Abstract
Arthritis of the first metatarsophalangeal (MTP) joint, hallux rigid, is a common and disabling source of foot pain in the adult population. Hallux rigidus is characterized by diseased cartilage and large, periarticular osteophytes that result in a stiff, painful joint. Activity modification, sensible shoes, orthotics, anti-inflammatory medications and occasional intra-articular steroid injections can be attempted to alleviate the discomfort associated with hallux rigidus. A number of surgical options exist for the treatment of recalcitrant hallux rigidus. Cheilectomy is a useful treatment for dorsal impingement pain seen in mild hallux rigidus. A new polyvinyl alcohol hemi-arthroplasty implant has shown promising early and midterm results in the treatment of advanced hallux rigidus; however, arthrodesis of the first MTP joint remains the gold standard treatment for advanced hallux rigidus because of unpredictable outcomes after early-generation joint replacement implants.
Keywords: forefoot disorders, hallux rigidus
Commentary: This excellent review paper examines the evidence supporting nonoperative and operative treatment methods for the very common condition of first metatarsaophalangeal arthritis. The authors present a balanced and objective evaluation and share their preferred treatment algorithm.
Introduction
The first metatarsophalangeal (MTP) joint is the most common arthritic site in the foot. 73 Also known as hallux rigidus, arthritis of the first MTP joint is characterized by decreased motion, pain, and osteophyte formation. Nearly 10% of adults have symptomatic hallux rigidus; however, radiographic evidence of arthritic change at the first MTP joint is present in 20% to 48% of adults older than 40 years.62,75 Symptomatic hallux rigidus can be quite debilitating and has been associated with lower scores on the SF-36 physical and social subscales.6,62
Hallux rigidus is a progressive condition that leads to osseous and soft tissue changes and resultant stiffness, inflammation, and pain. 67 The treatment of symptomatic hallux rigidus begins with nonsurgical intervention. Nonsteroidal anti-inflammatory drugs (NSAIDs), intra-articular steroid injections, orthotics, and shoe modifications designed to limit MTP joint motion can all be used. 30 Osteophyte removal and joint debridement (cheilectomy) can be used to treat mild hallux rigidus when symptoms are primarily driven by dorsal impingement. 15 A dorsal closing wedge osteotomy (Moberg) can be performed at the proximal phalanx to further improve dorsiflexion of the first MTP joint. 56 Joint-sacrificing procedures are used in more severe arthritis and can be divided into motion-sacrificing and motion-sparing techniques. Arthrodesis of the first MTP joint sacrifices motion but results in excellent pain relief. 26 Historically first MTP arthrodesis has been the gold standard treatment of severe arthritis given the inconsistent outcomes of motion-sparing procedures for severe hallux rigidus. Joint replacement surgeries initially demonstrated early pain relief; however, long-term follow-up revealed instability, malalignment, bone erosion, recurrent pain, and decreased range of motion.45,61,70,72 Interpositional arthroplasties have shown good pain relief, and the Food and Drug Administration (FDA) recently approved a novel polyvinyl alcohol (PVA) hydrogel implant (Cartiva Inc, Alpharetta, GA) which has demonstrated excellent pain relief and function at 2 and 5 year follow-up.3,17
Pathophysiology
Arthritis of the first MTP joint is idiopathic in the majority of cases and the underlying cause of hallux rigidus is likely multifactorial. Hallux rigidus is frequently bilateral, and up to two-thirds of patients have a family history of hallux rigidus. 14 Despite the idiopathic nature of hallux rigidus, multiple authors have noted an association between the development of arthritis and damage to the articular cartilage via both traumatic and iatrogenic causes.14,18 Furthermore, hallux valgus, metatarsus adductus and metatarsal head morphology have all been implicated in the development of hallux rigidus.14,15,18 Achilles contracture, shoe wear, and an elevated metatarsal head do not appear to contribute to the development of arthritis at the first MTP joint. 14
Hallux rigidus results in kinematic changes at the first MTP joint. The proximal phalanx glides eccentrically on the metatarsal head as a result of uncoupling of the normal center of rotation of the first MTP joint. 66 Dorsiflexion is restricted because of the preferential formation of dorsal periarticular osteophytes. 35
Clinical Evaluation
Patients with symptomatic hallux rigidus present with pain and stiffness at the first MTP joint. During typical walking, the symptoms are most severe at terminal heel-rise just before toe-off as a result of periarticular osteophyte formation and the resultant impingement. Activities such as stairs, running, and pushups that require increased dorsiflexion of the first MTP joint may be unbearable for patients with hallux rigidus. 35 Often localized swelling and a limp will be present. Dorsal osteophyte formation may lead to mechanical impingement with shoe wear or occasionally a compression neuritis of the dorsal digital nerve as it passes over the osseous prominence. 42 Frequently patients will note lateral border foot pain because of altered weight-bearing as they attempt to offload the great toe.
Clinical examination typically reveals large, tender osteophytes at the first MTP joint. Localized swelling and erythema are often present and first MTP joint motion will be significantly decreased in patients with hallux rigidus. 66 In patients with unilateral hallux rigidus, the difference in motion between feet can be striking. Patients often report pain at the extremes of dorsiflexion because of impinging dorsal osteophytes. Pain with plantarflexion may result from traction of the EHL over the osteophytes. 36 Axial load of the first MTP joint during the midrange of motion may indicate central cartilage loss and signal more advanced arthritis. Hyperextension at the interphalangeal joint of the hallux may develop to compensate for decreased dorsiflexion of the first MTP joint. Occasionally, Tinel testing of the dorsal digital nerve may elicit neuritic symptoms.
Radiographic evaluation of hallux rigidus consists of standard standing anteroposterior AP, oblique, and lateral foot radiographs. Joint space narrowing, subchondral sclerosis, and flattening and widening of the metatarsal head will be seen on the AP view. The lateral view typically demonstrates periarticular dorsal osteophytes both proximally and distally at the joint and may also show narrowing of the joint space. Hattrup and Johnson classified hallux rigidus into 3 different grades as based on radiographic changes at the joint (Table 1). 34 Coughlin and Shurnas introduced the most frequently adopted classification system for hallux rigidus (Table 2). 14 Their system takes both clinical and radiographic factors into account although the correlation between this classification and intraoperative findings has recently been called into question. 2 Advanced imaging may be indicated when focal osteochondral pathology is suspected but plays no role in the evaluation of typical hallux rigidus.
Table 1.
Hattrup and Johnson Radiographic Classification of Hallux Rigidus.
| Grade | Radiographic Findings |
|---|---|
| I | Mild to moderate osteophyte formation, preservation of joint space |
| II | Moderate osteophyte formation, joint space narrowing, subchondral sclerosis |
| III | Marked osteophyte formation, severe loss of joint space, subchondral cyst formation |
Table 2.
Coughlin and Shurnas Classification of Hallux Rigidus.
| Grade | Dorsiflexion | Radiographic Findings a | Clinical Findings |
|---|---|---|---|
| 0 | 40°-60° (20% loss of normal motion) | Normal | No pain. Only stiffness and loss of motion |
| 1 | 30°-40° (20%-60% loss of normal motion) | Dorsal osteophyte. Minimal joint space narrowing, periarticular sclerosis and flattening of the metatarsal head | Mild or occasional pain and stiffness at the extremes of movements |
| 2 | 10°-30° (50%-75% loss of normal motion) | Dorsal, lateral, possibly medial osteophytes with flattened appearance to the metatarsal head; less than one-fourth of the dorsal joint space is involved on the lateral radiograph; mild to moderate joint space narrowing and sclerosis; sesamoids not involved | Moderate to severe pain and stiffness. Pain occurs just before maximum dorsiflexion and maximum plantarflexion |
| 3 | ≤10° (75%-100% loss of normal motion). Loss of plantarflexion as well (often ≤10°) | Same as in grade 2 but with substantial narrowing, cystic changes, more than one-fourth of the dorsal joint space is involved on the lateral radiograph, sesamoids enlarged, cystic, and/or irregular | Constant pain and substantial stiffness at the extremes of range of motion but not at midrange |
| 4 | Same as in grade 3 | Same as in grade 3 | Same as in grade 3 but with hindrance of passive motion |
Weight-bearing anteroposterior and lateral.
Source: Adapted from Coughlin MJ, Shurnas PS. Hallux rigidus: grading and long-term results of operative treatment. J Bone Joint Surg Am 2003;85(11):2073.
Nonoperative Management
A 55% success rate with conservative management for symptomatic hallux rigidus patients was reported in a retrospective review of 772 patients, and these measures remain the first line of treatment in the majority of cases. 30
NSAIDs may alleviate acute pain and swelling; however, caution is advised for long-term use given their potential cardiac and renal side effects. Avoidance of activities that place the joint in a position of dorsiflexion should be encouraged. This includes running, jumping, and traveling upstairs. Recommended shoes incorporate a high and wide toe box to decrease contact pressure on dorsal osteophytes and have a stiff sole to decrease motion across the first MTP joint. Additionally, a rocker sole shoe will further decrease motion across the joint by allowing the foot to roll through the stance phase of gait (Figure 1).
Figure 1.

(A) A shoe with a rocker sole. (B) A carbon footplate. Both the rocker sole shoe and carbon footplate are designed to decrease motion with ambulation across the first MTP joint.
When shoe changes fail to provide adequate relief, orthotics can be utilized. A carbon footplate serves to stiffen the sole and decrease motion across the first MTP joint (Figure 1). A Morton’s extension only stiffens the great toe, which may be better tolerated by younger or more active patients. Carbon fiber inserts are paired with overlying insoles to cushion the foot. Although carbon footplates decrease motion across the first MTP joint, they may be poorly tolerated by some patients who wish to wear fashionable shoes.
Injections into the first MTP joint may provide temporary relief. Both steroid and hyaluronic acid have been advocated, although hyaluronic acid does not have FDA approval for use in the first MTP joint.58,69 Corticosteroid injections are most beneficial for patients with less severe arthritis, and their effectiveness in severe arthritis is limited. 69 When hyaluronic acid was compared to steroid in a prospective study of 37 patients, improvement in both function and pain was demonstrated in both groups at 3 months. 58 Hyaluronic acid was shown to be superior to steroid injection as measured by improved visual analog scale (VAS) scores with ambulation at 28 and 56 days; however, these improvements did not extend to pain at rest. 58 Furthermore, no differences were detected between groups with clinical examination. 58
Operative Management
Cheilectomy
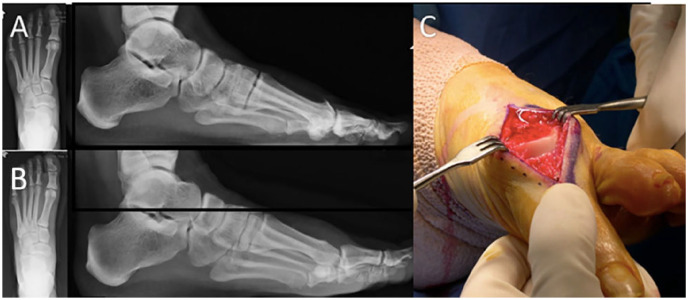
DuVries first described dorsal cheilectomy in 1959, and its widespread continued use is a testament to its clinical utility. 36 Cheilectomy involves debridement of dorsal osteophytes from the metatarsal head and proximal phalanx along with removal of the dorsal one-third of the articular surface (Figure 2). Synovitis is also debrided. The collateral ligaments should be preserved to prevent angular deformity and an overaggressive resection of the metatarsal head should be avoided to prevent subluxation of the proximal phalanx. 35 Cheilectomy is best reserved for patients whose symptoms primarily relate to pain from dorsal impingement of periarticular osteophytes. Additionally, the ideal patient will have preserved joint space on radiographs and minimal axial load pain on clinical examination.
Figure 2.
Cheilectomy. (A) Radiographic images demonstrating well-preserved joint space with large dorsal osteophyte. (B) Radiographic image following cheilectomy. (C) Operative image following dorsal cheilectomy. Note the obvious debridement of osteophytes, removal of the dorsal articular surface and maintained joint alignment.
The literature supporting cheilectomy demonstrates consistently good outcomes; however, the majority of studies supporting cheilectomy are of low quality (Level III or IV). 51 Among studies with a comparison group of arthrodesis, implant, or interpositional arthroplasty, outcomes from cheilectomy have been comparable or better than the alternative procedures in patients with Coughlin grade I or II hallux rigidus.4,42,59 Level IV studies have demonstrated good to excellent outcomes in 72% to 100% of patients. 51
Although satisfaction following cheilectomy is high, failures have been reported. Rates of conversion to arthrodesis have ranged from 7% to 9% within 10 years following surgery.15,54 Despite some failures, overall success and satisfaction in these studies was more than 90%.15,54 Dorsal osteophytes recur in 31% of patients following cheilectomy. 22 It is important to note, however, that 43% of the patients with recurrent osteophytes had pain in midrange of motion, which suggests that osteophyte recurrence most likely results from the progression of arthritis. 22
Advanced arthritis portends a poorer prognosis following cheilectomy. Patients with Hattrup and Johnson grade III hallux rigidus progressed to arthrodesis 25% of the time in one study, whereas patients with Coughlin and Shurnas grade III hallux rigidus required arthrodesis 56% of the time in another study.15,22 Advanced arthritis does not preclude a good outcome; however, these patients should be cautioned of the high rate of revision surgery.
Preoperative counseling should stress that pain relief is reliable following cheilectomy; however, improvement in motion is often limited. It is evident, despite the well-documented challenge in clinical evaluation of motion of the first MTP joint, that intraoperative motion is not preserved following cheilectomy.22,74 Measured dorsiflexion following cheilectomy has been reported to be between 21 and 39 degrees, which stands in stark contrast to intraoperative motion that often reaches 80 to 90 degrees.22,74 Two prospective gait studies of first MTP motion following cheilectomy have demonstrated that dorsiflexion improves between 12 and 17 degrees, which is physiologically decreased and will be noticeable to a patient with an unaffected contralateral toe.54,68
Clinical outcomes are not affected by progression of arthritis among patients with grade I or II hallux rigidus; however, patients should be cautioned that radiographic progression is common. Progression of arthritis has been demonstrated in 6 of 17 patients with grade I hallux rigidus, and in 24 of 39 patients with grade II hallux rigidus. 23 No patients, however, required additional surgery.
Finally, arthroscopic cheilectomy, which was first described in 1998, continues to experience limited use.38,41 The initial study of arthroscopic cheilectomy demonstrated high satisfaction, excellent pain relief and, as opposed to open cheilectomy, marked improvement in both overall motion and maximal dorsiflexion following surgery in 15 patients at an average follow up of 9 months. 41 To date, no comparative studies have been performed between open cheilectomy and arthroscopic cheilectomy and the learning curve limits its use; however, arthroscopy may play a role in select patients with arthritis of the first MTP joint. 38
Moberg Osteotomy
A dorsal closing wedge osteotomy, also known as a Moberg osteotomy, of the proximal phalanx can be done in conjunction with a cheilectomy to shift the arc of motion towards increased dorsiflexion. In addition to favorably altering the arc of motion, the Moberg osteotomy has been demonstrated to translate the joint contact pressure plantarward on the metatarsal head without altering joint contact area or peak pressures. 44 Cartilage loss in patients with hallux rigidus tends to be focused on the dorsal aspect of the metatarsal head; therefore, addition of a Moberg osteotomy may offload areas of residual diseased cartilage following cheilectomy.
As with cheilectomy, data supporting Moberg osteotomy is sparse and tends to be of low quality. 51 Existing studies pairing a Moberg osteotomy with cheilectomy have, however, demonstrated consistently favorable results.46,63,71 A retrospective review of 81 patients with Coughlin and Shurnas grade III hallux rigidus demonstrated excellent results even in this subset of patients with more severe arthritis when Moberg osteotomy was added to standard cheilectomy. 56 An 85% satisfaction rate was reported, with only 5% of patients requiring subsequent conversion to arthrodesis. 56
The biggest drawback to the Moberg osteotomy is potential increased challenge when conversion to arthrodesis is required because of failure of the primary procedure. The altered osteology of the proximal phalanx may preclude the use of popular countered first MTP joint arthrodesis plates favored by many surgeons, leading some authors to advocate isolated lag screws for arthrodesis fixation. 56
Keller Resection Arthroplasty
Keller resection arthroplasty is a treatment option for older, sedentary, and less active patients. This straightforward procedure decompresses the joint via resection of the base of the proximal phalanx. Dorsiflexion is increased at the expense of joint stability. Transfer metatarsalgia, weakness with toe-off, and cock-up deformity are reported complications that limit the pool of appropriate candidates for Keller resection arthroplasty.4,48 A mean American Orthopaedic Foot & Ankle Society (AOFAS) ankle-hindfoot score of 83 and a revision rate of 5% were demonstrated in a retrospective review of 87 patients after Keller resection at an average of 23 years. 64 The paradox of Keller resection arthroplasty is reliable pain relief with a high incidence of complications. A prospective study of 75 feet treated with a Keller resection arthroplasty found pain relief in 91% of patients but a cock-up toe deformity in 41% of patients at 31 months. 48 Overall satisfaction was 77% despite reliable improvement in pain, probably because of the high incidence of cock-up toe deformity. 48 The bone resection done for a Keller leads to worse outcomes when conversion to arthrodesis is required further limiting the procedure to a small subset of older, sedentary patients.
Interpositional Arthroplasty
Initial reports of interpositional arthroplasty were mired with complications including transfer metatarsalgia, hallux weakness, and cock-up toe deformity.12,46 Subsequent modifications of the initial technique preserved metatarsal length and the flexor hallucis brevis insertion, which improved outcomes. 12 Several variations of interpositional arthroplasty have been described that are in current use.
Multiple authors have described techniques that utilize allograft tissue as a biologic spacer. A retrospective review of 7 patients who underwent interposition of gracilis tendon into the first MTP joint demonstrated improved function and decreased pain at an average of 3.5 years following surgery. 13 Fifty-seven percent of patients, however, reported “mild” metatarsalgia. 13 Excellent results were described in 9 patients using an acellular dermal regenerative tissue matrix at an average of 12.7 months following surgery. 7 Six patients were identified in a follow-up study at an average of 5.4 years following surgery and all 6 patients remained satisfied. 39 Additionally, meniscal allograft, 21 amniotic fluid membrane, 24 and fascia lata 29 have been advocated. Other authors have advocated for local tissue transfer for interposition. Capsular interposition was described in 1997 and shown to have excellent outcomes in 37 feet. 33 Subsequent studies of capsular interposition have yielded similar positive outcomes.32,43
Among studies with a comparison group, the outcomes of interpositional arthroplasty are somewhat more mixed. When compared to arthrodesis, higher AOFAS scores and lower peak plantar pressures were found in the cohort of patients undergoing interpositional arthroplasty, suggesting interpositional arthroplasty may be a viable alternative to arthrodesis. 50 When interpositional arthroplasty is compared to cheilectomy, however, no difference in AOFAS scores, VAS, or SF-36 have been found. 46 Importantly, outcomes were less reliable in the interpositional arthroplasty group at a mean follow-up of 24 months. 46 It should be noted, however, that patients treated with interpositional arthroplasty had more significant arthritis preoperatively.
MTP Joint Arthroplasty
Although several authors have reported satisfactory results following implant arthroplasty of the first MTP joint,45,59,72 high rates of osteolysis, subsidence, and implant failure have limited its use (Figure 3).16,26,37,61,65 Initial attempts at joint replacement of the great toe utilized silastic implants. Not only were silastic implants plagued by osteolysis and subsidence, but immune reaction to the implant led to additional failures.16,65 The resultant bone loss was a clinical challenge when conversion to arthrodesis was attempted; thus, these implants are in limited use today. 47
Figure 3.

(A) Failed hemiarthroplasty. The patient experienced recurrent pain and stiffness within 10 years of surgery. (B) Conversion to first metatarsal phalangeal joint arthrodesis using an autograft tricortical iliac crest bone graft to restore metatarsal length.
Metallic implants have been used for both total joint arthroplasty and hemiarthroplasty of the first MTP joint. Results have been mixed. The developer of one such implant reported favorable results in a retrospective cohort of 279 patients following metallic hemiarthroplasty of the proximal phalanx. 72 Good to excellent results were reported in 95% of patients. A more recent study demonstrated improved SF-36 and AOFAS scores as well as increased motion in 26 patients following hemiarthroplasty at an average of 2.3 years following surgery. 45 Satisfaction was 100%, and the revision rate was 13% at follow-up. 45
Other authors have reported less favorable outcomes. Rates of revision range from 5.5% to 24.1% within 5 years of surgery in multiple well-performed studies of arthroplasty of the first MTP joint.37,60,61 Furthermore, implant subsidence was found in one-third of patients at midterm follow-up. 60 Ceramic implants yielded similarly poor results, with revision rates between 26% and 32%.19,53
Arthroplasty of the hallux has compared poorly to first MTP arthrodesis. A retrospective review of 21 metatarsal head hemiarthroplasties demonstrated that satisfaction was lower, pain VAS scores were higher, and AOFAS scores were worse compared to a cohort of 27 arthrodesis patients. 61 At a mean of 15 years following arthrodesis or arthroplasty, arthrodesis patients were found to experience less pain, higher satisfaction, and lower rates of revision when compared to arthroplasty patients. 70
Salvage of failed first MTP arthroplasty to arthrodesis is a potential challenge because of multiplanar deformity, poor bone quality, and bone loss with resultant metatarsal shortening (Figure 3). A bone block arthrodesis (Figure 3) is frequently required to restore metatarsal length, and multiple authors have reported series using both allograft and autograft techniques.10,49,52 Satisfactory outcomes have been reported following bone block arthrodesis.25,49,52 No studies, however, have compared bone block arthrodesis to primary arthrodesis. Nonetheless, relatively longer time to fusion, lower rates of fusion, and increased wound healing complications have all been found among bone block arthrodesis patients when compared to studies of outcomes following primary arthrodesis.10,25,31,49,52
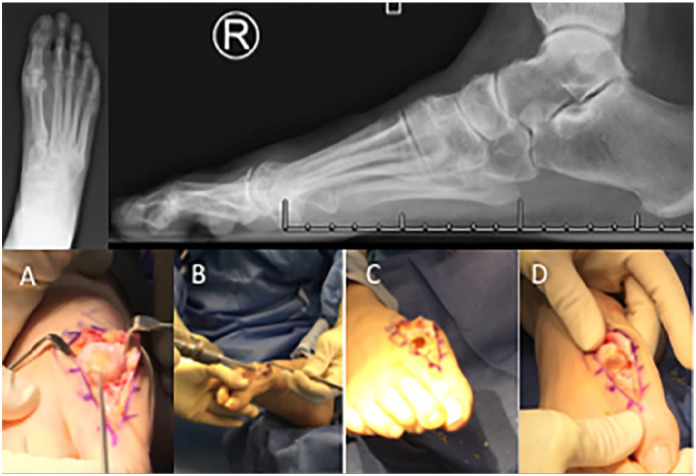
Polyvinyl Alcohol Hydrogel Hemiarthroplasty
A PVA hydrogel implant gained premarket approval from the FDA for implantation in the United States in July 2016. The implant has similar material properties to human articular cartilage in terms of water content, tensile strength, and compressive modulus.1,55 The implant is held in place via press fit and is intended to sit proud by 1.5 mm, allowing it to function as both a hemiarthroplasty and interpositional spacer between arthritic surfaces (Figure 4). 76
Figure 4.
Top row: Preoperative radiographs demonstrating decreased joint space and large osteophytes on the metatarsal head and the base of the proximal phalanx. Bottom row: (A) The guidewire placed centrally in the metatarsal head. (B) Over-reaming the guidewire with a 10-mm step drill. (C) The void left in place by the drill. Note the overall preservation of the metatarsal head morphology and length. (D) Implant in place.
A prospective, randomized, noninferiority study comparing the PVA hydrogel implant to arthrodesis demonstrated that postoperative pain, function, and rates of revision surgery were similar between groups at 12 and 24 months; however, motion improved by 27% in the PVA hydrogel implant group. 3 Similar outcomes between the PVA hydrogel implant group and arthrodesis group were recently confirmed among patients with deformity up to 20 degrees and with severe preoperative stiffness. 27 A subset of 29 patients were available for prospective evaluation at 5 years and demonstrated that pain VAS, SF-36, Foot and Ankle Ability Measure (FAAM) activities of daily living and FAAM sports subscales improved and closely resembled the scores found in the initial study. 17 Only 1 patient (4%) required revision to arthrodesis. 17 Neither study identified cases of implant wear, subsidence, loosening, or osteolysis.3,17 Furthermore, conversion of the PVA hydrogel implant to arthrodesis was demonstrated to yield equivalent results to primary arthrodesis, which marks a substantial improvement over previous attempts at first MTP joint arthroplasty. 3 Early and midterm results of the PVA hydrogel are encouraging; however, long-term studies are lacking.
First MTP Joint Arthrodesis
Arthrodesis of the first MTP joint remains the gold standard treatment for advanced arthritis (Figure 5). Arthrodesis is also the best option for patients with limited stability of the first MTP joint due to concomitant angular deformity (hallux varus and valgus), soft tissue compromise (rheumatoid arthritis), or neuromuscular disorders because of the challenge of maintaining joint alignment in these populations.
Figure 5.
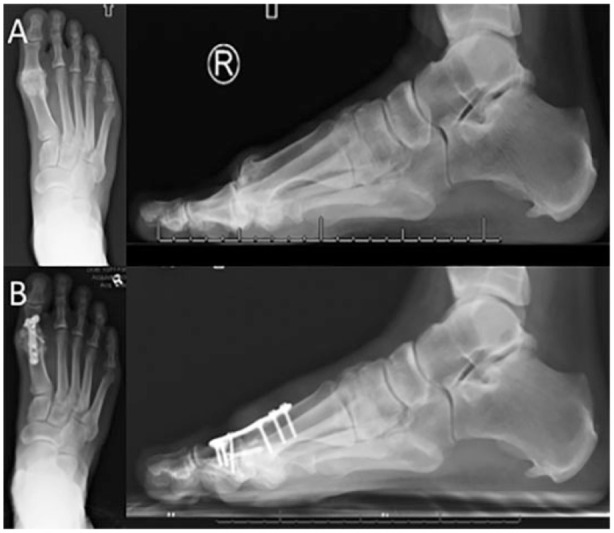
First metatarsophalangeal joint arthrodesis. (A) Significant sclerosis, joint space obliteration, and large periarticular osteophytes signify advanced arthritic changes. (B) Following arthrodesis with plate and screw construct. Note maintenance of physiologic valgus and dorsiflexion of the hallux.
Multiple techniques have been described for arthrodesis of the first MTP joint. Conical reamers allow for intraoperative adjustment of the arthrodesis position once the cartilage has been debrided (Figure 6). 28 Flat cuts can also be used although positioning the arthrodesis can be challenging after the cuts have been made if the initial alignment is not satisfactory. Shortening of the first ray is an additional risk and can lead to transfer metatarsalgia. The toe should be positioned in neutral rotation, 5 to 15 degrees of valgus and 10 to 15 degrees of dorsiflexion relative to the floor (Figure 6). 36 Physiologic valgus positions the hallux parallel to the second toe and allows for comfortable shoe wear. Dorsiflexion is measured with simulated weight-bearing on a sterile flat plate (Figure 6). When positioned properly, the pad of the hallux should rest on the plate but passively accommodate the surgeon’s finger (5-10 mm). 36 Fixation of the arthrodesis can be accomplished using crossed screws, a dorsal plate, or some combination of plate and screws. A biomechanical comparison of multiple constructs including single lag screw, dorsal plate in isolation, lag screw with dorsal plate, and crossed K-wires demonstrated that the lag screw with a dorsal plate was in the most stable construct. 57 The plate-and-screw construct was 3 times stronger than an isolated lag screw and 10 times stronger than crossed K-wires and dorsal plate in isolation. 57 Addition of a second screw in a screw-only construct more closely approximates the stiffness and load to failure of a plate-and-screw construct, but remains significantly weaker. 11 The clinical implications of construct strength and stiffness remain unknown, and the increased stability must be weighed against the increase in implant price, which can be substantial. 40
Figure 6.
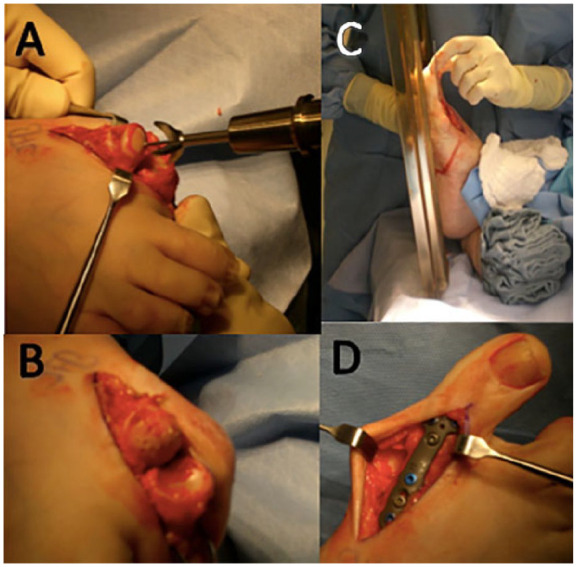
Intraoperative photograph of first metatarsophalangeal joint arthrodesis: (A) Conical reamers used to debride residual cartilage and create congruent surfaces for fusion. (B) The metatarsal head following joint preparation. Note the drill holes used to perforate the subchondral bone surface. (C) Flat plate used to judge great toe clearance in the proposed position of fusion. (D) Dorsal plate in place. Not seen is the lag screw placed from distal to proximal that compresses the joint surface.
Multiple authors have reported favorable outcomes following arthrodesis of the first MTP joint. A prospective cohort study of 50 patients undergoing first MTP joint arthrodesis found a high rate of satisfaction, a low rate of nonunion, and only a 4% incidence of revision surgery at an average of 1.3 years following surgery. 28 Another large, prospective cohort study demonstrated 1% revision rate using a plate and screw construct. 5
Activity level and gait following first MTP joint arthrodesis have been evaluated in a number of studies. Ninety-two percent of patients are able to return to hiking, 80% of patients are able to return to golf, and 75% of patients are able to jog and play tennis following first MTP joint arthrodesis. 9 Gait analysis following first MTP joint arthrodesis has revealed an increased step length with improved ankle plantarflexion and power.8,20 Furthermore, weight-bearing is restored to the medial column of the foot resulting in improved force at toe-off. 8 Despite improvements, these parameters are not improved to the level of the contralateral extremity. 20
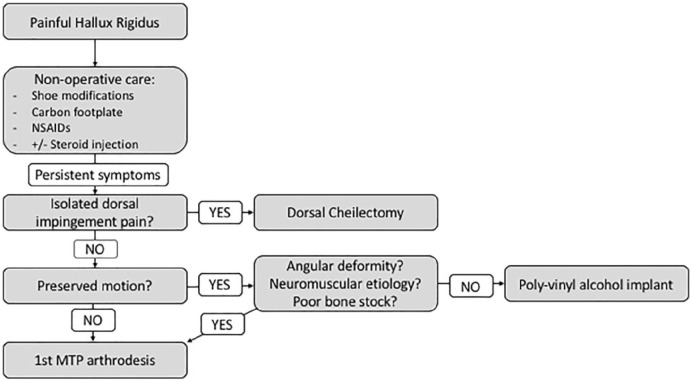
Authors’ Preferred Treatment
The authors have developed an algorithm to guide the treatment of hallux rigidus (Figure 7). We advocate nonoperative care for all patients on initial presentation for hallux rigidus. Our preferred treatment is a carbon footplate under the insole of the shoe or with an over-the-counter arch support. We recommend cautious use of NSAIDs as needed and judiciously inject the first MTP joint with corticosteroids before an important event such as a wedding or vacation. In general, we view the need for injection as a progression of disease that warrants surgical intervention.
Figure 7.
Authors’ preferred treatment algorithm for hallux rigidus.
We perform a cheilectomy for patients with pain only on passive or active dorsiflexion and view axial load pain (positive grind test) as progressive arthritis that cannot reliably be treated with cheilectomy. A Moberg osteotomy is reserved for patients with impingement symptoms and marked lack of dorsiflexion following cheilectomy; this is an intraoperative decision, and we discuss this with patients before surgery for the purposes of informed consent. Immediate weight-bearing in a postoperative shoe is permitted followed by gradual return to shoes as tolerated when the wound is well healed (generally by 2-3 weeks).
The PVA hydrogel implant has augmented our treatment options for advanced hallux rigidus. Prior to FDA approval of the device, we performed an arthrodesis using a single cannulated lag screw and anatomic dorsal plate for all patients with advanced arthritis of the first MTP joint. We recommend arthrodesis in patient with lack of motion at the first MTP joint given the modest postoperative improvement we have observed in range of motion. Furthermore, we view hallux varus, hallux valgus, neuromuscular conditions, and rheumatoid arthritis as contraindications to the PVA implant and continue to perform arthrodesis in these situations. For patients with advanced arthritis but residual motion, we have found that the PVA hydrogel implant is an appealing alternative to arthrodesis. Following arthrodesis, patients are made non–weight-bearing for 1 week followed by weight-bearing as tolerated in a cast or boot for an additional 5 weeks. Our postoperative protocol following the PVA hydrogel implant is the same as for cheilectomy: weight-bearing as tolerated in a postoperative shoe followed by progression to regular shoes as tolerated when the incision permits.
Our experience revising metallic first MTP arthroplasties from outside institutions has soured our enthusiasm for those implants and we do not use them in our practice. Prior to the PVA hydrogel implant, we would occasionally perform an interpositional arthroplasty using the dorsal capsular structures in older or sedentary patients in whom implant failure or nonunion may be a concern. We now use the PVA hydrogel implant in these situations provided the bone stock is adequate and there is no evidence of severe osteoporosis.
Conclusion
Hallux rigidus is a common condition encountered by orthopaedic foot and ankle surgeons. Initial nonoperative treatments are successful for approximately half of all patients and should be attempted before operative care. Patients with mild to moderate arthritis and symptoms primarily driven by dorsal impingement respond well to cheilectomy. Arthrodesis of the first MTP joint remains the gold standard option for advanced arthritis; however, the recent FDA approval of the PVA hydrogel implant has begun to change the management of advanced arthritis by providing a motion-sparing option with outcomes similar to arthrodesis.
Footnotes
This article was originally published as: Anderson MR, Ho BS, Baumhauer JF. Current concepts review: hallux rigidus. Foot Ankle Orthop. 2018 Jun 22;3(2):2473011418764461. doi:10.1177/2473011418764461.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Judith F. Baumhauer, MD, MPH, reports personal fees from CORR, personal fees from Best Doctors, personal fees from Cartiva Medical, personal fees from DJO, personal fees from Ferring Pharma, personal fees from Nextremity Solutions, personal fees from Wright Medical, outside the submitted work. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Baker MI, Walsh SP, Schwartz Z, Boyan BD. A review of polyvinyl alcohol and its uses in cartilage and orthopedic applications. J Biomed Mater Res B Appl Biomater. 2012;100(5):1451–1457. [DOI] [PubMed] [Google Scholar]
- 2. Baumhauer JF, Singh D, Glazebrook M, et al. Correlation of hallux rigidus grade with motion, VAS pain, intraoperative cartilage loss, and treatment success for first MTP joint arthrodesis and synthetic cartilage implant. Foot Ankle Int. 2017;38(11):1175–1182. [DOI] [PubMed] [Google Scholar]
- 3. Baumhauer JF, Singh D, Glazebrook M, et al. Prospective, randomized, multi-centered clinical trial assessing safety and efficacy of a synthetic cartilage implant versus first metatarsophalangeal arthrodesis in advanced hallux rigidus. Foot Ankle Int. 2016;37(5):457–469. [DOI] [PubMed] [Google Scholar]
- 4. Beertema W, Draijer WF, van Os JJ, Pilot P. A retrospective analysis of surgical treatment in patients with symptomatic hallux rigidus: long-term follow-up. J Foot Ankle Surg. 2006;45(4):244–251. [DOI] [PubMed] [Google Scholar]
- 5. Bennett GL, Sabetta J. First metatarsalphalangeal joint arthrodesis: evaluation of plate and screw fixation. Foot Ankle Int. 2009;30(8):752–757. [DOI] [PubMed] [Google Scholar]
- 6. Bergin SM, Munteanu SE, Zammit GV, Nikolopoulos N, Menz HB. Impact of first metatarsophalangeal joint osteoarthritis on health-related quality of life. Arthritis Care Res (Hoboken). 2012;64(11):1691–1698. [DOI] [PubMed] [Google Scholar]
- 7. Berlet GC, Hyer CF, Lee TH, et al. Interpositional arthroplasty of the first MTP joint using a regenerative tissue matrix for the treatment of advanced hallux rigidus. Foot Ankle Int. 2008;29(1):10–21. [DOI] [PubMed] [Google Scholar]
- 8. Brodsky JW, Baum BS, Pollo FE, Mehta H. Prospective gait analysis in patients with first metatarsophalangeal joint arthrodesis for hallux rigidus. Foot Ankle Int. 2007;28(2):162–165. [DOI] [PubMed] [Google Scholar]
- 9. Brodsky JW, Passmore RN, Pollo FE, Shabat S. Functional outcome of arthrodesis of the first metatarsophalangeal joint using parallel screw fixation. Foot Ankle Int. 2005;26(2):140–146. [DOI] [PubMed] [Google Scholar]
- 10. Brodsky JW, Ptaszek AJ, Morris SG. Salvage first MTP arthrodesis utilizing ICBG: clinical evaluation and outcome. Foot Ankle Int. 2000;21(4):290–296. [DOI] [PubMed] [Google Scholar]
- 11. Buranosky DJ, Taylor DT, Sage RA, et al. First metatarsophalangeal joint arthrodesis: quantitative mechanical testing of six-hole dorsal plate versus crossed screw fixation in cadaveric specimens. J Foot Ankle Surg. 2001;40(4):208–213. [DOI] [PubMed] [Google Scholar]
- 12. Can Akgun R, Sahin O, Demirors H, Cengiz Tuncay I. Analysis of modified oblique Keller procedure for severe hallux rigidus. Foot Ankle Int. 2008;29(12):1203–1208. [DOI] [PubMed] [Google Scholar]
- 13. Coughlin MJ, Shurnas PJ. Soft-tissue arthroplasty for hallux rigidus. Foot Ankle Int. 2003;24(9):661–672. [DOI] [PubMed] [Google Scholar]
- 14. Coughlin MJ, Shurnas PS. Hallux rigidus. Grading and long-term results of operative treatment. J Bone Joint Surg Am. 2003;85-A (11):2072–2088. [PubMed] [Google Scholar]
- 15. Coughlin MJ, Shurnas PS. Hallux rigidus: demographics, etiology, and radiographic assessment. Foot Ankle Int. 2003;24(10):731–743. [DOI] [PubMed] [Google Scholar]
- 16. Cracchiolo A, 3rd, Weltmer JB, Jr, Lian G, Dalseth T, Dorey F. Arthroplasty of the first metatarsophalangeal joint with a double-stem silicone implant. Results in patients who have degenerative joint disease failure of previous operations, or rheumatoid arthritis. J Bone Joint Surg Am. 1992;74(4):552–563. [PubMed] [Google Scholar]
- 17. Daniels TR, Younger AS, Penner MJ, et al. Midterm outcomes of polyvinyl alcohol hydrogel hemiarthroplasty of the first metatarsophalangeal joint in advanced hallux rigidus. Foot Ankle Int. 2017;38(3):243–247. [DOI] [PubMed] [Google Scholar]
- 18. D’Arcangelo PR, Landorf KB, Munteanu SE, Zammit GV, Menz HB. Radiographic correlates of hallux valgus severity in older people. J Foot Ankle Res. 2010;3:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Dawson-Bowling S, Adimonye A, Cohen A, et al. MOJE ceramic metatarsophalangeal arthroplasty: disappointing clinical results at two to eight years. Foot Ankle Int. 2012;33(7):560–564. [DOI] [PubMed] [Google Scholar]
- 20. DeFrino PF, Brodsky JW, Pollo FE, Crenshaw SJ, Beischer AD. First metatarsophalangeal arthrodesis: a clinical, pedobarographic and gait analysis study. Foot Ankle Int. 2002;23(6):496–502. [DOI] [PubMed] [Google Scholar]
- 21. DelaCruz EL, Johnson AR, Clair BL. First metatarsophalangeal joint interpositional arthroplasty using a meniscus allograft for the treatment of advanced hallux rigidus: surgical technique and short-term results. Foot Ankle Spec. 2011;4(3):157–164. [DOI] [PubMed] [Google Scholar]
- 22. Easley ME, Davis WH, Anderson RB. Intermediate to long-term follow-up of medial-approach dorsal cheilectomy for hallux rigidus. Foot Ankle Int. 1999;20(3):147–152. [DOI] [PubMed] [Google Scholar]
- 23. Feltham GT, Hanks SE, Marcus RE. Age-based outcomes of cheilectomy for the treatment of hallux rigidus. Foot Ankle Int. 2001;22(3):192–197. [DOI] [PubMed] [Google Scholar]
- 24. Ferguson CM, Ellington JK. Operative technique: interposition arthroplasty and biological augmentation of hallux rigidus surgery. Foot Ankle Clin. 2015;20(3):513–524. [DOI] [PubMed] [Google Scholar]
- 25. Garras DN, Durinka JB, Bercik M, Miller AG, Raikin SM. Conversion arthrodesis for failed first metatarsophalangeal joint hemiarthroplasty. Foot Ankle Int. 2013;34(9):1227–1232. [DOI] [PubMed] [Google Scholar]
- 26. Gibson JN, Thomson CE. Arthrodesis or total replacement arthroplasty for hallux rigidus: a randomized controlled trial. Foot Ankle Int. 2005;26(9):680–690. [DOI] [PubMed] [Google Scholar]
- 27. Goldberg A, Singh D, Glazebrook M, et al. Association between patient factors and outcome of synthetic cartilage implant hemiarthroplasty vs first metatarsophalangeal joint arthrodesis in advanced hallux rigidus. Foot Ankle Int. 2017;38(11):1199–1206. [DOI] [PubMed] [Google Scholar]
- 28. Goucher NR, Coughlin MJ. Hallux metatarsophalangeal joint arthrodesis using dome-shaped reamers and dorsal plate fixation: a prospective study. Foot Ankle Int. 2006;27(11):869–876. [DOI] [PubMed] [Google Scholar]
- 29. Gould JS, Florence MN. Interpositional arthroplasty of the great toe metatarsophalangeal joint using autogenous fascia lata for advanced hallux rigidus. Techn Foot Ankle Surg. 2015;14(2):65–68. [Google Scholar]
- 30. Grady JF, Axe TM, Zager EJ, Sheldon LA. A retrospective analysis of 772 patients with hallux limitus. J Am Podiatr Med Assoc. 2002;92(2):102–108. [DOI] [PubMed] [Google Scholar]
- 31. Gross CE, Hsu AR, Lin J, Holmes GB, Lee S. Revision MTP arthrodesis for failed MTP arthroplasty. Foot Ankle Spec. 2013;6(6):471–478. [DOI] [PubMed] [Google Scholar]
- 32. Hahn MP, Gerhardt N, Thordarson DB. Medial capsular interpositional arthroplasty for severe hallux rigidus. Foot Ankle Int. 2009;30(6):494–499. [DOI] [PubMed] [Google Scholar]
- 33. Hamilton WG, O’Malley MJ, Thompson FM, Kovatis PE. Roger Mann Award 1995. Capsular interposition arthroplasty for severe hallux rigidus. Foot Ankle Int. 1997;18(2):68–70. [DOI] [PubMed] [Google Scholar]
- 34. Hattrup SJ, Johnson KA. Subjective results of hallux rigidus following treatment with cheilectomy. Clin Orthop Relat Res. 1988;226:182–191. [PubMed] [Google Scholar]
- 35. Heller WA, Brage ME. The effects of cheilectomy on dorsiflexion of the first metatarsophalangeal joint. Foot Ankle Int. 1997;18(12):803–808. [DOI] [PubMed] [Google Scholar]
- 36. Ho B, Baumhauer J. Hallux rigidus. EFORT Open Rev. 2017;2(1):13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Horisberger M, Haeni D, Henninger HB, Valderrabano V, Barg A. Total arthroplasty of the metatarsophalangeal joint of the hallux. Foot Ankle Int. 2016;37(7):755–765. [DOI] [PubMed] [Google Scholar]
- 38. Hunt KJ. Hallux metatarsophalangeal (MTP) joint arthroscopy for hallux rigidus. Foot Ankle Int. 2015;36(1):113–119. [DOI] [PubMed] [Google Scholar]
- 39. Hyer CF, Granata JD, Berlet GC, Lee TH. Interpositional arthroplasty of the first metatarsophalangeal joint using a regenerative tissue matrix for the treatment of advanced hallux rigidus: 5-year case series follow-up. Foot Ankle Spec. 2012;5(4):249–252. [DOI] [PubMed] [Google Scholar]
- 40. Hyer CF, Glover JP, Berlet GC, Lee TH. Cost comparison of crossed screws versus dorsal plate construct for first metatarsophalangeal joint arthrodesis. J Foot Ankle Surg. 2008;47(1):13–18. [DOI] [PubMed] [Google Scholar]
- 41. Iqbal MJ, Chana GS. Arthroscopic cheilectomy for hallux rigidus. Arthroscopy. 1998;14(3):307–310. [DOI] [PubMed] [Google Scholar]
- 42. Keiserman LS, Sammarco VJ, Sammarco GJ. Surgical treatment of the hallux rigidus. Foot Ankle Clin. 2005;10(1):75–96. [DOI] [PubMed] [Google Scholar]
- 43. Kennedy JG, Chow FY, Dines J, Gardner M, Bohne WH. Outcomes after interposition arthroplasty for treatment of hallux rigidus. Clin Orthop Relat Res. 2006;445:210–215. [DOI] [PubMed] [Google Scholar]
- 44. Kim PH, Chen X, Hillstrom H, et al. Moberg osteotomy shifts contact pressure plantarly in the first metatarsophalangeal joint in a biomechanical model. Foot Ankle Int. 2016;37(1):96–101. [DOI] [PubMed] [Google Scholar]
- 45. Kline AJ, Hasselman CT. Metatarsal head resurfacing for advanced hallux rigidus. Foot Ankle Int. 2013;34(5):716–725. [DOI] [PubMed] [Google Scholar]
- 46. Lau JT, Daniels TR. Outcomes following cheilectomy and interpositional arthroplasty in hallux rigidus. Foot Ankle Int. 2001;22(6):462–470. [DOI] [PubMed] [Google Scholar]
- 47. Lawrence BR, Thuen E. A retrospective review of the primus first MTP joint double-stemmed silicone implant. Foot Ankle Spec. 2013;6(2):94–100. [DOI] [PubMed] [Google Scholar]
- 48. Love TR, Whynot AS, Farine I, et al. Keller arthroplasty: a prospective review. Foot Ankle. 1987;8(1):46–54. [DOI] [PubMed] [Google Scholar]
- 49. Luk PC, Johnson JE, McCormick JJ, Klein SE. First metatarsophalangeal joint arthrodesis technique with interposition allograft bone block. Foot Ankle Int. 2015;36(8):936–943. [DOI] [PubMed] [Google Scholar]
- 50. Mackey RB, Thomson AB, Kwon O, Mueller MJ, Johnson JE. The modified oblique Keller capsular interpositional arthroplasty for hallux rigidus. J Bone Joint Surg Am. 2010;92(10):1938–1946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. McNeil DS, Baumhauer JF, Glazebrook MA. Evidence-based analysis of the efficacy for operative treatment of hallux rigidus. Foot Ankle Int. 2013;34(1):15–32. [DOI] [PubMed] [Google Scholar]
- 52. Myerson MS, Schon LC, McGuigan FX, Oznur A. Result of arthrodesis of the hallux metatarsophalangeal joint using bone graft for restoration of length. Foot Ankle Int. 2000;21(4):297–306. [DOI] [PubMed] [Google Scholar]
- 53. Nagy MT, Walker CR, Sirikonda SP. Second-generation ceramic first metatarsophalangeal joint replacement for hallux rigidus. Foot Ankle Int. 2014;35(7):690–698. [DOI] [PubMed] [Google Scholar]
- 54. Nawoczenski DA, Ketz J, Baumhauer JF. Dynamic kinematic and plantar pressure changes following cheilectomy for hallux rigidus: a mid-term followup. Foot Ankle Int. 2008;29(3):265–272. [DOI] [PubMed] [Google Scholar]
- 55. Noguchi T, Yamamuro T, Oka M, et al. Poly(vinyl alcohol) hydrogel as an artificial articular cartilage: evaluation of biocompatibility. J Appl Biomater. 1991;2(2):101–107. [DOI] [PubMed] [Google Scholar]
- 56. O’Malley MJ, Basran HS, Gu Y, Sayres S, Deland JT. Treatment of advanced stages of hallux rigidus with cheilectomy and phalangeal osteotomy. J Bone Joint Surg Am. 2013;95(7):606–610. [DOI] [PubMed] [Google Scholar]
- 57. Politi J, John H, Njus G, Bennett GL, Kay DB. First metatarsal-phalangeal joint arthrodesis: a biomechanical assessment of stability. Foot Ankle Int. 2003;24(4):332–337. [DOI] [PubMed] [Google Scholar]
- 58. Pons M, Alvarez F, Solana J, Viladot R, Varela L. Sodium hyaluronate in the treatment of hallux rigidus. A single-blind, randomized study. Foot Ankle Int. 2007;28(1):38–42. [DOI] [PubMed] [Google Scholar]
- 59. Pontell D, Gudas CJ. Retrospective analysis of surgical treatment of hallux rigidus/limitus: clinical and radiographic follow-up of hinged, silastic implant arthroplasty and cheilectomy. J Foot Surg. 1988;27(6):503–510. [PubMed] [Google Scholar]
- 60. Pulavarti RS, McVie JL, Tulloch CJ. First metatarsophalangeal joint replacement using the bio-action great toe implant: intermediate results. Foot Ankle Int. 2005;26(12):1033–1037. [DOI] [PubMed] [Google Scholar]
- 61. Raikin SM, Ahmad J, Pour AE, Abidi N. Comparison of arthrodesis and metallic hemiarthroplasty of the hallux metatarsophalangeal joint. J Bone Joint Surg Am. 2007;89(9):1979–1985. [DOI] [PubMed] [Google Scholar]
- 62. Roddy E, Thomas MJ, Marshall M, et al. The population prevalence of symptomatic radiographic foot osteoarthritis in community-dwelling older adults: cross-sectional findings from the clinical assessment study of the foot. Ann Rheum Dis. 2015;74(1):156–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Roukis TS. Outcomes after cheilectomy with phalangeal dorsiflexory osteotomy for hallux rigidus: a systematic review. J Foot Ankle Surg. 2010;49(5):479–487. [DOI] [PubMed] [Google Scholar]
- 64. Schneider W, Kadnar G, Kranzl A, Knahr K. Long-term results following Keller resection arthroplasty for hallux rigidus. Foot Ankle Int. 2011;32(10):933–939. [DOI] [PubMed] [Google Scholar]
- 65. Sebold EJ, Cracchiolo A, 3rd. Use of titanium grommets in silicone implant arthroplasty of the hallux metatarsophalangeal joint. Foot Ankle Int. 1996;17(3):145–151. [DOI] [PubMed] [Google Scholar]
- 66. Shereff MJ, Bejjani FJ, Kummer FJ. Kinematics of the first metatarsophalangeal joint. J Bone Joint Surg Am. 1986;68(3):392–398. [PubMed] [Google Scholar]
- 67. Shurnas PS. Hallux rigidus: etiology, biomechanics, and nonoperative treatment. Foot Ankle Clin. 2009;14(1):1–8. [DOI] [PubMed] [Google Scholar]
- 68. Smith SM, Coleman SC, Bacon SA, Polo FE, Brodsky JW. Improved ankle push-off power following cheilectomy for hallux rigidus: a prospective gait analysis study. Foot Ankle Int. 2012;33(6):457–461. [DOI] [PubMed] [Google Scholar]
- 69. Solan MC, Calder JD, Bendall SP. Manipulation and injection for hallux rigidus. Is it worthwhile? J Bone Joint Surg Br. 2001;83(5):706–708. [DOI] [PubMed] [Google Scholar]
- 70. Stone OD, Ray R, Thomson CE, Gibson JN. Long-term follow-up of arthrodesis vs total joint arthroplasty for hallux rigidus. Foot Ankle Int. 2017;38(4):375–380. [DOI] [PubMed] [Google Scholar]
- 71. Thomas PJ, Smith RW. Proximal phalanx osteotomy for the surgical treatment of hallux rigidus. Foot Ankle Int. 1999;20(1):3–12. [DOI] [PubMed] [Google Scholar]
- 72. Townley CO, Taranow WS. A metallic hemiarthroplasty resurfacing prosthesis for the hallux metatarsophalangeal joint. Foot Ankle Int. 1994;15(11):575–580. [DOI] [PubMed] [Google Scholar]
- 73. van Saase JL, van Romunde LK, Cats A, Vandenbroucke JP, Valkenburg HA. Epidemiology of osteoarthritis: Zoetermeer survey. Comparison of radiological osteoarthritis in a Dutch population with that in 10 other populations. Ann Rheum Dis. 1989;48(4):271–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Vulcano E, Tracey JA, 3rd, Myerson MS. Accurate measurement of first metatarsophalangeal range of motion in patients with hallux rigidus. Foot Ankle Int. 2016;37(5):537–541. [DOI] [PubMed] [Google Scholar]
- 75. Wilder FV, Barrett JP, Farina EJ. The association of radiographic foot osteoarthritis and radiographic osteoarthritis at other sites. Osteoarthritis Cartilage. 2005;13(3):211–215. [DOI] [PubMed] [Google Scholar]
- 76. Younger ASE, Baumhauer JF. Polyvinyl alcohol hydrogel hemiarthroplasty of the great toe: technique and indications. Techn Foot Ankle Surg. 2013;12(3):164–169. [Google Scholar]