Abstract
Allergic Rhinitis is an immunological inflammatory response of the nasal mucosa to airborne allergens. Although Allergic Rhinitis is not a life-threatening disease, the symptoms of Allergic Rhinitis can be particularly bothersome and disruptive to a patient's sleep and overall quality of life. The coexistence of other allergic conditions like Asthma is very common. No satisfactory treatment is available in modern medicine for this disease. There is a need to search for satisfactory treatment available in another medical system. We present a case of Allergic Rhinitis that was successfully treated with Ayurvedic medicines. Allergic Rhinitis is characterized by watery nasal discharge, nasal obstruction, nasal mucosal pallor, sneezing, and itching in the eyes, palate, and pharynx.
A 18-year-old female patient presented with complaints of sneezing (80–100/day), rhinorrhea (watery discharge from nose), heaviness in the head region, weakness, and loss of concentration hampering daily life activity for one year.
The patient's clinical findings and symptoms were suggestive of Allergic Rhinitis, which is of perennial type. According to Ayurveda diagnosis was done as Vata-Kaphaj Pratishyay. Rajanyadi Churna was given to the patient for 15 days along with Guduchi Kwath (∼Guduchi decoction) followed by Shaman Snehapan (∼internal oleation) with Mahatiktak Ghrita.
The patient experienced a reduction in all the symptoms after 15 days. Allergy markers i.e. Absolute Eosinophil Count reduced to 360 cells/cu mm from 704 cells/cu mm and eosinophils in CBC reduced to 4.1%. The primary complaint of sneezing was significantly reduced to 3–4 times/day after completing the treatment.
Ayurvedic therapeutic interventions other than Nasya (∼Nasal oleation), and Dhoompana (∼medicated smoke) modalities showed encouraging results in managing Allergic Rhinitis in a short duration of time. This approach may be taken into consideration for further treatment and research work for Allergic Rhinitis.
Keywords: Allergic rhinitis, Vata-Kaphaj Pratishyay, Rajanyadi Churna, Absolute eosinophil count
1. Introduction
Allergic Rhinitis (AR) (ICD-10-CM J30.9) is an IgE-mediated response of nasal mucosa. It is a type of nasal mucosal inflammation occurring due to the hyper response to the allergen by the immune system. Allergic Rhinitis is triggered by breathing in tiny particles of allergens. The most common airborne allergens that cause rhinitis are dust mites, pollen and spores, and animal skin, urine, and saliva. Signs and symptoms include nasal obstruction, rhinorrhea, sneezing, nasal pruritus, and other ocular symptoms. Clear fluid is usually seen from the nose [1]. Following allergen exposure, symptoms appear within minutes and affect the quality of life like improper sleep, work productivity, and study [2]. Two clinical types of Allergic Rhinitis have been recognized. (a) Seasonal AR: Symptoms appear in or around a particular season when pollens of a particular plant, to which the patient is hypersensitive, are present in the air. The most common allergens in seasonal allergies are pollens from trees, grasses, or weeds. (b)Perennial AR: - symptoms are present throughout the year. The most common cause of perennial allergies is dust mites, animal dander, cockroaches, or mold. (c) Occupational AR- It is caused by an allergic reaction to a substance present in the workplace, such as grain, wood dust, chemicals or lab animals, etc.
The global prevalence of AR among adults ranges between 10 and 30%, while it was up to 40% in children [3]. The coexistence of AR and asthma is significantly high, the prevalence of coexisting Allergic Rhinitis was found to be 65.24% with the highest prevalence (80%) in southern regions of India [4]. The AR carries a heavy burden of disease as it impacts the quality of life [5]. The main symptoms are nasal obstruction/congestion, sneezing, nasal itching, and rhinorrhea. However nasal obstruction/congestion is the most worrisome symptom which affects sleeping and may cause obstructive sleep apnea because of continuous positive airway pressure [6]. The post-nasal dripping of mucous and watery rhinorrhea are more annoying than the sneezing or nasal itching. In the event of continuous or repeated exposure to allergens, acute phase symptomatology overlaps the late phase.
The recommended treatment options for AR includes (a) for episodic symptoms- oral or nasal H1 antihistamines, (b) for mild symptoms and seasonal or perennial AR-intranasal glucocorticoids, oral or nasal H1 antihistamines or leukotriene receptor antagonist like montelukast and (c) for moderate to severe symptoms-intranasal corticoids alone or with nasal H1 nasal antihistamines, subcutaneous or sublingual allergen immunotherapy (limited to the treatment of grass and ragweed allergy) administration [1]. However, intranasal corticoids have some adverse effects such as nasal irritation, bleeding, and septal perforation [7] and their efficacy for nasal congestion compared to antihistamines is uncertain. Antihistamines are having sedative effects and only give symptomatic relief temporarily. The nasal decongestants are having adverse effects such as nasal bleeding, stinging, burning, and dryness of the nose. It also induces hypertension, tachycardia, insomnia, headache, and irritability if used in the long term. The potential adverse effect of leukotriene antagonist receptors includes upper respiratory tract infection and headache [8]. Subcutaneous and sublingual allergen immunotherapy needs close observation to administer as it can be associated with anaphylaxis. The risk/benefit ratio of immunotherapy is not completely known [9].
Ayurveda is a science of life and it gives rational solutions for chronic ailments. The medicine described in the classical text are having diversity in mode of action and acts on various systems as per Dosha-Dushya vitiation. Pratishyay is a broad term mentioned in Ayurveda in which many types of rhinitis are covered. Characteristically Pratishyay is the disease in which Kapha and other Dosha get dragged towards Vayu and are expelled out through nostrils, is called Pratishyay. AR can be comparable with Vata-Kapha Dosha predominant Pratishyay according to Ayurveda. The signs and symptoms of AR typically indicate the vitiated Vata- Kapha Dosha (Table 1).
Table 1.
Similarities between Allergic Rhinitis and Vata and Kapha predominant Pratishyay
| Allergic Rhinitis | Vata predominant Pratishyay | Kaphaj predominant Pratishyay |
|---|---|---|
| Nasal obstruction | Stuffed and obstructed nose | Difficulty in breathing |
| Paroxysmal sneezing | Repeated sneezing | – |
| Post nasal drip | Cold clear nasal fluid nasal discharge | Sticky nasal discharge |
| Itching in nose and may involves eye, palate or pharynx | – | Itchy sensation in oral cavity |
| Chronic cough | – | Cough |
| Loss of smell | Anosmia | – |
Ghritapana (∼drinking Ghrita) was mentioned in Vataj as well as in Kaphaj Pratishyay. Also, modalities like Nasya (∼nasal oleation), Vamana (∼therapeutic emesis), Lepa (∼ointments), Dhumapana (∼medicated smoking), and Kawal (∼gargling) are mentioned in general for all types of Pratishyay. Rajanyadi Churna is indicated in Grahani (∼ irritable bowel syndrome), Shwas-Kaas (∼asthma and cough), Jwara (∼fever), Kamala (∼jaundice), and pediatric diseases. It is said to be Vatanulomak (∼brings normal Gati to Vata) in action [10] [Uttartantra 2/38–40]. However, Rajanyadi Churna is not directly indicated in Pratishyay (∼rhinitis) but all the ingredients work on Pranavaha Srotas (∼respiratory tract). Guduchi is having predominantly Tikta Rasa (∼bitter taste), Rasayan (∼tissue rejuvenating property), and Aam-pachan (∼alleviates toxins in the body) properties [11]. So Rajanyadi Churna was planned with Guduchi Kwath in AR in the case discussed here.
The present case is of Allergic Rhinitis and treated with polyherbal preparation of Rajanyadi Churna and Guduchi Kwath for 15 days. A good improvement was seen in Absolute Eosinophil Count and symptoms were reduced and patients felt relief from the disease in a short time.
1.1. Case report
An 18 years old female patient came to the Out Patient Section of the Department of Shalakyatantra at Sane Guruji Hospital, Hadapsar, Pune (Maharashtra) in February 2021. The patient had mild deviated nasal septum towards the left side and suffered from symptoms of Allergic Rhinitis (AR) for one year periodically 3–4 times a month lasting for 4–5 days. The patient had noticed that she was having symptoms when she comes in contact with dust and fumes from incense sticks. The patient took allopathic treatment for the same including oral anti-histaminic (Levocetrizine 5 mg with Montelukast 10 mg), decongestant (Oxymetazoline Hydrochloride), antihistaminic nasal sprays (Azelastin 0.1% w/v) and sometimes steroid nasal sprays (Mometasone 0.05%) thrice in a month for at least 3 days in continuation. The patient had taken an antibiotic (Cefuroxime 500 mg) 2 times for 5 days over a period of one year with the above medicines but symptoms reappears soon after she stop the medication. The details of medical history and the complaints at the time of the visit are as follows:
-
•
Left nostril was partially blocked along with bilateral nasal itchy feeling
-
•
Sneezing for up to 1 h–80 to 100 sneezes every day usually in the morning time
-
•
Watery discharge from the nose (rhinorrhea)
-
•
Heaviness in the head region
-
•
Loss of concentration
-
•
Weakness
The patient's symptom score was recorded on SFAR (Score For Allergic Rhinitis) (Annesi-Maesano et al. Allergy 2002) and it was 12 [Appendix 1] confirming the diagnosis.
1.2. Diet history
Dietary history of the patient reveals intake of curd regularly in lunch and twice to thrice intake of milkshakes in a week in the morning. The patient had a daily routine of day sleeping for about an hour after food
1.3. Drug history
The patient had no history of any major medical illness. Menstrual history reveals 4 days of cycle every 28 days. She did not have any history of taking any medications before, during, or after the menstrual cycle.
1.4. Family history
The patient's mother is a known case of asthma and was on an inhaler.
2. Findings
2.1. General examination
The patient had no history of any major illness. Her pulse was 84/minute and her blood pressure was 110/70 mmhg. She was not having any addictions like alcohol, smoking or tobacco chewing, etc. Due to multiple sneezing episodes, her quality of life was affected as she is a student her concentration on study was significantly affected due to the symptoms of AR.
2.2. Local examination
The patient had a mild C-shaped deviated nasal septum to the left side. Mild inferior turbinate hypertrophy in both nostrils. The nasal mucosa has pallor and mild edematous. A clear watery nasal discharge was noted in both nostrils. No other significant anatomical structural deformity was noted. A throat examination revealed no posterior pharyngeal wall congestion, both tonsils were normal, and the uvula is pink in color and rounded.
2.3. Systemic examination
The patient was conscious and oriented about the date, time, and place. Her respiratory and cardiovascular system examinations were normal. Respiratory rate was 18/minute at rest.
The eightfold examination was done and the findings were; Nadi (∼pulse) Vata Pradhan and Pittanubandhi, Mutra (∼urination) and Mala (∼bowel habit) was normal, Jivha (tongue) coated, Shabda (∼speech) was normal, Drik (∼vision) was normal (6/6 both eyes) and Akriti (∼built) was medium.
The tenfold examination revealed Dushya (∼any tissue of the body that gets vitiated) was Rasa and Rakta Dhatu, Desha (∼habitat)- Sadharan, Bala (∼strength)- Madhyam, Kala (∼time)- Sheet Rutu, Agni (∼digestive fire) – Mandya [12], Prakriti (∼body constitution)- Vata-Pitta [13], Vaya (∼age)- Tarun (∼young), Satva (∼psychic condition)- Madhyam, Satmya (∼homologation)- Sheet Jala (∼cold water), Ahar (∼diet)- Salty and sour food items eating twice in a day.
2.4. Vata-Kaphaj Pratishyay Samprapti (etiopathogenesis)
2.5. Investigations
To confirm the diagnosis of Allergic Rhinitis, the patient was advised to do Hemogram with Absolute Eosinophil Count (AEC). The AEC was 704 cells/cumm, Hb-14.7g/Dl, RBCs- 4.84∗103/μL, WBCs- 10.84∗103/μL, Platelets-383∗103/μL, Eosinophils-0.87 (8.1%). The raised value of AEC and eosinophil in blood suggested allergic pathology and eosinophilia. So based on the medical history given by the patient and pathological investigation reports the diagnosis for the patient was Allergic Rhinitis (AR) with mild deviated nasal septum with eosinophilia.
2.6. Diagnostic challenges
Allergic Rhinitis patients have a high prevalence of coexistence of asthma and other allergic conditions like atopic dermatitis and allergic conjunctivitis. Detailed personal medical history with pathological investigation reports helps to confirm the diagnosis. Skin test, nasal provocation test, and nasal cytology are some of the tests that can also confirm the diagnosis of AR. Recurrent nasal allergies may cause sinusitis and sometimes nasal polyp, or in long-standing it can also cause ear disease like serous otitis media. To differentiate and diagnose the condition nasal examination was done with a headlight and PNS (Para Nasal Sinuses) tenderness was checked to rule out any sinus involvement. An otoscopic examination was also done to rule out any associated ear pathology.
2.7. Therapeutic interventions
Written informed consent was taken from the patient before the start of medications. The therapeutic intervention involves Rajanyadi Churna (ETM. Oushadhsala India Ltd. Thrissur, Kerala) in 500 mg dose 3 times a day with Guduchi Kwath (∼medicated decoction prepared freshly with stem of Guduchi purchased from local market standard supplier) 40 ml for initial 15 days followed by Mahatiktak Ghrita (∼medicated ghee) (Arya Vaidya Sala, Kottakal, Kerala) 10 ml empty stomach in the morning followed by Koshna Jala (∼ lukewarm water) for 15 days. During Mahatiktak Ghritapana patient was kept on a light and easily digestible diet like Mudga Yusha (∼green gram soup) along with a normal diet and asked to refrain from curd, milkshakes, and other heavy food items like nonvegetarian.
Details of Rajanyadi Churna ingredients are shown in Table 2.
Table 2.
Ingredients and ayurvedic pharmacodynamics of Rajanyadi Churna
| Sr. no. | Sanskrit name | Common Name | Botanical name | Rasa | Vipaka | Veerya | Action |
|---|---|---|---|---|---|---|---|
| 1. | Rajani | Haldi/Turmeric | Curcuma longa L. | Tikta, Katu | Katu | Ushna | Rasagat Dosha alleviation, Rakta Prasadan, Rasa-Raktagata Aam Visha alleviation, Kapha-Pitta Shaman |
| 2. | Darvi | Devdaru/Deodar | Cedrus deodara Roxb. | Tikta | Katu | Ushna | Vata-Kapha Shaman, Kleda Shoshan(∼absorbs excessive moisture in tissue) |
| 3. | Saral | Cheed/Long- leaved pine/Chir pine | Pinus roxburghii Sarg. | Katu, Tikta, Madhur | Katu | Ushna | Vata-Kapha Shaman |
| 4. | Pippali | Pipali/Long pepper | Piper longum L. | Katu | Madhur | Anushnasheeta | Vata-Kapha Shaman, Rasayan, Aampachan |
| 5. | Bruhti (Laghu) | Choti Kateri, Ringni/Yellow Barried Night shade | Solanum surattense L. | Katu, Tikta | Katu | Ushna |
Vata-Kapha Shaman, Aampachan |
| 6. | Bruhti (Kantakari) | Badi Kateri/Indian Night shade | Solanum indicum L. | Katu, Tikta | Katu | Ushna |
Vata-Kapha Shaman, Indicated in Peenas disease. |
| 7. | Prishnaparni | Pithvan, Dabra | Uraria picta DC. | Madhur, Tikta | Madhur | Ushna | Tridoshaghna |
| 8. | Shatavah | Soyo/Indian dill | Anethum sowa Roxb. | Katu, Tikta | Katu | Ushna | Vata-Kapha Shaman |
2.8. Follow-ups and outcomes
The patient reported that she was doing well and experiencing health and did not have any previous symptomatology of AR, while she was not on any kind of medication for the last 15 days. The effect of medicines on hematological parameters is depicted in Table 3 and follow-up was taken up to one month after starting medication (Table .4)..
Table 3.
Effect on hematological parameters.
| Parameter | Before Treatment | After Treatment |
|---|---|---|
| Haemoglobin (g/dL) | 14.7 | 14 |
| RBCs (103/μL) | 4.84 | 4.64 |
| WBCs (103/μL) | 10.84 | 7.65 |
| Eosinophils (%) | 8.1 | 4.1 |
| Absolute Eosinophil Count | 704 | 360 |
| Platelets (103/μL) | 383 | 435 |
Table 4.
Follow up time line.
| Date | Treatment Plan | Aushadhi Sevan Kaal | Symptoms observed on follow up |
|---|---|---|---|
| 01/02/2021 | Rajanyadi Churna 500 mg with Guduchi Kwath 40 ml | Morning-Afternoon-Evening After breakfast, lunch and dinner |
Sneezing (80–100/day), nasal obstruction, nasal itchy sensation, rhinorrhea, heaviness in head, and loss of concentration on work |
| 07/02/2021 | Continue all medication | Same | Sneezing (40–50/day), nasal obstruction, rhinorrhea, nasal itchy sensation, improvement in the concentration of work due to reduced sneezing. |
| 12/02/2021 | Continue all medication for 3 days | Same | Sneezing (20–25), mild nasal obstruction, |
| 15/02/2021 | Mahatiktak Ghrita 10 ml with lukewarm water | Morning empty stomach | The number of sneezing was reduced to 2–4 per day and improvement in all symptoms noted. |
| 28/02/2021 | Observation only | – | No increase in symptoms |
| 15/03/2021 | Observation only | – | Patient stable with no any major symptom |
3. Discussion
AR is an acute condition of nasal mucosa associated with type-1 hypersensitivity reaction which involves periodic attacks of sneezing and watery discharge from the nose. When the substances like dust, pollen, mites, or fumes enter through the nose, the immune system overreacts with the production of antibodies that attacks the allergen producing the symptomatology of AR. Due to subclinical bronchospasm, the patient may experience tightness in the chest. AR is the commonest chronic ailment in ENT practice having multifactorial causation with multifocal manifestation. Industrialization and urbanization are responsible for environmental pollution and increased the incidence rate of AR. Genetic predisposition, local sensitivity of nasal mucosa, and IgA deficiency are some of the reported predisposing factors for AR. The dusty environment, crowding, use of air conditioners, dusty carpets, curtains, bookshelves, and occupational hazards play a significant role in precipitating allergic responses in residential or workplace conditions. An aerobiological flora contributes to AR as an etiological factor and manifests seasonal and perennial allergic rhinitis [14]. The second to fourth decade of life is having the highest prevalence of allergic rhinitis which subsides gradually in the later stage of life [15].
AR imposes a significant financial burden and affects the quality of life of an individual [5]. Treatment modalities for AR include avoidance of allergens, treatment with drugs and if drugs fail to control the disease immunotherapy is the choice of treatment. Drugs for treating Allergic Rhinitis include Antihistaminic, Sympathomimetic drugs, oral and topical corticosteroids, and leukotriene receptor antagonists. Among the several effective treatment modalities of AR, some of them are target receptors of bioactive mediators or inflammation. It has been reported that one-third of children and two third of adults having AR are experiencing insufficient relief with pharmacotherapy alone. Allergen immunotherapy is the potential curative therapy for seasonal and perennial AR. But these are not cost-effective and patient needs daily medication [16].
3.1. Vyadhikshamatva and allergic rhinitis
Vyadhikshamatva is a complex concept encompassing multiple factors, including Vyadhibala Virodhitva and Vyadhi Utapadaka Pratibandhakatva (∼resistance to the manifestation of the disease), dependent on Ojus (∼essence of body tissue) and its subtypes. It extends beyond mere immunity and refers to the body's capacity to resist various diseases, maintain Dosha (∼the functional principles that govern the body), Dhatu (∼tissues), and Mala (∼the waste products of metabolism) balance, and sustain overall health. Immunity, as a component of Vyadhikshamatva, plays an important role in diseases like AR, where local and systemic factors cause hypersensitivity reactions.
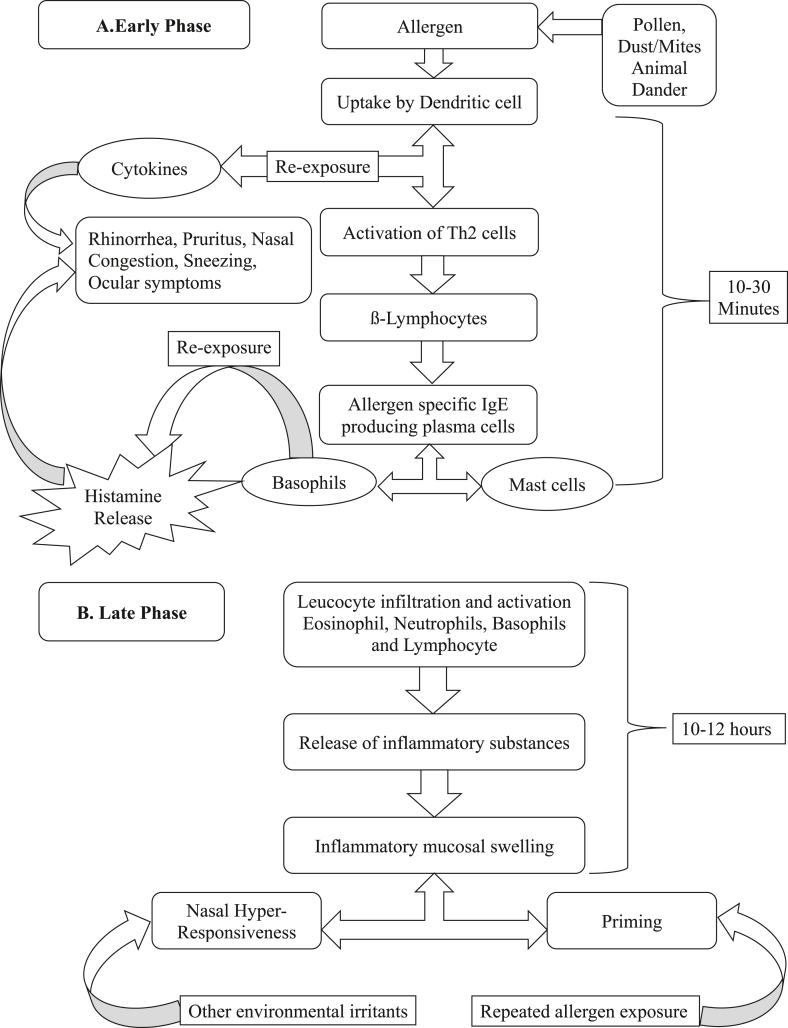
3.2. Pathology
The hypersensitivity reactions in AR are caused due to the substances, such as pollens, animal dander, food articles, and various drugs. The IgE produced in large quantities binds to the allergen on the mast cell surface and produces an immediate hypersensitivity reaction followed by several mediators’ release. The cascade involves the formation of IgE antibodies, binding with basophils and mast cells, the process of degranulation, and the release of pharmacologically active mediators in a very short time. This results in the symptomatology of allergic rhinitis, nasal mucosal edema, eosinophil infiltration, nasal gland secretion, etc. [17].
Clinically allergic response occurs in two phases as shown in Fig. 1 A & B [Source of diagrammatic presentation - Allergic Rhinitis: A Clinical and Pathophysiological Overview. Front Med (Lausanne). 2022].
Fig. 1.
A & B. The early and late phase response in AR.
A case of a female patient, who suffered from AR is reported here. Allergic Rhinitis is primarily associated with the vitiation of the Vata- Kapha Doshas in this case. Rajanyadi Churna was administered to the patient for 15 days along with Guduchi Kwath as Anupana (∼co-administers with medicines) followed by Shaman Snehapan (∼internal oleation) administered for 15 days.
Rajanyadi Churna is an Ayurvedic classical formulation mentioned in Ashtanga Hridaya which is indicated in the treatment of digestive disorders, fever, jaundice, anemia, and asthma [10. Uttartantra 2/38–40]. Although Rajanyadi Churna classically not indicated in Pratishyay but when we think about Doshas involved in Pratishyay and type 1 hypersensitivity (altered immune response), Tikta Rasa [10. Sutrasthana 10/14–16] Pradhan Dravya is the choice of therapeutic intervention to treat the symptomatology of AR which is Vata- Kapha predominant in nature.
Ingredients of Rajanyadi Churna mentioned in Table 2 have Tikta Rasa and Ushna Veerya properties which makes this Churna suitable to pacify Vata-Kapha predominant Pratishay. All the ingredients of Rajanyadi Churna are reported to have an anti-allergic, anti-inflammatory, anti-histaminic, and anti-asthmatic properties elaborated in Table 5.
Table 5.
Pharmacological action of ingredients of Rajanyadi Churna
| Sr. no. | Name of ingredient | Action |
|---|---|---|
| 1. |
Rajani Curcuma longa L. |
|
| 2. |
Darvi Cedrus deodara Roxb. |
|
| 3. |
Saral Pinus roxburghii Sarg. |
|
| 4. |
Pippali Piper longum L. |
|
| 5. |
Bruhti (Laghu) Solanum surattense L. |
|
| 6. |
Bruhti (Kantakari) Solanum indicum L. |
|
| 7. |
Prishnaparni Uraria picta DC. |
|
| 8. |
Shatavha Anethum sowa Roxb. |
|
The dosage of Churna is one Karsha i.e. 10 gm [27]. However, considering the palatability here the patient was given the dose of 500 mg three times a day with Guduchi Kwath (40 ml) as Anupana [10. Sutrasthan 8/51]. Because of Mandagni (∼low digestive fire) [28] [Chikitsasthana 15/50-51] of a patient and Aam-Visha [10. Sutrasthana8/13–14] associated with the disease, Guduchi (Tinospora cordifolia) [29] was used in the form of decoction as a compliant with Rajanyadi Churna as it is Agni Deepak (∼ boost digestive fire and metabolism), Rasayani (∼ maintain circulatory channels to produce optimum nutrition/tissue rejuvenation and quality of Rasa Dhatu), Tridoshaghni (∼pacifies all the three biological humors i.e. Vata, Pitta, Kapha). The T. cordifolia (TC) is having an immunostimulant effect and the primary target is believed to be the macrophages which play an important role in the generation of the immune response. TC was also demonstrated to decrease the histamine-induced bronchospasm in the guinea pig model, decreased the capillary permeability in the mice model, and decreased the number of disrupted mast cells in rat models. Some of the herbs-mineral preparation showed promising anti-allergic activity in cases of rhinitis without any side effects for long-term use. Guduchi as a single drug therapy also been shown to increase the leucocyte count. The TC extract is known to alleviate the symptoms of AR [30].
After pacifying the Aam- Visha, the patient was given Shaman Snehapan [10. Sutrasthana 16/17–19] with Mahatiktak Ghrita [28. Chikitsasthan 7/142-150] in 10 ml dose for the prevention of the disease and stabilizing altered immune response occurs in AR. However, Mahatiktak Ghrita is a polyherbal medicated Ghrita having one of the main ingredients as Amalaki Swaras (juice of Emblica officinalis). Amalaki has a variety of pharmaco-therapeutic actions such as immunomodulatory, anti-inflammatory, antioxidant, free radical scavenging, and cytoprotective. It is reported to stimulate humoral and cell-mediated immunity along with macrophage phagocytes, increase the percent lymphocyte distribution, and delayed-type hypersensitivity [31]. Mahatiktak Ghrita ingredients are mainly Tikta Rasa Pradhan (∼bitter taste). Tikta Rasa is Amapachaka and removes toxins from the body. Ghrita is Agnivardhak (∼ boosts digestive fire) and gives strength to body tissue.
In a nutshell, the causative factors of AR increase the Saam Kapha and Vata which gives rise to the symptomatology of AR. The Dravya does its functions by any five modalities namely Rasa, Guna, Veerya, Vipaka, and Prabhava, hence all these five modalities are Gunas by which a Dravya performs its Karma (∼action). All Oushadh Dravyas (∼medicinal Dravya) predominantly act by Veerya. A Dravya performs its action by primarily interacting with a specific structure in the body called an Adhikaran (∼receptor) [32]. It is the Vishishta Samarthya Sampanna Guna (∼potent and efficient most factor) called Veerya responsible for the efficacy of medicine against the pathogenesis.
Rajanyadi Churna is a polyherbal combination predominantly having Tikta Rasa and Ushna Veerya properties having the action of pacifying Saam Kapha Dosha which is responsible for causing Allergic Rhinitis. The synergist effect of the ingredients of Rajanyadi Churna thus subsides the disease. Allergens are substances that cause the immune system to respond abnormally, leading to symptoms including sneezing, itching, inflammation, and asthmatic symptoms. Imbalanced gut microbiota can result in a hyperactive immune system, which could worsen allergic reactions and respiratory symptoms. However, a healthy gut microbiota can help to control the immune system and lessen the chance of an excessive allergic reaction. This is due to the fact that the gut microbiota plays a key role in aiding the immune system to differentiate between harmful and harmless compounds [33]. As stated in the published case report, it strengthens the hypothesis of gut mediated/associated immune response [34]. Since Rajanyadi Churna has Deepan- Pachan (∼digestive and appetizing) properties and is indicated in digestive tract disorders, it has given results in immune-related diseases like AR.
During the initial 15 days of treatment, the patient was asked to refrain from milk and milk products, bakery products, and oily and spicy food which in general Guru, and Snigdha in nature, as these types of food can elevate the allergic condition due to its Abhishyandi (∼slowing down of cellular metabolism) nature.
After taking the Ayurvedic treatment patient was feeling healthy and did not experience the symptoms again when follow up taken after 15 days without any medication. Reports done before and after treatment shows evidence of the improvement in eosinophil count which tends to be high in allergic conditions, returns to normal suggesting altered immune response stabilization with Ayurveda medicines.
A further case study in such cases is required to substantiate the results in AR as reproducibility establishes the treatment protocol and gives a better and more in-depth understanding of the Ayurvedic perspective of disease.
3.3. Patient's perspective
Initially, when the patient visited first time to the outpatient department, she was very annoyed with the symptoms of AR particularly with multiple sneezing in a day affecting her quality of life and loss of concentration at work. She needs to take antihistamines every time causing sedation during study hours. But when she started to follow the Ayurvedic treatment her symptomatology was relieved in a short span of time and feels confident about the Ayurveda medicines. Her own perspective in the local language (∼Marathi) was uploaded as supplementary material.
3.4. Informed consent
A written informed consent has been taken from the patient for publication of the results for the sake of knowledge to the scientific society.
4. Conclusion
Allergic Rhinitis has annoying symptoms that have a greater impact on a patient's quality of life. It creates a significant amount of financial burden on society around the globe. Modern medicine lags in giving a permanent solution for AR. Ayurveda has a certain potential to tackle chronic allergic diseases. The present case of AR was treated with Rajanyadi Churna with Guduchi Kwath and in a short span of time patient showed improvement in symptomatology and hematological parameters.
5. Scope for further study
The treatment protocol of AR in modern medicine starts with pharmacotherapy which is insufficient and many a time patient needs to shift to immunotherapy. Ayurvedic formulations which work efficiently on Pranavaha (∼respiratory tract) and Annavaha(∼gastro-intestinal tract) Srotas need to evaluate through randomized controlled clinical trials on the patients of AR.
Sources of funding
None.
Conflict of interest
The authors declare they have no conflict of interest to disclose.
Author contribution
Rochan Sharma – Treatment design, Ayurvedic thought process, data collection, manuscript writing, and references collection. Pravin Bhat- Conceptualization and Design, manuscript writing, reference collection, critical editing, supervision, and final approval.
Acknowledgement
None.
Footnotes
Peer review under responsibility of Transdisciplinary University, Bangalore.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jaim.2023.100740.
Appendix A. Supplementary data
The following is the Supplementary data to this article.
References
- 1.Wheatley Lisa M., Togias Alkis. Clinical practice. Allergic rhinitis. N Engl J Med. 2015;372(5):456–463. doi: 10.1056/NEJMcp1412282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Meltzer E.O., Blaiss M.S., Derebery M.J., Mahr T.A., Gordon B.R., Sheth K.K., et al. Burden of allergic rhinitis: results from the Pediatric Allergies in America survey. J Allergy Clin Immunol. 2009 Sep;124(3 Suppl):S43–S70. doi: 10.1016/j.jaci.2009.05.013. Epub 2009 Jul 9. PMID: 19592081. [DOI] [PubMed] [Google Scholar]
- 3.Mims J.W. Epidemiology of allergic rhinitis. Int Forum Allergy Rhinol. 2014 Sep;4(Suppl 2):S18–S20. doi: 10.1002/alr.21385. PMID: 25182349. [DOI] [PubMed] [Google Scholar]
- 4.Jaggi V., Dalal A., Ramesh B.R., Tikkiwal S., Chaudhry A., Kothari N., et al. Coexistence of allergic rhinitis and asthma in Indian patients: the CARAS survey. Lung India. 2019 Sep-Oct;36(5):411–416. doi: 10.4103/lungindia.lungindia_491_18. PMID: 31464213; PMCID: PMC6710977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meltzer E.O. Allergic rhinitis: burden of illness, quality of life, comorbidities, and control. Immunol Allergy Clin. 2016 May;36(2):235–248. doi: 10.1016/j.iac.2015.12.002. Epub 2016 Mar 4. PMID: 27083099. [DOI] [PubMed] [Google Scholar]
- 6.Georgalas C. The role of the nose in snoring and obstructive sleep apnoea: an update. Eur Arch Oto-Rhino-Laryngol. 2011 Sep;268(9):1365–1373. doi: 10.1007/s00405-010-1469-7. Epub 2011 Feb 22. PMID: 21340561; PMCID: PMC3149667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thornhill S.M., Kelly A.M. Natural treatment of perennial allergic rhinitis. Alternative Med Rev. 2000 Oct;5(5):448–454. PMID: 11056414. [PubMed] [Google Scholar]
- 8.Glacy J., Putnam K., Godfrey S., Falzon L., Mauger B., Samson D., et al. Agency for Healthcare Research and Quality (US); Rockville (MD): 2013 Jul. Treatments for seasonal allergic rhinitis. [Internet] Report No.: 13-EHC098-EF. PMID: 23946962. [PubMed] [Google Scholar]
- 9.Durham S.R., Penagos M. Sublingual or subcutaneous immunotherapy for allergic rhinitis? J Allergy Clin Immunol. 2016 Feb;137(2):339–349.e10. doi: 10.1016/j.jaci.2015.12.1298. PMID: 26853126. [DOI] [PubMed] [Google Scholar]
- 10.Kaviraj Atridev Gupta. 6th ed. Chaukhambha Prakashan Varanasi; Reprint: 2011. Ashtang Hridaya of Srimadvagbhata, ‘Vidyotini’ Hindi Commentary. [Google Scholar]
- 11.Chunekar Dr K.C. 8–10. Guduchyadi Varga; 2002. Bhavaprakash Nighantu of Bhavmisra, chaukhambha Bharti academy Varanasi; p. 269. Reprint. [Google Scholar]
- 12.Eswaran H.T., Kavita M.B., Tripaty T.B., Shivakumar Formation and validation of a questionnaire to assess Jāṭharāgni. Ancient Sci Life. 2015 Apr-Jun;34(4):203–209. doi: 10.4103/0257-7941.159829. PMID: 26283805; PMCID: PMC4535068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rastogi S. Development and validation of a prototype Prakriti analysis Tool (PPAT): inferences from a pilot study. Ayu. 2012 Apr;33(2):209–218. doi: 10.4103/0974-8520.105240. PMID: 23559792; PMCID: PMC3611641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hazarika P., Nayak D., Balakrishna R. 4th ed. CBS Publishers & Distributors; New Delhi: 2019. Allergic Rhinitis, Chapter 34 . Textbook of ear, nose, throat and head & neck surgery (theory, clinical & practical) p. 249. [Google Scholar]
- 15.Yonekura S., Okamoto Y., Horiguchi S., Sakurai D., Chazono H., Hanazawa T., et al. Effects of aging on the natural history of seasonal allergic rhinitis in middle-aged subjects in South chiba, Japan. Int Arch Allergy Immunol. 2012;157(1):73–80. doi: 10.1159/000324475. Epub 2011 Sep 6. PMID: 21912176. [DOI] [PubMed] [Google Scholar]
- 16.Bernstein D.I., Schwartz G., Bernstein J.A. Allergic rhinitis: mechanisms and treatment. Immunol Allergy Clin. 2016;36(2):261–278. doi: 10.1016/j.iac.2015.12.004. May. Epub 2016 Mar 10. PMID: 27083101. [DOI] [PubMed] [Google Scholar]
- 17.Warren Levison, Review of medical microbiology and immunology. 14th ed.: McGraw Hill Education, p.569.
- 18.Wu S., Xiao D. Effect of curcumin on nasal symptoms and airflow in patients with perennial allergic rhinitis. Ann Allergy Asthma Immunol. 2016 Dec;117(6):697–702.e1. doi: 10.1016/j.anai.2016.09.427. Epub 2016 Oct 24. PMID: 27789120. [DOI] [PubMed] [Google Scholar]
- 19.Altıntoprak N., Kar M., Acar M., Berkoz M., Muluk N.B., Cingi C. Antioxidant activities of curcumin in allergic rhinitis. Eur Arch Oto-Rhino-Laryngol. 2016 Nov;273(11):3765–3773. doi: 10.1007/s00405-016-4076-4. Epub 2016 May 4. PMID: 27146978. [DOI] [PubMed] [Google Scholar]
- 20.Saab A.M., Gambari R., Sacchetti G., Guerrini A., Lampronti I., Tacchini M., et al. Phytochemical and pharmacological properties of essential oils from Cedrus species. Nat Prod Res. 2018 Jun;32(12):1415–1427. doi: 10.1080/14786419.2017.1346648. Epub 2017 Jul 3. PMID: 28670915. [DOI] [PubMed] [Google Scholar]
- 21.Kaushik P., Kaushik D., Khokra S.L. Ethnobotany and phytopharmacology of Pinus roxburghii Sargent: a plant review. J Integr Med. 2013 Nov;11(6):371–376. doi: 10.3736/jintegrmed2013053. PMID: 24299601. [DOI] [PubMed] [Google Scholar]
- 22.Kaushik D., Kumar A., Kaushik P., Rana A.C. Analgesic and anti-inflammatory activity of Pinus roxburghii Sarg. Adv Pharmacol Sci. 2012;2012 doi: 10.1155/2012/245431. Epub 2012 Jun 14. PMID: 22761611; PMCID: PMC3384912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aswar U., Shintre S., Chepurwar S., Aswar M. Antiallergic effect of piperine on ovalbumin-induced allergic rhinitis in mice. Pharm Biol. 2015;53(9):1358–1366. doi: 10.3109/13880209.2014.982299. Epub 2015 Apr 14. PMID: 25868617. [DOI] [PubMed] [Google Scholar]
- 24.Kaunda J.S., Zhang Y.J. The Genus Solanum: an ethnopharmacological, phytochemical and biological properties review. Nat Prod Bioprospect. 2019 Apr;9(2):77–137. doi: 10.1007/s13659-019-0201-6. Epub 2019 Mar 12. PMID: 30868423; PMCID: PMC6426945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nagarkar B., Nirmal P., Narkhede A., Kuvalekar A., Kulkarni O., Harsulkar A., et al. Comparative evaluation of the anti-inflammatory potential of medicinally important plants. Int J Pharm Pharmaceut Sci. 2013;5(3):239–243. [Google Scholar]
- 26.Saleh-E-In M.M., Choi Y.E. Anethum sowa Roxb. ex Fleming: a review on traditional uses, phytochemistry, pharmacological and toxicological activities. J Ethnopharmacol. 2021 Feb 25 doi: 10.1016/j.jep.2021.113967. Epub ahead of print. PMID: 33640440. [DOI] [PubMed] [Google Scholar]
- 27.Murthy K.R.Srikantha. Chaukhambha Orientalia, Varanasi; 2009. Sharangdhara Samhita of Sharangdhara, Madhyam khand; p. 84. [Chapter 6], Verse. 1. Reprint. [Google Scholar]
- 28.Dr, Chaturvedi Gorakhnath, Pandit Kashinath Shastri . Chaukhambha Bharti Academy; Varanasi, Reprint: 2016. Charak Samhita of Agnivesh revised by Charak and Dradhbala, Vidyotini Hindi commentary, Chikitsasthan. [Google Scholar]
- 29.Dr Gangasahay Pandey. Bhavprakash Nighantu of Bhavmishra, Guduchyadi Varga, Verse. 6-10. Chaukhambha Prakashan, Varanasi. 5th ed. p. 269.
- 30.Badar V.A., Thawani V.R., Wakode P.T., Shrivastava M.P., Gharpure K.J., Hingorani L.L., et al. Efficacy of Tinospora cordifolia in allergic rhinitis. J Ethnopharmacol. 2005 Jan 15;96(3):445–449. doi: 10.1016/j.jep.2004.09.034. Epub 2004 Nov 23. PMID: 15619563. [DOI] [PubMed] [Google Scholar]
- 31.Yadav S.S., Singh M.K., Singh P.K., Kumar V. Traditional knowledge to clinical trials: a review on therapeutic actions of Emblica officinalis. Biomed Pharmacother. 2017 Sep;93:1292–1302. doi: 10.1016/j.biopha.2017.07.065. Epub 2017 Jul 23. PMID: 28747010. [DOI] [PubMed] [Google Scholar]
- 32.Krishnan R. Evidence-based Ayurveda and rational prescribing. 2nd ed. Vision Graphic Publication; Trivandrum, Kerala: 2017. The Pharmacodynamics and kinetics in Ayurveda; p. 19. [Chapter 3] [Google Scholar]
- 33.Huang J., Zhang J., Wang X., Jin Z., Zhang P., Su H., et al. Effect of probiotics on respiratory tract allergic disease and gut microbiota. Front Nutr. 2022 Feb 22;9 doi: 10.3389/fnut.2022.821900. PMID: 35295917; PMCID: PMC8920559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nakanekar A., Kulkarni S., Khobarkar P., Belsare M. Integrative management of critical case of Covid 19 with Ayurvedaand Modern medicine: a case report. J Ayurveda Integr Med. 2021 Jul 28 doi: 10.1016/j.jaim.2021.07.012. Epub ahead of print. PMID: 34334979; PMCID: PMC8315940. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.