Abstract
Thoracic outlet syndrome (TOS) is a constellation of symptoms that occur due to the compression of neurovascular structures traversing the thoracic outlet. TOS manifests in 3 distinct forms: neurogenic, venous, and arterial. Among these, arterial TOS is the rarest. A 32-year-old man presenting with severe right arm pain was referred for CT angiography. The imaging revealed bilateral cervical ribs, with the right side showing more pronounced development and fusion with the first thoracic rib. At the fusion site of the right cervical rib and the first thoracic rib, a pseudoaneurysm of the right subclavian artery was detected. Additionally, there was evidence of acute thromboembolism in the right brachial artery at the mid-humerus. Arterial thoracic outlet syndrome is a rare form of TOS that can have detrimental consequences due to associated complications. Cross-sectional imaging, such as CT scans and MRI, is the preferred method for diagnosing TOS and identifying its specific form. Physicians are expected to be familiar with the various forms of TOS, the lesions mimicking TOS, and the imaging tools utilized for diagnosis.
Keywords: TOS, Arterial, Case report
Introduction
Thoracic outlet syndrome refers to a group of disorders caused by the compression of neurovascular structures passing through the thoracic outlet [1], [2], [3]. The brachial plexus, subclavian artery, and subclavian vein pass through thoracic outlet [1], and when these structures are compressed by any entity, they can cause symptoms in the upper extremity [4]. The thoracic outlet is formed by the bones of the sternum anteriorly, the first ribs laterally, and the vertebrae posteriorly [1], and is supplemented by the clavicle, forming its superior margin [1]. Thoracic outlet syndrome is categorized into 3 types based on its etiology: neurogenic, venous, and arterial forms [1,3,4]. The rarest form of thoracic outlet syndrome is the arterial type that accounts for 1%-2% of TOS cases [1]. Cervical ribs are the most common cause of thoracic outlet syndrome, particularly the arterial variety, which is observed in 85% of patients [1]. Prior to a thromboembolic episode, patients with arterial TOS show no symptoms. Poststenotic dilatation can lead to the development of thrombus and pseudoaneurysm, which may cause anterograde or retrograde thromboembolism. The development of thrombus and pseudoaneurysm as a result of poststenotic dilatation causes thromboembolism anterograde or retrograde [3]. Patients with the arterial type of thoracic outlet syndrome commonly present with symptoms of limb ischemia, and arterial stenosis [1].
Case presentation
A 32-year-old male complaining of a persistent right arm pain was referred to the radiology department for CT angiography of the right upper extremity. The physical examination revealed no noteworthy abnormal findings. There was no relevant antecedent medical, familial, or psychosocial history. CT angiography revealed bilateral cervical ribs, more prominent on the right side, which fused with the first thoracic rib (Figs. 1A-D). Additionally, a pseudoaneurysm of the subclavian artery was observed on the right side at the fusion site of the cervical and first thoracic ribs (Figs. 2A-C). Furthermore, there was a longitudinal luminal central filling defect observed within the right brachial artery, consistent with acute thromboembolism (Figs. 3A-C). The imaging features were characteristic of arterial thoracic outlet syndrome (Figs. 4A-D). No evidence of luminal defects in the visualized veins was observed. There was no evidence of tumors or imaging findings of vasculitis to mimic the TOS. However, the patient was lost to follow-up after receiving the imaging diagnosis.
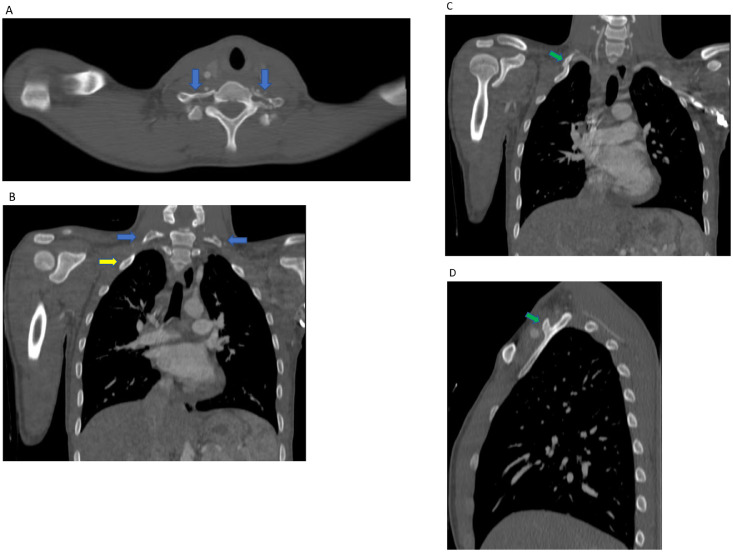
Fig. 1.
(A-D) Selected axial, coronal, and sagittal CT images of a bone window at the upper thorax demonstrating bilateral cervical ribs (blue arrows), and the first thoracic rib (yellow arrow). Note the fusion of the cervical rib with the first thoracic rib on the right side (green arrows).
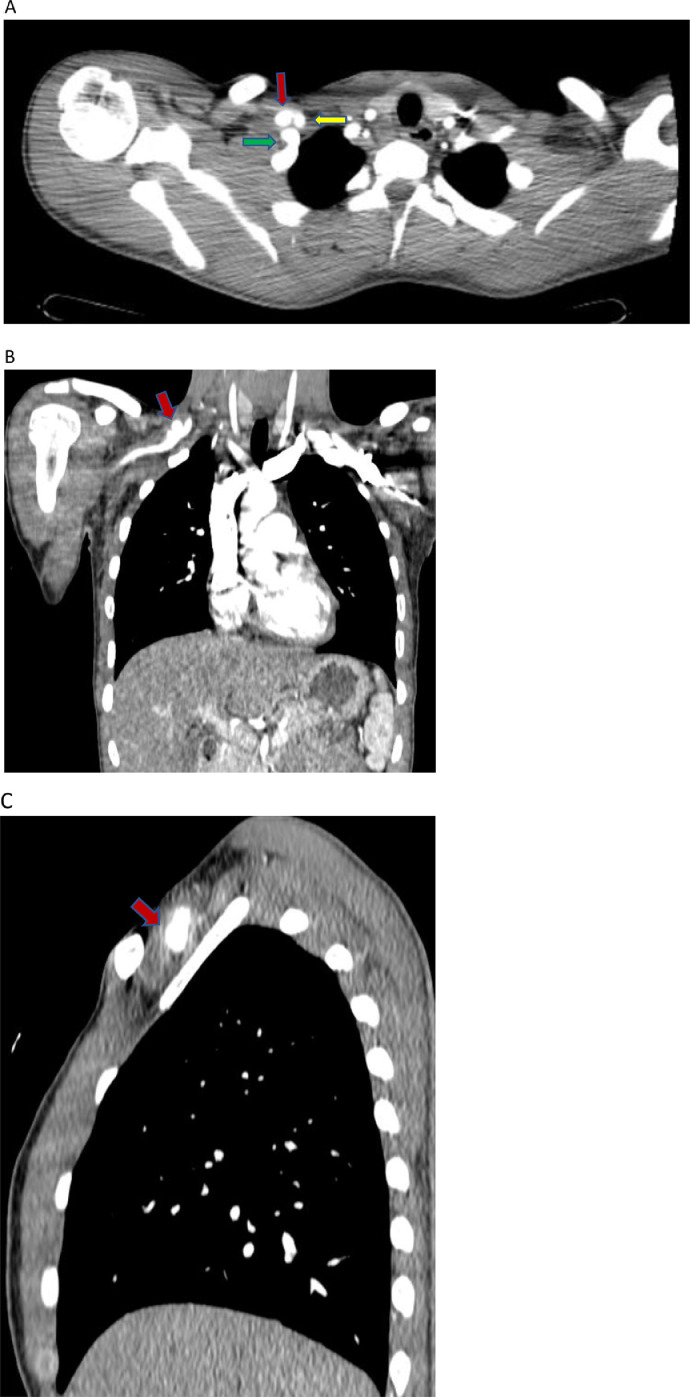
Fig. 2.
(A-C) Contrast-enhanced selected axial, coronal, and sagittal CT images at the level of upper thorax, demonstrating a fusion of the cervical rib and first thoracic rib (green arrow), upper aspect of the pseudoaneurysm (red arrow), and subclavian artery proximal to pseudoaneurysm (yellow arrow), all on the right side.
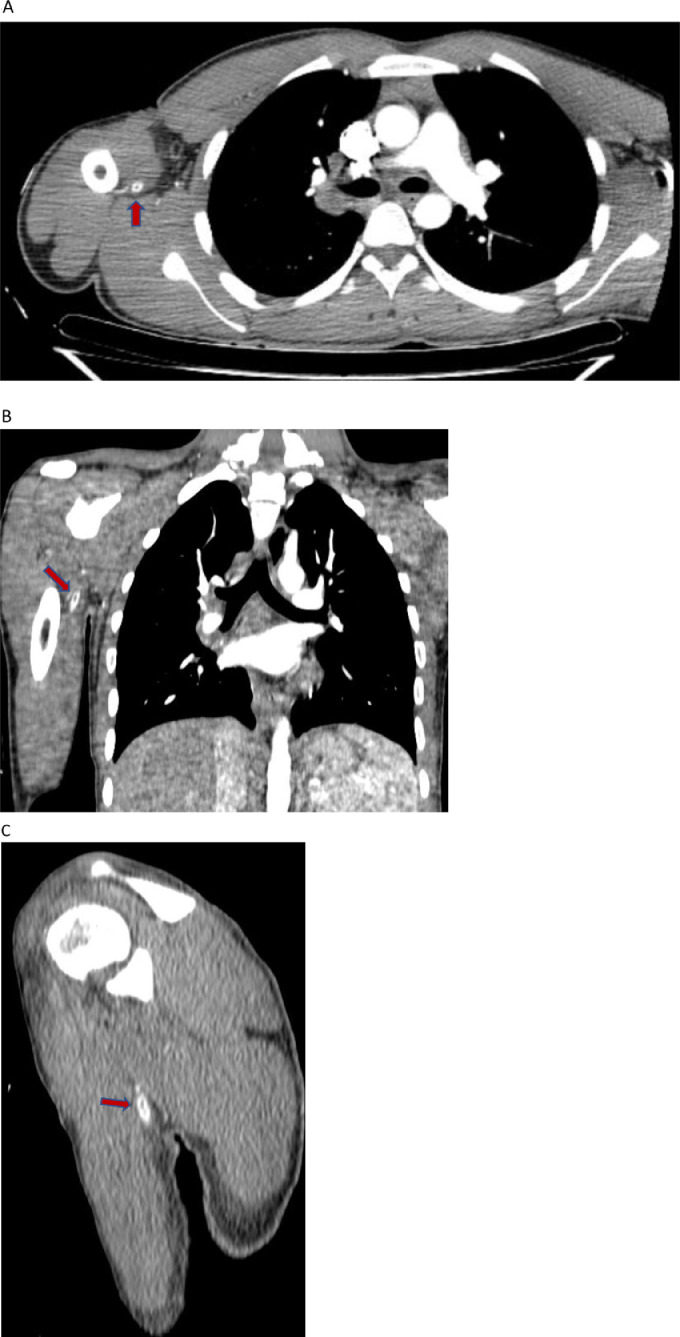
Fig. 3.
(A-C) Selected contrast-enhanced axial, coronal, and sagittal CT images with a central filling defect in the right brachial artery (red arrow), demonstrating acute thromboembolism.
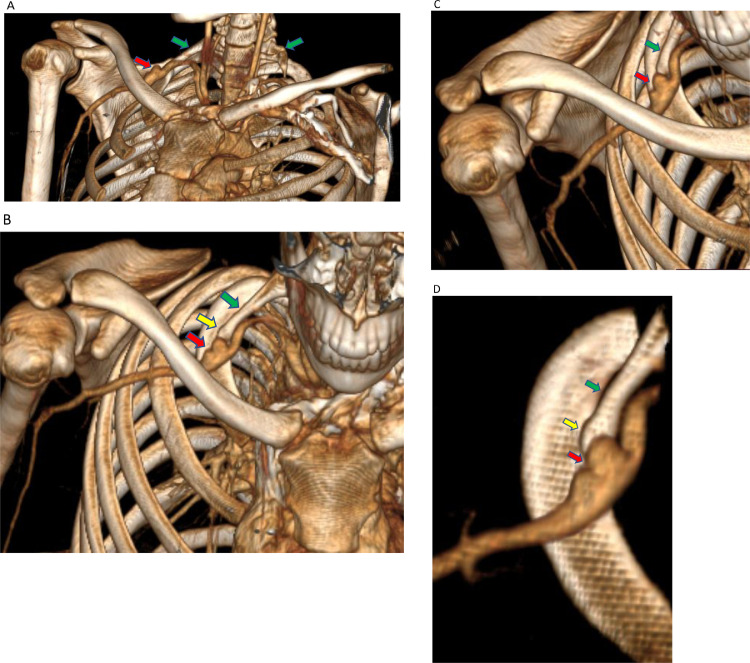
Fig. 4.
(A-D) 3D reconstructed images demonstrate cervical ribs on either side (green arrows), a fusion of the right cervical rib with the first thoracic rib (yellow arrow), and the formation of pseudoaneurysm on the right side (red arrow).
Discussion
The thoracic outlet has 3 spaces: the scalene triangle, costoclavicular space, and subcoracoid pectoralis minor space. Abduction of the ipsilateral arm can narrow these spaces [5]. As a result, TOS is defined as the compression of neurovascular structures due to anatomic predisposition and a precipitating factor [4]. Thoracic outlet syndrome can be congenital or acquired [1]. There are 3 types of thoracic outlet syndrome; [3] neurogenic
TOS is caused by the compression of brachial plexus at the scalene triangle and/or retro pectoral space; venous TOS is caused by the compression at the anterior costoclavicular junction; and arterial TOS is caused by the compression of the subclavian artery by a cervical rib [2].
The estimated occurrence of neurogenic TOS is 3 per 100,000 individuals, while venous TOS has an estimated rate of 1 per 100,000 [6]. Neurogenic thoracic outlet syndrome (90%) is the most common type, followed by venous TOS [5]. Arterial thoracic outlet syndrome is the least common type of TOS, with an occurrence rate of only 1%-2% among patients [1,4,5]. According to Illig et al. [2], the estimated prevalence of arterial TOS is around 2%. Although females are more likely to develop neurogenic TOS, there is no gender preference in arterial TOS [1]. Common causes of TOS include cervical ribs, muscle hypertrophy, trauma, and repetitive motions [1]. Patients with arterial TOS almost always have a cervical rib, a first rib anomaly, or a first rib or clavicle fracture [4,5]. The compression of the subclavian artery may result in the formation of an aneurysm, either prestenotic or poststenotic. Continuous compression of the subclavian artery can damage the intima and result in the formation of atheromas, which can serve as the basis for anterograde or retrograde thromboembolic events [1]. In fact, there are 2 components of damage: one at the site of direct impact on the subclavian artery and the other caused by a thromboembolic event distally [4,5].
The classic symptoms of arterial TOS, such as weakness, pain, and cold limb, are caused by distal ischemia [4]. A pulsatile mass in the supraclavicular space may be present in asymptomatic patients with arterial TOS due to aneurysm formation [4]. Clinical manifestations of arterial TOS include absent or diminished pulses, abnormal skin color changes, digit ischemia, and palpable supraclavicular pulse [3]. Cerebrovascular accident can also occur as a result of retrograde embolism, but it is uncommon [4].
Chest radiography is frequently used to rule out bony anomalies [4]. Both CT scans and MRI are considered the modalities of choice for diagnosing thoracic outlet syndrome [5,7]. MRA is superior to CT scans due to its superior tissue contrast and ability to evaluate veins and nerves [7]. The goal of imaging modalities is to identify the underlying cause of TOS, which can be anatomical or pathological. Vascular TOS is diagnosed when the subclavian artery narrows by more than 30% or the subclavian vein narrows by more than 50% [7]. It is crucial to administer contrast material on the opposite side to prevent streak artifacts [4,7]. In arterial TOS, the imaging findings include aneurysm or pseudoaneurysm formation of axillo-subclavian artery, arterial thrombosis, and focal fixed stenosis of subclavian artery on the side of compression [4,5]. In neurogenic TOS, MRI would reveal edema of the brachial plexus with loss of peripheral fat. To investigate for concurrent abnormalities, chest radiography [5] or CT scan may be added to MRI [4]. In venous TOS, the imaging findings include the detection of axillo-subcalvian thrombosis, venous stenosis, or the formation of collateral vessels [4].
Relying solely on the narrowed size of the arteries or veins in the absence of clinical symptoms can lead to misdiagnosis and overtreatment [4]. Asymptomatic patients would also demonstrate narrowing of the subclavian artery or vein, emphasizing the importance of correlating clinical and imaging findings in the diagnosis of TOS [7]. TOS is considered a diagnosis of exclusion. Other pathologic entities to rule out are neurogenic tumors, superior sulcus tumor, lipoma, Takayasu arteritis, and atherosclerosis, which can cause compression of neurovascular structures and produce symptoms similar to TOS [4].
Conclusion
TOS is classified into 3 types, the most common of which is neurogenic TOS, followed by venous TOS. Arterial TOS is the rarest form, and it is most commonly associated with the presence of a cervical rib. Cross-sectional imaging studies are important diagnostic tools for determining the type of TOS and ruling out other conditions with similar symptoms to prevent lethal complications. Physicians need to be aware of the different types of TOS, mimicry lesions, and imaging tools for diagnosis.
Ethics approval and consent to participate
The manuscript has got ethical review exemption from the Ethical Review Committee (ERC) of the authors’ institution (Wyagal Radiology Center - {WRC}) as case reports are exempted from review according to the institutional ethical review committee's policy. Written consent is obtained from the participants for publishing the case.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study (as this is a case report).
Authors’ contributions
All of the authors have participated sufficiently in the submission and take public responsibility for its content. NF: writing and editing the manuscript and selecting images, as well as corresponding with the journal. FF and YB: selecting the case and revising the manuscript. All of the authors have read and approved the final manuscript.
Patient consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
Footnotes
Acknowledgments: Not applicable.
Competing Interests: The authors declare that they have no competing interests.
References
- 1.Aghamiri SH, Assarzadegan F, Ghaffari M, Khorasani NM, Lima BS, Sepehrirad A, et al. Recurrent middle cerebral artery stroke caused by. Radiol Case Rep. 2022;17(5):1665–1669. doi: 10.1016/j.radcr.2022.02.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Illig KA, Rodriguez-zoppi E, Bland T, Muftah M, Jospitre E, Carolina S. The incidence of thoracic outlet syndrome. Ann Vasc Surg. 2020:1–10. doi: 10.1016/j.avsg.2020.07.029. [DOI] [PubMed] [Google Scholar]
- 3.Todnem N, Kilianski J, Reddy V, Rahimi S. Arteriogenic thoracic outlet syndrome presenting as cervical radiculopathy. Eur J Vasc Endovasc Surg. 2019;53(1):79–81. doi: 10.1177/1538574418794081. [DOI] [PubMed] [Google Scholar]
- 4.Raptis CA, Sridhar S, Thompson RW, Fowler KJ, Bhalla S. Imaging of the patient with thoracic outlet syndrome. Radiographics. 2016;36(4):984–1000. doi: 10.1148/rg.2016150221. [DOI] [PubMed] [Google Scholar]
- 5.Poyyamoli S, Swamiappan E, Gandhi J, Ranasingh RK, Cherian MP, Mehta P. Non-aortic vascular findings on chest CT angiogram: including arch vessels and bronchial arteries. Cardiovasc Diagn Ther. 2019;9(Suppl 1):S59–S73. doi: 10.21037/cdt.2018.09.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Illig KA, Rodriguez-Zoppi E. How common is thoracic outlet syndrome? Thorac Surg Clin. 2021;31(1):11–17. doi: 10.1016/j.thorsurg.2020.09.001. [DOI] [PubMed] [Google Scholar]
- 7.Ghouri MA, Gupta N, Bhat AP, Thimmappa ND, Saboo SS, Khandelwal A, et al. CT and MR imaging of the upper extremity vasculature: pearls, pitfalls, and challenges. Cardiovasc Diagn Ther. 2019;9(Suppl 1):S152–S173. doi: 10.21037/cdt.2018.09.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study (as this is a case report).