Abstract
PulseRider is a self-expanding stent implant used to treat wide-necked aneurysms. As this device has a lower metal mass than conventional stents, it is expected to have a lower rate of ischemic complications and a shorter period with antiplatelet drugs. We experienced in-stent stenosis after endovascular treatment with the PulseRider for a middle cerebral artery aneurysm. A 40-year-old woman with an unruptured aneurysm in the middle cerebral artery bifurcation underwent coil embolization using a PulseRider. The periprocedural course was not problematic, and postoperative angiography showed contrast filling in the aneurysm. The patient was discharged from our hospital on postembolization day 3. However, follow-up angiography after 6 months showed in-stent stenosis. Fortunately, no ischemic complications occurred after treatment. Although the PulseRider is characterized by a low metal mass, it should be noted that this device has some metal markers that can induce in-stent stenosis.
Keywords: Cerebral aneurysm, In-stent stenosis, PulseRider
Introduction
PulseRider (Cerenovus, New Brunswick, NJ) is a self-expanding stent implant for the treatment of wide-necked aneurysms. This device is made of nickel-titanium (nitinol) and has a Y- or T-shape, which provides scaffolding for the placement of endovascular coils inside the aneurysmal sac [1]. This function can prevent the protrusion of endovascular coils, even in a wide-necked anatomy. This device is characterized by a low metal mass concentrated in the aneurysmal neck. Therefore, the device is expected to have fewer ischemic events and achieve a shorter duration with antiplatelet drugs. Here, we report a rare case of in-stent stenosis (ISS) after PulseRider placement for a middle cerebral artery aneurysm.
Case report
A 40-year-old woman with an incidental unruptured middle cerebral artery (MCA) bifurcation aneurysm with a daughter sac underwent endovascular treatment.
The patient received dual antiplatelet therapy with 100 mg aspirin and 3.75 mg prasugrel daily for 10 days before the intervention. The intervention was performed using systemic heparinization. Angiography revealed that both the MCA M2 superior and inferior trunks were incorporated into the aneurysm wall and bifurcated laterally (Fig. 1). The aneurysm measurements were as follows: diameter - 5.7 mm, neck - 4.4 mm, and height - 5.6 mm. The dome-to-neck and aspect ratios were 1.30 and 1.27, respectively. A 6-French guiding sheath (FUBUKI Dilator kit; ASAHI INTECC Co., Ltd., Aichi, Japan) was positioned in the left cervical intracarotid artery (ICA). A Prowler Select Plus (Cerenovus) microcatheter was precisely placed in the middle of the left MCA relative to the aneurysm. A 2.7-3.5 mm 8T PulseRider was deployed in the extra-aneurysmal position with leaflets inside each MCA. High-resolution cone-beam computed tomography (CT) performed after deployment showed that the 2 arches of the PulseRider were positioned within both M2 trunks of the left MCA (Fig. 2). A Headway17 (Microvention Inc., Aliso Viejo, CA) microcatheter was then placed inside the aneurysm through PulseRider's leaflets. Coil embolization of the aneurysm was performed using 3 bare platinum coils. No intraprocedural complications occurred, and postoperative angiography showed contrast filling in the aneurysm (Fig. 3). The patient was discharged on postembolization day 3.
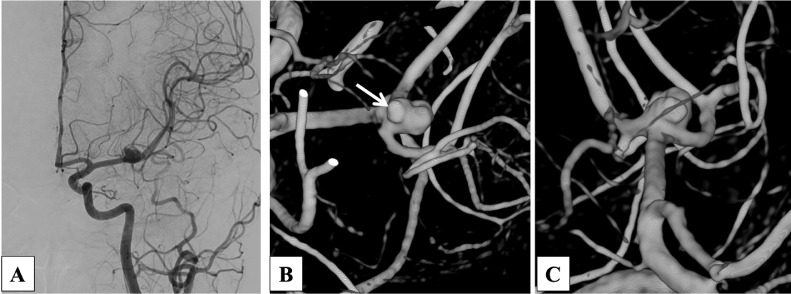
Fig. 1.
(A) Left common carotid angiography in anteroposterior view indicates a saccular aneurysm located in the left middle cerebral artery bifurcation. (B) 3-dimensional rotational angiography (3D-RA) indicates a daughter sac (white arrow). (C) 3D-RA shows that both MCA M2 superior trunk and inferior trunk were incorporated into the aneurysm wall and bifurcated laterally.
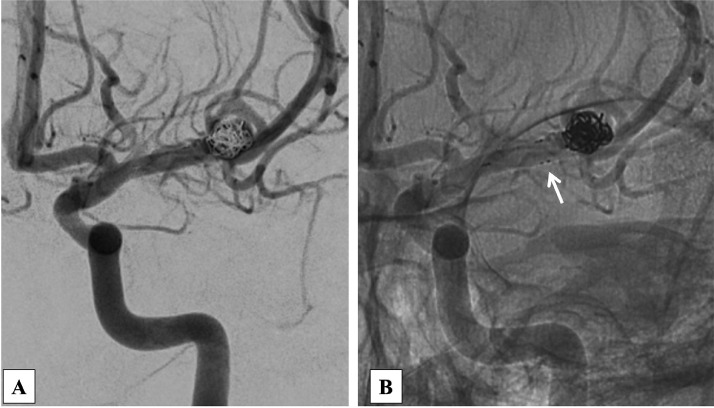
Fig. 2.
(A) The cone-beam computed tomography (CBCT) before detachment demonstrates the 2 arches of the PulseRider were positioned within both M2 trunks of left MCA and that the aneurysmal neck was covered (white arrowheads). (B) CBCT shows the markers of PulseRider that cohere the vessel wall (white arrows).
Fig 3.
(A) Left common carotid angiography after coil embolization shows contrast filling in the aneurysm. (B) There is no stenosis in the left middle cerebral artery.
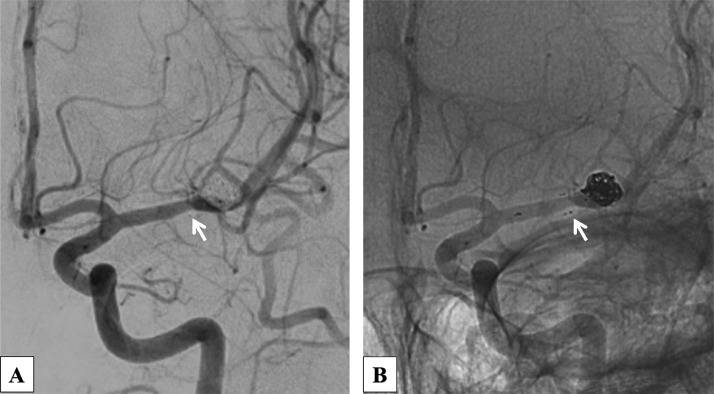
Six months after the procedure, follow-up angiography revealed complete occlusion of the aneurysm. However, ISS was observed near the medial markers of the PulseRider (Fig. 4). After the 6-month follow-up angiography, prasugrel was discontinued and aspirin was continued. No delayed-onset neurological complications have been reported.
Fig 4.
(A) Follow-up angiography showed complete occlusion of the aneurysm. (B) There is a mild stenosis due to intimal hyperplasia near the medial markers of PulseRider (white arrows).
Discussion
Embolization of aneurysms in a bifurcation artery with endovascular treatment remains difficult because of insufficient protection from coil collapse into daughter vessels. Flow diverters are not an effective treatment choice due to the risk of jailing another branch. The PulseRider is useful for achieving high aneurysm concentration rates to cover the wide neck of the aneurysm, which is located on the bifurcated artery. As mentioned above, it is characterized by a shorter period of dual antiplatelet treatment after the procedure than conventional stents because of the lower amount of metal remaining in the vessels. Although the long-term complications following PulseRider implantation are unclear, they are expected to result in fewer ischemic complications. The incidence of complications following PulseRider implantation is reported to be 0%-8.8%, and most complications occur periprocedurally. A meta-analysis reported that perioperative complications of the PulseRider include aneurysm rupture, thrombus formation, vessel dissection, and ischemic stroke [1,2].
To the best of our knowledge, ISS has never been reported in an aneurysmal embolization using the PulseRider. ISS is a relatively well-known complication of coronary artery disease treatment, with an incidence of 10%-50% [3]. Furthermore, ISS is a frequently delayed complication after endovascular treatment with a flow diverter, occurring in 15%-39% of patients receiving flow diverter stenting [4]. However, little is known about the mechanism underlying ISS formation. Neointimal hyperplasia is presumed to be caused by a localized reaction to the arterial wall injury generated during stent inflation [5]. Although the PulseRider is characterized by a low metal mass, it contains some metal markers that can induce arterial wall injury, followed by intimal hyperplasia.
The risk of ISS has been reported in balloon angioplasty and posterior circulation aneurysms after treatment with a flow diverter. Age > 54 years is a protective factor for ISS because older people lack endothelialization, which reduces the potential for neural stem cell proliferation and differentiation.
In the present case, the patient was 40 years old and susceptible to intimal hyperplasia, which may have induced ISS.
Recent reports have suggested that ISS leads to complete blood vessel occlusion, although it rarely causes serious symptoms y [4]. Gui et al. [4] noted that the treatment recommended for patients with ISS after treatment with a pipeline embolization device is tight follow-up and long-term antiplatelet therapy because 30% of patients with ISS developed parental artery occlusion. In contrast, Kim et al. reported that ISS after stent-assisted coil embolization is a dynamic process that appears to be a spontaneously reversible event [6]. In their report, they stated that only routine management of ISS should be performed because ISS might not cause adverse events that require additional treatment [6]. Due to the lack of evidence for optimal follow-up of ISS after PulseRider stenting, careful antiplatelet therapy was needed in this case.
Conclusion
Herein, we present a rare case of ISS after PulseRider placement for an MCA aneurysm. Although PulseRider is characterized by a low metal mass, it should be noted that this device has metal markers that can induce ISS.
Patient consent
Informed consent was obtained from the patient for the publication of this case report and accompanying images.
Footnotes
Competing Interests: The authors declare no conflict of interest.
References
- 1.Pranata R, Yonas E, Vania R, Sidipratomo P, July J. Efficacy and safety of PulseRider for treatment of wide-necked intracranial aneurysm—A systematic review and meta-analysis. Interv Neuroradiol. 2021;27(1):60–67. doi: 10.1177/1591019920940521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Suyama K, Nakahara I, Matsumoto S, Morioka J, Hasebe A, Tanabe J, et al. Brainstem infarctions caused by a Proximal marker of the PulseRider device obstructing the origin of a perforator. J Stroke Cerebrovasc Dis. 2022;31(4) doi: 10.1016/j.jstrokecerebrovasdis.2022.106332. [DOI] [PubMed] [Google Scholar]
- 3.Lowe HC, Oesterle SN, Khachigian LM. Coronay in-stent restenosis: current status and future strategies. J Am Coll Cardil. 2002;39(2):183–193. doi: 10.1016/s0735-1097(01)01742-9. [DOI] [PubMed] [Google Scholar]
- 4.Gui S, Chen X, Wei D, Deng D, You W, Meng X, et al. Long-term outcomes and dynamic changes of in-stent stenosis after Pipeline embolization device treatment of intracranial aneurysms. J NeuroIntervent Surg. 2023;0:1–8. doi: 10.1136/jnis-2022-019680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O'Connell BM, McGloughlin TM, Walch MT. Factors that affect mass transport from drug eluting stents into the artery wall. Biomed Eng Online 9:15, doi:10.1186/1475-925X-9-15 [DOI] [PMC free article] [PubMed]
- 6.Kim YS, Lee SW, Yeom JA, Yoon CH, Baik SH. Angiographic findings of in-stent intimal hyperplasia after stent-assited coil embolization: are they permanent findings? J Neurosurg. 2016;124(2):328–333. doi: 10.3171/2015.2.JNS142557. [DOI] [PubMed] [Google Scholar]