Abstract
Objective
This report presents a case of mechanical thrombectomy for left internal carotid artery (ICA) terminal portion occlusion performed by left common carotid artery recanalization during hospitalization after diagnosing bilateral common carotid artery occlusion due to Takayasu arteritis.
Case Presentation
A 25-year-old woman with fever and cervix pain a few months ago visited our department after repeated transient aphasic attacks. Magnetic resonance imaging (MRI) demonstrated diffuse infarction in the left middle cerebral artery (MCA) area, and she was diagnosed with Takayasu arteritis due to bilateral common carotid artery occlusion and left subclavian artery stenosis. On the 20th day of hospitalization, the terminal portion of the left ICA was occluded and thrombectomy was performed after balloon dilation of the left common carotid artery. Lastly, left common carotid artery stenting was performed. Aphasia and sensory disturbance remained, but she was transferred to a rehabilitation hospital with a modified Rankin Scale (mRS) of 2 on the 65th day of hospitalization. Antithrombotic and immunosuppressive therapy were performed, and restenosis did not develop.
Conclusion
Angioplasty and stenting of common carotid artery occlusion can be effective treatments in thrombectomy for intracranial occlusion due to Takayasu disease.
Keywords: acute-phase revascularization, mechanical thrombectomy, Takayasu arteritis, aortitis syndrome, occlusion of the common carotid artery
Introduction
Takayasu arteritis is a disease in which inflammation of the aorta or great vessels branching from the aorta occurs, inducing failure of multiple organs, such as the brain, heart, and kidneys, through vascular stenosis/occlusion. In some cases, common carotid or subclavian artery stenosis/occlusion causes acute ischemic stroke, but few studies have reported mechanical thrombectomy. A case of Takayasu arteritis with complete occlusion of bilateral common carotid arteries (CCA) developed a minor stroke and was hospitalized. The terminal portion of the left internal carotid artery (ICA) was newly occluded during hospitalization and thrombectomy was performed. It was not possible to recanalize by the approach via the left posterior communicating artery (PcomA), and it was possible to recanalize by the approach via the left common carotid artery after recanalizing the left common carotid artery.
Case Presentation
Patient: A 25-year-old woman.
Present illness: In February X, discomfort/pain of the left cervicothoracic to jaw appeared. In March X, she consulted a local clinic for fever. The C-reactive protein (CRP) level was 8.7 mg/dL, demonstrating an increase. She was referred to the department of cardiology of our hospital. On the initial consultation, the right upper limb blood pressure was 129/90 mmHg and the left upper limb blood pressure was not measured. Neither cardiac auscultation nor electrocardiography revealed any abnormalities. Elective transthoracic echocardiography was scheduled. However, she cancelled this appointment based on self-judgment because the symptoms spontaneously subsided. In May X, she had a sudden aphasic attack that persisted for 3 hours. However, it spontaneously subsided and she did not consult the hospital. In June X, discomfort of the right upper limb and aphasia developed. She consulted a local clinic. A head magnetic resonance imaging (MRI) revealed cerebral infarction and she was transferred to our hospital by ambulance 12 hours after onset.
Medical history: Not contributory.
Family history/lifestyle: Not contributory.
Physical examination: The body temperature and pulse rate were 37.8°C and 127 bpm, respectively. The left and right blood pressures were 89/92 and 151/103 mmHg, respectively. The left radial artery was weakly palpable. Consciousness was clear. The Japan Coma Scale (JCS) score was 0 and the Glasgow Coma Scale (GCS) score was E4V5M6. Bilateral carotid artery bruits were heard. There were no cardiac or abdominal vascular murmurs. Although there was no paralysis or objective sensory disturbance, dysesthesia of the right upper and lower limbs was noted. Non-fluent aphasia involving phonemic paraphasia was present. The National Institutes of Health Stroke Scale (NIHSS) score was 1.
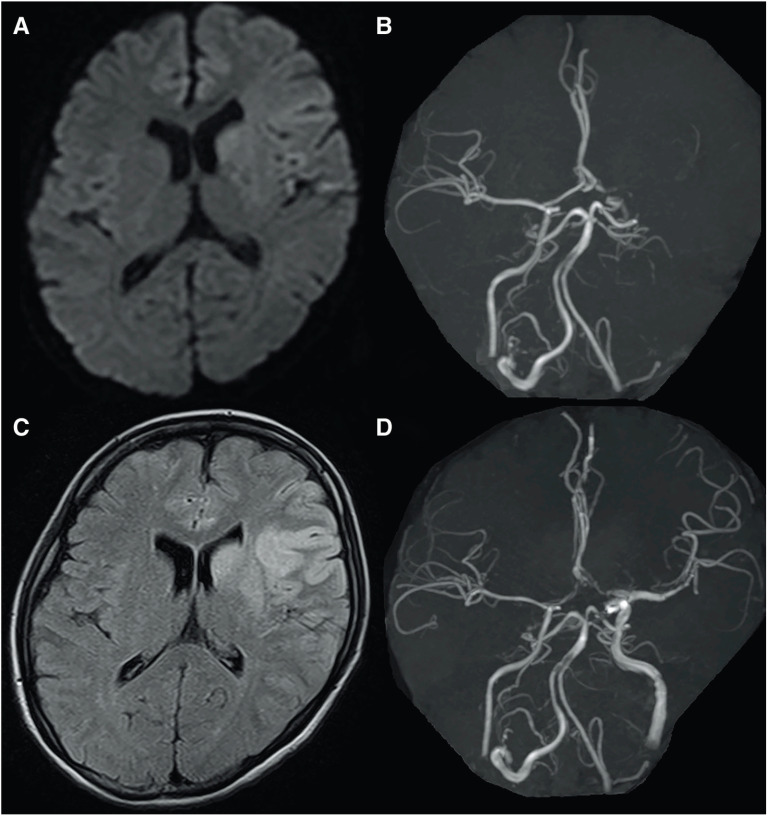
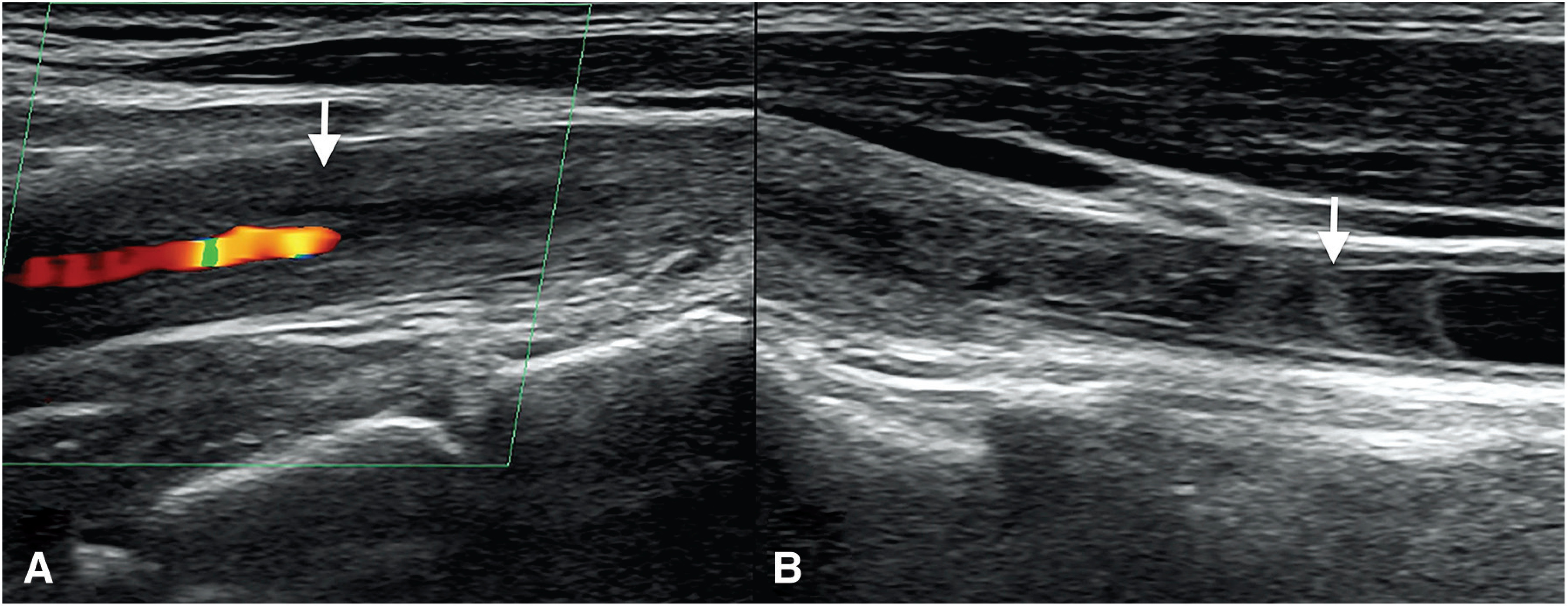
Laboratory data: Hematology demonstrated the leukocyte count, CRP level, and erythrocyte sedimentation rate to be 6600/mm3, 2.42 mg/dL, and 48 mm/h, respectively, suggesting slight inflammatory response. However, there was no abnormality in the coagulation system. A head MRI revealed diffuse minor infarction involving the left insular cortex to frontal lobe cortex. No intracranial major artery occlusion/stenosis was observed on magnetic resonance angiography (MRA). Cervical MRA revealed occlusion of the bilateral CCA. However, collateral pathways flowing in the bilateral external carotid arteries (ECA) were advanced and the bilateral ICA were visualized (Fig. 1A). Cerebral angiography demonstrated stenosis/occlusion of the left CCA; the stenotic site had tapered from the origin of this artery, involving a specific length (Fig. 1B). Marked stenosis at the origin of the left subclavian artery was observed (Fig. 1C). Inflow from the right ascending cervical artery to the right ECA, in addition to antegrade right ICA blood flow via the right CCA bifurcation, was confirmed. Furthermore, stasis related to inflow to the left CCA with proximal occlusion after inflow from the right inferior thyroid artery to the left ECA via the left superior thyroid artery was noted. Antegrade left ICA blood flow was confirmed (Fig. 1D and 1E). Carotid echography revealed marked thickening of the right CCA wall and complete occlusion involving the bifurcation. Blood flowing in the right ECA from a minor blood vessel had antegradely flowed in the right ICA via the bifurcation of the right CCA. Complete tapering-like occlusion of the left CCA was observed, exhibiting a macaroni sign specific to Takayasu arteritis (Fig. 2A). In the distal left CCA, which remained, a floating thrombus related to stasis of blood flowing from the left ECA was observed (Fig. 2B). Antegrade left ICA blood flow was confirmed. Echocardiography did not suggest valvular disease, wall movement disorder, or intra-cardiac thrombus. On electrocardiographic monitoring, there was no atrial fibrillation.
Fig. 1. (A) Cervical MRA. Bilateral CCA were occluded, but collateral blood flow into bilateral ECA developed and the bilateral ICA was visualized. (B) Left common carotid artery angiography. The left common carotid artery was tapered and occluded. (C) Left subclavian artery angiography. The left subclavian artery exhibited severe stenosis at the origin. (D) Innominate artery angiography (AP view). (E) Innominate artery angiography (lateral view). The right ascending carotid artery was flowing into the right ECA, and the right ICA was flowing antegradely via the right common carotid artery bifurcation. The right inferior thyroid artery was flowing into the left superior thyroid artery, then into the left ECA. The left common carotid artery was occluded in the middle, and its distal end was blinded and stagnant. The left ICA was flowing antegradely. CCA: common carotid arteries; ECA: external carotid artery; ICA: internal carotid artery; MRA: magnetic resonance angiography.
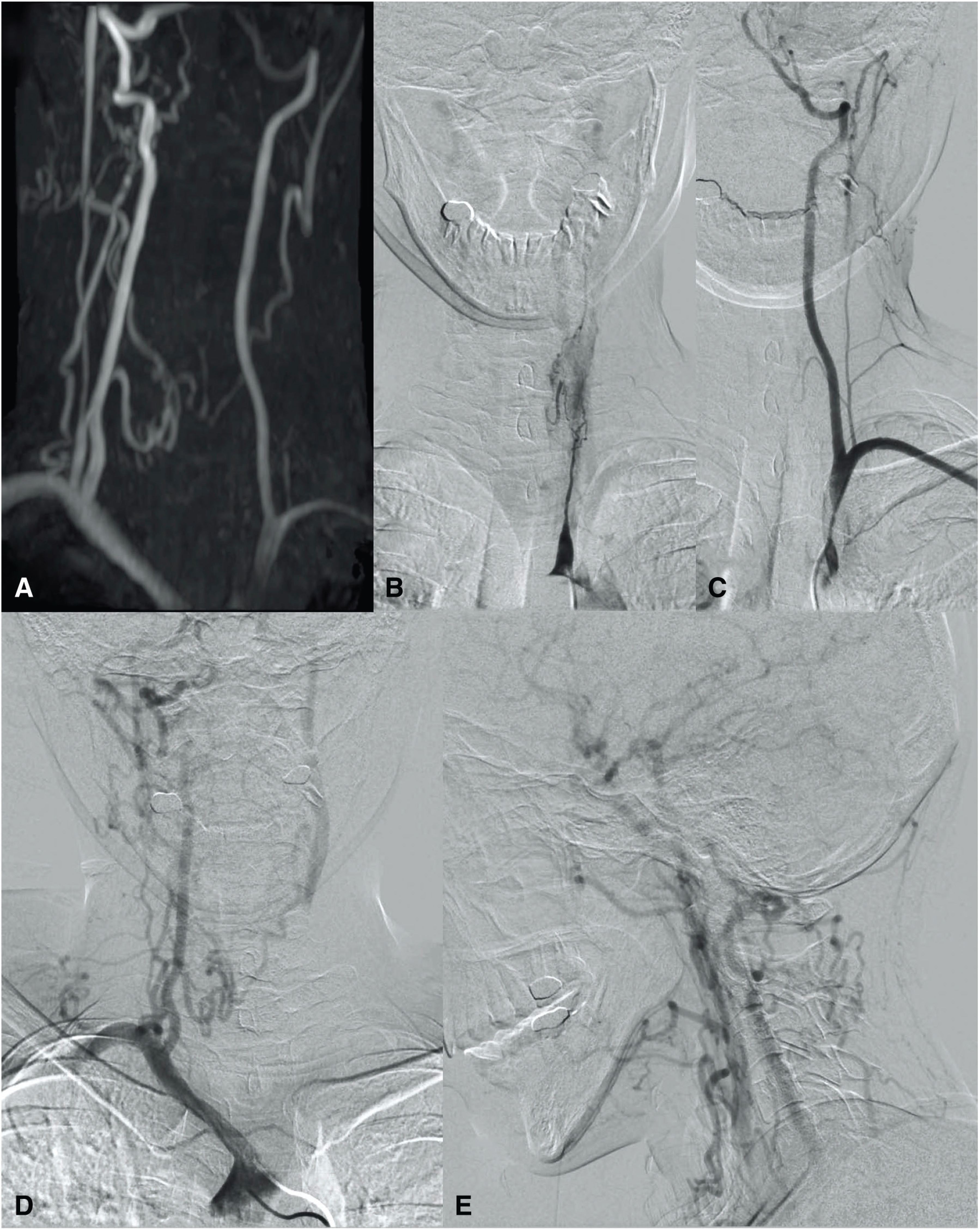
Fig. 2. Carotid artery echo. (A) The left common carotid artery had a “macaroni sign” (arrow). (B) The distal of left common carotid artery was not occluded and the blood clot was floating (arrow).
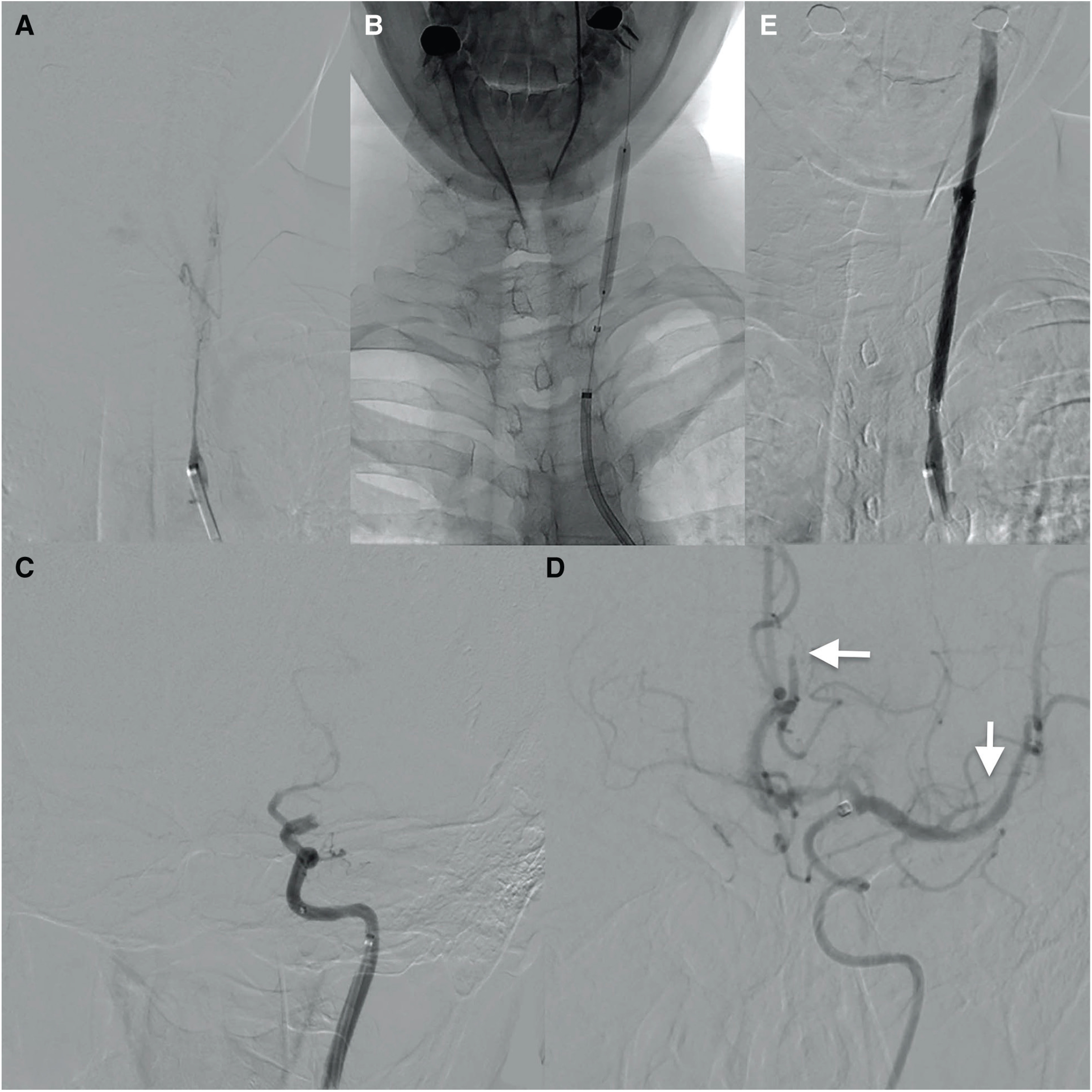
Course after admission: The patient was diagnosed with Takayasu arteritis-related occlusion of the left CCA and arteriogenic cerebral embolism related to a thrombus at its distal blind end based on the laboratory data. Treatment with 100 mg of aspirin and 40 mg of prednisolone (1 mg/kg body weight) was started, and rehabilitation gradually reduced aphasia. However, right complete paralysis and total aphasia suddenly developed in 20 days after admission (NIHSS score: 18). On a diffusion-weighted images (DWI) of head MRI 25 minutes after onset, a slight high-intensity signal was detected in the anterior territory of the left middle cerebral artery (MCA). The DWI-Alberta Stroke Program Early CT Score (ASPECTS) was 8 (Fig. 3A). MRA revealed occlusion at the terminal portion of the left ICA. The A1 portion of left anterior cerebral artery was slightly visualized through the anterior communicating artery, but visualization of the left MCA was poor (Fig. 3B). We considered mechanical thrombectomy to be indicated. The patient was immediately transferred to the cerebral angiography room and femoral artery puncture was performed 59 minutes after onset. Due to complete occlusion of the left CCA, this artery was not selected as a first-choice approach route. In the present case, the PcomA was advanced, reflecting the fetal type; therefore, we considered a method to access the left MCA through the PcomA from the posterior circulation. As stenosis at the origin of the left subclavian artery was observed, an approach through the right vertebral artery (VA), which was dilated in compensation, was selected. A 9Fr Optimo balloon guiding catheter (Tokai Medical Products, Aichi, Japan) was inserted into the brachiocephalic artery and a Penumbra 5MAX ACE (Penumbra Inc., Alameda, CA, USA) was guided into the right VA. Angiography confirmed occlusion at the terminal portion of the left ICA. This artery was retrogradely visualized (Fig. 4A). After 5000 units of heparin was intravenously injected, the Penumbra 5MAX ACE was guided into the basilar artery, and then into the distal M1 segment of left MCA via the P1 of left posterior cerebral artery and left PcomA using a Penumbra 3MAX (Penumbra Inc.) and CHIKAI 14 microguidewire 200 cm (Asahi Intecc, Aichi, Japan) (Fig. 4B). Initially, mechanical thrombectomy was attempted using a combined technique with a Trevo Xp 3.0/20 mm (Stryker, Kalamazoo, MI, USA) and Penumbra, but recanalization was not achieved. On the 2nd pass, a Trevo Xp 6.0/25 mm (Stryker) was used, but the Thrombolysis In Cerebral Infarction (TICI) grade was 1 (Fig. 4C). At this point, the interval from puncture was 105 minutes and flexion was marked; it was considered difficult to achieve recanalization using a similar approach. Although the left CCA was occluded, the left PcomA to distal left CCA was retrogradely enhanced and tapering-like occlusion was observed; therefore, the actual length of occlusion was considered to be short (Fig. 4D and 5A). The approach route was changed, considering that it may be possible to access the true lumen if lesion crossing was carefully performed. Using a 6Fr JB2 125 cm (Medikit, Tokyo, Japan), the Optimo was inserted to the origin of the left CCA for blood flow blockage. A Trevo PRO 14 microcatheter (Stryker) and CHIKAI microguidewire facilitated lesion crossing. As the Penumbra 5MAX ACE was unable to be passed, the site of left CCA occlusion was dilated at two points using a Shiden balloon catheter 4.0/40 mm (Kaneka Medics, Osaka, Japan) for angioplasty (Fig. 5B). Subsequently, the Penumbra 5MAX ACE alone was guided from the origin of the left CCA to the bifurcation while aspirating it with a pump, and inserted to the petrous portion by guiding the Penumbra 3MAX and CHIKAI microguidewire in advance. The Optimo was inserted to the cervical portion of the left ICA (Fig. 5C). As the Penumbra 5MAX ACE was unable to be guided beyond the cavernous portion of the left ICA, the Trevo Xp 6.0/25 mm was deployed through the M1 segment of left MCA after lesion crossing with the Penumbra 3MAX and CHIKAI microguidewire, and mechanical thrombectomy was performed using the combined technique. Distal embolism of the M2 segment of left MCA developed, but TICI 2a recanalization was achieved on the 4th pass 167 minutes after puncture. Distal embolism of the A2 segment of left anterior cerebral artery was also observed, and two passes with the Trevo Xp 3.0/20 mm did not lead to recanalization. Final angiography revealed improvement in the visualization of the M2 segment of left MCA and TICI 2b recanalization was achieved 232 minutes after puncture (291 minutes after onset) (Fig. 5D). On the other hand, marked stenosis of the left CCA involving an approximately 45-mm area remained, and left CCA stenting was performed considering the risk of embolism/re-occlusion. After distal blood flow blockage with a Guardwire 200 cm (Medtronic, Minneapolis, MN, USA), a Protégé RX 8.0/60 mm (Medtronic) was inserted. Post-dilation using a Sterling balloon catheter 4.0/40 mm (Boston Scientific, Natick, MA, USA) was conducted (Fig. 5E). Postoperative computed tomography (CT) revealed a slight low-density area in the anterior region of the left MCA and subarachnoid hemorrhage of the left Sylvian fissure. Hemorrhagic change was observed, but clopidogrel loading was conducted/added immediately after surgery as a stent was placed. Hypotensive and sedative treatments were performed. There was no enlargement of postoperative hemorrhage or hyperperfusion syndrome. It became possible to elevate the right upper and lower limbs the day after surgery, resisting gravity, although aphasia was marked (NIHSS score: 14). MRI demonstrated a high-intensity signal area in the anterior left frontal lobe on fluid-attenuated inversion recovery (FLAIR) images (Fig. 3C). MRA confirmed complete recanalization of the middle and anterior cerebral arteries (Fig. 3D). The subsequent course was favorable. Mild motor aphasia and sensory disturbance of the right body remained, but paralysis reduced and the patient became able to walk 15 days after surgery (NIHSS score: 5, modified Rankin Scale [mRS] score: 2). The dose of prednisolone was gradually decreased to 20 mg and the patient was referred to a rehabilitation hospital 65 day after admission. Treatment for left subclavian artery stenosis was next performed and dual antiplatelet therapy (DAPT) was continued for approximately 2 years. The dose of prednisolone was gradually decreased. Tocilizumab was additionally administered from June X+1 and methotrexate from October X+1. Cerebral angiography in September X+2 revealed intimal thickening at the site of left CCA stenting, but there was no significant restenosis. Although mild aphasia and sensory disturbance of the right half body remained, the patient was independent (mRS score: 2).
Fig. 3. (A) DWI on day 20 of hospitalization. (B) MRA on day 20 of hospitalization. (C) FLAIR on day 21 of hospitalization. (D) MRA on day of 21 of hospitalization. DWI: diffusion-weighed imaging; FLAIR: fluid-attenuated inversion recovery; MRA: magnetic resonance angiography.
Fig. 4. Thrombectomy on day 20 of hospitalization. (A) Right vertebral arteriography. The terminal portion of the left ICA was occluded. (B) We approached the lesion via the left PcomA. (C) Two passes were performed, but only TICI 1 recanalization was achieved. (D) The left ICA was retrogradely flowing to the left common carotid artery bifurcation. ICA: internal carotid artery; PcomA: posterior communicating artery; TICI: Thrombolysis In Cerebral Infarction.
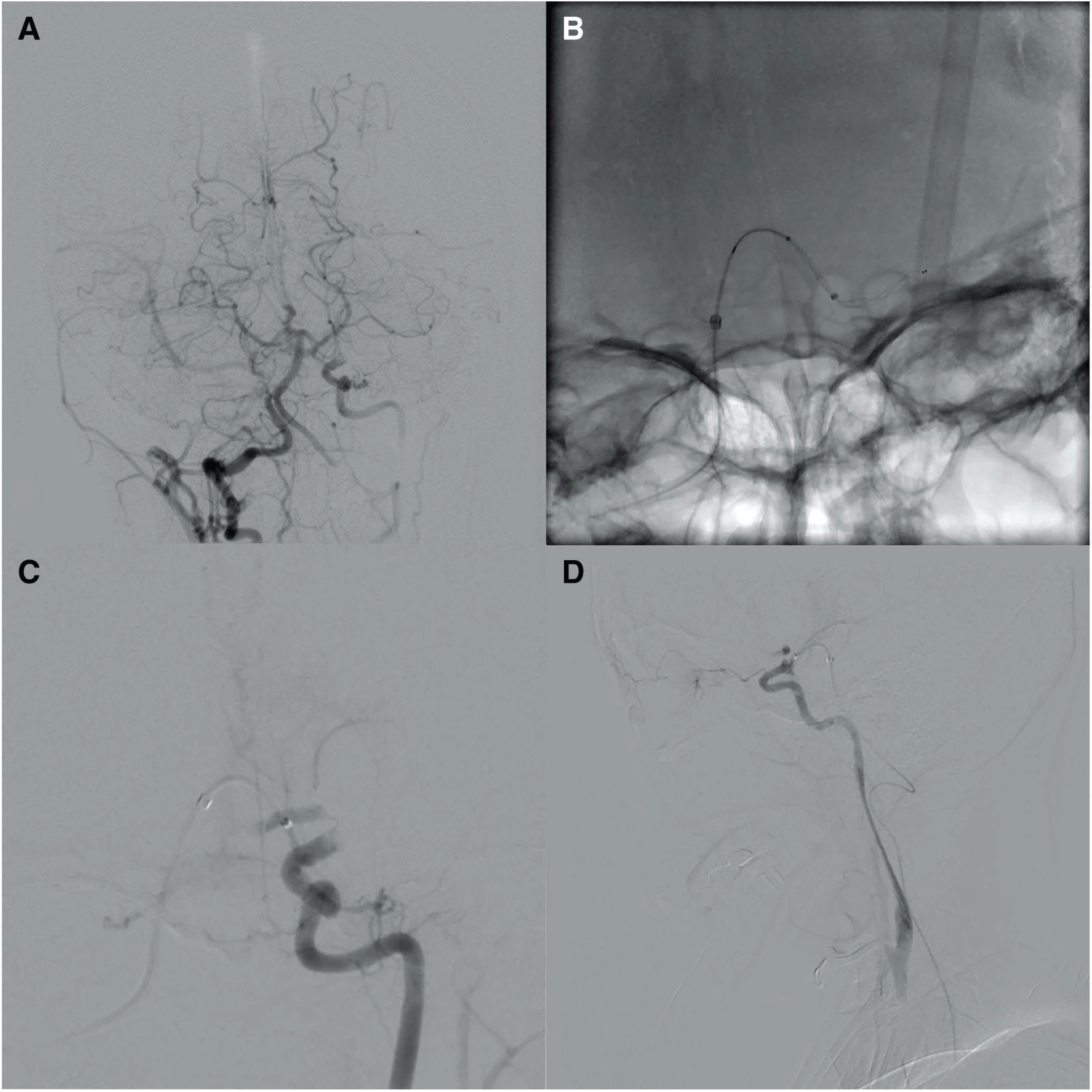
Fig. 5. (A) Left CCA angiography from Optimo. The net occlusion length of the left CCA was short. (B) Percutaneous angioplasty for CCA was performed. (C) Left ICA angiography. The terminal portion of the left ICA was still occluded. (D) TICI 2b recanalization was obtained by approaching from the left common carotid artery. The left A2 and left M2 were still occluded (arrow). (E) Carotid artery stenting was performed. CCA: common carotid artery; ICA: internal carotid artery; TICI: Thrombolysis In Cerebral Infarction.
Discussion
Aortitis is the general term for conditions related to inflammation of the aorta. As its etiology, giant cell arteritis is frequently detected in Europe and the United States, whereas Takayasu arteritis is frequently observed in Asia.1) Takayasu arteritis is frequent in young females and approximately 7000 patients have been registered as specific disease patients in Japan. The annual number of new-onset patients is estimated to be approximately 100–200.2) Takayasu arteritis is a disease in which inflammation of the aorta or great vessels branching from it occurs, causing cerebral ischemic symptoms/vision impairment/hearing loss/tooth pain related to aortic arch branch lesions, pulse absence or laterality of the blood pressure related to upper limb anemia, hypertension related to renal artery stenosis or aortic coarctation, pulmonary infarction related to pulmonary artery stenosis, and angina pectoris or myocardial infarction related to stenosis at the coronary orifice in some cases. The incidence of ischemic stroke in patients with Takayasu arteritis is reportedly 10%–20% in Europe and the United States.3) In Japan, Watanabe et al.4) reported that the incidence was 13.2%, and that embolism was observed in 3.7% of these patients. The pathogenesis of cerebral infarction in the presence of this disease is assumed as follows5): (1) vascular stenosis-related blood flow failure, (2) thrombus-derived embolism related to vascular-wall irregularity or turbulence, and (3) vascular occlusion related to dissection of the media. In the present case, blood flow stasis/a thrombus of the CCA as the blind end may have caused embolism, inducing ischemic stroke. Regarding acute-phase mechanical thrombectomy for major cerebral artery occlusion related to Takayasu arteritis, two case reports have been published.5,6) One patient had chronic occlusion of the left CCA and acute occlusion of the left MCA. For approaching, the left CCA was unable to be adopted and a posterior approach via the left PcomA was used. Urokinase at 480000 units was intra-arterially injected and aspiration with a Penumbra 3MAX led to recanalization.5) The other patient had occlusion of the bilateral ICA. Aspiration with a Penumbra for right ICA occlusion led to TICI 2b recanalization, and the use of a stent retriever for left ICA occlusion resulted in TICI 2b recanalization.6)
In the present case, an approach via the left PcomA was also initially selected, but it was difficult to achieve sufficient recanalization; therefore, the strategy was switched to another to achieve recanalization of the left CCA, which was completely occluded, leading to recanalization of the occluded intracranial blood vessel. In patients with Takayasu arteritis, thickening of the vascular wall is an etiological factor for occlusion. Recanalization was relatively readily achieved in comparison with atherothrombotic occlusion complicated by arteriosclerotic lesions. On the other hand, in the present case, marked stenosis involving a specific length remained after balloon dilation, and stenting was finally required to maintain sufficient intracranial blood flow and prevent recurrent embolic cerebral infarction involving the site of CCA occlusion and distal end. To our knowledge, this is the first case of acute-phase stenting for major cerebral artery occlusion related to this disease.
As a limitation of acute-phase carotid artery stenting for atherothrombotic occlusion, previous studies found that this procedure increased the risk of stroke/mortality.7) However, according to the STRATIS Registry, the results of mechanical thrombectomy for tandem lesions were compared between stenting and non-stenting groups, and the rate of patients with a favorable outcome was significantly higher in the former (68.5 vs. 42.2%, respectively). There were no significant differences in the mortality rate or incidence of symptomatic hemorrhage.8) Therefore, acute-phase carotid artery stenting for atherothrombotic occlusion may be an effective treatment option.
On the other hand, the limitations of stenting for stenosis/occlusion related to Takayasu arteritis slightly differ. Many studies reported that the incidence of restenosis after stenting for common carotid, subclavian, or VA stenosis was high (≥25%).9) In particular, concerning carotid artery stenting, restenosis was noted in two of three patients. Vision impairment was also reported.10)
Regarding the timing of treatment, in-stent restenosis may develop in the phase of high-level focal activity; this phase should be avoided.10) However, a previous study suggested that postoperative immunosuppressive therapy reduced the incidence of restenosis.11) Pathologically, the pathogenesis of vascular stenosis related to this disease is assumed as follows: inflammatory cell infiltration in the media to adventitia may result in media elastic fiber disappearance, exhibiting a moth-eaten appearance, and extensive fibrosis of the media and adventitia, leading to lumen stenosis through marked reactive fibrous thickening of the intima. Even in the chronic state in which a cicatricial lesion is present, inflammation with multinucleated giant cells at the lesion margin is sometimes observed.12) Therefore, if inflammation is reduced regardless of the timing, this may help prevent stenosis progression.
In the present case, complete occlusion of the left CCA was observed when the patient was admitted to our hospital after the onset of a transient ischemic attack (TIA) and minor stroke; the timing of occlusion is unclear. Major stroke occurred 20 days after admission and mechanical thrombectomy was performed after recanalization of the left CCA was achieved. In addition, left CCA stenting was conducted. Subsequently, there was no restenosis and the course was favorable. In the present case, the interval from the start of antiplatelet and immunosuppressive therapies until stenting was 19 days, and the CRP-negative finding may have aided in the prevention of perioperative complications such as re-occlusion related to stent thrombosis. Furthermore, strict medical management, including immunosuppressive therapy, reduced the disease activity; this may have been useful for the prevention of in-stent restenosis.
Conclusion
In a patient with bilateral CCA occlusion related to Takayasu arteritis, mechanical thrombectomy and left carotid artery stenting were performed to treat occlusion at the terminal portion of the left ICA, which newly developed, leading to recanalization of the left ICA area. Recanalization may be more readily achieved in patients with CCA occlusion related to Takayasu arteritis than in those with arteriosclerotic lesions, and this artery may be an approach route for distal cerebral blood vessel occlusion. After stenting, sufficient antiplatelet and immunosuppressive therapies may prevent restenosis, leading to a favorable outcome. Therefore, angioplasty for CCA occlusion and stenting on mechanical thrombectomy in the acute phase of this disease may be effective.
Disclosure Statement
The authors declare no conflict of interest.
References
- 1).Gornik HL, Creager MA: Aortitis. Circulation 2008; 117: 3039–3051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2).Isobe M: New diagnosis and treatment of Takayasu arteritis. J Jpn Soc Int Med 2014; 103: 2131–2136. (in Japanese) [DOI] [PubMed] [Google Scholar]
- 3).Duarte MM, Geraldes R, Sousa R, et al. : Stroke and transient ischemic attack in Takayasu’s arteritis: a systematic review and meta-analysis. J Stroke Cerebrovasc Dis 2016; 25: 781–791. [DOI] [PubMed] [Google Scholar]
- 4).Watanabe Y, Miyata T, Tanemoto K: Current clinical features of new patients with Takayasu arteritis observed from cross-country research in Japan: age and sex specificity. Circulation 2015; 132: 1701–1709. [DOI] [PubMed] [Google Scholar]
- 5).Ubagai R, Suyama T, Yamashita S, et al. : A case of left middle cerebral artery embolism due to Takayasu’s arteritis in the common carotid artery. Jpn J Stroke 2014; 36: 271–274. (in Japanese) [Google Scholar]
- 6).Ebata T, Uemura J, Yamazaki H, et al. : [A case of takayasu arteritis with acute bilateral occlusion of the internal carotid arteries]. Brain Nerve 2017; 69: 665–669. [DOI] [PubMed] [Google Scholar]
- 7).Topakian R, Strasak AM, Sonnberger M, et al. : Timing of stenting of symptomatic carotid stenosis is predictive of 30-day outcome. Eur J Neurol 2007; 14: 672–678. [DOI] [PubMed] [Google Scholar]
- 8).Jadhav AP, Zaidat OO, Liebeskind DS, et al. : Emergent management of tandem lesions in acute ischemic stroke. Stroke 2019; 50: 428–433. [DOI] [PubMed] [Google Scholar]
- 9).Horie N, Hayashi K, Morikawa M, et al. : Restenosis after endovascular PTA/stenting for supra-aortic branches in Takayasu aortitis: report of three cases and review of the literature. Acta Neurochir (Wien) 2011; 153: 1135–1139; discussion 1139. [DOI] [PubMed] [Google Scholar]
- 10).Kim YW, Kim DI, Park YJ, et al. : Surgical bypass vs endovascular treatment for patients with supra-aortic arterial occlusive disease due to Takayasu arteritis. J Vasc Surg 2012; 55: 693–700. [DOI] [PubMed] [Google Scholar]
- 11).Park MC, Lee SW, Park YB, et al. : Post-interventional immunosuppressive treatment and vascular restenosis in Takayasu’s arteritis. Rheumatology (Oxford) 2006; 45: 600–605. [DOI] [PubMed] [Google Scholar]
- 12).Hotchi M: Pathological studies on Takayasu arteritis. Heart Vessels Suppl 1992; 7: 11–17. [DOI] [PubMed] [Google Scholar]