Abstract
Background:
Hysteroscopy is the gold standard for evaluating intrauterine pathology. The majority of physicians currently perform hysteroscopy in the operating room. Lack of training has been cited as a barrier to performing office hysteroscopy; however, resident training in office hysteroscopy has not yet been evaluated.
Methods:
A prospective cross-sectional survey was performed. A validated 17 question survey tool was sent to 297 program directors of Accreditation Council for Graduate Medical Education accredited obstetrics and gynecology residency programs for distribution to their residents. The survey utilized a Likert scale to assess resident interest in learning office hysteroscopy, satisfaction in training, and perceived self-efficacy to perform office hysteroscopy independently upon graduation.
Results:
Two hundred and ninety-three obstetrics and gynecology residents responded. Of the respondents, 26.3% reported receiving training in office hysteroscopy. There was no statistically significant difference in training among postgraduate years or program regions. A greater proportion of male residents received training when compared to female residents (42.9% vs. 24.2%, p = 0.019). Ninety-four percent of residents reported interest in learning office hysteroscopy. Satisfaction with hysteroscopy training in the operating room versus the office was 91.1% vs. 11.3% respectively. Of the fourth-year residents, 17.4% felt they could perform office hysteroscopy independently upon graduation and 14.5% reported feeling comfortable performing the procedure.
Conclusions:
Residency training in office hysteroscopy is lacking and residents are unprepared to perform the procedure after graduation. Enhanced residency training in office hysteroscopy would likely improve resident comfort and ability to perform office hysteroscopy in practice.
Keywords: Curriculum, Education, Office Hysteroscopy, Residency
INTRODUCTION
Residency training is pivotal in preparing physicians to practice in their designated specialties and must be continuously adapted to ensure trainees develop appropriate competency. When surveyed on preparedness post residency, 28.2% of obstetrics and gynecology (OBGYN) graduates reported a lack of confidence in their surgical skills.1 Similarly, a survey of fellowship program directors found that residents’ surgical skills were deficient, and they were not adequately prepared for fellowship training.2 This further highlights the importance of optimizing resident surgical training. With patient care migrating from an inpatient to outpatient setting, surgical training must similarly adapt.3
Hysteroscopic procedures are a standard method for the evaluation and treatment of pathology within the uterine cavity. Hysteroscopy has proven to be both more sensitive and more specific for identifying uterine pathology when compared to alternative diagnostic tools and is essential in gynecologic care.4,5 Although traditionally performed in the operating room (OR), technological advancements have allowed hysteroscopy to be performed safely and effectively in an office setting, resulting in easier scheduling, shorter recovery times, decreased days off work, and higher patient satisfaction.6–8 Pain with the procedure is minimal and analgesia is often not required.9 Additionally, office hysteroscopy is cost-effective as the need for a more costly OR hysteroscopy is often eliminated.10,11
Despite its many benefits, it’s estimated that only 15% of providers perform office hysteroscopy.4 In addition to low reimbursement and high equipment cost, lack of training was one of the most cited reasons for not performing the procedure.12 In 2017, the Centers for Medicare and Medicaid Services increased relative value units and reimbursement for office hysteroscopic procedures and decreased reimbursement for procedures performed in a hospital or ambulatory outpatient setting.8 While this change eliminates the obstacle of low reimbursement, other barriers to performing office hysteroscopy, such as training, are still present.
The primary aim of this study was to determine what proportion of residents in Accreditation Council for Graduate Medical Education (ACGME) accredited OBGYN programs receive hysteroscopy training in an office setting. Secondary objectives were to assess residents’ interests in learning office hysteroscopy, their overall satisfaction with their training, and their perceived self-efficacy to perform office hysteroscopy independently upon graduation. We hypothesized that residency training in office hysteroscopy is lacking; leaving residents unprepared to perform the procedure upon graduation.
METHODS
This study was reviewed by the local institutional review board and deemed exempt under 45 CFR § 46.104(d)(2). The study design was created following the Checklist for Reporting Results of Internet E-surveys (CHERRIES) guidelines.13 A novel 17 question survey tool was created for the purpose of this study. The survey was validated utilizing face and construct validation by two experienced gynecology attending physicians.14 The questions were developed to address issues that have been previously cited as barriers to performing office hysteroscopy.4,12 Our study focused on the setting in which residents received hysteroscopy training. We did not differentiate between the other domains of hysteroscopic procedures such as pain management, model of care, type of procedure, or approach of procedure.15 We defined office hysteroscopy as any hysteroscopic procedure performed in an outpatient physician office in the absence of parenteral sedation, regional anesthesia, or general anesthesia.15 Conversely, OR hysteroscopies were those performed in an operating room where general anesthesia could be administered.15 A Likert scale was used to assess resident interest in learning office hysteroscopy, satisfaction in training, and perceived self-efficacy. Self-efficacy is the belief in one’s capability to accomplish a task.16 In contrast to traditional confidence measures, the social cognitive theory of self-efficacy is based on the notion that individual actions are situation-specific and influenced by the action of others.17 Prior studies have demonstrated self-efficacy as a valid and more precise measure of confidence.17 Basic demographic information was also collected. Survey data were collected using a password protected, cloud-based survey software (SurveyMonkey Inc., San Mateo, California, USA). The survey was anonymous and no personal information was collected. IP addresses were tracked to ensure unique responses to each survey and cookies were enabled to prevent multiple responses. The deidentified dataset was kept on password protected computers. The survey was voluntary. Residents were not compensated for their participation.
All OBGYN residents enrolled in an accredited ACGME residency program were eligible to participate. The only exclusion criteria were OBGYN residents not enrolled in an accredited ACGME program. This was a closed survey. Only individuals with the unique survey link were able to participate. Programs were contacted three times over the course of three months to participate (November 1, 2019 – January 31, 2020). The programs were substratified into Northeast, South, Midwest, West, and Canada based on U.S. census definitions for regional comparison.18 An email with an invitation link to participate was sent to the program coordinators and program directors of 298 programs to be disseminated to residents in their respective programs. Within the email, residents were informed of the purpose and of the study. Consent was indicated when a participant utilized the provided link to complete the survey.
Each survey was identical with some adaptive questioning based on the respondent’s response. Survey questions were not randomized. All survey questions included a “nonresponse” field to minimize missing data. All 17 survey questions were displayed on one page. Participants were given the option to withdraw at the end of the survey if they desired. Responses could not be changed once submitted. However, participants could review their answers prior to submission. Surveys with no missing data were classified as complete. Surveys with skipped questions were considered partially completed. Skipped questions were treated as missing data in analysis. No participants were removed from the study for completing the survey too quickly. A response rate of 5% was expected given the survey study design, lack of incentive, lack of face-to-face contact with participants, and indirect invitations through program coordinators and program directors. Therefore, our goal was a minimum of 261 responses based on the 5,226 reported active OBGYN residents.19
Data were analyzed using Stata version 12.1 (StataCorp, College Station, Texas) statistical software. Determination of normal data distribution was conducted by assessing skewness and kurtosis, the Shapiro-Wilk normality test, and evaluation of plotted histograms. After determination of data distribution, all normally distributed continuous variables were evaluated with a Student t-test, with correction if necessary for unequal variances. Nonnormally distributed variables were evaluated using a Mann-Whitney test. Categorical variables were evaluated with the χ2 test or Fisher exact test, as appropriate. Statistical significance was predetermined at P ≤ 0.05.
RESULTS
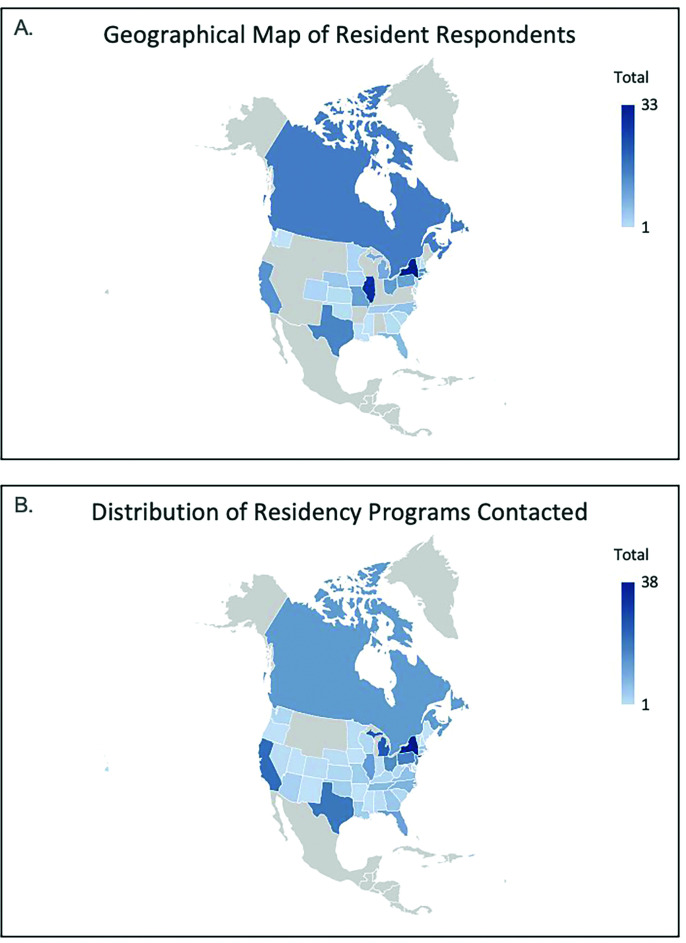
A total of 293 residents responded to the survey, with a median time to completion of 1 minute and 49 seconds. This response time did not impact the accuracy of the responses as the completion rate was 100%. The residents sampled represented 29 states and Canada (Figure 1). Resident demographics are summarized in Table 1. Residents were represented similarly in all postgraduate year (PGY) levels: 63 PGY1 (21.5%), 75 PGY2 (25.6%), 84 PGY3 (28.7%), 69 PGY4 (23.6%), 2 unspecified (0.7%). The study population included 257 females (87.7%) compared to 35 males (11.9%).
Figure 1.
A) Map of geographic locations of sampled residents’ residency programs. B) Map of accredited obstetrics and gynecology residency programs that were contacted to participate in the study.
Table 1.
Resident Demographics
| Demographic Characteristics | n (%), N = 293 |
|---|---|
| Year in Residency | |
| PGY1 | 63 (21.5%) |
| PGY2 | 75 (25.6%) |
| PGY3 | 84 (28.7%) |
| PGY4 | 69 (23.6%) |
| Not Specified | 2 (0.7%) |
| Sex | |
| Male | 35 (11.9%) |
| Female | 257 (87.7%) |
| Not Specified | 1 (0.3%) |
| Demographic Region | |
| Northeast | 77 (26.3%) |
| Midwest | 74 (25.3%) |
| West | 17 (5.8%) |
| South | 43 (14.7%) |
| Canada | 16 (5.5%) |
| Not Specified | 66 (22.5%) |
| Post Residency Plans | |
| General Obstetrics and Gynecology | 150 (51.4%) |
| Fellowship | 101 (34.5%) |
| Maternal Fetal Medicine | 26 (8.9%) |
| Minimally Invasive Gynecologic Surgery | 21 (7.2%) |
| Gynecologic Oncology | 20 (6.8%) |
| Urogynecology | 13 (4.5%) |
| Family Planning | 9 (3.1%) |
| Reproductive Endocrinology and Infertility | 9 (3.1%) |
| Pediatric & Adolescent Gynecology | 2 (0.7%) |
| Not Specified | 1 (0.3%) |
| Unsure | 41 (14.0%) |
| Not Specified | 1 (0.3%) |
Abbreviation: PGY, postgraduate year.
Of those responding, 37.2% of residents stated that office hysteroscopy was available at their institution, 49.5% of residents stated office hysteroscopy was not available at their institution and 13.3% of residents were unsure. Further, 26.3% (77/293; 95% confidence interval [CI], 21.3% – 31.7%) of residents reported receiving training in office hysteroscopy whereas 73.4% (215/293; 95% CI, 67.3% – 78.4%) reported that they did not. There was no statistically significant difference in training among postgraduate years or program regions. When stratified by sex, a higher proportion of male residents received office hysteroscopy training than their female peers (42.9% vs. 24.2% respectively, p = 0.019). The cited barriers to receiving training included: equipment not available (58.0%), attending physicians not trained to perform (17.7%), appropriate patient not encountered (16.5%), and attending physicians not willing to teach (4.5%). Analysis of the open-ended responses from the 31.3% of respondents who reported “other” barriers illustrated several themes including: lack of nursing, lack of anesthesia, training reserved for upper-level residents (i.e., PGY3 and PGY4 residents), and office hysteroscopy only offered in private clinics but not resident clinics. In the open-ended comments, many residents were also unsure why the procedure was not available.
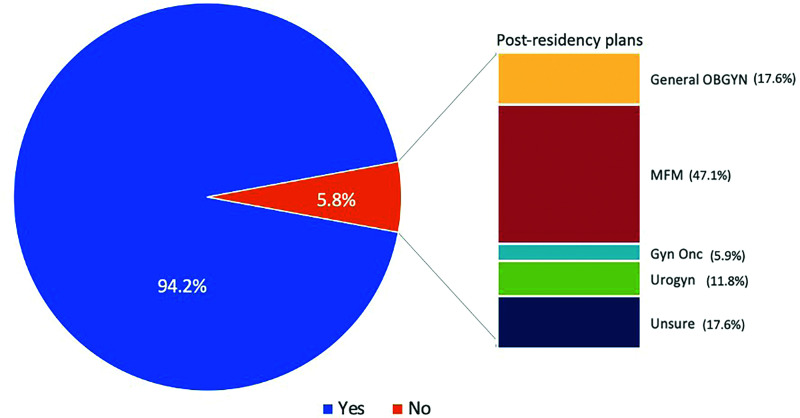
In response to interest in learning office hysteroscopy, majority of residents (93.9%; 275/293 95% CI, 90.5% – 96.3%) expressed interest in learning office hysteroscopy. PGY4 residents (52.9%, p < 0.05) and residents interested in maternal-fetal medicine (MFM) (47.1%, p < 0.05) comprised majority of the negative responses which was statistically significant (Figure 2). When assessing for collinearity, we determined that 75% of PGY4 residents who indicated disinterest in learning office hysteroscopy were also interested in pursuing a maternal-fetal medicine fellowship.
Figure 2.
Comparison of residents interested and not interested in learning office hysteroscopy. A subgroup analysis of residents not interested in office hysteroscopy illustrates their post-residency practice plans.
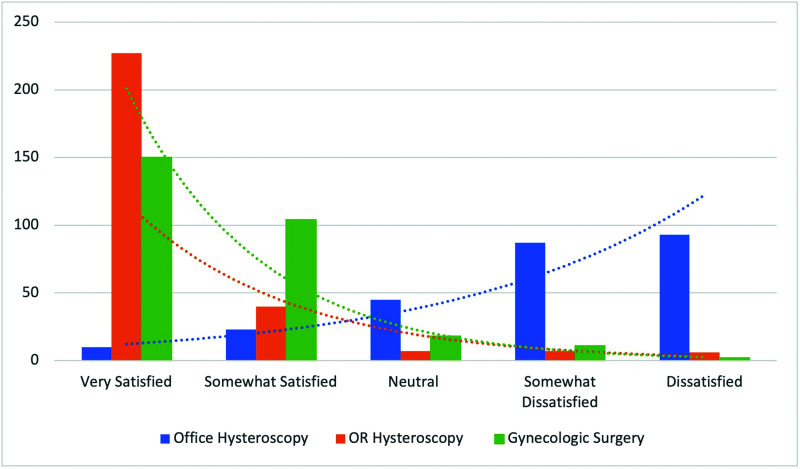
With respect to resident satisfaction with training, there was a statistically significant (p < 0.05) difference in satisfaction between OR hysteroscopy training (91.1%), other gynecological surgical training (86.7%), and office hysteroscopy training (11.3%) (Figure 3). Furthermore, only 17.4% of PGY4 residents reported they could perform office hysteroscopy independently upon graduating. Of the PGY4 residents who reported being able to perform office hysteroscopy independently, 83.3% of those residents (14.5% of all PGY4s) reported feeling comfortable performing the procedure. Less than half of PGY4 residents (42.0%), stated they could perform office hysteroscopy if proctored and 40.6% stated they could not perform the procedure even in a proctored environment.
Figure 3.
Evaluation of resident satisfaction with office hysteroscopy training, operating room hysteroscopy training, and other gynecological surgery training. satisfaction assessed on a five-point likert scale.
DISCUSSION
Hysteroscopic surgery is an invaluable tool for the assessment and treatment of gynecological problems in patients. Advancements in technology have helped tailor its use to evaluate and treat numerous gynecologic conditions in an office setting. However, our study identifies a gap in resident training in ACGME accredited programs with only 26.3% of residents receiving training in office hysteroscopy.
Office procedures pose unique obstacles and require a different skill set and expertise when compared to procedures performed in the operating room.12 Providers must have the basic surgical skills necessary to perform the procedure and the knowledge of how to navigate patient selection, pain, anxiety, and intolerance. At times procedural modifications may also be necessary in order to successfully complete the procedure, such as performing vaginoscopy, utilizing smaller instrumentation, or overcoming a stenotic cervix with micrograspers or scissors. Given these obstacles we argue that even though residents have demonstrated competency in performing hysteroscopy in the operating room those skills are not completely transferable to the office setting. Training in office procedures poses additional challenges as patients are awake and may be less amenable to having their procedure performed by a trainee.20 Therefore, a focus on improving office hysteroscopy training is critical as office hysteroscopy allows providers to offer the ideal method of endometrial sampling and cavity assessment in the most cost-effective manner.11,21,22
Interestingly, a greater proportion of males reported receiving training in office hysteroscopy than women which was statistically significant (p = 0.019). Implicit biases have been well documented within the medical field and not only impact the way physicians treat patients but how they view leadership in medicine.23,24 These biases in turn have resulted in gender disparities for women in medicine, particularly for those in surgical specialties.25 Studies have demonstrated the impact of gender disparities on resident surgical training including decreased operative autonomy and decreased surgical opportunities.25,26 In 2018, 83% of OBGYN residents were female.27 Despite the trend toward female predominance in the field, there are still gender disparities that are evident in training. Educators should be cognizant of, and address, these disparities given the potential impact on physician growth in the field.
We found that majority of residents desired to learn office hysteroscopy. In evaluating the minority of residents who were not interested in learning office hysteroscopy, nearly half reported an intent to pursue a fellowship in maternal-fetal medicine and likely did not feel that learning office hysteroscopy was relevant to their future practice. Residents also expressed satisfaction in their training in OR hysteroscopy and in their overall gynecological surgical training but had low satisfaction in office hysteroscopy training. These findings confirm that while overall residents feel that gynecological training is adequate, there is a deficiency in office hysteroscopy specifically.
With respect to resident preparedness for independent practice, our study found that less than one-fifth of graduating PGY4s felt comfortable performing office hysteroscopy upon graduation. Only 14.5% of the PGY4 residents felt comfortable performing office hysteroscopy and felt they could independently perform the procedure after graduation. In contrast, a recent study by Banks et al., found that 99.5% of fourth year residents felt prepared to perform operative hysteroscopy by the time of graduation. While 99.2% of those residents felt confident in their ability to do so.28 This again illustrates a large discrepancy in residents’ preparedness to perform office hysteroscopy compared to hysteroscopy in the operating room. This discrepancy is likely due to insufficient training in office procedures and highlights a need for more focus in this area during residency.
Strengths of this study are that it utilizes a validated survey tool and follows the formalized structure of the CHERRIES guidelines. It also addresses an area of research with limited data. In contrast to other studies that evaluate resident education and competence, we looked specifically at perceived confidence which heavily impacts whether a procedure is performed in independent practice. We ultimately identify a deficiency in residency training and the barriers to receiving office hysteroscopy. Our study is limited by its sample size. The demographics of the sample population mirrors the distribution of the programs that were sampled. However, there was a lower response rate from residents training in residency programs in the West. Therefore, these findings may not be as generalizable to western residency programs. Additionally, since residents were grouped by regions and not by their individual residency programs our study may be confounded by selection bias amongst the responders. Our study did not assess resident satisfaction with all office-based procedures. Therefore, it is unknown whether resident dissatisfaction with training is specific to office hysteroscopy or with office-based surgery in general. This would be a good area of research for the future. Finally, our study does not address whether improving training in office hysteroscopy would ultimately impact adoption of this modality in future practice.
CONCLUSION
In conclusion, while office hysteroscopy is a valuable gynecological procedure, resident training is lacking. Thus, residents are left unprepared to perform the procedure upon graduation. Our data demonstrate that residents are both interested in learning office hysteroscopy and are dissatisfied in their training. Programs should focus on increasing training in this area, as this would improve residents’ comfort and ability to adequately perform hysteroscopy in the office so that it can be incorporated into their future practice.
Footnotes
Acknowledgements: none.
Disclosure: none.
Conflict of interests: none.
Funding sources: none.
Informed consent: Dr. Lindsey Michel declares that written informed consent was obtained from the patient/s for publication of this study/report and any accompanying images.
Contributor Information
Lindsey Michel, Department of Obstetrics and Gynecology, Stamford Hospital, Stamford, CT. (all authors).
Scott Chudnoff, Department of Obstetrics and Gynecology, Stamford Hospital, Stamford, CT. (all authors); Department of Obstetrics and Gynecology, Columbia University Vagelos College of Physicians and Surgeons, New York, NY. (Dr. Chudnoff).
References:
- 1.Urban RR, Ramzan AA, Doo DW, Sheeder J, Guntupalli SR. The perceptions of gynecologic oncology fellows on readiness for subspecialty training following OB/GYNRESIDENCY. Gynecol Oncol Rep. 2019;28:104–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guntupalli SR, Doo DW, Guy M, et al. Preparedness of obstetrics and gynecology residents for fellowship training. Obstet Gynecol. 2015;126(3):559–568. [DOI] [PubMed] [Google Scholar]
- 3.DeFrancesco MS. Patient safety in outpatient procedures. Obstet Gynecol Clin North Am. 2019;46(2):379–387. [DOI] [PubMed] [Google Scholar]
- 4.Isaacson K. Office hysteroscopy: a valuable but under-utilized technique. Curr Opin Obstet Gynecol. 2002;14(4):381–385. [DOI] [PubMed] [Google Scholar]
- 5.Loffer FD. The time has come to quit relying on a blind endometrial biopsy or dilation and curettage to rule out malignant endometrial changes. J Minim Invasive Gynecol. 2019;26(7):1207–1208. [DOI] [PubMed] [Google Scholar]
- 6.Kremer C, Duffy S, Moroney M. Patient satisfaction with outpatient hysteroscopy versus day case hysteroscopy: randomised controlled trial. BMJ. 2000;320(7230):279–282. [PMC free article] [PubMed] [Google Scholar]
- 7.Mairos J, Di Martino P. Office hysteroscopy. An operative gold standard technique and an important contribution to patient safety. Gynecol Surg. 2016;13:111–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salazar CA, Isaacson KB. Office operative hysteroscopy: an update. J Minim Invasive Gynecol. 2018;25(2):199–208. [DOI] [PubMed] [Google Scholar]
- 9.Cicinelli E. Hysteroscopy without anesthesia: review of recent literature. J Minim Invasive Gynecol. 2010;17(6):703–708. [DOI] [PubMed] [Google Scholar]
- 10.Saridogan E, Tilden D, Sykes D, Davis N, Subramanian D. Cost-analysis comparison of outpatient see-and-treat hysteroscopy service with other hysteroscopy service models. J Minim Invasive Gynecol. 2010;17(4):518–525. [DOI] [PubMed] [Google Scholar]
- 11.Moawad NS, Santamaria E, Johnson M, Shuster J. Cost-effectiveness of office hysteroscopy for abnormal uterine bleeding. JSLS. 2014;18(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Siristatidis C, Chrelias C, Salamalekis G, Kassanos D. Office hysteroscopy: current trends and potential applications: a critical review. Arch Gynecol Obstet. 2010;282(4):383–388. [DOI] [PubMed] [Google Scholar]
- 13.Eysenbach G. Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res. 2004;6(3):e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bannigan K, Watson R. Reliability and validity in a nutshell. J Clin Nurs. 2009;18(23):3237–3243. [DOI] [PubMed] [Google Scholar]
- 15.Carugno J, Grimbizis G, Franchini M, et al. International consensus statement for recommended terminology describing hysteroscopic procedures. J Minim Invasive Gynecol. 2022;29(3):385–391. [DOI] [PubMed] [Google Scholar]
- 16.Bandura A. Guide for constructing self-efficacy scales. In: Urdan T, Pajares F, eds. Self-Efficacy Beliefs of Adolescents. Information Age Publishing, 2006:307–337. [Google Scholar]
- 17.Elfenbein DM. Confidence crisis among general surgery residents: a systematic review and qualitative discourse analysis. JAMA Surg. 2016;151(12):1166–1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bureau USC. Census Regions and Divisions of the United States. Available at: https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf.
- 19.Association of American Medical Colleges. Report on Residents. Available at: https://www.aamc.org/data-reports/students-residents/interactive-data/table-b3-number-active-residents-type-medical-school-gme-specialty-and-sex.
- 20.Enver N, Ramaswamy A, Sulica L, Pitman MJ. Office-based procedure training in laryngology fellowship programs. Laryngoscope. 2021;131(9):2054–2058. [DOI] [PubMed] [Google Scholar]
- 21.Parkash V, Fadare O, Tornos C, McCluggage WG. Committee opinion No. 631: endometrial intraepithelial neoplasia. Obstet Gynecol. 2015;126(4):897. [DOI] [PubMed] [Google Scholar]
- 22.Di Spiezio Sardo A, Di Carlo C, Minozzi S, et al. Efficacy of hysteroscopy in improving reproductive outcomes of infertile couples: a systematic review and meta-analysis. Hum Reprod Update. 2016;22(4):479–496. [DOI] [PubMed] [Google Scholar]
- 23.Dehon E, Weiss N, Jones J, Faulconer W, Hinton E, Sterling S. A systematic review of the impact of physician implicit racial bias on clinical decision making. Acad Emerg Med. 2017;24(8):895–904. [DOI] [PubMed] [Google Scholar]
- 24.Hansen M, Schoonover A, Skarica B, Harrod T, Bahr N, Guise JM. Implicit gender bias among US resident physicians. BMC Med Educ. 2019;19(1):396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Foley KE, Izquierdo KM, von Muchow MG, Bastawrous AL, Cleary RK, Soliman MK. Colon and rectal surgery robotic training programs: an evaluation of gender disparities. Dis Colon Rectum. 2020;63(7):974–979. [DOI] [PubMed] [Google Scholar]
- 26.Meyerson SL, Sternbach JM, Zwischenberger JB, Bender EM. The effect of gender on resident autonomy in the operating room. J Surg Educ. 2017;74(6):e111–e118. [DOI] [PubMed] [Google Scholar]
- 27.Lautenberger D, Dandar V. The state of women in academic medicine: the pipeline and pathways to leadership, 2018–2019. Available at: https://www.aamc.org/data-reports/faculty-institutions/report/state-women-academic-medicine.
- 28.Banks E, Gressel GM, George K, Woodland MB. Resident and program director confidence in resident surgical preparedness in obstetrics and gynecologic training programs. Obstet Gynecol. 2020;136(2):369–376. [DOI] [PubMed] [Google Scholar]