Abstract
Pharyngoesophageal diverticula are a rare anatomical abnormality and are classified in 3 types based on the area of their protrusion: Zenker diverticulum is the most common, followed by Killian-Jamieson diverticulum and the rarest, Laimer diverticulum. We report a case of a 68-year-old man who presented to our clinic with a 3-year history of moderate anemia uncovered after routine blood tests, progressive dysphagia for solids and food bolus impactions resolved spontaneously. Upper endoscopy revealed a wide-mouthed diverticulum, measuring 2-3 cm, with normal mucosa and food residue inside, just below the upper esophageal sphincter, on the left side of the esophageal wall and also hiatal hernia with diffuse mucosal bleeding. Subsequent barium swallow study showed as well a 25 mm left-sided outpouching arising from the anterolateral wall of the proximal cervical esophagus, consistent with a Killian-Jamieson diverticulum. Killian-Jamieson diverticulum is a rare condition with a highly variable clinical presentation, most often reported symptoms being dysphagia, regurgitation and globus sensation.
Keywords: Killian-Jamieson diverticulum, Pharyngoesophageal diverticulum, Dysphagia, Globus pharyngeus, Food bolus impaction
Introduction
Pharyngoesophageal diverticula are a rare anatomical abnormality and are classified in 3 types based on the area of their protrusion: Zenker diverticulum (ZD) is the most common, followed by Killian-Jamieson diverticulum (KJD) and the rarest, Laimer diverticulum (LD). The ZD develops in the Killian dehiscence; therefore, it arises from the posterior wall of the pharynx, superior to the cricopharyngeus muscle [1,2]. The LD also develops posteriorly, from the Laimer-Haeckerman triangle, localized bellow the cricopharyngeus muscle [3].
The KJD was first described in a 1983 paper by Nylander and Ekberg as an anterolateral pharyngoesophageal diverticulum. It was named after the physicians Gustav Killian and James Jamieson who were the first to describe the area of anatomic weakness where it herniates, located inferior to the cricopharyngeus muscle and lateral to the longitudinal muscle of the cervical esophagus. It is 4 times less common and, in average, smaller than ZD [4], [5], [6]. KJD can be classified pathophysiologically as pulsion diverticula and by composition as false diverticula, because they contain only mucosa and submucosa [2]. According to the most recent data, KJD presents at an average age of 58, predominantly in female patients and more frequently on the left side [1,4]. The pathogenesis of KJD is still unclear, but the acquired dyscoordination of pharyngeal and esophageal muscles is considered most probable [7].
At least one-third of patients with KJD have no aerodigestive symptoms. In symptomatic patients, dysphagia, regurgitation, and globus sensation (globus pharyngeus) were most often reported. Other clinical presentations may include cough, emesis, cervical pain, hoarseness, neck mass, heartburn, halitosis, and cervical cellulitis [1,4,8].
Case presentation
A 68-year-old man presented to our clinic with a 3-year history of moderate anemia uncovered after routine blood tests, progressive dysphagia for solids and food bolus impactions resolved spontaneously. His medical history was otherwise unremarkable, with no chronic medication. He decided to seek further investigation after the dysphagia has worsened and the food bolus impactions have become more frequent. The physical examination did not reveal any abnormalities. Laboratory tests revealed the following: moderate microcytic hypochromic anemia (Hb = 8.1 g/dL, Ht = 27.1%, MCV = 67.9 fL, MCH = 20.3 pg, MCHC = 29.9 g/dL), hyposideremia (Fe = 14 µg/dL), and hypoferritinemia (20 ng/mL). The patient underwent a thorough evaluation that includes upper endoscopy, barium swallow study and colonoscopy.
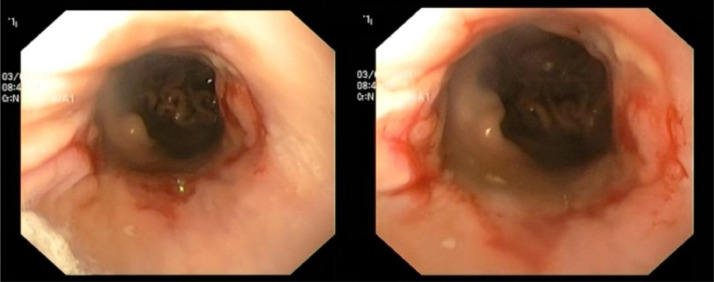
Upper endoscopy revealed a wide-mouthed diverticulum, measuring 2-3 cm, with food residue inside, just below the upper esophageal sphincter. The diverticulum's mucosa had no abnormalities (Fig. 1). At 30 cm from the incisors, a nonobstructing Schatzki ring was seen (Fig. 2). During the upper endoscopy, we also visualized a hiatal hernia with an estimated length of 4-5 cm, with diffuse mucosal bleeding (Fig. 3). No other lesions were detected.
Fig. 1.
Upper digestive endoscopy image of the Killian-Jamieson diverticulum. (A) The blue star indicates the esophageal lumen. The blue arrow indicates the diverticulum's opening; (B-D) Food residue inside the diverticulum.
Fig. 2.
Schatzki ring seen during upper endoscopy.
Fig. 3.
Hiatal hernia.
Subsequent barium swallow study also showed a 25 mm left-sided outpouching arising from the anterolateral wall of the proximal cervical esophagus, consistent with a KJD (Fig. 4) and hiatal hernia with an estimated length of 40 mm.
Fig. 4.
Barium swallow study showing a left-sided outpouching arising from the anterolateral wall of the proximal cervical esophagus. (A) Left lateral view; (B) anteroposterior view; (C) right lateral view.
The colonoscopic examination revealed only an uncomplicated sigmoid colonic diverticulum.
Both traditional transcervical diverticulectomy and endoscopic approach were presented as a possible treatment, the patient opting for the invasive procedure.
Discussion
ZD, KJD, and LD appear in the same region and have a similar clinical presentation; therefore, a comprehensive differential diagnosis is necessary.
KJD is a rare type of pharyngoesophageal diverticulum, with an incidence of only one-quarter of that of ZD. KJD tend to be left-sided, most likely due to a thinner muscle layer in that side, although there have been reports of right-sided and bilateral diverticula. Albeit very unusual, there have been cases of KJD associated with ZD, which could suggest possible interrelating pathogenesis. KJD presents at an average age of 58, predominantly in female patients. KJD have a median size of 2.1 cm (range 0.6-10 cm), with symptomatic diverticula larger (median 2.7 cm; range 1.3-10 cm) than asymptomatic ones (median 1.3; range 0.6-3.2 cm). Clinical presentations of KJD may include dysphagia (most often), regurgitation, globus sensation, cough, emesis, cervical pain, hoarseness, neck mass, odynophagia, heartburn, halitosis, and cervical cellulitis. Some pharyngoesophageal diverticula may develop malignant lesions. To this date, no KJD with malignancy has been reported. Only symptomatic patients should be offered treatment [2,4,9].
It is essential to distinguish between the 3 types of pharyngoesophageal diverticula in order to decide the proper treatment. KJD is more difficult to treat than ZD due to its extension in the upper mediastinum and proximity to the recurrent laryngeal nerve. As there are few cases cited in the literature, there is still no clear consensus on the best approach [1,4,10].
First-line treatment for pharyngoesophageal diverticula is open surgery, with procedural steps varying depending on the type of diverticulum. Diverticulectomy is preferred over diverticulopexy, because it can restore the pharyngoesophageal anatomy and eliminate the possibility of carcinogenesis in the diverticulum. Transcervical diverticulectomy/diverticulopexy offers better visibility and more space for maneuver, but it also has clear disadvantages like visible surgical scar, longer hospitalization, and delayed oral intake for a period of up to 5 days postoperatively [10], [11], [12].
In recent years, the interest for minimally invasive procedures has risen owing to a series of advantages like absence of external scar, short operative time, minimal blood loss, and faster return to oral intake. The endoscopic approach for KJD used to be avoided due to concern for recurrent laryngeal nerve injury and mediastinitis. In recent literature, varied endoscopic techniques for KJD diverticulotomy are described. For example, Yun et al. preferred endoscopic stapling, Chang et al. safely performed a rigid endoscopic CO2 laser diverticulotomy, and Yang and Draganov used a scissor-type electrosurgical knife [7,13,14]. Modayil et al. [1] described in their study 2 methods of successful endoscopic treatment, direct and tunneling diverticulotomy (with hypopharyngeal tunnel or ultra-short septal tunnel). Tunneling diverticulotomy with an ultra-short tunnel was their preferred method, because it allows complete myotomy without fear of mediastinal leak and minimal risk of recurrent laryngeal nerve injury [1]. Therefore, endoscopic treatment can be an attractive alternative to surgical excision, but these techniques should be performed only in experienced centers.
Conclusions
KJD is a rare condition with a highly variable clinical presentation, with most often reported symptoms being dysphagia, regurgitation and globus sensation.
While open surgery remains the standard of care for symptomatic KJD, endoscopic intervention can be a safe alternative.
Author contributions
Literature research: all authors; writing—original draft preparation: S.Z. and I.C.; writing—review and editing: S.Z. and I.C.; supervision: I.C. All authors have read and agreed to the published version of the manuscript.
Patient consent
Written informed consent has been obtained from the patient to publish this paper.
Footnotes
Acknowledgments: No external funding.
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Modayil R.J., Zhang X., Ali M., Das K., Gurram K., Stavropoulos S.N. Endoscopic diverticulotomy for Killian-Jamieson diverticulum: mid-term outcome and description of an ultra-short tunnel technique. Endosc Int Open. 2022;10(1):E119–E126. doi: 10.1055/a-1548-5552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stewart K.E., Smith D., Woolley S.L. Simultaneously occurring Zenker's diverticulum and Killian-Jamieson diverticulum: case report and literature review. J Laryngol Otol. 2017;131(8):661–666. doi: 10.1017/S0022215117001268. [DOI] [PubMed] [Google Scholar]
- 3.Ujiie N., Taniyama Y., Sato C., Kamei T. Surgical intervention for Laimer's diverticulum, a rare type of pharyngoesophageal diverticulum: a case report. OTO Open. 2019;3(2) doi: 10.1177/2473974X19847670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haddad N., Agarwal P., Levi J.R., Tracy J.C., Tracy L.F. Presentation and management of Killian-Jamieson diverticulum: a comprehensive literature review. Ann Otol Rhinol Laryngol. 2020;129(4):394–400. doi: 10.1177/0003489419887403. [DOI] [PubMed] [Google Scholar]
- 5.Undavia S., Anand S.M., Jacobson A.S. Killian-Jamieson diverticulum: a case for open transcervical excision. Laryngoscope. 2013;123(2):414–417. doi: 10.1002/lary.23639. [DOI] [PubMed] [Google Scholar]
- 6.Ekberg O., Nylander G. Lateral diverticula from the pharyngo-esophageal junction area. Radiology. 1983;146(1):117–122. doi: 10.1148/radiology.146.1.6401363. [DOI] [PubMed] [Google Scholar]
- 7.Yun P.J., Huang H.K., Chang H., Lee S.C., Huang T.W. Endoscopic diverticulotomy with a stapler can be an effective and safe treatment for Killian-Jamieson diverticulum. J Thorac Dis. 2017;9(9):E787–E791. doi: 10.21037/jtd.2017.08.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kitazawa M., Koide N., Saito H., Kamimura S., Uehara T., Miyagawa S. Killian-Jamieson diverticulitis with cervical cellulitis: report of a case. Surg Today. 2010;40(3):257–261. doi: 10.1007/s00595-009-4048-z. [DOI] [PubMed] [Google Scholar]
- 9.Alnimer L., Zakaria A., Piper M. Killian-Jamieson diverticulum: a rare cause of dysphagia. Cureus. 2021;13(3):e13654. doi: 10.7759/cureus.13654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kurahashi Y., Hojo Y., Nakamura T., Kumamoto T., Nakanishi Y., Ishida Y., et al. Endoscopic observation of the palisade vessels in Killian-Jamieson diverticulum was useful for diagnosis and surgical treatment: a case report. Surg Case Rep. 2020;6(1):192. doi: 10.1186/s40792-020-00949-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ataka R., Tsunoda S., Goto S., Nishigori T, Hisamori S, Obama K, et al. Killian-Jamieson diverticulum safely resected using a manual intraoperative neural monitoring system: a case report. Surg Case Rep. 2020;6:43. doi: 10.1186/s40792-020-00805-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saisho K., Matono S., Tanaka T., Mori N, Hino H, Fujisaki M, et al. Surgery for Killian-Jamieson diverticulum: a report of two cases. Surg Case Rep. 2020;6:17. doi: 10.1186/s40792-020-0789-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chang Y.C., Chi C.Y., Lee C.J. Rigid endoscopic LASER diverticulotomy for lateral pharyngoesophageal diverticuli: cases presentation and discussion. Eur Arch Otorhinolaryngol. 2016;273(12):4637–4642. doi: 10.1007/s00405-016-4080-8. [DOI] [PubMed] [Google Scholar]
- 14.Yang D., Draganov P.V. Endoscopic Killian-Jamieson diverticulotomy using a scissor-type electrosurgical knife. Endoscopy. 2018;50(7):E175–E176. doi: 10.1055/a-0601-6467. [DOI] [PubMed] [Google Scholar]