Abstract
Background
The post‐COVID‐19 condition (PCC) consists of a wide array of symptoms including fatigue and impaired daily living. People seek a wide variety of approaches to help them recover.
A new belief, arising from a few laboratory studies, is that 'microclots' cause the symptoms of PCC. This belief has been extended outside these studies, suggesting that to recover people need plasmapheresis (an expensive process where blood is filtered outside the body). We appraised the laboratory studies, and it was clear that the term 'microclots' is incorrect to describe the phenomenon being described. The particles are amyloid and include fibrin(ogen); amyloid is not a part of a thrombus which is a mix of fibrin mesh and platelets. Initial acute COVID‐19 infection is associated with clotting abnormalities; this review concerns amyloid fibrin(ogen) particles in PCC only.
We have reported here our appraisal of laboratory studies investigating the presence of amyloid fibrin(ogen) particles in PCC, and of evidence that plasmapheresis may be an effective therapy to remove amyloid fibrin(ogen) particles for treating PCC.
Objectives
Laboratory studies review
To summarize and appraise the research reports on amyloid fibrin(ogen) particles related to PCC.
Randomized controlled trials review
To assess the evidence of the safety and efficacy of plasmapheresis to remove amyloid fibrin(ogen) particles in individuals with PCC from randomized controlled trials.
Search methods
Laboratory studies review
We searched for all relevant laboratory studies up to 27 October 2022 using a comprehensive search strategy which included the search terms ‘COVID’, ‘amyloid’, ‘fibrin’, ‘fibrinogen’.
Randomized controlled trials review
We searched the following databases on 21 October 2022: Cochrane COVID‐19 Study Register; MEDLINE (Ovid); Embase (Ovid); and BIOSIS Previews (Web of Science). We also searched the WHO International Clinical Trials Registry Platform and ClinicalTrials.gov for trials in progress.
Selection criteria
Laboratory studies review
Laboratory studies that investigate the presence of amyloid fibrin(ogen) particles in plasma samples from patients with PCC were eligible. This included studies with or without controls.
Randomized controlled trials review
Studies were eligible if they were of randomized controlled design and investigated the effectiveness or safety of plasmapheresis for removing amyloid fibrin(ogen) particles for treating PCC.
Data collection and analysis
Two review authors applied study inclusion criteria to identify eligible studies and extracted data.
Laboratory studies review
We assessed the risk of bias of included studies using pre‐developed methods for laboratory studies. We planned to perform synthesis without meta‐analysis (SWiM) as described in our protocol.
Randomized controlled trials review
We planned that if we identified any eligible studies, we would assess risk of bias and report results with 95% confidence intervals. The primary outcome was recovery, measured using the Post‐COVID‐19 Functional Status Scale (absence of symptoms related to the illness, ability to do usual daily activities, and a return to a previous state of health and mind).
Main results
Laboratory studies review
We identified five laboratory studies. Amyloid fibrin(ogen) particles were identified in participants across all studies, including those with PCC, healthy individuals, and those with diabetes. The results of three studies were based on visual images of amyloid fibrin(ogen) particles, which did not quantify the amount or size of the particles identified. Formal risk of bias assessment showed concerns in how the studies were conducted and reported. This means the results were insufficient to support the belief that amyloid fibrin(ogen) particles are associated with PCC, or to determine whether there is a difference in the amount or size of amyloid fibrin(ogen) particles in the plasma of people with PCC compared to healthy controls.
Randomized controlled trials review
We identified no trials meeting our inclusion criteria.
Authors' conclusions
In the absence of reliable research showing that amyloid fibrin(ogen) particles contribute to the pathophysiology of PCC, there is no rationale for plasmapheresis to remove amyloid fibrin(ogen) particles in PCC. Plasmapheresis for this indication should not be used outside the context of a well‐conducted randomized controlled trial.
Keywords: Humans, COVID-19, Fibrin, Fibrin/therapeutic use, Plasmapheresis
Plain language summary
What is the evidence that 'microclots' cause the post‐COVID‐19 syndrome, and is removal using plasmapheresis justified?
Key messages
1. The term 'microclots' is not the correct term for the particles being investigated in people with post‐COVID‐19 syndrome, as they are not clots. The term 'amyloid fibrin(ogen) particles' is more appropriate.
2. The evidence shows that amyloid fibrin(ogen) particles are found in healthy people and those with other diseases, so they are not unique to post‐COVID‐19 condition.
3. Patients should not receive plasmapheresis for this indication outside the context of a properly conducted placebo (dummy)‐controlled randomized clinical trial (a type of study where participants are randomly assigned to one of two or more treatment groups).
What did we want to find out?
Post‐COVID‐19 condition (sometimes called 'long COVID') refers to a condition in which a patient experiences a variety of symptoms for at least 12 weeks after having initial (acute) COVID‐19 infection. Symptoms can range in severity and include fatigue, brain fog, and headaches, and lead to impaired quality of life. The cause of post‐COVID‐19 condition (PCC) is a source of debate. One theory is that it is caused by small clots in the blood, termed 'microclots' by the authors of a set of laboratory studies that investigate them. The particles described appear to contain proteins called amyloid and fibrin(ogen), so we refer to them as amyloid fibrin(ogen) particles to reflect their components.
It has been suggested that these particles could be removed from the blood using a technique called plasmapheresis, in which the blood is removed from the body and the plasma component of a patient's blood is filtered by a machine to remove any particles. If these particles were responsible for the symptoms of PCC, removing them may treat patients of their symptoms. The rationale for this treatment in PCC is unproven, and is associated with potential risks to patients.
What did we do?
We wanted to investigate the theory that amyloid fibrin(ogen) particles could be the cause of post‐COVID‐19 condition.
The review was done in two steps, as follows.
1. A review of laboratory studies that investigate whether amyloid fibrin(ogen) particles are found in blood samples from people with post‐COVID‐19 condition. This research is found in full detail in Appendix 1.
2. A review of randomized trials that investigate whether plasmapheresis is a safe and effective treatment for removing amyloid fibrin(ogen) particles in people with post‐COVID‐19 condition.
What did we find?
Laboratory studies review
We identified five studies that assessed whether amyloid fibrin(ogen) particles were present in the blood of patients with post‐COVID‐19 condition. The studies identified these particles in healthy controls, those with type 2 diabetes, and those with PCC, meaning they are not unique to PCC. We also identified problems with how these studies were conducted and how the findings were presented, for example it is unclear whether these particles were found in all participants with PCC, or only some.
Randomized controlled trials review
We found no studies where patients with post‐COVID‐19 condition had undergone plasmapheresis with the intention of removing amyloid fibrin(ogen) particles. We also did not find any ongoing trials that are investigating this.
What are the limitations of the evidence?
The evidence is unable to demonstrate if amyloid fibrin(ogen) particles contribute to the post‐COVID‐19 condition. Our analysis did not consider other supposed mechanisms for the post‐COVID‐19 condition and plasmapheresis in the context of other such mechanisms.
How up‐to‐date is this review?
We conducted a search for studies on 21 October 2022 (randomized controlled trials) and 27 October 2022 (laboratory studies).
Background
Description of the condition
The post‐COVID‐19 condition is an important public health problem. With an estimated global rate of over 609 million cases of SARS‐CoV‐2 infection and 5.5 million deaths due to acute COVID‐19 infection, an uncertain but likely considerable proportion of patients may develop persisting symptoms for more than 12 weeks (NHS 2023a), which is termed post‐COVID‐19 condition (PCC), or 'long COVID'. Post‐COVID‐19 condition appears to be comparable to other postviral conditions in that patients experience fatigue, and some experience other symptoms associated with the condition which impairs quality of life (Miller 2020; Owens 2022). These symptoms include pain, discomfort, problems with daily living, comorbid mental health conditions including depression and anxiety, and mobility issues (CDC 2022). One study estimated that 12.7% of individuals with COVID‐19 will experience long‐term symptoms (Ballering 2022).
There are several theories behind the pathophysiology of PCC. On one side, research suggests that the underlying mechanisms could include immune dysregulation, auto‐immunity, endothelial dysfunction, occult viral persistence, and coagulation activation (Castanares‐Zapatero 2022). On another side, pathophysiology may relate to disturbances in homeostatic mechanisms in the brain (Lemogne 2023). Some symptoms experienced by patients show no correlating abnormalities on biomedical tests (Mandal 2021). Although there are many similarities between PCC and other postviral syndromes, new theories have emerged for PCC. One proposed explanation for PCC is the symptoms are caused by amyloid fibrin(ogen) particles circulating in the blood (Pretorius 2021). According to this theory, amyloid fibrin(ogen) particles form, obstruct blood vessels, and cause the variety of symptoms seen in the condition. Whilst there appears to be some evidence for clotting dysfunction following acute COVID‐19 infection (Katsoularis 2022), whether this persists and causes PCC is unclear. This review concerns PCC only, and not acute COVID‐19.
Due to the uncertain pathophysiology of PCC, evidence‐based treatments for post‐COVID‐19 condition are limited. People with PCC may seek a wide variety of treatment options to alleviate their symptoms.
Description of the intervention
Plasmapheresis is a therapeutic procedure whereby whole blood is withdrawn from a large vein, and a machine is used to filter the blood in order to separate the liquid portion of blood (plasma) from the cellular element (NHS 2023b). This may be used to remove agents implicated in disease; with respect to PCC this could be 'microclots'. The cells are then transfused back into the vein along with a plasma replacement. Plasma replacement may include albumin, saline, or another plasma replacement fluid.
Plasmapheresis is technically challenging and requires specialist centres. Side effects are reported to occur in up to 36% of treatments (Shemin 2007). Serious adverse effects associated with plasmapheresis are uncommon (reported in 0.12% of 4857 treatments), but include bleeding, clotting abnormalities, infection, and allergic reactions (Basic‐Jukic 2005).
How the intervention might work
Plasmapheresis is performed on people with PCC in some specialist clinics with the intention of removing amyloid fibrin(ogen) particles. Clinics in Europe offering this treatment for PCC have been reported to charge EUR 1685 to EUR 2000 per session, with several sessions often recommended for patients to experience a change in their symptoms (Apheresis Center 2023; Madlen 2022). Patients can self‐refer for treatment by filling in a medical questionnaire, and it appears that no formal testing to determine if patients have amyloid fibrin(ogen) particles is performed prior to treatment, or afterwards, to determine if they have been removed (Apheresis Center 2023; BBraun 2023).
We therefore decided to conduct a formal systematic review and critical appraisal of laboratory studies investigating the presence of amyloid fibrin(ogen) in PCC. This systematic review is described briefly below, but is provided in full detail in Appendix 1.
It is possible that plasmapheresis may be offered for treating PCC under the rationale of other mechanisms; however, scientific and public interest is currently focused on the role of amyloid fibrin(ogen) particles. This review therefore focused on this proposed mechanism for treating PCC.
Laboratory studies review
Background
This protocol was developed in advance with quality assessment criteria, and conducted by a team of methodologists and topic specialists (Fox 2023a; Fox 2023b). Full details are provided in Appendix 1, and we have summarized the review and findings below.
We first appraised the term 'microclots'. It appears that the term 'clots' or 'microclots' which is adopted throughout the laboratory studies is not an accurate definition of the blood components involved. A clot is defined as fibrin and/or platelet clumping together, and a clot within a blood vessel is known as a thrombus (ASH 2023). Blood clots have a recognized structure consisting of a mesh of crosslinked fibrin protein together with aggregated platelets and red blood cells that form a plug to seal sites of injury (Mihalko 2020). The particles described in the studies include amyloid and either fibrinogen or fibrin (or both), and many other proteins are present in them, but they are not true clots. In this review, we use a more descriptive term for the blood components being reported, that is amyloid fibrin(ogen) particles. We suggest that future studies refrain from using the term 'microclot'. This is further detailed in Appendix 1.
Review purpose and inclusion criteria
The purpose was to appraise the research reports on amyloid fibrin(ogen) particles related to PCC. Studies included any participant diagnosed with PCC, with or without controls. We defined 'post‐COVID‐19 condition' as people with persistent symptoms for at least 12 weeks after an initial diagnosis of SARS‐CoV‐2 infection by polymerase chain reaction (PCR) (WHO 2021). Symptoms included demonstration of fatigue and impaired functioning. Outcomes extracted were presence of aggregate particles in plasma, using any one of the following techniques: fluorescence imaging, laser scanning confocal imaging, fluorescent dyes for amyloid proteins, mass spectrometry analysis of protein composition, and electron microscopy. In our assessment of study quality, we evaluated three domains: collection and handling of samples, experimental methods, and reporting of the results. The specific questions used in these assessments are outlined in Appendix 1.
Search strategy
We searched for all relevant laboratory studies up to 27 October 2022 using a comprehensive search strategy which included the search terms ‘COVID’, ‘amyloid’, ‘fibrin’, and ‘fibrinogen’. See Annex 1 in Appendix 1 for full search terms.
Studies identified
Of the 1735 records screened, we found five studies that met our inclusion criteria. These were laboratory studies which reported the presence of amyloid fibrin(ogen) particles in platelet‐poor plasma (PPP) samples from people with PCC, two of which are preprints that have not yet been validated (Laubscher 2023; Turner 2023).
Description of included studies
Pretorius 2022 was an uncontrolled study with 80 individuals who self‐identified as having PCC and had registered through an online platform; Pretorius 2021 was a study with four groups: 10 people with diabetes mellitus, 15 with acute COVID‐19, 13 healthy controls, and 11 with PCC. Kruger 2022 was a study with 29 healthy individuals and 99 individuals who self‐identified as having PCC and who had registered through an online platform. Laubscher 2023 was an uncontrolled before‐and‐after study of 91 volunteers with PCC receiving an anticoagulant regimen. Turner 2023 was controlled study comparing amyloid fibrin(ogen) particles from 40 participants with PCC and 20 healthy volunteers using flow cytometry.
Risk of bias
We assessed three domains to investigate risk of bias in the identified laboratory studies: collection and handling of samples, experimental methods, and reporting of the results. Four studies were at a high risk of bias across all domains due to factors such as inadequate description of the selection of patients and controls; lack of evidence of their history of diagnosis through PCR of SARS‐CoV‐2 infection and subsequent PCC; no statistical tests to compare values of patients and controls; and the reporting of observational results.
We judged four studies to be at overall high risk of bias (Kruger 2022; Laubscher 2023; Pretorius 2021; Pretorius 2022), and one study to have some concerns (Turner 2023).
Results
Pretorius 2021: The authors presented microscopy images of particles from one volunteer before COVID‐19, and the same volunteer with PCC. They also presented a further 12 selected microscopy images. The microscopy results of all participants are not presented in the study, and it is not stated if stained particles were observed in all samples analysed.
Pretorius 2022: The authors stated that thioflavin T stained amyloid fibrin(ogen) particles were observed in PPP samples from all 80 participants with PCC. Microscopy images of four participant samples are presented.
Kruger 2022: The authors obtained PPP samples from 29 healthy controls and 99 participants with PCC and stated that staining was performed on some of the samples. They presented a figure demonstrating the presence of stained particles in one control sample and two PCC samples. It is not reported whether these particles were observed in all samples.
Laubscher 2023: The authors stated that "significant" amyloid fibrin(ogen) particles were present in all 91 participants before treatment. Microscopy photographs for seven samples are presented.
Turner 2023: The median objects/millilitre in the control group was 7225 (interquartile range (IQR) 3320 to 24831) compared to 21,396 (IQR 11,973 to 60,745) in the PCC group. The median amyloid fibrin(ogen) particle mean area was 488 µm2 (IQR 421 to 555) in the control group and 584 µm2 (IQR 444 to 799) in the PCC group.
Analyses
We determined that it was not appropriate to perform our planned analyses due to concerns related to reporting of the results, as outlined above. We did not intend to include the preprint studies in our analysis as they are not yet validated (Laubscher 2023; Turner 2023).
Conclusion
Overall, there are issues with the reproducibility of these studies due to a considerable lack of reporting of methods for participant selection, sample collection, and experimental methods. These studies are inadequate to demonstrate the relationship between amyloid fibrin(ogen) particles and PCC. Further studies are needed to confirm or refute whether amyloid fibrin(ogen) particles are a biomarker for, or involved in any way in, PCC.
Why it is important to do this review
Despite people seeking this treatment (Cyprus Mail 2022; Madlen 2022), and some doctors and scientists recommending it, we have not been able to identify evidence rationalizing the use of plasmapheresis to remove amyloid fibrin(ogen) particles as a treatment for PCC. This treatment is not currently included in guidance for managing PCC (NICE 2022). In order for patients to make informed decisions on their health care, access to well‐conducted evidence‐based research is required. We therefore sought to summarize the evidence on the safety and efficacy of plasmapheresis to remove amyloid fibrin(ogen) particles for the treatment of PCC.
Objectives
The objective of the first part of the review was to appraise the laboratory research on amyloid fibrin(ogen) particles related to the post COVID‐19 condition. The full methods for the laboratory studies review are provided in Appendix 1, and are summarized briefly in the How the intervention might work section.
This section concerns the randomized controlled trial review, where our objective was to assess the evidence for the safety and efficacy of plasmapheresis to remove amyloid fibrin(ogen) particles in individuals with post‐COVID‐19 condition.
Methods
Criteria for considering studies for this review
Types of studies
Randomized controlled trials (RCTs) were eligible for inclusion in the review.
Types of participants
Eligible participants included any person diagnosed with post‐COVID‐19 condition (PCC) based on new and ongoing symptoms that have persisted for at least 12 weeks since an initial diagnosis with SARS‐CoV‐2 infection by reverse transcription polymerase chain reaction (RT‐PCR).
The PCC participants demonstrate levels of fatigue and impaired functioning, defined as being unable to perform usual duties/activities. This may be due to symptoms, pain, depression or anxiety, defined as grades 3 or 4 in the Post‐COVID‐19 Functional Status (PCFS) scale. A more detailed definition of PCC is described by the World Health Organization (WHO) (WHO 2021).
Types of interventions
Intervention
Plasmapheresis performed with the intention of removing amyloid fibrin(ogen) particles.
Control
Placebo or standard of care (supportive management and procedures required for specific symptoms and complications).
Types of outcome measures
We used the post‐COVID‐19 condition core outcome set (PC‐COS) recently published in The Lancet (Munblit 2022), which suggests the following outcomes.
Primary outcomes
Recovery, measured using the Post‐COVID‐19 Functional Status Scale (absence of symptoms related to the illness, ability to perform usual daily activities, and a return to a previous state of health and mind).
Secondary outcomes
Survival, measured as time until death
Respiratory functioning, symptoms and conditions, as assessed using the Medical Research Council (MRC) Dyspnoea Scale
Reduction in presence of amyloid fibrin(ogen) particles immediately after treatment and at longer‐term follow‐up
Change in symptom severity according to self‐reported COVID‐19 Yorkshire Rehabilitation Scale (C19‐YRSm)
Changes in the Chalder Fatigue Scale
Adverse effects relating to treatment (e.g. citrate toxicity, bleeding, clotting events, infection, hypovolaemia)
Cost of treatment
Since core outcome sets have only recently been published, we do not expect included studies to have incorporated these. We plan to assess any patient‐important outcomes that are reported in the included studies, as determined by clinical review authors.
Search methods for identification of studies
Electronic searches
We searched the following databases on 21 October 2022 using the search terms detailed in Appendix 2: Cochrane COVID‐19 Study Register (covid-19.cochrane.org/), MEDLINE (Ovid; 1946 to 20 October 2022), Embase (Ovid; 1947 to 2022 Week 41), and BIOSIS Previews (Web of Science; 1926 to 20 October 2022). We also searched ClinicalTrials.gov and the World Health Organization International Clinical Trials Registry Platform (WHO ICTRP) for trials in progress on 21 October 2022, using the terms shown in Appendix 2. We placed no language limits on the search. We did not expect to obtain any search results from before the start of the COVID‐19 pandemic (2019), and so applied a publication time limit from January 2000 to ensure that all eligible studies were captured.
Searching other resources
We did not formally contact experts or perform additional searches in other resources.
Data collection and analysis
We planned to utilize standard Cochrane methods for data collection and analysis as outlined in the Cochrane Handbook for Systematic Reviews of Interventions; however, no RCTs were identified for inclusion (Higgins 2022). The full intended analysis is outlined in the protocol (Fox 2023a).
Selection of studies
Two review authors (TF, RK) independently screened the titles and abstracts of the search results for potentially relevant articles using the inclusion criteria. Two review authors (TF, RK) independently reviewed the full texts of studies deemed potentially relevant during title and abstract screening for inclusion in the review, with any disagreements resolved by discussion with all review authors.
Data extraction and management
We planned that two review authors (TF, RK) would independently extract data using a standardized data extraction form. We planned to contact the study authors to obtain missing data if applicable. At each step of data extraction, we intended to resolve any discrepancies through discussion between all review authors.
We planned to extract the following information.
General information: author; title; publication date; country; date(s) of study; funding details; conflict of interest statement.
Study characteristics: study setting (inpatient or outpatient); study design; dates of recruitment; eligibility criteria; length of follow‐up; loss to follow‐up; and adherence to assigned treatment.
Participant characteristics: number of participants (recruited, allocated, and evaluated); source of participants; age; sex; disease severity; duration of symptoms associated with PCC; concurrent treatments; pregnancy; and comorbidity (e.g. diabetes, immunosuppression).
Interventions: type; frequency; duration of treatment; and duration of follow‐up.
Control: type (placebo/active treatment); frequency; duration of treatment; and duration of follow‐up.
Outcomes: data on the prespecified outcomes in both the intervention and control arms as follows: for dichotomous outcomes, number of events and participants; for continuous outcomes, mean, standard deviation (SD), and total number of participants; and for time‐to‐event outcomes, hazard ratios (HRs).
Assessment of risk of bias in included studies
We planned that two review authors (TF, RK) would independently assess risk of bias using the Cochrane risk of bias 2 tool (RoB 2) (Higgins 2022; Sterne 2019). We planned to justify judgements made in the risk of bias tables. The effect of interest was the effect of assignment to the intervention at baseline, regardless of whether the interventions were received as intended (the ‘intention‐to‐treat effect’). We intended to manage the assessments using the RoB 2 Excel tool for randomized trials and to assess risk of bias for all primary and secondary outcomes included in the analyses. We planned to use the following domains to assess bias:
bias arising from the randomization process;
bias due to deviations from intended interventions;
bias due to missing outcome data;
bias in measurement of the outcome; and
bias in selection of the reported result.
We planned to answer signalling questions outlined in the tool as yes; probably yes; probably no; no; or no information. We would then use these to determine the overall risk of bias for each domain (high, some concerns, low) and later, the overall risk of bias for the primary outcome from the included studies (high, some concerns, low). We planned to judge study outcomes as having an overall low risk of bias if all domains were at low risk; overall some concerns if any domain had some concerns; and overall high risk of bias if any domain was at high risk of bias.
Measures of treatment effect
We planned to extract data from each study and to calculate risk ratios (RRs) for dichotomous data and mean differences (MDs) for continuous data. We planned to present all statistics with the corresponding 95% confidence interval (CI).
Unit of analysis issues
The unit of analysis was the individual randomized participant. We did not encounter any unit of analysis issues.
Dealing with missing data
We planned to contact study authors to obtain missing study characteristics.
We planned to assess the risk of reporting bias due to missing studies and missing outcomes as described in the Assessment of reporting biases section.
We planned that if we were unable to obtain missing summary data, we would calculate or estimate the required data from other reported statistics using formulas specified in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2022).
We planned that if we were unable to obtain missing individual data, we would assess risk of bias using the RoB 2 tool (Higgins 2022; Sterne 2019). In the first instance, we planned to conduct a complete case‐analysis, and we could perform analyses to investigate the impact of missing data. For example, we could vary the event rate within missing individuals from intervention and control groups within plausible limits, or we could exclude studies thought to be at risk of bias from our meta‐analyses.
Assessment of heterogeneity
We planned to present results of the included studies in forest plots, which we inspected visually to assess heterogeneity (i.e. non‐overlapping CIs generally signify statistical heterogeneity). We also planned to use the Chi2 test with a P value of less than 0.1 to indicate statistical heterogeneity. We planned to quantify heterogeneity using the I2 statistic, which describes the percentage of the variability in effect estimates that is due to heterogeneity rather than to sampling error. We would interpret this statistic using the following guidance from the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2022):
0% to 40%: might not be important;
30% to 60%: may represent moderate heterogeneity;*
50% to 90%: may represent substantial heterogeneity;*
75% to 100%: considerable heterogeneity.*
*The importance of the observed value of I2 depends on (1) magnitude and direction of effects, and (2) strength of evidence for heterogeneity (e.g. P value from the Chi2 test, or a CI for I2: uncertainty in the value of I2 is substantial when the number of studies is small).
Assessment of reporting biases
We planned that if we included 10 or more studies in a meta‐analysis, we would explore the possibility of small‐study biases (a tendency for estimates of the intervention effect to be more beneficial in smaller studies) for the primary outcome using funnel plots. In the case of asymmetry, we planned to consider various explanations such as publication bias, poor study design and the effect of study size.
Data synthesis
We planned to analyse data using Review Manager Web (RevMan Web 2022).
Subgroup analysis and investigation of heterogeneity
Amyloid fibrin(ogen) particles are known to be present individuals with maturity‐onset diabetes, therefore we planned to investigate the effect of comorbidity with this disease on the results.
We also intended to subgroup participants based on the plasmapheresis technique used in their treatment, such as plasma exchange, double‐membrane‐filtration plasmapheresis (DFP), or low‐density lipoprotein adsorbent column.
Sensitivity analysis
We indicated that we may perform sensitivity analyses to investigate the impact of missing data. For example, we may vary the event rate within missing participants from intervention and control groups within plausible limits, or we may exclude studies thought to be at high risk of attrition bias from our meta‐analyses. However, due to not identifying any completed studies this was not performed.
Summary of findings and assessment of the certainty of the evidence
We planned to present the main results of the review in summary of findings tables including our rating of the certainty of evidence based on the GRADE approach. We planned to follow current GRADE guidance as recommended in the Cochrane Handbook for Systematic Reviews of Interventions (Schünemann 2022).
We planned that two review authors (TF, RK) would assess the certainty of the evidence based on the five GRADE considerations of risk of bias, inconsistency, imprecision, indirectness, and publication bias.
The summary of findings table would include the following outcomes.
Recovery, measured using the Post‐COVID‐19 Functional Status Scale (absence of symptoms related to the illness, ability to perform usual daily activities, and a return to a previous state of health and mind)
Survival, measured as time until death
Respiratory functioning, symptoms, and conditions, assessed using the Medical Research Council (MRC) Dyspnoea Scale
Reduction in presence of amyloid fibrin(ogen) particles immediately after treatment and at longer‐term follow‐up
Adverse effects (e.g. citrate toxicity, bleeding, clotting events, infection, hypovolaemia)
Change in symptom severity according to self‐reported COVID‐19 Yorkshire Rehabilitation Scale (C19‐YRSm)
Changes in the Chalder Fatigue Scale
Results
Description of studies
This results section concerns results for the review of RCTs investigating the effectiveness and safety of plasmapheresis to remove amyloid fibrin(ogen) particles for treating PCC (the results of the laboratory studies review are shown in Appendix 1).
Results of the search
We identified 95 potentially relevant studies through our search strategy. After removal of duplicates, we screened 86 records, two of which we reviewed based on full text. No completed RCTs met our inclusion criteria (Figure 1). We assessed two ongoing RCTs as awaiting classification (NCT05445674; NCT05543590), as they plan to investigate plasmapheresis for treating PCC, although they do not specify that plasmapheresis is being investigated for the removal of amyloid fibrin(ogen) particles.
1.

PRISMA flow diagram.
Given that we did not identify any RCTs, we rescreened our search results to identify any before‐and‐after studies of participants with PCC that had undergone plasmapheresis to remove amyloid fibrin(ogen) particles. Such studies would provide evidence of the safety and efficacy of the plasmapheresis; however, no studies of this design were identified.
Included studies
We included no completed RCTs in the review.
Excluded studies
We did exclude any studies at full‐text stage.
Risk of bias in included studies
We did not identify any completed studies. When studies publish data that can be included in the review, we will assess risk of bias.
Effects of interventions
We found no completed RCTs meeting our inclusion criteria.
Discussion
Summary of main results
Laboratory studies review
This Cochrane analysis first carries out a systematic review and critical appraisal of laboratory studies that investigate the presence of amyloid fibrin(ogen) particles in people with PCC. We reviewed five laboratory studies (three published, two preprints) that investigate the presence of amyloid fibrin(ogen) particles in the bloodstream of people with PCC.
Across these studies, amyloid fibrin(ogen) particles were found in healthy individuals, those with diabetes, and those with PCC. As amyloid fibrin(ogen) particles are found in non‐infectious conditions, and they are amyloid derived, this does not support that they would represent a general phenomenon caused by viral infection. Our review identified problems with the methods used to conduct these studies, as well as how the results were reported and interpreted by the study authors. We judged four studies to be at high risk of bias across all domains (collection and handling of samples, experimental methods, and reporting of results), and one study to have some concerns, concluding that these studies are unable to demonstrate whether amyloid fibrin(ogen) particles are associated with PCC, or whether there is any difference in amyloid fibrin(ogen) particles in the plasma of people with PCC compared to healthy controls.
Randomized controlled trials review
We sought trials of plasmapheresis for removing amyloid fibrin(ogen) particles to treat PCC. There are no trials evaluating plasmapheresis in this condition, and we found no studies reporting the presence of amyloid fibrin(ogen) particles before and after plasmapheresis treatment.
Overall completeness and applicability of evidence
Laboratory studies review
There is a paucity of reliable laboratory evidence on amyloid fibrin(ogen) particles and PCC, therefore we are uncertain what role they may have in PCC.
Randomized controlled trials review
We included no completed RCTs in the review. Individuals seeking plasmapheresis for the treatment of PCC should be aware that there is no evidence that amyloid fibrin(ogen) particles are causal for PCC, and that there is no evidence to support plasmapheresis as an effective treatment for removing amyloid fibrin(ogen) particles in PCC.
We identified two ongoing trials that plan to investigate the safety and efficacy of plasmapheresis for treating PCC: one trial registration suggests that plasmapheresis could be used to decrease blood levels of pro‐inflammatory cytokines or autoimmune markers, or both (NCT05543590); however, the other does not provide a rationale for undertaking plasmapheresis for PCC (NCT05445674). Whilst these trials do not plan to assess the removal of amyloid fibrin(ogen) particles and have an unclear rationale, they may be useful in assessing the safety and tolerability of plasmapheresis for people with PCC, and indeed in determining if plasmapheresis may be effective in treating symptoms of PCC by another mechanism.
Certainty of the evidence
Laboratory studies review
We did not plan to perform a GRADE assessment of the outcomes of the laboratory studies review. We assessed four studies as at high risk of bias and one as having some concerns, and we identified serious concerns relating to how the studies were conducted and how results were presented.
Randomized controlled trials review
Since no studies were identified, we could not perform a GRADE assessment.
Potential biases in the review process
We attempted to minimize bias at all stages in the review process and performed study screening, data extraction, and risk of bias assessments in duplicate. We only included studies available in the English language, therefore we may have missed studies published in other languages.
Agreements and disagreements with other studies or reviews
We are not aware of any other studies or independent reviews on this topic, further highlighting the lack of evidence in this field.
Authors' conclusions
Implications for practice.
Whilst we acknowledge that there may be other reasons for considering plasmapheresis, we conclude that there is no evidence indicating that amyloid fibrin(ogen) particles contribute to the pathophysiology of post‐COVID‐19 condition (PCC). Thus, there is no rationale for plasmapheresis to remove amyloid fibrin(ogen) particles in PCC, and a lack of data on the safety of this treatment in people with PCC. Patients should not receive plasmapheresis outside the context of a properly conducted placebo‐controlled randomized clinical trial.
Implications for research.
Further studies will help elucidate whether amyloid fibrin(ogen) particles are related to the PCC. We need to understand more about amyloid fibrin(ogen) particles in PCC and other conditions in which they occur, as well as what triggers their formation and whether they are occurring within the body or if they are a postphlebotomy event. Our review did not consider other putative mechanisms for PCC and plasmapheresis in the context of other such mechanisms. We did, however, identify two ongoing randomized controlled trials that may provide data on the safety and tolerability of this treatment for people with PCC and indicate whether plasmapheresis has any effect on alleviating the symptoms of PCC.
Acknowledgements
The Cochrane Infectious Diseases Group (CIDG) editorial base is funded by UK aid from the UK government for the benefit of low‐ and middle‐income countries (project number 300342‐104). The views expressed herein do not necessarily reflect the UK government’s official policies.
Tilly Fox and Rebecca Kuehn are supported by the Research, Evidence and Development Initiative (READ‐It). READ‐It (project number 300342‐104) is funded by UK aid from the UK government; however, the views expressed herein do not necessarily reflect the UK government’s official policies.
Editorial and peer‐reviewer contributions
The following people conducted the editorial process for this article:
Sign‐off Editors (final editorial decision): Dr Paul Hine, CIDG; Professor Lise J Estcourt, Cochrane Haematology
Managing Editor (selected peer reviewers, collated peer‐reviewer comments, provided editorial guidance to authors, edited the article): Dr Deirdre Walshe, CIDG;
Copy Editor (copy editing and production): Lisa Winer, Cochrane Central Production Service;
-
Peer reviewers (provided comments and recommended an editorial decision):
Ingeborg Welters, MD/PhD, University of Liverpool, Liverpool, UK; Professor Alan J Carson, University of Edinburgh (clinical/content review)
Mohamad Whdan (consumer review)
Marty Chaplin, Statistical Editor (CIDG) (statistical review)
Ina Monsef, Cochrane Haematology, Department I of Internal Medicine, Center for Integrated Oncology Aachen Bonn Cologne Duesseldorf, Faculty of Medicine and University Hospital Cologne, University of Cologne, Germany (search review)
Appendices
Appendix 1. Laboratory studies review
Background
Some researchers report an association between 'microclots' (tiny clots in the blood) and post‐COVID‐19 condition (PCC) (Kruger 2022; Pretorius 2021; Pretorius 2022). This is providing a rationale for people with PCC to seek anticlotting therapies, including plasmapheresis, to remove these particles.
In considering whether to conduct a Cochrane Review of randomized controlled trials of plasmapheresis as an intervention for PCC, it became clear that a thorough assessment of the laboratory evidence often cited in support of this association was required. We therefore first conducted a systematic review of the laboratory studies that investigate the presence of 'microclots' in plasma from people with PCC. This is what is reported in this Appendix.
We first appraised the term 'microclots'. It appears that the term clots or 'microclots' used throughout the laboratory studies is not an accurate definition of the blood components involved. A clot is defined as fibrin and/or platelet clumping together, and a clot within a blood vessel is known as a thrombus (ASH 2023). Blood clots have a recognised structure consisting of a mesh of crosslinked fibrin protein together with aggregated platelets and red blood cells that form a plug to seal sites of injury (Mihalko 2020). In contrast, 'microclots' are poorly characterized and are demonstrated through laboratory analysis centred on amyloid protein staining (Pretorius 2021), thus they include amyloid and either fibrinogen or fibrin (or both), and many other proteins are present in them, but they are not true thrombi.
In this review, we therefore use a more descriptive term for the blood components being reported: amyloid fibrin(ogen) particles, with each term explained below:
amyloid is misfolded, aggregating protein containing cross‐b structures that stain positive for stains such as congo red or thioflavin;
fibrinogen is a soluble clotting protein precursor that is converted to insoluble fibrin by thrombin in the activated coagulation pathway;
fibrin is the insoluble protein after thrombin cleavage of fibrinogen that polymerizes into a fibre network.
The protocol was developed by a research team that included methodologists in synthesis, specialists in the laboratory methods, and thrombosis and haemostasis specialists, and was registered on PROSPERO (Fox 2023b).
Aim
To summarize and appraise the research reports on amyloid fibrin(ogen) particles related to PCC.
Methods
Inclusion of studies
Types of studies
Laboratory studies that investigate the presence of amyloid fibrin(ogen) particles in plasma samples from patients with PCC. This includes studies without or with controls.
Types of participants
Eligible participants include any person diagnosed with PCC based on new and ongoing symptoms that have persisted for at least 12 weeks since an initial diagnosis with SARS‐CoV‐2 infection by reverse transcription polymerase chain reaction (RT‐PCR).
People with PCC demonstrate levels of fatigue and impaired functioning, defined as being unable to perform usual duties/activities. This may be due to symptoms, pain, depression or anxiety, defined as grades 3 or 4 on the Post‐COVID‐19 Functional Status (PCFS) Scale. A more detailed definition of PCC is described by the World Health Organization (WHO) (WHO 2021).
Control population
We included studies with and without controls.
In controlled studies, we expected the control participants to be either:
people who did not have COVID‐19, with sufficient antibody tests to be able to rule out infection; or
people who reported having had a positive COVID‐19 polymerase chain reaction (PCR) test, but gave a history of full recovery.
Outcomes
Types of outcome measures
Presence of aggregate particles in plasma by one of the following techniques: fluorescence imaging, laser scanning confocal imaging, fluorescent dyes for amyloid proteins, mass spectrometry analysis of protein composition, and electron microscopy.
Search strategy
We searched for all relevant laboratory studies up to 27 October 2022 using a comprehensive search strategy which included the search terms ‘COVID’, ‘amyloid’, ‘fibrin’, and ‘fibrinogen’. See Annex 1 below for full search terms.
Data collection and analyses
Selection of studies
Two review authors (TF, RK) independently screened all titles and abstracts and all potentially eligible full texts against the eligibility criteria. Any disagreements were resolved through discussion, or by consulting another review author or experienced clinician.
Data extraction and management
Two review authors (TF, RK) independently extracted all data of interest.
We extracted the following information.
General study information: first author; publication date; title; and source.
Study characteristics: study country; study design; dates of recruitment; eligibility criteria.
Participant or sample characteristics: number of participants or samples (recruited, allocated, and evaluated); source of participants or samples; age; sex; disease severity; vaccination status; comorbidity (e.g. heart disease, diabetes, respiratory disease, immunosuppression).
Laboratory methods: sample preparation techniques; description of methods used such as microscopy techniques and description of fluorescent probes, process of validation for new assays if applicable; timing of experiments; planned statistical analyses.
We planned that in the event of missing study information, we would contact the study authors.
Assessment of risk of bias of included studies
We developed a formal method of appraisal of laboratory studies. Two review authors (TF, RK) used the following tool to independently assess the risk of bias in each included study, resolving any disagreements through discussion or by consulting other review authors (PG, GJT, BJH). We appraised three domains:
collection and handling of samples;
experimental methodology;
reporting and interpretation of the results.
The questions addressed in each domain are detailed in Table 3 below.
If all questions in a given domain were answered as yes, then the overall judgement for that domain was low risk of bias. If one question was answered as no, then the overall judgement for that domain was some concerns. If more than one question was answered as no, then the overall judgement for that domain was high risk of bias.
If all the individual domains were judged as low risk of bias, then the overall judgement for the study was low risk of bias. If any domain was judged as some concerns, then the overall judgement for the study was some concerns. If any domain was judged as high concerns, then the overall judgement for the study was high risk of bias. This draws on the methods used for the Cochrane RoB 2 instrument.
Strategy for data synthesis
We planned to perform synthesis without meta‐analyis (SWiM), utilizing methods from Campbell 2020. We planned to present a summary of the methods and results in tables, and if possible synthesize results from controlled studies using vote counting based on the direction of effect, unless the risk of bias assessment deemed the studies as unreliable (Fox 2023b).
If different laboratory techniques for assessing the presence of aggregate particles in plasma were used (see 'Types of outcome measures', above), we planned to summarize the results from each technique separately.
Results
We identified 1734 potentially relevant studies through our search strategy. We also identified two preprints through our author team. After removal of duplicates, we screened 1112 records, nine of which we reviewed based on full text. Five of these studies met our inclusion criteria, all of which were conducted by one laboratory group (Figure 2).
2.
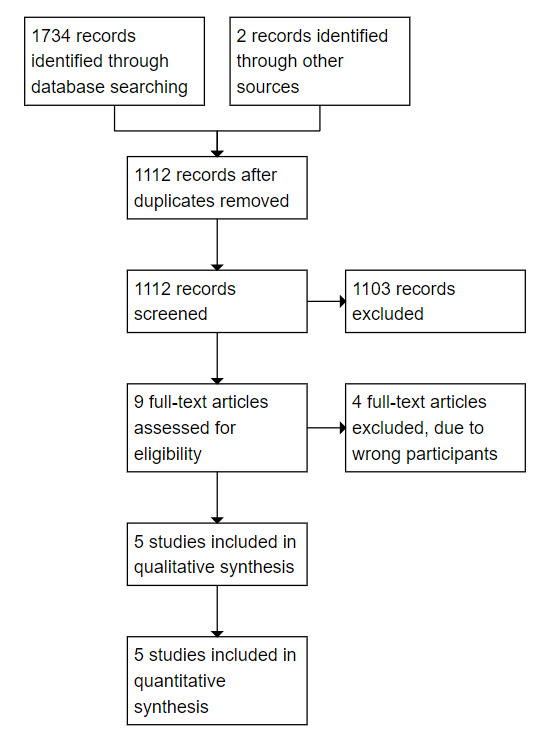
PRISMA diagram for laboratory studies review.
One study identified in the literature search examined a series of biomarkers in PCC, of which one was fibrinogen (Maamar 2022). We carefully considered whether this study met our inclusion criteria; however, we determined that it was not eligible as it did not investigate the presence of amyloid fibrin(ogen) particles and so was not informative of our research question.
Included studies
Study design
Completed studies
Pretorius 2022: an uncontrolled study investigating the presence of amyloid fibrin(ogen) particles and platelet pathology associated with persistent symptoms after recovery from acute COVID‐19.
Pretorius 2021: a controlled study investigating if the lingering symptoms manifested in individuals with PCC might be due to the presence of persistent circulating plasma amyloid fibrin(ogen) particles that are resistant to fibrinolysis.
Kruger 2022: a controlled study conducting a more extensive analysis of the contents of amyloid fibrin(ogen) particles, in which they also repeated experiments outlined in the above studies to detect the presence of these abnormal particles in individuals with PCC.
Preprint studies (non‐validated)
Laubscher 2023: a before‐and‐after study of participants with PCC receiving an anticoagulant regimen. The presence of amyloid fibrin(ogen) particles before and after treatment was measured.
Turner 2023: a controlled study comparing amyloid fibrin(ogen) particles from individuals with PCC and healthy controls using flow cytometry.
Participant groups
The history of diagnosis of SARS‐CoV‐2 infection through PCR is not reported for either the PCC or the control groups in any of the studies.
Pretorius 2022 was a report without controls in which platelet‐poor plasma samples were extracted from a subset of 80 individuals who self‐identified with PCC and registered through an online platform. The online platform was created for a study that aimed to determine the extent of symptoms that might be experienced after recovery from COVID‐19. Participants provided the date of their initial COVID‐19 diagnosis, listed the recurring long‐term symptoms after they had contracted acute COVID‐19, and stated any comorbidities; these details provided by the included participants were not reported in the study.
Pretorius 2021 was a report of four participant groups: 10 individuals with type 2 diabetes mellitus, 15 with acute COVID‐19, 13 healthy controls, and 11 with PCC. It is unclear from where the PCC group were recruited, but their inclusion criteria stated that they must have suffered from persistent PCC symptoms for at least two months after they had first developed acute COVID‐19.
Kruger 2022 included two participant groups: 29 healthy individuals, and 99 individuals who self‐identified with PCC and had registered through the same online platform used in Pretorius 2022 and detailed above.
Laubscher 2023 included 91 volunteers diagnosed with PCC. There was no control group.
Turner 2023 included 20 healthy volunteers recruited at a clinical practice, and 40 individuals who self‐identified with PCC and had registered online or who were recruited at a clinical practice.
It is unclear whether Kruger 2022, Pretorius 2021, Pretorius 2022, Laubscher 2023, and Turner 2023 contain mutually exclusive patients and samples, or whether there is some degree of overlap of samples between the reports.
Key participant characteristics are summarized in Table 1 below.
Table 1: Participant characteristics
| Study | Participant group (n) | Source of participants | History of diagnosis of SARS‐CoV‐2 infection | Inclusion criteria for post‐COVID‐19 condition participants |
| Pretorius 2022 | PCC (80) | Self‐identified participants in South Africa registered in an online registry | Not reported | Self‐reported symptoms of PCC, defined as “recurring long‐term symptoms after you have recovered from acute COVID‐19” |
| Pretorius 2021 | PCC (11) | Source unclear; possibly from self‐identified participants in South Africa registered in an online registry | Not reported | Symptoms of PCC and at least 2 months since acute COVID‐19. Unclear if self‐reported or medically diagnosed |
| Control (13) | People attending clinic prior to SARS‐CoV‐2 outbreak | N/A as prior to SARS‐CoV‐2 outbreak | ‐ | |
| Kruger 2022 | PCC (99) | Self‐identified participants in South Africa registered in an online registry | Not reported | Self‐reported symptoms of PCC, defined as “recurring long‐term symptoms after you have recovered from acute COVID‐19” |
| Control (29) | Described as "volunteers" recruited via a clinical practice | Not reported | ‐ | |
| Laubscher 2023 | PCC (91) | Described as "volunteers" recruited via a clinical practice | Not reported | Diagnosed based on symptoms and clinical examination. Methods not clearly described. |
| Turner 2023 | PCC (40) | Self‐identified participants in South Africa registered in an online registry | Not reported | Self‐reported symptoms of PCC, defined as “recurring long‐term symptoms after you have recovered from acute COVID‐19” |
| Control (20) | Described as "volunteers" recruited via a clinical practice | Not reported | ‐ | |
| Abbreviations: N/A: not applicable; PCC: post‐COVID‐19 condition | ||||
Methods
Four studies used the same laboratory methods, where platelet‐poor plasma samples were exposed to fluorescent amyloid dye, thioflavin T (ThT), for 30 min at room temperature (Kruger 2022; Laubscher 2023; Pretorius 2021; Pretorius 2022). Fluorescence microscopy was used to visualize samples, but no normal range from healthy volunteers was presented. There were no data on the reproducibility and reliability of this assay, for example the coefficient of variation for intra‐assay and inter‐assay variability (see Table 2 below).
One study used an Amnis FlowSight Imaging Flow Cytometer from Luminex (Turner 2023). For acquisition, a template was created where the 405‐ and 488‐nanometre lasers were turned on, and a gate was established to collect all ThT positive (ThT +) events by using a negative control (water and ThT), a second negative control (platelet‐poor plasma (PPP) without ThT), and a standard PPP control as reference. The brightfield images were viewed in Channel 1, and ThT‐positive events were viewed in Channel 7 using the 405 laser. All samples were acquired using the same acquisition template for 5 minutes each. Given a sample flow rate of 2.58 µL/min, the sample volume assessed during this time was 13 microlitres.
We then formally assessed each aspect in all the studies.
Table 2: Experimental methods
| Study | Experimental methods | Quantification of results | Availability of results |
| Pretorius 2022 | Fluorescence microscopy, not clearly described | No methods reported for experimental repeats. Criteria used to quantify amyloid fibrin(ogen) particles reported. No data on assay reproducibility | A combined severity score for amyloid fibrin(ogen) and platelet pathology is reported. 4 microscopy images presented. No individual results |
| Pretorius 2021 | Fluorescence microscopy, not clearly described | No methods reported for duplication of experiments or quantification of amyloid fibrin(ogen) particles. No data on assay reproducibility reported. | 14 microscopy images presented. Individual sample results not reported. |
| Kruger 2022 | Fluorescence microscopy, not clearly described | No methods reported for duplication of experiments or quantification of amyloid fibrin(ogen) particles. No data on assay reproducibility reported. | 3 microscopy images reported. Individual sample results not reported. |
| Laubscher 2023 | Fluorescence microscopy, not clearly described | No methods reported for duplication of experiments or quantification of amyloid fibrin(ogen) particles. No data on assay reproducibility reported. | 7 microscopy images reported. Individual sample results not reported. |
| Turner 2023 | Flow cytometry | Quantified by objects/mL, mean area, and amyloid fibrin(ogen) particles in area range | Median values presented for the sample set. |
Risk of bias
The full results of the risk of bias assessment are detailed in Table 3, below.
Domain 1: Collection and handling of samples
We judged four studies to be at high risk of bias for this domain (Kruger 2022; Laubscher 2023; Pretorius 2021; Pretorius 2022), and one study to have some concerns (Turner 2023).
The method of diagnosis of PCC and recruitment of participants is inadequately described across all five studies. In four studies there is no information on whether participants providing samples had been clinically evaluated to ensure that they fulfilled the criteria for PCC, and limited reporting of PCR diagnosis of initial SARS‐CoV‐2 infection (Kruger 2022; Pretorius 2021; Pretorius 2022; Turner 2023). For example, Pretorius 2022 states that 90% of people on their Long COVID/PASC registry reported a COVID‐19 PCR test, but it is not stated whether only those with evidence of testing were included in the study cohort.
Pretorius 2022 and Laubscher 2023 utilized samples collected continuously from March 2021 onwards, whilst Pretorius 2021 used samples from prior to the SARS‐CoV‐2 outbreak for their control groups. It is not clear what impact the long‐term storage of samples may have had on the results. Kruger 2022 and Turner 2023 utilized samples that had been collected within a two‐week period.
Domain 2: Experimental methods
We judged four studies to be at high risk of bias for this domain (Kruger 2022; Laubscher 2023; Pretorius 2021; Pretorius 2022). Whilst the authors of these studies reported their basic experimental methods, the staining methodology was not clearly described. With a new assay one would expect to have coefficients of variation for intra‐ and inter‐assay variability and presentation of a normal range. There was no reporting of statistical tests that would be expected to have been used to determine differences in the presence of amyloid fibrin(ogen) particles between study groups. In the studies that had more than one participant group (Kruger 2022; Pretorius 2021), the researchers were not blinded to the source of the samples. Based on this lack of reported laboratory governance, there is a high risk of bias.
The methods used in Turner 2023 are reported in detail. The authors describe a normal range obtained from control samples, and appropriate statistical tests were planned to compare values of patients with controls. However, the researchers were not blinded to the source of samples. As a result, we judged Turner 2023 to have some concerns for this domain.
Domain 3: Reporting of the results
We judged four studies to be at high risk of bias for this domain (Kruger 2022; Laubscher 2023; Pretorius 2021; Pretorius 2022). One study reported some methods for quantifying the amount of amyloid fibrin(ogen) particles detected in the PCC samples (Pretorius 2022), but this was inadequately described and only reported for a subset of participants (30 out of 80), with no reference to the missing samples. The other three studies did not report any result quantitation, which prevents any comparison of the quantity, size, or fluorescence of amyloid fibrin(ogen) particles detected in the control and PCC groups. Instead, these studies presented a subset of microscopy photographs that appear to have been specifically selected from a larger set of photographs or observations without the use of methods to prevent bias.
One study appropriately quantified the results of their investigations and presented data for all samples analysed (Turner 2023). We judged this study to be at low risk of bias for this domain.
Overall risk of bias
We assessed four studies as at overall high risk of bias (Kruger 2022; Laubscher 2023; Pretorius 2021; Pretorius 2022), and one study as overall some concerns (Turner 2023). The full risk of bias assessment is outlined in Table 3.
Table 3: Risk of bias assessment
| Study ID | Pretorius 2021 | Pretorius 2022 | Kruger 2022 | Laubscher 2023 | Turner 2023 | |
| Domain 1: Collection and handling of samples | Have patients been clinically evaluated to ensure that they fulfil the criteria for PCC? | No: source not described | No: self‐identified participants | No: self‐identified participants | No: no reference to clinical diagnostic criteria | No: self‐identified participants |
| Are samples contemporaneous? | No: samples from healthy participants and those with diabetes were obtained prior to the SARS‐CoV‐2 outbreak | No: samples collected from March 2021 onwards | Yes: samples were collected over a 2‐week period | No: samples collected from March 2021 onwards | Yes: samples were collected over a 2‐week period | |
| Have patients been matched on age, sex, or health status? | No: no statistical comparison of study groups | N/A | No: no statistical comparison of study groups | N/A | Yes | |
| Have samples from both groups been collected and prepared in the same way? | Yes: stored at −80 °C and prepared in the same way | N/A | Yes | N/A | Yes | |
| Risk of bias for domain 1 | High risk of bias | High risk of bias | High risk of bias | High risk of bias | Some concerns | |
| Domain 2: Experimental methods | Is a validated methodology used? If not, is the methodology well described? | No: the staining methodology is not well described or validated | No: the staining methodology is not well described or validated | No: the staining methodology is not well described or validated | No: the staining methodology is not well described or validated | Yes |
| Has a normal range been calculated for the control group of the study or referenced? | No | No | No | No | Yes: values for a control group with median [Q1‐Q3] are presented | |
| Has a statistical test been used to compare values of patients with controls? | No | N/A | No | N/A | Yes: data were analysed using a one‐tailed t‐test with Welch’s correction, or a one‐tailed Mann‐Whitney test | |
| Are the people evaluating the data blind to the source of the samples? | No | N/A | No | N/A | No | |
| Is an internal control used? | Yes | Yes | Yes | Yes | Yes | |
| Risk of bias for domain 2 | High risk of bias | High risk of bias | High risk of bias | High risk of bias | Some concerns | |
| Domain 3: Reporting of the results | Are the results quantified and with statistical analysis? (e.g. mean or median, range or SD) | No: results are narratively described and no statistical analysis | No: the scoring system used is not described, and individual sample data are not provided | No: results are narratively described and no statistical analysis | No: results are narratively described and no statistical analysis | Yes |
| Are all, or nearly all, data available? If a subset of data is presented in the article, is this randomly selected? | No: a subset of data is presented in photographs. Does not seem to be randomly selected | No: results are only presented for 30/80 participants | No: a subset of data is presented in photographs. Does not seem to be randomly selected | No: a subset of data is presented in photographs. Does not seem to be randomly selected | Yes: blood samples from PCC and control populations were randomly selected | |
| Are appropriate statistical tests used to test for differences? | No: no quantification of data and no statistical tests | No: uncontrolled study, so no tests for differences | No: no quantification of data and no statistical tests described | No: no quantification of data and no statistical tests described | Yes | |
| Are the data available on a data repository and available to others? | Yes: microscopic images available online but without a scale bar. Online statistics and proteomics files inaccessible | No: authors state available on request | No: not stated | No: not stated | No: not stated | |
| Risk of bias for domain 3 | High risk of bias | High risk of bias | High risk of bias | High risk of bias | Low risk of bias | |
| Overall risk of bias | High risk of bias | High risk of bias | High risk of bias | High risk of bias | Some concerns | |
| Abbreviations: N/A: not applicable; PCC: post‐COVID‐19 condition; SD: standard deviation | ||||||
Results
Three studies aimed to identify the presence of amyloid fibrin(ogen) particles in PPP as one of their study outcomes (Kruger 2022; Pretorius 2021; Pretorius 2022). Laubscher 2023 aimed to demonstrate the effect of an anticoagulation regimen on PCC symptoms and the amount of amyloid fibrin(ogen) particles present in blood samples from before and after treatment. Turner 2023 aimed to demonstrate an alternative tool for analysing amyloid fibrin(ogen) particles. There was a lack of reporting of results across most studies, which is assessed in detail in the risk of bias assessment.
Pretorius 2021: The authors present microscopy images of particles that have stained with ThT in PPP samples taken from one volunteer before COVID‐19, and the same volunteer with PCC. They also present a further 12 selected microscopy images not clearly attributable to a definite number of participants with PCC. The microscopy results of all participants are not presented in the study, and it is not stated if stained particles were observed in all samples analysed.
Pretorius 2022: The authors state that ThT‐stained amyloid fibrin(ogen) particles were observed in PPP samples from all 80 participants with PCC. Microscopy images of four participant samples are presented.
Kruger 2022: The authors obtained PPP samples from 29 healthy controls and 99 participants with PCC and stated that ThT staining to observe amyloid fibrin(ogen) particles was performed on some of the samples. They present a figure demonstrating the presence of stained particles in one control sample and two PCC samples. It is not reported whether these particles were observed in all samples.
Laubscher 2023: The authors state that "significant" amyloid fibrin(ogen) particles were present in all 91 participants before treatment. The definition of "significant" is not stated. Microscopy photographs are presented for seven samples.
Turner 2023: The authors utilized flow cytometry to measure amyloid fibrin(ogen) objects/mL, amyloid fibrin(ogen) particle mean area, and amyloid fibrin(ogen) count within four area ranges for 20 controls and 40 PCC participants. The median objects/mL was 7225 (interquartile range (IQR) 3320 to 24,831) in the control group compared to 21,396 (IQR 11,973 to 60,745) in the PCC group. The median amyloid fibrin(ogen) particle mean area was 488 µm2 (IQR 421 to 555) in the control group and 584 µm2 (IQR 444 to 799) in the PCC group.
Analysis
We determined that it was not appropriate to perform our planned analyses due to concerns related to the reporting of the results, as outlined above. Two of the controlled studies, Kruger 2022 and Pretorius 2021, did not provide sufficient evidence to determine whether the amount (quantity, size, or fluorescence) of amyloid fibrin(ogen) particles is greater in control samples or PCC samples to allow us to perform vote counting on the direction of effect (McKenzie 2022), and we determined that this would not have been appropriate due to the high risk of bias identified. We did not intend to include the preprint studies in our analysis (Laubscher 2023; Turner 2023).
Discussion
We identified problems with the laboratory studies, such that it remains uncertain whether amyloid fibrin(ogen) particles are causal of the symptoms of PCC. In particular, we were concerned in the following areas.
Research methods
The research methods are inadequately described in the majority of studies. There is no reported quality control in the study methods (coefficients of variation for intra‐ and inter‐assay variability and presentation of a normal range), the laboratory assessments made, and in the reporting of the methods. This is evident in a) the identification of the patients and controls, and the evaluation of their comparability; and b) basic laboratory procedures, with no quantification of the phenomena identified in three studies, and no quantitative assessment of differences between groups in four studies. The published literature uses a wide range of criteria for the diagnosis of PCC, which was the case in these studies, making direct comparisons between participants difficult.
The use of well‐defined and contemporaneous controls and patient samples that have been stored for the same time period and sampled in the same way the same number of times is important; for example, repeatedly freeze thawing one set of samples and not another, or storing one set of samples longer than another, can cause differences in their properties, such as changes in protein denaturation and solubility, which could confound the interpretation of results.
Interpretation
There is a large gap between the laboratory observations described and the conclusions drawn throughout the studies. For example, there is no demonstration that the amyloid fibrin(ogen) particles observed by the researchers are related to activation of the coagulation pathway, therefore the term 'microclots' is not justified. Consequently, the relationship suggested by the papers, that amyloid fibrin(ogen) particles may explain PCC as a result of poor oxygenation of tissues due to clotting in the vessels, is unproven. The changes seen, whilst interesting, may be a phenomenon that occurs within the plasma postvenesection, meaning there is no evidence that amyloid fibrin(ogen) particles are present in the blood vessels of those with PCC. Furthermore, the proposed mechanism has no other supporting clinical evidence, for as yet PCC has not been associated with increased rates of thrombosis, and exactly how such particulate matter might cause general symptoms such as fatigue, another defining symptom of PCC, is unexplained. Moreover, the authors themselves have demonstrated this particulate matter in blood taken from patients with type 2 diabetes, where most patients have a very different set of symptoms from PCC (or even no symptoms at all). It is therefore unclear how the particulate matter can be involved in aetiology in one group of patients but not another. Lastly, there are as yet no studies of amyloid fibrin(ogen) particles in animal models of disease. It will be important to establish whether amyloid fibrin(ogen) particles actually occur and cause occlusion of blood microvessels during in vivo models of disease, and whether they are either causative or sequelae of disease mechanisms.
Our risk of bias assessment highlights concerns with study design and performance of the assay without adequate laboratory governance, with observational results and a lack of appropriate statistical analysis across four studies. We conclude that further studies are necessary to confirm or refute whether amyloid fibrin(ogen) particles are a biomarker for PCC or part of the pathogenesis of PCC, or both.
Reflexivity statement
Tilly Fox is an early career researcher who has worked in a laboratory and is experienced in advanced systematic reviews including complex intervention reviews, diagnostic test reviews, and reviews of adverse effects. She is a methodologist and has no views on causality in the PCC.
Beverley J Hunt is a clinician and academic with wide expertise in managing and preventing thrombotic disorders as well as running a research laboratory investigating thrombotic disorders. She has published extensively on thrombosis in acute COVID‐19.
Robert AS Ariëns is a vascular biologist with substantial expertise in mechanisms of haemostasis and thrombosis. He has published widely on the role of fibrinogen and clot structure in mechanisms that underpin diseases related to thrombosis.
Greg J Towers is a Professor of Molecular Virology at University College London leading a team working on understanding host responses to viral infection including HIV and SARS‐CoV‐2.
Robert Lever is an Infectious Diseases Specialist Registrar working at Imperial College London NHS trust. He has a background in both clinical and basic science research and an interest in viral pathogenesis and tropical infections.
Paul Garner is a public health specialist working in evidence synthesis, having set up the Cochrane Infectious Diseases Group. He recovered from the PCC, and is forming an understanding of the evidence base around causes and recovery in postviral conditions.
Rebecca Kuehn is a clinician and researcher experienced in systematic reviews including complex intervention reviews and reviews of adverse effects. She has no involvement in the treatment of patients with PCC.
Annex 1
Based on guidance from an Information Specialist, we trialled the search both with and without including the term 'microclot'. Inclusion of the term 'microclot' yielded an exceptionally high number of results, but we determined that these studies were not relevant to our review. We found that all relevant studies were captured in our search without the use of the term 'microclot', hence it is not included in our final search strategy.
Ovid MEDLINE(R) and In‐Process, In‐Data‐Review & Other Non‐Indexed Citations <1946 to 27 October 2022>
1 (COVID* or SARS‐CoV‐2 or SARSCoV2).tw. or Coronavirus/ or Coronavirus Infections/
2 Amyloid/bl, ch or Fibrin/ch, me or Fibrinogen/ or fibrinogen.ti,ab.
3 Amyloid.mp
4 2 or 3
5 1 and 4
6 limit 5 to yr="2020 ‐Current"
Embase <1996 to 2022 Week 43>
1 (COVID* or SARS‐CoV‐2 or SARSCoV2).tw. or Coronavirus/ or Coronavirus Infections/ or *coronavirus disease 2019/
2 amyloid.ti,ab.
3 *amyloid/
4 *fibrinogen/
5 2 or 3 or 4
6 1 and 5
7 limit 6 to yr="2020 ‐Current"
BIOSIS Previews (Web of Science):
(Abstract ) COVID* or SARS‐CoV‐2 or SARSCoV2 or Coronavirus
AND
(Abstract) amyloid or fibrinogen
Appendix 2. Search strategy for main review
Ovid MEDLINE(R) and In‐Process, In‐Data‐Review & Other Non‐Indexed Citations <1946 to 20 October 2022>
1 (COVID* or SARS‐CoV‐2 or SARSCoV2).tw. or Coronavirus/ or Coronavirus Infections/ or COVID‐19/
2 amyloid*.ti,ab.
3 Amyloid/bl, ch
4 Fibrinogen.mp.
5 Fibrin/ or fibrin.mp.
6 2 or 3 or 5
7 1 and 6
8 *Blood Component Removal/
9 apheresis.ti,ab.
10 plasmapheresis.mp. or Plasmapheresis/
11 plasma exchange.mp. or Plasma Exchange/
12 8 or 9 or 10 or 11
13 7 and 12
Embase <1996 to 2022 Week 41>
1 (covid‐19 or "sars*cov*2" or severe acute respiratory syndrome coronavirus* 2).mp. or coronavirus disease 2019/
2 amyloid*.mp.
3 Fibrinogen.mp.
4 Fibrin/ or fibrin.mp.
5 2 or 3 or 4
6 1 and 5
7 apheresis/ or apheresis.mp.
8 plasmapheresis/ or plasmapheresis.mp.
9 plasma exchange/
10 7 or 8 or 9
11 6 and 10
BIOSIS Previews (Web of Science)
(Abstract ) COVID* or SARS‐CoV‐2 or SARSCoV2 or Coronavirus AND (Abstract) amyloid or fibrinogen
Cochrane COVID‐19 study register
amyloid or fibrinogen
ClinicalTrials.gov and WHO ICTRP:
(COVID* or SARS‐CoV‐2 or SARSCoV2 or Coronavirus) AND (amyloid or fibrinogen)
Characteristics of studies
Characteristics of studies awaiting classification [ordered by study ID]
NCT05445674.
| Methods | Study title: Plasma exchange therapy for post‐COVID‐19 condition: a pilot, randomized double‐blind study Study design: prospective, randomized (1:1), double‐blind, randomized placebo‐controlled trial (RCT). Study type: interventional Country: Spain Number of centres: 1 Estimated participants: 50 Date posted: 6 July 2022 Last update: 17 March 2023 Estimated completion date: July 2023 |
| Participants | Inclusion criteria:
Exclusion criteria:
|
| Interventions | Experimental arm: plasma exchanges will be performed with 5% albumin as the replacement fluid. The typical schedule prescribed will be an exchange of 1 volaemia. Blood will be separated into cells and plasma; the cells will be combined with reconstituted 5% human serum albumin and reinfused into the participant with normal saline. Plasma exchange sessions will occur on days 1, 3, 8, 10, 15, and 17. Control arm: sham plasma exchange procedures, involving a sound behind the curtain performed imitating the sound of the cell processing platform. In these cases, only 1 infusion of 200 to 250 mL of sterile saline solution 0.9% will be performed during the time established for all procedures. Sham plasma exchange sessions will occur on days 1, 3, 8, 10, 15, and 17. |
| Outcomes | Primary outcomes:
Secondary outcomes:
Quality of life questionnaires: EQ‐5D questionnaire, with 5 the better outcome and 15 the worse outcome
Quality of life questionnaires: MOS‐HIV questionnaire, with 4 the better outcome and 1 the worse outcome
The neurocognitive evaluation assessed by the NeuScreen fluency test (Seconds)
The neurocognitive evaluation assessed by questionnaire, with 0 the better outcome and 120 the worst outcome
The neurocognitive evaluation assessed by the HADS questionnaire, with 0 the better outcome and 21 the worst outcome
Changes in cellular anti‐SARS‐CoV‐2 immunity associated with PE in participants with PCC by the determination of SARS‐CoV‐2 specific igG in plasma (Arbitrary Units, AU)
Changes in cellular anti‐SARS‐CoV‐2 immunity associated with PE in participants with PCC by the analysis of reciprocal titres of neutralizing antibodies against SARS‐CoV‐2
Changes in cellular anti‐SARS‐CoV‐2 immunity associated with PE in participants with PCC by the reduction of T‐cell response (%) from plasma samples
Virological assessment to determine the residual SARS‐CoV‐2 RNA (copies/mL)
Stool assessment to determine the residual SARS‐CoV‐2 RNA (copies/mL) |
| Notes | Sponsor: Fundación FLS de Lucha Contra el Sida, las Enfermedades Infecciosas y la Promoción de la Salud y la Ciencia Collaborators: IrsiCaixa, Banc de Sang i Teixits Current status: not yet recruiting |
NCT05543590.
| Methods | Study title: Effect of plasmapheresis on clinical improvement and biological parameters of patients with long‐haul COVID: PLEXCOVIL Study, a Randomized Controlled Study Study design: open‐label, parallel‐assignment RCT Study type: interventional Country: France Number of centres: 1 Estimated participants: 60 Date posted: 16 September 2022 Last update: 16 September 2022 Estimated completion: October 2025 |
| Participants | Inclusion criteria:
Exclusion criteria:
|
| Interventions | Intervention arm: plasmapheresis involving 5 sessions of plasma exchange Control arm: no treatment |
| Outcomes | Primary outcome:
Secondary outcomes:
|
| Notes | Sponsor: Hôpital Européen Marseille Current status: not yet recruiting |
Abbreviations: FSS: fatigue severity scale; HADS: Hospital Anxiety and Depression Scale; IgG: immunoglobulin G; MOS‐HIV: Medical Outcomes Study HIV Health Survey; PCC: post‐COVID‐19 condition; PCFS: Post‐COVID‐19 Functional Status; PCR: polymerase chain reaction; PE: plasma exchange; PGIC: Patients' Global Impression of Change scale; RAT: rapid antigen test; RCT: randomized controlled trial; RNA: ribonucleic acid; RT‐PCR: reverse transcription polymerase chain reaction; SF‐36: 36‐Item Short Form Health Survey; TMA: transcription‐mediated amplification
Differences between protocol and review
The methods used in the review are consistent with the planned methods published in the protocol (Fox 2023a; Fox 2023b).
Given that we identified no randomized controlled trials, we were unable to perform the risk of bias assessment, planned analyses, or GRADE assessment, hence we have no summary of findings table. Due to the lack of randomized controlled trials, we also screened our results for controlled before‐and‐after studies which we had not planned in our methods as we felt this study design would provide the next best quality of evidence in the absence of trials. No studies of this design were identified.
Contributions of authors
Tilly Fox (TF) and Rebecca Kuehn (RK) selected studies. TF and RK extracted study data and characteristics and assessed risk of bias. All review authors contributed to the development of the review, including the risk of bias methods for assessing laboratory studies. All review authors contributed to review design and approved the final version.
Sources of support
Internal sources
Liverpool School of Tropical Medicine, UK
External sources
-
Foreign, Commonwealth and Development Office (FCDO), UK
Project number 300342‐104
Declarations of interest
TF is a Cochrane Infectious Diseases Group (CIDG) Research Associate and was not involved in the editorial process of this review. She has no known conflicts of interest to declare.
BJH is a Professor of Thrombosis and Haemostasis at King's College London, and a consultant at Guy's and St Thomas' NHS Foundation Trust. She is a trustee of Thrombosis UK, which has not expressed an opinion on this area. She has worked with BMJ/ITN News to express my interest in this area and concerns about lack of evidence, but did not express a view as to whether she was pro or con this testing.
RASA is a Professor of Vascular Biology at the University of Leeds. He has a published opinion in this area (BMJ 2022;378:o1671 http://dx.doi.org/10.1136/bmj.o1671). He has no other known conflicts of interest to declare.
GJT is a Professor of Molecular Virology at University College London. He has no conflicts of interest to declare.
RL is an Infectious Diseases Registrar at Imperial College London NHS Trust. He has no conflicts of interest to declare.
PG is Professor Emeritus in Infectious Diseases at Liverpool School of Tropical Medicine. He is a CIDG Editor, and was not involved in the editorial process of this review. He expressed the view that the theory that 'microclots' cause post‐COVID‐19 condition is unproven in one TV appearance on CNN in 2022.
RK is a CIDG Research Associate, and was not involved in the editorial process of this review. She has no known conflicts of interest to declare.
New
References
References to studies awaiting assessment
NCT05445674 {published data only}
- NCT05445674. Plasma exchange therapy for post-COVID-19 condition: a pilot, randomized double-blind study. clinicaltrials.gov/ct2/show/NCT05445674 (first received 6 July 2022).
NCT05543590 {published data only}
- NCT05543590. Effect of plasmapheresis on clinical improvement and biological parameters of patients with long-haul COVID (PLEXCOVIL) [Effect of plasmapheresis on clinical improvement and biological parameters of patients with long-haul COVID: PLEXCOVIL study, a randomized controlled study]. clinicaltrials.gov/ct2/show/NCT05543590 (first received 16 September 2022).
Additional references
Apheresis Center 2023
- Apheresis Center. Online microclots indication test. apheresiscenter.eu/microclots-test (accessed 14 February 2023).
ASH 2023
- American Society of Hematology. Blood clots. hematology.org/education/patients/blood-clots (accessed 21 February 2023).
Ballering 2022
- Ballering AV, Zon SKR, olde Hartman TC, Rosmalen J. Persistence of somatic symptoms after COVID-19 in the Netherlands: an observational cohort study. Lancet 2022;400(10350):452-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Basic‐Jukic 2005
- Basic-Jukic N, Kes P, Glavas-Boras S, Brunetta B, Bubic-Filipi L, Puretic Z. Complications of therapeutic plasma exchange: experience with 4857 treatments. Therapeutic Apheresis and Dialysis 2005;9(5):391-5. [DOI] [PubMed] [Google Scholar]
BBraun 2023
- B Braun Medical Care Agnephrology and Dialysis Centers. FAQs on H.E.L.P. apheresis. bbraun.ch/de/betroffene-und-patienten/dialyse/bmc-en/apheresis/faq-apheresis (accessed 14 February 2023).
Campbell 2020
- Campbell M, McKenzie JE, Sowden A, Vittal Katikireddi S, Brennan SE, Ellis S, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ 2020;368:el6890. [DOI] [PMC free article] [PubMed] [Google Scholar]
Castanares‐Zapatero 2022
- Castanares-Zapatero D, Chalon P, Kohn L, Dauvrin M, Detollenaere J, Maertens de Noordhout C, et al. Pathophysiology and mechanism of long COVID: a comprehensive review. Annals of Medicine 2022;54(1):1473-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
CDC 2022
- Centers for Disease Control and Prevention. Long COVID or post-COVID conditions. cdc.gov/coronavirus/2019-ncov/long-term-effects/ (accessed 9 February 2023).
Cyprus Mail 2022
- Cyprus Mail. Larnaca health centre offering Long Covid treatment. cyprus-mail.com/2022/07/15/larnaca-health-centre-offering-long-covid-treatment/ (accessed 14 February 2023).
Higgins 2022
- Higgins JPT, Savović J, Page MJ, Elbers RG, Sterne JAC. Chapter 8: Assessing risk of bias in a randomized trial. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (updated February 2022). Cochrane, 2022. Available from training.cochrane.org/handbook.
Katsoularis 2022
- Katsoularis I, Fonseca-Rodríguez O, Farrington P, Häggström Lundevaller E, Lindmark K, Fors Connolly AM. Risks of deep vein thrombosis, pulmonary embolism, and bleeding after COVID-19: nationwide self-controlled cases series and matched cohort study. BMJ 2022;377:e069590. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kruger 2022
- Kruger B, Vlok M, Turner S, Venter C, Laubscher GJ, Kell D, et al. Proteomics of fibrin amyloid microclots in long COVID/post-acute sequelae of COVID-19 (PASC) shows many entrapped pro-inflammatory molecules that may also contribute to a failed fibrinolytic system. Cardiovascular Diabetology 2022;21(1):190-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
Laubscher 2023
- Laubscher GJ, Khan MA, Venter C, Pretorius JH, Kell DB, Pretorius E. Treatment of Long COVID symptoms with triple anticoagulant therapy. Research Square 2023;1:1-23. [DOI: 10.21203/rs.3.rs-2697680/v1] [DOI] [Google Scholar]
Lemogne 2023
- Lemogne C, Gouraud C, Pitron V, Ranque B. Why the hypothesis of psychological mechanisms in long COVID is worth considering. Journal of Psychosomatic Research 2023;165:111135. [DOI] [PMC free article] [PubMed] [Google Scholar]
Maamar 2022
- Maamar M, Artime A, Pariente E, Fierro P, Ruiz Y, Gutiérrez S, et al. Post-COVID-19 syndrome, low-grade inflammation and inflammatory markers: a cross-sectional study. Current Medical Research and Opinion 2022;38(6):901-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Madlen 2022
- Madlen D. Long covid patients travel abroad for expensive and experimental “blood washing”. BMJ 2022;378:o1671. [DOI] [PubMed] [Google Scholar]
Mandal 2021
- Mandal S, Barnett J, Brill SE, Brown JS, Denneny EK, Hare SS, et al, ARC Study Group. ‘Long-COVID’: a cross-sectional study of persisting symptoms, biomarker and imaging abnormalities following hospitalisation for COVID-19. BMJ Thorax 2021;76(4):396-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
McKenzie 2022
- McKenzie JE, Brennan SE. Chapter 12: Synthesizing and presenting findings using other methods. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (updated February 2022). Available from training.cochrane.org/handbook.
Mihalko 2020
- Mihalko E, Brown AC. Clot structure and implications for bleeding and thrombosis. Seminars in Thrombosis and Hemostasis 2020;46(1):96-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
Miller 2020
- Miller A. COVID-19: not just an acute illness. Trends in Urology & Men's Health 2020;11(6):17-9. [Google Scholar]
Munblit 2022
- Munblit D, Nicholson T, Akrami A, Apfelbacher C, Chen J, De Groote W, et al. A core outcome set for post-COVID-19 condition in adults for use in clinical practice and research: an international Delphi consensus study. Lancet Respiratory Medicine 2022;10(7):715-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
NHS 2023a
- National Health Service (NHS). Post-COVID syndrome (long COVID). england.nhs.uk/coronavirus/post-covid-syndrome-long-covid/ (accessed 9 February 2023).
NHS 2023b
- NHS Neuroimmunology Centre in collaboration with the Child and Family Information Group. Plasma exchange in immune-mediated neurological conditions. gosh.nhs.uk/conditions-and-treatments/procedures-and-treatments/plasma-exchange-immune-mediated-neurological-conditions/ (accessed 13 February 2023).
NICE 2022
- National Institute for Health and Care Excellence (NICE). COVID-19 rapid guideline: managing the longterm effects of COVID-19. nice.org.uk/guidance/NG188 (accessed 14 February 2023).
Owens 2022
- Owens B. How “long covid” is shedding light on postviral syndromes. BMJ 2022;378:o2188. [DOI] [PubMed] [Google Scholar]
Pretorius 2021
- Pretorius E, Vlok M, Venter C, Bezuidenhout J, Jacobus Laubscher G, Steenkamp J, et al. Persistent clotting protein pathology in Long COVID/Post-Acute Sequelae of COVID-19 (PASC) is accompanied by increased levels of antiplasmin. Cardiovascular Diabetology 2021;20:172. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pretorius 2022
- Pretorius E, Venter C, Laubscher GJ, Kotze MJ, Oladejo SO, Watson LR, et al. Prevalence of symptoms, comorbidities, fbrin amyloid microclots and platelet pathology in individuals with Long COVID/Post-Acute Sequelae of COVID-19 (PASC). Cardiovascular Diabetology 2022;21(1):148. [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan Web 2022 [Computer program]
- Review Manager Web (RevMan Web). Version 4.12.0. The Cochrane Collaboration, 2022. Available at revman.cochrane.org.
Schünemann 2022
- Schünemann HJ, Higgins JP, Vist GE, Glasziou P, Akl EA, Skoetz N, et al. Chapter 14: Completing ‘Summary of findings’ tables and grading the certainty of the evidence. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (updated February 2022). Cochrane, 2022. Available from training.cochrane.org/handbook.
Shemin 2007
- Shemin D, Briggs D, Greenan M. Complications of therapeutic plasma exchange: a prospective study of 1,727 procedures. Journal of Clinical Apheresis 2007;22(5):270-6. [DOI] [PubMed] [Google Scholar]
Sterne 2019
- Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. [DOI] [PubMed] [Google Scholar]
Turner 2023
- Turner S, Laubscher GJ, Khan MA, Kell DB, Pretorius E. Rapid flow cytometric analysis of fibrin amyloid microclots in Long COVID. Research Square 2023. [DOI: 10.21203/rs.3.rs-2731434/v1] [DOI] [PMC free article] [PubMed]
WHO 2021
- World Health Organization. A clinical case definition of post COVID-19 condition by a Delphi consensus, 6 October 2021. who.int/publications/i/item/WHO-2019-nCoV-Post_COVID-19_condition-Clinical_case_definition-2021.1.
References to other published versions of this review
Fox 2023a
- Fox T, Hunt B, Ariens R, Towers G, Lever R, Garner P, et al. Plasmapheresis to remove amyloid fibrin(ogen) particles for treating the post-COVID-19 syndrome. crd.york.ac.uk/prospero/display_record.php?ID=CRD42023401431 (first received 20 February 2023).
Fox 2023b
- Fox T, Hunt B, Ariens R, Towers G, Lever R, Garner P, et al. Amyloid fibrin(ogen) particles and post-COVID-19 syndrome: systematic review of laboratory studies. crd.york.ac.uk/prospero/display_record.php?RecordID=402427 (first received 27 February 2023).


