Abstract
Accessory breast tissue (supernumerary breast tissue) is due to the absence of regression of the primitive milk lines during embryonic life which extends from the axilla to the groin. It is mostly located in the axilla where it is often confused with the axillary extension of the breast, or any pathological process occurring in armpits. Ectopic mammary glands should not be misdiagnosed as it can potentially undergo the same pathological processes that occur in a normally located breast including benign or malignant breast tumors. We report the case of an intracystic papilloma arising from left axillary accessory breast tissue in a 63-year-old woman. The principal symptom was pain in a palpable left axillary mass without inflammatory signs. Subsequent imaging and histopathologic examination proved it to be a papillary tumor in ectopic breast tissue.
Keywords: Accessory breast tissue, Axillary, Papilloma
Introduction
Mammary gland (breast) development begins as ectodermal thickening during the early embryonic phase, and transforms into breast milk lines, that grow along the sides of the embryo during the sixth week of development, extending from the axillary region to the groin [1].
This milk line normally regresses except for 2 segments in the pectoral region that later form breasts. Failure of this line's regression may occur at any level from the axilla to the groin area, which leads to the development of ectopic breast tissue.
This condition is also known as supernumerary breast, ectopic breast, and polymastia, and it frequently develops along the “milk line” or mammary line [2], [3], [4]. Gender, geographical area, race, and inheritance have all been proven to influence the incidence of accessory breast tissue. The prevalence ranges from 0.22% to 6% of the general population [5].
We present a case of axillary accessory breast papilloma that was clinically diagnosed as a lipoma. We are reporting this unusual occurrence because it is uncommon as a seat in this anatomic site. Furthermore, as seen in our case study, this situation might create a diagnostic challenge to clinicians by mimicking lymphoma or other forms of lymphadenopathy. Our goal was to emphasize the significance of including accessory breast and its accompanying pathology in the differential diagnosis of axillary masses.
Case presentation
A 63-year-old patient presented with a 4-year history of left axillary swelling that became recently painful. The swelling began modest and gradually grew larger until it reached its current size. Except from the recent onset of pain and discomfort, there was no history of nipple discharge, nor history of general symptoms such as cough, fever, weight loss, nocturnal sweating, or other symptoms. Her previous medical and surgical history revealed a thyroidectomy with histological examination of a noninvasive follicular thyroid neoplasm.
Her general state was stable. The following vital signs were recorded: pulse rate of 70 beats per minute; blood pressure of 110/80 mmHg; respiratory rate of 18 breaths per minute; and temperature of 37°C.
There was a 4 × 4 cm solitary mass in the left axilla, well-defined and soft. This lump did not appear to be linked to the skin or the chest wall, and it did not produce any inflammation or skin retraction, however. Skin over the swelling was hyperpigmented suggesting an ectopic areola. There was no abnormality found in the same region on her right breast. The axillary and supraclavicular lymph nodes were absent (Fig. 1).
Fig. 1.
Left supernumerary breast with areola.
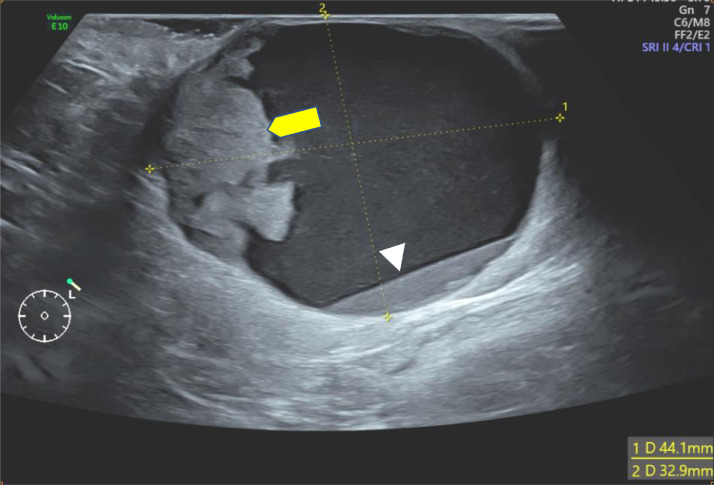
Ultrasonography was first performed showing a supernumerary breast tissue, of left axillary location, with a complex cystic mass containing an echogenic-anechoic liquid level, and a tissue component, that appears hyperechoic, with ill-defined margins, homogeneous (Fig. 2), with vascular pedicle in color Doppler (Fig. 3) and hard elasticity in ultrasound elastography (Fig. 4).
Fig. 2.
Ultrasound of the left axilla showing a complex cystic and solid mass, containing an echogenic-anechoic liquid level (head arrow), and a tissue component (yellow arrow).
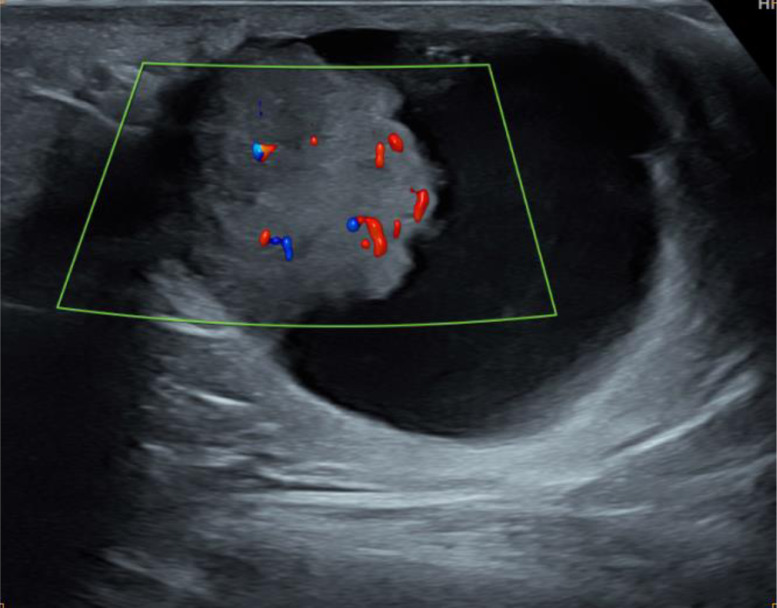
Fig. 3.
Ultrasound of the left axilla showing Doppler vascularization of the tissue component.
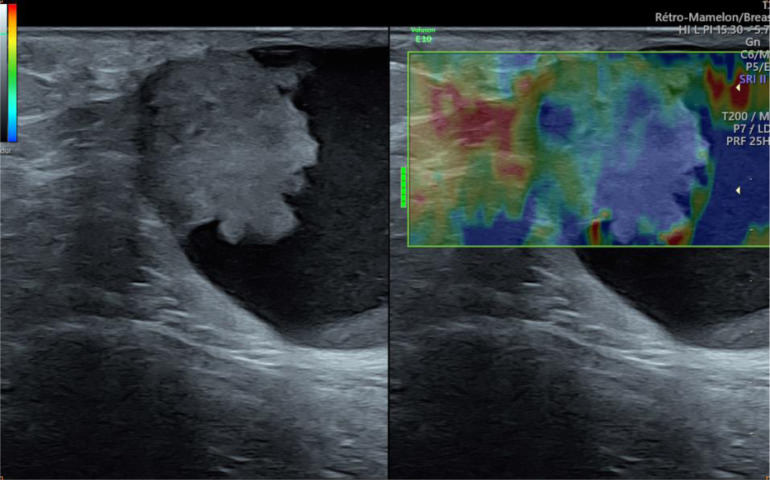
Fig. 4.
Ultrasound elastography showing hard elasticity of the tissue component.
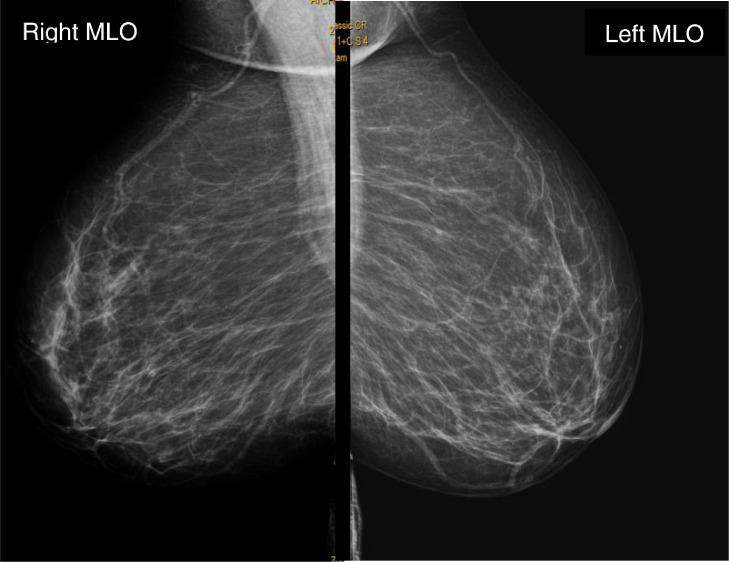
Mammogram and ultrasound of breasts were also performed and showed no notable abnormalities (Fig. 5).
Fig. 5.
Mammogram in mid-lateral-oblique incidence.
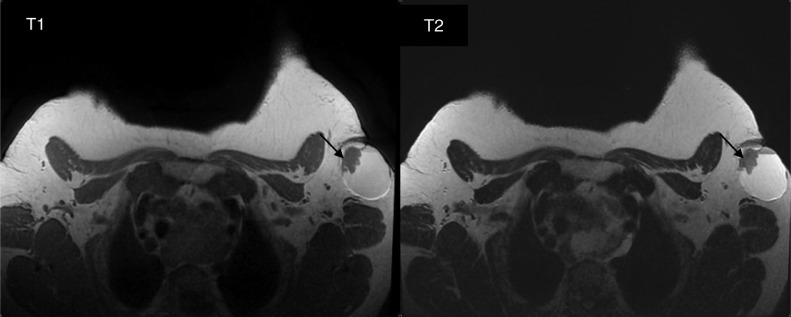
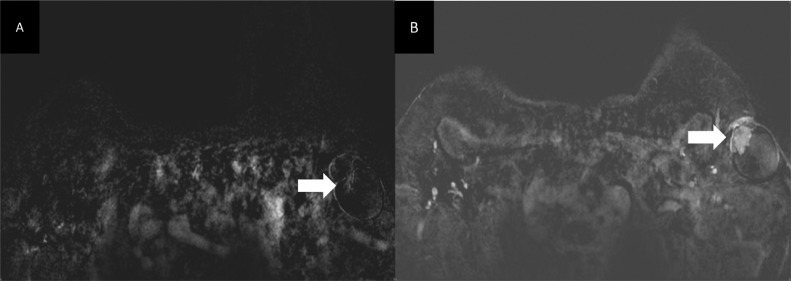
Breast MRI was used to further describe the cystic mass and to seek for other possible breast abnormalities. It revealed a complex mass in the left axilla with hemorrhagic cystic component, and solid content with low signal on T1-weighted images, and intermediate signal on T2-WI. On dynamic sequences after gadolinium, a fast and early enhancement of the solid portion was found (Fig. 6, Fig. 7, Fig. 8).
Fig. 6.
Axial T1-weighted image (left) and axial T1 with fat saturation sequence (right) showing the cystic mass in the left axilla with hemorrhagic content, that appears hyperintense in T1 not suppressed in fat saturation sequence (arrows).
Fig. 7.
Axial T1- and T2-weighted images show the solid component (arrows) that appears hypointense in T1 with intermediate T2 signal.
Fig. 8.
Axial T1 GE 3D subtracted sequences showing rapid homogenous enhancement of the solid component (arrow).
Ultrasound-guided 16-G core-needle biopsy was performed, revealing an intracystic papilloma. The patient underwent wide local excision for the lesion. She was discharged on the next day, with appointments arranged for follow-up and wound care. Diagnosis was confirmed with the histologic examination of the entire mass.
Discussion
Accessory breast, also known as polymastia, or supernumerary breasts, is the condition of having more than 2 breasts with or without a nipple and areola. It generally results from an involutional failure of the embryonic milk lines, and may extend from the axilla to the groin but it most commonly arises in the axillary region,
In 1915, Kajava established the accessory breast classification system, which is being used today [[6], [7], [8]] (Table 1). Our case is classified as class III since we only have glandular tissue (detected as papilloma) and areola without nipple.
Table 1.
| Type (class) | Description |
|---|---|
| Class I | Consists of a complete breast including glandular tissue, nipple, and areola |
| Class II | Consists of only glandular tissue and nipple, without areola |
| Class III | Consists of only glandular tissue and areola, without nipple |
| Class IV | Consists of only glandular tissue |
| Class V | Consists of only nipple and areola, without glandular tissue (pseudomamma) |
| Class VI | Consists of only the nipple (polythelia) |
| Class VII | Consists of only the areola (polythelia areolaris) |
| Class VIII | Consists of only hair (polythelia pilosa) |
Accessory breast tissue responds to hormones and can develop benign and malignant pathologic processes comparable to those found in normal breast tissue, such as fibrocystic disease, intraductal papilloma, lactating adenoma, fibroadenoma, and carcinoma [[9], [10], [11], [12]].
While papilloma is a frequent benign lesion in normal breast tissue, that affects 2%-3% of the population [[13], [14]], its presence in accessory breast tissue is uncommon. Papilloma may arise in a duct as a single mass or multiple masses, or develop into a cystically dilated duct known as intracystic papillomas which was the case of our patient. Unlike intraductal papillomas, intracystic papillomas are seldomly found and tend to occur in postmenopausal women [[15], [16]]. Clinically, papillomas may present with bloody or clear nipple discharge or a palpable sub areolar mass [[17], [18]].
On mammogram, they may present as multiple circular or linear dense soft tissue masses with well-defined or partially circumscribed margi [[19], [20]]. Ultrasound findings describe 3 main patterns of papillomas, including (1) intraductal mass with or without ductal dilatation, (2) intracystic mass due to concomitant excess fluid production in a blocked duct, and (3) primarily solid pattern with intraductal mass completely filling the duct [[21], [22]].
Diagnostic and therapeutic approaches for tumors in accessory breast tissue are the same as for a normal breast mass. Yet, because of its rarity and lack of suspicion, diagnosis may be neglected, delaying prompt treatment.
Conclusion
While examining a patient with axillary swelling, accessory breast tissue conditions must be addressed as a differential diagnosis for early identification and therapy. This case demonstrates that accessory breast tissue, like normal breast tissue, is subject to the same physiologic and pathologic disease processes, including neoplasms. The majority of care is surgical intervention with excision, when tumors or nodules are discovered along the mammary line, the existence of breast tissue should be investigated to rule out the correct diagnosis and to guide the proper management strategy.
Ethics approval and consent to participate
Not applicable.
Availability of data and materials
The data sets are generated on the data system of the CHU Hassan II of Fes, including the biological data and the interventional report.
Patient consent
I, the author of the article “Unusual intra ductal papilloma in ectopic axillary breast tissue: Case report,” approve that the patient gives her consent for information to be published in Radiology Case Reports.
Footnotes
Acknowledgments: No source of funding was received.
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Saddler TW. Lippincott Williams and Wilkins; Philadelphia: 2012. Langman's medical embroyology; p. 354. [Google Scholar]
- 2.Amir M, Aravind K, Shaikh H. A rare case of fibroadenoma in ectopic breast tissue of axilla: case report. Int Surg J. 2018;5(10):3446–3449. doi: 10.18203/2349-2902.isj20184108. [DOI] [Google Scholar]
- 3.Dixon J, Mansel R. Congenital problems and aberrations of normal breast development and involution. Br Med J. 1994;309(6957):797–800. doi: 10.1136/bmj.309.6957.797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Surd A, Mironescu A, Gocan H. Fibroadenoma in axillary supernumerary breast in a 17-year-old girl: case report. J Pediatr Adolesc Gynecol. 2016;29(5):e79–e81. doi: 10.1016/j.jpag.2016.04.008. [DOI] [PubMed] [Google Scholar]
- 5.Schmidt H. Supernumerary nipples: prevalence, size, sex and side predilection—a prospective clinical study. Eur J Pediatr. 1998;157(10):821–823. doi: 10.1007/s004310050944. [DOI] [PubMed] [Google Scholar]
- 6.Burdick AE, Thomas KA, Welsh E, Powell J, Elgart GW. Axillary polymastia. J Am Acad Dermatol. 2003;49(6):1154–1156. doi: 10.1016/S0190-9622(03)00467-5. [DOI] [PubMed] [Google Scholar]
- 7.Gabriel A. Breast embryology. Available at: http://emedicine.medscape.com/article/1275146-overview#showall. [accessed 20.8.2011].
- 8.Kajava Y. The proportions of supernumerary nipples in the Finnish population. Duodecim. 1915;1:143–170. [Google Scholar]
- 9.Grossl NA. Supernumerary breast tissue: historical perspectives and clinical features. South Med J. 2000;93(1):29–32. doi: 10.1097/00007611-200093010-00005. [DOI] [PubMed] [Google Scholar]
- 10.Gajaria PK. Fibroadenoma in axillary ectopic breast tissue mimicking lymphadenopathy. J Clin Diagn Res. 2017;11(3):10–11. doi: 10.7860/JCDR/2017/23295.9358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kohli S, Garg P, Kharkwal S, Verma AK. Rare clinical entity—fibroadenoma of ectopic breast tissue. Indian J Basic Appl Med Res. 2015;5(1):575–578. [Google Scholar]
- 12.Shin SJ, Sheikh FS, Allenby PA, Rosen PP. Invasive secretory (juvenile) carcinoma arising in ectopic breast tissue of the axilla. Arch Pathol Lab Med. 2001;125(10):1372–1374. doi: 10.5858/2001-125-1372-ISJCAI. [DOI] [PubMed] [Google Scholar]
- 13.Amaranathan A, Balaguruswamy K, Bhat RV, Bora MK. An ectopic breast tissue presenting with fibroadenoma in axilla. Case Rep Surg. 2013;2013:1–3. doi: 10.1155/2013/947295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Landthaler M, Hofstaedter F, Meisel C. Fibroadenoma of the axilla. Coras. Hohenleutner U. Dermatol Surg. 2005;31:1152–1154. doi: 10.1097/00042728-200509000-00015. [DOI] [PubMed] [Google Scholar]
- 15.Sadofsky M. Benign papilloma of the breast. Acad Pathol. 2017;4:1–3. doi: 10.1177/2374289517711714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pisano ED, Braeuning MP, Burke E. Diagnosis please. Case 8: solitary intraductal papilloma. Radiology. 1999;210(3):795–798. doi: 10.1148/radiology.210.3.r99mr37795. [DOI] [PubMed] [Google Scholar]
- 17.Cardenosa G. 2nd ed. Lippincott Williams and Wilkins; Philadelphia: 2001. Breast imaging companion; p. 224. [Google Scholar]
- 18.Harvey JA, March DE. Elsevier; Philadelphia: 2013. Making the diagnosis: a practical guide to breast imaging; pp. 401–406. [Google Scholar]
- 19.Ueng SH, Mezzetti T, Tavassoli FA. Papillary neoplasms of the breast: a review. Arch Pathol Lab Med. 2009;13:893–907. doi: 10.5858/133.6.893. [DOI] [PubMed] [Google Scholar]
- 20.Ganesan S, Karthik G, Joshi M, Damodaran V. Ultrasound intraductal papillary neoplasms of breast. Br J Spectr Radiol. 2006;79:843–849. doi: 10.1259/bjr/69395941. [DOI] [PubMed] [Google Scholar]
- 21.Kopans DB. JB Lippincot; Philadelphia (PA): 1998. Pathologic, mammographic and sonographic correlation in breast imaging; pp. 516–521. [Google Scholar]
- 22.Mesurolle B, Kethani K, EI-Khoury M, Meterissian S. Intraductal papilloma in a reconstructed breast: mammographic and sonographic appearance with pathologic correlation. Breast. 2006;15:680–682. doi: 10.1016/j.breast.2005.10.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data sets are generated on the data system of the CHU Hassan II of Fes, including the biological data and the interventional report.