Abstract
Background and Objectives:
Robotic gynecologic surgery has outpaced data showing risks and benefits related to cost, quality outcomes, and patient safety. We aimed to assess how credentialing standards and perceptions of safe use of robotic gynecologic surgery have changed over time.
Methods:
An anonymous, online survey was distributed in 2013 and in 2021 to attending surgeons and trainees in accredited obstetrics and gynecology residency programs.
Results:
There were 367 respondents; 265 in 2013 and 102 in 2021. There was a significant increase in robotic platform use from 2013 to 2021. Percentage of respondents who ever having performed a robotic case increased from 48% to 79% and those who performed > 50 cases increased from 25% to 59%. In 2021, a greater percentage of attending physicians reported having formalized protocol for obtaining robotic credentials (93% vs 70%, p = 0.03) and maintaining credentialing (90% vs 27%, p < 0.01). At both time points, most attendings reported requiring proctoring for 1 – 5 cases before independent use. Opinions on the number of cases needed for surgical independence changed from 2013 to 2021. There was an increase in respondents who believed > 20 cases were required (from 58% to 93% of trainees and 29% to 70% of attendings). In 2021, trainees were less likely to report their attendings lacked the skills to safely perform robotic surgery (25% to 6%, p < 0.01).
Discussion:
Greater experience with robotic platforms and expansion of credentialing processes over time correlated with improved confidence in surgeon skills. Further work is needed to evaluate if current credentialing procedures are sufficient.
Keywords: Credentialing, Gynecologic surgery, Robotic surgery, Safety
INTRODUCTION
Since robotic assisted surgery was approved for gynecologic procedures in 2005, its use has increased exponentially.1–3 Studies have shown robotic surgery has clear benefits over open abdominal surgery, similar to other forms of minimally invasive surgery,4 however without clear superiority over traditional laparoscopy and potentially at greater cost.5–8 There is concern that the rapid adoption of robotic surgery has outpaced data showing risks and benefits related to cost, quality outcomes, and patient safety.
Mastery of robotics requires integration of a new set of skills not found in either open or conventional laparoscopic surgery, such as simultaneous management of multiple instruments, multiple energy sources, foot and hand controls, lack of haptics, and a complex patient cart. Prior studies have shown a prolonged learning curve is needed, ranging between 20 and 200 cases to achieve proficiency, and 20 to 50 cases to reduce operating time and improve cost efficiency.9–16
To address concerns of lack of standardized approaches to robotic training and credentialing, both the American College of Obstetricians and Gynecologists (ACOG) and the American Association of Gynecologic Laparoscopists (AAGL) have released statements recommending rigorous training and credentialing standards, minimum case numbers, proctoring, and peer case review.5,17 Although some residency graduates have enough exposure and training to practice independently after graduation, residency robotic training curricula continue to vary widely,18 calling into question the credentialing and safety of robotic practice among attending gynecologic surgeons.
The objective of this survey study was to assess how credentialing standards and perceptions of safe use of robotic surgery in gynecology have changed over time. Specifically, we sought to assess if management of and standards for robotic training and credentialing are perceived to correlate with safe incorporation of robotic surgery into practice.
METHODOLOGY
This was an anonymous, voluntary, internet-based cohort survey study conducted at two time points, 2013 and 2021. An open survey invitation was emailed to all Accreditation Council for Graduate Medical Education (ACGME) accredited obstetrics and gynecology residency program coordinators in the United States for electronic distribution to their associated attending physician and trainee (residents and fellows) listservs. At both time points, usability and technical functionality of the electronic questionnaire were tested prior to distribution. Informed consent was obtained and no personal data or identifying information was collected. Respondents entered their information directly into a SurveyMonkey (Momentive, San Mateo, CA) database for the 2013 survey and into a Qualtrics XM (Provo, UT) database for the 2021 survey. There were 22 questions for trainees and 29 questions for attending surgeons. The survey collected respondent demographic information (geographic location, surgical volume, type of cases performed), institutional credentialing protocols, and personal experience with and opinion on how robotics is being incorporated into the gynecologic surgery. All answers were included in analysis, regardless of completeness with no statistical correction such as weighting of items or propensity scores. Missing data was noted in tables, but not included in analysis or percentages.
We used χ2 test and descriptive statistics to compare the distribution of responses between trainees and attendings and changes over time. A P-value of 0.05 was set to denote statistical significance. Data analysis was performed using SAS 9.4 software (SAS Institute INC, Cary, NC). The study protocol was approved by the University of North Carolina Institutional Review Board number 19–0045 for the 2021 survey and Henry Ford Health System Institutional Review Board number 7564 for the 2013 survey.
RESULTS
A total of 367 individuals including 157 attendings and 210 trainees responded to the surveys. Of these, 265 were from the 2013 cohort and 102 were from the 2021 cohort. The demographic information in 2021 (location, training year, years of practice) was different from the 2013 cohort, including a greater percentage of attendings located in the southeast U.S. (52% vs 18%) and a greater percentage of the trainees being fellows vs residents (29% vs 10%) (Table 1).
Table 1.
Demographics of Survey Sample
| Residents/Fellows |
Attendings |
|||||
|---|---|---|---|---|---|---|
| 2013 Survey n = 137 (%) |
2021 Survey n = 73 (%) |
P-value | 2013 Survey n = 128 (%) |
2021 Survey n = 29 (%) |
P-value | |
| Practice Location | ||||||
| Midwest | 42 (31) | 9 (12) | < 0.01 | 37 (29) | 3 (10) | < 0.01 |
| Northeast | 43 (32) | 36 (49) | 52 (41) | 9 (31) | ||
| Southeast | 24 (18) | 24 (33) | 23 (18) | 15 (52) | ||
| Southwest | 13 (10) | 3 (4) | 14 (11) | 2 (7) | ||
| West | 14 (10) | 1 (1) | 1 (1) | 0 | ||
| Missing | 1 | 1 | ||||
| Training Year | ||||||
| Fellow Year 1 | 5 (4) | 4 (5) | < 0.01 | – | – | |
| Fellow Year 2 | 7 (5) | 10 (14) | – | – | ||
| Fellow Year 3 | 1 (1) | 7 (10) | – | – | ||
| PGY1 | 22 (16) | 7 (10) | – | – | ||
| PGY2 | 28 (20) | 16 (22) | – | – | ||
| PGY3 | 39 (28) | 14 (19) | – | – | ||
| PGY4 | 35 (26) | 15 (21) | – | – | ||
| Years in Practice | ||||||
| 0 – 4 years | – | – | 24 (19) | 6 (21) | 0.78 | |
| 5 – 9 years | – | – | 29 (23) | 6 (21) | ||
| 10 – 14 years | – | – | 19 (15) | 6 (21) | ||
| 15+ years | – | – | 56 (44) | 10 (36) | ||
| Missing | – | – | 1 | |||
Abbreviation: PGY, post graduate year.
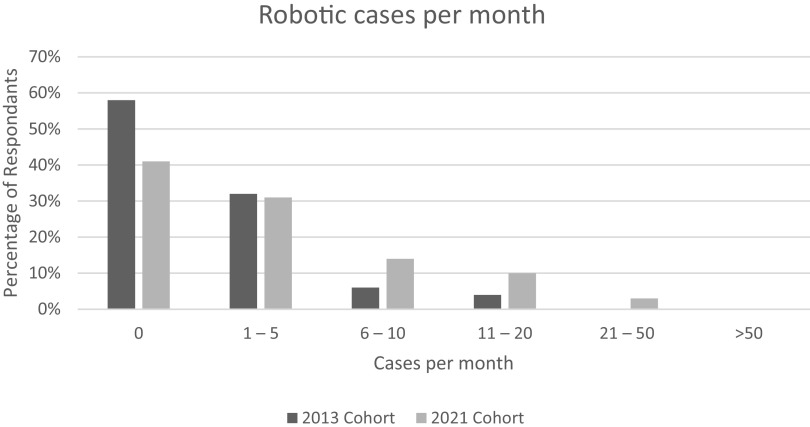
Case Volume
The length of time participants had at least one robotic platform at their institution significantly increased over time, with 30% of 2013 respondents reporting > 5 years compared to 89% of 2021 respondents (Table 2). Of those that had a robotic platform at their institution, all had an Intuitive da Vinci surgical systems robotic platform. The total number of cases attending physicians performed increased over time (P < 0.01), with the percentage of attendings who have ever performed a robotic case increasing from 48% to 79% and the percentage of those who performed > 50 cases increasing from 25% to 59%. The number of robotic cases per month per attending physician increased, with 27% performing > 6 cases per month in the 2021 cohort compared to just 10% in the 2013 cohort (P = 0.05, Figure 1). There was not a significant difference between time points for robotic cases per month for trainees. Respondents reported using the robotic platform for hysterectomy, sacrocolpopexy, myomectomy, adnexal surgery, and gynecologic oncology surgery, with hysterectomy cited most commonly in all groups.
Table 2.
Robotic Case Volume
| Residents/Fellows |
Attendings |
|||||
|---|---|---|---|---|---|---|
| 2013 Survey n = 137 (%) |
2021 Survey n = 73 (%) |
P-value | 2013 Survey n = 128 (%) |
2021 Survey n = 29 (%) |
P-value | |
| How long has your institution had the robotic platform? | ||||||
| < 1 year | 2 (2) | 0 | < 0.01 | 2 (2) | 0 | < 0.01 |
| 1 – 2 years | 10 (8) | 0 | 12 (10) | 0 | ||
| 3 – 5 years | 42 (33) | 6 (8) | 63 (51) | 0 | ||
| 6 – 10 years | 31 (24) | 13 (18) | 22 (18) | 6 (21) | ||
| > 10 years | 2 (2) | 15 (21) | 4 (3) | 13 (45) | ||
| I don’t know | 41 (32) | 39 (53) | 20 (16) | 10 (34) | ||
| Missing | 9 | 0 | 4 | |||
| How many robotics cases do you participate in per month? | ||||||
| 0 cases | 21 (16) | 14 (19) | 0.42 | 72 (58) | 12 (41) | 0.05 |
| 1 – 5 cases | 70 (55) | 32 (44) | 40 (32) | 9 (31) | ||
| 6 – 10 cases | 24 (19) | 16 (22) | 7 (6) | 4 (14) | ||
| 11 – 20 cases | 11 (9) | 8 (11) | 5 (4) | 3 (10) | ||
| 21 – 50 cases | 1 (1) | 3 (4) | 0 | 1 (3) | ||
| > 50 cases | 1 (1) | 0 | 0 | 0 | ||
| Missing | 9 | 0 | 4 | |||
| The total number of robotic GYN cases I have completed at the console as an attending is | ||||||
| 0 cases | – | – | 64 (52) | 6 (21) | < 0.01 | |
| 1 – 5 cases | – | – | 5 (4) | 0 | ||
| 6 – 10 cases | – | – | 5 (4) | 2 (7) | ||
| 11 – 20 cases | – | – | 6 (5) | 3 (10) | ||
| 21 – 50 cases | – | – | 11 (9) | 1 (3) | ||
| > 50 cases | – | 31 (25) | 17 (59) | |||
| Missing | – | – | 6 | 0 | ||
Figure 1.
Change in robotic case volume for gynecologic surgeons from 2013 to 2021.
Credentialing and Training
The percentage of attendings who reported having formalized protocols for obtaining robotic credentials increased significantly from 2013 to 2021 (70% to 93%, P = 0.03). The number of cases attending participants reported bedside assisting prior to doing console work significantly increased (P < 0.01), with those reporting any cases increased from 45% to 79%. At both time points, most attendings reported requiring proctoring for 1 – 5 cases prior to independent use. The percentage of attendings who reported their department required a minimum number of robotic cases for surgeons to maintain robotic credentials increased significantly from 27% to 90% (P < 0.01). Of those that knew of minimum numbers, most the attendings (76%) reported requiring 10 – 20 cases per year to maintain credentialing (only asked in the 2021 cohort). (Table 3).
Table 3.
Information About Robotic Platform Credentialing and Training from Attending Physicians
| 2013 Survey n = 128 (%) |
2021 Survey n = 29 (%) |
P-value | |
|---|---|---|---|
| My institution has a formalized protocol for gaining credentials as a robotic surgeon | |||
| True | 87 (70) | 27 (93) | 0.03 |
| False | 10 (8) | 0 | |
| I don’t know | 28 (22) | 2 (7) | |
| Missing | 3 | 0 | |
| The total number of robotic cases I bedside assisted prior to EVER doing console work was | |||
| 0 cases | 65 (55) | 6 (21) | < 0.01 |
| 1 – 5 cases | 29 (25) | 6 (21) | |
| 6 – 10 cases | 9 (8) | 5 (17) | |
| 11 – 20 cases | 9 (8) | 3 (10) | |
| > 20 cases | 6 (5) | 9 (31) | |
| Missing | 10 | 0 | |
| Before completing cases independently, my institution requires proctoring in | |||
| 1 – 5 cases | 64 (52) | 10 (34) | < 0.01 |
| 6 – 9 cases | 9 (7) | 1 (3) | |
| 10 – 20 cases | 6 (5) | 3 (10) | |
| 21 – 50 cases | 1 (1) | 0 | |
| > 50 cases | 0 | 0 | |
| Does not require if documentation/experience provided | NA | 5 (17) | |
| My institution doesn’t require proctoring | 0 | 1 (3) | |
| I don’t know | 42 (34) | 9 (31) | |
| Missing | 6 | 0 | |
| I have to maintain certain amount of robotic cases per month/year to keep credentialed | |||
| True | 33 (27) | 19 (90) | < 0.01 |
| False | 24 (20) | 2 (10) | |
| I don’t know | 64 (53) | 8 (28) | |
| Missing | 7 | 0 | |
| What is the minimum number of cases that your institution requires yearly to maintain credentialed? | |||
| 1 – 5 cases | – | 1 (3) | |
| 6 – 9 cases | – | 3 (10) | |
| 10 – 20 cases | – | 13 (45) | |
| 21 – 50 cases | – | 0 | |
| > 50 cases | – | 0 | |
| My institution does not require a minimum number of cases | – | 0 | |
| Missing | – | 12 | |
Questions about resident/fellow training were only asked in the 2021 cohort. Fifty-four percent of trainees reported a curriculum in place to become trained in robotic hysterectomy. Sixty-eight percent of residents reported regular use of a teaching console.
Learning Curve
Attending physicians and trainees differed in their opinions of the number of cases needed to become an independent robotic surgeon at both time points, although both increased over time (P < 0.01). The percent that reported that number to be > 20 cases increased for trainees (58% to 93%) and for attendings (29% to 70%) (Table 4).
Table 4.
Opinions on Learning Curve of Using Robotic Platform
| Residents/Fellows |
Attendings |
|||||
|---|---|---|---|---|---|---|
| 2013 Survey n = 137 (%) |
2021 Survey n = 73 (%) |
P-value | 2013 Survey n = 128 (%) |
2021 Survey n = 29 (%) |
P-value | |
| How many cases do you think one generally needs to perform to become independent? | ||||||
| 1 – 5 cases | 0 | 0 | < 0.01 | 13 (12) | 1 (4) | < 0.01 |
| 6 – 10 cases | 7 (6) | 0 | 22 (21) | 2 (7) | ||
| 11 – 20 cases | 36 (30) | 4 (6) | 41 (39) | 5 (19) | ||
| 21 – 50 cases | 54 (45) | 36 (55) | 23 (22) | 13 (48) | ||
| > 50 cases | 15 (13) | 25 (38) | 7 (7) | 6 (22) | ||
| Missing | 18 | 7 | 22 | 3 | ||
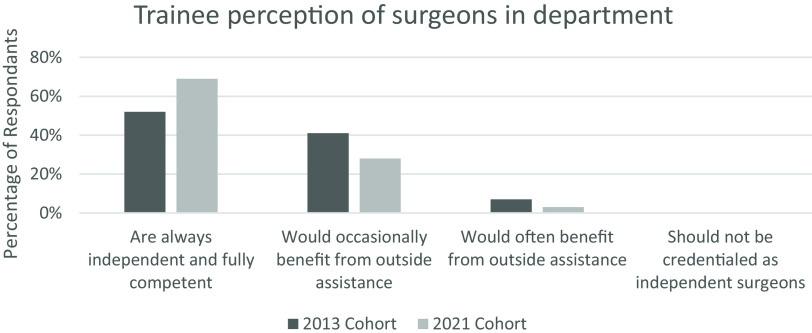
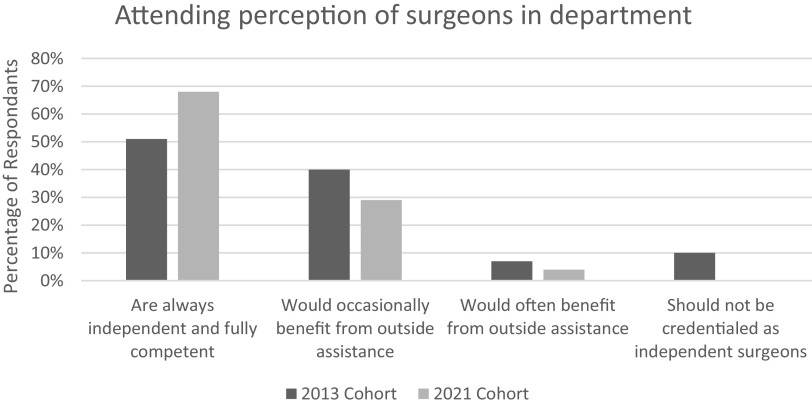
Perception of Safety
Over time, both trainees and attending physicians had more confidence in the robotic surgeons in their departments. More respondents reported that attending gynecologic robotic surgeons are always fully independent and competent (52% to 69% for trainees, 51% to 68% for attendings), but this change was not significant for either group (Figures 2 and 3). Similarly, the percentage of trainees and attendings who felt there were people doing robotic cases who lacked the skills to do so safely decreased for both groups, although only significantly for trainees (25% to 6% for trainees, P < 0.01, 30% to 21% for attendings, P = 0.32). The percentage of trainees who ever wished someone more expert was in the room during robotic cases decreased, with trends towards significance (67% to 48%, P = 0.06). For attending physicians, this percentage increased, but there was not a significant difference between time points (46% to 67% P = 0.11). Similarly, the percentage of trainees who felt cases were ever booked above their attendings’ skill level decreased (69% to 56%, P < 0.01) while the percentage of attendings who reported this about themselves increased, although not significantly (31% to 50%, P = 0.16) (Table 5).
Figure 2.
Trainee perception of attending surgeon independence and safety from 2013 to 2021.
Figure 3.
Attending surgeon perception of colleagues’ independence and safety from 2013 to 2021.
Table 5.
Opinions on Safety of Robotic Platform in Gynecologic Surgery
| Residents/Fellows |
Attendings |
|||||
|---|---|---|---|---|---|---|
| 2013 Survey n = 137 (%) |
2021 Survey n = 73 (%) |
P-value | 2013 Survey n = 128 (%) |
2021 Survey n = 29 (%) |
P-value | |
| On average GYN attendings in my department | ||||||
| Are always independent and fully competent | 61 (52) | 45 (69) | 0.07 | 56 (51) | 19 (68) | 0.44 |
| Would occasionally benefit from outside assistance | 48 (41) | 18 (28) | 44 (40) | 8 (29) | ||
| Would often benefit from outside assistance | 8 (7) | 2 (3) | 8 (7) | 1 (4) | ||
| Should not be credentialed as independent surgeons | 0 | 0 | 1 (1) | 0 | ||
| Missing | 20 | 8 | 19 | 1 | ||
| I feel that there are attendings/people doing robotic cases independently who lack the skills to do so safely on a consistent basis | ||||||
| True | 30 (25) | 4 (6) | < 0.01 | 34 (30) | 6 (21) | 0.32 |
| False | 90 (75) | 61 (94) | 79 (70) | 23 (79) | ||
| Missing | 17 | 8 | 15 | 0 | ||
| I wish there were someone more expert in the room | ||||||
| Never | 38 (32) | 34 (52) | 0.06 | 46 (54) | 8 (33) | 0.11 |
| Rarely | 55 (47) | 23 (35) | 25 (29) | 14 (58) | ||
| Sometimes | 19 (16) | 7 (11) | 8 (9) | 1 (4) | ||
| Frequently | 5 (4) | 1 (2) | 3 (4) | 1 (4) | ||
| Always | 0 | 0 | 3 (4) | 0 | ||
| Missing | 20 | 8 | 43 | 5 | ||
| I feel that cases are booked beyond my/the attending’s skill level | ||||||
| Never | 36 (31) | 29 (45) | < 0.01 | 67 (69) | 12 (50) | 0.16 |
| Rarely | 60 (51) | 32 (49) | 29 (30) | 11 (46) | ||
| Sometimes | 20 (17) | 1 (2) | 1 (1) | 1 (4) | ||
| Frequently | 1 (1) | 1 (2) | 0 | 0 | ||
| Always | 0 | 2 (3) | 0 | 0 | ||
| Missing | 20 | 8 | 31 | 6 | ||
Institutional Application of Robotic Surgery
Trainees were significantly more likely to agree that the robot is being utilized in a way that consistently improves quality of patient care in 2021 compared to 2013 (90% vs 66%, P < 0.01). While there was also an increase in this metric for attending surgeons, this change was not significant (55% to 66%, P = 0.46). However, both groups had a significant increase in respondents who agreed that the robot was being chosen for appropriate cases on a consistent basis (67% to 100% of trainees, P < 0.01; 59% to 96% for attending surgeons, P < 0.01). The slight majority of trainees at both time points agreed that their institution wanted more gynecologists to become trained in robotics (59% and 58%), while the minority of attending respondents agreed with this statement, and this decreased overtime (46% to 21%, P = 0.02). Most trainee and attending respondents at both time points believed that the robotic platform makes minimally invasive surgery more accessible to those lacking straight stick laparoscopic skills; however, this decreased for trainees (69% to 53%, P = 0.03) and increased for attending physicians (59% to 79%, P = 0.05) (Table 6).
Table 6.
Opinions on Institutional Use of Robotic Platform
| Residents/Fellows |
Attendings |
|||||
|---|---|---|---|---|---|---|
| 2013 Survey n = 137 (%) |
2021 Survey n = 73 (%) |
P-value | 2013 Survey n = 128 (%) |
2021 Survey n = 29 (%) |
P-value | |
| I believe that in my institution/department the robot is being utilized in a way that consistently improves quality of patient care/outcomes | ||||||
| Strongly Agree | 27 (23) | 27 (42) | < 0.01 | 29 (25) | 9 (33) | 0.46 |
| Somewhat Agree | 51 (43) | 31 (48) | 35 (30) | 9 (33) | ||
| Neutral | 25 (21) | 6 (9) | 14 (12) | 4 (15) | ||
| Somewhat Disagree | 14 (12) | 1 (2) | 30 (25) | 5 (19) | ||
| Strongly Disagree | 2 (2) | 0 | 10 (8) | 0 | ||
| Missing | 18 | 8 | 10 | 3 | ||
| I believe that in my institution the robot is being chosen for appropriate cases on a consistent basis | ||||||
| True | 80 (67) | 65 (100) | < 0.01 | 68 (59) | 23 (96) | < 0.01 |
| False | 39 (33) | 0 | 47 (41) | 1 (4) | ||
| Missing | 18 | 8 | 13 | 5 | ||
| I believe that my institution wants more of our gynecologists to become robot trained | ||||||
| True | 70 (59) | 38 (58) | 0.82 | 56 (46) | 6 (21) | 0.02 |
| False | 48 (41) | 28 (42) | 65 (54) | 22 (79) | ||
| Missing | 19 | 7 | 7 | 1 | ||
| I believe the robotic platform makes minimally invasive surgery more accessible to those lacking traditional (i.e., straight stick) laparoscopic skills | ||||||
| True | 83 (69) | 35 (53) | 0.03 | 68 (59) | 22 (79) | 0.05 |
| False | 37 (31) | 31 (47) | 48 (41) | 6 (21) | ||
| Missing | 17 | 7 | 12 | 2 | ||
DISCUSSION
This study sought to explore and compare the learning curve, credentialing process, and the safe and efficient application of robotic gynecologic surgery across two time points, including both trainees and attending surgeons. In each survey we evaluated how credentialing programs related to confidence of independent case completion, and personal beliefs on how the use of robotics affects patient safety and outcomes. Given the two time points, we were able to report on how these factors may have changed over time, with better development and implementation of robotics training at individual institutions.
Case Volume, Credentialing, Training, and Learning Curve
As expected, in 2021 participants reported performing a greater number of robotic cases and having better access to robotic platforms at their institution for more years. This follows reports from with other national studies showing increasing numbers for robotic gynecologic procedures being performed.1–3
Aligned with the increased use of robotics across institutions, formal credentialing processes also increased from 70% to 93% from 2013 to 2021. A call for the standardization of robotic credentialing to demonstrate proficiency, ensure patients safety, and provide reproducible results has been recommended by professional organization position statements.5,17,19
Defining robotic proficiency is challenging; previous studies have found a set number of cases completed cannot sufficiently substitute individual appraisal of operative skill, given that the learning curve for each individual will vary.17,20 Additionally, most obstetrics and gynecology residencies now include training on the robotic platform, although curricula vary greatly. In our study, we found most attending physicians reported a requirement of 1 – 5 proctored cases prior to credentialing, similar in 2013 and 2021. It remains unclear if this is referring to surgeons who already reached robotic proficiency and were new to an institution or those who were newly trained in robotic surgery. This number is similar to survey results obtained from the second World Robotic Gynecology Congress in 2010 in which surgeons reported on average being proctored in 3.29 cases prior to independent practice.20 Similarly, one study of multiple hospitals found that a median of 5 cases performed in residency was sufficient for credentialing, with most hospitals not requiring any proctored cases if a case list and note from a program director were provided.21,22 Given that published literature previously established a learning curve of at least 20 cases9–16 and the findings in our study that most trainees and attendings in 2021 agreed that at least 20 cases are needed to be a safe and efficient independent robotic surgeon, then 5 cases may not be sufficient for someone who is new to robotic surgery. It should be questioned whether surgeons who have performed robotic cases independently only 1 – 5 times in a monitored environment have sufficient training and comfort to implement this complicated technology in clinical practice.
This may be partially mitigated by the increase in percentage of surgeons who have bedside-assisted prior to sitting at the console; however, almost one-quarter of surgeons reported never having bedside-assisted prior to console work, and over half had assisted in ≤ 10 cases. This practice is contrary to the recommended AAGL privileging guidelines17 and prior reports suggesting that bedside assisting in > 10 cases is instrumental in order to understand the platform’s uses and limitations to operate it safely at a distance from the bedside.23,24 The console surgeon, remote from the patient and the operating instruments, is required to diagnose and resolve technical problems encountered at distant areas of the operating room. Proficiency in this practice is only gained through repeated exposure to the potential issues, which is ideally first encountered at the bedside with an experienced robotic proctor who can guide through this trouble-shooting process.
In our study, there was a significant increase in the number of attendings who reported institutional requirements for a minimum case volume per month or year to remain credentialed (27% to 90%). Across most medical certifications, regardless of specialty, re-examination of skill and knowledge is required for continued medical practice. Case specific gynecologic surgical volume has recently come to the forefront of gynecologic surgery, with better postoperative surgical outcomes reported in high volume surgeons compared to low volume surgeons.25,26 This further supports the practice of requiring minimum case volume in order to maintain credentialing in a procedure to best optimize patient safety and outcomes. It is encouraging there was an increase in institutional requirements for case minimums; however, concerning that there are still some academic institutions without these guidelines in place. From an institutional standpoint, one must consider that robotic time is often limited and in high demand. An unintended consequence of minimum case volumes may be to encourage surgeons to perform cases robotically that otherwise would have been performed laparoscopically, unnecessarily utilizing this limited resource and potentially adding unnecessary time or cost to their cases.
Standardized training for residents and fellows has also become a priority with the expansion of robotic surgery in clinical practice. While many programs have a curriculum, the current edition of the Council on Resident Education in Obstetrics and Gynecology Core Curriculum does not have specific criteria for training in robotic surgery.5 Studies have shown diverse training curricula, including virtual reality simulators, didactics, and wet labs. However, there are not yet strong data on the most effective training for surgical trainees.18 In the 2021 cohort, only 54% of trainees reported an institutional curriculum to become robotically trained. This is not significantly different than a 2011 survey of the ACGME obstetrics and gynecology residency programs, showed 58% of residency programs included a robotic curriculum in their residency training.27 This is surprising given the increase in robotic hysterectomies over the last ten years and development of national programs such as the Robotic Training Network, and the Fundamentals of Robotic Surgery. Interestingly, while there was a significant increase in robotic case volume for attendings from 2013 to 2021, the case volumes for trainees were not significantly different at the two time points. This may be due to impact from the COVID-19 pandemic; while attendings considered their prepandemic numbers, trainees may not have been performing any robotic cases prior to 2020. Another residency consideration regarding the increased adoption of robotic surgery is the potential for robotics to impinge on training in other minimally invasive techniques. As more cases are performed robotically, fewer may be performed via traditional laparoscopy or vaginal surgery, raising concerns about sufficient experience and skill to confidently perform these other modalities of hysterectomy upon graduation.
Concerns around robotic credentialing and training extend across specialties. The American Urologic Association created guidelines on robotic privileging that include recommendations on residency numbers (20 cases) or alternative pathways post-residency including online courses, industry sponsored training, a skills checklist, and the approval of a proctor.28 The Institute for Surgical Excellence recently convened a multidisciplinary group of experts to develop robotic credentialing guidelines after identifying technical proficiency and patient safety concerns due to the heterogeneity in credentialing between hospitals and specialties. They concluded credentialling should focus on performance evaluation rather than just case numbers. This would include knowledge evaluations, simulation, bedside assisting, proctoring, and a video case review as well as multifaceted requirements for privileging maintenance.29
Overall, the expansion of credentialing and training in robotic gynecology is encouraging; however, this may still be insufficient, as both trainees and attendings continue to report concerns regarding the safety of the robotic practices at their institutions.
Perception of Safety
Compared to the 2013 cohort, in 2021 more attendings and residents agreed that gynecology attendings in their departments are always fully independent and competent when performing robotic surgery (52% to 69% for trainees, 51% to 68% for attendings), but this change was not significant for either group. This means about one-third of both groups felt the attending surgeons in their department were not fully independent. Additionally, in 2021 almost a quarter of attending physicians felt their colleagues were consistently performing unsafe surgeries, which was similar to the 2013 numbers. Greater than 50% of trainees and attendings reported that cases were booked above the attending’s skill level, although this largely seen as a rare event. This is a significant safety concern, even if only happening occasionally.
It is possible that the robotic platform allows for a false sense of security, encouraging surgeons to book cases above their skill level. Given the varying degrees of experience, skill, and surgical volume among attendings in any given gynecology department, it is also possible there would be similar percentages reported if asking about other procedures, such as abdominal or laparoscopic hysterectomy. These data may be an indictment of our credentialing programs as a whole and is highlighted in robotics only due to the new paradigms required to teach and integrate new users in robotics. The complexity of the robotic platform and necessarily deliberate approach to teaching it leads to greater scrutiny of the process, which is necessary to ensure patient safety.
In general, attendings seem to become less confident over time in their own skills and those in their department, although our smaller sample size of 2021 attendings did not show any of these changes to be significant. Trainees, on the other hand, became more confident in the skills and safety of those they trained under.
Institutional Application of Robotic Surgery
Both trainee and attending respondents generally felt more positively about how the robotic platform was being used at their institutions. There was an increase in those that agreed the robotic platform was being utilized in a way that improved patient care and that appropriate cases were selected. As the robotic platform becomes increasingly available, it is not surprising there is a wider acceptance of it. Attending surgeons reported a decrease in institutional desire for more gynecologists to be trained in robotics (46% to 21%). This may be because a larger proportion of surgeons were already trained in robotic surgery either in residency or early in their career. At both time points, most trainee and attending respondents believed that the robotic platform makes minimally invasive surgery more accessible to those lacking traditional laparoscopic skills. This highlights a potentially significant benefit of the robotic platform: allowing more surgeons to offer a minimally invasive alternative to open surgery.
Limitations
We acknowledge the limitations of our study. The survey study design limits generalizability to all practitioners of robotic surgery as participants are self-selecting and we are unable to comment on response rate given we do not know how many gynecologists received the survey. Additionally, this study was conducted only at academic institutions, which may have very different practice patterns and perceptions than community hospitals. The two time points did not survey the same participants, used a different survey platform, and there were demographic differences between cohorts, such as training level and geography, making comparisons between them less reliable. Additionally, the robotic surgery platforms have been improved over time, so the technology utilized was likely not the same between groups. There are no validated survey tools in this area of study, so these survey questions were not validated. Our sample was a convenience sample, without equal representation of institutions across geographic area. The sample size was relatively small, which may have limited the ability to identify significant findings.
CONCLUSION
Use of robotic surgery in gynecology has increased overtime, which has been accompanied by an expansion of credentialing and privilege maintenance protocols. Perceptions of safety and competency have also improved over time, specifically by trainees who are more likely to witness the skills of multiple faculty in their department. However, questions remain on whether the current credentialing and privilege maintenance protocols are sufficient. The specific goals of the credentialing process must be clearly outlined at the institutional level to ensure patient safety. Standards for credentialing should be set by surgical and specialty societies such as ACOG and the AAGL in order to achieve uniformity of expectations and expertise amongst those practicing robotic gynecologic surgery. These should go beyond the previously recommended minimum of two proctored cases as there is evidence that current standards may not be sufficient to ensure patient safety and surgeon competency. Requiring at least 20 cases with clear demonstration of proficiency through standardized skill assessment prior to full independent privileges is better aligned with data on the robotic platform learning curve and surgeon perspectives.
Footnotes
Acknowledgements: none.
Disclosure: none.
Conflict of interests: none.
Funding sources: none.
Informed consent: Dr. R. Gina Silverstein declares that written informed consent was obtained from the patient/s for publication of this study/report and any accompanying images.
Contributor Information
R. Gina Silverstein, Department of Obstetrics and Gynecology, University of North Carolina – Chapel Hill, Chapel Hill, NC. (All authors).
Kristin J. Moore, Department of Obstetrics and Gynecology, University of N Carolina – Chapel Hill, Chapel Hill, NC. (All authors).
Erin T. Carey, Department of Obstetrics and Gynecology, University of N Carolina – Chapel Hill, Chapel Hill, NC. (All authors).
Lauren D. Schiff, Department of Obstetrics and Gynecology, University of N Carolina – Chapel Hill, Chapel Hill, NC. (All authors).
References:
- 1.Aarts JWM, Nieboer TE, Johnson N, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev. 2015;2015(8):CD003677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boitano TKL, Smith HJ, Cohen JG, Rossi EC, Kim KH. Implementation and evaluation of a novel subspecialty society fellows robotic surgical course: The sgo minimally invasive academy surgical curriculum. J Gynecol Oncol. 2021;32(2):e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abel MK, Chan JK, Chow S, et al. Trends and survival outcomes of robotic, laparoscopic, and open surgery for stage II uterine cancer. Int J Gynecol Cancer. 2020;30(9):1347–1355. [DOI] [PubMed] [Google Scholar]
- 4.Madueke-Laveaux OS, Advincula AP. Robot-assisted laparoscopy in benign gynecology: advantageous device or controversial gimmick? Best Pract Res Clin Obstet Gynaecol. 2017;45:2–6. [DOI] [PubMed] [Google Scholar]
- 5.Robot-Assisted Surgery for Noncancerous Gynecologic Conditions: ACOG COMMITTEE OPINION SUMMARY, Number 810. Obstetrics and Gynecology. 2020;136(3):e22–e30. [DOI] [PubMed] [Google Scholar]
- 6.Wright JD, Ananth CV, Lewin SN, et al. Robotically assisted vs laparoscopic hysterectomy among women with benign gynecologic disease. JAMA. 2013;309(7):689–698. [DOI] [PubMed] [Google Scholar]
- 7.Swenson CW, Kamdar NS, Harris JA, Uppal S, Campbell DA, Morgan DM. Comparison of robotic and other minimally invasive routes of hysterectomy for benign indications. Am J Obstet Gynecol. 2016;215(5):650.e1–650.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lawrie TA, Liu H, Lu DH, et al. Robot-assisted surgery in gynaecology. Cochrane Database Syst Rev. 2019;4(4):CD011422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lin JF, Frey M, Huang JQ. Learning curve analysis of the first 100 robotic-assisted laparoscopic hysterectomies performed by a single surgeon. Int J Gynaecol Obstet. 2014;124(1):88–91. [DOI] [PubMed] [Google Scholar]
- 10.Lenihan JP, Kovanda C, Seshadri-Kreaden U. What is the learning curve for robotic assisted gynecologic surgery? J Minim Invasive Gynecol. 2008;15(5):589–594. [DOI] [PubMed] [Google Scholar]
- 11.Kim S, Ryu KJ, Min KJ, et al. Learning curve for sentinel lymph node mapping in gynecologic malignancies. J Surg Oncol. 2020;121(4):599–604. [DOI] [PubMed] [Google Scholar]
- 12.Tang FH, Tsai EM. Learning curve analysis of different stages of robotic-assisted laparoscopic hysterectomy. Biomed Res Int. 2017;2017:1827913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sharma S, Calixte R, Finamore PS. Establishing the learning curve of robotic sacral colpopexy in a start-up robotics program. J Minim Invasive Gynecol. 2016;23(1):89–93. [DOI] [PubMed] [Google Scholar]
- 14.Akdemir A, Zeybek B, Ozgurel B, Oztekin MK, Sendag F. Learning curve analysis of intracorporeal cuff suturing during robotic single-site total hysterectomy. J Minim Invasive Gynecol. 2015;22(3):384–389. [DOI] [PubMed] [Google Scholar]
- 15.Woelk JL, Casiano ER, Weaver AL, Gostout BS, Trabuco EC, Gebhart JB. The learning curve of robotic hysterectomy. Obstetrics and Gynecology. 2013;121(1):87–95. [DOI] [PubMed] [Google Scholar]
- 16.Payne TN, Dauterive FR. A comparison of total laparoscopic hysterectomy to robotically assisted hysterectomy: surgical outcomes in a community practice. J Minim Invasive Gynecol. 2008;15(3):286–291. [DOI] [PubMed] [Google Scholar]
- 17.Guidelines for privileging for robotic-assisted gynecologic laparoscopy. J Minim Invasive Gynecol. 2014;21(2):157–67. [DOI] [PubMed] [Google Scholar]
- 18.Azadi S, Green IC, Arnold A, Truong M, Potts J, Martino MA. Robotic surgery: the impact of simulation and other innovative platforms on performance and training. J Minim Invasive Gynecol. 2021;28(3):490–495. [DOI] [PubMed] [Google Scholar]
- 19.Lee YL, Kilic GS, Phelps JY. Medicolegal review of liability risks for gynecologists stemming from lack of training in robot-assisted surgery. J Minim Invasive Gynecol. 2011;18(4):512–515. [DOI] [PubMed] [Google Scholar]
- 20.Lenihan JP. Navigating credentialing, privileging, and learning curves in robotics with an evidence and experienced-based approach. Clin Obstet Gynecol. 2011;54(3):382–390. [DOI] [PubMed] [Google Scholar]
- 21.Erickson BK, Gleason JL, Huh WK, Richter HE. Survey of robotic surgery credentialing requirements for physicians completing OB/GYN residency. J Minim Invasive Gynecol. 2012;19(5):589–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Crane AK, Illanes DS, Adams SR, et al. Surgical privileging in gynecology: a fellows’ pelvic research network study. Female Pelvic Med Reconstr Surg. 2014;20(1):19–22. [DOI] [PubMed] [Google Scholar]
- 23.Rashid HH, Leung YYM, Rashid MJ, Oleyourryk G, Valvo JR, Eichel L. Robotic surgical education: a systematic approach to training urology residents to perform robotic-assisted laparoscopic radical prostatectomy. Urology. 2006;68(1):75–79. [DOI] [PubMed] [Google Scholar]
- 24.Rocco B, Lorusso A, Coelho RF, Palmer KJ, Patel VR. Building a robotic program. Scand J Surg. 2009;98(2):72–75. [DOI] [PubMed] [Google Scholar]
- 25.Vree FEM, Cohen SL, Chavan N, Einarsson JI. The impact of surgeon volume on perioperative outcomes in hysterectomy. JSLS. 2014;18(2):174–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mowat A, Maher C, Ballard E. Surgical outcomes for low-volume vs high-volume surgeons in gynecology surgery: a systematic review and meta-analysis. Am J Obstet Gynecol. 2016;215(1):21–33. [DOI] [PubMed] [Google Scholar]
- 27.Gobern JM, Novak CM, Lockrow EG. Survey of Robotic Surgery Training in Obstetrics and Gynecology Residency. J Minim Invasive Gynecol. 2011;18(6):755–760. [DOI] [PubMed] [Google Scholar]
- 28.American Urological Association. Robotic Surgery (Urologic) Standard Operating Procedure (SOP) n.d. Available at: https://www.auanet.org/guidelines-and-quality/guidelines/other-clinical-guidance/robotic-surgery-(urologic)-sop (Accessed April 6, 2023).
- 29.Stefanidis D, Huffman EM, Collins JW, Martino MA, Satava RM, Levy JS. Expert consensus recommendations for robotic surgery credentialing. Ann Surg. 2022;276(1):88–93. [DOI] [PubMed] [Google Scholar]