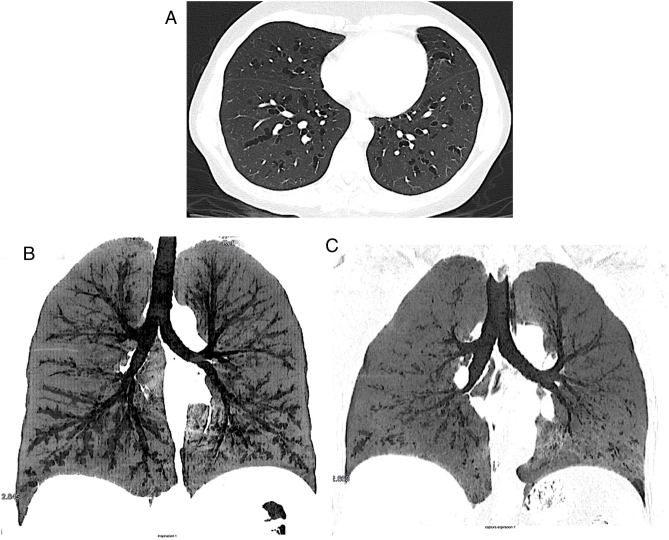
A 57-year-old female, with repetitive episodes of cough, upper airway symptoms and moderate exertion dyspnea, showed multiples centrals bilaterals bronchiectasis in bronchus from 3rd to 8th generation sparing periphery on a chest computed tomography (CT) as part of her cough tests (Fig. 1a), respiratory functional tests were normal, but after analyzing the CT images, we decided to perform a low-dose CT during full expiration (Fig. 1b, c), this showed an approximately 80% collapse of the previously ecstatic bronchi, this was consistent with cartilage deficit and with Williams-Capmbell syndrome.
Fig. 1.
(a) Shows the centrals bronchiectasis and how they change during the inspiration (b) and expiration (c) chest CT.
Williams-Campbell syndrome is a rare syndrome consisting of a total or partial deficit of the subsegmental bronchi cartilage, usually affecting between the 4th and 6th generation, this results in bronchiectasis in the affected bronchi. This syndrome is generally diagnosed in childhood due to its congenital nature1; however other authors speak about the possibility of secondary acquisition.2
The diagnosis of this syndrome usually requires bronchoscopy, in our case expiration/inspiration CT was enough for diagnosis. Taking into account CT its non-invasive methodology, easy of execution and good patient tolerance, and considering lung biopsy has several complications, the expiratory/inspiratory chest CT procedure should be included in patients with central diffuse cylindrical bronchiectasis.1
Informed consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Funding
The authors declare that no funding was received for this article.
Authors’ contribution
All authors have contributed significantly to the research and preparation, revision and final production of the manuscript and approve its submission.
Conflict of interest
The authors declare to have no conflict of interest directly or indirectly related to the manuscript contents.
References
- 1.Noriega Aldave A.P., William Saliski D.O. The clinical manifestations, diagnosis and management of Williams-Campbell syndrome. N Am J Med Sci. 2014 doi: 10.4103/1947-2714.1416201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Manzke, H., n.d. Irreversible generalized pulmonary emphysema resulting from destructive bronchitis and bronchiolitis following adenovirus infection. Klin Padiatr 194, 387–92. 10.1055/s-2008-1033842. [DOI] [PubMed]