Abstract
Objectives
We carried out this work with the aim of assessing the effectiveness of a set of interventions over time for the administration of antibiotics.
Design
Prospective observational study.
Setting
Patients admitted to the emergency room and ICU of the hospital where the study was conducted are evaluated daily for some sociodemographic and clinical variables. Among them are some quality indicators, such as the time between the diagnosis of sepsis or septic shock until the start of the infusion of antibiotics. This indicator reflects several aspects related to a set of assistance measures (adequacy of antibiotic dispensation, rapid response team (RRT), sepsis care quality improvement program, antimicrobial management program, improvements in emergency department assistance).
Patients or participants
Patients with sepsis or septic shock were admitted to the ICU of a university and public hospital in southern Brazil.
Main variables of interest
The time between the diagnosis of sepsis or septic shock and the beginning of the infusion of antibiotics.
Results
Between 2013 and 2018, 1676 patients were evaluated. The mean time for antibiotic infusion decreased from 6.1 ± 8.6 hours to 1.7 ± 2.9 hours (p < 0.001). The percentage of patients who received antibiotics in the first hour increased from 20.7 to 59.0% (p < 0.001).
Conclusion
In this study, we demonstrated that a set of actions adopted in a large tertiary hospital was associated with decreased time to start antibiotic therapy in septic patients.
How to cite this article
Moraes RB, Haas JS, Vidart J, Nicolaidis R, Deutschendorf C, Moretti MMS, et al. A Coordinated and Multidisciplinary Strategy can Reduce the Time for Antibiotics in Septic Patients at a University Hospital. Indian J Crit Care Med 2023;27(7):465–469.
Keywords: Antibiotic, Quality improvement, Sepsis, Septic shock
Highlights
Adequacy of dispensing antibiotics by the pharmacy, Implementation of a rapid response team (RRT), creation of an intrahospital program to combat sepsis (IPCS), antimicrobial stewardship program (ASP) by physicians and pharmacists and assistance improvements in the emergency department were the strategies used to reduce the time from 6.1 to 1.7 hours.
Introduction
Sepsis is described by organ dysfunction that occurs through a response to infection, being one of the main causes of death in the world. Afterwards, an inflammatory response in the host is triggered, releasing meters that can be used as biomarkers for diagnosing sepsis.1,2 Sepsis is an important public health problem, given the increased incidence, high mortality and costs associated with its treatment. The management of sepsis patients is based on the adequacy of interventions and includes (1) early recognition, (2) early and adequate empirical administration of antibiotics, (3) control of the infectious focus, and (4) volume resuscitation with intravenous fluids and use vasoactive drugs when needed.3 Observational studies have shown that delaying the administration of antibiotic therapy appears to significantly increase mortality for each hour of delay.4,5 Among all recommended interventions, studies suggest that the initiation of antibiotic therapy appears to have the greatest impact on sepsis mortality.6,7 Although there is controversy about how early the administration should be performed, it is difficult to argue against starting antibiotics as early as possible after the diagnosis of sepsis.7,8 Thus, the guidelines of the Survival Sepsis Campaign establish as a strong recommendation for the infusion of intravenous antibiotics in the first hour after diagnosis of sepsis.3 In countries with low- and middle-income or health systems lacking resources and organization, interventions that must be carried out to implement early antibiotic therapy and its effects are poorly studied.9 In Brazil, public hospitals, when compared with private hospitals, are an independent risk factor for sepsis-related mortality.10 Delays in antimicrobial administration are common and represent a marker in the overall quality of care. However, despite the early administration of antibiotics being a strong recommendation, the effort to reduce the time of initiation of antibiotics is challenging.11 The improvement of the processes that lead to more agile, and early administration is the result of a multidisciplinary effort and involves nurses, doctors, and pharmacists.12 Our study prospectively evaluated the effect of a set of interventions adopted in a public university hospital to decrease the time to initiate antibiotic therapy in septic patients.
Methods
Prospective cohort study conducted at a university hospital. This study was conducted as recommended by the Declaration of Helsinki and approved by the Research Ethics Committee of Hospital de Clínicas de Porto Alegre (HCPA, number: 2016-0317). As this is an observational study, it was not considered necessary to apply an informed consent form.
Patients diagnosed with sepsis (infection with organ dysfunction) and septic shock (sepsis with hypotension refractory to fluid replacement) were included according to the SEPSIS-2 consensus13 and hospitalized in the ICU diagnosed with sepsis in the wards, emergency department (ED) or in the ICU between March 2013 and December 2018. Patients under 18 years old, with readmission in the same period of the study, or with an indication of therapeutic limitation were excluded.
Epidemiological data, APACHE II, SAPS 3, the time of onset of antimicrobials after the diagnosis of sepsis, and mortality rate were collected. Time-related data for the diagnosis of sepsis and antimicrobial treatment were obtained from the electronic medical records. Antibiotic initiation time was calculated as the time difference in hours elapsed between registering in the medical record of sepsis or septic shock and the start of the infusion of the first dose of antibiotics intravenously, as registered by the nurse.
Patients who were previously using antibiotics and those who had switched its antimicrobial regimen due to a new episode of sepsis were excluded. And HCPA is a public, tertiary, and university hospital. Approximately, 95% of consultations are performed by the public health system, being a regional reference center for highly complex consultations. The adult ICU consists of 45 beds with the hospital having approximately 600 beds for adults. Since 2013, HCPA has instituted several measures to reduce the time for an infusion of the first dose of antibiotics in septic patients. The measures implemented are as follows:
Adequacy of dispensing antibiotics by the pharmacy. The Hospital de Clínicas de Porto Alegre has several surgical, clinical, and psychiatric wards for adult patients, an ED on the ground floor, and an adult ICU on the 13th floor. Until 2013, to obtain the prescribed medications, a nursing technician had to travel to the central pharmacy on the 9th floor. The emergency room satellite pharmacy started its activities in 2013. The ICU has had a satellite pharmacy since 2009. In addition, an automated medication supply system was implemented between 2013 and 2018 (Pyxis®) in all wards. An automated medication supply system allows the storage and organization of medication dispensing accessed by authorized employees with a barcode reader. The set of these interventions ended with the displacement of the nursing technician to the central pharmacy.
Implementation of an RRT. The creation of the RRT was a decision by the institution's medical administration to improve emergency care in adult wards.14,15 The RRT is composed of intensive care physicians, working 24 hours a day, 7 days a week, being triggered by the nurse responsible for each ward through pre-established clinical triggers. The RRT defines the suspicion of sepsis as a trigger and is responsible for the application of the initial sepsis management protocol that includes the prescription of empirical antibiotics and the definition of ICU admission.
Creation of the IPCS. The IPCS is composed of five doctors (three intensivists, an emergency physician, and a doctor from the RRT), three nurses, and a nursing student. The program collects patient data and recommends assistance policies and conduct to the hospital's medical management. The program does not act directly on patient care, which is carried out by the RRT, emergency responders, intensivists, and other professionals at the institution. The IPCS monitors variables related to the quality of care (e.g., time for antibiotic therapy), adapts processes, and identifies barriers to the care of septic patients. Also, the program institutes and updates sepsis protocol, and operates in continuing education through face-to-face classes and distance learning, targeting all employees who work with septic patients, such as doctors, nurses, nursing technicians, pharmacists, nutritionists, physiotherapists, and technicians who collect blood for laboratory tests. During the study period, structured and repeated training was conducted annually with a focus on the nursing team, highlighting the importance of nurses at the bedside for the early identification of septic patients through triggers defined in institutional sepsis protocol, as well as the importance of administration of the immediate antibiotic.
Antimicrobial Stewardship Program. The ASP is composed of infectiologists, intensivists, pediatricians, nurses, and pharmacists. It works by monitoring the bacterial resistance profile of the hospital, generating annual reports on them, making and updating protocols for the use of antimicrobials, and providing advice to an infectiologist to decide on the use of antibiotics on a full-time basis. During the study period, Hospital Infection Control Committee (HICC) started to audit all antimicrobials prescribed in the hospital within a maximum of 24 hours to assess the adequacy of the prescription. Over these years, there has been a gradual increase in the rate of the adequacy of antimicrobial prescriptions, and is currently 85%.
Assistance improvements in the ED. In the ED, several logistical interventions were adopted, such as the adoption of time to start antibiotic therapy as a marker of care quality, the adoption of the PDSA methodology (Plan, Do, Study, Act),16 and signaling septic patients in electronic medical records.
Statistical Analysis
Statistical analysis was performed using the SPSS 16 program. Descriptive analysis was performed, and the data are presented as means and standard deviations or as medians and interquartile ranges for continuous variables and absolute and relative frequencies for categorical variables. To identify the differences between the variables, the Chi-square or Fisher's exact tests were performed for categorical variables, and the Mann–Whitney test for continuous variables. The level of significance was 0.05.
Results
Between March 2013 and December 2018, 2513 patients with sepsis or septic shock were admitted to the ICU were identified. Of these, 837 patients received antibiotics before meeting the criteria for sepsis or septic shock, while 1,676 patients received antibiotics after meeting these criteria. The profile of patients who received antibiotics after the diagnosis of sepsis or septic shock is given in Table 1. The interventions used to achieve a reduction in the time of antibiotic onset are described in Box. The mean time to start of the antibiotic infusion decreased from 6.13 ± 8.6 hours to 1.7 ± 2.9 hours between 2013 and 2018 (p < 0.001) (Fig. 1). The percentage of patients who received antibiotics in the first hour after the diagnosis of sepsis increased from 20.7 to 59.0% (p < 0.001) (Fig. 2). No decrease in lethality was observed during the study period (52% vs 54%).
Table 1.
Patient characteristics
| Sepsis (n = 805) | Septic shock (n = 871) | |
|---|---|---|
| Age (mean ± SD) | 58.8 ± 17.2 | 60.4 ± 16.7 |
| Sex (% male) | 54.4 | 53.8 |
| APACHE II (mean ± SD) | 21.5 ± 7.1 | 26.9 ± 8.9 |
| SOFA (mean ± SD) | 4.6 ± 3 | 8.6 ± 3 |
| SAPS 3 (mean ± SD) | 65.8 ± 14.1 | 71.4 ± 13.5 |
| MV (%) | 43.8 | 83.4 |
| Infectious focus | ||
| Lung (%) | 52.6 | 53.9 |
| Abdomen (%) | 17.05 | 21.4 |
| Urinary tract (%) | 11.1 | 6.3 |
| Catheter (%) | 1 | 2.1 |
| Others (%) | 17.8 | 16.3 |
| Treated outside the ICU (%)* | 48.9 | 13.6 |
| Coming from ED (%) | 49.7 | 47.1 |
APACHE II, acute physiology and chronic health evaluation II; ED, emergency department; MV, mechanical ventilation; SAPS 3 score, simplified acute physiology score; SOFA score, the sequential organ failure assessment score;
*Patients whose treatment took place outside the ICU (ED or ward) in the first 24 hours after diagnosis of sepsis or septic shock
Box: Measures used to improve the time to start antibiotic therapy
Rapid response team
Pharmacy interventions
Satellite Pharmacies (ICU and Emergency)
Pyxis® (Automatic medication dispensers)
Interventions of the Sepsis Care Quality Improvement Program
Sepsis protocol
Face-to-face classes, distance learning
Continuous monitoring of results and management of protocols
Interventions of the Antimicrobial Stewardship Program
Monitoring of the hospital's microbiological profile
Protocols for the use of antimicrobials
Full-time antimicrobial decision-making advice
Emergency department interventions
Adoption of time for antibiotic therapy as a care indicator
Adoption of the PDSA methodology (Plan, Do, Study, Act)
Signaling in the electronic system of septic patients
Fig. 1.
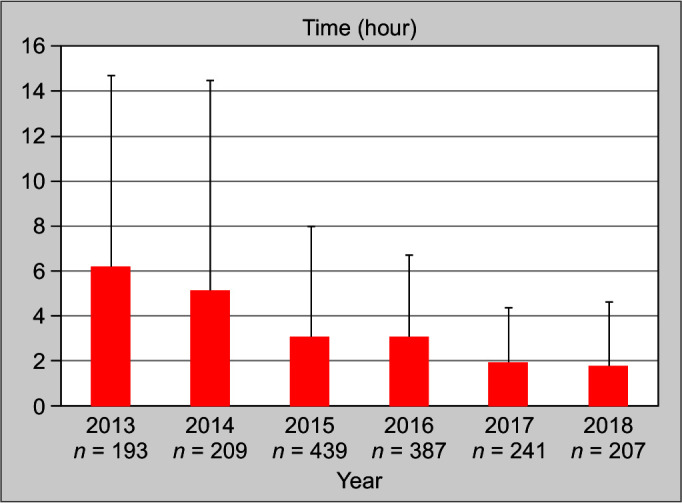
Time to start antibiotic therapy in septic patients
Fig. 2.
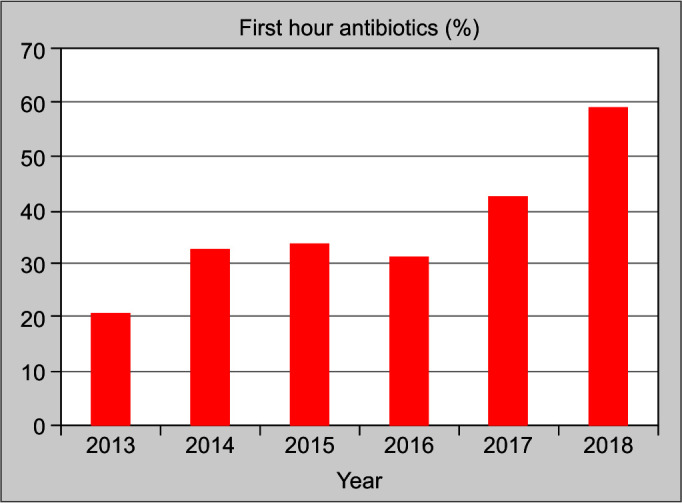
The percentage of patients who received antibiotics in the first hour increased over time
Discussion
In this cohort, the adoption of a set of measures was associated with a significant decrease in the time to start antibiotic therapy in septic patients and an increase in the percentage of adequacy to the recommendation to start antibiotic administration in 1 hour. These measures demand integrated actions from different services, involving the Sepsis Care Quality Improvement Program, RRT, ASP, Pharmacy and Emergency Department, as well as the multidisciplinary involvement of doctors, nurses, and pharmacists. Our results are similar to a previous study, whose mean time for an infusion of antibiotics decreased from 6 hours to 1.4 hours.17 Our study was not designed to indicate which measures individually are capable of speeding up the time for the infusion of antibiotics. Some studies emphasize the importance of prompt availability of the drug in the unit where the patient is hospitalized,18,19 what was addressed in our intervention with the availability of satellite pharmacies and the use of an automated medication supply system (Pyxis®). Other studies emphasize the importance of optimizing the electronic prescription and continuing education system.20,21 The association between early antibiotic use and decreased mortality observed in several studies supports the SSC recommendation3 for patients with sepsis or septic shock.5,22,23 Despite this evidence, there is concern that the early use of antimicrobials is associated with unnecessary use, especially in patients with low-severity infections, and with the induction of microbial resistance.24 Some authors are concerned that the obsession with starting antibiotics within 1 hour is a “septic hysteria.”25 Concerns about the unnecessary use of antibiotics seem to be relevant in places where the prevalence of septic patients of low severity and low mortality and who have effective health systems, is the most common scenario in developed countries. However, our data show a different scenario, typical of a developing country. In low- and middle-income countries, where most cases of sepsis and septic shock are found, the diagnosis of sepsis and recommended initial interventions are delayed, which appears to be a consequence of the low capacity of precarious health systems to effectively care for these patients.11 However, regardless of the controversy about the need to administer antibiotics as early as possible, time to start antibiotic therapy is an indicator of quality, and the reduction in this time seems to reflect the ability to improve care for septic patients.4,6 Our study supports the principle of health care improvement and the coordination of several measures was associated with reduced time to administer antibiotics. Although studies demonstrate the benefits of optimizing antibiotic prescriptions quickly, there is a lack of studies describing how to achieve this goal.26 The early start of antimicrobials seems to be a simple intervention, but several processes need to be aligned from the prescription to the infusion of the antibiotic so that this occurs in the shortest possible time. The implementation of the RRT optimizes the communication between the prescribing physician and the nursing team responsible for the infusion of the antibiotic.27 Structural and logistical measures, such as the implementation of satellite pharmacies and automated medication supply system, streamline the delivery of antibiotics to the location and to the patient who should receive the medication, corroborating the reduction and optimization of the workload of the pharmacy and nursing staff.28 The adoption of protocols and consultancy carried out by ASP makes it possible to standardize prescriptions, optimize the availability of the drug and make the quickest decision on the best antibiotic therapy to be employed.29 In the ED, the implementation of assistance improvements made it possible to prioritize the identification and treatment of septic patients, increasing the visibility of the problem and the engagement of professionals in the care of these patients. Education is relevant so that all professionals working in the process are aware of the importance of administering antibiotics as quickly as possible, feeling engaged in the patient care process, avoiding delaying the time of the antibiotic infusion, or postponing its use delaying the patient's transfer to the ICU.26 Continuing education was offered to all professionals at the institution who participate in the care of septic patients, but there was particular attention in ensuring the training of nurses and nursing technicians. These professionals are fundamental in the evaluation and therapeutic implementation of septic patients. Nursing professionals are those who are in the longest contact with the patient, thus being able to recognize signs of sepsis earlier. They are also the professionals responsible for the initial application of care, such as the infusion of antibiotics. Protocols centered on the nurse's performance in the treatment of sepsis have been associated in several studies with improved patient care, among these improvements and the reduction of antibiotic administration time.30–32
Our study has limitations. As this is an observational study, it is not possible to state that there is a causal relationship between the interventions implemented during the study period and the decreased time for infusion of antibiotic therapy, and it is possible to infer an association between the interventions and the outcome. In addition, other interventions not measured, but adopted during the study period, as well as the evolution of patient care, may also be associated with the results. The interventions adopted at the institution were implemented simultaneously and gradually, making it impossible to measure the individual effect of each intervention. Unlike studies that demonstrate an association between decreased mortality and early prescription, we did not observe this in our study.5,6 We speculate that although we have shortened the time to use antibiotics, a significant percentage of patients do not receive antibiotics in the first hour. In addition, all patients studied were admitted to the ICU and the severity was very high. Finally, our data indicate that we are still flawed in early diagnosis, which is the biggest trigger that leads to early interventions.33
Conclusion
The adoption of a package of measures involving various services and professionals was associated with a significant decrease in the time to start the first dose of antibiotics and increased the percentage of patients with sepsis or septic shock who received antibiotics within 1 hour at a university hospital in a developing country.
Orcid
Rafael Barberena Moraes https://orcid.org/0000-0001-6631-7260
Jaqueline Sangiogo Haas https://orcid.org/0000-0001-9721-9903
Josi Vidart https://orcid.org/0000-0003-2392-6247
Rafael Nicolaidis https://orcid.org/0000-0003-1981-471X
Caroline Deutschendorf https://orcid.org/0000-0002-6114-824X
Miriane Melo Silveira Moretti https://orcid.org/0000-0002-5365-5997
Gilberto Friedman https://orcid.org/0000-0001-9369-2488
Daiandy Silva https://orcid.org/0000-0001-8421-4716
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Azim A. Presepsin: a promising biomarker for sepsis [Internet]. 2021;25(2):117–118. doi: 10.5005/jp-journals-10071-23741. www.ijccm.org. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gupta R, Ray S. Advances in microcirculatory assessment: a game changer in sepsis management or the latest fad? Indian J Crit Care Med. 2022;26(3):261–263. doi: 10.5005/jp-journals-10071-24162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43(3):304–377. doi: 10.1007/s00134-017-4683-6. [DOI] [PubMed] [Google Scholar]
- 4.Seymour CW, Gesten F, Prescott HC, Friedrich ME, Iwashyna TJ, Phillips GS, et al. Time to treatment and mortality during mandated emergency care for sepsis. N Engl J Med. 2017;376(23):2235–2244. doi: 10.1056/NEJMoa1703058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006;34(6):1589–1596. doi: 10.1097/01.CCM.0000217961.75225.E9. [DOI] [PubMed] [Google Scholar]
- 6.Ferrer R, Martin-Loeches I, Phillips G, Osborn TM, Townsend S, Dellinger RP, et al. Empiric antibiotic treatment reduces mortality in severe sepsis and septic shock from the first hour: results from a guideline-based performance improvement program. Crit Care Med. 2014;42(8):1749–1755. doi: 10.1097/CCM.0000000000000330. [DOI] [PubMed] [Google Scholar]
- 7.Vazquez-Guillamet C, Scolari M, Zilberberg MD, Shorr AF, Micek ST, Kollef M. Using the number needed to treat to assess appropriate antimicrobial therapy as a determinant of outcome in severe sepsis and septic shock. Crit Care Med. 2014;42(11):2342–2349. doi: 10.1097/CCM.0000000000000516. [DOI] [PubMed] [Google Scholar]
- 8.Spiegel R, Farkas JD, Rola P, Kenny JE, Olusanya S, Marik PE, et al. The 2018. Surviving sepsis campaign's treatment bundle: when guidelines outpace the evidence supporting their use. Ann Emerg Med. 2019;73(4):356–358. doi: 10.1016/j.annemergmed.2018.06.046. [DOI] [PubMed] [Google Scholar]
- 9.Abe T, Kushimoto S, Tokuda Y, Phillips GS, Rhodes A, Sugiyama T, et al. Implementation of earlier antibiotic administration in patients with severe sepsis and septic shock in Japan: a descriptive analysis of a prospective observational study. CritCare. 2019;23(1):360. doi: 10.1186/s13054-019-2644-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Machado FR, Cavalcanti AB, Bozza FA, Ferreira EM, Angotti Carrara FS, Sousa JL, et al. The epidemiology of sepsis in Brazilian intensive care units (the Sepsis PREvalence Assessment Database, SPREAD): an observational study. Lancet Infect Dis. 2017;17(11):1180–1189. doi: 10.1016/S1473-3099(17)30322-5. [DOI] [PubMed] [Google Scholar]
- 11.Conde KA, Silva E, Silva CO, Ferreira E, Freitas FG, Castro I, et al. Differences in sepsis treatment and outcomes between public and private hospitals in Brazil: a multicenter observational study. PLoS One. 2013;8(6):e64790. doi: 10.1371/journal.pone.0064790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Delawder JM, Hulton L. An interdisciplinary code sepsis team to improve sepsis-bundle compliance: a quality improvement project. J Emerg Nurs. 2020;46(1):91–98. doi: 10.1016/j.jen.2019.07.001. [DOI] [PubMed] [Google Scholar]
- 13.MacMillan A, Rudinsky D, Han G, Elliott JO, Jordan K. Multidisciplinary approach to improve sepsis outcomes. J Healthc Qual. 2019;41(4):220–227. doi: 10.1097/JHQ.0000000000000166. [DOI] [PubMed] [Google Scholar]
- 14.Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 200 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003;31(4):1250–1256. doi: 10.1097/01.CCM.0000050454.01978.3B. [DOI] [PubMed] [Google Scholar]
- 15.Boniatti MM, Azzolini N, Viana MV, Ribeiro BS, Coelho RS, Castilho RK, et al. Delayed medical emergency team calls and associated outcomes. Crit Care Med. 2014;42(1):26–30. doi: 10.1097/CCM.0b013e31829e53b9. [DOI] [PubMed] [Google Scholar]
- 16.Salvatierra G, Bindler RC, Corbett C, Roll J, Daratha KB. Rapid response team implementation and in-hospital mortality*. Crit Care Med. 2014;42(9):2001–2006. doi: 10.1097/CCM.0000000000000347. [DOI] [PubMed] [Google Scholar]
- 17.Coury J, Schneider JL, Rivelli JS, Petrik AF, Seibel E, D’Agostini B, et al. Applying the Plan-Do-Study-Act (PDSA) approach to a large pragmatic study involving safety net clinics. BMC Health Serv Res. 2017;17(1):411. doi: 10.1186/s12913-017-2364-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McGregor C. Improving time to antibiotics and implementing the “Sepsis 6”. BMJ Qual Improv Rep. 2014;2(2):u202548–w1443. doi: 10.1136/bmjquality.u202548.w1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stephen G, Moran D, Broderick J, Shaikh HA, Tschudy MM, Connors C, et al. A quality improvement intervention reduces the time to administration of stat medications. Pediatr Qual Saf. 2017;2(3):e021. doi: 10.1097/pq9.0000000000000021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Amado VM, Vilela GP, Queiroz A,, Jr., Amaral ACK. Effect of a quality improvement intervention to decrease delays in antibiotic delivery in pediatric febrile neutropenia: a pilot study. J Crit Care. 2011;26(1):103–112. doi: 10.1016/j.jcrc.2010.05.034. [DOI] [PubMed] [Google Scholar]
- 21.Matthews PC, Wangrangsimakul T, Borthwick M, Williams C, Byren I, Wilkinson D. Electronic prescribing: reducing delay to first dose of antibiotics for patients in intensive care. BMJ Qual Improv Rep. 2014;2(2):u202241–w1120. doi: 10.1136/bmjquality.u202241.w1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gaieski DF, Mikkelsen ME, Band RA, Pines JM, Massone R, Furia FF, et al. Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. Crit Care Med. 2010;38(4):1045–1053. doi: 10.1097/CCM.0b013e3181cc4824. [DOI] [PubMed] [Google Scholar]
- 23.Puskarich MA, Trzeciak S, Shapiro NI, Arnold RC, Horton JM, Studnek JR, et al. Association between timing of antibiotic administration and mortality from septic shock in patients treated with a quantitative resuscitation protocol. Crit Care Med. 2011;39(9):2066–2071. doi: 10.1097/CCM.0b013e31821e87ab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Infectious Diseases Society of America (IDSA) POSITION STATEMENT: Why IDSA Did Not Endorse the Surviving Sepsis Campaign Guidelines. Clin Infect Dis. 2018;66(10):1631–1635. doi: 10.1093/cid/cix997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Singer M, Inada-Kim M, Shankar-Hari M. Sepsis hysteria: excess hype and unrealistic expectations. Lancet. 2019;394(10208):1513–1514. doi: 10.1016/S0140-6736(19)32483-3. [DOI] [PubMed] [Google Scholar]
- 26.Emerson BL, Prozora S, Jacob A, Clark K, Kotrady D, Edwards L, et al. An initiative to decrease time to antibiotics for patients with fever and neutropenia. Am J Med Qual. 2019;34(2):158–164. doi: 10.1177/1062860618792305. [DOI] [PubMed] [Google Scholar]
- 27.Khanina A, Cairns KA, McGloughlin S, Orosz J, Bingham G, Dooley M, et al. Improving sepsis care for hospital inpatients using existing medical emergency response systems. Infect Dis Health. 2020 doi: 10.1016/j.idh.2019.10.003. [DOI] [PubMed] [Google Scholar]
- 28.Almalki O, Levine AR, Turner E, Newman K, DeMoya M, Lee J, et al. Impact of a multidisciplinary bundle on time to antibiotic administration in septic SICU patients. J Intensive Care Med. 2017;32(8):494–499. doi: 10.1177/0885066616656344. [DOI] [PubMed] [Google Scholar]
- 29.Rosa R, Zavala B, Cain N, Anjan S, Aragon L, Abbo LM. Antimicrobial Stewardship program implementation of a quality improvement intervention using real-time feedback and an electronic order set for the management of Staphylococcus aureus bacteremia. Infect Control Hosp Epidemiol. 2018;39(3):346–349. doi: 10.1017/ice.2017.325. [DOI] [PubMed] [Google Scholar]
- 30.Kumar P, Jordan M, Caesar J, Miller S. Improving the management of sepsis in a district general hospital by implementing the ‘Sepsis Six’ recommendations. BMJ Qual Improv Rep. 2015;4(1):u207871–w4032. doi: 10.1136/bmjquality.u207871.w4032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mattison G, Bilney M, Haji-Michael P, Cooksley T. A nurse-led protocol improves the time to first dose intravenous antibiotics in septic patients post chemotherapy. Support Care Cancer. 2016;24(12):5001–5005. doi: 10.1007/s00520-016-3362-4. [DOI] [PubMed] [Google Scholar]
- 32.Bruce HR, Maiden J, Fedullo PF, Kim SC. Impact of nurse-initiated ED sepsis protocol on compliance with sepsis bundles, time to initial antibiotic administration, and in-hospital mortality. J Emerg Nurs. 2015;41(2):130–137. doi: 10.1016/j.jen.2014.12.007. [DOI] [PubMed] [Google Scholar]
- 33.Ferrer R, Martinez ML, Goma G, Suarez D, Alvarez-Rocha L, de la Torre M, et al. Improved empirical antibiotic treatment of sepsis after an educational intervention the ABISS-Edusepsis study. Crit Care. 2018;22(1):167. doi: 10.1186/s13054-018-2091-0. [DOI] [PMC free article] [PubMed] [Google Scholar]


