Abstract
Objectives:
Few studies have examined risk factors leading to painful colonoscopy and prolonged cecal intubation time in female patients. We aimed to determine the factors associated with painful colonoscopy and prolonged cecal intubation time in female patients.
Methods:
This retrospective study analyzed prospectively collected data from a randomized controlled trial with female patients who underwent colonoscopy. Multivariate logistic and linear regression analyses were performed using the following factors that might be associated with painful colonoscopy and prolonged cecal intubation time, respectively: age, body mass index, history of colonoscopy, previous abdominal surgery, routine use of laxatives, inadequate bowel preparation, sigmoid colon diverticulosis, use of a small-caliber colonoscope, and an inexperienced operator.
Results:
The study enrolled 219 female patients aged >20 years. Using the receiver operating characteristic curve, painful colonoscopy was defined in cases where the visual analogue scale of overall pain was ≥50 mm. Logistic regression analysis for risk factors associated with painful colonoscopy revealed that sigmoid colon diverticulosis [odds ratio (OR), 2.496; 95% confidence interval (CI), 1.013-5.646; p=0.028] was a risk factor for painful colonoscopy; conversely, the use of a small-caliber colonoscope was a negative factor for painful colonoscopy (OR, 0.436; 95% CI, 0.214-0.889, p=0.022). In linear regression analysis, inadequate bowel preparation was significantly associated with prolonged cecal intubation time (β-coefficient, 3.583; 95% confidence interval, 0.578-6.588; p=0.020).
Conclusions:
Female patients with sigmoid colon diverticulosis are more likely to experience severe pain during colonoscopy, and those with inadequate bowel preparation may require more time for cecal intubation.
Keywords: cecal intubation time, colonoscopy, colorectal cancer, pain, woman
Introduction
Globally, colorectal cancer (CRC) is the third-most diagnosed cancer and the second leading cause of cancer-related death in female patients[1]. Therefore, CRC screening programs are recommended for older female patients in many countries[2]. In Japan, all female individuals aged ≥40 years are offered fecal immunohistochemical tests as part of a CRC screening program, and those with positive findings are referred for colonoscopy. This has led to an increase in the number of colonoscopies performed nationally.
Colonoscopies performed during CRC screening programs must be acceptable and tolerable for participants. In particular, the degree of pain that patients experience should be minimal, and completion of cecal intubation should be easy. These are important factors in promoting colonoscopy during the CRC screening programs[3-5]. However, previous studies have reported that female patients experience more pain and longer cecal intubation time during colonoscopy than male patients[6,7]. This is because colonic looping is more frequent in female patients owing to the angulated colon and adhesions following previous gynecological surgery[8-10]. Therefore, female patients often hesitate to attend colonoscopy during CRC screening programs.
Strategies to prevent severe pain and prolonged cecal intubation time during colonoscopy in female patients have been developed and reported in previous works; these include the use of water-exchange intubation techniques[11-13], small-caliber colonoscopes[14-17], sedation[18,19], and modified bowel preparation regimens[20]. However, these strategies also have certain disadvantages, such as longer cecal intubation time, poor manipulation, adverse effects, or higher costs[13,20-23]. Therefore, they should be used only in female patients who have factors that put them at risk of painful colonoscopy and prolonged cecal intubation time. However, to our knowledge, only a few studies have examined the factors associated with painful colonoscopy and prolonged cecal intubation time in female patients. Thus, we aimed to determine these factors using prospectively collected data from a randomized controlled trial (RCT).
Methods
Ethics approval and consent to participate
This study was approved by the institutional review board on May 10, 2021 (approval number: H2021-094). All procedures were performed in accordance with the guidelines of the committee responsible for human experimentation (institutional and national), and the 1964 Helsinki Declaration and its later amendments. Our institutional ethics committee also approved the opt-out method of obtaining consent for the study; accordingly, patients provided informed consent on the institutional website.
Study population
This study was a post-hoc analysis of an RCT that investigated the efficacy of a small-caliber colonoscope in reducing pain during colonoscopy in female patients[17]. The trial was conducted at our institution between October 2013 and November 2017. The study included 220 female patients aged ≥20 years who underwent unsedated colonoscopy. They were randomly assigned in a 1:1 ratio to either undergo the colonoscopy using a small-caliber (PCF-PQ260L; Olympus Medical Systems, Tokyo, Japan) or a standard (CF-Q260AI; Olympus Medical Systems) colonoscope.
Procedure
All study participants underwent bowel preparation with 2 L of polyethylene glycol solution. The endoscopists assessed the quality of bowel preparation based on the extent of the mucosa visible after suctioning the fluid residue; this was performed using the Aronchick Bowel Preparation Scale (excellent, good, fair, poor, or inadequate)[24]. The procedures were performed by eight experienced operators (board-certified fellows of the Japan Gastroenterological Endoscopy Society, each of whom had performed >2,000 colonoscopies) and four inexperienced operators (trainees, each of whom had performed <500 colonoscopies). During the colonoscopy, a 2-mm transparent cap was attached to the tip of the colonoscope.
All patients underwent colonoscopy using air insufflation. Conventional insertion techniques, including loop resolution, position change, and abdominal compression were used if necessary. Cecal intubation time was defined as the time from the intubation of the rectum to the time when the tip of the colonoscope passed to a point proximal to the ileocecal valve so that the base of the cecum was visible. When the colonoscope could not be inserted further, the colonoscopy was deemed unsuccessful and a second colonoscopy was performed using the alternative colonoscope during the same session by the same endoscopists. Withdrawal time was defined as the time taken to withdraw the tip of the colonoscope from the base of the cecum to the anus and included the amount of time required for observation and biopsy of any detected polyps. We examined the polyp pathology by performing a biopsy during the colonoscopy or an endoscopic resection at a later date. Adverse events included post-procedural bleeding and perforation.
Pain scale
Pain during colonoscopy was assessed using a 100-mm visual analogue scale (VAS). Scores of 0 and 100 points indicated no pain and extreme pain, respectively. Before the procedure, the endoscopists or medical assistants explained the VAS scoring system to the patients. After the procedure, the patients were asked to report the overall pain and maximum pain during the colonoscopy using the VAS. In addition, the patient's unacceptance for unsedated colonoscopy was assessed using a questionnaire, with acceptable or unacceptable responses.
Statistical analyses
Continuous variables are expressed as means and standard deviations (SDs), and categorical variables are expressed as numbers and proportions. Based on previous clinical knowledge and our experience[9,25-33], linear or logistic regression analyses were performed using the following factors that might affect pain and cecal intubation time during the colonoscopy: older age, body mass index (BMI) [low (<18.5 kg/m2) or high (>25.0 kg/m2)], history of colonoscopies, previous abdominal surgery, routine use of laxatives, inadequate bowel preparation (fair, poor, or inadequate based on the Aronchick Bowel Preparation Scale), sigmoid colon diverticulosis, use of a small-caliber colonoscope, and an inexperienced operator. Factors with statistical significance in univariate analysis were included in the multivariate analysis. A receiver operating characteristic (ROC) curve was constructed using the results of the questionnaire on the patient's unacceptance for unsedated colonoscopy. The cut-off value for the overall pain VAS score used to predict patient intolerability for unsedated colonoscopy was determined at the inflection point of the ROC curve. Consequently, a painful colonoscopy requiring sedation was defined as a case with a VAS score above the cut-off value. All statistical analyses were performed using SPSS version 26 (IBM Corp., Armonk, NY, USA). All tests were two-sided, and a P-value <0.05 indicated statistical significance.
Results
Baseline characteristics of enrolled patients
The patient selection process is presented in Figure 1. Of the 220 patients originally enrolled in the RCT, one patient with use of sedation for severe pain during colonoscopy was excluded from the current analysis; thus, the patient cohort included 219 female patients (Figure 1). The baseline characteristics of the enrolled patients are presented in Table 1. The mean (SD) patient age was 62.8 (12.9) years. The major indication for colonoscopy was a positive fecal immunohistochemical test result (34.2%). A total of 112 (51.1%) and 119 (54.8%) patients had previously undergone colonoscopy and abdominal surgery, respectively.
Figure 1.
Patient selection process.
Table 1.
Baseline Clinical Characteristics (n=219).
| Factors | Values |
|---|---|
| Age, mean (SD), years | 62.8 (12.9) |
| Height, mean (SD), cm | 154.2 (6.0) |
| Weight, mean (SD), kg | 52.7 (10.0) |
| Waist circumference (SD), cm | 79.4 (10.8) |
| Body mass index, n (%) | |
| Normal (18.5–25.0 kg/m2) | 149 (68.0) |
| Low (<18.5 kg/m2) | 32 (14.6) |
| High (>25.0 kg/m2) | 38 (17.4) |
| Indication for colonoscopy, n (%) | |
| Positive fecal immunochemical test | 75 (34.2) |
| Screening | 45 (20.5) |
| Polyp surveillance | 39 (17.8) |
| Hematochezia | 17 (7.8) |
| Others | 43 (19.6) |
| Pre-existing factors, n (%) | |
| History of colonoscopy | 112 (51.1) |
| Previous abdominal surgery | 120 (54.8) |
| Routine use of laxatives | 26 (11.9) |
| Sigmoid colon diverticulosis | 34 (15.5) |
SD, standard deviation
Procedural outcomes
The procedural outcomes are shown in Table 2. The mean (SD) overall and maximum pain scores were 26.0 (24.0) mm and 37.9 (29.7) mm, respectively. The mean (SD) cecal intubation and withdrawal times were 12.3 (8.8) min and 12.3 (5.3) min, respectively. The rate of inadequate bowel preparation was 18.3% (40/219). Colorectal adenomas were detected in 43.4% (95/219) of the patients. The rate of patients' unacceptance for colonoscopy was 6.7% (15/219). No adverse events were observed in any patients.
Table 2.
Procedural Outcomes of the Patients (n=219).
| Factors | Values |
|---|---|
| Inexperienced operator, n (%) | 68 (31.1) |
| Use of a small-caliber colonoscope, n (%) | 109 (49.8) |
| Procedural pain score, mean (SD), mm* | |
| Overall pain | 26.0 (24.0) |
| Maximum pain | 37.9 (29.7) |
| Cecal intubation time, mean (SD), min | 12.3 (8.8) |
| Withdrawal time, mean (SD), min | 12.3 (5.3) |
| Total procedure time, mean (SD), min | 24.6 (10.1) |
| Use of abdominal compression, n (%) | 128 (58.4) |
| Change of colonoscope, n (%) | 8 (3.7) |
| Inadequate bowel preparation, n (%) † | 40 (18.3) |
| Adenoma detection, n (%) | 95 (43.4) |
| Patient’s unacceptance for unsedated colonoscopy, n (%) | 15 (6.7) |
| Adverse events, n (%) | 0 (0.0) |
SD, standard deviation
*Procedural pain was evaluated using the visual analog scale.
†Fair, poor, or inadequate based on the Aronchick Bowel Preparation Scale.
Cut-off value for painful colonoscopy
As presented in Figure 2, a ROC curve was used to determine the cut-off value to predict intolerability for unsedated colonoscopy. Consequently, the cut-off value was a VAS score of 50 mm with a sensitivity of 73.3% and a specificity of 84.3. The area under the curve was 83.3. Thus, a painful colonoscopy was defined as a case with a VAS score of overall pain ≥50 mm.
Figure 2.
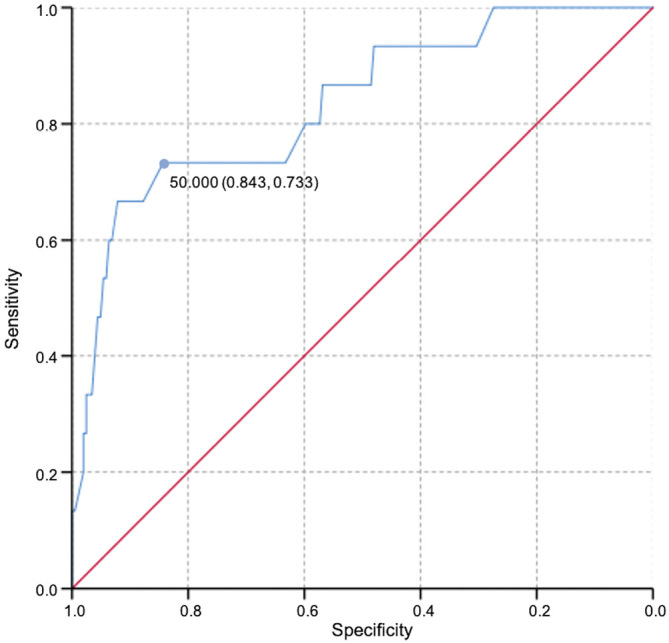
Cut-off value by receiver operating characteristic curve. The cut-off value of the visual analogue scale of overall pain that was associated with painful colonoscopy is 50 mm (sensitivity, 73.3%; specificity, 84.3%; area under the curve, 0.841).
Factors associated with painful colonoscopy
The results of the logistic regression analyses for factors associated with painful colonoscopy are presented in Table 3. The sigmoid colon diverticulosis and the use of a small-caliber colonoscope had a significant difference in the univariate analysis. These factors were also identified as independent factors in multivariate analyses (sigmoid colon diverticulosis: OR, 2.496; 95% CI, 1.103-5.646, p=0.028; use of a small-caliber colonoscope: OR, 0.436; 95% CI, 0.214-0.889, p=0.022).
Table 3.
Results of the Logistic Regression Analysis of Factors Responsible for Painful Colonoscopy.
| Factors | Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|---|
| Odds ratio (95% CI) | P-value | Odds ratio (95% CI) | P-value | ||
| Older age, years | 0.997 (0.972–1.023) | 0.823 | |||
| BMI | |||||
| Normal (18.5–25.0 kg/m2) | 1 | ||||
| Low (<18.5 kg/m2) | 1.850 (0.769–4.460) | 0.170 | |||
| High (>25.0 kg/m2) | 1.260 (0.519–3.060) | 0.608 | |||
| History of colonoscopy | |||||
| Absent | 1 | ||||
| Present | 1.001 (0.514–1.950) | 0.998 | |||
| Previous abdominal surgery | |||||
| Absent | 1 | ||||
| Present | 1.334 (0.676–2.632) | 0.405 | |||
| Routine use of laxatives | |||||
| Absent | 1 | ||||
| Present | 0.718 (0.234–2.204) | 0.563 | |||
| Inadequate bowel preparation* | |||||
| Absent | 1 | ||||
| Present | 1.238 (0.539–2.842) | 0.614 | |||
| Sigmoid colon diverticulosis | |||||
| Absent | 1 | 1 | |||
| Present | 2.710 (1.215–6.044) | 0.015 | 2.496 (1.103–5.646) | 0.028 | |
| Use of a small-caliber colonoscope | |||||
| Absent | 1 | 1 | |||
| Present | 0.412 (0.204–0.832) | 0.013 | 0.436 (0.214–0.889) | 0.022 | |
| Inexperienced operator | |||||
| Absent | 1 | ||||
| Present | 0.829 (0.397–1.735) | 0.620 | |||
BMI, body mass index; CI, confidence interval
*Fair, poor, or inadequate based on the Aronchick Bowel Preparation scale.
Factors associated with increased cecal intubation time
The results of the linear regression analyses for factors associated with increased cecal intubation time are presented in Table 4. The inadequate bowel preparation had a significant difference in the univariate analysis. It was also identified as a factor associated with increased cecal intubation time (β-coefficient, 3.583; 95% CI, 0.578-6.588, p=0.020).
Table 4.
Results of the Linear Regression Analysis of Factors Leading to Prolonged Cecal Intubation Time.
| Factors | Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|---|
| β-coefficient
(95% CI) |
Standard
error |
P-value | β-coefficient
(95% CI) |
Standard
error |
P-value | ||
| Older age, years | 0.020 (-0.069–16.796) | 0.046 | 0.633 | ||||
| BMI | |||||||
| Normal (18.5–25.0 kg/m2) | 1 | ||||||
| Low (<18.5 kg/m2) | 0.260 (-3.124–3.644) | 1.717 | 0.880 | ||||
| High (>25.0 kg/m2) | 2.130 (-1.027–5.286) | 2.130 | 0.185 | ||||
| History of colonoscopy | |||||||
| 1 | |||||||
| 0.522 (-1.829–2.873) | 1.193 | 0.662 | |||||
| Previous abdominal surgery | |||||||
| 1 | |||||||
| 1.173 (-1.184–3.530) | 1.196 | 0.328 | |||||
| Routine use of laxatives | |||||||
| 1 | |||||||
| 0.496 (-3.139–4.130) | 1.844 | 0.788 | |||||
| Inadequate bowel preparation* | |||||||
| 1 | 1 | ||||||
| 3.583 (0.578–6.588) | 1.525 | 0.020 | 3.583 (0.578–6.588) | 1.525 | 0.020 | ||
| Sigmoid colon diverticulosis | |||||||
| 1 | |||||||
| 1.799 (-1.438–5.037) | 1.643 | 0.275 | |||||
| Use of a small-caliber colonoscope | |||||||
| 1 | |||||||
| -1.326 (-3.671–1.018) | 1.190 | 0.266 | |||||
| Inexperienced operator | |||||||
| 1 | |||||||
| 0.908 (-1.630–3.446) | 1.288 | 0.481 | |||||
BMI, body mass index; CI, confidence interval
* Fair, poor, or inadequate based on the Aronchick Bowel Preparation scale.
Discussion
In the study limited to female patients, we found that sigmoid colon diverticulosis was an independent risk factor for painful colonoscopy, and the use of a small-caliber colonoscope was a negative independent factor for painful colonoscopy. In addition, inadequate bowel preparation was significantly associated with prolonged cecal intubation time.
Many studies have suggested that female sex is a risk factor leading to painful colonoscopy and prolonged cecal intubation time[9,34,35]. Generally, female patients have a more angular sigmoid colon than male patients because of differences in musculoskeletal structure. Moreover, after gynecological surgery, female patients may have adhesions in the pelvis and a freely moving sigmoid colon owing to the larger intra-pelvic space[36-40]. Consequently, these factors may cause severe pain and prolonged cecal intubation time during colonoscopy. Therefore, female patients often hesitate to undergo colonoscopy during CRC screening programs.
To overcome this issue, several strategies have been reported to reduce the pain and cecal intubation time during colonoscopy, such as the water exchange technique[11-13], use of a small-caliber colonoscope[14-17], sedation[18,19], and modified bowel preparation regimens[20]. However, these strategies also have certain disadvantages. Water-exchange intubation techniques usually have a longer cecal intubation time than those of conventional intubation techniques[12]. A small-caliber colonoscope is less manipulatable than a standard colonoscope, and it is unsuitable for therapeutic colonoscopies. Sedation is associated with various adverse events[21-23]. Modified bowel preparation regimens have a higher cost than those of conventional regimens[20]. Therefore, these strategies should be used only in female patients with risk factors that might lead to painful colonoscopy and prolonged cecal intubation time. However, only a few studies have examined the risk factors associated with painful colonoscopy and prolonged cecal intubation time in female patients.
We examined the factors associated with painful colonoscopy and prolonged cecal intubation time in female patients, based on previous reports and our own experience[9,25-33]. We discovered that the following independent factors play a crucial role: sigmoid colon diverticulosis is associated with painful colonoscopy, and inadequate bowel preparation is associated with prolonged cecal intubation time. Sigmoid colon diverticulosis was reported to be associated with painful colonoscopy[31]. The sigmoid colon diverticulum often becomes infected, causing recurrent diverticulitis. Consequently, this may lead to adhesions in the sigmoid colon, causing severe pain during the passage of a colonoscope. Inadequate bowel preparation has been reported to be associated with prolonged cecal intubation time as the residual stool impairs visualization of the colon[9,30,32]. Therefore, the results of our study are in line with these previous findings.
In this study, the mean cecal intubation time was 12.3 min, which is longer than the corresponding in previous reports (approximately 5-7 min)[14,41]. This difference may be attributed to the following reasons. First, the study participants who were limited to female patients affected the cecal intubation time. Interestingly, female sex was reported to be a risk factor for prolonged cecal intubation time[42]. Second, the study participants were limited to patients who underwent unsedated colonoscopy. Especially, previous studies have reported that pain during cecal intubation in unsedated colonoscopy is associated with prolonged cecal intubation time[43,44]. These factors might have led to a longer cecal intubation time than that of previous studies.
Our study had several strengths. First, the original data were prospectively collected for an RCT, which minimized measurement bias. Second, even after full recovery of consciousness, sedated colonoscopy may have caused memory bias in some participants. In contrast, the participants of our study were not given any sedation; therefore, the pain scale could accurately reflect the participant's pain during colonoscopy. Third, this study set a cut-off value for painful colonoscopy and conducted multivariate regression analyses to find the risk factors associated with painful colonoscopy. This result could help clinicians select which patient population might be more suitable to undergo additional interventions, such as sedation or a small-caliber colonoscope.
However, our study had some limitations. First, we could not evaluate the factors that could influence the perception of pain, such as a patient's physical condition and anxiety, which may have increased or decreased the pain threshold. Second, the inadequate bowel preparation rate in this study was 18.3%, higher than those reported in previous studies[45,46]. The reason is considered that more than half of the study participants had a history of abdominal surgery. Previous studies have reported that previous abdominal surgery was an independent risk factor for inadequate bowel preparation[47,48]. The higher rate of inadequate bowel preparation may have affected the study outcomes, which resulted in a bias. Third, this was a single-center study, and the results may not be as generalizable as those obtained from a multicenter study. Similar studies with additional cases and other cohorts will be required to validate our findings.
In conclusion, female patients with sigmoid colon diverticulosis are more likely to experience severe pain during colonoscopy. Moreover, those with inadequate bowel preparation may require more time for cecal intubation. These findings can help guide clinicians to implement targeted strategies to minimize pain and cecal intubation time during colonoscopy for patients with these risk factors.
Conflicts of Interest
There are no conflicts of interest.
Author Contributions
Yasuhiko Hamada contributed to the study conception and design. Yasuhiko Hamada, Kyosuke Tanaka, Yohei Ikenoyama, Noriyuki Horiki, Junya Tsuboi, Reiko Yamada, and Misaki Nakamura contributed to the data collection. Hayato Nakagawa supervised the study. The first draft of the manuscript was written by Yasuhiko Hamada, and all authors reviewed the subsequent versions of the manuscript. All authors have read and approved the final manuscript.
Approval by Institutional Review Board (IRB)
The study was approved by the ethics committee of Mie University Hospital on May 10, 2021 (approval number H2021-094).
Acknowledgements
The authors would like to thank the medical staff members of the Department of Endoscopy at the institution for their contributions to our study. We would also like to thank Editage (www.editage.com) for English language editing.
References
- 1.Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021 May; 71(3): 209-49. [DOI] [PubMed] [Google Scholar]
- 2.Bénard F, Barkun AN, Martel M, et al. Systematic review of colorectal cancer screening guidelines for average-risk adults: Summarizing the current global recommendations. World J Gastroenterol. 2018 Jan; 24(1): 124-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pylvänäinen K, Kairaluoma M, Mecklin JP. Compliance and satisfaction with long-term surveillance in Finnish HNPCC families. Fam Cancer. 2006; 5(2): 175-8. [DOI] [PubMed] [Google Scholar]
- 4.McLachlan SA, Clements A, Austoker J. Patients' experiences and reported barriers to colonoscopy in the screening context--a systematic review of the literature. Patient Educ Couns. 2012 Feb; 86(2): 137-46. [DOI] [PubMed] [Google Scholar]
- 5.Denters MJ, Schreuder M, Depla AC, et al. Patients' perception of colonoscopy: patients with inflammatory bowel disease and irritable bowel syndrome experience the largest burden. Eur J Gastroenterol Hepatol. 2013 Aug; 25(8): 964-72. [DOI] [PubMed] [Google Scholar]
- 6.Ghanouni A, Plumb A, Hewitson P, et al. Patients' experience of colonoscopy in the English Bowel Cancer Screening Programme. Endoscopy. 2016 Mar; 48(3): 232-40. [DOI] [PubMed] [Google Scholar]
- 7.Grilo Bensusan I, Herrera Martín P, Aguado Álvarez MV. Prospective study of anxiety in patients undergoing an outpatient colonoscopy. Rev Esp Enferm Dig. 2016 Dec; 108(12): 765-9. [DOI] [PubMed] [Google Scholar]
- 8.Saunders BP, Fukumoto M, Halligan S, et al. Why is colonoscopy more difficult in women? Gastrointest Endosc. 1996 Feb; 43(2 Pt 1): 124-6. [DOI] [PubMed] [Google Scholar]
- 9.Kim WH, Cho YJ, Park JY, et al. Factors affecting insertion time and patient discomfort during colonoscopy. Gastrointest Endosc. 2000 Nov; 52(5): 600-5. [DOI] [PubMed] [Google Scholar]
- 10.Shah SG, Brooker JC, Thapar C, et al. Patient pain during colonoscopy: an analysis using real-time magnetic endoscope imaging. Endoscopy. 2002 Jun; 34(6): 435-40. [DOI] [PubMed] [Google Scholar]
- 11.Hsieh YH, Koo M, Leung FW. A patient-blinded randomized, controlled trial comparing air insufflation, water immersion, and water exchange during minimally sedated colonoscopy. Am J Gastroenterol. 2014 Sep; 109(9): 1390-400. [DOI] [PubMed] [Google Scholar]
- 12.Cadoni S, Falt P, Gallittu P, et al. Water exchange is the least painful colonoscope insertion technique and increases completion of unsedated colonoscopy. Clin Gastroenterol Hepatol. 2015 Nov; 13(11): 1972-80. [DOI] [PubMed] [Google Scholar]
- 13.Cadoni S, Sanna S, Gallittu P, et al. A randomized, controlled trial comparing real-time insertion pain during colonoscopy confirmed water exchange to be superior to water immersion in enhancing patient comfort. Gastrointest Endosc. 2015 Mar; 81(3): 557-66. [DOI] [PubMed] [Google Scholar]
- 14.Sato K, Ito S, Shigiyama F, et al. A prospective randomized study on the benefits of a new small-caliber colonoscope. Endoscopy. 2012 Aug; 44(8): 746-53. [DOI] [PubMed] [Google Scholar]
- 15.Nemoto D, Utano K, Endo S, et al. Ultrathin versus pediatric instruments for colonoscopy in older female patients: A randomized trial. Dig Endosc. 2017 Mar; 29(2): 168-74. [DOI] [PubMed] [Google Scholar]
- 16.Sofi AA, Nawras A, Khan MA, et al. Meta-analysis of the performance of ultrathin vs. standard colonoscopes. Endoscopy. 2017 Apr; 49(4): 351-8. [DOI] [PubMed] [Google Scholar]
- 17.Hamada Y, Tanaka K, Katsurahara M, et al. Efficacy of a small-caliber colonoscope for pain in female patients during unsedated colonoscopy: a randomized controlled study. Endosc Int Open. 2021 Jul; 9(7): E1055-e61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dossa F, Dubé C, Tinmouth J, et al. Practice recommendations for the use of sedation in routine hospital-based colonoscopy. BMJ Open Gastroenterol. 2020; 7(1): e000348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schult AL, Botteri E, Hoff G, et al. Women require routine opioids to prevent painful colonoscopies: a randomised controlled trial. Scand J Gastroenterol. 2021 Dec; 56(12): 1480-9. [DOI] [PubMed] [Google Scholar]
- 20.Millien VO, Mansour NM. Bowel preparation for colonoscopy in 2020: A look at the past, present, and future. Curr Gastroenterol Rep. 2020 May; 22(6): 28. [DOI] [PubMed] [Google Scholar]
- 21.Hassan C, Rex DK, Cooper GS, et al. Endoscopist-directed propofol administration versus anesthesiologist assistance for colorectal cancer screening: a cost-effectiveness analysis. Endoscopy. 2012 May; 44(5): 456-64. [DOI] [PubMed] [Google Scholar]
- 22.Lee SW, Chang JH, Ji JS, et al. Effect of Dynamic position changes on adenoma detection during colonoscope withdrawal: a randomized controlled multicenter trial. Am J Gastroenterol. 2016 Jan; 111(1): 63-9. [DOI] [PubMed] [Google Scholar]
- 23.Wernli KJ, Brenner AT, Rutter CM, et al. Risks associated with anesthesia services during colonoscopy. Gastroenterology. 2016 Apr; 150(4): 888-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kastenberg D, Bertiger G, Brogadir S. Bowel preparation quality scales for colonoscopy. World J Gastroenterol. 2018 Jul; 24(26): 2833-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Waye JD, Bashkoff E. Total colonoscopy: is it always possible? Gastrointest Endosc. 1991 Mar-Apr; 37(2): 152-4. [DOI] [PubMed] [Google Scholar]
- 26.Church JM. Complete colonoscopy: how often? And if not, why not? Am J Gastroenterol. 1994 Apr; 89(4): 556-60. [PubMed] [Google Scholar]
- 27.Cirocco WC, Rusin LC. Factors that predict incomplete colonoscopy. Dis Colon Rectum. 1995 Sep; 38(9): 964-8. [DOI] [PubMed] [Google Scholar]
- 28.Anderson JC, Gonzalez JD, Messina CR, et al. Factors that predict incomplete colonoscopy: thinner is not always better. Am J Gastroenterol. 2000 Oct; 95(10): 2784-7. [DOI] [PubMed] [Google Scholar]
- 29.Anderson JC, Messina CR, Cohn W, et al. Factors predictive of difficult colonoscopy. Gastrointest Endosc. 2001 Nov; 54(5): 558-62. [DOI] [PubMed] [Google Scholar]
- 30.Bernstein C, Thorn M, Monsees K, et al. A prospective study of factors that determine cecal intubation time at colonoscopy. Gastrointest Endosc. 2005 Jan; 61(1): 72-5. [DOI] [PubMed] [Google Scholar]
- 31.Dafnis G, Granath F, Påhlman L, et al. Patient factors influencing the completion rate in colonoscopy. Dig Liver Dis. 2005 Feb; 37(2): 113-8. [DOI] [PubMed] [Google Scholar]
- 32.Takahashi Y, Tanaka H, Kinjo M, et al. Prospective evaluation of factors predicting difficulty and pain during sedation-free colonoscopy. Dis Colon Rectum. 2005 Jun; 48(6): 1295-300. [DOI] [PubMed] [Google Scholar]
- 33.Chung YW, Han DS, Yoo KS, et al. Patient factors predictive of pain and difficulty during sedation-free colonoscopy: a prospective study in Korea. Dig Liver Dis. 2007 Sep; 39(9): 872-6. [DOI] [PubMed] [Google Scholar]
- 34.Park DI, Kim HJ, Park JH, et al. Factors affecting abdominal pain during colonoscopy. Eur J Gastroenterol Hepatol. 2007 Aug; 19(8): 695-9. [DOI] [PubMed] [Google Scholar]
- 35.Elphick DA, Donnelly MT, Smith KS, et al. Factors associated with abdominal discomfort during colonoscopy: a prospective analysis. Eur J Gastroenterol Hepatol. 2009 Sep; 21(9): 1076-82. [DOI] [PubMed] [Google Scholar]
- 36.Bat L, Williams CB. Usefulness of pediatric colonoscopes in adult colonoscopy. Gastrointest Endosc. 1989 Jul-Aug; 35(4): 329-32. [DOI] [PubMed] [Google Scholar]
- 37.Marshall JB. Use of a pediatric colonoscope improves the success of total colonoscopy in selected adult patients. Gastrointest Endosc. 1996 Dec; 44(6): 675-8. [DOI] [PubMed] [Google Scholar]
- 38.Han Y, Uno Y, Munakata A. Does flexible small-diameter colonoscope reduce insertion pain during colonoscopy? World J Gastroenterol. 2000 Oct; 6(5): 659-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Marshall JB, Perez RA, Madsen RW. Usefulness of a pediatric colonoscope for routine colonoscopy in women who have undergone hysterectomy. Gastrointest Endosc. 2002 Jun; 55(7): 838-41. [DOI] [PubMed] [Google Scholar]
- 40.Anderson JC, Walker G, Birk JW, et al. Tapered colonoscope performs better than the pediatric colonoscope in female patients: a direct comparison through tandem colonoscopy. Gastrointest Endosc. 2007 Jun; 65(7): 1042-7. [DOI] [PubMed] [Google Scholar]
- 41.von Renteln D, Robertson DJ, Bensen S, et al. Prolonged cecal insertion time is associated with decreased adenoma detection. Gastrointest Endosc. 2017 Mar; 85(3): 574-80. [DOI] [PubMed] [Google Scholar]
- 42.Jaruvongvanich V, Sempokuya T, Laoveeravat P, et al. Risk factors associated with longer cecal intubation time: a systematic review and meta-analysis. Int J Colorectal Dis. 2018 Apr; 33(4): 359-65. [DOI] [PubMed] [Google Scholar]
- 43.Wang L, Jia H, Luo H, et al. A novel intubation discomfort score to predict painful unsedated colonoscopy. Medicine (Baltimore). 2021 Mar; 100(10): e24907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hsieh YH, Koo M, Tseng CW. Factors associated with prolonged cecal insertion time in patients undergoing water exchange colonoscopy. J Gastroenterol Hepatol. 2022 Jul; 37(7): 1326-32. [DOI] [PubMed] [Google Scholar]
- 45.Dik VK, Moons LM, Hüyük M, et al. Predicting inadequate bowel preparation for colonoscopy in participants receiving split-dose bowel preparation: development and validation of a prediction score. Gastrointest Endosc. 2015 Mar; 81(3): 665-72. [DOI] [PubMed] [Google Scholar]
- 46.Machlab S, Martínez-Bauer E, López P, et al. Comparable quality of bowel preparation with single-day versus three-day low-residue diet: Randomized controlled trial. Dig Endosc. 2021 Jul; 33(5): 797-806. [DOI] [PubMed] [Google Scholar]
- 47.Gimeno-García AZ, Baute JL, Hernandez G, et al. Risk factors for inadequate bowel preparation: a validated predictive score. Endoscopy. 2017 Jun; 49(6): 536-43. [DOI] [PubMed] [Google Scholar]
- 48.Woo DH, Kim KO, Jeong DE, et al. Prospective analysis of factors associated with inadequate bowel preparation for colonoscopy in actual clinical practice. Intest Res. 2018 Apr; 16(2): 293-8. [DOI] [PMC free article] [PubMed] [Google Scholar]



