Abstract
Background:
Ankle fracture surgeries are generally safe and effective procedures; however, as quality-based reimbursement models are increasingly affected by postoperative readmission, we aimed to determine the causes and risk factors for readmission following ankle fracture surgery.
Methods:
Ankle fracture cases were identified from the prospectively collected American College of Surgeons National Surgical Quality Improvement Program from 2013 to 2014. Demographics, comorbidities, and fracture characteristics were collected. Rates of 30-day adverse events and readmissions were determined as well as the causes for readmission. Multivariable logistic regression analyses were performed to identify risk factors associated with having any adverse events and being readmitted within 30 days of surgery.
Results:
There were 5056 patients included; 167 (3.3%) were open fractures. The rate of any postoperative adverse event was 5.2%. There were 116 unplanned readmissions, with a readmission rate of 2.3%. Of the 116 unplanned readmissions, 49 (42.2%) were for reasons related to the surgery or surgical site, with the most common causes being deep surgical site/hardware infections (12.9%), superficial site infections (11.2%), and wound disruption (6.9%). Most readmissions were for reasons unrelated to the surgical site (51.7%), including cardiac disorders (8.6%), pulmonary disorders (7.8%), and neurological/psychiatric disorders (6.9%). The cause of readmission was unknown for 6% of readmissions. With multivariable logistic regression, the strongest risk factors for readmission were a history of pulmonary disease (odds ratio [OR], 2.29), American Society of Anesthesiologists (ASA) class ≥3 (OR, 2.28), and open fractures (OR, 2.04) (all P < .05).
Conclusion:
In this cohort of 5056 ankle fracture cases, 2.3% of patients were readmitted within 30 days, with at least 51.7% of all unplanned readmissions due to causes unrelated to the surgery or surgical site. Predictors of readmission included a history of pulmonary disease, higher ASA class, and open fractures. Based on these findings, we advocate close medical follow-up with nonorthopaedic providers after discharge for high-risk patients.
Level of Evidence:
Level III.
Keywords: ankle fracture, open reduction internal fixation, readmissions, outcomes, complications
Commentary: A database study using NSQIP 2013-2014 examining 30 day adverse events, readmission rate and cause in 5056 patients. They found that most readmissions were unrelated to the surgical site, and of those at the surgical site deep infections, superficial infections, and wound disruption were most common.
Ankle fractures are common injuries, comprising approximately 9% of all fractures, and are often indicated for operative management.6,12 Although ankle fracture surgery is largely effective and relatively safe, it is nonetheless associated with postoperative morbidity and postdischarge readmissions.2,11,13 –15,17,18 However, the causes for readmission following ankle fracture surgery are poorly understood.
In an effort to improve quality and coordination of care, the Centers for Medicare and Medicaid Services introduced models involving bundled payments to align financial incentives and performance among health care providers. As of April 1, 2016, the Bundled Payments for Care Improvement initiative has 1521 participants including hospitals, physician group practices, and other facilities that receive bundled reimbursements for 30-day postacute care and readmissions. 5 As these quality-based bundled payment models become more common, identifying risk factors and causes for readmission may help decrease its incidence.
Given the relatively low incidence of postoperative readmissions and complications following ankle fracture surgery, the use of a large multicenter database provides the necessary statistical power to examine the preoperative characteristics associated with these adverse events. One such database, the American College of Surgeons National Surgical Quality Improvement Program (NSQIP), began collecting data regarding the causes for postoperative readmission within 30 days starting in 2013. 1 Using the NSQIP from 2013 to 2014, the most recent year of data available at the time of writing, the purpose of this study was to determine (1) the causes of readmission within 30 days, (2) the risk factors associated with readmission, and (3) the risk factors for any postoperative adverse event following ankle fracture surgery.
Materials and Methods
The NSQIP from years 2013 and 2014 was used for this retrospective cohort study. This database includes prospectively collected clinical data from more than 400 participating medical centers throughout the United States. 1 Data collection was performed at each site by clinical reviewers through a prospective review of operative cases. With frequent auditing to ensure data quality, the overall interrater disagreement rate for the NSQIP has been reported to be about 2%. 1 Irrespective of the discharge date, clinical information is collected up to the 30th postoperative day. An exemption was granted by our institutional review board for this study.
NSQIP years 2013 and 2014 were used for this study due to the availability of readmission data, as 2013 was the first NSQIP dataset that included readmission diagnosis codes. Cases with a principal diagnosis of an ankle fracture were identified with the use of International Classification of Diseases, Ninth Revision (ICD-9) codes 824 to 824.9. These ICD-9 codes allowed for the differentiation between fracture types, such as lateral malleolar, medial malleolar, bimalleolar, and trimalleolar as well as the identification of open fractures. Cases without essential preoperative data such as age, sex, height, and weight were excluded from the analysis. A total of 5056 ankle fracture cases were included in the study.
The body mass index was determined for each patient directly from the height and weight. Patients were categorized based on the World Health Organization system for obesity into nonobese (<30 kg/m2), obese I (30-34.9 kg/m2), obese II (35-39.9 kg/m2), or obese III (≥40 kg/m2). The type of anesthesia used and American Society of Anesthesiologists (ASA) classes were collected as well as the preoperative functional status in terms of independence with activities of daily living. The modified Charlson comorbidity index (CCI) based on information available in the NSQIP was determined for each patient as a measure of overall medical comorbidity burden. A similar methodology has been used in orthopaedic clinical outcomes research using the NSQIP.3,4,8
Postoperative study outcomes included any adverse events, major adverse events, minor adverse events, and unplanned readmissions within 30 days, irrespective of the day of discharge. Therefore, adverse events may have occurred both before and after discharge and may not specifically correspond to reasons for later readmission. Major adverse events included wound dehiscence, pneumonia, unplanned reintubation, prolonged ventilator requirement, acute renal insufficiency or failure, coma, cerebrovascular accident, deep vein thrombosis, pulmonary embolism, cardiac arrest, myocardial infarction, sepsis or septic shock, or return to the operating room. Minor adverse events included superficial surgical site infections, urinary tract infections, and blood transfusions. These criteria for major and minor postoperative adverse events have been previously established in studies using the NSQIP.7,10
Patient cases that had unplanned readmission within 30 postoperative days were individually reviewed, with the cause of readmission documented in the NSQIP through ICD-9 codes. The time to readmission (in days) was determined for each case. Reasons for readmission were categorized based on whether they were related to the ankle surgical site. Among unplanned readmissions for reasons unrelated to the surgical site, the reasons were classified by organ system for ease of interpretation.
Multivariable logistic regression models were constructed to determine the preoperative risk factors for unplanned readmission and any postoperative adverse events. Covariates included in the models were age, sex, CCI ≥4, ASA class ≥3, diabetes, hypertension, any pulmonary comorbidity, any cardiac comorbidity, history of smoking, preoperative functional status, open fracture, obesity class, and trimalleolar fracture versus other fracture types. These clinical thresholds for the CCI and ASA class have been established in previous studies using the NSQIP for facilitating the use of the CCI and ASA class as dichotomous risk predictors.8,9 Odds ratios with 95% confidence intervals were reported. Statistical significance was set at P < .05. Analysis was performed using SPSS 22 (IBM Corp, Armonk, NY, USA).
Results
In our cohort of 5056 patients, a history of diabetes was present in 11.8% of patients, and 26.9% had a history of smoking within the past year. In terms of the fracture type, 3.3% were open fractures, and 27.3% were trimalleolar fractures (Table 1).
Table 1.
Preoperative Patient Characteristics.
| n (%) | |
|---|---|
| Overall | 5056 (100.0) |
| Age, y | |
| <50 | 2362 (46.7) |
| 50-69 | 1962 (38.8) |
| ≥70 | 732 (14.5) |
| Sex | |
| Female | 3071 (60.7) |
| Male | 1985 (39.3) |
| Obesity class | |
| Nonobese (<30 kg/m2) | 2704 (53.5) |
| Obese I (30-34.9 kg/m2) | 1244 (24.6) |
| Obese II (35-39.9 kg/m2) | 663 (13.1) |
| Obese III (≥40 kg/m2) | 445 (8.8) |
| Modified Charlson comorbidity index | |
| 0-1 | 2400 (47.5) |
| 2-3 | 1715 (33.9) |
| ≥4 | 941 (18.6) |
| Anesthesia type | |
| General | 4420 (87.4) |
| Regional/spinal/epidural | 479 (9.5) |
| Other | 157 (3.1) |
| American Society of Anesthesiologists class ≥3 | 1429 (28.3) |
| History of diabetes | 595 (11.8) |
| History of hypertension | 1693 (33.5) |
| History of pulmonary disease | 265 (5.2) |
| History of cardiac disease | 15 (0.3) |
| History of smoking | 1360 (26.9) |
| Chronic steroid use | 84 (1.7) |
| Nonindependent functional status | 204 (4.0) |
| Open fracture | 167 (3.3) |
| Fracture type | |
| Medial malleolar | 248 (4.9) |
| Lateral malleolar | 937 (18.5) |
| Bimalleolar | 1732 (34.3) |
| Trimalleolar | 1379 (27.3) |
| Unspecified | 760 (15.0) |
The overall postoperative adverse event rate was 5.2%. Complications classified as major adverse events occurred at a rate of 3.2%, and 2.8% of patients had minor adverse events (Table 2). Among major adverse events, the most common were return to the operating room (1.4%), pneumonia (0.5%), and deep vein thrombosis (0.5%). There were 116 (2.3%) unplanned readmissions within 30 days.
Table 2.
Postoperative Adverse Events.
| Outcome | n (%) |
|---|---|
| ≥1 adverse event(s) | 262 (5.2) |
| Any major adverse event(s) | 161 (3.2) |
| Death | 10 (0.2) |
| Wound dehiscence | 14 (0.3) |
| Pneumonia | 23 (0.5) |
| Unplanned reintubation | 14 (0.3) |
| Ventilator >48 h | 14 (0.3) |
| Acute renal failure/insufficiency | 4 (0.1) |
| Coma >24 h | 0 (0.0) |
| Stroke/cerebrovascular accident | 2 (0.0) |
| Deep vein thrombosis | 23 (0.5) |
| Pulmonary embolism | 12 (0.2) |
| Cardiac arrest | 4 (0.1) |
| Myocardial infarction | 7 (0.1) |
| Sepsis/septic shock | 14 (0.3) |
| Return to operating room | 73 (1.4) |
| Any minor adverse event(s) | 141 (2.8) |
| Surgical site infection | 63 (1.2) |
| Urinary tract infection | 48 (0.9) |
| Blood transfusion | 37 (0.7) |
| Unplanned readmission | 116 (2.3) |
The 116 (2.3%) unplanned readmissions occurred at a mean of 15.8 days postoperatively (Table 3). Of these 116 unplanned readmissions, 49 (42.2%) were for reasons related to the surgical site, most commonly deep space surgical site or hardware infection (n = 15), superficial surgical site infection (n = 13), and wound disruption or nonhealing (n = 8). Sixty (51.7%) readmissions were for reasons unrelated to the surgical site. Among these, cardiac arrhythmia or other cardiac disorders (n = 10) were most commonly implicated, followed by pulmonary disorders or infections (n = 9) and neurological or psychiatric disorders including postoperative delirium (n = 8).
Table 3.
Reasons for and Timing of Unplanned Readmissions.
| n (%) | Mean Time to Readmission, d | |
|---|---|---|
| Total unplanned readmissions | 116 (100.0) | 15.8 |
| Unplanned readmission related to surgical site | 49 (42.2) | 18.1 |
| Deep space surgical site/hardware infection | 15 (12.9) | 18.3 |
| Superficial surgical site infection | 13 (11.2) | 18.5 |
| Wound disruption/nonhealing | 8 (6.9) | 23.1 |
| Acute postoperative pain | 6 (5.2) | 2.5 |
| Fracture nonunion/malunion | 3 (2.6) | 20.7 |
| Other hardware complication | 3 (2.6) | 27.0 |
| Heel pressure ulcer | 1 (0.9) | 27.0 |
| Unplanned readmission unrelated to surgery | 60 (51.7) | 14.4 |
| Cardiac arrhythmia/disorder | 10 (8.6) | 13.0 |
| Pulmonary disorder/infection | 9 (7.8) | 17.7 |
| Neurological/psychiatric disorder | 8 (6.9) | 13.4 |
| Gastrointestinal disorder/infection | 7 (6.0) | 14.9 |
| Urinary tract infection | 7 (6.0) | 17.7 |
| Deep vein thrombosis requiring therapy | 6 (5.2) | 14.7 |
| Pulmonary embolism | 6 (5.2) | 10.8 |
| Other unrelated trauma | 3 (2.6) | 16.0 |
| Sepsis/septic shock/other infectious disorder | 2 (1.7) | 8.0 |
| Metabolic derangement | 2 (1.7) | 12.0 |
| Unknown | 7 (6.0) | — |
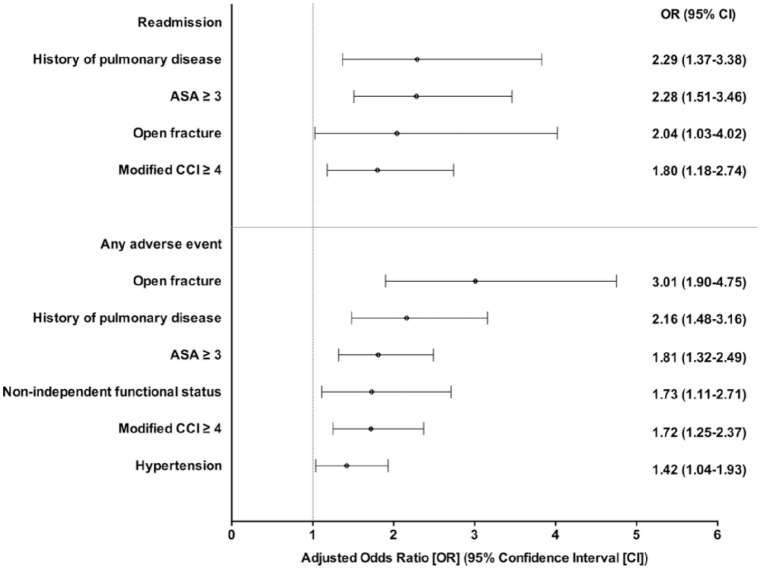
With multivariable logistic regression analyses, risk factors significantly associated with readmission were a history of pulmonary disease, ASA class ≥3, open fractures, and modified CCI ≥4 (Table 4). Risk factors that were significant predictors of postoperative adverse events included open fractures, a history of pulmonary disease, ASA class ≥3, preoperative nonindependent functional status, modified CCI ≥4, and hypertension (Figure 1).
Table 4.
Results of Multivariable Analyses for Risk Factors Associated With Any Adverse Event and Readmission.
| Outcome/Risk Factor | Odds Ratio (95% Confidence Interval) | P Value |
|---|---|---|
| Readmission | ||
| History of pulmonary disease | 2.29 (1.37-3.83) | .002 |
| ASA class ≥3 | 2.28 (1.51-3.46) | <.001 |
| Open fracture | 2.04 (1.03-4.02) | .040 |
| Modified CCI ≥4 | 1.80 (1.18-2.74) | .007 |
| Any adverse event | ||
| Open fracture | 3.01 (1.90-4.75) | <.001 |
| History of pulmonary disease | 2.16 (1.48-3.16) | <.001 |
| ASA class ≥3 | 1.81 (1.32-2.49) | <.001 |
| Nonindependent functional status | 1.73 (1.11-2.71) | .016 |
| Modified CCI ≥4 | 1.72 (1.25-2.37) | .001 |
| Hypertension | 1.42 (1.04-1.93) | .027 |
ASA, American Society of Anesthesiologists; CCI, Charlson comorbidity index.
Figure 1.
Forest plot of adjusted odds ratios (ORs) for significant predictors of readmission and any adverse event after ankle fracture surgery. Error bars indicate 95% confidence intervals (CIs). A 95% CI that does not include an OR of 1.0 indicates P < .05 and statistical significance.
Discussion
In this study of 5056 ankle fracture cases taken from a large prospectively collected multicenter database, we found that a majority of 30-day postoperative readmissions were for reasons unrelated to the surgical site. Risk factors associated with unplanned readmission included pulmonary disease, ASA class ≥3, and open fractures.
This study has several limitations. First, the NSQIP only provides postoperative data on readmissions and adverse events up to the 30th postoperative day. While this is aligned with most bundled payment models that include reimbursements for care for 30 postoperative days, it does not consider clinically important outcomes beyond this time window. In addition, the NSQIP does not include orthopaedic- and foot and ankle–specific outcomes, such as functional outcomes, range of motion, and pain scores. Furthermore, specific postoperative rehabilitation protocols and deep vein thrombosis prophylaxis regimens were also unavailable in the NSQIP.
In this study cohort, 53.3% of patients were ≥50 years of age, 11.8% of patients had a history of diabetes, and 28.3% of patients were ASA class ≥3. This is in line with cohorts in other ankle fracture studies. SooHoo et al 18 studied 57 183 patients with ankle fractures in the California state discharge database, and 50% of that cohort were older than 50 years of age, with a 10.4% prevalence of diabetes. Similarly, Basques et al 2 examined a cohort of 4412 patients with ankle fractures from the NSQIP from 2005 to 2012, and 37% of those patients were aged 40 to 59 years, 34% were aged ≥60 years, and 28% were ASA class ≥3. Lastly, McDonald et al 13 retrospectively reviewed 622 patients with ankle fractures from a single institution. In their cohort, more than 40% were aged ≥50 years, and 38% of patients were ASA class 3 or 4. Overall, data on our current cohort are reasonably consistent with those of previous ankle fracture studies in the literature.
The 30-day readmission rate reported in this study, 2.3%, is largely consistent with previously reported readmission rates.2,19 Only 42.2% of these readmissions were for reasons related to the surgical site, such as surgical site infections and wound disruption. Miller et al 14 previously reported on the risk factors associated with wound-related complications following ankle fracture surgery and identified peripheral vascular disease as the strongest predictor. It was not noted if these wound complications led to readmissions. Of note, the majority (51.7%) of readmissions in this cohort were for reasons unrelated to the surgical site, including cardiac disorders (8.6%), pulmonary disorders (7.8%), and neurological or psychiatric disorders (6.9%). To our knowledge, this is the first large-scale examination of the causes for readmission following ankle fracture surgery.
We found that the strongest risk factors associated with readmission were a history of pulmonary disease, ASA class ≥3, and open fractures. Our results are consistent with those of previous studies that have identified ASA classes to be significantly associated with higher readmission rates for ankle fractures 2 as well as other orthopaedic traumatic injuries. 16 Additionally, open ankle fractures have also been shown to be associated with increased postoperative morbidity relative to closed fractures. 18 To a lesser but still significant extent, we found that a modified CCI ≥4 was also associated with an increased readmission risk. Voskuijl et al 19 examined the association of the CCI with readmission following orthopaedic trauma injuries overall and found the CCI to account for 10% of the variation in readmissions, with each point increase in the CCI correlated to a 0.63% increase in postoperative readmissions.
We also found that 161 patients (3.2%) suffered a major adverse event, which was consistent with a previous analysis of the NSQIP. 2 Minor adverse events occurred in 141 (2.8%) patients, most commonly consisting of surgical site infections. The factors most significantly associated with any adverse event also included open fractures, higher ASA class, and a history of pulmonary disease. In addition, other risk factors with a significant association to adverse events included nonindependent functional status, modified CCI ≥4, and hypertension, suggesting that these factors should also be included as part of the preoperative risk assessment. At our tertiary academic level I trauma center, it is standard protocol to conduct a preoperative medical evaluation and risk stratification in elderly patients or those with medical comorbidities, whenever feasible. However, patients with ankle fractures identified to be at a higher risk for postoperative adverse events and readmission may benefit from close postdischarge medical follow-up and optimization.
In summary, these findings demonstrate that most readmissions following ankle fracture surgery are not directly related to the surgical site. Perioperative medical optimization and postdischarge medical follow-up may lead to decreased readmissions following the inpatient treatment of ankle fractures; however, future studies in this area are warranted.
Footnotes
This article was originally published as: Fu MC, Young K, Cody E, Schairer WW, Demetracopoulos CA, Ellis SJ. Most readmissions following ankle fracture surgery are unrelated to surgical site issues: an analysis of 5056 cases. Foot Ankle Orthop. 2017 Apr 7;2(2):2473011417695254. doi:10.1177/2473011417695254.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. American College of Surgeons. User guide for the 2013 ACS NSQIP participant use data file. Available at: http://site.acsnsqip.org/wp-content/uploads/2014/11/NSQIP.PUF_.ProcedureTargeted.UserGuide.2013.pdf. Accessed March 24, 2016.
- 2. Basques BA, Miller CP, Golinvaux NS, Bohl DD, Grauer JN. Morbidity and readmission after open reduction and internal fixation of ankle fractures are associated with preoperative patient characteristics. Clin Orthop Relat Res. 2015;473(3):1133–1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Basques BA, Toy JO, Bohl DD, Golinvaux NS, Grauer JN. General compared with spinal anesthesia for total hip arthroplasty. J Bone Joint Surg Am. 2015;97(6):455–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bohl DD, Fu MC, Gruskay JA, et al. “July effect” in elective spine surgery: analysis of the American College of Surgeons National Surgical Quality Improvement Program database. Spine (Phila Pa 1976). 2014;39(7):603–611. [DOI] [PubMed] [Google Scholar]
- 5. Centers for Medicare and Medicaid Services. Bundled Payments for Care Improvement (BPCI) initiative: general information. Available at: https://innovation.cms.gov/initiatives/bundled-payments/. Accessed July 10, 2016.
- 6. Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37(8):691–697. [DOI] [PubMed] [Google Scholar]
- 7. Fu MC, Buerba RA, Grauer JN. Preoperative nutritional status as an adjunct predictor of major postoperative complications following anterior cervical discectomy and fusion. Clin Spine Surg. 2016;29(4):167–172. [DOI] [PubMed] [Google Scholar]
- 8. Fu MC, D’Ambrosia C, McLawhorn AS, et al. Malnutrition increases with obesity and is a stronger independent risk factor for postoperative complications: a propensity-adjusted analysis of total hip arthroplasty patients. J Arthroplasty. 2016;31(11):2415–2421. [DOI] [PubMed] [Google Scholar]
- 9. Fu MC, Gruskay JA, Samuel AM, et al. Outpatient anterior cervical discectomy and fusion is associated with fewer short-term complications in one-and two-level cases: a propensity-adjusted analysis. Spine (Phila Pa 1976). Epub November 18, 2016. [DOI] [PubMed] [Google Scholar]
- 10. Garcia GH, Fu MC, Dines DM, Craig EV, Gulotta LV. Malnutrition: a marker for increased complications, mortality, and length of stay after total shoulder arthroplasty. J Shoulder Elbow Surg. 2016;25(2):193–200. [DOI] [PubMed] [Google Scholar]
- 11. Jameson SS, Augustine A, James P, et al. Venous thromboembolic events following foot and ankle surgery in the English National Health Service. J Bone Joint Surg Br. 2011;93(4):490–497. [DOI] [PubMed] [Google Scholar]
- 12. Mandi DM. Ankle fractures. Clin Podiatr Med Surg. 2012;29(2):155–186, vii. [DOI] [PubMed] [Google Scholar]
- 13. McDonald MR, Sathiyakumar V, Apfeld JC, et al. Predictive factors of hospital length of stay in patients with operatively treated ankle fractures. J Orthop Traumatol. 2014;15(4):255–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Miller AG, Margules A, Raikin SM. Risk factors for wound complications after ankle fracture surgery. J Bone Joint Surg Am. 2012;94(22):2047–2052. [DOI] [PubMed] [Google Scholar]
- 15. Ovaska MT, Makinen TJ, Madanat R, et al. Risk factors for deep surgical site infection following operative treatment of ankle fractures. J Bone Joint Surg Am. 2013;95(4):348–353. [DOI] [PubMed] [Google Scholar]
- 16. Sathiyakumar V, Molina CS, Thakore RV, Obremskey WT, Sethi MK. ASA score as a predictor of 30-day perioperative readmission in patients with orthopaedic trauma injuries: an NSQIP analysis. J Orthop Trauma. 2015;29(3):e127–e132. [DOI] [PubMed] [Google Scholar]
- 17. SooHoo NF, Eagan M, Krenek L, Zingmond DS. Incidence and factors predicting pulmonary embolism and deep venous thrombosis following surgical treatment of ankle fractures. Foot Ankle Surg. 2011;17(4):259–262. [DOI] [PubMed] [Google Scholar]
- 18. SooHoo NF, Krenek L, Eagan MJ, et al. Complication rates following open reduction and internal fixation of ankle fractures. J Bone Joint Surg Am. 2009;91(5):1042–1049. [DOI] [PubMed] [Google Scholar]
- 19. Voskuijl T, Hageman M, Ring D. Higher Charlson comorbidity index scores are associated with readmission after orthopaedic surgery. Clin Orthop Rel Res. 2014;472(5):1638–1644. [DOI] [PMC free article] [PubMed] [Google Scholar]