Abstract
Objective
Mechanical thrombectomy enables histopathological examination of clots in patients who have suffered acute ischemic strokes. Many studies have described about the relationship between the histopathological compositions of retrieved thrombi and imaging findings, clinical outcomes, and stroke etiology without consensus. In this study, we examined the histological composition of thrombi according to their retrieval site and methods.
Methods
We divided retrieved clots into three parts (those retrieved from the proximal and distal parts of the stent retriever, and those aspirated through the guiding catheter) and then histopathologically analyzed their compositions by measuring the area occupied by red blood cells (RBCs), fibrin/platelets (F/Ps), and white blood cells (WBCs).
Results
Each specimen showed various composition even within the same patient. For example, the area occupied by RBCs was 20.9% ± 12.1%, 30.5% ± 13.5%, and 41.3% ± 16.1% in the clot retrieved from the proximal and distal parts of the stent retriever, and those aspirated through the guiding catheter, respectively.
Conclusion
Histopathological clot composition may vary even within the patient. Further research is needed to investigate more objective methods of histopathological analysis and their clinical significance.
Keywords: clot histopathology, acute ischemic stroke, mechanical thrombectomy
Introduction
Mechanical thrombectomy can be used to obtain thrombi from patients who have suffered acute ischemic strokes. Histopathologically, examining those clots may elucidate the relationship between histopathology and clinical characteristics.
Previous studies have reported on the relationship between the histopathological findings of retrieved thrombi and stroke etiology, without consensus. Many of these studies have measured the areas occupied by red blood cells (RBCs), fibrin/platelets (F/Ps), and white blood cells (WBCs), and examined the relationship between clot composition and clinical characteristics.1–12) However, it is unknown whether the histopathological findings of one cross-section represent the overall composition of the clot. Histopathological composition may differ according to the site of the observed cross-section, even in the same thrombus. One clot formation hypothesis suggests that the original clot causes blood flow stasis, including a new clot to form around the original clot.6–8) Based on this hypothesis, histological analyses using only one sliced specimen for each case might not reflect the entire thrombus. Therefore, we divided retrieved clots into three parts according to their retrieval area and device; the proximal region of the stent retriever, the distal region of the stent retriever, or those aspirated through the guiding catheter, and then histopathologically analyzed the composition of each group. To the best of our knowledge, this is the first study to histopathologically examine clots according to their area of retrieval.
Materials and Methods
Patients
Six consecutive patients who had undergone mechanical thrombectomy as a treatment for acute ischemic strokes caused by occlusion of the internal carotid artery (ICA), middle cerebral artery (MCA), or basilar artery (BA) between July 2019 and December 2019 were enrolled in this study. The subtypes of ischemic stroke were determined according to the Trial of ORG 10172 in Acute Stroke Treatment classification. A case involving atrial fibrillation without significant arteriosclerosis was diagnosed as cardioembolism.
Mechanical thrombectomy procedure
Patients who suffered occlusion of the ICA or MCA underwent simple manual aspiration using inflated Optimo EPD 9F balloon catheters (Tokai Medical Products, Aichi, Japan), which were placed at the origin of the cervical segment of the ICA, followed by thrombectomy with a Solitaire Platinum stent retriever (Medtronic, Minneapolis, MN, USA). Patients who suffered BA occlusion underwent simple thrombectomy with the Solitaire stent retriever.
Histopathological analysis
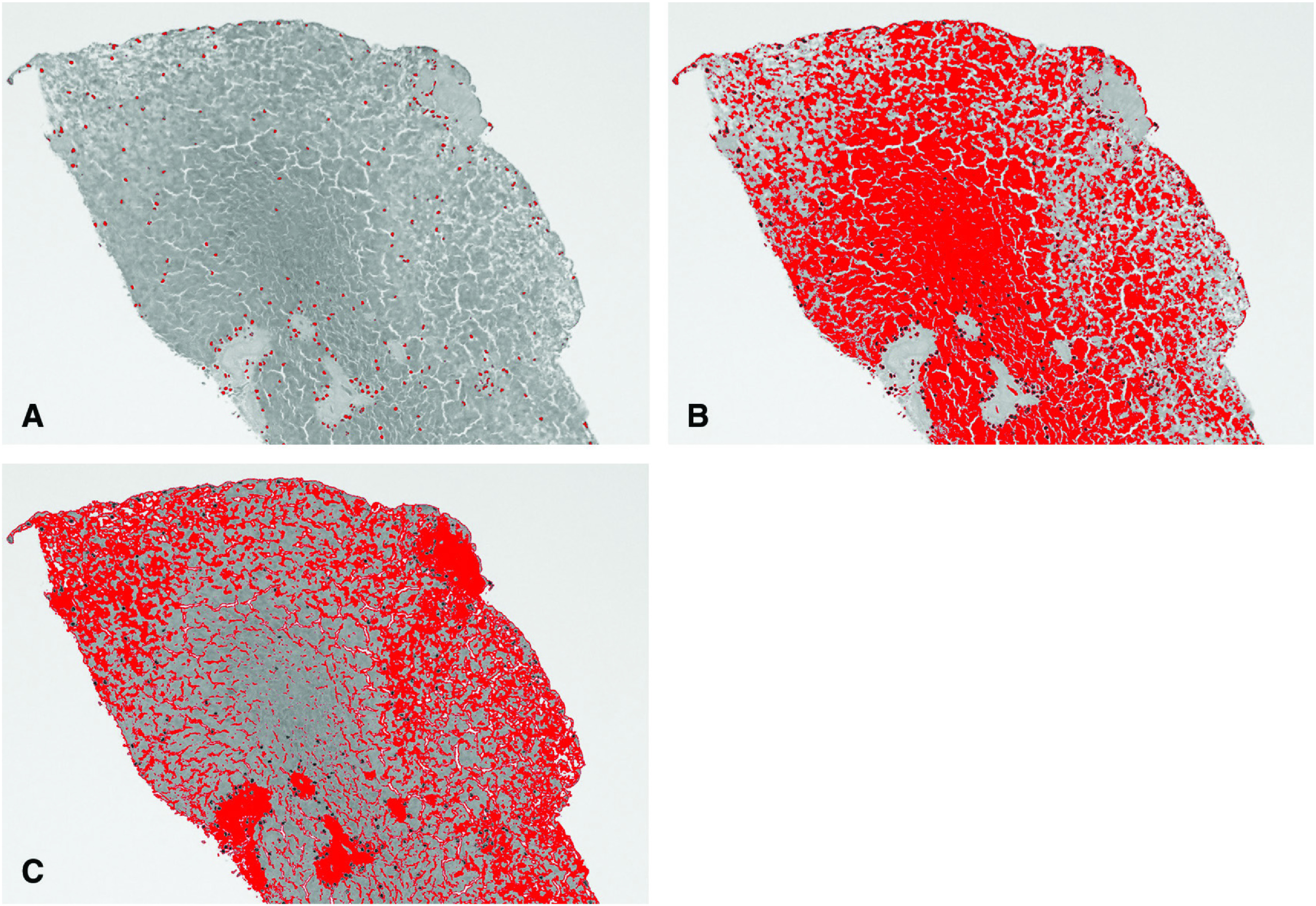
The retrieved thrombus material was divided into three parts; the part retrieved from the proximal region of the Solitaire device, the part retrieved from the distal region of the Solitaire device, and the part aspirated through the guiding catheter. When the clot was retrieved one cluster, it was divided into a proximal half and a distal half. When multiple thrombi were retrieved in the Solitaire device, the most proximal thrombus was sampled as the proximal thrombus, and the most distal one was sampled as the distal thrombus. The thrombi were fixed in 10% formalin, embedded in paraffin, and sliced into 2-μm-thick sections for hematoxylin and eosin staining (Fig. 1). The slides were scanned at ×100 using cellSens Standard software (Olympus, Tokyo, Japan). ImageJ software (National Institutes of Health, Bethesda, Maryland, USA) was employed for the relative quantitative analysis of RBCs, F/Ps, and WBCs using color-based segmentation (Fig. 2). The pictures were converted to grayscale images, then the thresholds of the pixel value were manually set to distinguish between the different cell types and the cells were analyzed automatically. The areas containing each type of cell were measured, and the relative size of each area was calculated. These results were verified by subjecting Masson’s trichrome-stained sections to the same ImageJ-based analysis in some cases.
Fig. 1. Microscopic view of the thrombi retrieved in case 4. (A) Hematoxylin–eosin stained section (100× magnification), WBC (arrows), RBC (arrowheads), and F/P (white arrowheads); (B) Masson’s trichrome-stained section (100× magnification); (C) hematoxylin-eosin stained section (20× magnification). F/P: fibrin/platelet; RBC: red blood cell; WBC: white blood cell.
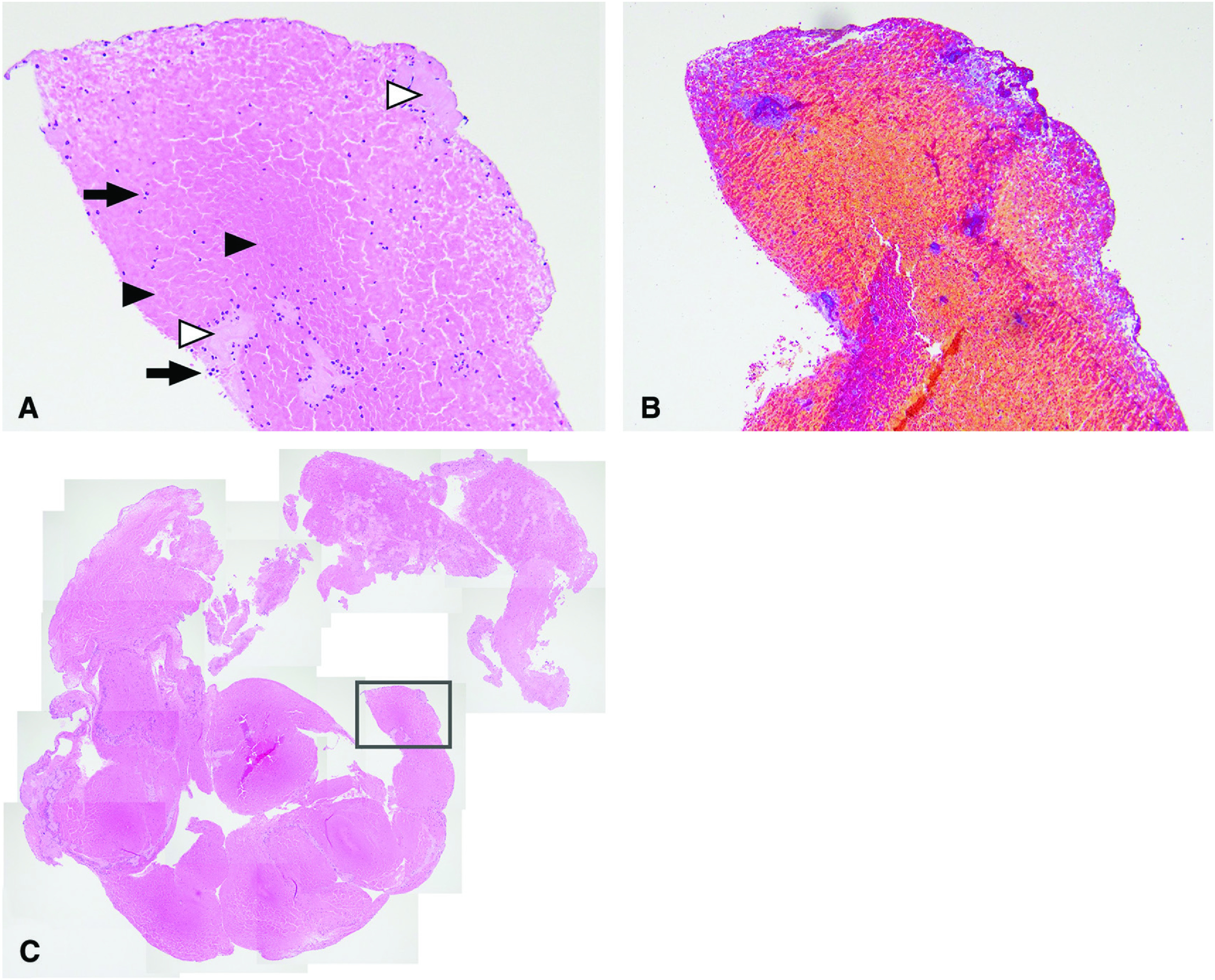
Fig. 2. Histopathological analysis of a retrieved thrombus using the ImageJ software. (A) WBC are depicted in red. (B) RBC are depicted in red. (C) F/P is depicted in red. F/P: fibrin/platelet; RBC: red blood cell; WBC: white blood cell.
Results
Patients’ characteristics
The patients’ characteristics are shown in Table 1. Four patients suffered ICA occlusion, one patient suffered MCA occlusion, and one patient suffered BA occlusion. The subtypes of stroke were classified as large artery atherosclerosis in one case and cardioembolism in five cases. Four patients were treated with intravenous thrombolysis and a recombinant tissue plasminogen activator before mechanical thrombectomy. Mechanical recanalization was accomplished within a mean of 1.5 ± 0.34 passes. Five patients achieved a modified Thrombolysis in Cerebral Infarction (mTICI) score of 3, and one patient achieved an mTICI score of 2B.
Table 1. Patients’ characteristics.
| Case | Age | Sex | NIHSS | Lesion site | Af | HT | HL | DM | Prior antithrombotic therapy | Hyperdense CT sign | WBC (/μg) | Neu (/μg) | CRP (mg/dL) | D-dimer (μg/mL) | Fibrinogen (mg/dL) | t-PA | Onset-to-puncture time (min) | Onset-to-recanalization time (min) | Pass number | TICI grade | mRS | TOAST classification |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 90 | F | 7 | Rt IC | – | + | + | + | – | – | 5320 | 3940 | 0.18 | 2.9 | N/A | + | 395 | 455 | 1 | 3 | 6 | LAO |
| 2 | 79 | M | 15 | Lt IC | + | + | + | + | Warfarin 2 mg | + | 4920 | 2910 | 0.10 | 0.4 | 407 | – | 130 | 520 | 1 | 3 | 2 | CE |
| 3 | 79 | F | 24 | Lt IC | + | + | – | – | Clopidogrel 75 mg | – | 5320 | 3850 | 0.39 | 3.9 | 522 | + | 275 | 310 | 2 | 3 | 5 | CE |
| 4 | 94 | F | 25 | BA | + | + | + | – | Aspirin 100 mg | – | 6600 | 5180 | 0.42 | 4.4 | 378 | – | 210 | 475 | 1 | 3 | 6 | CE |
| 5 | 78 | M | 14 | Rt IC | + | + | + | – | Clopidogrel 75 mg | – | 5530 | 3660 | 0.05 | 1.9 | 375 | + | 145 | 180 | 1 | 3 | 3 | CE |
| 6 | 76 | F | 16 | Lt M1 | – | + | + | – | Clopidogrel 75 mg | + | 4060 | 2900 | 0.82 | 0.4 | 374 | + | 180 | 270 | 3 | 2B | 4 | CE |
Af: atrial fibrillation; BA: basilar artery; CE: cardioembolism; CRP: C-reactive protein; DM: diabetes mellitus; HL: hyperlipidemia; HT: hypertension; IC: internal carotid artery; LAO: large-artery atherosclerosis; mRS: modified Rankin Scale; M1: middle cerebral artery M1 section; Neu: neutrophil count; NIHSS: National Institutes of Health Stroke Scale; t-PA: tissue plasminogen activator; TICI: thrombolysis in cerebral infarction score; TOAST: trial of ORG 10172 in acute stroke treatment; WBC: white blood cells
Histopathological analysis
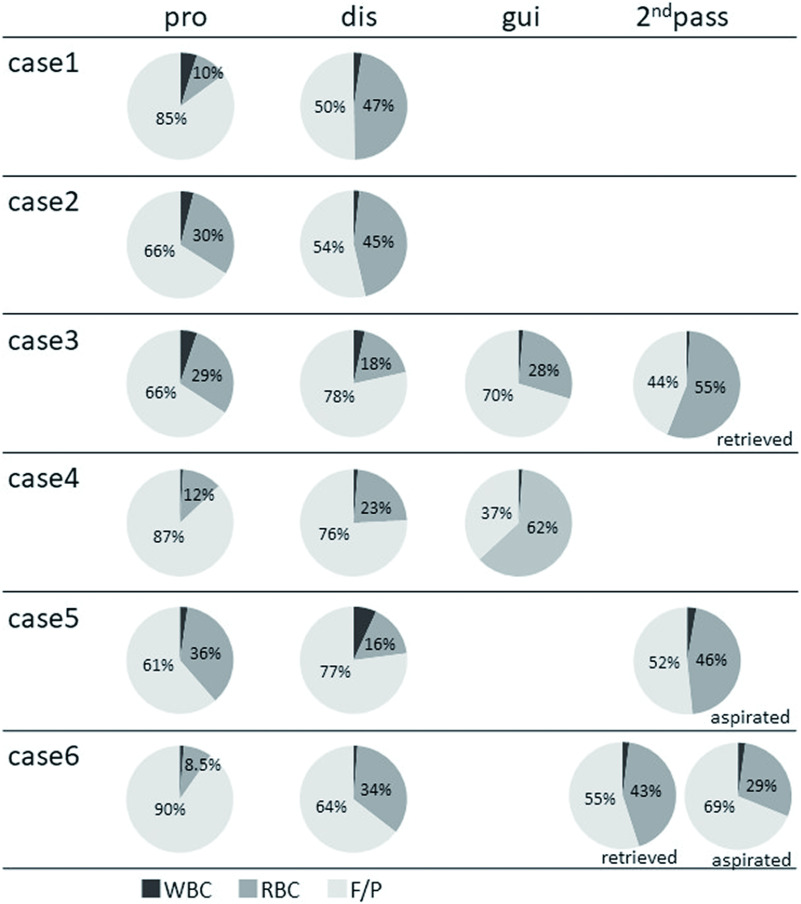
The results of the histopathological analysis are shown in Fig. 3. The mean composition of thrombi was WBCs 2.6% ± 1.7%, RBCs 31.8% ± 15.7%, and F/Ps 65.6% ± 15.0%. In all the specimens, the area occupied by WBCs was the smallest. The area occupied by RBCs was 20.9% ± 12.1%, 30.5% ± 13.5%, and 41.3% ± 16.1% in the clot retrieved from the proximal and distal parts of the stent retriever, and those aspirated through the guiding catheter, respectively. Regarding the retrieved thrombus, clots from the proximal part of the stent retriever had a tendency to have smaller RBCs ratio than that retrieved from the distal part of the stent retriever (Fig. 3). The RBCs ratios tended to be larger in the clots aspirated through the guiding catheter (41.3% ± 16.1%) and those retrieved at the second attempt (43.3% ± 10.8%) (Fig. 3). The histopathological compositions of the clots showed various composition even within the same patient.
Fig. 3. Histopathological composition of thrombus. dis: thrombus retrieved from the distal portion of the Solitaire device; F/P: fibrin/platelet; gui: thrombus aspirated through the guiding catheter; pro: thrombus retrieved from the proximal portion of the Solitaire device; RBC: red blood cell; ret: thrombus retrieved from the Solitaire device at the second attempt; WBC: white blood cell.
Discussion
By dividing retrieved clots into three parts, we showed that clot composition may vary within the same patient. Several studies have examined the relationship between the clinical features and the histopathological findings of retrieved clots, but no consensus has been reached. In terms of imaging findings, the hyperdense artery sign has been associated with RBC-rich thrombi.1–3) Furthermore, one study previously reported that clot permeability, assessed on non-contrast CT and CT angiography, was associated with higher RBC density,4) while another report showed that permeable thrombi strongly correlated with lower fractions of RBC and more F/P conglomerations.5) As for treatment outcomes, some studies have shown that high RBC composition was associated with successful recanalization,6,7) whereas another study reported that a clot with a high number of RBCs had a higher risk of migration, which could lead to worse outcomes.8) Concerning the stroke etiology, several studies reported that the percentage of RBC was higher in clots from patients with cardioembolisms,9,10) but other studies have demonstrated that cardioembolic thrombi contained higher proportions of F/P.11,12)
In all the above studies, only one specimen for each case was subjected to histopathological analysis. Based on our results, it is suspicious whether the histopathological composition of one specimen represents that of the entire thrombus in vivo, which may explain the contradiction in the previous studies.
Some previous studies focused on pathology-specific histological findings. For example, bacteria were detected in clots retrieved from septic emboli caused by infective endocarditis.13,14) Another study reported that cases with thrombi that included vascular wall components were associated with high numbers of device passages and tended to have less frequent successful recanalization.15) Pathology-specific findings can invite clinical suggestions that are not dependent on the composition of the clot.
In this study, the thrombi retrieved from the proximal part of the stent retriever had a tendency to have smaller RBCs ratio than that retrieved from the distal part of the stent retriever. This tendency may relate to the process of clot formation, whereby new clot forms around an original clot.16–18) Histopathological analysis for every divided thrombus may provide new insights into the mechanism of clot formation in acute ischemic stroke. However, there is no evidence that the original construction of the clot in vivo is maintained even in the stent retriever, needing further studies.
We also found that the clots retrieved from the guiding catheter tended to include more RBCs than that retrieved from the stent retriever. This may indicate that stent-retriever thrombectomy has difficulties retrieving RBC-rich clots. Thus, the differing histopathological analysis of thrombi retrieved from different areas in this study may reflect device compatibility, and therefore may offer insight into device selection.
This study has limitations that should be acknowledged. First, it did not include a sufficient number of patients, and the occlusion site was not considered. Second, because the subtypes of stroke were large artery cardioembolism in five cases and atherosclerosis in only one case, our results might not reflect the general population of acute ischemic stroke patient indicated for mechanical thrombectomy. The findings should be viewed as preliminary and further studies are needed to determine the thrombus effect of the retrieved site on histopathological findings in clinical features.
Conclusion
Histopathological clot composition may vary even within the same patient. It may be difficult to evaluate the association with clinical features without considering such differences. We found that the clot composition may differ depending on the position of the clot or the thrombectomy method used, which is meaningful for further research.
Disclosure Statement
The authors have no conflicts of interest that are related to the content of this article.
References
- 1).Maekawa K, Shibata M, Nakajima H, et al. : Erythrocyte-rich thrombus is associated with reduced number of maneuvers and procedure time in patients with acute ischemic stroke undergoing mechanical thrombectomy. Cerebrovasc Dis Extra 2018; 8: 39–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2).Brinjikji W, Duffy S, Burrows A, et al. : Correlation of imaging and histopathology of thrombi in acute ischemic stroke with etiology and outcome: a systematic review. J Neurointerv Surg 2017; 9: 529–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3).Songsaeng D, Kaeowirun T, Sakarunchai I, et al. : Efficacy of thrombus density on noninvasive computed tomography neuroimaging for predicting thrombus pathology and patient outcome after mechanical thrombectomy in acute ischemic stroke. Asian J Neurosurg 2019; 14: 795–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4).Benson JC, Fitzgerald ST, Kadirvel R, et al. : Clot permeability and histopathology: is a clot's perviousness on CT imaging correlated with its histologic composition? J Neurointerv Surg 2020; 12: 38–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5).Berndt M, Friedrich B, Maegerlein C, et al. : Thrombus permeability in admission computed tomographic imaging indicates stroke pathogenesis based on thrombus histology. Stroke 2018; 49: 2674–2682. [DOI] [PubMed] [Google Scholar]
- 6).Shin JW, Jeong HS, Kwon HJ, et al. : High red blood cell composition in clots is associated with successful recanalization during intra-arterial thrombectomy. PLoS One 2018; 13: e0197492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7).Hashimoto T, Hayakawa M, Funatsu N, et al. : Histopathologic analysis of retrieved thrombi associated with successful reperfusion after acute stroke thrombectomy. Stroke 2016; 47: 3035–3037. [DOI] [PubMed] [Google Scholar]
- 8).Maegerlein C, Friedrich B, Berndt M, et al. : Impact of histological thrombus composition on preinterventional thrombus migration in patients with acute occlusions of the middle cerebral artery. Interv Neuroradiol 2018; 24: 70–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9).Gong L, Zheng X, Feng L, et al. : Bridging therapy versus direct mechanical thrombectomy in patients with acute ischemic stroke due to middle cerebral artery occlusion: a clinical- histological analysis of retrieved thrombi. Cell Transplant 2019; 28: 684–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10).Kim SK, Yoon W, Kim TS, et al. : Histologic analysis of retrieved clots in acute ischemic stroke: correlation with stroke etiology and gradient-echo MRI. Am J Neuroradiol 2015; 36: 1756–1762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11).Boeckh-Behrens T, Kleine JF, Zimmer C, et al. : Thrombus histology suggests cardioembolic cause in cryptogenic stroke. Stroke 2016; 47: 1864–1871. [DOI] [PubMed] [Google Scholar]
- 12).Simons N, Mitchell P, Dowling R, et al. : Thrombus composition in acute ischemic stroke: a histopathological study of thrombus extracted by endovascular retrieval. J Neuroradiol 2015; 42: 86–92. [DOI] [PubMed] [Google Scholar]
- 13).Bhaskar S, Cordato D, Cappelen-Smith C, et al. : Clarion call for histopathological clot analysis in “cryptogenic” ischemic stroke: implications for diagnosis and treatment. Ann Clin Transl Neurol 2017; 4: 926–930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14).Bhaskar S, Saab J, Cappelen-Smith C, et al. : Clot histopathology in ischemic stroke with infective endocarditis. Can J Neurol Sci 2019; 46: 331–336. [DOI] [PubMed] [Google Scholar]
- 15).Funatsu N, Hayakawa M, Hashimoto T: Vascular wall components in thrombi obtained by acute stroke thrombectomy: clinical significance and related factors. J Neurointerv Surg 2019; 11: 232–236. [DOI] [PubMed] [Google Scholar]
- 16).Qazi EM, Sohn SI, Mishra S, et al. : Thrombus characteristics are related to collaterals and angioarchitecture in acute stroke. Can J Neurol Sci 2015; 42: 381–388. [DOI] [PubMed] [Google Scholar]
- 17).Zhang R, Zhou Y, Yan S, et al. : Slow collateral flow is associated with thrombus extension in patients with acute large-artery occlusion. AJNR Am J Neuroradiol 2018; 39: 1088–1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18).Minnerup J, Kleinschnitz C: Visualization of clot composition in ischemic stroke: do we get what we see? Stroke 2011; 42: 1193–1194. [DOI] [PubMed] [Google Scholar]