrillator during training could significantly dampen training outcomes, which is another matter that should be considered. This leaves many nurses uncertain about using these devices, leading to less experience and lower levels of knowledge and self-efficacy. In addition, the lack of availability of a defibrillator during training courses will often result in a lack of theoretical and practical knowledge in carrying out defibrillation with an Automated External Defibrillation (AED) (Aranzábal-Alegría et al., 2017). Besides the obvious problems associated with having lower levels of practical skills, the gap in theoretical knowledge could also lead to lower self-efficacy, which tends to be more evident in some self-efficacy subscales explaining clinical laboratory findings and critical values and using existing resources external experts.
According to the relationship between knowledge and self-efficacy regarding CPR-D, knowledge and self-efficacy had a weak and positive correlation. The positive relationship explains how there would be a high level of self-efficacy if there were a high level of knowledge. Partiprajak and Thongpo (2016) highlighted the importance of having high levels of knowledge and self-efficacy for obtaining a better standard of care and higher effectiveness of CPR-D performance. Dayapoglu and Tan (2016) emphasized the significance of awareness, which was correlated with CPR-D self-efficacy. In managing cardiac arrest cases, Turner et al. (2009) suggested that healthcare professionals’ self-efficacy is as essential as the other main factors: knowledge, skill, and attitude. Gusnia and Saragih (2013) have strengthened this idea by considering self-efficacy as the dominant factor for adapting novice nurses to the profession.
Considering all these findings, the effect of self-efficacy on CPR-D performance was strong. Still, having higher levels of self-efficacy in terms of CPR-D has other benefits for healthcare workers’ performance in terms of their attitudes and behaviors.
The major strength of this study was that no data were missing due to the use of an online survey, which required answering all the questions. On the other hand, this study has some limitations. The sample in this study represented participants only from KAUH in Jeddah, which might affect the generalizability of the findings to all hospitals in Saudi Arabia. Additionally, the format was ideal for measuring the nurses’ CPR-D performance by the observation method. However, because of the COVID-19 pandemic, we preferred to use the former method.
In addition, this study has several implications for improving knowledge about CPR-D among nurses. First, applying the CPR-D curricula during internships for healthcare providers is recommended to increase the likelihood of witnessing CPR-D and improving nurses’ practices. Second, the results indicated that continually updating CPR-D knowledge and skills can be helpful for healthcare workers, particularly for nurses, who are usually the first to encounter cardiac arrest patients in the hospital. Moreover, we recommend further research to explore the factors affecting nurses’ knowledge and self-efficacy to improve CPR-D’s early initiation. Finally, future study is required to identify the effect (whether positive or negative) on self-efficacy of witnessing and practicing CPR-D.
Conclusion
Knowledge and self-efficacy are key elements that affect the early initiation of CPR-D by nurses in patients with cardiac arrest. In addition, considering their influence on various factors, they are also good indicators of CPR-D performance. Thus, increasing the levels of knowledge of nursing staff and supporting their self-efficacy for potential clinical scenarios is critical.
Acknowledgment
The authors would like to thank King Abdulaziz University Hospital’s nurses in Jeddah, Saudi Arabia, for their participation.
Declaration of Conflicting Interest
The authors declare no conflicting interest in this study.
Funding
None.
Authors’ Contributions
ZA conceptualized, analyzed, and drafted the manuscript. AA, ME critically reviewed and revised the manuscript. All authors agreed on the final version of the article to be published.
Authors’ Biographies
Zainah D. Alaryani is a Master Student at the Medical-Surgical Nursing, Faculty of Nursing, King Abdulaziz University, Jeddah, Saudi Arabia.
Dr. Aisha Alhofaian is an Assistant Professor at the Medical-Surgical Nursing, Faculty of Nursing, King Abdulaziz University, Jeddah, Saudi Arabia.
Dr. Mona Elhady is an Associate Professor at the Emergency and Critical Care Nursing, Faculty of Nursing, King Abdulaziz University, Jeddah, Saudi Arabia.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- Aranzábal-Alegría, G., Verastegui-Díaz, A., Quiñones-Laveriano, D. M., Quintana-Mendoza, L. Y., Vilchez-Cornejo, J., Espejo, C. B., … Mejia, C. R. (2017). Factors associated to the level of knowledge in cardiopulmonary rejection in hospitals of Peru. Revista Colombiana de Anestesiologia, 45(2), 114-121. 10.1016/j.rca.2016.12.004 [DOI] [Google Scholar]
- Bray, J. E., Smith, K., Case, R., Cartledge, S., Straney, L., & Finn, J. (2017). Public cardiopulmonary resuscitation training rates and awareness of hands-only cardiopulmonary resuscitation: A cross-sectional survey of Victorians. Emergency Medicine Australasia, 29(2), 158-164. 10.1111/1742-6723.12720 [DOI] [PubMed] [Google Scholar]
- Byun, G. J. (2014). The effect of the practice while watching cardiopulmonary cerebral resuscitation education on the competence of cardiopulmonary cerebral resuscitation of the nurses. (Doctoral dissertation), University of Kyungpook National, Daegu. Retrieved from http://dcollection.knu.ac.kr/public_resource [Google Scholar]
- CARES . (2017). CARES summary report: Demographics and survival characteristics of OHCA. CARES reports user guide. Retrieved from https://mycares.net
- Cartledge, S., Saxton, D., Finn, J., & Bray, J. E. (2020). Australia’s awareness of cardiac arrest and rates of CPR training: Results from the Heart Foundation’s HeartWatch survey. BMJ Open, 10(1), e033722. 10.1136/bmjopen-2019-033722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dayapoglu, N., & Tan, M. (2016). Clinical nurses’ knowledge and attitudes toward patients with epilepsy. Epilepsy & Behavior, 61, 206-209. 10.1016/j.yebeh.2016.05.009 [DOI] [PubMed] [Google Scholar]
- Desiani, S., Nuraeni, A., & Priambodo, A. P. (2017). How do knowledge and self-efficacy of internship nursing students in performing cardiopulmonary resuscitation? Belitung Nursing Journal, 3(5), 612-620. 10.33546/bnj.147 [DOI] [Google Scholar]
- Gusnia, S. S., & Saragih, N. (2013). Hubungan karakteristik perawat pada program preceptorship terhadap proses adaptasi perawat baru [Relationship of nurses’ characteristics, preceptorship program, and adaptation process of new nurses]. Jurnal Keperawatan Padjadjaran, 1(1), 10-17. 10.24198/jkp.v1i1.47 [DOI] [Google Scholar]
- Jamieson, L., Williams, L. M., & Dwyer, T. (2002). The need for a new advanced nursing practice role for Australian adult critical care settings. Australian Critical Care, 15(4), 139-145. 10.1016/S1036-7314(02)80028-5 [DOI] [PubMed] [Google Scholar]
- Kim, S., Kim, S. K., Kim, J.-I., Chang, O. J., Choi, J. Y., & Nam, M. R. (2017). Acquisition of CPR-related self-efficacy through BLS program among undergraduate nursing students in Korea. Research Journal of Pharmacy and Technology, 10(7), 2265-2270. 10.5958/0974-360X.2017.00401.2 [DOI] [Google Scholar]
- Kleinman, M. E., Brennan, E. E., Goldberger, Z. D., Swor, R. A., Terry, M., Bobrow, B. J., … Rea, T. (2015). Part 5: adult basic life support and cardiopulmonary resuscitation quality: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation, 132(18_suppl_2), S414-S435. 10.1161/CIR.0000000000000259 [DOI] [PubMed] [Google Scholar]
- Koster, R. W., Baubin, M. A., Bossaert, L. L., Caballero, A., Cassan, P., Castrén, M., … Perkins, G. D. (2010). European Resuscitation Council guidelines for resuscitation 2010 section 2. Adult basic life support and use of automated external defibrillators. Resuscitation, 81(10), 1277-1292. 10.1016/j.resuscitation.2010.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moon, H., & Hyun, H. S. (2019). Nursing students’ knowledge, attitude, self-efficacy in blended learning of cardiopulmonary resuscitation: A randomized controlled trial. BMC Medical Education, 19(1), 1-8. 10.1186/s12909-019-1848-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mozaffarian, D., Benjamin, E. J., Go, A. S., Arnett, D. K., Blaha, M. J., Cushman, M., … Howard, V. J. (2015). Executive summary: heart disease and stroke statistics–2015 update: A report from the American Heart Association. Circulation, 131, 434-441. 10.1161/CIR.0000000000000157 [DOI] [PubMed] [Google Scholar]
- Partiprajak, S., & Thongpo, P. (2016). Retention of basic life support knowledge, self-efficacy and chest compression performance in Thai undergraduate nursing students. Nurse Education in Practice, 16(1), 235-241. 10.1016/j.nepr.2015.08.012 [DOI] [PubMed] [Google Scholar]
- Raosoft . (2004). Sample size calculator. Retrieved from http://www.raosoft.com/samplesize.html
- Roh, Y. S., Issenberg, S. B., Chung, H. S., & Kim, S. S. (2012). Development and psychometric evaluation of the Resuscitation Self-efficacy Scale for nurses. Journal of Korean Academy of Nursing, 42(7), 1079-1086. 10.4040/jkan.2012.42.7.1079 [DOI] [PubMed] [Google Scholar]
- Sachdeva, S. (2020). A study to assess knowledge and practice of basic life support among nurses working in tertiary care hospital, New Delhi, India. Nursing & Care Open Access Journal, 7(2), 48-52. 10.15406/ncoaj.2020.07.00217 [DOI] [Google Scholar]
- Shammah, A. A., Elbakh, A., Jamal, M. M., Dakhiel, A., Althubyani, A., & Mohammed, Z. (2018). Attitudes and awareness towards cardiopulmonary resuscitation among preparatory year students of Umm Al-Qura University. International Journal of Community & Family Medicine, 3, 136. 10.15344/2456-3498/2018/136 [DOI] [Google Scholar]
- Sharp, A. C., Brandt, L., Tuft, E. A., & Jay, S. (2016). Relationship of self-efficacy and teacher knowledge for prospective elementary education teachers. Universal Journal of Educational Research, 4(10), 2432-2439. 10.13189/ujer.2016.041022 [DOI] [Google Scholar]
- Turner, N. M., Lukkassen, I., Bakker, N., Draaisma, J., & ten Cate, O. T. J. (2009). The effect of the APLS-course on self-efficacy and its relationship to behavioural decisions in paediatric resuscitation. Resuscitation, 80(8), 913-918. 10.1016/j.resuscitation.2009.03.028 [DOI] [PubMed] [Google Scholar]
- Verkuyl, M., Atack, L., McCulloch, T., Liu, L., Betts, L., Lapum, J. L., … Romaniuk, D. (2018). Comparison of debriefing methods after a virtual simulation: An experiment. Clinical Simulation in Nursing, 19, 1-7. 10.1016/j.ecns.2018.03.002 [DOI] [Google Scholar]
- Waloyo, E. (2016). Hubungan pengetahuan resusitasi jantung paru dengan self-efficacy perawat di RSUD Wonogiri [Relationship of knowledge ofcardiopulmonary resuscitation and nurses self efficacy in Wonogiri General Hospital]. Surakarta, Indonesia: Stikes Kusuma Husada. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.