Abstract
The crisis of the coronavirus disease (COVID-19) is causing damage to the social and medical community. However, extreme emergency neuro-interventions such as mechanical thrombectomy still require the healthcare workers to offer the appropriate treatment while preventing further spread of the infection. This article outlines the necessary steps in managing a possible COVID-19 patient starting from patient screening to personnel infection and environmental contamination measures.
Keywords: coronavirus disease, infection control, mechanical thrombectomy
Introduction
As the crisis of the coronavirus disease (COVID-19),1 caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is spreading out globally, the demand on the care of the COVID-19 patients in various fields is inevitable. In a study involving a cohort of COVID-19 patients in Wuhan, China, the incidence of stroke in the severe respiratory symptom group of COVID-19 was 5.7%, with most as ischemic stroke.2 Although the details of the ischemic stroke was not mentioned, the authors described a significant increase in the d-dimer level that can be considered as a risk factor for embolic stroke.3
A recommendation for the care of emergent neurointerventional patients in the setting of COVID-19 has recently been released by the Society of NeuroInterventional Surgery.4 However, the precautions that can be readily put into use are rather limited. In this article, we introduce our infection control manual ready to be applied in most neurointerventional units. This should also be applicable in many situations where rapid neuro-intervention cannot be avoided in COVID-19 patients.
The benefit of mechanical thrombectomy (MT) for acute stroke patients due to large vessel occlusion that fulfill the treatment criteria is well proven,5 and the treatment indication should not be altered in COVID-19 patients. Minimum delay in the initiation of the diagnostic step to the intervention step should be avoided as the MT is a highly time-sensitive procedure, but at the same time, the risk to care providers must be fully eliminated.
This protocol contains three major steps: patient screening, initial evaluation, and care provider/environmental protection. The goals are to provide the necessary endovascular therapies such as MT while avoiding risk to the interventionist and medical staff and to provide a guideline for disinfection of the environment to prevent nosocomial infection.
Methods
Preparedness is the key to controlling a pandemic. To create this protocol, we have gathered the latest information from various sources shown in the reference section, together with the advice we could obtain from the hospital infection control team. After several revisions, we came up with the steps mentioned in the next section that should be followed according to the status of the COVID-19 in the area.
Patient Screening
The following protocol was made based on recent reports and discussion with the emergency and critical care department and radiology department, and a rehearsal was done in the actual angiography room environment.
For a COVID-19-positive patient, proceed with interventions such as thrombectomy as usual as soon as the personal protection equipment (PPE) and zoning preparation are ready. Patients with an unknown status of COVID-19 should be screened using the following protocol.
High risk of COVID-19-positive patient screening criteria
At first contact, if any suspicion arises, put a protective mask on the patient. If needed to give oxygen, place an oxygen cannula under the mask.
A patient with any of the following criteria should be considered as a suspected case of COVID-19:
1) travel history within 14 days to places considered as endemic areas (according to the data of the World Health Organization or other appropriate sources) or a a history of close contact with a COVID-19-positive or -suspected patient,
2) fever without other obvious causes,
3) respiratory symptoms or signs without other obvious causes, and
4) cases in which information mentioned above cannot be obtained without delay.
Initial Evaluation
Chest CT has been shown to be beneficial in detecting COVID-19 in high-risk population, even in patients with minimal respiratory symptoms.6,7 However, chest CT abnormalities can only be detected in 54% of asymptomatic cases,7 suggesting that there is no highly reliable screening test in this group. The steps involved in initial evaluation are as follows:
1) Perform a chest CT scan at the same time as initial intracranial imaging.
2) If any of the chest CT findings such as ground-glass opacities, involvement of multiple lobes, subpleural or peripheral distribution, consolidations, septal thickening, bronchial dilation, and wall thickening are found, consider the patient as a highly suspected case of COVID-19-positive case.
3) If neuro-intervention is to be performed under general anesthesia, the patient should be intubated in a designated area (negative pressure room with staff in proper PPE) if possible. Also consider performing MT under general anesthesia for patients with respiratory distress, active cough, or restlessness.
A patient with chest CT finding(s) compatible with those described earlier should be managed with proper PPE as described in the following. However, for those without abnormal CT findings, COVID-19 still cannot be completely ruled out.
The chance of having an asymptomatic COVID-19 patient cannot be ruled out in any patient. Practice hand hygiene and wear surgical mask when in contact with patients at all time. Use proper PPE according to epidemicity of COVID-19 in the area.
Medical Staff and Equipment/Environmental Protection
To prevent further spread of infection to other patients and healthcare workers, the following infection prevention protocol must be applied to each personnel and contamination prevention to the environment must be well respected.
Recommended PPE (Fig. 1)
Fig. 1. A sample of PPE setup. A N95 mask must be of correct size and worn properly. Another surgical mask with a face shield is worn over the N95 mask to prevent the N95 mask from being contaminated. The N95 mask, when used properly, can be reused for up to 1 month. Gloves must be worn so that they cover the sleeves and not leave any skin in contact with the body fluid of the patient. Great care must be taken when removing the PPE, not to contaminate oneself or the surrounding. Any equipment not fully covered by the surgical gown, such as X-ray thyroid shields, should be disinfected after the procedure. PPE: personal protective equipment.
—Operators, assistants, and nurses working close to the patient
Surgical gloves, N95 mask or surgical mask (N95 use should be limited to cases with aerosol-producing procedures, such as intratracheal aspiration, endotracheal intubation/extubation, bronchoscopy, and obtaining swap sample, as the number is limited. During such procedures, one must always wear a surgical mask with a face shield over an N95 mask in addition to the above), surgical mask with face shield, disposable cap, and surgical gown (Association for the Advancement of Medical Instrumentation level 3) are necessary.8 Attention must be paid not to have a direct exposure to the patient body fluid (waterproof shoe and leg covers should be used).
To prevent infection among medical staff, limit the number of medical staff participating in the procedure. If the number of staff is sufficient, work in separate teams.
—Circulating nurses and other assistants outside the operative field
Wash hands. Use a surgical mask, a long sleeve gown, and gloves. For splash/spray-producing procedure, use protection for the face and the eyes (mask with face shield or goggles). For any aerosol-producing procedure, in addition to the abovementioned equipment, use also an N95 mask. An N95 mask may be reused up to 1 month if not contaminated.
Zoning and cleaning
During transporting of the patient and for CT/MRI rooms, the following precautions are to be taken:
1) When transporting the patient, try to use a path separated from other patients.
2) CT and MRI rooms must be disinfected after each examination. In AIS of COVID-19-suspected case, consider using only CT and CTA to prevent contamination to the MRI room.
Angiography room area
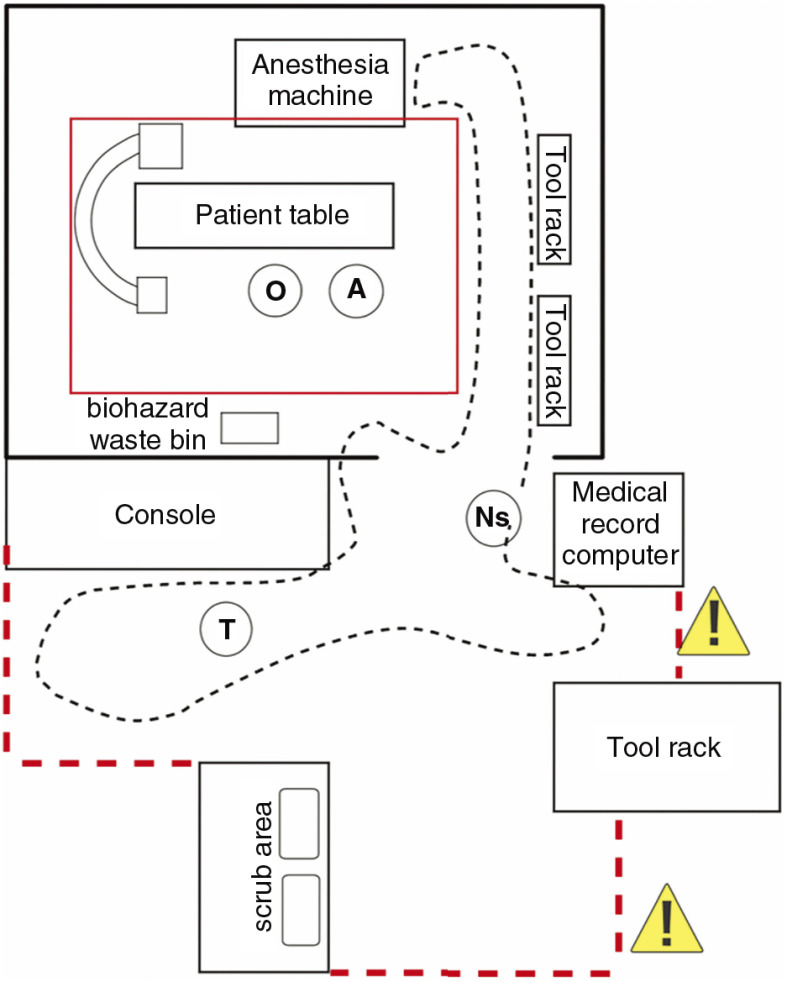
Zoning
To prevent the contamination of the the room and the equipment, proper zoning has to be planned in advance and well respected during and after the procedure.
There should be lines demonstrating the contaminated zone, intermediate zone, and clean zone on the floor of the rooms and corridors.
Staff with PPE working directly on the patient must not leave the contaminated zone with the contaminated PPE. The circulating nurse can go in and out of the angiosuite for necessary assistance but must not enter the contaminated zone (Fig. 2).
Fig. 2. A sample of zoning around the area of angiography room. The red dotted line indicates the area of no entry for other personnel (intermediate area). There should be only minimum number of staff participating. After transferring the patient on the table, only the operator (O) and the scrub in assistance (A) are allowed inside the highly contaminated area (inside the red line). The circulating nurse and the technician can enter the room if necessary but should be limited to the area of the dotted line. The yellow triangles with exclamation marks represent a sign displaying “COVID-19 area,” informing other personnel not to enter the area. The gloves and the surgical gowns must be removed properly before exiting the red line area. The area outside the red dotted line is considered as a “clean” area. When the structure of the angiography room area does not allow to create an intermediate zone, care must be taken not to contaminate equipment that cannot be disinfected easily. COVID-19: coronavirus disease.
Cleaning and disinfecting of the environment
The length of the time spent in the area of the angiography room is usually longer than that in other areas. This time includes a special attention in cleaning. Effective disinfection can be done by wiping of surfaces using alcohol cleaning cloths with alcohol concentration higher than 70%.9 Sodium hypochlorite solution as low as 0.21% has also been shown to be effective.9 Although the SARS-CoV-2 is considered to remain viable in aerosols for 3 hours,10 with proper ventilation of the room, 1 hour allowing the air change is considered to be a practical and safe option.11
1) For medical instruments, wipe clean with alcohol cleaning cloths. Blood residuals must be removed prior to the disinfection process using alcohol.
2) For washable materials, use detergent to wash, followed by immersing in 0.1% sodium hypochlorite solution for 30 minutes. Rinse and dry. For materials that can be sterilized, sterilize according to the type of material.
3) Other metallic containers should be cleaned and sterilized in a normal manner.
4) Linens should be put in double-layered plastic bags and labeled as “COVID-19”.
5) Clean the floor surface using sodium hypochlorite solution with a disposable mop.
6) Allow 1 hour for natural air change in the angiography room before starting the next examination.
It is of extreme importance that all members of the team are familiar with this protocol. Training for proper use and removal of the PPE are vital in preventing contamination, which tends to occur especially after the procedure. A COVID-19 emergency protocol drill should be carried out at least once among the team. These infection prevention measures would take extra 10–15 minutes compared to the regular procedure in our experience with practice. However, we believe that these extra minutes will ensure safety to healthcare workers and other patients.
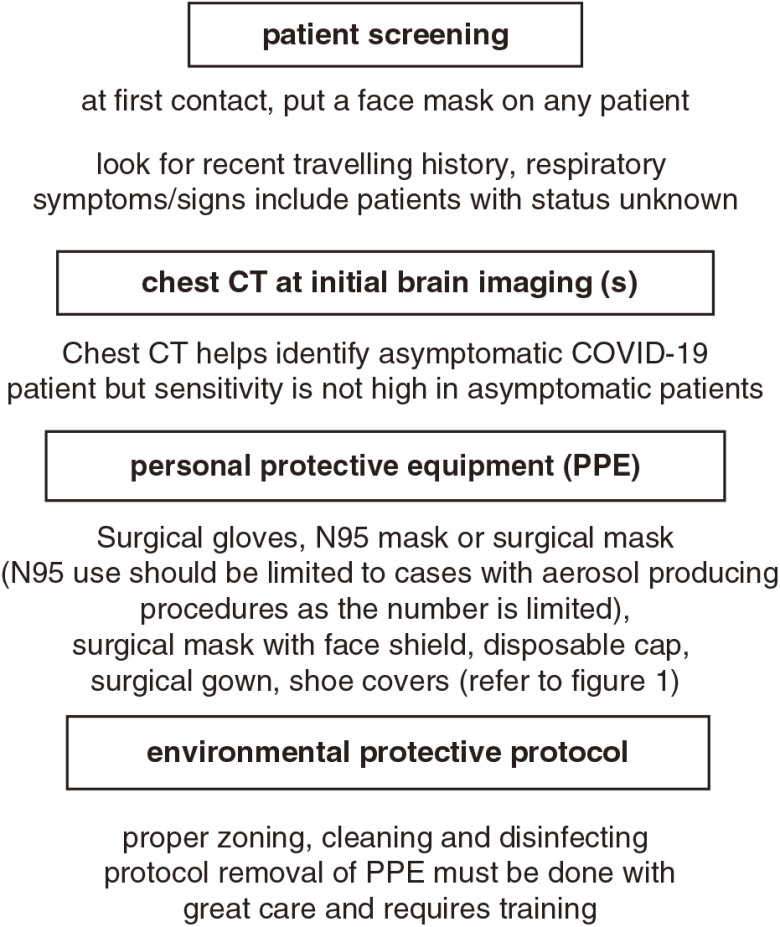
A quick flowchart is outlined in Fig. 3.
Fig. 3. A chart showing the important steps in managing a stroke patient with possible COVID-19. COVID-19: coronavirus disease.
Limitations
The protocol proposed in this article should be used with flexibility because our protocol is made based on medical source in our hospital and current COVID-19 epidemicity. Screening of the patient and the range of application of using the suggested PPE will depend on the epidemicity in the area or the availability of PPE. COVID-19 is a new disease with growing evidence. The more we learn about it, the more efficient we can be in protecting our environment. We stress, for one more time, the importance of keeping the N95 masks for reusage when the supply is low and the importance of training for proper use of PPE.
Acknowledgments
The authors deeply thank Dr. Shinichi Matsuda, a pediatrician in our hospital, for the inspiration for starting this project. The authors also thank Michiko Kobayashi, an infection control nurse in our hospital, for providing help in training the staff according to this protocol. All authors pledge that this manuscript does not contain previously published material and is not under consideration for publication elsewhere.
Disclosure Statement
The authors declare no conflicts of interest.
References
- 1).World Health Organization : Naming the coronavirus disease (COVID-19) and the virus that causes it. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(COVID-2019)-and-the-virus-that-causes-it (Accessed: April 3, 2020). [Google Scholar]
- 2).Mao L, Wang M, Chen S, et al. : Neurological manifestations of hospitalized patients with COVID-19 in Wuhan, China: a retrospective case series study. medRxiv 2020:2020.02.22.20026500. doi: 10.1101/2020.02.22.20026500. [Google Scholar]
- 3).Folsom AR, Gottesman RF, Appiah D, et al. : Plasma d-Dimer and incident ischemic stroke and coronary heart disease: the Atherosclerosis Risk in Communities Study. Stroke 2016; 47: 18–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4).Fraser FJ, Authur A, Chen M, et al. : Society of NeuroInterventional Surgery recommendations for the care of emergent neurointerventional patients in the setting of COVID-19. 2020. March. https://www.snisonline.org/wp-content/uploads/2020/03/SNIS-COVID-Stroke-Protocol.pdf (Accessed: March 30, 2020). [DOI] [PubMed] [Google Scholar]
- 5).Goyal M, Menon BK, van Zwam WH, et al. : Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomized trials. Lancet 2016; 23: 1723–1731. [DOI] [PubMed] [Google Scholar]
- 6).Inui S, Fujikawa A, Jitsu M, et al. : Chest CT findings in cases from the cruise ship “Diamond Princess” with coronavirus disease 2019 (COVID-19). Radiol Cardiothorac Imaging 2020; 2. doi.org/10.1148/ryct.2020200110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7).Fang Y, Zhang H, Xie J, et al. : Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology Feb 19, 2020. doi.org/10.1148/radiol.2020200432. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8).Cheng VCC, Wong SC, Chen JHK, et al. : Escalating infection control response to the rapidly evolving epidemiology of the coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect Control Hosp Epidemiol March 5, 2020. doi: 10.1017/ice.2020.58. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9).Kampf G, Todt D, Pfaender S, et al. : Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect 2020; 104: 246–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10).van Doremalen N, Bushmaker T, Morris DH, et al. : Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med March 17, 2020. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11).Mossa-Basha M, Meltzer CC, Kim DC, et al. Radiology department preparedness for COVID-19: radiology scientific expert panel. Radiology March 16, 2020. doi: 10.1148/radiol.2020200988. [DOI] [PMC free article] [PubMed] [Google Scholar]