Abstract
The cavernous sinus (CS) is a dural sinus located on each side of the pituitary fossa. Neoplastic and vascular lesions, such as arteriovenous fistulas, frequently involve the CS. This sinus plays a role as a crossroad receiving venous blood flow from the facial, orbital, meningeal, and neural venous tributaries. The relationship between these surrounding relevant veins and the CS, as well as the CS itself, varies anatomically. For safe and effective surgical and endovascular treatment of lesions involving the CS, knowledge of the anatomy and variations of the CS and the relevant surrounding veins is highly important. In this section, the anatomy and variations of the CS and the relevant surrounding veins are outlined.
Keywords: cavernous sinus, laterocavernous sinus, anatomy, relevant veins
Introduction
The cavernous sinus (CS) is the dural sinus that lies on the bilateral sides of the pituitary fossa of the sphenoidal body. It functions as a venous channel receiving many types of venous structures, including facial and orbital veins, meningeal veins, pituitary veins, and cerebral superficial and deep veins. These surrounding venous structures present complex anatomy, and the CS can be affected by neoplasms and vascular disease. Such lesions can be targeted by endovascular treatment. When planning endovascular treatment, the neuronal venous drainage, which can terminate at the CS or other surrounding veins, should be carefully considered. Thus, knowledge of the anatomy and variations of the CS and its surrounding venous structures is important for the treatment of pathological conditions. In this section, the functions and imaging anatomy of the CS and relevant surrounding veins are reviewed.
Basis Anatomy of the CS and Its Variations
Basic anatomy
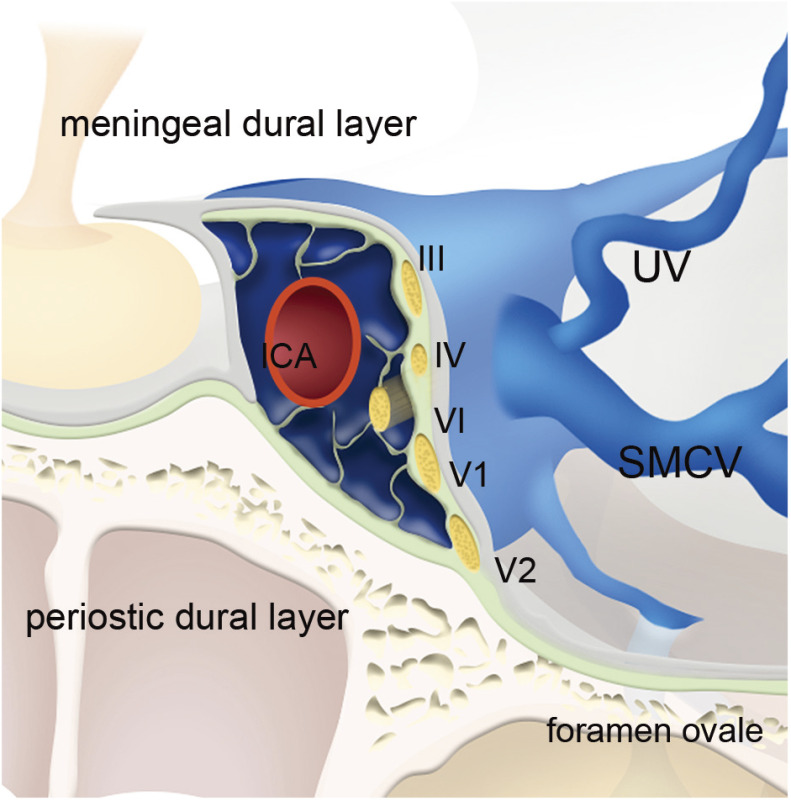
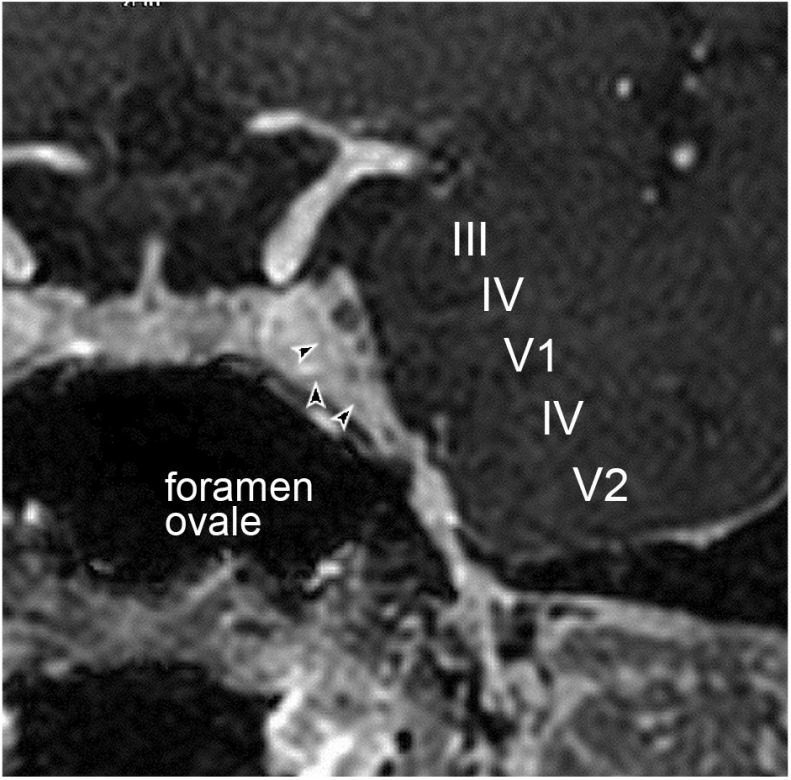
The CS is a dural sinus located between the superior orbital fissure and the petrous apex of the temporal bone at the medial part of the sphenoid body, and is surrounded by periosteum and dura mater. Campero et al. reported that the CS is a dural sinus surrounded by two layers, the outer layer and the inner layer, and the construction of the layers differs depending on the aspects of the sinus.1) The lateral and superior walls of the CS comprise the outer layer and the inner layer. Umansky and Nathan also revealed that the lateral wall of the CS was formed by two layers, the superficial layer and the deep layer.2) According to the report, the superficial layer is the dense fibrous membrane that continues laterally to the middle cranial base, medially to the diaphragma sellae, anteriorly to the sphenoid wing, and posteriorly to the tentorium cerebelli.2) The deep layer is a thin and transparent layer comprising loose connective tissue, which contains the cranial nerves III, IV, V1, and V2 on their way passing through the lateral wall.1,2) The medial wall of the CS consists of a single outer layer. The inner cavity of the CS contains the trabeculated venous channel, through which the internal carotid artery and cranial nerve VI travel (Figs. 1 and 2).
Fig. 1. Schematic drawing of basic anatomy of CS (anterolateral view of coronal section). Lateral and superior walls of the CS comprise meningeal dural layer (gray-colored layer) and periostic dural layer (light green-colored layer). Meningeal dural layer continues laterally to middle cranial base, medially to diaphragm sellae, anteriorly to sphenoid wing, and posteriorly to tentorium cerebelli. Periostic dural layer contains cranial nerves III, IV, V1, and V2 on their way. Medial wall of CS consists of meningeal dual layer. Inner cavity of CS contains trabeculated venous channel, through which ICA and cranial nerve VI travel. CS: cavernous sinus; ICA: internal carotid artery; SMCV: superficial middle cerebral vein; UV: uncal vein; III: third cranial nerve; IV: fourth cranial nerve; V1: first branch of fifth cranial nerve; V2: second branch of fifth cranial nerve.
Fig. 2. MR image of normal CS. Coronal reconstruction of contrast-enhanced fast-field echo MRI demonstrates internal configuration of CS. III, VI, V1, V2, and VI cranial nerves travel through lateral wall and internal part of CS. Linear hypointensity areas indicating trabeculations are also seen (arrowheads). CS: cavernous sinus; III: third cranial nerve; V1: first branch of fifth cranial nerve; V2: second branch of fifth cranial nerve; VI: sixth cranial nerve.
Variations
The formation of the trabeculations in the CS can vary among individuals. According to a previous histological study of 34 CSs, densely formed trabeculations were noted in 18%, some trabeculations running inferiorly in the medial side of the internal carotid artery were noted in 64%, and a few trabeculae were noted in the remaining 18%.3) In another report of 46 CSs, the trabeculations were densely or scarcely observed in 92%, whereas scattered small venous channels were observed within the adipose and connective tissues in 8%.4) Endothelial cell linings were also found on the CS wall and trabeculations.4)
Variations in the locations of the internal carotid artery and cranial nerve VI, and their frequencies were previously reported as follows: type A, both the internal carotid artery and the sixth cranial nerve were surrounded by the venous sinus in 48%; type B, the internal carotid artery was surrounded by the venous sinus and the sixth cranial nerve traveled in the lateral wall of the CS in 24%; type C, both the internal carotid artery and the sixth cranial nerve traveled in the lateral wall in 24%; and type D, the internal carotid artery traveled in the lateral wall and the sixth cranial nerve was surrounded by the venous sinus in 4%.3)
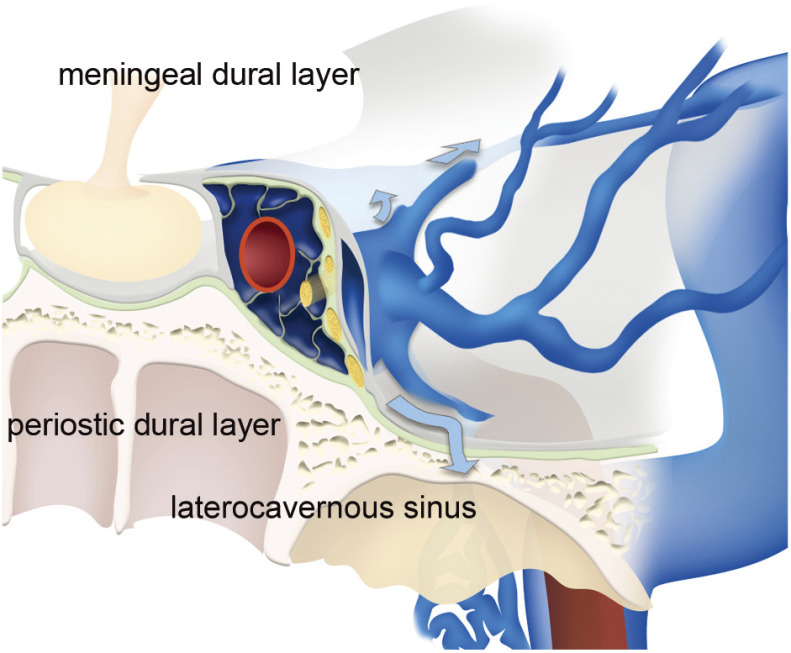
The slit-like venous channel is known to exist in the lateral wall of the CS.4) This venous channel was reported as the laterocavernous sinus, which was considered a drainage route of the superficial middle cerebral vein (SMCV) in previous studies.5,6) San Millán Ruíz et al. reported that the laterocavernous sinus was able to be observed in 14 (24%) of 58 sides in 29 cadavers.5) There was no detailed description about the relationship between the laterocavernous sinus and the dural layers in their report, but their histological examination suggested that the laterocavernous sinus existed within the meningeal dual layer. Most laterocavernous sinuses were a venous channel that functioned as a drainage route of the SMCV. In their study, this was noted in 13 of 14 sides of the CS; the remaining one side was a drainage route of the uncal vein (UV).5) The laterocavernous sinus itself drained into the superior petrosal sinus in 10, the pterygoid plexus in three, and the posterior part of the CS in one. Gailloud et al. reported that the SMCV drained into the laterocavernous sinus in 22% on internal carotid arteriography, and among them, the laterocavernous sinus emptied into the pterygoid plexus in 27%, the posterior part of the CS in 32%, and the superior petrosal sinus in 18%.6) Ide et al. investigated the uncal venous drainage route in 118 cases of carotid arteriography. According to the report, 13% of the UV drained into the laterocavernous sinus; the drainage routes of the laterocavenous sinus were the CS in 1%, pterygoid plexus ion in 5%, and both the CS and pterygoid plexus in 7%.7)
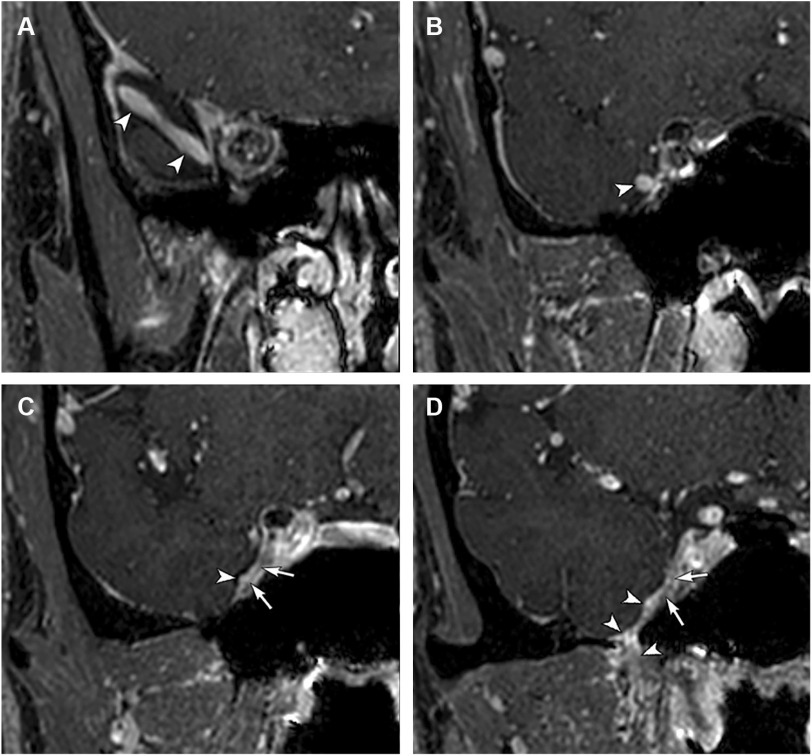
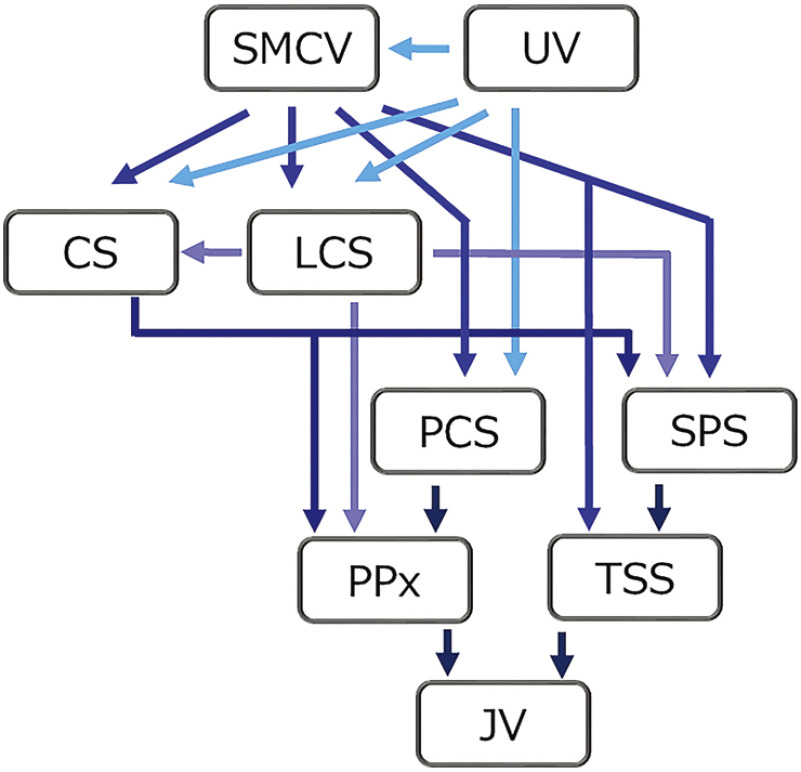
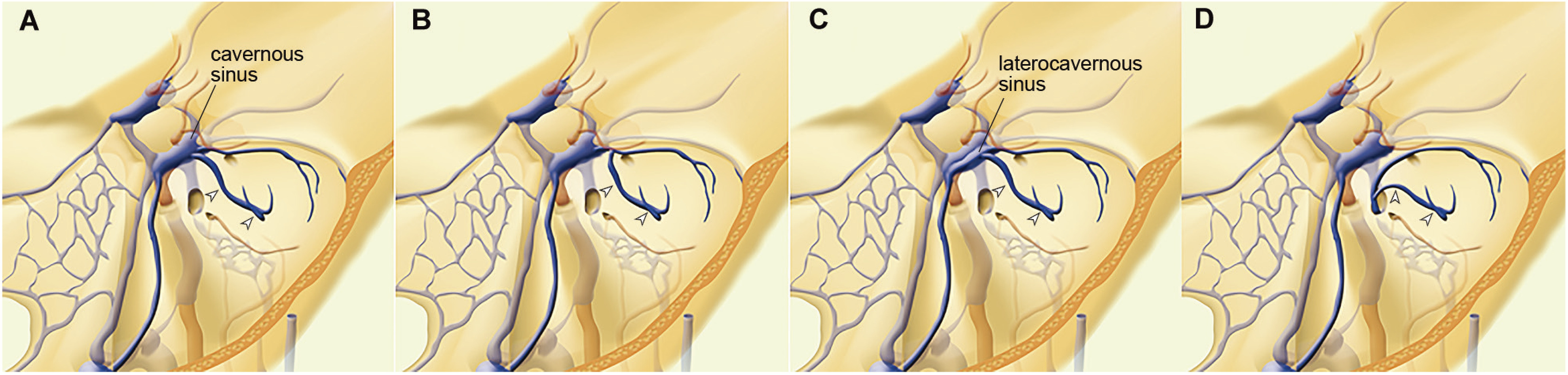
These previous anatomical and radiological reports revealed that the laterocavernous sinus exists at a certain frequency and that it functions as a drainage route from the SMCV and the UV. The laterocavernous sinus itself can drain into the posterior part of CS, the superior petrosal sinus, the pterygoid plexus, and their combination (Figs. 3 and 4). The SMCV and the UV demonstrate variable drainage patterns because of the combination of their terminations and the termination of the laterocavernous sinus (Fig. 5).
Fig. 3. Schematic drawing of anatomy of laterocavernous sinus (anterolateral view of coronal section). Laterocavernous sinus is a slit-like venous channel lying at the outer layer of lateral wall of CS. This channel plays a role of a drainage route of SMCV and UV. Laterocavernous sinus drains into the posterior part of CS, the superior petrosal sinus, the pterygoid plexus, and their combination (arrows). CS: cavernous sinus; SMCV: superficial middle cerebral vein; UV: uncal vein.
Fig. 4. MR image of laterocavernous sinus. (A–D) Coronal reconstructions of contrast-enhanced fast-field echo MRI (in rostral to caudal order) demonstrate SMCV draining into laterocavernous sinus and pterygoid plexus (arrowheads). Laterocavernous sinus is bounded medially by linear low intensity from CS (C and D, arrows). CS: cavernous sinus; SMCV: superficial middle cerebral vein.
Fig. 5. Diagram showing relationships among CS and other relevant venous structures. SMCV, UV, LCS, CS, and other relevant venous structures show complicated relationships generated by combinations of various drainage patterns. CS: cavernous sinus; LCS: laterocavernous sinus; SMCV: superficial middle cerebral vein; UV: uncal veina.
Basic Anatomy of Relevant Surrounding Veins and Their Variations
The CS is connected by many surrounding veins. It receives the facial and orbital venous drainage anteriorly via the ophthalmic veins, the meningeal and osseous venous drainage laterally via the sphenoparietal sinus, the neuronal venous drainage via the SMCV and UV, the pituitary venous drainage medially, and the clival meningeal/osseous venous drainage posteromedially. The CS has also connections to the contralateral sinus medially via the intercavernous sinus. The CS may also receive bridging veins from the pontine veins at the posterior part and the superior petrosal sinus at the posterolateral part.
The venous outflow from the CS empties into other venous structures via several routes. It drains into the jugular vein via the inferior petrosal sinuses and into the pterygoid venous plexus via the emissary veins.
Superior/inferior ophthalmic veins
The superior ophthalmic vein exhibits a constant course. It originates from the superomedial orbital rim, obliquely courses along the orbital roof, and enters into the cranial space to join the anterior aspects of the CS via the superior orbital fissure.8) This vein also communicates with the facial veins medially via the angular vein and with the tributary of the superficial temporal vein superolaterally. These potential communications are similar to the anatomical relationships among the supraorbital artery, facial artery, lacrimal artery, and transverse facial artery.
The inferior ophthalmic vein courses via the inferior orbital fissure to empty the pterygoid plexus and flows into the superior ophthalmic vein or the CS posteriorly.8)
SMCV and UV
The SMCV generally courses along the lesser sphenoid wing and flows into the anterolateral part of the CS directly or via the sphenoparietal sinus. The UV joins the proximal part of the SMCV or the lateral part of the CS. In other variations, the SMCV may join the laterocavernous sinus posteriorly, as described earlier; course along the middle cranial base and join the pterygoid plexus (paracavernous sinus); or posteriorly travel along the middle cranial fossa to join the superior petrosal sinus or lateral tentorial sinus (Figs. 6 and 7).6,9,10) The type of SMCV passing posteriorly along the middle cranial base was named as “sphenopetrosal vein” by Hacker.11) The type of SMCV passing through the middle cranial base to join the pterygoid venous plexus is known as “sphenobasal vein.”11) According to the report of Gailloud et al., using DSA images, the SMCV was absent in 19%, drained into the lateral wall of the CS in 20%, drained into the laterocavernous sinus in 22%, and drained into the paracavernous sinus in 39%.6) The UV exhibits anatomical variations in its course. It may drain into the lateral wall of the CS, the SMCV, the laterocavernous sinus, or the paracavernous sinus (Figs. 7 and 8).7)
Fig. 6. Schematic drawings of variations in terminations of SMCV. SMCV runs along Sylvian fissure and terminates in the proximal segment of sphenoparietal sinus, lateral wall of CS (A), laterocavernous sinus (B), pterygoid plexus via foramen ovale (paracavernous sinus) (C), and superior petrosal sinus, or lateral tentorial sinus (D). CS: cavernous sinus; SMCV: superficial middle cerebral vein.
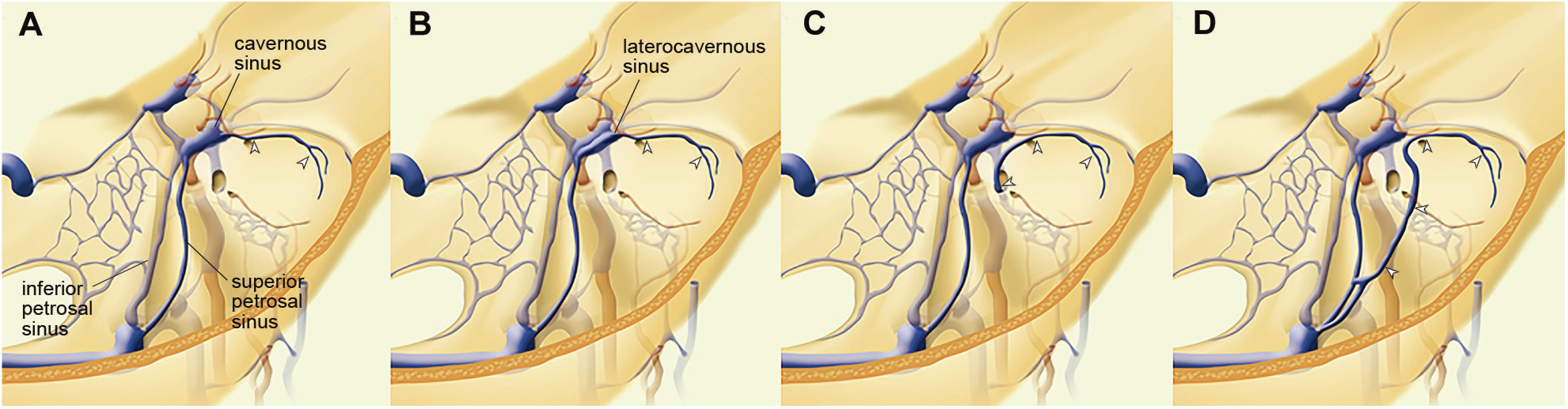
Fig. 7. Angiographic findings of variations in termination of SMCV and UV. (A and B) Venous phase of right internal carotid arteriography (A, frontal view; B, lateral view) shows SMCV terminating in the lateral wall of CS (black arrowheads). UV terminating in SMCV is also identified (white arrowheads). (C and D) Venous phase of right internal carotid arteriography (C, frontal view; D, lateral view) shows SMCV (black arrowheads) terminating in slit-like venous structure (laterocavernous sinus). Laterocavernous sinus is draining into pterygoid plexus via middle cranial fossa (arrows). UV terminating in SMCV is also identified (white arrowheads). (E and F) Venous phase of right internal carotid arteriography (E, frontal view; F, lateral view) shows SMCV (black arrowheads) terminating in pterygoid plexus via middle cranial fossa (paracavernous sinus). UV terminating at SMCV is also identified (white arrowheads). (G and H) Venous phase of right internal carotid arteriography (G, frontal view; H, lateral view) shows SMCV (black arrowheads) terminating in transverse sinus via lateral tentorial sinus. UV terminates at lateral wall CS (white arrowheads). CS: cavernous sinus; SMCV: superficial middle cerebral vein; UV: uncal vein.
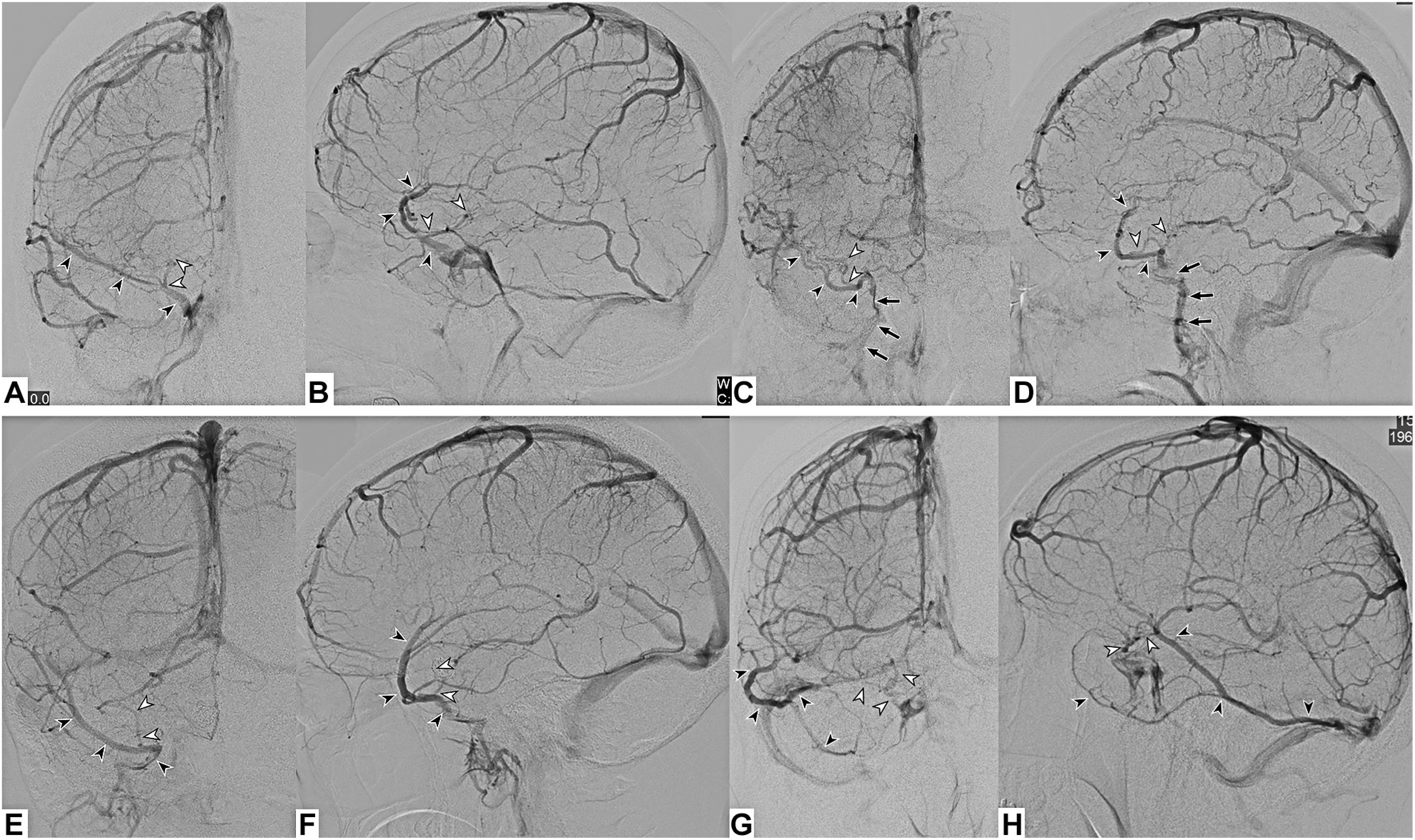
Fig. 8. Schematic drawings of variations in terminations of UV. UV terminates in the lateral aspect of CS (A) or SMCV emptying to CS (B), laterocavernous sinus (C), or SMCV emptying to laterocavernous sinus, pterygoid plexus via foramen ovale or SMCV emptying to pterygoid plexus (paracavernous sinus drainage type SMCV) (D). CS: cavernous sinus; SMCV: superficial middle cerebral vein; UV: uncal vein.
Superior petrosal sinus
The superior petrosal sinus has been recognized as a dural sinus connecting the CS with the transverse–sigmoid junction. This sinus plays a role as a venous drainage route from the petrosal vein, emptying the cerebellar and brain stem venous flow. A recent radiological investigation demonstrated that this sinus does not have constant continuity from the CS to the transverse–sigmoid junction; it demonstrated several patterns of venous flow from the petrosal vein to only the posterior segment of the superior petrosal sinus, from the petrosal vein to only the anterior segment of the superior petrosal sinus, and from the petrosal vein to the anterior and posterior segments of the petrosal sinus with interruption of the middle portion of the superior petrosal sinus.12)
Inferior petrosal sinus
The inferior petrosal sinus connects the posterolateral part of the CS with the jugular vein. The merging point of this sinus to the jugular bulb can exhibit variations. A previous study demonstrated variable merging points, including the jugular bulb, the segment of the jugular vein close to the lateral opening of the hypoglossal canal, the lower extracranial segment of the jugular bulb, the vertebral venous plexus without the connection to the jugular vein.13)
Intercavernous sinus
The intercavernous sinus is the sinus connecting the bilateral CSs at the midline. This sinus lies between the meningeal dural layer surrounding the pituitary gland and the endosteal dural layer on the floor of the sella turcica.14) This sinus exists in any part of the intercavernous area, but it generally exists in the anterior and/or posterior part of the sella turcica.15) According to a previous study, the sinus most frequently exhibits both anterior and posterior intercavernous sinuses, and less frequently only anterior or posterior.14)
Bridging vein
The CS receives the bridging veins draining venous blood flow from the venous networks surrounding the brain stem. These bridging veins are difficult to identify on conventional angiography in the case of normal venous flow. According to a previous anatomical and radiological report, the bridging veins frequently connect the transverse pontine vein and the anterior pontomesencephalic vein with the posterior aspect of the CS.16,17)
Emissary veins and pterygoid venous plexus
The venous blood flow of the CS empties into the infratemporal fossa via the emissary veins through the foramina. The foramen ovale emissary vein constantly exists with draining the venous blood flow from the CS to the pterygoid venous plexus.18,19) There can be an inconsistent communication between the CS and the pterygoid venous plexus via the foramen Vesalius emissary vein.18) The foramen Vesalius emissary vein is located anteromedially to the foramen ovale.
The pterygoid venous plexus is a complex plexiform venous structure that lies around or within the pterygoid muscles. This venous plexus anteriorly receives the orbital and nasopharyngeal venous blood flow via the inferior ophthalmic vein and sphenopalatine vein.20) This posteriorly converges to form the internal maxillary vein and drain into the superficial temporal vein. This venous plexus also has communications anterolaterally with the facial vein.20)
Basilar venous plexus
The basilar venous plexus is a plexiform venous channel that lies at the clivus. This venous channel interconnects the bilateral inferior petrosal sinus, the CS, and the marginal sinus at the internal surface of the clivus. This venous plexus also has communications with the cervical epidural vein and vertebral venous plexus.21) The basilar venous plexus plays a role of providing the collateral pathway from the CS to the extracranial veins.
Inferior petroclival (petro-occipital) vein
The inferior petroclival (petro-occipital) vein (IPCV) is a venous structure that regularly connects the CS with anterior condylar confluence. Ruiz et al. reported that the IPCV regularly existed as a tributary of the anterior condylar confluence draining from the carotid canal venous plexus (CCVP) at the foramen lacerum in 12 cadaveric study.22) IPCV runs extracranial aspect of the petroclival fissure parallel with the inferior petrosal sinus. The IPCV communicates with other veins at clivus and petrous apex. Mizutani et al. reported the clival diploic venous networks among the IPCV, the inferior petrosal sinus, the basilar venous plexus, the anterior/lateral/posterior condylar vein, and the anterior condylar confluence.23) They called the diploic venous networks mainly within the jugular tuberculum as the jugular tuberculum venous complex.
Superficial tributaries of external/internal jugular vein
Facial vein
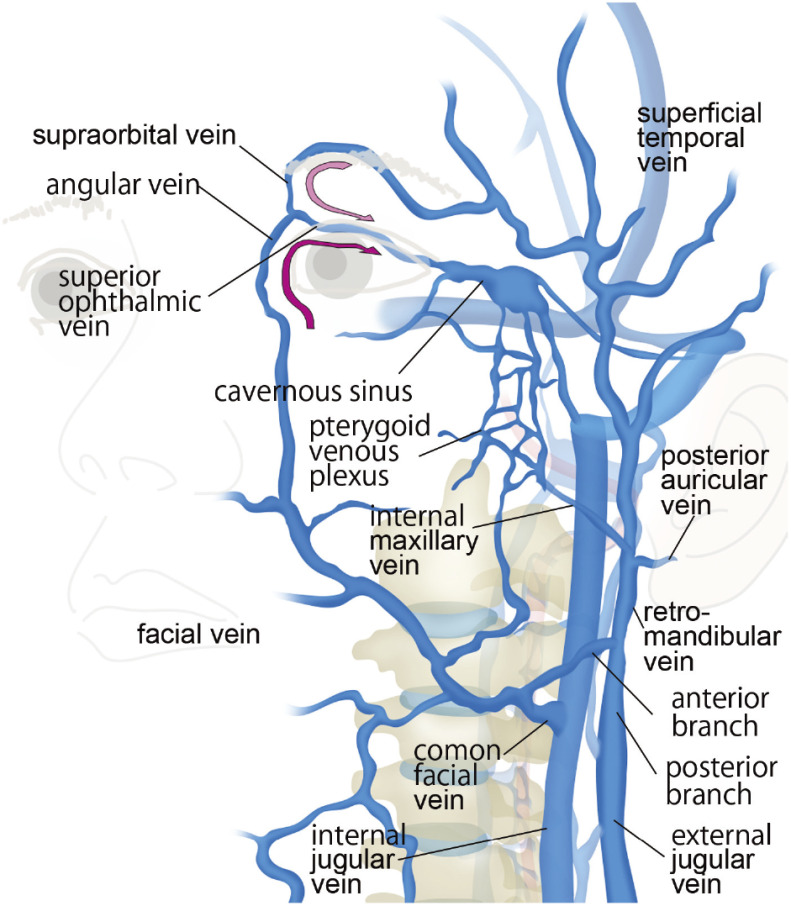
The facial vein lies lateral to the nose bottom collecting the venous blood flow from the superficial face and nose. This connects with the superior ophthalmic vein via the angular vein at the medial angle of the eye and travels downward and backward to join the anterior branch of the retromandibular vein to form the common facial vein. The common facial vein drains into the internal jugular vein. This vein may drain into the external jugular vein and rarely into the subclavian vein (Fig. 9).24)
Fig. 9. Schematic drawing of superficial tributaries of external and internal jugular vein (left anterior oblique view of face). Superficial temporal vein draining into external jugular vein and facial vein draining into internal jugular vein anastomose with superior ophthalmic vein via angular vein surrounding anterior orbital opening. These venous networks can be alternative access routes into CS (curved arrows). CS: cavernous sinus.
Superficial temporal vein
The superficial temporal vein receives the venous blood flow from the scalp and descends at the temporal region. This vein joins with the posterior auricular vein to form the retromandibular vein. The retromandibular vein gives off the anterior branch and posterior branch; the anterior branch drains into the internal jugular vein forming the common facial vein, and the posterior branch drains into the external jugular vein. The retromandibular vein may form single trunk and drain into the external jugular vein receiving the facial vein.25) The superficial temporal vein can anterosuperiorly anastomose with the superior ophthalmic vein via the supraorbital vein and the superior palpebral vein, which are tributaries of the superficial temporal vein (Fig. 9).
Clinical Implications of the Anatomy and Variations of the CS and Surrounding Veins
For endovascular treatment of cavernous sinus dural arteriovenous fistulas (CSDAVF), transvenous embolization is generally selected as the first-line treatment. When considering transvenous embolization, the locations of the shunts (shunted venous pouch), their feeding arteries and the drainage route, including the accessible routes, should be determined. In addition, the normal venous flows of the SMCV and UV or the coexistence of retrograde venous reflux into them and bridging veins should also be carefully evaluated. Kiyosue et al. reported that shunted venous pouches were able to be observed in the posteromedial, posterolateral, medial and lateral parts of the CS on evaluation of the 3D-DSA images of patients with CSDAVF.26) Selective transvenous embolization for shunted venous pouches is feasible to reduce the number of coils and to avoid damaging the sixth cranial nerve and unexpected increase in shunt flow into the cortical veins during closure of the outflows.
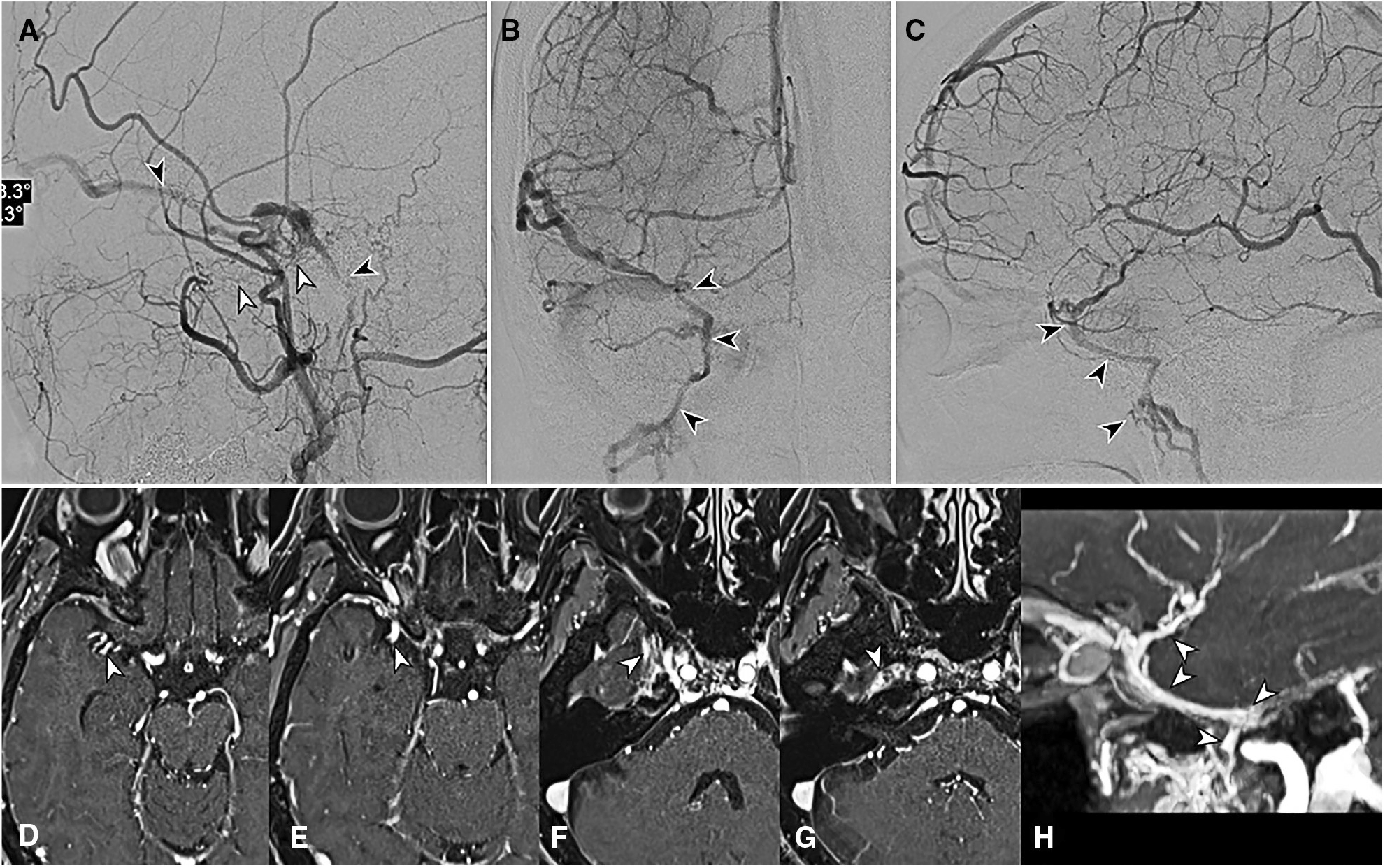
When selective embolization of the shunted venous pouches is difficult due to lack of the shunted venous pouch, coil embolization of the outlet to the SMCV and UV, and/or packing of the CS should be considered in cases of retrograde cortical venous reflux. In such situations, the operators should confirm the accessibility to cortical veins. The anatomical relationships between the CS and the SMCV and UV, and the existence of the laterocavernous sinus should be carefully evaluated using the reconstructed images of 3D-DSA and/or MRI before treatment (Fig. 10).
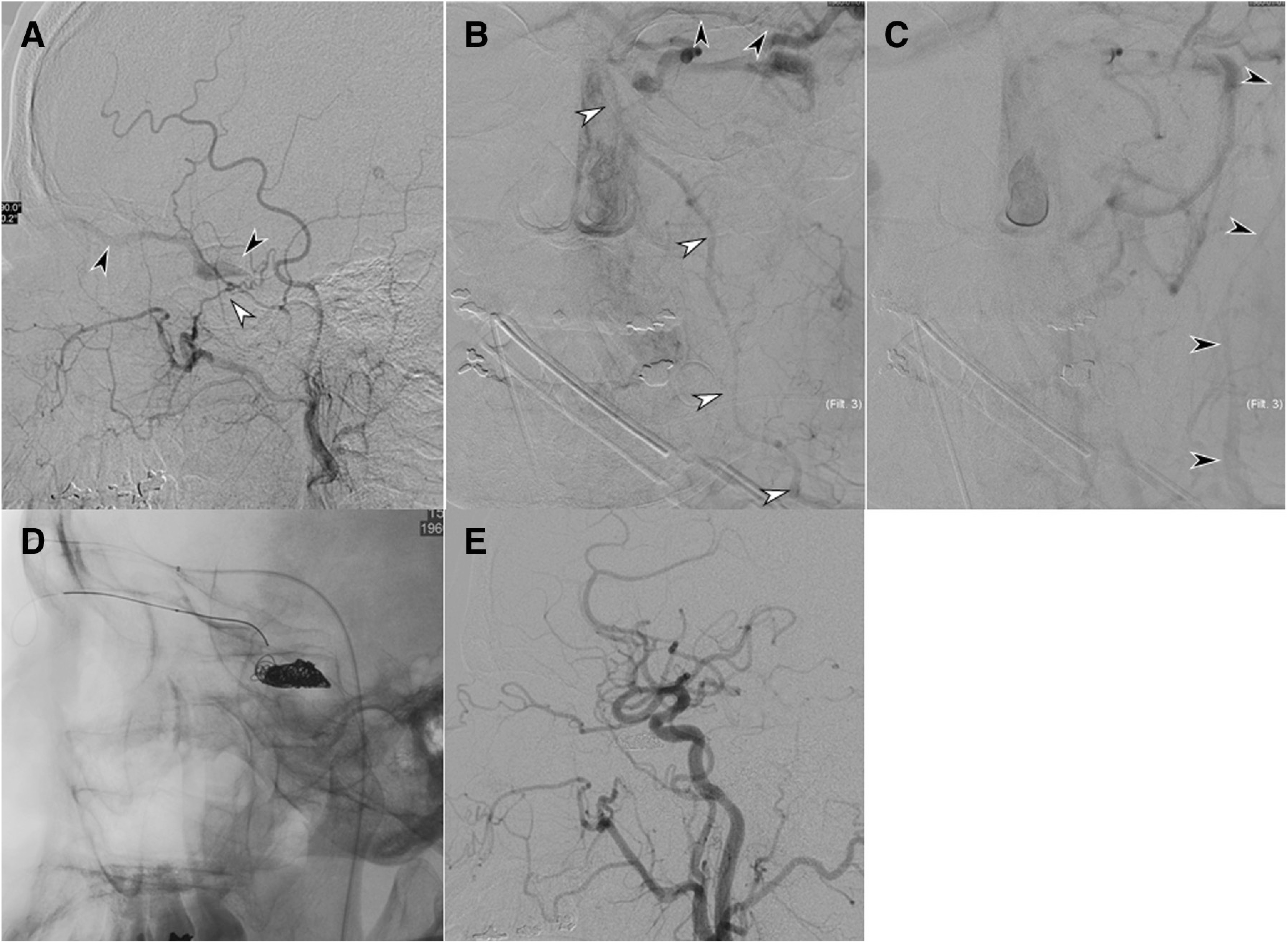
Fig. 10. A case with right CS dural arteriovenous fistula. (A) Lateral view of right external carotid arteriogram shows cavernous dural arteriovenous fistula mainly fed by artery of foramen rotundum and CS branch of middle meningeal artery (white arrowheads) and draining into superior ophthalmic vein and inferior petrosal sinus (black arrowheads). (B and C) Venous phase of right internal carotid arteriogram (B, frontal view; C, lateral view) shows SMCV and UV draining antegradely into pterygoid plexus via middle cranial fossa (arrowheads). (D–H) Postcontrast images of 3D fast-field echo sequence (D–G, axial reconstructions in rostral to caudal order; H, oblique sagittal reconstruction) show SMCV emptying to pterygoid plexus via foramen ovale (arrowheads) without connection to CS. In this case, there was little risk of reflux into SMCV. CS: cavernous sinus; SMCV: superficial middle cerebral vein; UV: uncal vein.
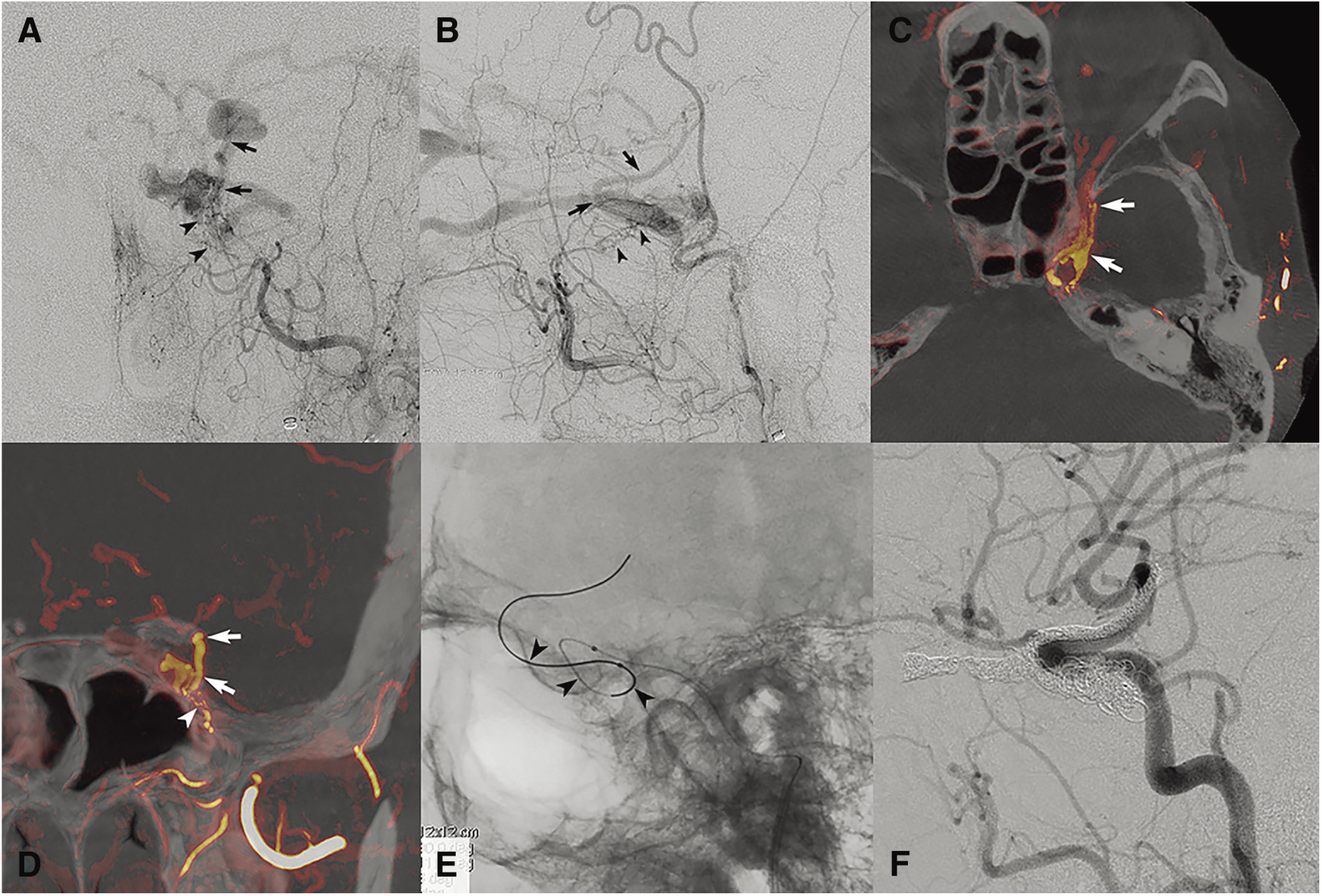
CSDAVF sometimes develop in patients with cortical venous drainage into the laterocavernous sinus. Okahara et al. reported four cases of CSDAVF involving the laterocavernous sinus in their 27-case series.27) According to the report, the shunt points were observed at the posterior segment in three and the anterior segment of the laterocavernous sinus in one. All four cases exhibited retrograde venous reflux into the SMCV, UV, or both. When the shunt point is at the laterocavernous sinus, sinus packing of the CS alone may lead to residual reflux into the cortical veins and loss of the accessible route. In cases of CSDAVF combined with laterocavernous sinus drainage of the shunt flow for which transvenous embolism is planned, detailed assessment of the relationships between the laterocavernous sinus and the SMCV, UV, and CS is needed (Fig. 11). Previous reports revealed several routes between the CS and laterocavernous sinus, with connections at the medial or posterior part of the lateral wall of the CS.6,27)
Fig. 11. A case with left CS dural arteriovenous fistula involving laterocavernous sinus. (A and B) Left external carotid arteriogram (A, frontal view; B, lateral view) shows cavernous dural arteriovenous fistula mainly fed by artery of foramen rotundum (arrowheads) and draining into inferior ophthalmic vein and SMCV (arrows). (C and D) Color fusion images of 3D external carotid arteriogram (C, axial reconstruction; D, coronal reconstruction) demonstrate draining into SMCV via laterocavernous sinus (arrows). Laterocavernous sinus is connected with CS at posterior compartment. Note arteriovenous shunt at the caudal part of laterocaverous sinus (D, arrowhead). (E) Fluorogram after navigation of microcatheter and guidewire (arrowheads) into laterocavernous sinus and SMCV through connection at posterior segment. (F) Lateral view of left common carotid arteriogram after coil packing of SMCV, ophthalmic vein, laterocavernous sinus, and CS shows complete disappearance of dural arteriovenous fistula. CS: cavernous sinus; SMCV: superficial middle cerebral vein.
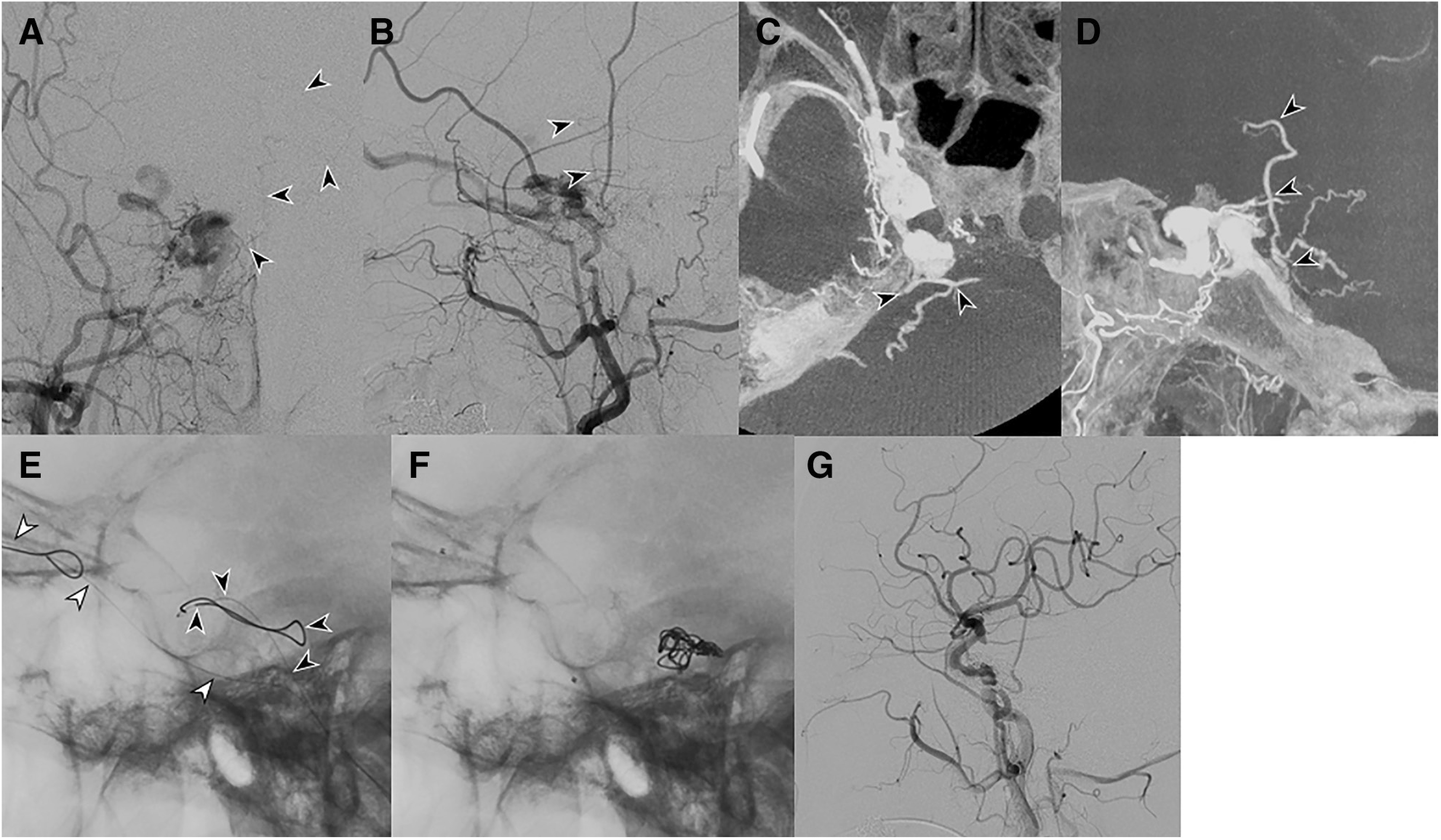
CSDAVF occasionally combine retrograde reflux into the veins in the posterior fossa, causing pontine and cerebellar congestion/hemorrhage. Retrograde reflux can present via three routes, the bridging vein–transverse pontine vein, the UV–basal vein of the Rosenthal-lateral mesencephalic vein, and the superior petrosal sinus–petrosal vein. Residual or recurrent flow after the transvenous embolization of the CSDAVF may cause a markedly poor outcome; thus, the outlet of reflux into the posterior fossa veins should be predominantly embolized (Fig. 12). Careful evaluation of the anatomical relationships between the CS and the veins to the posterior fossa is essential.
Fig. 12. A case with right CS dural arteriovenous with retrograde venous reflux to posterior fossa via bridging vein. (A and B) Right external carotid arteriogram (A, frontal view; B, lateral view) shows cavernous dural arteriovenous fistula draining into superior ophthalmic vein and the deep venous system via anterior pontomesencephalic vein and peduncular vein (arrowheads). (C and D) Partial MIP reconstructions of 3D rotational right external carotid arteriogram (C, axial reconstruction; D, sagittal reconstruction) show contrast filling of anterior pontomesencephalic vein via bridging vein (arrowheads). (E) Fluorogram after navigation of microcatheters. One catheter is navigated into the posterior segment of CS after deflection within anterior segment (black arrowheads). Another catheter is navigated into superior ophthalmic vein (white arrowheads). (F) Fluorogram during insertion of microcoils. Microcoils were initially placed in the posterior compartment of CS to occlude retrograde reflux into the deep venous system. (G) Lateral view of right common carotid arteriogram shows complete disappearance of dural arteriovenous fistula after packing of CS. CS: cavernous sinus.
The common transvenous approach route to the CS is the inferior petrosal sinus. When the route is not accessible, the surrounding veins including basilar plexus, the IPCV, and the pterygoid plexus can be alternative approach routes. In addition, if the transvenous approach through the occluded inferior petrosal sinus is difficult, especially in case with the CSDAVF, the extracranial venous networks around the orbit can be the approach route via the anastomoses with the superior ophthalmic vein (Fig. 13).28–30) In such cases, the accessible drainage route can be demonstrated on the preoperative postcontrast CT and/or MRI as well as the angiograph. The careful assessment of these imaging findings is mandatory.
Fig. 13. A case with left CSDAVF treated by a superficial temporal venous approach. (A) Lateral view of left external carotid arteriogram shows CSDAVF mainly fed by artery of foramen rotundum (white arrowhead) and draining into superior ophthalmic vein (black arrowheads). (B and C) Frontal view of left common carotid arteriogram (B, early venous phase; C, late venous phase) shows extracranial venous drainage via angular vein, facial vein (white arrowheads), and superficial temporal vein (black arrowheads). (D) Lateral fluorogram of transvenous coil embolization via superficial temporal vein and superior ophthalmic vein. (E) Lateral view of left common carotid arteriogram shows complete disappearance of DAVF. CSDAVF: cavernous sinus dural arteriovenous fistulas; DAVF: dural arteriovenous fistulas.
As mentioned earlier, for safe and effective transvenous embolization, precise assessment of the shunt points on the CS and laterocavernous sinus, and of the venous drainage routes, including access routes, is highly important.
Conclusion
The CS and related venous structures exhibit anatomical variations. Knowledge and careful assessment of the imaging anatomy and variations are of significant importance, especially for transvenous embolization of CSDAVF.
Disclosure Statement
The authors have no conflicts of interest directly relevant to the content of this study.
References
- 1).Campero A, Campero AA, Martins C, et al. : Surgical anatomy of the dural walls of the cavernous sinus. J Clin Neurosci 2010; 17: 746–750. [DOI] [PubMed] [Google Scholar]
- 2).Umansky F, Nathan H: The lateral wall of the cavernous sinus. With special reference to the nerves related to it. J Neurosurg 1982; 56: 228–234. [DOI] [PubMed] [Google Scholar]
- 3).Bedford MA: The “cavernous” sinus. Br J Ophthalmol 1966; 50: 41–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4).Miyazaki H: The “cavernous” sinus. No Shinkei Geka 1981; 9: 1131–1138. (in Japanese) [PubMed] [Google Scholar]
- 5).San Millán Ruiz D, Gailloud P, de Miquel Miquel MA, et al. : Laterocavernous sinus. Anat Rec 1999; 254: 7–12. [DOI] [PubMed] [Google Scholar]
- 6).Gailloud P, San Millán Ruíz D, Muster M, et al. : Angiographic anatomy of the laterocavernous sinus. AJNR Am J Neuroradiol 2000; 21: 1923–1929. [PMC free article] [PubMed] [Google Scholar]
- 7).Ide S, Kiyosue H, Tanoue S, et al. : Anatomical variations in termination of the uncal vein and its clinical implications in cavernous sinus dural arteriovenous fistulas. Neuroradiology 2014; 56: 661–668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8).Cheung N, McNab AA: Venous anatomy of the orbit. Invest Ophthalmol Vis Sci 2003; 44: 988–995. [DOI] [PubMed] [Google Scholar]
- 9).Tanoue S, Kiyosue H, Okahara M, et al. : Para-cavernous sinus venous structures: anatomic variations and pathologic conditions evaluated on fat-suppressed 3D fast gradient-echo MR images. AJNR Am J Neuroradiol 2006; 27: 1083–1089. [PMC free article] [PubMed] [Google Scholar]
- 10).Suzuki Y, Matsumoto K: Variations of the superficial middle cerebral vein: classification using three-dimensional CT angiography. AJNR Am J Neuroradiol 2000; 21: 932–938. [PMC free article] [PubMed] [Google Scholar]
- 11).Hacker H: Normal supratentorial veins and dural sinus. In: Newton TH, Potts DG. eds.; Radiology of the Skull and Brain. Saint Louis: Mosby, 1974. [Google Scholar]
- 12).Shimada R, Kiyosue H, Tanoue S, et al. : Superior petrosal sinus: hemodynamic features in normal and cavernous sinus dural arteriovenous fistulas. AJNR Am J Neuroradiol 2013; 34: 609–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13).Mitsuhashi Y, Nishio A, Kawahara S, et al. : Morphologic evaluation of the caudal end of the inferior petrosal sinus using 3D rotational venography. AJNR Am J Neuroradiol 2007; 28: 1179–1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14).Tubbs RS, Griessenauer C, Loukas M, et al. : The circular sinus: an anatomic study with neurosurgical and neurointerventional applications. World Neurosurg 2014; 82: e475–478. [DOI] [PubMed] [Google Scholar]
- 15).Harris FS, Rhoton AL: Anatomy of the cavernous sinus. A microsurgical study. J Neurosurg 1976; 45: 169–180. [DOI] [PubMed] [Google Scholar]
- 16).Matsushima T, Rhoton AL, de Oliveira E, et al. : Microsurgical anatomy of the veins of the posterior fossa. J Neurosurg 1983; 59: 63–105. [DOI] [PubMed] [Google Scholar]
- 17).Kiyosue H, Tanoue S, Sagara Y, et al. : The anterior medullary-anterior pontomesencephalic venous system and its bridging veins communicating to the dural sinuses: normal anatomy and drainage routes from dural arteriovenous fistulas. Neuroradiology 2008; 50: 1013–1023. [DOI] [PubMed] [Google Scholar]
- 18).Leonel LCPC, de Sousa SDG, Liberti EA: Topographic and microscopic anatomical description of the emissary sinus of foramen ovale in adult humans. Clin Neurol Neurosurg 2018; 169: 77–85. [DOI] [PubMed] [Google Scholar]
- 19).Mortazavi MM, Tubbs RS, Riech S, et al. : Anatomy and pathology of the cranial emissary veins: a review with surgical implications. Neurosurgery 2012; 70: 1312–1318; discussion 1318–1319. [DOI] [PubMed] [Google Scholar]
- 20).Deplus S, Brémond-Gignac D, Gillot C, et al. : The pterygoid venous plexuses. Surg Radiol Anat 1996; 18: 23–27. [DOI] [PubMed] [Google Scholar]
- 21).Miller DL, Doppman JL, Chang R: Anatomy of the junction of the inferior petrosal sinus and the internal jugular vein. AJNR Am J Neuroradiol 1993; 14: 1075–1083. [PMC free article] [PubMed] [Google Scholar]
- 22).San Millán Ruíz D, Gailloud P, Rüfenacht DA, et al. : The craniocervical venous system in relation to cerebral venous drainage. AJNR Am J Neuroradiol 2002. Oct; 23(9): 1500–1508. [PMC free article] [PubMed] [Google Scholar]
- 23).Mizutani K, Akiyama T, Minami Y, et al. : Intraosseous venous structures adjacent to the jugular tubercle associated with an anterior condylar dural arteriovenous fistula. Neuroradiology 2018; 60: 487–496. [DOI] [PubMed] [Google Scholar]
- 24).Prakash R, Prabhu LV, Kumar J, et al. : Variations of jugular veins: phylogenic correlation and clinical implications. South Med J 2006; 99: 1146–1147. [DOI] [PubMed] [Google Scholar]
- 25).Pai MP, Vadgaonkar R, Shetty P: The different termination patterns of the facial vein. A cadaveric study. Fırat Tıp Dergisi 2008; 13: 32–34. [Google Scholar]
- 26).Kiyosue H, Tanoue S, Hori Y, et al. : Shunted pouches of cavernous sinus dural AVFs: evaluation by 3D rotational angiography. Neuroradiology 2015; 57: 283–290. [DOI] [PubMed] [Google Scholar]
- 27).Okahara M, Kiyosue H, Hori Y, et al. : Transvenous embolization of cavernous sinus dural arteriovenous fistulas with shunts involving the laterocavernous sinus. JNET J Neuroendovasc Ther 2016; 11: 1–7. [Google Scholar]
- 28).Biondi A, Milea D, Cognard C, et al. : Cavernous sinus dural fistulae treated by transvenous approach through the facial vein: report of seven cases and review of the literature. AJNR Am J Neuroradiol 2003; 24: 12400–1246. [PMC free article] [PubMed] [Google Scholar]
- 29).Yu SC, Cheng HK, Wong GK, et al. : Transvenous embolization of dural carotid-cavernous fistulae with transfacial catheterization through the superior ophthalmic vein. Neurosurgery 2007; 60: 1032–1037; discussion 1037–1038. [DOI] [PubMed] [Google Scholar]
- 30).Cheng KM, Chan CM, Cheung YL: Transvenous embolisation of dural carotid-cavernous fistulas by multiple venous routes: a series of 27 cases. Acta Neurochir (Wien) 2003; 145: 17–29. [DOI] [PubMed] [Google Scholar]