Abstract
Objectives:
To evaluate the effect of a traditional “center-center” endpoint for distal tibia nailing in comparison to a lateral-of-center endpoint on fracture malalignment in a cadaver model.
Methods:
Nine matched pairs of human cadaveric lower-extremity specimens were utilized to model the effect of nail endpoint on fracture alignment in extra-articular distal tibia fractures. After simulation of the fracture through a standardized osteotomy, one member of each pair was fixed with an intramedullary nail utilizing a “center-center” endpoint, while a lateral-of-center endpoint was used for the other member of the pair. Specimens were stripped of soft tissue, and digital calipers were utilized to measure fracture translation and gap medially, laterally, anteriorly, and posteriorly. Coronal plane angulation at each fracture was measured on the final mortise image.
Results:
The average coronal angulation was 7.0 degrees of valgus (with a standard deviation [SD] of 4.1) in central-endpoint specimens versus 0.2 degrees of valgus (SD=1.5) in lateral-endpoint specimens (p<0.001). Lateral endpoint specimens also demonstrated significantly less fracture gap medially (mean 0.2-mm versus 3.1-mm for central endpoint specimens, p<0.001), anteriorly (0.1-mm vs. 1.3-mm, p=0.003), and posteriorly (0.3-mm vs. 2.2-mm, p=0.003). Lateral endpoint specimens also showed less lateral translation (0.6-mm vs. 1.6-mm, p=0.006).
Conclusions:
Lateral-of-center nail endpoints may help surgeons restore native alignment in extra-articular distal tibia fractures and avoid valgus malalignment.
Keywords: Tibia, intramedullary nail, distal tibia, Cadaver model
INTRODUCTION
Tradeoffs are inherent to the surgical treatment of extra-articular distal tibial fractures. Open reduction and plate fixation provides an opportunity to restore length, alignment, and rotation under direct visualization,1–11 while intramedullary nailing reduces “biologic insult” at the potential cost of increased malalignment.12–20 Recent randomized comparisons of nail versus plate have demonstrated coronal malalignment, typically valgus deformity, greater than 5 degrees, in 12–23% of those treated by intramedullary nailing versus 0–8.3% treated by plate fixation.14,19,21 Coronal plane malalignment of greater than 5 degrees has been associated with subtalar stiffness, knee pain, and ankle pain.22,23
Recent evidence has suggested that the use of a lateral nail endpoint may be an avenue for minimizing coronal malalignment in the intramedullary nailing of distal tibia fractures. Computed tomography-based studies have shown that the terminal position of a straight line passing down the tibial shaft is lateral to the center of the plafond, approximately 64% of the way across the plafond from the medial tibial cortex.24,25 In a retrospective clinical study, Triantafillou et al. examined the coronal alignment of 85 distal tibia fractures treated with intramedullary nailing: 2.9% of 34 fractures with nails ending lateral-of-center had coronal malalignment greater than 5 degrees versus 27.5% of 51 fractures with nails ending medial-of center.26 This finding that the lateral endpoint is associated with less malalignment has yet to be confirmed causally in a comparative anatomic model.
The purpose of this study was to evaluate the effect of a traditional “center-center” endpoint for distal tibia nailing in comparison to a lateral endpoint on fracture malalignment in a cadaver model. The researchers hypothesized that lateral endpoint specimens would exhibit less malalignment than central endpoint specimens.
MATERIALS AND METHODS
A power analysis was first performed utilizing figures provided in the retrospective series by Triantafillou et al.26 Based on figures from this paper including group means of 1.4° and 3.5°, an estimated standard deviation of 2.1°, and planning an alpha level of 0.05 and matched pairs analysis, the authors determined that nine matched pairs would be needed to achieve a power of 80%.
Nine matched pairs of human cadaveric lower-extremity specimens were obtained. All specimens were visually inspected to ensure the absence of prior fractures, previous arthroplasty, prior surgical fixation, or other obvious gross pathology. Each pair was randomized to designate the left or right leg as the lateral endpoint specimen. Consistent with the aforementioned CT-based analyses, the lateral endpoint was defined on a mortise fluoroscopic image as the junction between the middle third and lateral third of the talar dome (Figure 1). The sagittal endpoint was defined as the center of the plafond on a lateral image (Figure 2C), and this sagittal endpoint was used for all specimens.
FIGURE 1.
Nail endpoint locations. The central endpoint (C) was in the center of the talar dome on the mortise view. The lateral endpoint (L) was the border of the middle third and lateral third of the talar dome.
FIGURE 2.
Surgical technique. A hole was drilled in the plafond to establish the designated endpoint utilizing a cannulated drill in a retrograde fashion (A–D). The start point was obtained (E–F). A guidewire was placed through the hole in the plafond and reaming was performed (G). The guidewire was retracted, and a transverse osteotomy was measured and then cut 4-cm above the tibial plafond (H–I). The guidewire was then passed through the appropriate endpoint, and the tibial nail was inserted (J). The fracture was exposed and measurements were made (K–L).
The initial surgical technique deviated from the technique used clinically in that a path was created in the plafond at the designated endpoint to position the guidewire in a reproducible manner. A Kirschner wire was driven retrograde from the bottom of the foot through the appropriate endpoint in the plafond (Figure 2A–C). A 5.0-mm cannulated drill was then drilled over the guidewire 2 cm proximal to the physeal scar (Figure 2D).
After creating the designated path in the plafond, the standard clinical technique for intramedullary nailing was utilized. Through a suprapatellar approach, appropriate starting points just medial to the lateral tibial spine, and just anterior to the tibial crest, were obtained (Figure 2E–F). Following entry reamer placement, a long guidewire was passed down the canal and through the corresponding endpoint in the tibial plafond. Sequential reaming took place until adequate chatter was achieved, and all nails were reamed to 1.5-mm above the final nail size (Figure 2G). Following final reaming, the long guidewire was withdrawn. A vertical incision was made anteromedially on the tibia, and a transverse osteotomy was made 4 cm proximal to the joint in both the tibia and fibula (Figure 2H–I). The fracture was then reduced with closed manipulation, the long guidewire was again passed through the appropriate endpoint, and the intramedullary nail (AUTOBAHN® Tibial Nailing System, Globus Medical, Inc., Audubon, PA, USA) was passed down to the physeal scar (Figure 2J). For each pair of cadavers, the same-sized nail was used in both left and right tibiae. One distal interlock and one proximal interlock were placed. Final fluoroscopic images were obtained including an anteroposterior, mortise, and lateral image centered over the fracture site. Specimens were stripped of soft tissue, and digital calipers were utilized to measure fracture translation at four locations 90-degree angles to each other: medially, laterally, anteriorly, and posteriorly (Figure 2K–L). Fracture gap was also measured with digital calipers at the same four locations: medially, laterally, anteriorly, and posteriorly. Final mortise images were obtained of each fixed specimen (Figure 3). The coronal plane angulation at each fracture was measured on the final mortise image as the angle between a line drawn across the plafond and a line bisecting the tibial shaft just proximal to the osteotomy site minus 90 degrees. Negative angulations were valgus; positive angulations were varus. Final lateral radiographs were also obtained at the ankle, and the sagittal plane angulation was measured on the lateral image as the angle between the fracture surfaces of the distal and proximal fragments. Negative angulations were recurvatum; positive angulations were procurvatum.
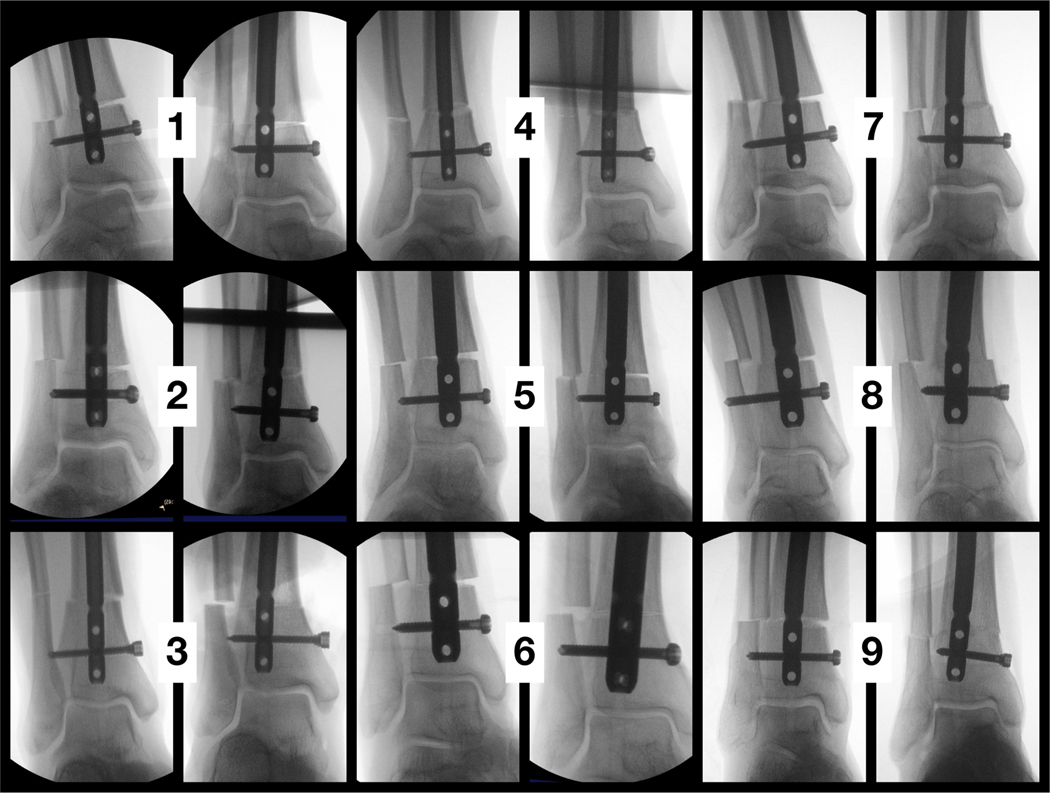
FIGURE 3.
Mortise images of fixed specimens. Each of nine pairs is shown, with the central endpoint specimen on the left and the lateral endpoint specimen on the right.
Statistical analysis of angulation, gapping, and translation measurements utilized a Student’s t-test for matched-pairs data. Angles were measured in ImageJ software (National Institutes of Health, Bethesda, MD, USA) and statistical analysis was performed in Excel (Microsoft Corporation, Redmond, WA, USA).
RESULTS
The average coronal angulation as measured in fixed specimens was 7.0 degrees valgus (with a standard deviation [SD] of 4.1) in central-endpoint specimens versus 0.2 degrees valgus (SD=1.5) in lateral-endpoint specimens (Table 1, Figure 4). This difference was statistically significant (p<0.001). Six out of nine central-endpoint specimens demonstrated greater than 5 degrees of malalignment versus zero out of nine lateral-endpoint specimens. Lateral endpoint specimens also demonstrated significantly less fracture gap on the medial side (mean 0.2-mm versus 3.1-mm for central endpoint specimens, p<0.001, Figure, Supplemental Digital Content 1,http://links.lww.com/JOT/B674), less anterior gap (0.1-mm vs. 1.3-mm, p=0.003), and less posterior gap (0.3-mm vs. 2.2-mm, p=0.003). Lateral endpoint specimens also showed less lateral translation (0.6-mm vs. 1.6-mm, p=0.006). The sagittal plane angulation, lateral gap, and medial, anterior, and posterior translations were statistically equivalent between lateral- and central-endpoint specimens (p>0.05).
Table 1:
Reduction parameters in fixed specimens
| Matched Pair | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Measure* | Endpoint | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Mean | SD | P-value |
| Coronal angulation | Central | −13.6 | −2.2 | −4.0 | −5.4 | −5.3 | −8.4 | −12.4 | −8.7 | −2.7 | −7.0 | 4.1 | 0.0003 |
| Lateral | −1.2 | 1.6 | 1.5 | 0.1 | −0.4 | 1.4 | −2.6 | −1.7 | −0.7 | −0.2 | 1.5 | ||
| Sagittal angulation | Central | −5.4 | 0.6 | −2.7 | −5.6 | 1.4 | −4.5 | −3.3 | 2.1 | −2.1 | −2.2 | 2.9 | 0.2670 |
| Lateral | 1.1 | −1.4 | 1.4 | −0.9 | −4.6 | 1.2 | −0.5 | −1.1 | 1.0 | −0.4 | 1.9 | ||
| Medial gap | Central | 4.2 | 2.6 | 2.4 | 1.8 | 4.4 | 2.8 | 4.3 | 2.0 | 3.4 | 3.1 | 1.0 | 0.0000 |
| Lateral | 0.3 | 0.0 | 0.0 | 0.0 | 1.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.2 | 0.3 | ||
| Lateral gap | Central | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.7 | 0.0 | 0.0 | 0.0 | 0.1 | 0.2 | 0.1799 |
| Lateral | 0.4 | 0.0 | 0.0 | 0.0 | 0.0 | 1.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.3 | ||
| Anterior gap | Central | 0.69 | 1.21 | 0.56 | 1.12 | 2.92 | 1.2 | 1.57 | 0.3 | 1.88 | 1.3 | 0.8 | 0.0033 |
| Lateral | 0.63 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.1 | 0.2 | ||
| Posterior gap | Central | 2.13 | 0.6 | 0.83 | 4.15 | 2.13 | 2.1 | 2.72 | 1.78 | 3.47 | 2.2 | 1.1 | 0.0025 |
| Lateral | 0.72 | 0 | 0 | 0 | 1.51 | 0.86 | 0 | 0 | 0 | 0.3 | 0.6 | ||
| Medial translation | Central | 1.4 | 1.0 | 1.8 | 0.4 | 0.3 | 0.9 | 2.8 | 1.1 | 2.6 | 1.4 | 0.9 | 0.1326 |
| Lateral | 0.5 | 0.0 | 0.7 | 1.1 | 0.0 | 0.4 | 1.1 | 2.5 | 0.5 | 0.7 | 0.7 | ||
| Lateral translation | Central | 1.4 | 0.4 | 2.1 | 0.7 | 1.2 | 1.1 | 2.0 | 2.5 | 2.8 | 1.6 | 0.8 | 0.0059 |
| Lateral | 0.3 | 0.0 | 0.9 | 1.1 | 0.0 | 0.8 | 0.9 | 0.8 | 0.5 | 0.6 | 0.4 | ||
| Anterior translation | Central | 0.83 | 1.59 | 0 | 0 | 1.51 | 0.54 | 1.65 | 0.88 | 2.15 | 1.0 | 0.8 | 0.6060 |
| Lateral | 0.53 | 3.12 | 0.5 | 1.7 | 0.11 | 1.46 | 2.24 | 1.57 | 0 | 1.2 | 1.0 | ||
| Posterior translation | Central | 1.07 | 0.65 | 1.55 | 0 | 1.59 | 1.39 | 2.13 | 1.54 | 3.28 | 1.5 | 0.9 | 0.5471 |
| Lateral | 0.56 | 2.27 | 0.21 | 1.13 | 0.31 | 1.62 | 2.3 | 1.99 | 0 | 1.2 | 0.9 | ||
Angulation was measured in degrees. Other measurements were made in millimeters.
FIGURE 4.
Scatter plot of valgus malalignment by nail endpoint. Negative values are varus malalignment. ***p<0.001.
DISCUSSION
This study demonstrated that a lateral endpoint minimizes valgus malalignment compared to the traditional central endpoint when treating distal tibia fractures with an intramedullary nail. Malalignment was a frequent problem with the central endpoint, as six of the nine central-endpoint specimens demonstrated greater than 5 degrees of malalignment compared to zero of the nine lateral-endpoint specimens. This simple technique therefore addresses an important clinical problem in distal tibia fracture treatment. In one randomized comparison of nail versus plate with a mean 22-month follow-up, 36% of patients with malalignment >5 degrees reported knee or ankle pain at follow-up versus 20% of patients with <5 degrees of malalignment, a difference that was statistically significant.22 In another series with mean 36-month follow-up, there was a significant association between overall malalignment of the lower limb (hip-knee-ankle angle outside the normal range of 6.25° of varus to 4.75° of valgus) and subtalar stiffness.23 Thus, a technique that minimizes malalignment, such as the lateral endpoint tested here, may help mitigate some negative clinical outcomes with intramedullary nailing of distal tibia fractures.
The terminal endpoint of tibial nails in the coronal plane has been suggested in surgical technique guides and by the AO organization as “center-center.” Recently, a slightly lateral endpoint has been suggested as the endpoint that provides the best coronal alignment for distal tibia fractures, challenging the traditional center-center endpoint. In particular, valgus malalignment of the distal tibia increased with progressively increased medial termination of the nail in a study by Brinkman et al.27 In a study by Schumaier et al, the distance from the medial cortex to the nail center as a ratio of medial-lateral tibial width was 0.63.24 Similarly, the results of the present study suggest improved coronal alignment with a lateral endpoint. Though this investigation is not the first to suggest a benefit with the lateral endpoint, to the best of the authors’ knowledge it is the first study that demonstrates this benefit using a controlled, randomized design. The current study builds on the existing literature in two important ways. First, the matched-pairs design and standardized technique, with randomization of specimens within pairs, isolated the effect of the nail endpoint on fracture alignment. Short of a randomized controlled clinical trial, which may not have equipoise given the current evidence, a matched-pairs cadaver model is likely the best achievable experimental model to test the present question. Second, while Triantafillou et al compared lateral-of-center to medial-of-center endpoints26, the traditional teaching has been to utilize a true central endpoint.1 Therefore, the present study, which had in the control group a central endpoint rather than a medial-of-center endpoint, shows more conclusively that the traditionally taught central endpoint may be more prone to fracture malalignment compared to a lateral endpoint. Furthermore, the impact of the central endpoint in this study represented a best-case scenario for the central endpoint, as all reaming took place in an intact tibia with the osteotomy performed just prior to nail placement.
The observed benefit of the lateral endpoint over the central endpoint demonstrates the importance of tibial anatomy, endpoint, and nail geometry as significant variables. One possible explanation for the improved alignment with a lateral endpoint is that the distal tibia metaphysis is asymmetric, and the lateral plafond is the true inferior extent of a straight line drawn down the tibial shaft. In one CT-based study, Schumaier et al. characterized the cross-sectional anatomy of the tibia with regard to the position of an intramedullary nail passing down the shaft.24 They performed post-nail insertion CT scans in 8 patients with mid-shaft tibial fractures, as well as 6 intact cadaveric legs, and showed that the nail center was, on average, 64% of the way across the tibial plafond from the medial side. Trompeter et al. corroborated this anatomic finding by showing in an industry database of 860 CT-derived tibia models that a line drawn through the midpoint of the diaphysis intersects the plafond a mean 4.4mm lateral of center in the coronal plane.25 These studies showed that the true anatomic axis of the tibia intersects the plafond lateral of center.
While the present study helps establish the role of the coronal plane endpoint on fracture alignment, the role of the sagittal plane endpoint remains unknown. Trompeter et al. showed that the mean anteroposterior offset of the tibial nail exit path was 0.6-mm anterior to the center of the plafond in the sagittal plane, although they acknowledged that this fact could not dictate the sagittal endpoint of every nail, as some manufacturers’ nails have different distal sagittal bends.25 Schumaier et al, in their analysis of post-nail CTs in 14 limbs, showed that the nail center in the sagittal plane was at a point 50% of the anterior-posterior width.24 Triantafillou et al found that nails ending posterior of center had slightly less malalignment than nails ending anterior of center.26 Notably, in the present study, the average sagittal plane angulation was 0.4 degrees and the average anterior and posterior fracture gaps were 0.2-mm and 0.6mm in lateral endpoint specimens, suggesting that a central endpoint in the sagittal plane is close to the ideal endpoint. The sagittal plane endpoint remained consistent in this study to isolate the effect of the coronal plane endpoint on coronal alignment.
One limitation of this study was that, in an effort to standardize the model, the fracture pattern and fixation technique differed somewhat from typical findings and techniques in clinical practice. A transverse osteotomy was made across the tibia and fibula at the same level, in contrast to some fractures seen clinically which may have obliquity and/or fibula fractures at a different level than the tibia fracture. The authors believed that the transverse osteotomy was an ideal model because it was reproducible, would not obviously bias the angulation in one direction or the other, and because the deforming forces, tibial anatomy, and nail geometry were otherwise analogous to the corresponding factors in the clinical setting. Furthermore, the guidewire placement differed from the clinical technique. In this study, a path was drilled retrograde in the plafond and the guidewire was inserted antegrade into this path. This would not be expected to undermine generalizability because the guidewire can readily be placed laterally in clinical practice utilizing a distal bend in the wire, as shown by Triantafillou et al.26 A third deviation from typical clinical findings and techniques occurred with the use of a single interlock screw rather than two interlock screws distal to the fracture. Because weight bearing and other load cycling did not occur in this model however, a single interlock was adequate to stabilize the construct and it is unlikely this deviation introduced any systematic bias.
An additional limitation was that the authors were unable to obtain full-length tibia films to measure angulation. The measurement of coronal plane angulation on a mortise ankle view required inferring the position of the tibial shaft by drawing a bisecting line through the visible segment of the shaft just above the osteotomy. While this may have deviated slightly from the “true” angulation between the plafond and shaft and introduced small inaccuracies in individual specimens, the matched-pairs design should mitigate much of the bias potentially introduced, as statistical inferences were derived from the differences between members of the matched pair rather than from the differences in angulations across all specimens.
Though valgus malalignment has historically been a challenge with intramedullary nail treatment of distal tibia fractures, this study demonstrated that targeting the nail laterally in the distal tibia nearly eliminates this problem. The authors recommend accomplishing this by placing a bend approximately 1–2cm proximal from the distal end of the ball-tipped guidewire, passing the guidewire to the distal tibial metaphysis, and then utilizing fluoroscopy to aim the bend laterally and advance the wire to the distal lateral physeal scar. Blocking screws or wires may also be utilized to help target the guidewire. This technique “pearl” may help surgeons restore alignment in extra-articular distal tibia fractures, avoiding the potential drawbacks of plate fixation without sacrificing reduction quality. Tibial nail technique guides should potentially be revised to establish the lateral endpoint as the “correct” endpoint for nailing distal tibia fractures.
Supplementary Material
Footnotes
The authors report no conflicts of interest related to this work.
REFERENCES
- 1.Bilat C, Leutenegger A, Ruedi T. Osteosynthesis of 245 tibial shaft fractures: early and late complications. Injury. 2004;35:349–358. [DOI] [PubMed] [Google Scholar]
- 2.Littenberg B, Weinstein LP, McCarren M, et al. Closed fractures of the tibial shaft. A meta-analysis of three methods of treatment. J Bone Joint Surg. 1998;80A:174–183. [DOI] [PubMed] [Google Scholar]
- 3.Schmidt AH, Finkmeier CG, Tornetta P III. Treatment of closed tibial fractures. J Bone Joint Surg. 2003;85A:352–368. [PubMed] [Google Scholar]
- 4.Siebenrock KA, Schillig B, Jakob RP. Treatment of complex tibial shaft fractures. Arguments for early secondary intramedullary nailing. Clin Orthop. 1993;290:269–274. [PubMed] [Google Scholar]
- 5.Teeny SM, Wiss DA. Open reduction and internal fixation of tibial plafond fractures. Variables contributing to poor results and complications. Clin Orthop Relat Res. 1993;108–117. [PubMed] [Google Scholar]
- 6.Collinge C, Sanders R, DiPasquale T. Treatment of complex tibial shaft fractures. Arguments for early secondary intramedullary nailing. Clin Orthop. 2000;375:69–77. [Google Scholar]
- 7.Helfet DL, Shonnard PY, Levine D, et al. Minimally invasive plate osteosynthesis of distal fractures of the tibia. Injury. 1997;28:A42–A47. [DOI] [PubMed] [Google Scholar]
- 8.Oh CW, Kyung HS, Park IH, et al. Distal tibia metaphyseal fractures treated by percutaneous plate osteosynthesis. Clin Orthop. 2003;408:286–291. [DOI] [PubMed] [Google Scholar]
- 9.Redfern DJ, Syed SU, Davies SJ, Fractures of the distal tibial minimally invasive plate osteosynthesis. Injury. 2004;35:615–620. [DOI] [PubMed] [Google Scholar]
- 10.Sathiyakumar V, Thakore RV, Ihejirika RC, et al. Distal tibia fractures and medial plating: factors influencing re-operation. Int Orthop. 2014;38:1483–1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Collinge C, Protzman R. Outcomes of minimally invasive plate osteosynthesis for metaphyseal distal tibia fractures. J Orthop Trauma. 2010;24:24–29. [DOI] [PubMed] [Google Scholar]
- 12.Avilucea FR, Triantafillou K, Whiting PS, et al. Suprapatellar intramedullary nail technique lowers rate of malalignment of distal tibia fractures. J Orthop Trauma. 2016;30:557–560. [DOI] [PubMed] [Google Scholar]
- 13.Guo JJ, Tang N, Yang HL, et al. A prospective, randomized trial comparing closed intramedullary nailing with percutaneous plating in the treatment of distal metaphyseal fractures of the tibia. J Bone Joint Surg Br. 2010;92:984–988. [DOI] [PubMed] [Google Scholar]
- 14.Im GI, Tae SK. Distal metaphyseal fractures of the tibia: a prospective randomized trial of closed reduction and intramedullary nail versus open reduction and plate and screws fixation. J Trauma. 2005;59:1219–1223. [DOI] [PubMed] [Google Scholar]
- 15.Janssen KW, Biert J, vanKampen A. Treatment of distal tibia fractures: plate versus nail. A retrospective outcome analysis of matched pairs of patients. Int Orthop. 2007;31:709–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li Y, Jiang X, Guo Q, et al. Treatment of distal tibial shaft fractures by three different surgical methods: a randomized, prospective study. Int Orthop. 2014;38:1261–1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mauffrey C, McGuinness K, Parsons N, et al. A randomized pilot traila of “locking plate” fixation versus intramedullary nailing for extra-articular fractures of the distal tibia. J Bone Joint Surg Br. 2012;94:704–708. [DOI] [PubMed] [Google Scholar]
- 18.Vallier HA, Le TT, Bedi A. Radiographic and clinical comparisons of distal tibia shaft fractures (4 to 11 cm proximal to the plafond): plating versus intramedullary nailing. J Orthop Trauma. 2008;22:307–311. [DOI] [PubMed] [Google Scholar]
- 19.Vallier HA, Cureton BA, Patterson BM. Randomized, prospective comparison of plate versus intramedullary nailing fixation for distal tibia shaft fractures. J Orthop Trauma. 2011;25:736–741. [DOI] [PubMed] [Google Scholar]
- 20.Yang SW, Tzeng HM, Chou YJ, et al. Treatment of distal tibial metaphyseal fractures: plating versus shortened intramedullary nailing. Injury. 2006;37:531–535. [DOI] [PubMed] [Google Scholar]
- 21.Casstevens C, Le T, Archdeacon MT, et al. Management of extra-articular fractures of the distal tibia: intramedullary nailing versus plate fixation. J Am Acad Orthop Surg. 2012;20:675–683. [DOI] [PubMed] [Google Scholar]
- 22.Vallier HA, Cureton BA, Patterson BM. Factors influencing functional outcomes after distal tibial shaft fractures. J Orthop Trauma. 2012;26:178–183. [DOI] [PubMed] [Google Scholar]
- 23.Milner SA, Davis TRC, Muir KR, et al. Long-term outcome after tibial shaft fracture: is malunion important? J Bone Joint Surg Am. 2002;84:971–980. [DOI] [PubMed] [Google Scholar]
- 24.Schumaier AP, Avilucea FR, Southam BR, et al. Terminal position of a tibial intramedullary nail: a computed tomography (CT) based study. Eur J Trauma Emerg Surg. 2020;46(5):1077–1083. [DOI] [PubMed] [Google Scholar]
- 25.Trompeter A, Williamson M, Bates P, et al. Defining the ideal “nail exit path” of a tibial intramedullary nail – a computed tomography analysis of 860 tibiae. J Orthop Trauma. 2021;Mar 2. [DOI] [PubMed] [Google Scholar]
- 26.Triantafillou K, Barcak E, Villarreal A, et al. Proper distal placement of tibial nail improves rate of malalignment for distal tibia fractures. J Orthop Trauma. 2017;31:e407–e411. [DOI] [PubMed] [Google Scholar]
- 27.Brinkmann E, DiSilvio F, Tripp M, et al. Distal nail target and alignment of distal tibia fractures. J Orthop Trauma 2019;33(3):137–142. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.