Highlights
-
•
Vulvar leiomyosarcoma is a rare malignant smooth muscle tumor.
-
•
Vulvar leiomyosarcoma may be easily mistaken for a benign mass, making necessary a pre-surgical biopsy of any suspicious mass.
-
•
We present the first case of vulvar leiomyosarcoma reported in Haiti.
-
•
We highlight barriers to safe delivery of cancer care in Haiti. It is critical to develop the pathologic and gynecologic oncology capacity in the developing world.
Keywords: Vulvar leiomyosarcoma, Sarcoma, Vulvar cancer, Vulvar mass
Abstract
Vulvar leiomyosarcoma is a rare malignant smooth muscle tumor and the most common type of vulvar sarcoma. It can mimic benign tumors, and misdiagnosis may delay appropriate treatment. A 35-year-old woman presented to the outpatient gynecology clinic at the Mirebalais Teaching Hospital for a right vulvar mass. A complete excision of the mass was performed. Histopathology with immunohistochemistry demonstrated leiomyosarcoma. We describe the contextual challenges that ultimately compromised her care, highlighting the challenges to safe delivery of cancer care in our setting.
1. Introduction
Primary vulvar sarcomas are tumors of mesenchymal origin. They are very rare and represent approximately 1 to 3 % of malignant vulvar tumors (Tjalma and Colpaert, 2005). Of the primary vulvar sarcomas, leiomyosarcoma is the most common histological type. It is a smooth muscle tumor commonly found in the abdomen, retroperitoneum, large blood vessels and uterus (George et al., 2018).
Vulvar leiomyosarcoma can be misdiagnosed as a benign vulvar lesion such as a Bartholin's cyst (Reinicke et al., 2022). Clinical differentiation of benign and malignant forms of vulvar smooth muscle tumor is a major diagnostic challenge, as many vulvar lesions have similar appearances, physical findings and gross features at surgery (Reyad et al., 2006). This similarity can lead to a delay in treatment or loss to follow up, thus worsening the patient's prognosis.
The definitive diagnosis of vulvar leiomyosarcoma requires pathological examination (Korkmaz et al., 2016). The 2020 World Health Organization (WHO) classification of female genital tumors indicates that, in the context of a smooth muscle neoplasm, the presence of moderate to severe atypia, elevated mitotic count, and/or necrosis warrants designation as leiomyosarcoma; these criteria are similar to the lesion’s uterine counterparts.
Given the rarity of vulvar leiomyosarcomas, an optimal therapeutic algorithm is not established. The main treatment of choice is surgery with wide excision or radical hemi vulvectomy (Korkmaz et al., 2016). This case aims to contribute to the literature on vulvar leiomyosarcoma and to describe its diagnosis and management in a low-resource context; in our case, it was initially mistaken for a fibroma of the labia majora.
2. Case report
A 35-year-old patient, G3P3, came to the outpatient gynecology clinic at the Mirebalais Teaching Hospital, Haiti for a vulvar mass that had been palpable for 1 year. She had no significant past medical, surgical, or family history. Her gynecological history was unremarkable; she gave birth to three children vaginally in a hospital environment. She did not use alcohol, tobacco or illicit drugs. On physical examination, her vital signs were within normal limits, and cardiopulmonary and abdominal evaluation were unremarkable. Gynecological examination revealed a painless, non-infiltrating, multi-lobed, irregularly contoured, firm and mobile mass of approximately 9 cm in its longest axis at the level of the right vulva in the region of the Bartholin gland. The mass was covered with intact skin. (Fig. 1A, Fig. 1B). No lymph nodes were palpated in the inguinal regions and in the other lymph node areas. Vaginal examination and ultrasound of the pelvic organs were unremarkable.
Fig. 1A.
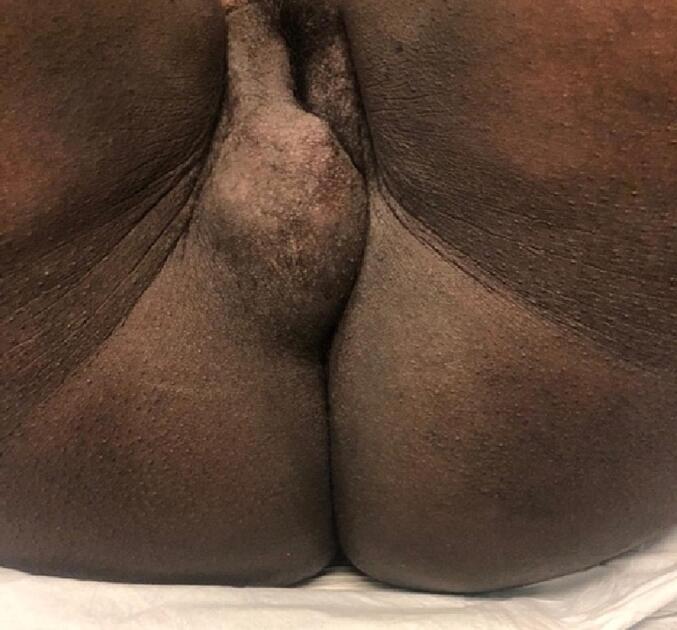
Mass before intervention.
Fig. 1B.
Mass before intervention.
After evaluation, the initial clinical impression was a fibroma of the right labia majora. Routine testing (including complete blood count, and HIV and Syphilis serology) were within normal limits. Given the clinical impression and the lack of pathology capacity available locally in Haiti, a biopsy of the mass was not performed, and it was excised two days later under local anesthesia. An incision was made on the inner face of the labia majora at the level of Hart's line reaching the wall of the mass. Given the intraoperative macroscopic appearance of the mass (Fig. 2A), the team retained the initial clinical impression of a benign fibroma and proceeded with enucleation and complete excision of the mass with minimal blood loss (Fig. 2B). The excess skin was resected and the wound sutured (Fig. 2C). The surgical specimen was sent to the Pathology department for histologic diagnosis.
Fig. 2A.

Perioperative resection of mass.
Fig. 2B.

Mass after resection.
Fig. 2C.
Immediate post-op vulva.
The patient was seen again two months later for follow-up, but at that time the pathological results were not yet available. She presented with a healed vulvar wound, and with no evidence of recurrence of the mass (Fig. 3). Three months after the surgery, our pathology department was able to process the specimen, and, with international support via telepathology, the diagnosis of leiomyosarcoma was reached (Fig. 4A, Fig. 4B, Fig. 4C, Fig. 4D, Fig. 4E).
Fig. 3.
Vulva at 2 months post-Op.
Fig. 4A.
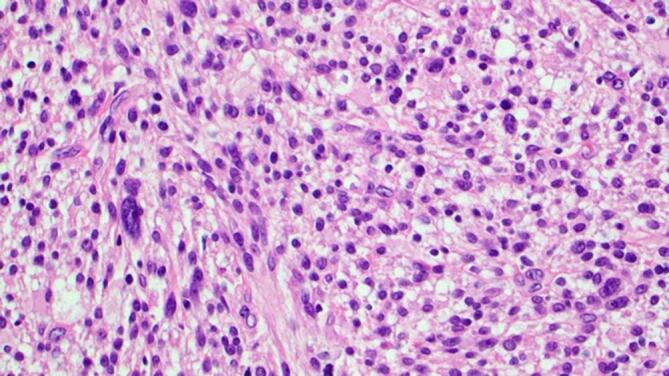
Cellular neoplasm composed of spindle cells with hyperchromatic, irregular and pleomorphic nuclei.
Fig. 4B.
Nuclear atypia is evident, in the form of pleomorphism and coarse chromatin distribution.
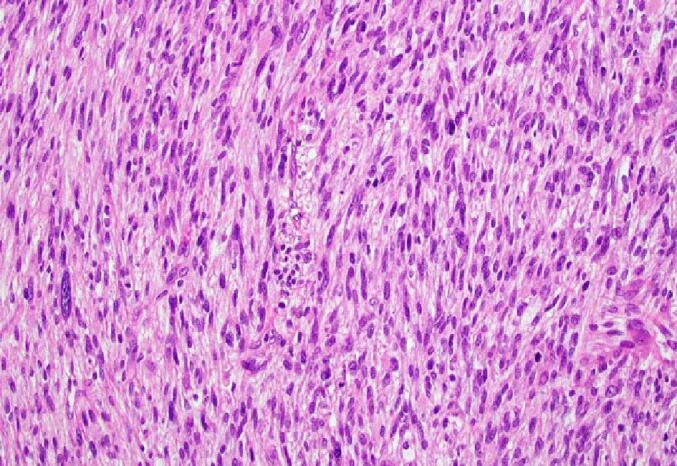
Fig. 4C.
Numerous mitotic figures are identified.
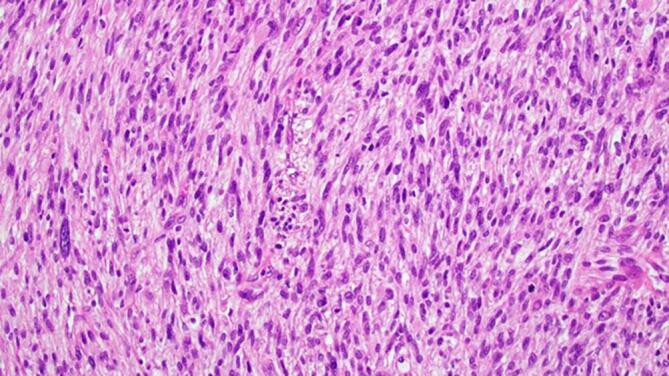
Fig. 4D.
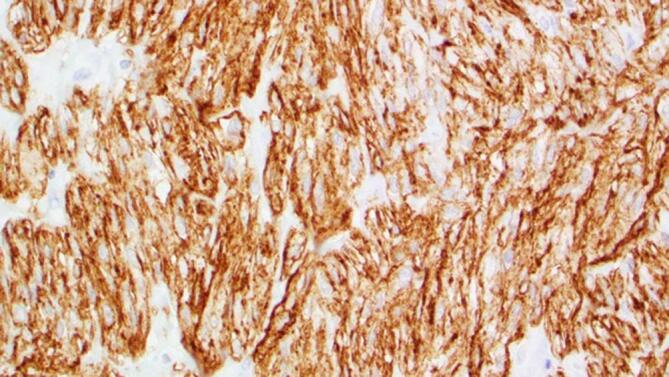
Tumor cells are strongly positive for caldesmin.
Fig. 4E.
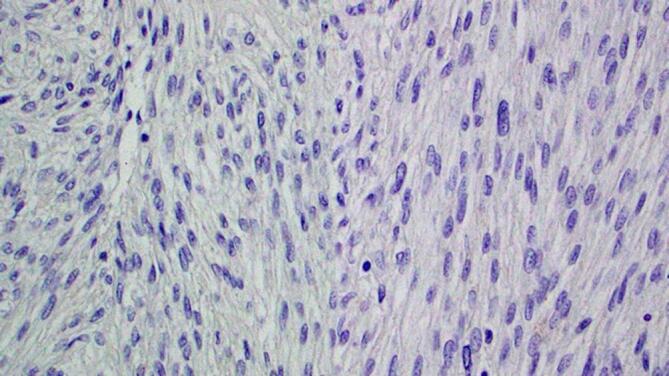
Tumor cells are negative for epithelial membrane antigen (EMA).
As no attempt had been made at the initial procedure to achieve negative surgical margins, our plan was to recommend that the patient return for re-evaluation with careful examination, imaging, and a second surgery to perform a radical local excision of the surgical site. Despite multiple attempts, however, we were unable to make contact with the patient to advise her to return for follow-up.
3. Discussion
Our patient presented with painless, enlarging vulvar mass. While its clinical characteristics suggested a more commonly encountered fibroma of the labia majora, the lesion was ultimately diagnosed as a vulvar leiomyosarcoma. To our knowledge, this is the only case of vulvar leiomyosarcoma ever recorded in Haiti, which may speak both to the rarity of the diagnosis and the difficulty to obtain timely and accurate pathological diagnosis in a low resource context.
According to the World Health Organization (WHO) 2020 classification of tumors of the female reproductive organs, three main elements are evaluated to determine the type of tumor of the smooth muscles of the uterus: the mitotic index, tumor cell necrosis and the extent of cellular atypia. Site-specific criteria for vulvar smooth muscle neoplasms, first outlined by (Tavassoli and Norris, 1979) are also useful to identify cases with malignant potential; these criteria include necrosis, cytologic atypia, mitotic index > 5 mitoses per 10 HPFs, tumor size > 5 cm and infiltrative growth. Our case had four of these site-specific criteria for leiomyosarcoma: atypia, necrosis, mitotic count and tumor size (Fig. 3). Immunohistochemical studies demonstrated that the tumoral cells were strongly positive for caldesmin and were negative for EMA (Fig. 3).
Because benign soft tissue masses are at least 100 times more common than malignant soft tissue sarcomas, it can be difficult to determine which soft tissue masses warrant further evaluation (WHO Classification of tumors, 2020). This challenge is especially acute in settings, like Haiti, where resources are limited. The United Kingdom Department of Health has published the following criteria for urgent referral of a soft tissue mass: >5 cm in size, painful, gradually increasing in size, any sized mass located in depth in the muscle fascia, or recurrence of the mass after resection (Sinha and Peach, 2010).
A core needle biopsy might have allowed our team to diagnose the leiomyosarcoma, and better plan the resection of the lesion. Surgery is the mainstay of treatment for vulvar leiomyosarcoma, but due to its rarity, evidence-based treatment algorithms are not available (Chokoevaa et al, 2015). The treatment of choice for leiomyosarcomas is complete and wide local excision with the aim of pathologically confirming negative margins of 1–2 cm of normal tissue, which prevents local and distant metastases (Teramae et al, 2014). In this case, the lack of a pre-operative biopsy diagnosis prevented us from planning a more appropriate initial surgery. By the time pathological results were obtained, the patient was lost to follow up, though the team continues to search for this patient to ensure adequate follow-up. We would therefore recommend resection with a clear margin for the management of such cases if preoperative biopsy diagnosis is unavailable.
The long delay of a pathology diagnosis, due to a lack of medical resources locally and nationally, caused us to miss an opportunity to recommend a second surgery. At the time of writing, we believe there were fewer than five pathologists working in Haiti, a nation of almost 12 million. In addition, it is likely that the ongoing insecurity in Haiti, pre-existing poverty, social displacement, and severe limits of infrastructure further exacerbated the challenge of contacting the patient later and delivering recommended care.
This highlights the need to build pathology capacity in a low resource environment, and to also build a social and medical infrastructure that facilitates patient access to both their medical information and medical care. We see this as an example of our moral obligation to continue to build the skills, structures and systems to deliver safe high quality cancer care to the most vulnerable around the world.
4. Conclusion
Due to their clinical overlap with a number of benign conditions, vulvar leiomyosarcomas are often misdiagnosed before biopsy. The diagnosis can be anticipated based on a combination of clinical signs but histopathology and immunohistochemistry are needed to definitively make the diagnosis. The lack of diagnostic resources, and especially the lack of timely histopathology results, make management of vulvar leiomyosarcomas and other rare tumors especially challenging in low-resource environments such as Haiti. Any vulvar lesion with unusual features or insidious evolution in the region of the labia majora or Bartholin's glands should be carefully evaluated, and every effort should be made to do this in a timely fashion, especially in a low resource setting.
5. Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
CRediT authorship contribution statement
Bernard Gilles: Writing – original draft, Conceptualization. Christophe Millien: Validation, Writing – review & editing, Supervision. Giovanni A. Bordes: . Rebecca R. Henderson: Writing – review & editing. Carlos E. Parra-Herran: Writing – review & editing. Thomas C. Randall: Writing – review & editing, Validation.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Chokoevaa, A.A., Tchernev, G., Cardoso, J.C., et al., 2015. Vulvar sarcomas: short guideline for histopathological recognition and clinical management. Part 1. Int. J. Immunopathol. Pharmacol. 28, 168-177. [DOI] [PubMed]
- George, S., Serrano, C., Hensley, M.L., Ray-Coquard, I., 2018. Soft tissue and uterine leiomyosarcoma. J. Clin. On-col. 36, 144-50. 10.1200/JCO.2017.75.9845. [DOI] [PMC free article] [PubMed]
- Korkmaz, V., Kurdoğlu, Z., Kardag, B., Arslanca, T., Caydere, M., Ergun, Y., 2016. A rare case of leiomyosarcoma localized in the Bartholin's gland area and review of the literature. J. Obstet. Gynaecol. Res. 42, 589-592. doi: 10.1111/jog.12943. [DOI] [PubMed]
- Reinicke, T., Anderson, D.J., Kumar, D., et al. Vulvar Leiomyosarcoma Masquerading as a Bartholin’s Gland Cyst in an Adolescent. Cureus; 14(1): e21674. doi: 10.7759/cureus.21674. [DOI] [PMC free article] [PubMed]
- Reyad, M.M., Gazvani, M.R., Khine, M.M., 2006. A rare case of primary leiomyoma of the vulva. J. Obstet. Gynecol.: J Inst.Obstet>Gynaecol., 26 (1), 73-74. doi:10.1080/01443610500419451. [DOI] [PubMed]
- Sinha, S., Peach, A.h., 2010. Diagnosis and management of soft tissue sarcoma. BMJ, 341, c7170. [DOI] [PubMed]
- Tavassoli, F.A., Norris, H.J., 1979. Smooth muscle tumors of the vulva. Obstet Gynecol. 1979 Feb;53(2):213-7. PMID: 418977. [PubMed]
- Teramae, M., Fukuda, T., Imai, K., et al., 2014. Leiomyosarcoma of the vulva: a case report. Int. J. Reprod. Contracept. Obstet. Gynecol., 225-228.
- Tjalma, W.A., Colpaert, C.G., 2005. Myxoid leiomyosarcoma of the vulva. Gynecol. Oncol, 96, 548–551. [DOI] [PubMed]
- WHO Classification of Tumors Editorial Board: WHO Classification of tumors, 5th Edition, Volume 4: Female Genital Tumors. International Agency for Research on Cancer, Lyon; 2020.





