Abstract
Purpose:
To examine the longitudinal associations between parental perceptions of their child’s actual weight (PPCA=parental perception of child’s actual) and ideal weight (PPCI=parental perception of child ideal) in early childhood and the child’s own perceptions of their actual weight (APA=adolescent perceived actual) and ideal weight (API=adolescent perceived ideal) during early adolescence among a low income population.
Methods:
Using a longitudinal study design, 136 child/parent pairs were asked to assess the child’s actual and ideal weight using figure rating scales. When children were 4-7 years old, parents reported on their perception of their child’s weight; when children were 10-12 years old, the child reported on their own weight perceptions. Actual weight, ideal weight, and the difference between ideal and actual weight perception were assessed at the respective timepoints. Regressions were used to examine the relationship between parental weight perceptions (PPCA and PPCI) and later adolescent weight perception (APA and API).
Results:
On average, PPCI was higher than PPCA, whereas API was lower than APA. We found a positive relationship between PPCI and API (β=0.309, p=.029). PPCA was positively associated with API (β=0.304, p=.015) and marginally positively associated with the APA (β=0.242, p=.077). However, the difference between PPCI and PPCA did not predict either APA or API.
Conclusions:
Parental perception of their child’s weight may relate to the adolescent’s weight perception, particularly ideal weight. However, several null and marginal associations suggest that parental weight perception in early childhood may not be the most salient factor in determining weight perception in early adolescence.
Level of Evidence:
Level III, well designed longitudinal cohort study.
Keywords: weight perception, parental weight perception, childhood, adolescence, weight
Introduction
The prevalence of eating disorders worldwide has increased over time [1]. Approximately 8.4% of women and 2.2% of men will develop an eating disorder in their lifetime, and millions more will have a subthreshold eating disorder [2]. Eating disorders are an important public health concern, as they are debilitating diseases and are associated with numerous physical and mental conditions including anxiety [3], increased risk for suicidality [4], cardiac arrhythmias [5], and lower bone mineral density [6]. Adolescence is a period of critical importance in the development of eating disorders due to puberty-related changes in body shape and composition accompanied by societal pressures surrounding appearance that occur during that time [7]. It is estimated that 90% of eating disorder onset occurs between the ages of 12-25 [8], making the early adolescent years immediately preceding this age range a critical period for preventive interventions.
One risk factor for eating disorders that has garnered attention in recent years is weight perception, including one’s perception of both their actual and ideal weight. Research has consistently shown that adolescents who perceive themselves to be overweight are more likely to report trying to lose weight or being on a diet [9, 10], which is a risk factor for future eating disorder onset [11]. Further, adolescents who perceive themselves as overweight are more likely to engage in disordered weight control behaviors compared to adolescents who perceive themselves to be ‘about the right weight’ [12–14]. Eating disorders are also often characterized by perceiving one’s actual weight as higher than it actually is, and reporting a lower ideal weight, making weight perception a salient issue in eating disorders prevention [15, 16]. Thin-ideal internalization, the belief that thinness equates to beauty and the extent to which an individual has the desire to conform to this beauty ideal [17], is also a strong predictor of future eating disorders and eating pathology [17, 18]. Given the associations between eating disorder risk and individuals’ weight perceptions, research examining predictors of both perceived actual and ideal weight is needed. Outside of eating disorder risk, perceiving oneself as overweight in adolescence is associated with numerous other negative health-related outcomes including higher blood pressure over time [19], less healthy dietary intake and reduced physical activity [9], more weight gain over time [20], and worse physical, emotional, social, and school health-related quality of life [21].
While there have been many studies examining the implications of weight perception, few studies have attempted to understand predictors of weight perception in adolescence. One area of interest is early childhood parental perception of their child’s weight. Parent’s weight perception of their child may alter interactions with their child, which could in turn impact the child’s own perceptions [22]. Specifically, parents who perceive their child to be overweight, irrespective of their actual weight, were less likely to restrict their child’s screen time, or provide healthy dietary and physical activity behaviors for them [23]. Additionally, parents may be more likely to make comments about their child’s weight which may impact the child’s body satisfaction [24]. In support of this potential link are findings from a longitudinal study that found that fathers’ perception of their child’s weight during adolescence predicted later adolescent weight concern [22]. These findings suggest that having a weight that is higher than what is considered ideal by parents may lead a child to idealize a lower weight, suggesting that the deviation of the child’s actual body weight from the parent’s ideal may be an important factor to consider. Ultimately, the role of parental weight perception on a child’s weight perception may have implications for the development of eating disorders.
Given the potential importance of parental weight perception on adolescent weight perception, the overall objective of the study was to determine if parents’ perceptions in early childhood of their child’s actual weight (PPCA=parent’s perception of their child’s actual weight in early childhood) and ideal weight (PPCI=parent’s perception of their child’s ideal weight in early childhood) prospectively predict the adolescent’s self-perception of their actual weight (APA=adolescent’s perception of their actual weight in early adolescence) and ideal weight (API=adolescent’s perception of their ideal weight in early adolescence). In this study we had 3 hypotheses: 1) Parents perceiving their children to have a higher body weight in early childhood (i.e. higher PPCA) would predict adolescents perceiving themselves to have a higher body weight (i.e. higher APA) and lower ideal weight (i.e. API), 2) that parents perceiving their children to have a higher ideal weight (i.e. higher PPCI) in early childhood would be associated with adolescents perceiving themselves to have a higher body weight (i.e. higher APA) and higher ideal weight (i.e. higher API) in early adolescence, and 3) parents believing that their child had a higher body weight than ideal (i.e. PPCA>PPCI) in early childhood would predict adolescent’s believing themselves to have a higher body weight (i.e. higher APA), lower ideal weight (i.e. lower API), and adolescents’ would believe themselves to have a higher body weight than ideal (i.e. APA> API) in early adolescence.
Methods
Participants and Study Design
The present study utilized data from the ABC (Appetite Behavior and Cortisol) Study, a longitudinal study of children’s eating behaviors [25]. Child/parent pairs were initially recruited from Head Start in Southeastern Michigan, a federally funded preschool program for low-income children. Children and a parent (their primary caregiver and legal guardian) were invited to participate in a study about their child’s eating behaviors. Exclusion criteria at the time of recruitment into the original cohort were: the parent or child did not speak English, parent had a bachelor’s degree or higher, child was in foster care, child had food allergies, child had significant medical problems or perinatal complications, or child had a gestational age less than 35 weeks. Participants were invited at later points to participate in two follow-up studies being utilized in the present research which had the same exclusion criteria as the original study. The present study utilized data from the early childhood (approximately 4-7 years of age) and early adolescent (approximately 10-12 years of age) follow-up waves of the study [26] and consisted of 136 child/parent pairs. For recruitment into the early childhood wave of data collection, families were told that the purpose of the study was, “to understand how mothers and caregivers feed their children.” For recruitment into the early adolescent data wave, families were told that the purpose of the study was, “understanding the kinds of things that affect kids’ eating habits as they get older.” Data collectors met with families in community locations. At both time points, children’s weight and height were measured. Parents responded to questionnaires at both time points, and children participated in questionnaires at only the early adolescent time point. Both studies were approved by the Institutional Review Board at the University of Michigan.
Measures
Parental Weight Perception.
When their child was in early childhood, the parent was shown the Children’s Body Image Scale (CBIS)[27] which includes seven age and sex specific silhouettes of increasingly higher body weights. The CBIS was developed so that ratings represented the following body mass index percentiles according to CDC growth charts: 1=3rd percentile, 2=10th, 3=25th, 4=50th, 5=75th, 6=90th and 7=97th. To assess PPCA, parents were first asked, “Looking at these pictures of [child’s age] [girls or boys], which picture best shows your child’s body type?” Then, to assess PPCI parents were asked, “Looking at these pictures, which picture best shows the ideal body type for a child this age?” PPCA as well as the PPCI for a child of the same age and gender, were therefore each rated 1 to 7, with higher scores indicating a higher weight. From these ratings, we calculated the difference (Δ) between PPCI and PPCA, resulting in a continuous score ranging from −6 to +6. Negative values indicate that the PPCI was lower than the PPCA (i.e. parents perceive their child to weigh more than is ideal) and positive values indicating that the PPCI was higher than the PPCA (i.e. parent’s perceive their child’s weight to be lower than is ideal); a value of 0 indicated that the PPCI was the same as the PPCA. From this continuous variable, we also created a categorical variable: no difference (Δ=0), PPCI higher than PPCA (Δ= a positive value), and PPCI less than PPCA (Δ= a negative value).
Child Weight Perception.
When the child was approximately 10-12 years old (early adolescence) the child was shown the Contour Drawing Rating Scale [28] which includes 9 sex specific silhouettes of increasingly higher body weights. The scale was not developed to represent specific BMI percentiles, rather authors developed the scale so that ratings of 1 to 3 represented individuals perceived as potentially “underweight”, 4 to 6 as “normal weight”, and 7-9 as “overweight”. The Contour Drawing Rating Scale was developed with high test-retest reliability (r=0.78) and validity among undergraduate students [28] which has been extended by other researchers to have high test-retest reliability (r=0.84 at two weeks, r=0.77 at 14 weeks) and high construct validity for body dissatisfaction among early adolescent girls [29]. To assess APA, adolescents were first asked to, “Choose the number on the line closest to your present size. That is, the size you are at the moment.” Then to assess API, adolescents were asked to, “Choose the number on the line closest to your ideal size. That is the size you would like to be.” The APA and API were therefore each rated 1 to 9, with higher scores indicating a higher weight. From these ratings, we calculated the difference (Δ) between the API and APA, resulting in a continuous score ranging from −8 to +8, with a negative value indicating that the API was lower than the APA (i.e. adolescents perceiving they weigh more than is ideal) and positive values indicating that the API was higher than APA (i.e. adolescents perceiving their weight to be lower than ideal); a value of 0 indicated that the API was the same as the APA. From this continuous variable, we also created a categorical variable: no difference (Δ=0), API higher than APA (Δ= a positive value), and API less than APA (Δ= a negative value). The difference between the API and APA is often used as a marker of body dissatisfaction, with a difference of 0 indicating body satisfaction and any positive or negative value indicating body dissatisfaction [30].
Sociodemographic Characteristics.
The child’s birthdate, sex, and race/ethnicity were reported by the parent in early childhood. Age at the study visits was calculated using the reported birthdate. Children were weighed and measured using a Detecto Portable Scale Model no. DR550 and a Seca 217 portable stadiometer. From these measurements, body mass index (BMI) was calculated and BMI z-scores were determined based on the sex-specific standards set forth by the US Centers for Disease Control and Prevention [31].
Statistical Analysis
Univariate statistics were used to describe the study sample. To test our hypotheses, we used multiple regression models adjusting for the child’s race/ethnicity, sex, age at early childhood assessment, measured BMI z-score at early childhood, and parental BMI at early childhood. We used 9 models to test the associations of each of 3 predictors as continuous variables (PPCA, PPCI, and Δ [PPCI - PPCA]) with each of 3 outcomes (APA, API, and Δ [API - APA]), In addition we ran 3 models utilizing the Δ in parental perception as a categorical variable, with Δ=0 being the reference category. Adjusted betas and p-values were calculated and are reported for all models. Results were considered statistically significant if p<0.05. Findings with p<0.10 were determined to be of marginal significance. All analyses were conducted using SAS 9.4.
Results
Demographic characteristics of the children can be found in Table 1. There were more females (53.7%) than males in the sample. Over half of the children were non-Hispanic White (53.7%) and among the other race/ethnicity participants, there was a high proportion of biracial children (19.1%). The cohort of children had an average age of 72.5 months during the early childhood data collection wave, and 129.2 months at the early adolescence data collection wave. At early childhood, approximately one quarter (25.6%) of children had a BMI at or above the 95th percentile, one fifth (20.8%) had a BMI at or above the 85th percentile but less than the 95th percentile, and 53.6% of children had a BMI below the 85th percentile.
Table 1.
Demographic characteristics of children in the sample (n=136), n (%) or mean (SD)
| N (%) | |
|---|---|
| Sex | |
| Female | 73 (53.7) |
| Male | 63 (46.3) |
| Race/Ethnicity | |
| Non-Hispanic White | 73 (53.7) |
| Other | 63 (46.3) |
| Mean (SD) | |
|
| |
| BMI z-score at early childhood | 0.97 (0.98) |
| Age in months at early childhood | 72.5 (7.2) |
| Age in months at early adolescence | 129.2 (6.5) |
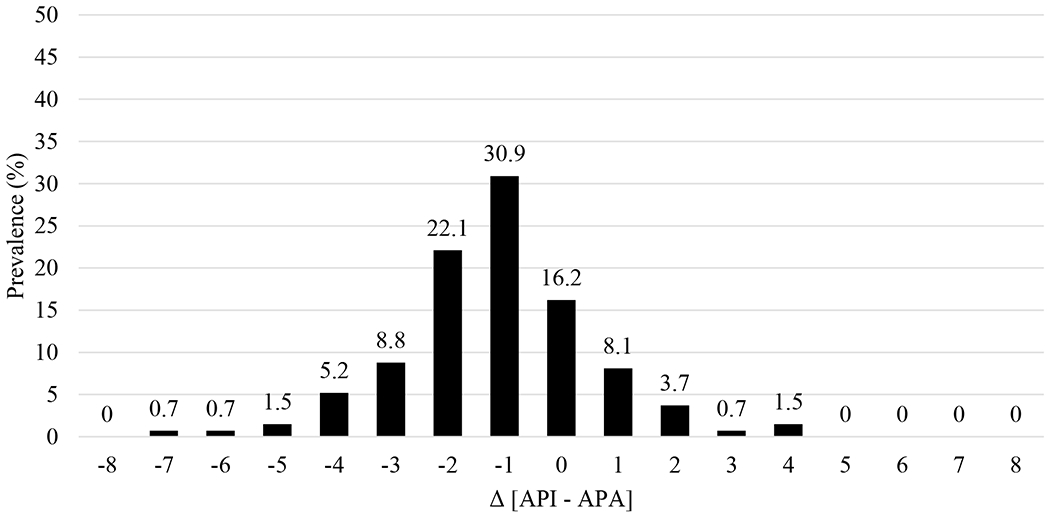
Distributions of parental and adolescent weight perceptions are shown in Figures 1–4. In early childhood, mean PPCA was 3.32, and mean PPCI was 3.45 (both values representing BMIs between the 25th- 50th percentiles) as seen in Figure 1. Parents rated the ideal weight of a child as higher than their perception of their own child’s weight (Δ [PPCI – PPCA] M=0.13). In early childhood, no parents selected the largest silhouette (7, representing a BMI at the 97th percentile) as the ideal weight of a child and only 10.3% selected an ideal weight ≥ 5 (representing a BMI ≥ 75th percentile). Distribution of Δ [PPCI – PPCA] can be found in Figure 2.
Figure 1.
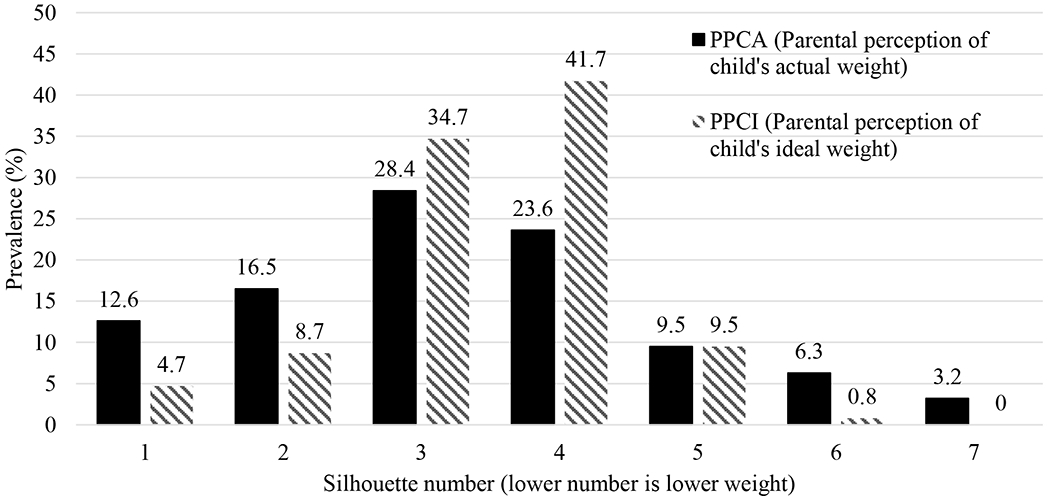
Parental perception of their child’s actual weight (PPCA) and ideal weight (PPCI) in early childhood on Children’s Body Image Scale (CBIS)[27]
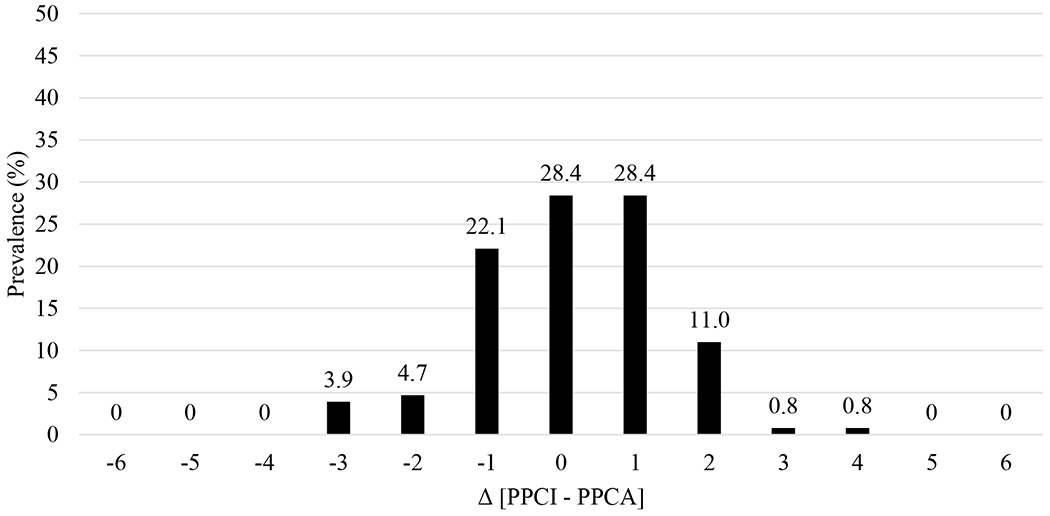
Figure 4.
Difference in adolescent’s self-perception of their ideal weight (API) and their actual weight (APA) on Contour Drawing Rating Scale [28]
*The difference between API and APA is a marker of body dissatisfaction. A difference of 0 indicates body satisfaction; negative numbers indicate adolescents perceiving they weigh more than is ideal; positive numbers indicate adolescents perceiving their weight to be lower than ideal.
Figure 2.
Difference in parent’s perception of their child’s ideal weight (PPCI) and actual weight (PPCA) in early childhood on Children’s Body Image Scale (CBIS)[27]
*Negative numbers indicate parents perceive their child to weigh more than is ideal; positive numbers indicate parents perceive their child’s weight to be lower than is ideal.
APA and API distributions can be found in Figure 3. The mean value for APA was 5.07 (representing a weight in “normal” range) and mean API was 3.91 (between values representing “underweight” and “normal” weight). On average, adolescents rated their ideal weight as lower than their perceived actual weight (Δ [API – APA] M=−1.15). At least one adolescent selected each of the nine silhouettes as their perceived actual weight and silhouettes 1-8 were selected by at least one adolescent as their ideal weight. Distribution of Δ [API – APA] can be found in Figure 4.
Figure 3.
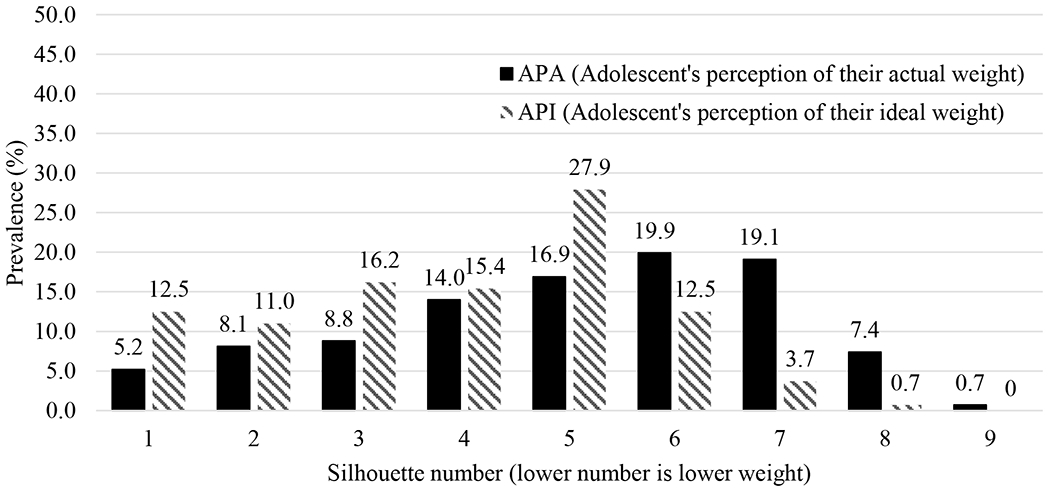
Adolescent’s perception of their actual weight (APA) and ideal weight (API) in early adolescence Contour Drawing Rating Scale [28]
Overall, the distribution of API skewed lower than PPCI. In addition, 69.9% of adolescents believed their actual weight was higher than ideal whereas 30.7% of parents believed that their child’s actual weight was higher than ideal in early childhood.
Parent’s perception in early childhood of child’s actual weight (PPCA) predicting adolescent weight perceptions
Results from multiple linear regressions can be found in Table 2. PPCA was marginally positively associated with APA (β=0.242, p=.077), positively associated with API (β=0.304, p=.015), but was not associated with the Δ [API – APA] (i.e., body dissatisfaction).
Table 2.
Relationship between parental perception ot child’s weight in early childhood and child’s perception of their own weight in early adolescence
| Predictor: Parent’s perception in early childhood | Outcome: Adolescent’s self-perception | β (SE)a | p-value |
|---|---|---|---|
| Child’s actual weight (PPCA) | Actual weight (APA) | 0.242 (0.136) | .077 |
| Ideal weight (API) | 0.304 (0.123) | .015 | |
| Δ [API-APA] | 0.061 (0.132) | .644 | |
|
| |||
| Ideal weight of a child (PPCI) | Actual weight (APA) | 0.227 (0.154) | .143 |
| Ideal weight (API) | 0.309 (0.140) | .029 | |
| Δ [API-APA] | 0.082 (0.149) | .585 | |
|
| |||
| Δ [PPCI-PPCA] | Actual weight (APA) | −0.083 (0.157) | .596 |
| Ideal weight (API) | −0.080 (0.144) | .581 | |
| Δ [API-APA] | 0.004 (0.151) | .981 | |
All models adjusted for child’s race/ethnicity, sex, age at early childhood assessment, BMI z-score at early childhood assessment, and parental BMI at early childhood assessment.
Parent’s perception in early childhood of ideal weight of a child (PPCI) predicting adolescent weight perceptions
PPCI was not associated with the APA or the Δ [API – APA] (i.e., body dissatisfaction). However, PPCI was positively associated with the API (β=0.309, p=0.029).
Difference in parent’s perception of ideal child weight compared to actual weight of child (Δ [PPCI – PPCA]) predicting adolescent weight perceptions
In models utilizing the difference in parent’s perception in early childhood of ideal weight compared to actual weight of their child (Δ [PPCI – PPCA]) as a continuous variable, the Δ [PPCI – PPCA] was not associated with the child’s report in adolescence of perceived actual weight (APA), ideal weight (API) or difference in the adolescent’s perceived ideal and actual weights Δ [API – APA] (i.e., body satisfaction).
Results utilizing the difference in parent’s perception in early childhood of ideal weight compared to actual weight of their child (Δ [PPCI – PPCA]) as a categorical variable can be found in Table 3. For children whose parents thought they were above or below ideal, they did not have significantly different perceptions of their own actual weight (APA), or difference in their perceived ideal and actual weights Δ [API – APA] (i.e., body satisfaction) compared to children whose parents who believed their children had matched ideal and actual weights. However, having parents rate their child’s ideal weight as higher than their actual weight in early childhood compared to equal is marginally associated with the child having a higher ideal weight in early adolescence (β=0.686 p=0.052).
Table 3.
Relationships between child’s perceptions of their own weight in early adolescence and difference in parental perception of child’s ideal and actual weight (Δ [PPCI – PPCA]) as a categorical predictor in early childhood
| Outcome: Adolescent Self-Perception | Predictor: Parents Categorical Δ [Ideal (PPCI) –Actual weight (PPCA)] | β (SE)a | p-value |
|---|---|---|---|
| Actual weight (ACA) | Δ < 0 | 0.497 (0.430) | .250 |
| Δ = 0 | REF | REF | |
| Δ > 0 | 0.183 (0.385) | .636 | |
|
| |||
| Ideal weight (ACI) | Δ < 0 | 0.626 (0.389) | .111 |
| Δ = 0 | REF | REF | |
| Δ > 0 | 0.686 (0.349) | .052 | |
|
| |||
| Δ [ACI - ACA] | Δ < 0 | 0.130 (0.412) | .753 |
| Δ = 0 | REF | REF | |
| Δ > 0 | 0.503 (0.370) | .176 | |
All models adjusted tor child–s race/ethnicity, sex, age at early childhood assessment, BMI z-score at early childhood assessment, and parental BMI at early childhood assessment.
Discussion
The objective of this study was to determine if parental perceptions of their child’s weight in early childhood prospectively predicted the child’s own weight perception during early adolescence. We found that few parents believed in early childhood that their child’s weight was higher than ideal, whereas most early adolescents believed that their weight was higher than ideal. In longitudinal analyses, parental perception in early childhood of their child’s actual weight, as well as the ideal weight of a child, were positively associated with the adolescent’s perceived ideal weight (but not the adolescent’s perceived actual weight). In addition, compared to parents who reported in early childhood that their child’s actual weight matched the ideal weight of a child, perceiving the child’s actual weight as higher than ideal was marginally associated with the adolescent perceiving a higher weight to be ideal.
The present study extends existing literature on both parental weight perception and weight perception in adolescence. Prior research has shown that adolescents who perceive themselves to have a higher body weight have higher rates of body dissatisfaction [32]. Therefore, the positive association between the parent’s perception of their child’s weight and the adolescent’s ideal weight was unexpected. This may be due in part to adolescents’ acceptance of their body weight, and less internalization of the thin ideal. Similar to previous findings which show that parents generally do not recognize their children as overweight, nor do they perceive their child to be larger than they actually are [33], few parents in our study rated their child’s ideal body weight as lower than it actually was in early childhood. The observed marginal positive association between parental perception of their child’s actual weight in early childhood and the adolescent’s perception of their actual weight may be due to the relationships between dieting, weight perception, and weight gain. Previous research has shown that parents who perceive their child to be overweight (i.e., above their ideal) are more likely to encourage them to diet [34]. These children also tend gain more weight over time compared to children whose parents think their children are about the right weight [35], perhaps in part as a result of failed weight loss attempts leading to future weight gain [36].
Congruent with our hypothesis, adolescents whose parents believed that their ideal weight was higher than their actual weight in early childhood had a higher perceived ideal weight in early adolescence, although this relationship did not meet statistical significance. However, contrary to our hypothesis, adolescents with parents who believed that their weight was higher than ideal in early childhood had a higher ideal weight, although this association also did not reach statistical significance. Interestingly, we found that no form of parental weight perception predicted the difference between adolescent’s ideal and actual body weights. Because parental perception of their adolescent’s weight is known to predict future weight concern [22], it may be that early childhood is before the period where children are vulnerable to their parents’ beliefs about their body. Further, unique features of this population (e.g. poverty and socioeconomic-related stressors) may make parental weight perception a less salient predictor of adolescent weight perception.
This study had several key strengths, particularly the longitudinal design that allowed us to examine how early childhood exposures predicted early adolescent weight perception. Further, we were able to use silhouettes to assess weight perception rather than a multiple-choice questionnaire which allowed us to examine weight perception in a more nuanced way than in prior work which largely uses single item questions. Specifically, we were able to treat perception as a semi-continuous variable rather than categorical with terms such as ‘underweight’ and ‘overweight’. While the Children’s Body Image Scale is a validated measure among children self-identifying their own weight perceptions [27], to our knowledge it has not yet been tested for reliability and validity among parents identifying their perception of their child’s weight. Height and weight were also measured, which allowed us to adjust for BMI more accurately in these relationships rather than using self-reported measurements. While adolescent weight perception is well studied, this is the first to our knowledge to examine weight perception in early adolescence specifically. However, the study was not without limitations. Firstly, the sample size was relatively small which may have limited our ability to detect associations. Further, the sample was recruited from a low-income population, and the results may therefore not be generalizable to other populations, although they do provide valuable information among this population. Additionally, weight perceptions were generated from a single measure. However, the evidence suggests that more sophisticated methods of estimating body weight do not provide a large increase in validity [37]. We also were not able to adjust for the child’s own weight perceptions at baseline.
The findings from the current study provide important information about early adolescent weight perception, particularly predictors of weight perception in early childhood. Specifically, parental perception of their child’s weight is associated with early adolescents’ weight perception, particularly ideal weight, which could ultimately impact the child’s health, including their eating disorder risk. We found several null and marginal associations between parental and adolescent weight perceptions, suggesting that parental weight perception in early childhood may not be the most salient factor in determining weight perception during early adolescence in this population. The largely null results indicate that further research is needed to determine the factors that impact adolescent weight perception, given the health implications of weight perception in adolescence. Specifically, the longitudinal relationships between parental and child weight perception should be explored in larger and more economically and racially diverse populations, as well as parental perception of their child’s weight in later childhood, sex specific relationships, and potential mediators and moderators. In addition, other social and behavioral predictors of adolescent weight perception should be explored.
What is already known on this subject?
While research has examined effects of weight perception, little is known about what may influence weight perception in adolescence.
What your study adds?
This study adds valuable information on the potential impacts of parental weight perception, as well as understanding on what may influence adolescent weight perception.
Funding:
The data collected and used for the present study was supported by grant # R01DK098983 (MPI’s: Julie Lumeng/Alison Miller) and R01HD061356 (PI: Julie Lumeng) from the National Institutes of Health and grant # SDG25700093 (PI: Kendrin Sonneville) from the American Heart Association. Additionally, the corresponding author’s time was partially supported by Grant Number T32MH082761 from the National Institute of Mental Health (PI: Scott Crow). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health, National Institute of Health, or the American Heart Association.
Footnotes
Conflicts of interest/Competing interests: The authors declare that they do not have any conflicts of interest.
Ethics approval: Both study waves of the ABC study were approved by the Institutional Review Board at the University of Michigan. Consent from parents and assent from the child were obtained prior to their participation in the study.
Consent for publication: No identifying details were included, and thus, consent for publication is not applicable.
Code availability: Code for this study is not publicly available
Availability of data and material:
Data from the Appetite Behavior and Cortisol Study are not publicly available.
References
- 1.Galmiche M, Déchelotte P, Lambert G, Tavolacci MP: Prevalence of eating disorders over the 2000–2018 period: a systematic literature review. The American Journal of Clinical Nutrition, 109, 1402–1413, 2019. [DOI] [PubMed] [Google Scholar]
- 2.Hay PJ, Mond J, Buttner P, Darby A: Eating disorder behaviors are increasing: findings from two sequential community surveys in South Australia. PLoS One, 3, e1541,2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hudson JI, Hiripi E, Pope HG Jr., Kessler RC: The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry, 61, 348–358, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smith AR, Zuromski KL, Dodd DR: Eating disorders and suicidality: what we know, what we don’t know, and suggestions for future research. Curr Opin Psychol, 22, 63–67, 2018. [DOI] [PubMed] [Google Scholar]
- 5.Klein-Weigel P, Rein P, Kronenberg F, List E, Kinzl J, Biebl W, Fraedrich G: Microcirculatory assessment of vascular acrosyndrome in anorexia nervosa and analysis of manifestation factors. J Psychosom Res, 56, 145–148, 2004. [DOI] [PubMed] [Google Scholar]
- 6.Herzog W, Minne H, Deter C, Leidig G, Schellberg D, Wuster C, Gronwald R, Sarembe E, Kroger F, Bergmann G, et al. : Outcome of bone mineral density in anorexia nervosa patients 11.7 years after first admission. J Bone Miner Res, 8, 597–605, 1993. [DOI] [PubMed] [Google Scholar]
- 7.Klump KL: Puberty as a critical risk period for eating disorders: a review of human and animal studies. Horm Behav, 64, 399–410, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Substance Abuse and Mental Health Services Administration: Handout - Eating Disorders. In: Services C.f.M.H. (Ed.), 2003. [Google Scholar]
- 9.Hahn SL, Borton KA, Sonneville KR: Cross-sectional associations between weight-related health behaviors and weight misperception among U.S. adolescents with overweight/obesity. BMC Public Health, 18, 514, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rahman M, Berenson AB: Self-perception of weight and its association with weight-related behaviors in young, reproductive-aged women. Obstet Gynecol, 116, 1274–1280, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Striegel-Moore RH, Bulik CM: Risk factors for eating disorders. Am Psychol, 62, 181–198, 2007. [DOI] [PubMed] [Google Scholar]
- 12.Hazzard VM, Hahn SL, Sonneville KR: Weight misperception and disordered weight control behaviors among U.S. high school students with overweight and obesity: Associations and trends, 1999-2013. Eat Behav, 26, 189–195, 2017. [DOI] [PubMed] [Google Scholar]
- 13.Eichen DM, Conner BT, Daly BP, Fauber RL: Weight perception, substance use, and disordered eating behaviors: comparing normal weight and overweight high-school students. J Youth Adolesc, 41, 1–13, 2012. [DOI] [PubMed] [Google Scholar]
- 14.Ibrahim C, El-Kamary SS, Bailey J, St George DM: Inaccurate weight perception is associated with extreme weight-management practices in U.S. high school students. J Pediatr Gastroenterol Nutr, 58, 368–375, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Penas-Lledo E, Bulik CM, Lichtenstein P, Larsson H, Baker JH: Risk for self-reported anorexia or bulimia nervosa based on drive for thinness and negative affect clusters/dimensions during adolescence: A three-year prospective study of the TChAD cohort. Int J Eat Disord, 48, 692–699, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fernandez F, Probst M, Meermann R, Vandereycken W: Body size estimation and body dissatisfaction in eating disorder patients and normal controls. Int J Eat Disord, 16, 307–310, 1994. [DOI] [PubMed] [Google Scholar]
- 17.Thompson JK, Eric S: Thin-Ideal Internalization: Mounting Evidence for a New Risk Factor for Body-Image Disturbance and Eating Pathology. Current Directions in Psychological Science, 10, 181–183. [Google Scholar]
- 18.Stice E, Gau JM, Rohde P, Shaw H: Risk factors that predict future onset of each DSM-5 eating disorder: Predictive specificity in high-risk adolescent females. J Abnorm Psychol, 126, 38–51,2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Unger ES, Kawachi I, Milliren CE, Sonneville KR, Thurston IB, Gooding HC, Richmond TK: Protective Misperception? Prospective Study of Weight Self-Perception and Blood Pressure in Adolescents With Overweight and Obesity. J Adolesc Health, 60, 680–687, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sonneville KR, Thurston IB, Milliren CE, Kamody RC, Gooding HC, Richmond TK: Helpful or harmful? Prospective association between weight misperception and weight gain among overweight and obese adolescents and young adults. Int J Obes (Lond), 40, 328–332, 2016. [DOI] [PubMed] [Google Scholar]
- 21.Farhat T, Iannotti RJ, Summersett-Ringgold F: Weight, Weight Perceptions, and Health-Related Quality of Life Among a National Sample of US Girls. J Dev Behav Pediatr, 36, 313–323, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hochgraf AK, McHale SM, Fosco GM: Interparental conflict and gender moderate the prospective link between parents’ perceptions of adolescents’ weight and weight concerns. Int J Eat Disord, 52, 904–913, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang T, Cai L, Jing J, Ma L, Ma J, Chen Y: Parental perception of child weight and its association with weight-related parenting behaviours and child behaviours: a Chinese national study. Public Health Nutr, 21, 1671–1680, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Neumark-Sztainer D, Bauer KW, Friend S, Hannan PJ, Story M, Berge JM: Family weight talk and dieting: how much do they matter for body dissatisfaction and disordered eating behaviors in adolescent girls? J Adolesc Health, 47, 270–276, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lumeng JC, Miller A, Peterson KE, Kaciroti N, Sturza J, Rosenblum K, Vazquez DM: Diurnal cortisol pattern, eating behaviors and overweight in low-income preschool-aged children. Appetite, 73, 65–72, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Age limits and adolescents. Paediatr Child Health, 8, 577–578, 2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Truby H, Paxton SJ: Development of the Children’s Body Image Scale. Br J Clin Psychol, 41, 185–203, 2002. [DOI] [PubMed] [Google Scholar]
- 28.Thompson MA, Gray JJ: Development and validation of a new body-image assessment scale. J Pers Assess, 64, 258–269, 1995. [DOI] [PubMed] [Google Scholar]
- 29.Wertheim EH, Paxton SJ, Tilgner L: Test-retest reliability and construct validity of Contour Drawing Rating Scale scores in a sample of early adolescent girls. Body Image, 1, 199–205, 2004. [DOI] [PubMed] [Google Scholar]
- 30.Lombardo C, Battagliese G, Pezzuti L, Lucidi F: Validity of a figure rating scale assessing body size perception in school-age children. Eat Weight Disord, 19, 329–336, 2014. [DOI] [PubMed] [Google Scholar]
- 31.Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, Wei R, Curtin LR, Roche AF, Johnson CL: 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 11, 1–190, 2002. [PubMed] [Google Scholar]
- 32.Miller CT, Downey KT: A Meta-Analysis of Heavyweight and Self-Esteem. Personality and Social Psychology Review, 3, 68–84, 1999. [Google Scholar]
- 33.Rietmeijer-Mentink M, Paulis WD, van Middelkoop M, Bindels PJ, van der Wouden JC: Difference between parental perception and actual weight status of children: a systematic review. Matern Child Nutr, 9, 3–22, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Neumark-Sztainer D, Wall M, Story M, van den Berg P: Accurate parental classification of overweight adolescents’ weight status: does it matter? Pediatrics, 121, e1495–1502, 2008. [DOI] [PubMed] [Google Scholar]
- 35.Robinson E, Sutin AR: Parental Perception of Weight Status and Weight Gain Across Childhood. Pediatrics, 137, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Robinson E, Sutin AR, Daly M: Self-perceived overweight, weight loss attempts, and weight gain: Evidence from two large, longitudinal cohorts. Health Psychol, 37, 940–947, 2018. [DOI] [PubMed] [Google Scholar]
- 37.Stunkard A: Old and new scales for the assessment of body image. Percept Mot Skills, 90, 930, 2000. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data from the Appetite Behavior and Cortisol Study are not publicly available.


