Abstract
Background
Early identification of patients with an emergent large vessel occlusion (ELVO) ischemic stroke is crucial in the Emergency Department (ED), as they are the ideal candidates for endovascular therapy.
With this study, we have attempted to use Vision, Aphasia, Neglect (VAN) screening tool in the ED for rapid identification of ELVO ischemic stroke and compared its performance with the National Institute of Health Stroke Severity (NIHSS) scale.
Materials and methods
A prospective observational study was conducted in the ED of a tertiary care hospital over 18 months among all suspected stroke patients. Vision, aphasia, neglect and NIHSS scores were calculated on arrival. Magnetic resonance imaging + magnetic resonance angiography (MRI + MRA) were taken as gold standard.
Results
This study found that VAN identified ELVO with 85.19% sensitivity (p-value < 0.0001), 88.64% specificity (p-value < 0.0001), and 87% diagnostic accuracy, with respect to the gold standard test. Vision, aphasia, neglect had a positive predictive value (PPV) and negative predictive value (NPV) of 82.14% and 90.7%, respectively. Time taken to perform VAN score in the ED was on average 2 minutes. National Institute of Health Stroke Severity detected ELVO with a sensitivity of 88%, specificity of 51.11%, a PPV of 53.33%, and a NPV of 88.4%. Diagnostic accuracy was 66%, and it took approximately 5 minutes to perform. When both scores were applied together for ELVO detection, NPV was 100%.
Conclusion
Vision, Aphasia, Neglect score as well as NIHSS scale are both tools for clinical prediction of ELVO with VAN having a better diagnostic accuracy and utility as a screening tool in the ED.
How to cite this article
Krishnan A, Srinivasarangan M, Jagadish S, Bheemanna AS, Sivasankar A. The Efficacy of Vision, Aphasia, Neglect Assessment in Predicting Emergent Large Vessel Occlusion in Patients Presenting with a Cerebrovascular Accident to the Emergency Department. Indian J Crit Care Med 2023;27(7):475–481.
Keywords: Aphasia, Cerebrovascular accident, Emergency Department, Emergent large vessel occlusion stroke, Magnetic resonance angiography, Magnetic resonance imaging, National Institute of Health Stroke Severity, Neglect, Vision
Highlights
Large vessel occlusion stroke is a neurological emergency which requires early detection and endovascular intervention.
Vision, Aphasia, Neglect (VAN) assessment is a novel screening tool to clinically detect emergent large vessel occlusion (ELVO) stroke. With this study, we attempt to study the utility of VAN score in the Emergency Department (ED) for the same.
Introduction
Stroke is an epidemic of the modern times. Globally, every one in four people over the age of 25 today have a probability of having at least one stroke in their lifetime.1 It is currently the second leading cause of death worldwide, exceeded only by ischemic heart disease. It is also one of the leading causes of adult disability, with 116 million years of healthy life lost to this disease annually.2,3 Today, two-thirds of the entire stroke disease burden is contributed by low- and middle-income countries, including India.1 The recent COVID-19 outbreak has increased the risk of occurrence of ischemic strokes.4,5
By definition, a stroke or a cerebrovascular accident (CVA) is the sudden onset of a neurologic deficit resulting from a vascular pathology; on an average 85% CVAs are ischemic and 15% are hemorrhagic.6 Acute ischemic stroke is a time-critical7 condition with a significant residual neurological burden. Hence, early recognition is one of the key concepts in the “Chain of Survival” as described by the American Heart Association (AHA)/American Stroke Association guidelines.8 Recent therapeutic advances such as endovascular mechanical thrombectomy and thrombolysis have been shown to significantly reduce mortality and morbidity among the ischemic stroke population.9,10 Earlier initiation of therapy has been found to correlate with better clinical outcomes in these patients.11
This brings the spotlight of stroke care onto the ED to develop systems to recognize and triage these patients to adequately equipped centers. The challenge now is to not only detect stroke symptoms but also to identify those patients with a possible emergent large vessel occlusion12 (ELVO is defined as a thromboembolic occlusion of a M1 segment of the middle cerebral artery, internal carotid artery, basilar artery, or occlusion of the M2 segment). Emergent large vessel occlusion stroke accounts for nearly one-third of all ischemic strokes. These patients are the ideal candidates for endovascular therapy and thus may benefit from early referral to a center with endovascular capabilities.
Current AHA guidelines endorse a National Institute of Health Stroke Severity (NIHSS) score ≥ 6 as a criterion for intervention and identification of stroke patients with an ELVO.8
Vision, Aphasia, Neglect is a novel ELVO screening tool13 that has been developed to quickly identify the possibility of ELVO in stroke patients based on their clinical symptoms at presentation.
A search of existing literature reveals a lack of research pertaining to the Indian population on the use of VAN scores as well as NIHSS for clinical detection of ELVO from the ED.
Therefore, with this study, we have attempted to study the efficacy of VAN in clinically detecting patients with an ELVO stroke presenting to the ED. We also compared the performance of VAN score with that of NIHSS in the ED.
Materials and Methods
This was a single-center, prospective observational study conducted in the ED of a tertiary care hospital. The subjects were all patients presenting to the ED with symptoms suggestive of a cerebrovascular accident in the time period of 18 months. Institutional Ethical Committee approval was obtained prior to initiation of the study (Ref. no.: JSS/ MC/PG/5189/2019-20).
Selection of Subjects
All suspected stroke patients who presented to the ED were evaluated. Those who were above 18 years with symptoms suggestive of stroke (which may be any of the following: limb weakness, visual abnormalities, speech abnormalities, paresthesia, giddiness/vomiting, and headache) were initially included after obtaining informed consent. We excluded patients who were unresponsive to commands, stroke mimics, trauma, or those with prior CVA with residual deficit or prior audiovisual disabilities at the initial evaluation.
Outcomes
The main objective was to study the efficacy of the VAN tool in identifying patients who present with a possible ELVO stroke to the ED of a tertiary care center in India, with respect to the gold standard test for ELVO detection, i.e., MR angiogram.
We also attempted to compare the performance of VAN with respect to the prediction by NIHSS scoring with a threshold of ≥ 6, to identify patients with ELVO.
Sampling Technique
With respect to the pilot study which had a sample size of 62 patients, calculation by purposive sampling was undertaken (formula: Z2Pq/d2). To achieve an adequate power of 80%, a sample size of 70 was arrived.13
Data Collection
Eligible patients’ data were captured on a semistructured pro forma that included:
Demographic details.
Time of symptom onset and time of presentation to the hospital.
Nature of symptoms and respective comorbidities.
Vital signs’ recording.
Neurological assessment of the patient.
VAN score calculation (Table 1) and NIHSS score calculation.
Table 1.
VAN score
| Vision-Aphasia-Neglect scoring | |
|---|---|
| Motor drift |
|
| How weak is the patient? (assess with both arms lifted to shoulder level, palm facing upwards) |
|
| Visual disturbance |
|
| Aphasia |
|
| Neglect |
|
Patient must have motor weakness plus one/all of the V, A, N to be VAN POSITIVE
Study Protocol
In all eligible patients who presented with symptoms suggestive of a CVA, neurological assessment was done. Vision, Aphasia, Neglect and NIHSS scores were calculated by the emergency physician, and the patient was sent for MRA. The angiography was reported by a blinded radiologist, and the prediction by the scoring systems was compared and analyzed with the MRA report (Flowchart 1).
Flowchart 1.
Flowchart of the study protocol
Statistical Analysis
Data were entered into a Microsoft Excel datasheet and were analyzed using SPSS 22 version software. Categorical data were represented in the form of frequencies and percentage. Chi-square test/Pooled Chi-square was used as the test of significance for qualitative data. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated for the diagnostic test in comparison with the gold standard test. Receiver operating characteristic (ROC) curve analysis was done to estimate the area under the curve.
Graphical Representation of Data
MS Excel and MS Word were used.
A p-value < 0.05 was considered as statistically significant after assuming all the rules of statistical tests.
Results
In our study, there were 70 patients who fit the inclusion criteria. Stroke mimics were ruled out.
Our study population was predominantly male, comprising 67% of the total study population, with the maximum percentage being in the 40–65-year age-group. On evaluation, most patients had comorbidities with hypertension and diabetes mellitus being the most common. Two-thirds of the study population gave a history of smoking and alcohol consumption.
On initial evaluation by the emergency physician, 40% of our study population were VAN-positive with the most prevalent component being the presence of aphasia, followed by neglect. The time taken for VAN assessment was on an average 2 minutes.
The average NIHSS score of patients in this study was 9, with the lowest score being 2 and the highest being 20. The time taken to score NIHSS was 5 minutes.
On MRA, 27 patients were found to have large-vessel occlusion (LVO), and the most commonly involved vessel was the middle cerebral artery.
Vision, Aphasia, Neglect score for detection of ELVO in the study population was found to have a sensitivity of 85.19% and a specificity of 88.64% with a p-value < 0.0001 and a diagnostic accuracy of 87%.
In our study, a cutoff NIHSS value of 6 was found to detect ELVO with a sensitivity of 88% as well as a specificity of 51.11%. The accuracy of the test was 66%.
When both VAN and NIHSS with a cutoff of 6 were applied, NPV for ELVO detection was 100%.
By plotting ROC curves, VAN was found to have a larger area under the curve (AUC) with 0.8 as opposed to 0.7 for NIHSS (with a cutoff of 6). By Younden Index, it was found that an NIHSS score cutoff >7 yields the highest combined sensitivity and specificity for detection of ELVO than the AHA-recommended score of 6.
Discussion
Stroke or cerebrovascular accident is one of the major contributors to global mortality, with an annual death rate of five million. The burden of stroke lies not only in the high mortality rates but also in its high morbidity.14
The unique aspect of this disease is that it is time-sensitive. American Heart Association states that the dictum “Time is Brain” should be the leading factor while planning stroke evaluation and intervention. A stroke patient loses nearly two million neurons for every minute that treatment is delayed. This leads to irreversible consequences in the form of residual disabilities and a reduced quality of daily life in stroke survivors.15
Specific subsets of ischemic strokes are the ELVO strokes, which are caused by thrombi occluding the large cerebral vessels. Recent advances have brought up several novel treatment modalities for ischemic strokes, chiefly intravascular thrombolysis, and endovascular therapy.
At present, an NIHSS score of ≥6 is recommended by AHA as a criterion for eligibility for endovascular therapy as well as for the identification of ELVO stroke.8 But this has been found to be associated with a large number of false negatives, leading to a number of potentially treatable cases being missed.
In our study, the demographic and clinical characteristics of our patient population mirrored the global and regional trends for stroke, as shown by comparison with the Heart Disease and Stroke Statistics update 2015 as well as studies by Sylaja et al.,16 Ojha et al.,17 The INTERSTROKE study,18 as well the Indo-US Collaborative Stroke Project16 (Table 2).16,19
Table 2.
Patient demographics
| Age-group (years) | Age-wise distribution of patients | ||
|---|---|---|---|
| No. of patients | Percentage (%) | ||
| 20–30 | 4 | 5.63 | |
| 30–40 | 5 | 7.04 | |
| 40–50 | 14 | 19.71 | |
| 50–60 | 16 | 22.53 | |
| 60–70 | 18 | 25.35 | |
| 70–80 | 13 | 18.3 | |
| >80 | 1 | 1.4 | |
| Gender-wise distribution of patients | |||
| No. of patients | Percentage (%) | ||
| Gender | |||
| Female | 23 | 32.4 | |
| Male | 48 | 67.6 | |
| Comorbidities | |||
| Absent | 11 | ||
| Present | 60 | ||
| Additional risk factors | |||
| No. of patients | Percentage (%) | ||
| Alcohol | Absent | 55 | 77.5 |
| Present | 16 | 22.5 | |
| Smoking | Absent | 50 | 70.4 |
| Present | 21 | 29.6 | |
The ideal window period for intervention for IV thrombolysis is within 4 hours and for endovascular therapy is within 6 hours of symptom onset. In our study, 20% of the population presented to the ED within 4 hours and 40% within 6 hours of symptom onset (Table 3).
Table 3.
Presentation statistics
| Time from onset to presentation | No. of patients | Percentage (%) |
|---|---|---|
| Onset | ||
| Within 3 hours | 5 | 7 |
| 3–4.5 hours | 9 | 12 |
| 4–6 hours | 13 | 18 |
| 6–16 hours | 26 | 36 |
| >16 hours | 18 | 25 |
| Presenting complaints | No. of patients | Percentage (%) |
| Limb weakness | 60 | 84.50 |
| Speech abnormality | 44 | 61.97 |
| Slurring of speech | 23 | |
| Aphasia | 21 | |
| Giddiness | 15 | 21.11 |
| Vomiting | 14 | 19.71 |
| Neglect | 8 | 25.35 |
| Headache | 7 | 9.85 |
| Paresthesia | 5 | 7.04 |
| Visual abnormality | 3 | 4.22 |
| Average vitals on presentation | Mean vitals | |
| Pulse rate | 85/min | |
| Systolic BP | 167 mm Hg | |
| Diastolic BP | 93 mm Hg | |
| SpO2 | 97% at room air | |
| CBG | 162 mg/dL |
Hence, based on the time of presentation itself, a large proportion of our study population was out of the eligibility time frame for consideration of IV thrombolysis, but they were still in the time period for eligibility for endovascular therapy. This makes it even more important that we screen these patients for ELVO and triage them to adequately equipped centers.
Our study showed that the ED application of VAN yielded a higher specificity, positive and negative predictive value, and diagnostic accuracy and was faster when compared with NIHSS (Tables 4 to 8).
Table 4.
Distribution of NIHSS score in patients
| No. of patients | Percentage (%) | ||
|---|---|---|---|
| NIHSS | Less than 6 | 26 | 36.6 |
| More than 6 | 45 | 63.4 |
Table 8.
Analysis
(A) Vision, Aphasia, Neglect
| Large artery occlusion | |||||
|---|---|---|---|---|---|
| Present | Absent | ||||
| No. of patients | Percentage (%) | No. of patients | Percentage (%) | ||
| VAN | Positive | 23 | 85.2 | 5 | 11.4 |
| Negative | 4 | 14.8 | 39 | 88.6 | |
Table 5.
VAN score in patients
| No. of patients | Percentage (%) | ||
|---|---|---|---|
| VAN | Negative | 43 | 60.6 |
| Positive | 28 | 39.4 |
Table 6.
Time taken to calculate VAN vs NIHSS in the ED
| Score | Time (average no. of minutes) |
|---|---|
| VAN | 2 |
| NIHSS | 5 |
Table 7.
Large artery occlusion detected on MRA
| No. of patients | Percentage (%) | ||
|---|---|---|---|
| Large artery occlusion | Absent | 44 | 62.0 |
| Present | 27 | 38.0 |
(B).
Statistics- VAN
| Statistic | Value | 95% CI |
|---|---|---|
| Sensitivity | 85.19% | 66.27–95.81% |
| Specificity | 88.64% | 75.44–96.21% |
| Positive likelihood ratio | 7.50 | 3.24–17.37 |
| Negative likelihood ratio | 0.17 | 0.07–0.42 |
| Positive predictive value | 82.14% | 66.51–91.42% |
| Negative predictive value | 90.70% | 79.68–96.04% |
| Accuracy | 87.32% | 77.30–94.04% |
(C).
Test of significance (VAN)
| Pearson Chi-square tests | ||
|---|---|---|
| Occlusion | ||
| VAN | Chi-square | 38.178 |
| Df | 1 | |
| Sig. | 0.0001* | |
(D).
NIHSS ≥ 6
| Large artery occlusion | |||||
|---|---|---|---|---|---|
| Present | Absent | ||||
| Count | Column N% | Count | Column N% | ||
| NIHSS score | Positive | 24 | 88.8 | 21 | 47.7 |
| Negative | 3 | 11.2 | 23 | 52.3 | |
(E).
Statistics – NIHSS ≥ 6
| Statistic | Value | 95% CI |
|---|---|---|
| Sensitivity | 88.89% | 70.84–97.65% |
| Specificity | 52.27% | 36.69–67.54% |
| Positive likelihood ratio | 1.86 | 1.33–2.61 |
| Negative likelihood ratio | 0.21 | 0.07–0.64 |
| Positive predictive value (*) | 53.33% | 44.94–61.55% |
| Negative predictive value (*) | 88.46% | 71.77–95.85% |
| Accuracy (*) | 66.20% | 53.99–77.00% |
A study conducted by Navalkele et al.20 compared VAN with NIHSS (with a cutoff value greater than or equal to 6) as well as other established prehospital ELVO screening tools such as rapid arterial occlusion evaluation scale (RACE), field assessment stroke triage for emergency destination (FAST-ED), and cincinnati prehospital stroke scale (CPSS) and found VAN to have the highest NPV among all screening assessments (88%). Our study found VAN to have an even higher NPV of 90%.
This implied that application of VAN in the ED produced a larger number of true positives and true negatives, which is important to screen for ELVO. It tests only for the presence / absence of specific cortical symptoms with no score calculations and hence requires lesser skill and training to apply than NIHSS. The presence of these symptoms in combination has been proven to be associated with LVO. Vision, Aphasia, Neglect is positive/negative based on the presence of symptoms, irrespective of the severity of any individual symptom. Hence, from our stud`y, we inferred that VAN is a better tool to screen for ELVO strokes in patients presenting to the ED, but however, it cannot be used to assess stroke severity.
Also, we found the VAN is quicker to apply when compared with NIHSS (2 minutes vs 5 minutes). Hence, this makes it a more practical screening tool for strokes in the ED, where time is the brain.
When both VAN and NIHSS were applied together, it did not miss any case with ELVO on the angiogram. In other words, they had a combined NPV of 100%. This shows that both tests are necessary, with VAN performing better for quick screening purposes in the ED.
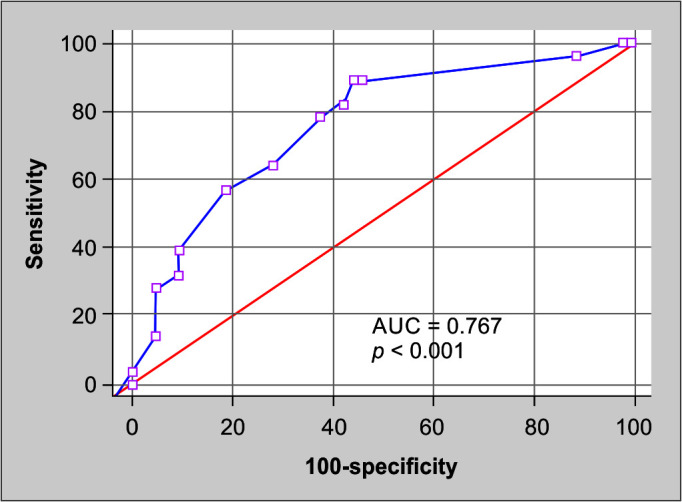
Analysis using ROC curves (Figs 1 to 3) indicated that VAN score had a better accuracy than NIHSS with a cutoff score 6 (0.869 vs 0.706). Also, additional analysis using Youden Index (Table 9) showed that an NIHSS score cutoff >7 yields the highest combined sensitivity and specificity for detection of ELVO as opposed to the AHA-recommended standard of 6.
Fig. 1.

NIHSS (score >6) vs MR angiogram
Fig. 3.
NIHSS score. As per the ROC curve, an NIHSS score cutoff >7 yielded the highest combined sensitivity and specificity for detection of ELVO
Table 9.
Youden index
| Youden index J | 0.4510 |
| Associated criterion | >7 |
| Sensitivity | 89.29 |
| Specificity | 55.81 |
As per the ROC curve and its Youden Index, an NIHSS score cut-off >7 yielded the highest combined sensitivity and specificity for detection of ELVO.
Fig. 2.
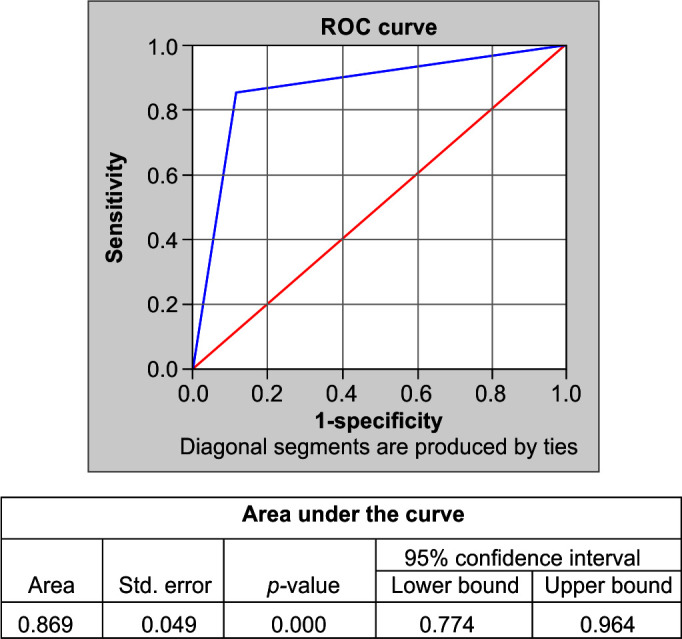
VAN vs MR angiogram
(9A).
Criterion values and coordinates of the ROC curve
| Criterion | Sensitivity | Specificity | +LR | –LR | +PV | –PV |
|---|---|---|---|---|---|---|
| ≥2 | 100.00 | 0.00 | 1.00 | 39.4 | ||
| >2 | 100.00 | 2.33 | 1.02 | 0.00 | 40.0 | 100.0 |
| >3 | 96.43 | 11.63 | 1.09 | 0.31 | 41.5 | 83.3 |
| >4 | 89.29 | 53.49 | 1.92 | 0.20 | 55.6 | 88.5 |
| >7 | 89.29 | 55.81 | 2.02 | 0.19 | 56.8 | 88.9 |
| >8 | 82.14 | 58.14 | 1.96 | 0.31 | 56.1 | 83.3 |
| >9 | 78.57 | 62.79 | 2.11 | 0.34 | 57.9 | 81.8 |
| >10 | 64.29 | 72.09 | 2.30 | 0.50 | 60.0 | 75.6 |
| >11 | 57.14 | 81.40 | 3.07 | 0.53 | 66.7 | 74.5 |
| >12 | 39.29 | 90.70 | 4.22 | 0.67 | 73.3 | 69.6 |
| >13 | 32.14 | 90.70 | 3.46 | 0.75 | 69.2 | 67.2 |
| >14 | 28.57 | 95.35 | 6.14 | 0.75 | 80.0 | 67.2 |
| >17 | 14.29 | 95.35 | 3.07 | 0.90 | 66.7 | 63.1 |
| >18 | 3.57 | 100.00 | 0.96 | 100.0 | 61.4 |
Hence, our study found that VAN score as well as NIHSS are both tools for clinical prediction of ELVO in stroke patients, with VAN having better diagnostic accuracy and utility as a screening tool in the ED.
Conclusion
Vision, Aphasia, Neglect score as well as NIHSS are both tools for clinical prediction of ELVO in stroke patients with VAN having a better diagnostic accuracy and utility as a screening tool in the ED. Further studies with a more diverse study population and more importantly in the prehospital scenario for ELVO screening among suspected stroke patients are warranted.
Limitations
The study population was restricted to a single center.
Only patients presenting to the ED were included in the study, and the scoring was done by the emergency physician.
The performance of the VAN score was not studied in the prehospital population, which is where it is expected to have the greatest utility.
Orcid
Aishwarya Krishnan https://orcid.org/0000-0003-0558-4546
Madhu Srinivasarangan https://orcid.org/0000-0003-3310-7018
Sriharsha Jagadish https://orcid.org/0000-0001-9901-4979
Adarsh SB https://orcid.org/0000-0002-9322-5393
Abhijith Sivasankar https://orcid.org/0000-0002-3010-4666
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.WSO. World Stroke Organization [cited November 23, 2021]. Available from: https://www.world-stroke.org.
- 2.Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Heart disease and stroke statistics – 2018 update: A report from the American Heart Association. Circulation. 2018;137(12):e67–e492. doi: 10.1161/CIR.0000000000000558. [DOI] [PubMed] [Google Scholar]
- 3.Cortesi PA, Fornari C, Madotto F, Conti S, Naghavi M, Bikbov B, et al. Trends in cardiovascular diseases burden and vascular risk factors in Italy: The Global Burden of Disease study 1990–2017. Eur J Prev Cardiol. 2021;28(4):385–396. doi: 10.1177/2047487320949414. [DOI] [PubMed] [Google Scholar]
- 4.Merkler AE, Parikh NS, Mir S, Gupta A, Kamel H, Lin E, et al. Risk of ischemic stroke in patients with coronavirus disease 2019 (COVID-19) vs patients with influenza. JAMA Neurol. 2020;77(11):1–7. doi: 10.1001/jamaneurol.2020.2730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kakkar G, Zirpe KG, Sapra H, Dixit S, Chugh C, Nagaiyan S, et al. Practice implications for acute ischemic stroke during the COVID-19 pandemic for the Indian scenario: Realistic and achievable recommendations by the Society of Neurocritical Care (SNCC), India. Indian J Crit Care Med. 2020;24(9):757–762. doi: 10.5005/jp-journals-10071-23511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harrison's Principles of Internal Medicine, 20e | AccessMedicine | McGraw Hill Medical, 2021 [Google Scholar]
- 7.Chugh C. Acute ischemic stroke: Management approach. Indian J Crit Care Med. 2019;23(Suppl 2):S140–S146. doi: 10.5005/jp-journals-10071-23192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jauch EC, Saver JL, Adams HP, Bruno A, Connors JJB, Demaerschalk BM, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870–947. doi: 10.1161/STR.0b013e318284056a. [DOI] [PubMed] [Google Scholar]
- 9.Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372(11):1019–1030. doi: 10.1056/NEJMoa1414905. [DOI] [PubMed] [Google Scholar]
- 10.Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015;372(24):2296–2306. doi: 10.1056/NEJMoa1503780. [DOI] [PubMed] [Google Scholar]
- 11.Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: A meta-analysis of individual patient data from randomised trials. Lancet. 2014;384(9958):1929–1935. doi: 10.1016/S0140-6736(14)60584-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leslie-Mazwi T, Chandra RV, Baxter BW, Arthur AS, Hussain MS, Singh IP, et al. ELVO: An operational definition. J Neurointerv Surg. 2018;10(6):507–509. doi: 10.1136/neurintsurg-2018-013792. [DOI] [PubMed] [Google Scholar]
- 13.Teleb MS, Ver Hage A, Carter J, Jayaraman MV, McTaggart RA. Stroke vision, aphasia, neglect (VAN) assessment – a novel emergent large vessel occlusion screening tool: Pilot study and comparison with current clinical severity indices. J Neurointerv Surg. 2017;9(2):122–126. doi: 10.1136/neurintsurg-2015-012131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Donkor ES. Stroke in the 21st century: A snapshot of the burden, epidemiology, and quality of life. Stroke Res Treat. 2018;2018:3238165. doi: 10.1155/2018/3238165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Saver JL. Time is brain–quantified. Stroke. 2006;37(1):263–266. doi: 10.1161/01.STR.0000196957.55928.ab. [DOI] [PubMed] [Google Scholar]
- 16.Sylaja PN, Pandian JD, Kaul S, Srivastava MVP, Khurana D, Schwamm LH, et al. Ischemic stroke profile, risk factors, and outcomes in India. Stroke. 2018;49(1):219–222. doi: 10.1161/STROKEAHA.117.018700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ojha PT, Basak S, Aglave V, Yadav J. Incidence of stroke in adults according to age, sex and subtypes in urban Indian population. Neurol Neurosci Rep. 2020;3(1) doi: 10.15761/NNR.1000117. [DOI] [Google Scholar]
- 18.O’Donnell MJ, Chin SL, Rangarajan S, Xavier D, Liu L, Zhang H, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): A case-control study. Lancet. 2016;388(10046):761–775. doi: 10.1016/S0140-6736(16)30506-2. [DOI] [PubMed] [Google Scholar]
- 19.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics–2015 update: A report from the American Heart Association. Circulation. 2015;131(4):e29–e322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 20.Navalkele D, Vahidy F, Kendrick S, Traylor A, Haydel M, Drury S, et al. Vision, Aphasia, Neglect assessment for large vessel occlusion stroke. J Stroke Cerebrovasc Dis. 2020;29(1):104478. doi: 10.1016/j.jstrokecerebrovasdis.2019.104478. [DOI] [PubMed] [Google Scholar]



