Abstract
Purpose
The purpose of this study was to assess patient satisfaction and identify risk factors for dissatisfaction after anterior stabilised conventional total knee arthroplasty (TKA) without patellar resurfacing, using the Goodman score.
Methods
We conducted a cross-sectional study using data from our institutional database from 1 January 2018 to 1 March 2021. Patients who underwent TKA with the Vanguard® Cruciate Retaining Anterior Stabilized Knee System (Zimmer Biomet, Warsaw, Indiana, USA) without patellar replacement were included. Patients with other bearing surfaces (posterior stabilised or medial congruent) or diagnosed with infection or instability were excluded. Patients' reported outcomes, body mass index (BMI), passive range of motion, the timed up-and-go test, sit-up test, and algometry were assessed. Patients were also asked if they had anterior knee pain. Satisfaction was assessed using the Goodman scale, and logistic multivariate regression was used to identify variables associated with dissatisfaction and perceived improvement in quality of life.
Results
A total of 131 TKA patients were included in the study. The median satisfaction score was 100 (interquartile range [IQR], 87.5 to 100), with the 75-point threshold at the 90th percentile according to Section A of Goodman. Section B of Goodman showed that 113 TKA patients (86.26%) reported "great improvement" or "more than I ever dreamed." Multivariate logistic regression revealed that anterior knee pain (OR 5.16, 95% CI 1.24 to 21.39), the sit-up test (OR 0.63, 95% CI 0.49 to 0.81), and BMI (OR 0.84, 95% CI 0.70 to 0.99) were significantly associated with patient dissatisfaction and a worse perceived improvement in quality of life. The receiver operating characteristics curve for the models had areas under the curve of 0.83 (95% CI 0.69 to 0.97) and 0.82 (95% CI 0.70 to 0.94), respectively.
Conclusion
Anterior stabilised TKA without patellar resurfacing can achieve 90% satisfaction and 86% improvement in quality of life. To improve these results, it is essential to prevent and treat anterior knee pain and enhance quadriceps strength.
Level of evidence
Level III (retrospective cohort study).
Keywords: Satisfaction, Total knee replacement, Total knee arthroplasty, Anterior knee pain, Patellar resurfacing, Patellar preservation, Anterior stabilized
Introduction
Total knee arthroplasty (TKA) is a common procedure aiming to restore function and alleviate pain in patients with end-stage knee osteoarthritis [48]. The impact of this procedure on quality of life has led to the adoption of the number of TKAs per 100,000 inhabitants as a quality indicator of health standards by the Organisation for Economic Co-operation and Development (OECD) [46].
Patient satisfaction and improvement in quality of life are the primary outcomes to be achieved after TKA. Recently, Goodman et al. developed a reliable scale to objectively measure both outcomes, which has been validated and adapted for Spanish speakers [7, 18]. Historically, dissatisfaction rates were set at 20% [31, 55]. However, advancements in pain management, implant technologies, and surgical understanding have raised satisfaction levels to nearly 90%, according to recent reports [12].
Currently, numerous technical controversies exist, such as the choice of polyethylene insert and the necessity of performing patella resurfacing [57]. Many studies have shown no significant differences in anterior knee pain incidence, functional outcomes, and range of motion (ROM) after patellar resurfacing [19, 21]. Additionally, the likelihood of reducing knee pain after TKA by performing secondary patellar replacement is similar to chance [49]. The advantages of not replacing the patella include preserving bone stock, avoiding patellar complications related to cuts—such as fracture or malalignment of the insert—and saving time [49]. Recent literature has not demonstrated a significant difference between cruciate retaining (CR) or posterior stabilised (PS) techniques, leaving the decision to the surgeon's preferences [51].
Our institution is a university hospital that led the TKA volume in our country from 2004 to 2019 [4]. The most common TKA procedure in our university hospital involves not replacing the patella and using a CR anterior stabilised insert. At present, the quality and quantity of satisfaction reports after TKA are limited, with study heterogeneity [26] complicating data pooling, making it difficult to extrapolate these results to all TKAs. The purpose of this study was to determine satisfaction following an anterior stabilized conventional total knee replacement without patellar resurfacing, using the Goodman score, and to identify risk factors for dissatisfaction after TKA. We hypothesize that this cohort will achieve a higher level of satisfaction than the historical average of 80%, and we anticipate identifying at least one factor that can predict satisfaction.
Materials and methods
A cross-sectional study was designed and approved by our local ethics committee and was conducted in accordance with the declaration of Helsinki. The institutional database was reviewed from 1 January 2018 to 1 March 2021. Patients were invited to participate in the study if they had undergone TKA using the Vanguard® Cruciate Retaining Anterior Stabilised Knee System (Zimmer Biomet, Warsaw, Indiana, USA) without patellar replacement. Patients were excluded if another bearing surface was used (PS or medial congruent) or if they had a diagnosis of infection or instability. TKA was performed using a medial parapatellar approach and eversion of the patella. Neither a tourniquet nor wound drainage was used. Extra or intramedullary guidance for tibial alignment was used according to the surgeon's preference, while intramedullary guidance for femoral alignment was used in all cases. The epicondylar axis and the Whiteside line were used for rotational alignment on the femoral component; conversely, the posterior cruciate ligament to tibial tubercle axis and the anterior cortex were used as reference points for rotation on the tibia. The surgeons in this study never replaced the patella and always performed patellar denervation.
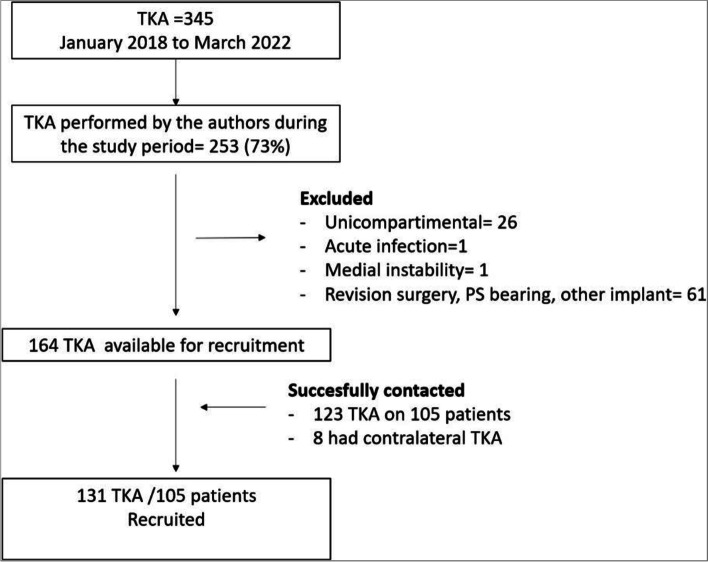
A total of 345 TKAs were identified. The four surgeons who participated in the study carried out 253 of them (73%). Twenty-six of the 253 (10%) were unicompartmental arthroplasties, and 61 (24%) TKAs were not included because they were revision surgeries, or a PS bearing was used. One hundred sixty-six TKAs were identified for recruitment, of which one patient was excluded for acute infection (0.6%) and one (0.6%) for medial instability. Finally, 123 of 164 TKAs (75%), corresponding to 105 patients, were successfully contacted and agreed to participate in the study. All of them received counselling and then signed written informed consent to participate. If a patient had a contralateral TKA performed before the time frame of this study at our institution using the same model, both TKAs were recruited. This occurred in eight patients (8/105; 7.6%), totalling 131 recruited TKAs in 105 patients (Fig. 1).
Fig. 1.
Flow chart. Abbreviations: TKA, total knee arthroplasty; PS, posterior stabilised
All evaluations were performed by the same physiotherapist (MaB) from March 2022 to September 2022. The assessment included patients' reported outcomes, body mass index (BMI), passive ROM, the timed up-and-go (TUG) test, sit-up test, and algometry. Additionally, all patients were asked if they experienced AKP during their daily activities, regardless of intensity and frequency (daily or weekly). The response was recorded as either yes or no.
The principal outcome of the study was satisfaction and patients' perceived improvement in their quality of life after TKA, using the Goodman scale, which has been validated for TKA and adapted for Spanish speakers [7, 18, 56]. This scale has two sections. The first section ("A") aims to evaluate satisfaction using four questions ranging from 0 "very dissatisfied" to 4 "very satisfied." These four questions can be summarised by calculating the average score and multiplying by 25, with the minimum score being 0 "very dissatisfied" and the maximum score 100 being "very satisfied." A score of at least 75 was considered satisfactory as it represents an average of 3 on the four questions. The second section ("B") aims to evaluate the degree of improvement perceived by the patient compared to their pre-surgery status. This item is a Likert scale from 1 "worst" to 6 "better than I ever dreamed." Furthermore, patients were asked to complete the Western Ontario and McMaster Universities Arthritis Index (WOMAC), Kujala, and Knee Injury and Osteoarthritis Outcome Score (KOOS) questionnaires to assess their quality of life.
The passive ROM was assessed with the participant in the supine position, with hips in the neutral position. A 360° universal plastic goniometer with a 30-cm movable arm and a scale of 1° increments (Baseline®, Chattanooga Group, Inc, Hixson, Tennessee, USA) was used for all measurements. The stationary arm was placed along the femur to the greater trochanter. The movement arm was placed along the fibula to the lateral malleolus. The fulcrum was visually positioned at the trans epicondylar axis of the knee joint. For knee flexion, the heel of the foot was required to be in contact with the examination couch during the assessment. For passive knee extension, a cylindrical roll was placed underneath the heel of the foot to allow the knee to extend as much as possible. Both knees were assessed [47].
The TUG test corresponds to the time it takes for a patient to get up from a chair, walk 1.5 m in a straight line, turn around, and return (covering a total distance of 3 m). The time was recorded in seconds [22]. For the sit-up test, the patient was asked to complete as many sit-and-stand cycles as quickly as possible in 30 s with their arms crossed over their chest. Then, the muscle power was estimated using a previously published formula. [2, 45]: The algometry, the patient was asked to kneel over a weighting machine three times, and the maximum kilograms that the patient tolerated was recorded and compared with the contralateral knee.
Continuous variables were summarised as median (50th percentile), range, and IQR (25th percentile to 75th percentile). Categorical variables were summarised using frequency and percentages. A comparison was performed for all variables between patients with one-sided TKA and those with bilateral TKA.
The Goodman scale was the primary outcome [20]. A quantile regression was estimated to determine the variables that could predict the score of Section A. The pseudoR2 was used to determine the ability to predict. For those variables with a significant coefficient (p < 0.05) and a pseudoR2 above 0.15, a bootstrapped multivariate quantile regression with 200 repetitions using stepwise was estimated. Additionally, the score was dichotomised using the score 75 as the threshold, and a multivariate logistic regression was estimated. After logistic regression, the goodness of fit test was performed to determine if the model was adequately estimated.
Section "B" was dichotomised into two categories for analysis purposes: answers from 1 to 4 were classified as "Same or Worse", and answers from 5 to 6 as "Much better". Then, a logistic regression was estimated to determine risk factors for "Same or Worse". For those variables with a significant odds ratio (OR), the area under the receiver operating characteristic (ROC) curve was estimated to evaluate the ability to discriminate. A bootstrapped multivariate logistic regression (MLR) with 200 repetitions using stepwise was performed. After the MLR, the goodness of fit test, with a maximum of 10 group covariances, was conducted to determine if the model was adequately estimated.
Results
A total of 131 TKAs were recruited from 105 patients, of whom 46 were men (43.81%). The median age at surgery was 66 years (range, 47 to 88; IQR, 62 to 71), 78 TKAs were on the right side (59.54%), and 13 patients underwent bilateral TKA. The median follow-up was 2.74 years (range, 1.01 to 5.1; IQR, 1.71 to 3.85).
No clinically relevant difference in functional evaluation was found between patients with one-sided TKA and bilateral TKA (Table 1); thus, no inferential statistics were performed. The median ROM was 115, with a median difference of -5 degrees to the contralateral side, which increased by five degrees more in the case of unilateral TKA (Table 1). Two patients required a second intervention; one underwent mobilisation under anaesthesia and arthroscopic debridement for arthrofibrosis, with a final ROM of 100 degrees and a side-to-side difference of 28 (unilateral TKA); their satisfaction was 100 (Goodman A) and improvement 6 ("most I ever dreamed"). The other required selective embolisation for recurrent hemarthrosis and reported a score of 100 in Goodman A and 5 in Section B.
Table 1.
Clinical evaluations for the total cohort, one-sided TKA, and bilateral TKA
| Total patients | One-side TKA | Bilateral TKA | |
|---|---|---|---|
| Flexion | 112 (82 to 135) (106 to 120) | 112 (82 o 135) (106 to 120) | 111 (90 to 127) (105 to 119) |
| -Diff | -5 (-42.3 to 21) (-12 to 2) | -10.4 (-42 to 21) (-14 to -4) | N/A |
| EXT | 2 (-12 to 16) (0 to 6) | 2 (-6 to 16) (0 to 6) | 3 (-12 to 15) (0 to 6) |
| -Diff | 0 (-12 to 16) (-2 to 4) | 2 (-8 to 16) (0 to 6) | N/A |
| ROM | 115 (80 to 147) | 116 (80 to 147) (108 to 124) | 115 (91 to 132) (107 to 122) |
| -Diff | -5 (-44 to 25) | -9 (-44 to 25) (-15 to 3) | N/A |
| Algometry | 11 (0 to 36) (7 to 14) | 10 (0 to 25) (6 to 15) | 11 (3 to 37) (8 to 14) |
| -Diff | -2 (-16 to 10) (-6 to 1) | -4 (-17 to 10) (-8 to 1) | N/A |
| Sit-up test | 14 (3 to 27) (11 to 15) | 14 (3 to 27) (12 to 15) | 14 (3 to 21) (11 to 15) |
| 218 (43 to 405) (172 to 268) | 222 (79 to 405) (172 to 268) | 217 (43 to 390) (177 to 268) | |
| TUG | 10 (6 to 33) (8 to 11) | 9 (6 to 23) (8 to 11) | 9 (6 to 33) (8 to 11) |
| BMI at evaluation | 31 (21 to 44) (28 to 32) | 31 (21 to 44) (27 to 33) | 31 (25 to 43) (29 to 33) |
Abbreviations: TKA Total knee arthroplasty, TUG Timed up-and-go test, BMI Body mass index, ROM Range of motion, EXT Extension
Algometry showed a side-to-side median difference of 2 kg, which increased to a median of 4 kg in unilateral cases. The median sit-up and TUG tests were 14 sit-ups and 10 s, respectively. The BMI at follow-up ranged from 21 to 44 kg/m2, with 55 patients (42%) between 30 to 35 kg/m2 and 20 patients (15%) above 35 kg/m2 (Table 1). Anterior knee pain was reported by 27% (95% Confidence Interval [95%CI], 19% to 35%) of the included TKAs; no clinical difference between one-sided TKA and bilateral TKA was found, reaching 26% (95% CI, 15% to 41%) and 27% (95% CI, 18% to 38%), respectively. All patients' reported outcomes are summarised in Table 2.
Table 2.
Patient reported outcomes
| Median (Range) | IQ range | |
|---|---|---|
| Goodman A | 100 (0 to 100) | 87.5 to 100 |
| Goodman B | 5 (1 to 6) | 5 to 6 |
| WOMAC-pain | 2 (0 to 15) | 1 to 5 |
| - Normalized | 0.1 (0 to 0.75) | 0.05 to 0.25 |
| WOMAC-stiffness | 1 (0 to 8) | 0 to 2 |
| - Normalized | 0.13 (0 to 1) | 0 to 0.25 |
| WOMAC-Function | 9 (0 to 55) | 4 to 19 |
| - Normalized | 0.13 (0 to 0.81) | 0.06 to 0.30 |
| Kujala | 75 (20 to 100) | 63 to 86 |
| KOOS QL | 62.5 (5 to 100) | 43.75 to 81.25 |
Abbreviations: WOMAC Western Ontario and McMaster Universities Osteoarthritis Index, KOOS QL Knee injury and osteoarthritis outcome score quality of life, IQ Interquartile
The median satisfaction was 100 (IQR, 87.5 to 100), according to Section A of the Goodman scale (Table 2). The 75-point threshold was at the 90th percentile, with only seven cases reporting a score of 50 or lower. The lowest satisfaction percentage (20 TKAs, 15.3%) was achieved in question 3 of Section A, which asked about satisfaction with performing physical activities (Table 3). In Section B of the Goodman scale, 113 TKAs (86.26%) reported "great improvement" or "more than I ever dreamed"; conversely, 18 (patients 13.74%) rated their improvement as moderate or less (Table 4).
Table 3.
Distribution of answers of Section A of the Goodman scale by each question
| Satisfaction with | Very Unsatisfied | Somewhat Unsatisfied | Neither | Somewhat satisfied | Very satisfied |
|---|---|---|---|---|---|
| Pain relief | 3 (2.3%) | 1 (0.8%) | 4 (3.1%) | 17 (12.98%) | 106 (80.9%) |
| Ability to do house/yard work | 2 (1.5%) | 0 | 8 (6.1%) | 26 (19.9%) | 95 (72.5%) |
| Ability to do recreational activities | 4 (3.1%) | 4 (3.1%) | 12 (9.2%) | 37 (28.2%) | 74 (56.5%) |
| Overall Satisfaction | 2 (1.5%) | 0 | 8 (6.1%) | 15 (11.5%) | 106 (80.9%) |
Table 4.
Frequency of answers in the B section of the Goodman Scale (patient-perceived improvement)
| Goodman B | Frequency | Frequency | |
|---|---|---|---|
| Worse | 1 (0.76%) | Same or worse | 18 (13.74%) |
| Same as before | 5 (03.82%) | ||
| Low improvement | 6 (04.58%) | ||
| Moderate improvement | 6 (04.58%) | ||
| Great improvement | 74 (56.49%) | Much Better | 113 TKA (86.26%) |
| More than I ever dreamed | 39 (29.77%) |
Abbreviation: TKA Total knee arthroplasty
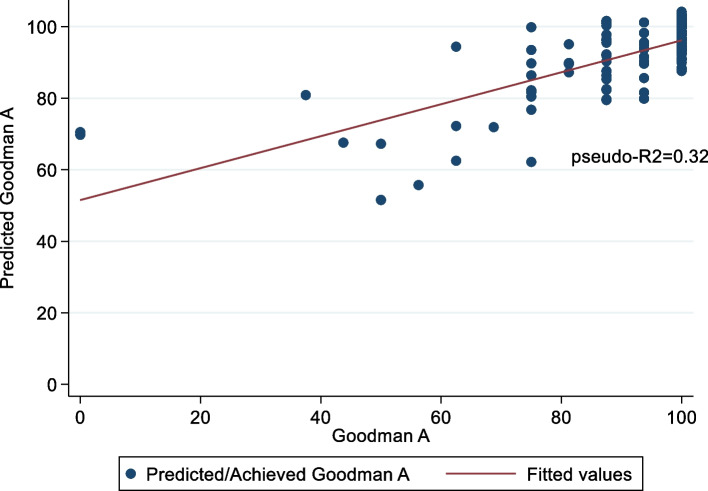
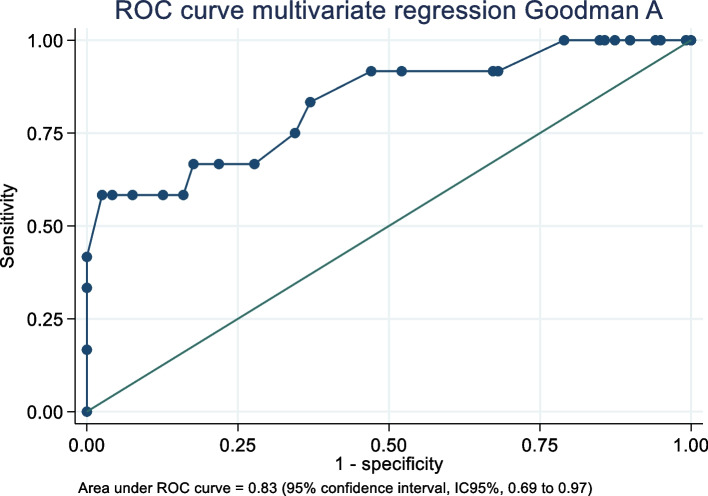
The quantile regression estimated that no functional evaluation—ROM, sit-up, or TUG—nor BMI had a significant association with patient satisfaction (Goodman A). Anterior knee pain and gender showed a significant coefficient but with a low pseudo R2. Conversely, patient-reported outcomes demonstrated a significant coefficient with pseudo-R2 ranging from 0.18 to 0.26. Multivariate bootstrapped quantile regression indicated that the best-predicted model was the pain and stiffness WOMAC and the Kujala score (Table 5). The predicted Goodman A (PGoodmanA) was estimated as follows: PGoodmanA = 88.14103 + (-1.602564 * WOMAC A) + (-2.350427 * WOMAC B) + (0.1602564 * Kujala), reaching a pseudo-R2 of 0.32. The scatter plot (Fig. 2) shows that the model fails to predict the lowest scores of Goodman A but provides a good estimation for scores above 40 points. Conversely, when the score was dichotomised using 75 points as the threshold, an MLR demonstrated that anterior knee pain (OR 5.16, 95% CI 1.24 to 21.39) and sit-up test (OR = 0.63, 95% CI 0.49 to 0.81) were significant. The area under the ROC curve was 0.83 (95% CI, 0.69 to 0.97), and the goodness-of-fit test had a probability of 0.71 (Fig. 3).
Table 5.
Coefficient, p-value and pseudo-R2 after univariate quantile regression to predict the Goodman A score
| Variable | Coefficient | P-Value | Pseudo-R2 |
|---|---|---|---|
| Age | 0 (-0.32 to 0.32) | 0.999 | 0.001 |
| Male | -6.25 (-11.94 to -0.56) | 0.030* | 0.001 |
| WOMAC-pain | -2.84 (–3.33 to -2.36) | < 0.000* | 0.260 |
| WOMAC-Stiffness | -6.25 (-7.43 to -5.07) | < 0.000* | 0.240 |
| WOMAC-Function | -0.80 (-0.95 to 105.03) | < 0.000* | 0.240 |
| Kujala | 0.42 (0.26 to 0.59) | < 0.000* | 0.200 |
| KOOS QL | 0.22 (0.12 to 0.32) | < 0.000* | 0.180 |
| Anterior knee pain | -12.5 (-20.6 to -4.41) | 0.003* | 0.060 |
| Follow-up | -0.70 (-2.51 to 1.11) | 0.444 | 0.010 |
| ROM | 0 (-0.21 to 0.21) | 0.999 | 0.001 |
| Extension | 0 (-0.61 to 0.61) | 0.999 | 0.001 |
| Extension difference | 0 (-0.61 to 0.61) | 0.999 | 0.001 |
| Flexion | 0 (-0.25 to 0.25) | 0.999 | 0.001 |
| Flexion difference | 0 (-0.24 to 0.24) | 0.999 | 0.001 |
| BMI at FU | 0 (-0.59 to 0.59) | 0.999 | 0.001 |
| Up and Go test | -0.64 (-1.32 to 0.05) | 0.070 | 0.020 |
| Situp test | 0 (-0.81 to 0.81) | 0.999 | 0.001 |
| Muscular force | 0 (-0.03 to 0.03) | 0.999 | 0.001 |
| Algometry | 0.32 (-0.12 to 0.77) | 0.150 | 0.002 |
Abbreviations: WOMAC Western Ontario and McMaster Universities Osteoarthritis Index, KOOS QL Knee injury and osteoarthritis outcome score quality of life, ROM Range of motion, BMI Body mass index, FU Follow-up
*significant coefficient (p-value < 0.05)
Fig. 2.
A scatter plot between the predicted score and the actual score of Section A of the Goodman scale. The red line corresponds to the fitted linear prediction
Fig. 3.
The ROC curve was estimated to determine the model's discrimination for Section A of the Goodman scale. The independent variables were anterior knee pain and the number of sit-ups performed in 30 s at the final follow-up. Abbreviations: ROC, receiver operating characteristics
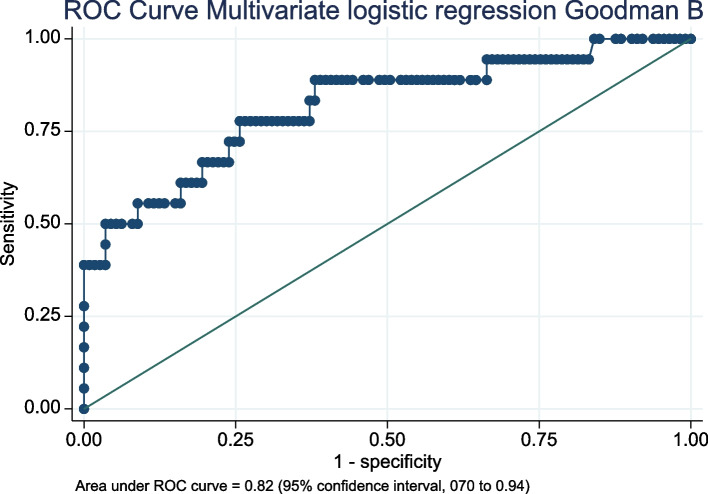
Logistic regression showed a significant association between the perceived improvement by patients (Goodman B) and patient-reported outcomes, anterior knee pain, years at follow-up, BMI at follow-up, sit-up, and TUG tests (Table 6). MLR indicated that anterior knee pain, sit-up test, and BMI were associated with patient-perceived improvement (Goodman B). Patients with anterior knee pain showed an odds ratio (OR) of 4.29 (95%CI, 1.20 to 15.30), BMI exhibited an OR of 0.84 (95%CI, 0.70 to 0.99), and sit-up was 0.74 (95%CI, 0.57 to 0.97), meaning that patients without anterior knee pain, higher BMI, and better performance in the sit-up test were more likely to perceive a better impact after TKA. The area under the ROC curve was 0.82 (95%CI, 0.70 to 0.94), and the goodness-of-fit test had a probability of 0.16 (Fig. 4). Multivariate models using patient-reported outcomes did not significantly improve the area under the ROC curve.
Table 6.
Comparison of patient-reported outcomes and functional evaluation among those patients who scored 5 or 6 (“Much better”) on Section B of the Goodman scale and those scoring 4 or less (“Same or worse”)
| Variable | Much better | Same or worse | Odd Ratio | AUC |
|---|---|---|---|---|
| Age at surgery | 65 (48 to 86) (62 to 70) | 70 (47 to 88) (62 to 77) | 1.04 (0.98 to 1.11) | N/A |
| Male | 49 (43%) | 9 (50%) | 1.31 (0.48 to 3.54) | N/A |
| WOMAC-pain | 2 (0 to 8) (1 to 3) | 10 (2 to 15) (6 to 14) | 1.98 (1.47 to 2.68)* | 0.94 (0.87 to 0.99) |
| WOMAC-Stiffness | 1 (0 to 3) (0 to 2) | 3 (0 to 8) (2 to 5) | 3.00 (0.01 to 0.07)* | 0.83 (0.71 to 0.95) |
| WOMAC-Function | 7 (0 to 36) (4 to 14) | 30 (11 to 55) (26 to 44) | 1.17 (1.10 to 1.25)* | 0.93 (0.87 to 0.98) |
| Kujala | 77 (32 to 100) (66 to 87) | 43 (29 to 78) (34 to 60) | 0.89 (0.85 to 0.93)* | 0.91 (0.84 to 0.98) |
| KOOS QL | 69 (5 to 100) (50 to 81) | 34 (12 to 87.5) (18.75 to 50) | 0.95 (0.92 to 0.97)* | 0.81 (0.69 to 0.93) |
| Anterior knee pain | 25 (22%) | 10 (56%) | 4.4 (1.57 to 12.33)* | 0.67 (0.54 to 0.79) |
| Follow-up | 2.7 (1 to 5) (2 to 4) | 3 (1 to 4) (2 to 4) | 1.03 (0.77 to 1.40)* | 0.58 (0.44 to 0.72) |
| ROM | 115 (91 to 147) (107 to 123) | 116 (80 to 132) (109 to 123) | 0.98 (0.94 to 1.02) | N/A |
| Extension | 2 (-6 to 16) (0 to 6) | 2 (-12 to 12) (0 to 6) | 0.92 (0.82 to 1.03) | N/A |
| Extension difference | 2 (-12 to 16) (-2 to 4) | 0 (-8 to 12) (4 to -4) | 1.03 (0.93 to 1.15) | N/A |
| Flexion | 112 (89 to 135) (106 to 120) | 113 (82 to 127) (109 to 123) | 0.99 (0.94 to 1.04) | N/A |
| Flexion difference | -5 (-33 to 21) (-12 to 2) | -8 (-42 to 17) (-12 to 0) | 1.02 (0.97 to 1.06) | N/A |
| BMI at FU | 31 (21 to 44) (29 to 33) | 28 (23 to 37) (25 to 31) | 0.83 (0.72 to 0.97)* | 0.70 (0.56 to 0.83) |
| Up and Go test | 9 (6 to 26) (8 to 10) | 12 (6 to 33) (8 to 14) | 1.16 (1.05 to 1.28)* | 0.69 (0.52 to 0.86) |
| Sit-up test | 14 (7 to 27) (12 to 15) | 11 (3 to 19) (9 to 13) | 0.74 (0.62 to 0.88)* | 0.73 (0.58 to 0.88) |
| Muscular force | 222 (94 to 405) (185 to 290) | 177 (43 to 313) (118 to 246) | 0.98 (0.98 to 0.99)* | 0.69 (0.55 to 0.84) |
| Algometry | 11 (2 to 37) (7 to 15) | 8 (0 to 22) (5.4 to 12) | 0.91 (0.82 to 1.01) | N/A |
The OR was estimated using univariate logistic regression to predict whether to be in the same or worse group. The AUC was estimated when the OR was significant
Abbreviations: WOMAC Western Ontario and McMaster Universities Osteoarthritis Index, KOOS QL Knee injury and osteoarthritis outcome score quality of life, ROM Range of motion, BMI Body mass index, FU Follow-up, OR Odds ratio, AUC Area under the curve
*significant coefficient (p-value < 0.05)
Fig. 4.
The ROC curve of the bootstrapped multivariate logistic regression was estimated to predict Section B of the Goodman scale. The independent variables were the presence of anterior knee pain, BMI, and the number of sit-ups performed in 30 s at the final follow-up. Abbreviations: ROC, receiver operating characteristics; BMI, body mass index
Discussion
The main finding of this study was that 86% of patients reported significant improvement, and 90% reported at least 75 points out of 100 in satisfaction after TKA with anterior stabilisation insert and no patellar resurfacing. Dissatisfaction after TKA has been historically documented to be around 20% [20]. A recent study showed dissatisfaction to be 22.2% and identified several risk factors: residual pain, female gender, primary diagnosis, ROM after surgery, and wound healing [44]. Nevertheless, other studies have recently reported that satisfaction rates are increasing after TKA, with rates nearing 90% achieved, as in this current study [12].
The main reasons for improved satisfaction after TKA are better implant design, increased understanding of TKA biomechanics and patellar tracking, and advancements in perioperative pain management [17, 38, 42, 54]. The recent development of better instruments to assess satisfaction has enabled researchers to compare more reliable results and establish what satisfaction means for patients [27]. The Goodman scale is reliable and aims to determine satisfaction and patients' self-perceived improvement after TKA [7, 18, 56].
Knee anterior pain and performance in the sit-up test were significantly associated with satisfaction and the improvement perceived by patients. This is consistent with other studies, as patients' expectations before surgery are a well-documented risk factor for dissatisfaction [39]. These expectations are mainly related to pain relief and function [35, 36].
We report a relatively high incidence of anterior knee pain after AS TKA, but within the range found in the literature [37, 43]. A simple explanation for anterior knee pain could be patellar preservation. Nevertheless, the incidence of anterior knee pain has been reported to be no different in cases of patellar resurfacing, due to component alignment in the axial patellar view [29, 40]. In the case of patellar retaining TKA, a more trochlear-friendly design has been shown to decrease the incidence of anterior knee pain [14, 32]. Moreover, a better understanding of the patellofemoral relationship in TKA is paramount: femoral offset, sagittal alignment, and rotation are essential for improving results in TKA without patellar resurfacing [1, 28, 29]. Roessler et al. reported that tibial component rotation was an important factor in predicting which TKA would require secondary patellar resurfacing [50]. Future studies must relate anterior knee pain to radiological parameters.
Additionally, the type of bearing surface seems to be related to anterior knee pain, with secondary patellar replacement being performed more frequently on PS cases, according to the German registry [5]. Nevertheless, meta-analyses have shown no difference in the prevalence of anterior knee pain between PS or CR TKA designs [25, 34].
A recent study comparing TKA with patellar resurfacing and TKA with patellar denervation found that denervation decreased the intensity of anterior knee pain the most, with similar satisfaction among groups at 24-month follow-ups [24]. Denervation is routinely performed in our TKA and could explain why some patients are satisfied despite residual anterior knee pain. However, other studies suggest a diminishing effect on anterior pain with denervation as the follow-up increases [59]. Another explanation for patients being satisfied despite anterior knee pain is that having anterior knee pain before surgery is a risk factor for experiencing it after surgery [17, 53]. Thus, surgery may not eliminate the pain, but if the intensity of pain is significantly decreased, patients might report satisfaction.
Infection and malalignment should be ruled out in cases of anterior knee pain after surgery. Subsequently, an interdisciplinary approach must be taken for pain management [13, 41]. Radiofrequency ablation of the genicular nerves has been proposed for treating anterior knee pain in patients with osteoarthritis, mainly in patients with a high perioperative risk [6]. This interventional technique could also maximise results after TKA, especially in those with a documented neuroma [15], but also in patients unsatisfied by anterior knee pain without a clear cause. In the latter, a previous blockage of the genicular nerves could be used as a diagnostic test to proceed further with the ablation [10].
Performance in TUG, muscular force, and the sit-up test were significantly associated with the patient's perception of improvement. The latter was also significant in the multivariate analysis for both sections of the Goodman scale. All these tests indirectly assess quadriceps strength, which is impaired after TKA compared to age-matched controls. Furthermore, low quadriceps strength before surgery has been associated with a longer period of recovery after TKA [23]. No specific muscle strength programme has shown superiority over others [3, 16, 52], but it seems that an exercise programme should be continued long-term after TKA [23]. This cohort had undergone heterogeneous exercise programmes after TKA, and those who performed better on the performance test were associated with greater satisfaction and perceived outcome.
Quadriceps strength and anterior knee pain are well-known related problems as well [30]. Anterior knee pain might lead patients to avoid strengthening programmes, leading to quadriceps atrophy which increases anterior pain [33]. This relationship has been found to be significant in patients after TKA [8], which might explain the association of anterior knee pain and the sit-up test found in the multivariate analysis of this study.
Another finding in our report was that patients with greater BMI had a significant trend to self-perceive a more remarkable improvement after TKA, but similar satisfaction. Contradictory statements are found in the literature on this topic [11]. Our results could be explained because the status before surgery in patients with greater BMI was worse than those with lesser BMI [58]. Therefore, patients with increased BMI should be given appropriate advice on their increased risk of infection and other complications [9]; however, both the surgeon and the patients should be aware that these patients are more likely to improve after surgery. Also, patients tend to increase their weight after surgery, according to the literature [11], so this finding could be interpreted as indicating that although patients gain weight after surgery, they can expect improvement compared to their pre-surgery status.
Finally, WOMAC, Kujala, and KOOS quality of life were strongly related to the Goodman scale, which makes our results more reliable and not biased by one patient-reported outcome. Also, it could help other surgeons to estimate their patients' satisfaction.
The main limitation of our study is the low sample size compared to other studies. Nevertheless, the findings consistently show that the same variables—anterior knee pain and sit-up test—were related to satisfaction and patients' improvement, and the bootstrapped regression accounts for this limitation. Also, these findings cannot be instantaneously extrapolated to other types of insert or patellar resurfacing. Additionally, this study did not use radiological assessment, which may bias the results. A further step in our research is determining which radiological parameters predict anterior knee pain in TKA without patellar resurfacing.
Conclusions
Anterior stabilised TKA without patellar resurfacing can achieve 90% satisfaction and 86% improvement in quality of life. To improve these results, it is essential to prevent and treat anterior knee pain and enhance quadriceps strength.
Acknowledgements
None.
Abbreviations
- 95%CI
95% Confidence Interval
- BMI
Body Mass Index
- CR
Cruciate Retaining
- IQR
Interquartile Range
- KOOS
Knee injury and Osteoarthritis Outcome Score
- MLR
Multivariate Logistic Regression
- OR
Odds Ratio
- PS
Posterior Stabilised
- ROC
Receiver Operating Characteristic
- ROM
Range of Motion
- TKA
Total Knee Arthroplasty
- TUG
Timed Up and Go
- WOMAC
Western Ontario and McMaster Universities Osteoarthritis Index
Authors’ contributions
MB contributed the original idea, conceived the study, performed surgery and the statistical analysis, and performed a critical review of the final paper. CB, a senior surgeon, supervised the study and critically reviewed the final paper. AA performed the screening to identify eligible patients and drafted the manuscript. MP was a surgeon and drafted the manuscript. MaB performed all functional tests and applied the patient’s reported outcome to all patients. TN performed the screening to identify eligible patients and contacted them by phone to schedule an appointment. JH, a senior surgeon, supervised the study and critically reviewed the final paper. AZ performed surgery and presented the investigation to the ethical committee. JC, a senior surgeon, supervised the study and critically reviewed the final paper. CI, a senior surgeon, supervised the study and critically reviewed the final paper.
Funding
This project was supported by funds awarded in the "Free Topics for Clinical and Basic-Clinical Research 2021" competition of the Research Support Office (OAIC) of the Hospital Clinico Universidad de Chile.
Availability of data and materials
The datasets used or analyzed during the current study are available from the corresponding author on reasonable request and approval from the ethical board commitee of our institution.
Declarations
Ethics approval and consent to participate
This study was approved by Ethics Research Board of the Hospital Clinico Universidad de Chile.
Consent for publication
All patients received proper information and provided written informed consent before inclusion in the study.
Competing interests
The authors declare no conflicts of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Abadie P, Galaud B, Michaut M, Fallet L, Boisrenoult P, Beaufils P. Distal femur rotational alignment and patellar subluxation: a CT scan in vivo assessment. Orthop Traumatol Surg Res. 2009;95(3):267–271. doi: 10.1016/j.otsr.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 2.Alcazar J, Aagaard P, Haddock B, Kamper RS, Hansen SK, Prescott E, et al. Assessment of functional sit-to-stand muscle power: Cross-sectional trajectories across the lifespan. Exp Gerontol. 2021;152:111448 . doi: 10.1016/j.exger.2021.111448. [DOI] [PubMed] [Google Scholar]
- 3.Bade MJ, Struessel T, Dayton M, Foran J, Kim RH, Miner T, et al. Early high-intensity versus low-intensity rehabilitation after total knee arthroplasty: a randomized controlled trial. Arthritis Care Res. 2017;69(9):1360–1368. doi: 10.1002/acr.23139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barahona M, Barrientos C, Escobar F, Sr, Diaz N, Palma D, Sr, Barahona MA, Martinez A, Sr, Infante CA. Trends in Knee and Hip Arthroplasty in Chile Between 2004 and 2019. Cureus. 2020;12(12):e12185 . doi: 10.7759/cureus.12185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bauer L, Woiczinski M, Thorwächter C, Melsheimer O, Weber P, Grupp TM, et al. Secondary patellar resurfacing in TKA: A combined analysis of registry data and biomechanical testing. J Clin Med. 2021;10(6):1227. doi: 10.3390/jcm10061227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beckwith M, Cushman D, Clark T, Park PK, Burnham T, Burnham R, et al. Radiofrequency Ablation of the Infrapatellar Branch of the Saphenous Nerve for the Treatment of Chronic Anterior Inferomedial Knee Pain. Pain Med. 2023;24(1):150–157. doi: 10.1093/pm/pnac108. [DOI] [PubMed] [Google Scholar]
- 7.Brañes J, Barahona M, Carvajal S, Wulf R, Barrientos C. Validation of the Spanish version of the Goodman score in total hip arthroplasty. J Orthop Surg Res. 2021;16(1):512–517. doi: 10.1186/s13018-021-02653-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Breugem SJM, Haverkamp D. Anterior knee pain after a total knee arthroplasty: what can cause this pain? World J Orthop. 2014;5(4):163–170. doi: 10.5312/wjo.v5.i3.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chaudhry H, Ponnusamy K, Somerville L, McCalden RW, Marsh J, Vasarhelyi EM. Revision rates and functional outcomes among severely, morbidly, and super-obese patients following primary total knee arthroplasty: a systematic review and meta-analysis. JBJS Rev. 2019;7(7):e9 . doi: 10.2106/JBJS.RVW.18.00184. [DOI] [PubMed] [Google Scholar]
- 10.Choi W-J, Hwang S-J, Song J-G, Leem J-G, Kang Y-U, Park P-H, et al. Radiofrequency treatment relieves chronic knee osteoarthritis pain: a double-blind randomized controlled trial. Pain. 2011;152(8):1933–1934. doi: 10.1016/j.pain.2010.09.029. [DOI] [PubMed] [Google Scholar]
- 11.Coelho A, Leal-Blanquet J, Sánchez-Soler JF, Torres-Claramunt R, Hinarejos P, Monllau JC. Patients lose weight after a total knee arthroplasty: myth or reality? Int Orthop. 2022;46(6):1299–1304. doi: 10.1007/s00264-022-05387-0. [DOI] [PubMed] [Google Scholar]
- 12.DeFrance M, Scuderi G. Are 20% of patients actually dissatisfied following total knee arthroplasty? A systematic review of the literature. J Arthroplasty. 2023;38(3):594–599. doi: 10.1016/j.arth.2022.10.011. [DOI] [PubMed] [Google Scholar]
- 13.Dennis DA. Evaluation of painful total knee arthroplasty. J Arthroplasty. 2004;19(4 Suppl 1):35–40. doi: 10.1016/j.arth.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 14.Deroche E, Batailler C, Swan J, Sappey-Marinier E, Neyret P, Servien E, Lustig S. No difference between resurfaced and non-resurfaced patellae with a modern prosthesis design: a prospective randomized study of total knee arthroplasties. Knee Surg Sports Traumatol Arthrosc. 2021;30(3):1025–1038. doi: 10.1007/s00167-021-06521-y. [DOI] [PubMed] [Google Scholar]
- 15.Giannetti A, Valentino L, Mazzoleni MG, Tarantino A, Calvisi V. Painful total knee arthroplasty: Infrapatellar branch of the saphenous nerve selective denervation. A case series. Knee. 2022;39:197–202. doi: 10.1016/j.knee.2022.09.010. [DOI] [PubMed] [Google Scholar]
- 16.Gianola S, Stucovitz E, Castellini G, Mascali M, Vanni F, Tramacere I, Fusaro I, Colle F, Zerbinati E, Sansone V. Effects of early virtual reality-based rehabilitation in patients with total knee arthroplasty: a randomized controlled trial. Medi (Baltimore) 2020 doi: 10.1097/MD.0000000000019136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gibon E, Goodman MJ, Goodman SB. Patient satisfaction after total knee arthroplasty: a realistic or imaginary goal? Orthop Clin North Am. 2007;48(4):421–431. doi: 10.1016/j.ocl.2017.06.001. [DOI] [PubMed] [Google Scholar]
- 18.Goodman SM, Mehta BY, Kahlenberg CA, Krell EC, Nguyen J, Finik J, et al. Assessment of a satisfaction measure for use after primary total joint arthroplasty. J Arthroplasty. 2020;35(7):1792–1799. doi: 10.1016/j.arth.2020.02.039. [DOI] [PubMed] [Google Scholar]
- 19.Grassi A, Compagnoni R, Ferrua P, Zaffagnini S, Berruto M, Samuelsson K, et al. Patellar resurfacing versus patellar retention in primary total knee arthroplasty: a systematic review of overlapping meta-analyses. Knee Surg Sports Traumatol Arthrosc. 2018;26(11):3206–3218. doi: 10.1007/s00167-018-4831-8. [DOI] [PubMed] [Google Scholar]
- 20.Gunaratne R, Pratt DN, Banda J, Fick DP, Khan RJ, Robertson BW. Patient dissatisfaction following total knee arthroplasty: a systematic review of the literature. J Arthroplasty. 2017;32(12):3854–3860. doi: 10.1016/j.arth.2017.07.021. [DOI] [PubMed] [Google Scholar]
- 21.Ha C, Wang B, Li W, Sun K, Wang D, Li Q. Resurfacing versus not-resurfacing the patella in one-stage bilateral total knee arthroplasty: a prospective randomized clinicaltrial. Int Orthop. 2019;43(10):2519–2527. doi: 10.1007/s00264-019-04361-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hinzpeter J, Barahona M, Aliste J, Barrientos C, Zamorano A, Palet M, et al. Gonyautoxins 2/3 local periarticular injection for pain management after total knee arthroplasty: a double-blind, randomized study. J Knee Surg. 2023;36(4):389–396. doi: 10.1055/s-0041-1735312. [DOI] [PubMed] [Google Scholar]
- 23.Ishii Y, Noguchi H, Sato J, Sakurai T, Toyabe S-i. Quadriceps strength impairment in the mid- to long-term follow-up period after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2017;25(11):3372–3377. doi: 10.1007/s00167-016-4333-5. [DOI] [PubMed] [Google Scholar]
- 24.Ji X, Huang X, Zhang Y, Zhao M, Liu Y, Cheng Y. Peripheral patellar denervation has a better effect in reducing postoperative anterior knee pain than patellar resurfacing in TKA. Med (Baltimore) 2022 doi: 10.1097/MD.0000000000031584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jiang C, Liu Z, Wang Y, Bian Y, Feng B, Weng X. Posterior cruciate ligament retention versus posterior stabilization for total knee arthroplasty: a meta-analysis. PLoS One. 2016;11(1):e0147865 10.1371/journal.pone.0147865. doi: 10.1371/journal.pone.0147865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kahlenberg CA, Gibbons JAB, Mehta BY, Antao VC, Lai EY, Do HT, et al. Satisfaction with the process vs outcome of care in total hip and knee arthroplasty. J Arthroplasty. 2022;37:419–424. doi: 10.1016/j.arth.2021.11.010. [DOI] [PubMed] [Google Scholar]
- 27.Kahlenberg CA, Nwachukwu BU, McLawhorn AS, Cross MB, Cornell CN, Padgett DE. Patient satisfaction after total knee replacement: a systematic review. HSS J. 2018;14(3):192–201. doi: 10.1007/s11420-018-9614-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Keshmiri A, Maderbacher G, Baier C, Sendtner E, Schaumburger J, Zeman F, Grifka J, Springorum HR. The influence of component alignment on patellar kinematics in total knee arthroplasty: an in vivo study using a navigation system. Acta Orthop. 2015;86(3):444–450. doi: 10.3109/17453674.2015.1005907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kim JH, Yoo BW, Kim CW. Influence of the rotational alignment of the femoral and patellar components on patellar tilt in total knee arthroplasty. Knee Surg Relat Res. 2015;27(3):163–167. doi: 10.5792/ksrr.2015.27.3.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim S, Park J. Patients with chronic unilateral anterior knee pain experience bilateral deficits in quadriceps function and lower quarter flexibility: a cross-sectional study. Physiother Theory Pract. 2022;38(13):2531–2543. doi: 10.1080/09593985.2021.1946871. [DOI] [PubMed] [Google Scholar]
- 31.Kim TK, Chang CB, Kang YG, Kim SJ, Seong SC. Causes and predictors of patient's dissatisfaction after uncomplicated total knee arthroplasty. J Arthroplasty. 2009;24(2):263–271. doi: 10.1016/j.arth.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 32.Koh IJ, Kim MS, Sohn S, Song KY, Choi NY, In Y. Patients undergoing total knee arthroplasty using a contemporary patella-friendly implant are unaware of any differences due to patellar resurfacing. Knee Surg Sports Traumatol Arthrosc. 2019;27(4):1156–1164. doi: 10.1007/s00167-018-5120-2. [DOI] [PubMed] [Google Scholar]
- 33.Laubach M, Hellmann JT, Dirrichs T, Gatz M, Quack V, Tingart M, Kuhlmann B, Nöth U. Anterior knee pain after total knee arthroplasty: a multifactorial analysis. J Orthop Surg (Hong Kong) 2020 doi: 10.1177/2309499020918947. [DOI] [PubMed] [Google Scholar]
- 34.Li N, Tan Y, Deng Y, Chen L. Posterior cruciate-retaining versus posterior stabilized total knee arthroplasty: a meta-analysis of randomized controlled trials. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):556–564. doi: 10.1007/s00167-012-2275-0. [DOI] [PubMed] [Google Scholar]
- 35.Lingard EA, Sledge CB, Learmonth ID, Group KO Patient expectations regarding total knee arthroplasty: differences among the United States, United Kingdom, and Australia. J Bone Joint Surg Am. 2006;88(6):1201–1207. doi: 10.2106/JBJS.E.00147. [DOI] [PubMed] [Google Scholar]
- 36.Londhe SB, Shah RV, Doshi AP, Upasani T, Antao N, Agrawal G. What do patients want out of their Total Knee Arthroplasty?: An Indian perspective. J Clin Orthop Trauma. 2022 doi: 10.1016/j.jcot.2022.101761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Longo UG, Ciuffreda M, Mannering N, D'Andrea V, Cimmino M, Denaro V. Patellar resurfacing in total knee arthroplasty: systematic review and meta-analysis. J Arthroplasty. 2018;33(3):620–632. doi: 10.1016/j.arth.2017.08.041. [DOI] [PubMed] [Google Scholar]
- 38.Lustig S, Servien E, Batailler C. How to optimize patellar tracking in knee arthroplasty? Orthop Traumatol Surg Res. 2023;109(1S):103458 . doi: 10.1016/j.otsr.2022.103458. [DOI] [PubMed] [Google Scholar]
- 39.Lützner C, Beyer F, David L, Lützner J. Fulfilment of patients’ mandatory expectations are crucial for satisfaction: a study amongst 352 patients after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2023 doi: 10.1007/s00167-022-07301-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Matz J, Howard JL, Morden DJ, MacDonald SJ, Teeter MG, Lanting BA. Do changes in patellofemoral joint offset lead to adverse outcomes in total knee arthroplasty with patellar resurfacing? A radiographic review J Arthroplasty. 2017;32(4):783–787. doi: 10.1016/j.arth.2016.08.032. [DOI] [PubMed] [Google Scholar]
- 41.McDowell M, Park A, Gerlinger TL. The painful total knee arthroplasty. Orthop Clin North Am. 2016;47(4):317–326. doi: 10.1016/j.ocl.2015.09.008. [DOI] [PubMed] [Google Scholar]
- 42.Memtsoudis SG, Cozowicz C, Bekeris J, Bekere D, Liu J, Soffin EM, et al. Peripheral nerve block anesthesia/analgesia for patients undergoing primary hip and knee arthroplasty: recommendations from the International Consensus on Anesthesia-Related Outcomes after Surgery (ICAROS) group based on a systematic review and meta-analysis of current literature. Reg Anesth Pain Med. 2021;46(10):971–985. doi: 10.1136/rapm-2021-102750. [DOI] [PubMed] [Google Scholar]
- 43.Michalik R, Rath B, Springorum HR, Lüring C, Tingart M. Anterior knee pain after total knee arthroplasty: causes, diagnosis and treatment. Orthopade. 2016;45(5):386–398. doi: 10.1007/s00132-016-3256-7. [DOI] [PubMed] [Google Scholar]
- 44.Muertizha M, Cai X, Ji B, Aimaiti A, Cao L. Factors contributing to 1-year dissatisfaction after total knee arthroplasty: a nomogram prediction model. J Orthop Surg Res. 2022;17(1):1–13. doi: 10.1186/s13018-022-03205-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Núñez-Cortés R, Cruz-Montecinos C, Martinez-Arnau F, Torres-Castro R, Zamora-Risco E, Pérez-Alenda S, et al. 30 s sit-to-stand power is positively associated with chest muscle thickness in COVID-19 survivors. Chron Respir Dis. 2022 doi: 10.1177/14799731221114263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.OECD Health at a Glance 2021: OECD Indicators. OECD Publishing, Paris, 2021 doi: 10.1787/ae3016b9-en. [DOI] [Google Scholar]
- 47.Oyarzun A, Barrientos C, Barahona M, Martinez Á, Soto-Arellano V, Courtin C, et al. Knee haemophilic arthropathy care in Chile: Midterm outcomes and complications after total knee arthroplasty. Haemophilia. 2020;26(3):179–186. doi: 10.1111/hae.14004. [DOI] [PubMed] [Google Scholar]
- 48.Price AJ, Alvand A, Troelsen A, Katz JN, Hooper G, Gray A, et al. Knee replacement. Lancet. 2018;392(10158):1672–1682. doi: 10.1016/S0140-6736(18)32344-4. [DOI] [PubMed] [Google Scholar]
- 49.Putman S, Boureau F, Girard J, Migaud H, Pasquier G. Patellar complications after total knee arthroplasty. Orthop Traumatol Surg Res. 2019;105(Suppl 1):43–51. doi: 10.1016/j.otsr.2018.04.028. [DOI] [PubMed] [Google Scholar]
- 50.Roessler PP, Moussa R, Jacobs C, Schüttler KF, Stein T, Schildberg FA, et al. Predictors for secondary patellar resurfacing after primary total knee arthroplasty using a “patella-friendly” total knee arthroplasty system. Int Orthop. 2019;43(3):611–617. doi: 10.1007/s00264-018-4075-8. [DOI] [PubMed] [Google Scholar]
- 51.Raja BS, Gowda AK, Ansari S, Choudhury AK, Kalia RB. Comparison of functional outcomes, femoral rollback and sagittal stability of anterior-stabilized versus posterior-stabilized Total knee Arthroplasty: a systematic review and Meta-analysis of randomized controlled trials. Indian J Orthop. 2021;55(5):1076–1086. doi: 10.1007/s43465-021-00494-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sattler LN, Hing WA, Vertullo CJ. What is the evidence to support early supervised exercise therapy after primary total knee replacement? A systematic review and meta-analysis. BMC Musculoskelet Disord. 2019;20(1):1–11. doi: 10.1186/s12891-019-2415-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Silva DDO, Webster KE, Feller JA, McClelland JA. Anterior Knee Pain Following Primary Unilateral Total Knee Arthroplasty With Posterior-Stabilized Prosthesis and Patellar Resurfacing: Prevalence and Clinical Implications. J Arthroplasty. 2023;38(1):281–285. doi: 10.1016/j.arth.2022.08.042. [DOI] [PubMed] [Google Scholar]
- 54.Simpson CJ, Ng N, Ndou S, Wright E, Yap NJ, Scott CE, et al. Patellar resurfacing was not associated with a clinically significant advantage when a modern patellar friendly total knee arthroplasty is employed: A systematic review and meta-analysis. Knee. 2023;41:329–341. doi: 10.1016/j.knee.2023.01.021. [DOI] [PubMed] [Google Scholar]
- 55.Tilbury C, Haanstra T, Leichtenberg C, Verdegaal S, Ostelo R, de Vet H. Unfulfilled expectations after total hip and knee arthroplasty surgery: there is a need for better preoperative patient information and education. J Arthroplasty. 2016;31(10):2139–2145. doi: 10.1016/j.arth.2016.02.061. [DOI] [PubMed] [Google Scholar]
- 56.Ulivi M, Orlandini L, Meroni V, Viganò M, D’Errico M, Perrotta R, et al. Italian Translation, Adaptation, and Validation of the Novel Satisfaction Measure Assessment after Primary Total Joint Arthroplasty: The Goodman Score Questionnaire. Healthcare (Basel) 2022 doi: 10.3390/healthcare10050769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Van der Merwe JM, Mastel MS. Controversial topics in Total knee arthroplasty: a 5-year update (part 1) J Am Acad Orthop Surg Glob Res Rev. 2020;4(1):e1900047 . doi: 10.5435/JAAOSGlobal-D-19-00047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vitaloni M, Botto-van Bemden A, Sciortino Contreras RM, Scotton D, Bibas M, Quintero M, et al. Global management of patients with knee osteoarthritis begins with quality of life assessment: a systematic review. BMC Musculoskelet Disord. 2019 doi: 10.1186/s12891-019-2895-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yuan MC, Ding ZC, Ling TX, Zhou Z. Patellar Denervation with Electrocautery Reduces Anterior Knee Pain within 1 Year after Total Knee Arthroplasty: A Meta-Analysis of Randomized Controlled Trials. Orthop Surg. 2021;13(1):14–27. doi: 10.1111/os.12735. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used or analyzed during the current study are available from the corresponding author on reasonable request and approval from the ethical board commitee of our institution.