Abstract
Objective
Dural arteriovenous fistula (dAVF) is an abnormal vascular communication between the meningeal artery and vein at the dura mater, with frequent recruitment of collateral arterial pedicles. In recent years, Onyx embolization has become the mainstay intervention for dAVF at various locations, although an unfavorable vascular anatomy often limits effective obliteration of the lesion. Balloon assistance may facilitate curable occlusion of the abnormal shunt with Onyx while preserving the patency of the affected sinus, even in complicated dAVFs.
Methods
We retrospectively reviewed the clinical and angiographic findings of patients with dAVF treated endovascularly in our institution between September 2018 and August 2019. Based on the detailed analysis of individual angioarchitecture, we defined complicated dAVF as lesions for which a complete cure is considered difficult to achieve with simple transarterial Onyx embolization alone, primarily due to a high flow and/or diffuse shunt with or without drainage to the functioning but compromised sinus. We evaluated the preoperative symptoms, anatomical classification, endovascular procedure, radiologic results, and clinical outcomes of these patients.
Results
Five patients met our criteria, all of whom were treated with balloon-assisted Onyx embolization (two superior sagittal sinus dAVF, two transverse–sigmoid sinus dAVF, and one torcular dAVF). In four cases, Onyx was injected from a tiny branch of the middle meningeal artery under balloon occlusion of the collateral arteries or balloon devascularization of the competitive inflow. In three cases, balloon sinus protection was performed to prevent the inadvertent occlusion of the vital venous outflow with Onyx. In one case, for the complementary occlusion of the remnant shunt through the previously coiled but recanalized occipital artery, Onyx was injected from the wire lumen of a dual-lumen balloon catheter to avoid undesirable reflux. The angiographic results were an anatomical cure in four cases and near-complete occlusion in one case. No procedural complications were observed in any cases. The clinical outcome was a complete cure in four cases and improvement in one case.
Conclusion
Our cases suggest that balloon devascularization can improve the unfavorable flow environment and simplify the vascular anatomy. Balloon sinus protection can support not only securing the patency of the normal venous outflow but also encourage aggressive intervention. Onyx injection via a dual-lumen balloon catheter can augment the controllability of embolization while preventing reflux. Each of these techniques can facilitate safe and effective Onyx embolization in the treatment of complicated dAVFs, and their combination may further expand the therapeutic horizon.
Keywords: balloon-assist technique, dural AVF, Onyx, transarterial embolization
Introduction
Dural arteriovenous fistula (dAVF) is an abnormal vascular communication between the meningeal artery and vein at the dura mater, with frequent recruitment of transosseous branches from the scalp arteries. In recent years, endovascular occlusion using Onyx (eV3, Irvine, CA, USA), a liquid and non-adhesive embolic material, has become the mainstay intervention for dAVF at various locations. However, an unfavorable vascular anatomy, such as a huge number of arterial pedicles and/or drainage to the functioning sinus, often limits the safe and effective obliteration of the shunt.1) In such disadvantageous situations, balloon-assisted techniques may facilitate curable arterio-arterial filling of the abnormal vascular networks with Onyx while preserving the patency of the functioning but compromised sinus, even with complicated dAVFs.2–13)
We herein report our experience with balloon-assisted Onyx embolization in the treatment of complicated dAVFs and discuss its utility and future perspective.
Materials and Methods
We retrospectively reviewed the clinical and angiographic findings of the patients with dAVF treated endovascularly in our institution between September 2018 and August 2019. Based on the detailed analysis of individual angioarchitecture, we defined complicated dAVF as lesions for which a complete cure is considered difficult to achieve with simple transarterial Onyx embolization alone, primarily due to a high flow and/or diffuse shunt with or without drainage to the functioning but compromised sinus. Five of 11 patients met our criteria, all of whom were treated with balloon-assisted Onyx embolization. The endovascular treatment strategy, such as the selection of the injecting artery and type of balloon assistance, was personalized based on each individual’s angioarchitecture. All patients gave their written informed consent before receiving intervention. We evaluated the preoperative symptoms, anatomical classification, endovascular procedure, radiologic results, and clinical outcome of these patients.
Results
Tables 1–3 summarize the clinical and radiological characteristics of the five patients with complicated dAVF. Figures 1–3 show the various types of balloon-assisted techniques. Figures 4 and 5 show representative cases of balloon-assisted Onyx embolization. In four cases, Onyx was injected via a tiny branch of the middle meningeal artery under balloon occlusion of the collateral inflow with the use of HyperForm 4.0 × 7.0 mm (Medtronic, Minneapolis, MN, USA). In three cases, balloon sinus protection was performed to secure the patency of the vital venous outflow using SHOURYU SR 4.0 × 15.0 mm (Kaneka, Osaka, Japan), although it had not been recommended as dimethyl sulfoxide (DMSO) compatible device. In one case, for the complementary occlusion of the remnant shunt through the previously coiled but recanalized occipital artery, Onyx was injected via an inflated DMSO compatible dual-lumen balloon catheter (Scepter C 4.0 × 11.0 mm; Microvention, Aliso Viejo, CA, USA) to prevent undesirable reflux. The angiographic results were an anatomical cure in four cases and near-complete occlusion in one case. No procedural complications were observed in any cases. The clinical outcome was a complete cure in four cases and improvement in one case.
Table 1. Clinical characteristics of five patients with complicated dural arteriovenous fistula.
| No. | Age/Sex | Preoperative symptoms | Location | Arterial supply | Venous drainage | Borden/Cognard |
|---|---|---|---|---|---|---|
| 1 | 71/M | Transient hemiparesis* | SSS | Bil MMA, bil STA, bil OA, AFA | Antegrade | 3/4 |
| 2** | 42/M | Hemorrhage, seizure, venous hypertension/infarction | SSS | Bil MMA, bil STA, bil OA, AFA | Antegrade | 3/3 |
| 3*** | 20/M | Headache and tinnitis | Torcular | Bil. PMA | Antegrade | 1/1 |
| 4**** | 63/M | Headache and tinnitis | Rt TS-SS | Rt. MMA, Rt. STA, Rt OA | Antegrade | 1/1 |
| 5***** | 72/F | Tinnitis and diplopia | Lt TS-SS | Lt MMA, bil STA, bil OA | Antegrade | 1/1 |
*Preoperative single-photon emission computed tomography (SPECT) revealed broad hemodynamic impairment in both hemispheres, presumably a cause of the transient neurological symptom.
**The patient underwent urgent occlusion of the left MMA with coils and the right MMA with n-butyl-2-cyanoacrylate. Because intractable seizure persisted postoperatively and diffusion-weighted image/fluid-attenuated inversion recovery mismatch with marked hemodynamic impairment on SPECT was evident in the right parietooccipital lobe on the following day, transvenous balloon reopening of the occluded SSS was performed, with resolution of the neurological symptoms except for quadrantic hemianopsia. Curable Onyx embolization was performed a few weeks later.
***The patient had a history of subarachnoid hemorrhage secondary to acute sinus thrombosis that was successfully managed with anticoagulation therapy. Twelve months later, the patient presented with headache and tinnitis, and angiography revealed development of torcular dAVF with nearly occlusion of the left TS, which had not been detected on a previous angiogram.
****The patient had a history of symptomatic left TS-SS dAVF that had completely disappeared after sinus packing with coils. Eighteen months later, the patient presented with headache and tinnitis, and angiography revealed the new development of the right TS-SS dAVF.
*****The patient underwent urgent coil ligation of the left OA for provisional flow reduction because of the rapid worsening of diplopia, which promptly disappeared after intervention. Curable Onyx embolization was performed a few weeks later. AFA: anterior falcine artery; dAVF: dural arteriovenous fistula; MMA: middle meningeal artery; OA: occipital artery; PMA: posterior meningeal artery; SPECT: single-photon emission computed tomography; SS: sigmoid sinus; SSS: superior sagittal sinus; STA: superficial temporal artery; TS: transverse sinus
Table 2. Endovascular procedure of the patients.
| No. | Arterial pedicles for TAE | Type of balloon assistance | Site of balloon |
|---|---|---|---|
| 1 | Rt MMA | Balloon devascularization | Bil STA + Lt OA |
| 2 | Lt MMA | Balloon devascularization | Bil STA |
| 3 | Lt PMA | Sinus protection | Rt TS-Torcular |
| 4 | Rt MMA | Balloon devascularization + sinus protection | Rt OA + Rt TS-SS |
| 5 | Lt MMA + Lt OA* | Balloon devascularization + sinus protection + proximal flow control | Bil OA + Lt TS-SS |
*Complementary injection from the OA was added for the remnant shunt following the single injection of Onyx through a tiny branch of the MMA in the same session.
MMA: middle meningeal artery; OA: occipital artery; PMA: posterior meningeal artery; SS: sigmoid sinus; STA: superficial temporal artery; TAE: transarterial embolization; TS: transverse sinus.
Table 3. Radiological and clinical results of the patients.
| No. | Total number of endovascular sessions | Total radiation dose (mGy) | Anatomical result | Procedural complication | Clinical outcome (mRS) |
|---|---|---|---|---|---|
| 1 | 1 (balloon-assisted Onyx TAE) | 3854 | anatomical cure; unchanged at 1 yr | none | complete cure, 19 mo (0) |
| 2 | 3 (Feeder ligation/sinus reopening/balloon-assisted Onyx TAE) | 7513* + 5226 + 5747 = 18486 | anatomical cure; unchanged at 1 mo | none | improved, 1 mo (1; quadrantic hemianopsia) |
| 3 | 2 (TAE/balloon-assisted Onyx TAE) | 2722 + 4846 = 7568 | anatomical cure; unchanged at 6 mo | none | complete cure, 14 mo (0) |
| 4 | 2 (contralateral TVE/balloon-assisted Onyx TAE) | 6267 + 5001 = 11268 | anatomical cure; unchanged at 6 mo | none | complete cure, 13 mo (0) |
| 5 | 2 (Feeder ligation/balloon-assisted Onyx TAE) | 3545 + 4040 = 7585 | near complete occlusion | none | complete cure, 8 mo (0) |
*Urgent occlusion of the left middle meningeal artery with coils and the right middle meningeal artery with n-butyl-2-cyanoacrylate are performed in a single session.
mRS: modified Rankin Scale; TAE: transarterial embolization; TVE: transvenous embolization.
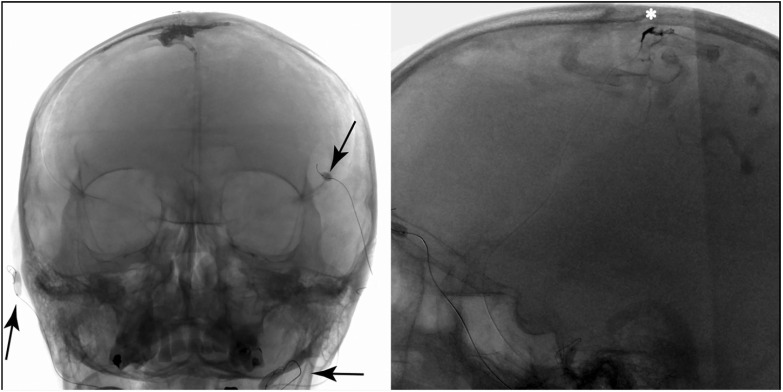
Fig. 1. Intraoperative fluoroscopic image of case 1 showing simultaneous balloon occlusion of the bilateral superior temporal arteries and left occipital artery as balloon devascularization (arrows, HyperForm, 4.0 × 7.0 mm). Note the preoperative injection via the microcatheter (asterisk), which helps increase the physician’s understanding of the core angioarchitecture of the lesion.
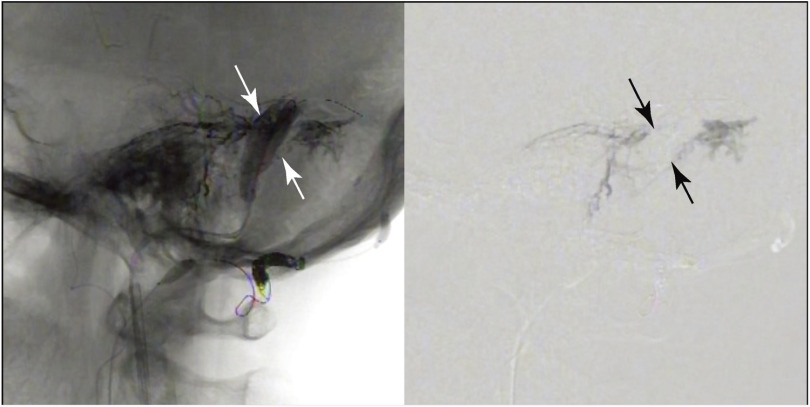
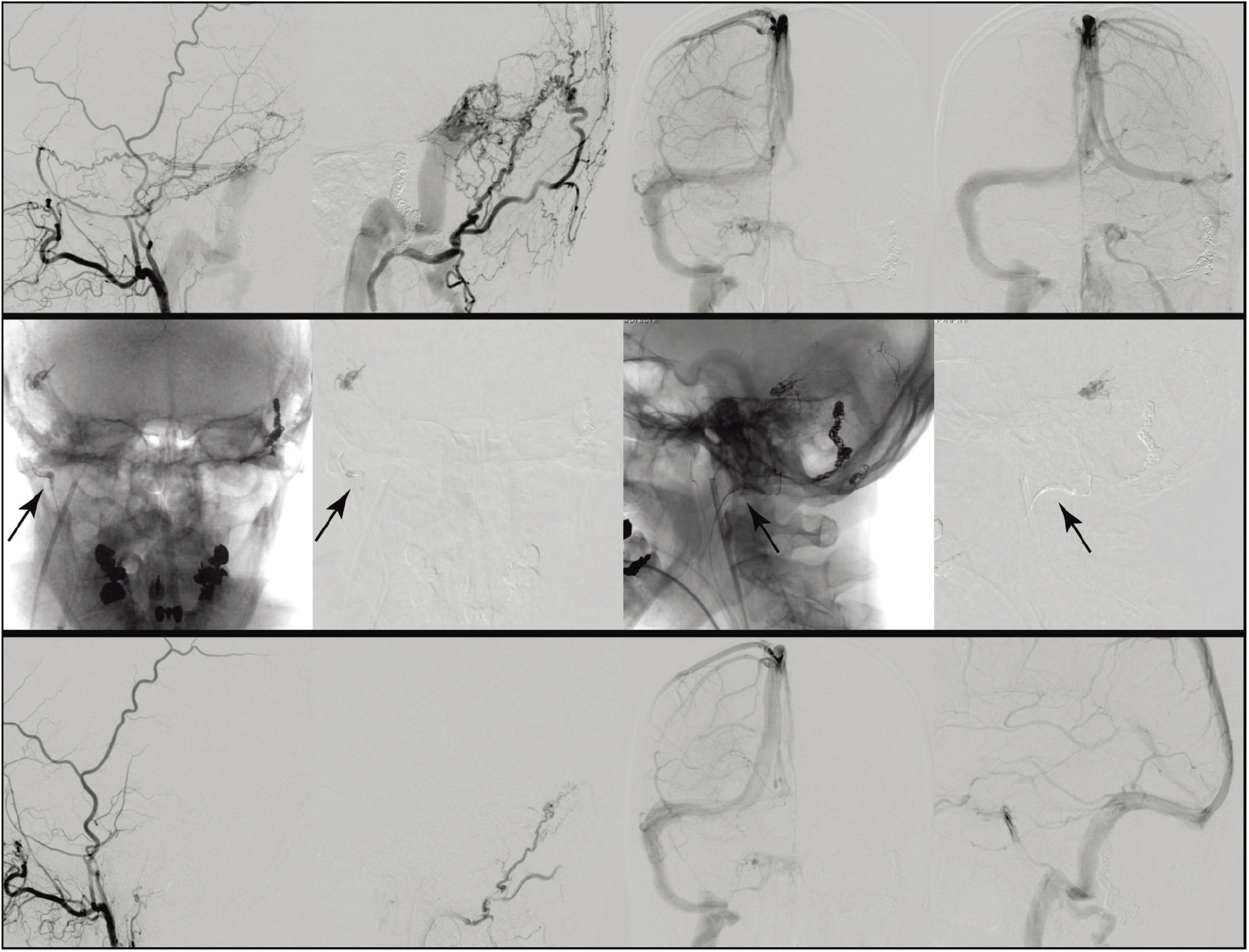
Fig. 2. Intraoperative fluoroscopic image and corresponding blank roadmap image of case 5, showing the balloon sinus protection technique (arrows, SHOURYU SR, 4.0 × 15.0 mm). The injected Onyx propagates across the sigmoid sinus, which is occupied by inflated balloons. Precaution is important for preventing the cranial nerve palsy, and injection should be strictly controlled when Onyx comes near to dangerous anastomosis, as is facial arcade in this case.
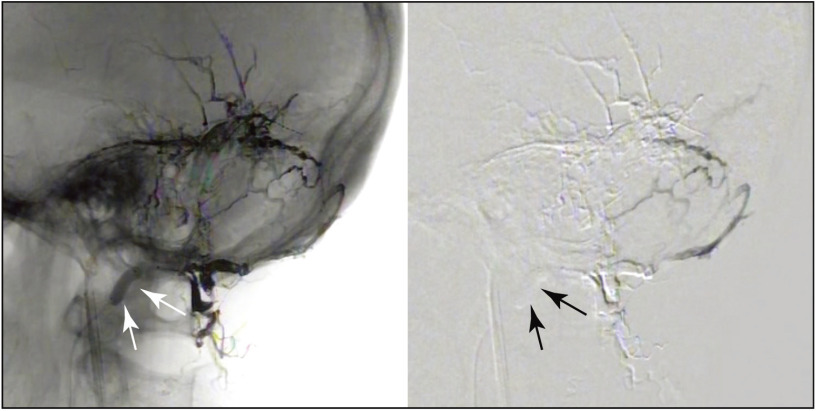
Fig. 3. Intraoperative fluoroscopic image and corresponding blank roadmap image of case 5, showing the proximal balloon flow control technique. The Onyx injected via the wire lumen of a dual-lumen balloon catheter (arrows, Scepter XC, 4.0 × 7.0 mm) penetrates far beyond the previously coiled but recanalized occipital artery while effectively filling the remnant shunt without undesirable refluxing. Close attention is needed for avoiding the iatrogenic embolic stroke, and injection should be strictly controlled when Onyx comes near to the dangerous anastomosis, as is occipital-vertebral anastomoses in this case.
Fig. 4. Case 1. (Upper column) A preoperative angiogram of the external carotid artery and internal carotid artery. The dural arteriovenous fistula is supplied by the bilateral middle meningeal arteries, bilateral superficial temporal arteries, bilateral occipital arteries, and anterior falcine artery (not shown) with direct connection to the parasagittal dilated cortical vein and draining into the superior sagittal sinus. (Middle column) Intraoperative fluoroscopic images and corresponding blank roadmap images. Onyx is injected via the tiny branch of the right middle meningeal artery while occluding the bilateral superficial temporal arteries and left occipital artery with balloons for devascularization (HyperForm, 4.0 × 7.0 mm). Note that the Onyx crosses the midline through the roof of the superior sagittal sinus (arrow) and refluxes into the transosseous branches (arrowhead), and the injection is ceased just before disturbing the normal venous circulation (asterisk). (Lower column) A postoperative angiogram of the external and internal carotid arteries. The shunt has disappeared with preservation of the normal venous outflow in a single session.
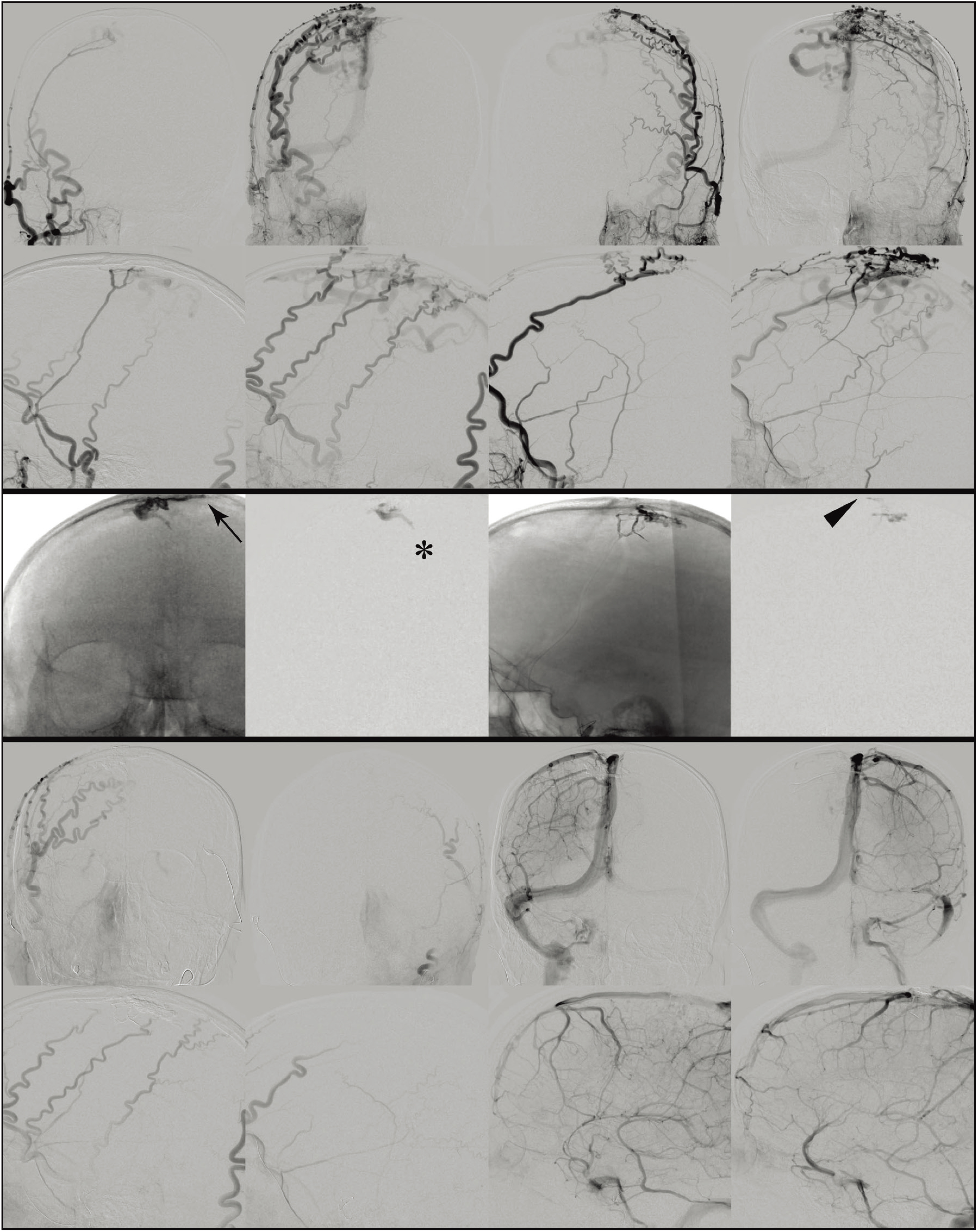
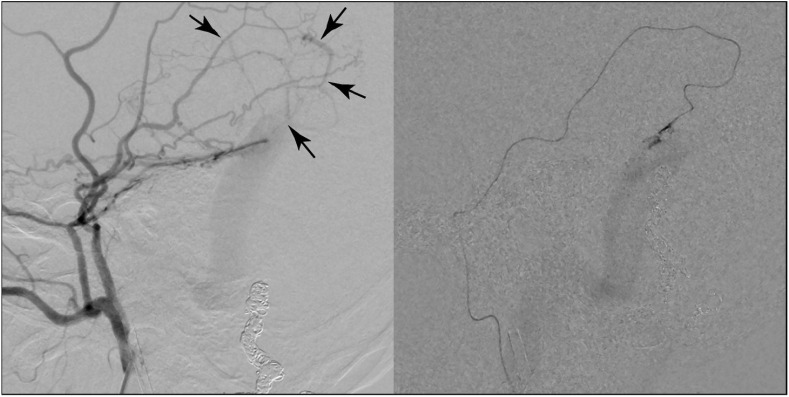
Fig. 5. Case 4. (Upper column) A preoperative angiogram of the right distal external carotid artery, right occipital artery, and bilateral internal carotid artery. The dural arteriovenous fistula is supplied by the right middle meningeal artery, right superficial temporal artery, and right occipital artery with a connection to the right transverse–sigmoid sinus without cortical venous reflux. Note that the left transverse–sigmoid sinus is occluded due to previous treatment of the dural arteriovenous fistula with sinus packing. (Middle column) Intraoperative fluoroscopic images and corresponding blank roadmap images. The Onyx is injected via a tiny branch of the right middle meningeal artery while occluding the prominent right occipital artery with a balloon (arrows, HyperForm, 4.0 × 7.0 mm). (Lower column) A postoperative angiogram of the right distal external carotid artery, right occipital artery, and right internal carotid artery. The shunt is no longer presented with the preservation of the normal venous outflow after a single Onyx injection.
Discussion
Balloon-assisted techniques for transarterial Onyx embolization generally include balloon devascularization,5) sinus protection,9,10,12,14) proximal flow control,2–11) and combinations thereof.5,9,10) Previous studies reported that these adjunctions have several advantages over the simple technique, such as an improved occlusion rate, reduced reflux to feeding artery, lower injected volume of material, decreased periprocedural time, and protective effect for compromised sinus,2–13) although concern about procedure-related neurological complication remains. In particular, the petrosal branch of the middle meningeal artery, stylomastoid branch of the posterior auricular artery, and neuromeningeal trunk of the ascending pharyngeal artery feed facial and lower cranial nerves,14) carrying a risk of damage if the physician fails to recognize them and occludes them with Onyx. Furthermore, the lack of recognition of extracranial–intracranial anastomoses can cause iatrogenic embolic stroke during Onyx injection. While whether or not balloon assistance significantly increases the incidence of these event is unclear, precautions against such avoidable complications are extremely important, just in case, when using these adjunctive techniques.
Balloon occlusion of the collateral arteries, or balloon devascularization, results in the reduction of the competitive inflow within the abnormal shunt networks. Since the liquid material flows according to the pressure gradient, the suppression of the competing inflow makes it easier for the penetration of Onyx to flow to a more upstream side of the collateral arteries. This is essential for preventing recurrence because insufficient arterio-arterial filling of the abnormal vascular network can result in the development of abnormal arterial pedicles postoperatively. Furthermore, balloon devascularization can simplify the vascular anatomy, thereby improving the physician’s understanding of the core angioarchitecture, which becomes more important with the increasing complexity of the vascular anatomy.
Occlusion of the collateral arteries using particle embolization, coil ligation, and n-butyl-2-cyanoacrylate can also decrease any competing inflow. However, when attempting Onyx embolization under preparatory devascularization with these methods, the irradiation dose is inevitably increased in comparison to balloon devascularization. Accordingly, if there are multiple candidate arteries for devascularization, as is frequently seen in complicated dAVF, then balloon use is clearly less invasive than these methods. More importantly, in contrast to the irreversible devascularization associated with these methods, balloon use can preserve the accessible collateral branches, thus providing a second chance to achieve complete occlusion when the remnant shunt exists after a single Onyx injection.
Balloon occlusion of the affected sinus or sinus protection can occupy the intraluminal space and provide counterpressure at the wall, acting as a scaffolding to prevent inadvertent migration of the Onyx toward the venous side. In the early series of 21 dAVFs treated with Onyx without sinus protection, the patency of the related sinus was impaired in 35% of cases.15) Balloon sinus protection techniques may be useful for preventing iatrogenic occlusion of the vital venous structures, even if anastomotic channels are diffusely present along the sinus wall.
In our series, we placed double 4.0 × 15.0 mm balloons (SHOURYU SR) in parallel for sinus protection, which seemed much safer than using larger but shorter ones (e.g. 7.0 × 7.0 mm intracranial balloon). The intracranial macroballoon such as Copernic RC (Balt; Montmorency, France), which has a single-lumen flexible balloon catheter 8.0 or 10.0 mm in diameter and 80.0 mm in length, can sufficiently occlude the sinus even with a single use, although the device is not permitted for domestic use in Japan at present. This macroballoon has widespread availability and has been applied in a number of different settings, such as for percutaneous transluminal angioplasty of acute sinus thrombosis, sinus occlusion testing in a preoperative patient with a skull base tumor, and for the protection of the internal and common carotid arteries during Onyx injection to a carotid body tumor.
Balloon occlusion of the injecting artery, or proximal flow control, can simulate a wedge flow condition and allow for the broad propagation of the liquid embolic agent with improved controllability without undesirable reflux.2–11) However, this procedure usually involves navigating a dual-lumen balloon catheter a fair distance to the target vessel, which can be difficult due to anatomic reasons, such as a small caliber and/or tortuous branch course. In the present case, we used this technique in a prominent occipital artery to achieve distal progression of the Onyx while preventing proximal reflux to the branches, which might have caused ischemic complications if they had become occluded.
The combination of different techniques may expand the therapeutic horizon of Onyx embolization for complicated dAVFs.5,9,10) For instance, combining proximal flow control and sinus protection not only secures the vital venous outflow but also encourages aggressive Onyx injection. Indeed, with this approach, injected Onyx can spread far over abnormal vascular networks, which seems difficult to achieve with the conventional plug and push technique alone. However, a dual-lumen balloon catheter often cannot be used to endovascularly access small and/or tortuous feeder vessels. The pressure cooker technique may be useful in some such cases,16) although the original technique requires the use of a detachable DMSO compatible catheter, which has not yet been approved for domestic use in Japan. However, when deliberately selecting a tiny branch of the dural artery as the injecting vessel, as shown in Fig. 6, a wedge flow-like condition can be created, and this approach seems to function well with balloon devascularization and sinus protection, as was performed in cases 4 and 5. There remains room for the further development of these techniques, devices, and their combinations, and the accumulation of more information is earnestly awaited.
Fig. 6. Case 5. (Left) Preoperative angiogram of the right distal external carotid artery. Note the tip of the 4-Fr catheter is advanced beyond the orifice of the right occipital artery to simplify the anatomy and identify the subtle shunt point. We deliberately selected a tiny branch of the right middle meningeal artery as the safe injecting vessel (arrows). (Right) The tip of the microcatheter was navigated very close to the fistula. Transvenous sinus balloons (SHOURYU SR, 4.0 × 15.0 mm) are next prepared to prevent inadvertent occlusion of the venous outflow during Onyx injection.
Conclusion
Our cases suggest that balloon devascularization can improve the unfavorable flow environment and simplify the vascular anatomy. Balloon sinus protection can not only help secure the patency of the normal venous outflow but also facilitate aggressive intervention. Onyx injection using an inflated dual-lumen balloon catheter can augment the controllability of embolization while preventing undesirable reflux. Each of these techniques facilitates safe and effective Onyx embolization in the treatment of complicated dAVFs, and the combination of these techniques may further expand the therapeutic horizon.
Disclosure Statement
The authors declare no conflicts of interest associated with this manuscript.
References
- 1).Gross BA, Albuquerque FC, Moon K, et al. : Evolution of treatment and a detailed analysis of occlusion, recurrence, and clinical outcomes in an endovascular library of 260 dural arteriovenous fistulas. J Neurosurg 2017; 126: 1884–1893. [DOI] [PubMed] [Google Scholar]
- 2).Andreou A, Ioannidis I, Nasis N: Transarterial balloon-assisted glue embolization of high-flow arteriovenous fistulas. Neuroradiology 2008; 50: 267–272. [DOI] [PubMed] [Google Scholar]
- 3).Chiu AH, Aw G, Wenderoth JD: Double-lumen arterial balloon catheter technique for Onyx embolization of dural arteriovenous fistulas: initial experience. J Neurointerv Surg 2014; 6: 400–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4).Dabus G, Linfante I, Martínez-Galdámez M: Endovascular treatment of dural arteriovenous fistulas using dual lumen balloon microcatheter: technical aspects and results. Clin Neurol Neurosurg 2014; 117: 22–27. [DOI] [PubMed] [Google Scholar]
- 5).Huo X, Li Y, Jiang C, et al. : Balloon-assisted endovascular treatment of intracranial dural arteriovenous fistulas. Turk Neurosurg 2014; 24: 658–663. [DOI] [PubMed] [Google Scholar]
- 6).Kim JW, Kim BM, Park KY, et al. : Onyx embolization for isolated type dural arteriovenous fistula using a dual-lumen balloon catheter. Neurosurgery 2016; 78: 627–636. [DOI] [PubMed] [Google Scholar]
- 7).Kim ST, Jeong HW, Seo J: Onyx embolization of dural arteriovenous fistula, using scepter c balloon catheter: a case report. Neurointervention 2013; 8: 110–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8).Paramasivam S, Niimi Y, Fifi J, et al. : Onyx embolization using dual-lumen balloon catheter: initial experience and technical note. J Neuroradiol 2013; 40: 294–302. [DOI] [PubMed] [Google Scholar]
- 9).Piechowiak E, Zibold F, Dobrocky T, et al. : Endovascular treatment of dural arteriovenous fistulas of the transverse and sigmoid sinuses using transarterial balloon-assisted embolization combined with transvenous balloon protection of the venous sinus. AJNR Am J Neuroradiol 2017; 38: 1984–1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10).Shi ZS, Loh Y, Duckwiler GR, et al. : Balloon-assisted transarterial embolization of intracranial dural arteriovenous fistulas. J Neurosurg 2009; 110: 921–928. [DOI] [PubMed] [Google Scholar]
- 11).Spiotta AM, Miranpuri AS, Vargas J, et al. : Balloon augmented Onyx embolization utilizing a dual lumen balloon catheter: utility in the treatment of a variety of head and neck lesions. J Neurointerv Surg 2014; 6: 547–555. [DOI] [PubMed] [Google Scholar]
- 12).Vollherbst DF, Ulfert C, Neuberger U, et al. : Endovascular treatment of dural arteriovenous fistulas using transarterial liquid embolization in combination with transvenous balloon-assisted protection of the venous sinus. AJNR Am J Neuroradiol 2018; 39: 1296–1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13).Zhang Y, Li Q, Huang QH: Embolization of a superior sagittal sinus dural arteriovenous fistula under intrasinus balloon protection: a case report. Interv Neuroradiol 2015; 21: 94–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14).Geibprasert S, Pongpech S, Armstrong D, et al. : Dangerous extracranial-intracranial anastomoses and supply to the cranial nerves: vessels the neurointerventionalist needs to know. AJNR Am J Neuroradiol 2009; 30: 1459–1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15).Abud TG, Nguyen A, Saint-Maurice JP, et al. : The use of Onyx in different types of intracranial dural arteriovenous fistula. AJNR Am J Neuroradiol 2011; 32: 2185–2191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16).Chapot R, Stracke P, Velasco A, et al. : The pressure cooker technique for the treatment of brain AVMs. J Neuroradiol 2014; 41: 87–91. [DOI] [PubMed] [Google Scholar]