Abstract
Background
Despite current recommendation, vaccination coverage (VC) for patients with heart failure (HF) remains far too limited.
Aims
To evaluate the VC of HF patients followed in our hospital center and investigate the barriers to vaccination and the ways to address them.
Methods
This was a cross-sectional monocentric descriptive study conducted between December 2019 and January 2021 at the University Hospital of Montpellier, France. Patients with HF history hospitalized in cardiology unit (CU) and patients in a HF telemonitoring program (TP) were included. An interview was conducted by a pharmacist to find out the patient's vaccination status against influenza and pneumococcus. For non-vaccinated patients, opinion and willingness to be vaccinated were also obtained.
Results
Data from 335 patients were collected (185 in CU, 150 in TP). The mean age was 69.3 years and the proportion of males was 72%. About 65% were vaccinated against influenza in the last year (60% in CU, 72% in TP, p = 0.022) and 22% were up to date with pneumococcal vaccination (11% in CU, 35% in TP, p < 0.001). Among patients not vaccinated, 17% refused vaccination. Among unvaccinated patients who consider vaccination, 69% wanted to be vaccinated by their general practitioner (GP).
Conclusions
The VC of HF patients remains insufficient. Patients in TP are more vaccinated than patients in CU, which could involve better management. The low rate of vaccinated patients is mainly explained by a lack of awareness. The medical team, including the clinical pharmacist by his dedicated time during medication reconciliation may play a major role in the management of hospitalized patients as well as GP's as local actors.
Keywords: Heart failure, Vaccination coverage, Influenza vaccination, Pneumococcal vaccination, Clinical pharmacy
1. Introduction
The prevalence of heart failure (HF) is estimated at 1-2% of the general population in developed countries and is over 10% in people aged 70 years or older [1]. Despite marked pharmacologic and device-based advances for HF with reduced ejection fraction (HFrEF) in recent years, HF is associated with significant morbidity, mortality, and a heavy economic burden.
Recent European data (ESC-HF pilot study) show that the one-year all-cause mortality rates for inpatients and outpatients with HF were 17% and 7% respectively, and the one-year hospitalisation rates were 44% and 32% respectively [2].
Infections can be responsible for acute HF exacerbation and increased hospitalisation in people with HF [3]. Indeed, in a large cohort of 9,335 HF patients with a mean followed-up period of 2.8 ± 2.6 years, 38% of the study cohort experienced at least one infection-related hospital admission. Among infections, pneumonia and chronic obstructive pulmonary disease (COPD) exacerbations were the most common symptoms [4]. Moreover, large HF registry data have shown that lung infections are the leading cause of hospitalisation (15.3%) ahead of ischaemic causes (14.7%) and rhythm disorders (13.5%). In addition, they are also associated with higher hospital mortality [5]. Vaccination may reduce the incidence and/or severity of respiratory infection, and thereby, reduce the risk of HF exacerbation.
Three vaccines are recommended (but not mandatory) for patients with HF: influenza vaccine, pneumococcal vaccine and now, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vaccine [[6], [7], [8], [9]].
Recent evidence from PARADIGM-HF trial found that influenza vaccination was associated with a reduced risk of all-cause mortality in a cohort of patients with HFrEF [10]. Even more recently, the randomised, double-blind IVVE trial compared an inactivated influenza vaccine with a placebo, given annually for 3 influenza seasons in HF patients. No statistically significant difference was observed between the two groups in the two primary endpoints: cardiovascular deaths, non-fatal heart attacks, non-fatal strokes, and hospitalisations for HF. However, influenza vaccination was associated with less pneumonia (−42%) and all causes hospitalisations in HF patients (−16%), and fewer deaths (−21%) and cardiovascular events (−18%), particularly during periods of viral circulation. A reduction in the risk of hospitalisation for HF was observed with vaccination but outside the period of virus circulation (−24%) [11].
By contrast, the effectiveness of pneumococcal vaccine seems less reliable as the protective effect evidenced relies on observational studies only [12], although the risk of pneumococcal infection is 4 times higher in patients with HF [13].
Despite the potential benefits, vaccination coverage for patients with HF remains far too limited, as illustrated in the PARADIGM-HF trial, where the influenza vaccination rate for winter 2014/2015 was estimated at 39%, and only 20% of patients had at least one pneumococcal vaccination in a cohort of 200 HF patients in a Belgian hospital [14].
The reasons for such a huge gap between guidelines and their application remains to be investigated. To our knowledge, there are currently no data on the causes of non-vaccination in HF patients.
The aim of our study was first to evaluate the vaccination coverage of HF patients followed in our tertiary hospital center and then investigate the barriers to vaccination and the ways to address them.
2. Methods
2.1. Study design, setting and participants
This was a cross-sectional monocentric descriptive study conducted between December 2019 and January 2021. Participation to this study was proposed by a clinical resident pharmacist to adult patients (>18 years) with HF history admitted in the two complete hospitalisation (32 beds each) cardiology units University Hospital of Montpellier and to patients included in our telemonitoring program (connected scale with daily weight tracking), permitting the inclusion of patients followed by cardiologists from other centers in a large region. Patients hospitalized in these units are only admitted for acute reasons or interventional cardiology procedures. Depending on the need, they are reviewed later by their usual cardiologist, or in our outpatient department. Patients who were newly diagnoses HF were not included in this study. Patients receiving immunosuppressive treatment, people whose physical and/or psychological health is severely impaired (whose health condition does not allow them to give consent to participate in the study or to answer questions), people living in semi-liberty or institutionalised, people under guardianship or curatorship, and people who do not speak French were also not included. The investigation conforms to the principles outlined in the Declaration of Helsinki and was approved by the Hospital Institutional Review Board (IRB-MTP_2020_07_202000541).
2.2. Pharmaceutical intervention
In our clinical practice, a pharmaceutical team, including a senior pharmacist and/or a resident and pharmacy students, conducted a medication reconciliation process within 24 h of admission or on the first working day following admission to the unit. During the patient's hospitalisation, the pharmacist or resident pharmacist participates in optimising the management of patients with HF and in the reviewing of drug prescriptions (issuing pharmaceutical advice, proposing therapeutic optimisation in collaboration with the medical team).
As part of this practice, the pharmaceutical team assesses vaccination coverage with the patient, but also with the community pharmacist and the general practitioner (GP).
The interview with the patient included a 4-questions knowledge questionnaire: a question on the principles of vaccination (4 items), a question on the content of vaccines (4 items), a question on influenza vaccination (5 items) and a question on pneumococcal vaccination (4 items) (Appendix A). An answer was considered correct if all the items in a question were correct. A 4-point score was established for all patients. A score of 0 or 1 on the knowledge questionnaire was defined as a low score, while a score ≥2 was considered as a high score. The responses to the questionnaire were given to all patients after they had completed it. The pharmaceutical team also answered any questions the patients had at the end of the interview. For all patients, medication compliance was determined by the Girerd score [15], and for non-vaccinated patients, opinion and willingness to be vaccinated were also obtained during the interview. After each pharmaceutical interview, the patients were given an information leaflet on how the vaccination works and on the usefulness of carrying out these vaccinations for patients with HF.
If patients are not up to date with their vaccinations, a vaccination strategy has been set up with the patients, their cardiologist or their general practitioner.
2.3. Study outcomes
The primary outcome was to determine the proportion of patients who were up to date with influenza, pneumococcal vaccination during the study period.
The secondary outcomes were to assess the proportion of patients who were favorable, had mixed opinion or who were against vaccination, to study the factors influencing vaccination, to collect the proportion of patient with a high knowledge score about vaccination, the kinds of methods desired by unvaccinated patients to achieve vaccination and the kind of methods in which patients were informed of the need of vaccination.
2.4. Data collection
Socio-demographic (age, sex), clinical (vaccination status, reason for hospitalisation, left ventricular ejection fraction (LVEF)), compliance score, knowledge score and biological (NT-proBNP at admission) data were collected. Biological data and transthoracic echocardiography were all performed during the patient's stay, or at the last visit for telemonitored patients. Patients were considered with HFrEF if LVEF was ≤40% and with HF with preserved ejection fraction (HFpEF) if LVEF was >40% associated with elevated BNP and echocardiographic criteria according to ESC 2016 guidelines [16].
The vaccination status was obtained from patient self-reporting, and by systematically checking all patients with their pharmacist and general practitioner. It was collected for all patients during the hospital interview for patients in cardiology units, and by a phone interview for telemonitored patients. In case of discrepancies between the patients' declaration and the pharmacists/general practitioners, or in the absence of recollection by the patient, we took into consideration the information obtained from the pharmacists and doctors. Patients were considered to be unvaccinated against pneumococcus if they have had only a 13-valent pneumococcal conjugate vaccine (13PCV) or a 23-valent pneumococcal polysaccharide vaccine (23PPV), in accordance with French vaccination recommendations. On the other hand, they were considered vaccinated if they received a 13PCV followed within a minimum of two-month intervals by a 23PPV in the last five years. Patients vaccinated first with 23PPV were also considered vaccinated if they were subsequently vaccinated with 13PCV at least one year later [6]. For influenza vaccination, patients were considered vaccinated if they received the vaccine during the last vaccination campaign. Patients were considered unvaccinated even if they informed us that they wanted to be vaccinated soon. Patients’ opinions on vaccination, the way in which they were informed of the vaccination and the method of vaccination for those who are not vaccinated and who wish to be vaccinated were also collected. The questions regarding opinion on covid-19 vaccination were asked before the vaccines were available in France i.e. from July 2020.
2.5. Statistical analysis
Patients’ characteristics, vaccination status and patient answers were described with numbers and proportions for categorical variables and with medians and inter-quartile ranges (IQR25–75) for quantitative variables because they did not follow a normal distribution.
The vaccination status (for influenza, pneumococcal) of patients in the cardiology unit and telemonitored patients, the rate of vaccination between patient with HFrEF and HFpEF, the relationship between the opinion on vaccination and the knowledge score as well as the difference between the number of correct answers concerning influenza vaccination and pneumococcal vaccination were analysed using a bilateral Chi square test.
Multivariable logistic regression analysis was performed between influenza vaccine status and gender, age, pneumococcal vaccination, medication compliance, knowledge score, patient's group (cardiology unit or telemonitoring) and between pneumococcal vaccination status and influenza vaccination, knowledge score and patient's group. The variables used for the multivariable logistic regression were those with a p-value <0.1 in univariate analysis (Appendix B and C). Finally, variables retained were selected using a backward stepwise selection procedure (Akaike Information Criterion).
Statistical analyses were performed at the conventional two-tailed α level of 0.05 using R version 4.0.4.3.
3. Results
3.1. Population description
Data from 335 patients were collected (185 in cardiology units and 150 in telemonitoring program). The proportion of males was 71.9% (n = 241) and the sex ratio was 2.6 (Table 1). The median age was 71 years with a minimum age of 28 years and a maximum age of 97 years. Median LVEF and median Nt-pro-BNP were respectively 42% and 2,296 ng/L (n = 267 patients). 11.3% of patients (n = 34) had a history of hospitalisation for pulmonary infection (on 300 patients, based on reporting by GP's and notifications in medical records). Medication compliance was good for 49.6% of patients (n = 166), moderate for 37.9% (n = 127), bad for 3.9% (n = 13) and unknown for 8.6% (n = 29, including 3 patients with no treatments).
Table 1.
Population description (Results are expressed as percentages or median and interquartile ranges [25–75] as appropriate).
| N | 335 |
| % male | 71.9 |
| % female | 28.1 |
| Age (years) | 71 [62–78] |
| LVEF (%) | 42 [32–55] |
| Nt-pro-BNP (ng/L) | 2,296 [1,109.5-5,857.5] |
| History of hospitalisation for pulmonary disease (n = 300) | 34 (11.3%) |
| Medication compliance | |
| Good | 166 (49.6%) |
| Moderate | 127 (37.9%) |
| Bad | 13 (3.9%) |
| Unknown | 29 (8.6%) |
LVEF: Left Ventricular Ejection Fraction.
3.2. Vaccination coverage
20.0% of the patients (n = 67) were vaccinated against both influenza and pneumococcus, 10.3% (n = 19) in cardiology units’ group and 32.0% (n = 48) in the telemonitoring program group (p < 0.001).
65.4% of the patients (n = 219) were vaccinated against influenza in the last year, 60.0% (n = 111) in the cardiology units’ group and 72.0% (n = 108) in the telemonitoring program group (p = 0.022) (Table 2).
Table 2.
Influenza vaccination and pneumococcal vaccination. (The percentage of vaccinated patients in the cardiology unit and telemonitored patients was analysed using a bilateral Chi square test.)
| Vaccination status | Influenza vaccination (p = 0.022) |
||
|---|---|---|---|
| Cardiology unit (n = 185) | Telemonitoring (n = 150) | Total (n = 335) | |
| Vaccinated | 60.0% (111) | 72.0% (108) | 65.4% (219) |
| Unvaccinated |
40.0% (74) |
28.0% (42) |
34.6% (116) |
|
Pneumococcal vaccination (p < 0.001) |
|||
|
Cardiology unit (n=185) |
Telemonitoring (n=150) |
Total (n=335) |
|
| Vaccinated | 11.4% (21) | 35.3% (53) | 22.1% (74) |
| Unvaccinated | 85.9% (159) | 59.4% (89) | 74.0% (248) |
| Unknown | 2.7% (5) | 5.3% (8) | 3.9% (13) |
Regarding pneumococcal vaccination, 22.1% of patients (n = 74) were up to date, 11.4% (n = 21) in the cardiology units’ group and 35.3% (n = 53) in the telemonitoring program group (p < 0.001) (Table 2). No patients were in the process of completing their immunization schedule.
3.3. Opinion on vaccination
Regardless of vaccination status and type of vaccination, 68.0% of the patients (n = 204) were in favour of the vaccination, 23.0% (n = 69) had a mixed opinion and 9.0% (n = 27) were against it. In cardiology units and in telemonitoring program they were respectively 70.0% and 66.0% in favour (n = 105, n = 99), 22.0% and 24.0% with mixed opinion (n = 33, n = 36), 8% and 10.0% against vaccination (n = 12, n = 15) (p = 0.73).
Among the patients asked about vaccination against covid-19 (n = 198, 106 in cardiology units and 92 in telemonitoring program), 59.6% (n = 118) were in favour, 29.8% (n = 59) were still hesitating and 10.6% (n = 21) were against it. Among the unvaccinated patients who refused to be vaccinated against influenza or pneumococcus (n = 24), 58.3% (n = 14) were still considering vaccination against covid-19. Among the patients considering or wishing to be vaccinated against influenza or pneumococcus (n = 134), only 6.7% (n = 9) refused to be vaccinated against covid-19.
3.4. Questionaries’ analyses
Concerning the answers to the knowledge questionnaire, only 1.0% of patients had good response to all items (n = 3). 11.0% got a score of 3/4 (n = 33) and 34.3% had 2/4 (n = 103). More than half of the patients had a low questionnaire score, with 32.0% scoring 1/4 (n = 96) and about 21.7% scoring 0/4 (n = 65).
They were respectively 45.3% (n = 68) and 47.3% (n = 71) with high knowledge score in cardiology units and in telemonitoring program (p = 0.73).
We noticed that 52.0% (n = 156) of patients had a good answer to the influenza question, compared to 19.0% (n = 57) to pneumococcal question (p < 0.001).
Among patients with a low knowledge score (0–1) and with high knowledge score (2- 3–4), respectively 65.8% (n = 106) and 70.5% (n = 98) were in favour to vaccination (p = 0.39).
3.5. Factors influencing vaccination
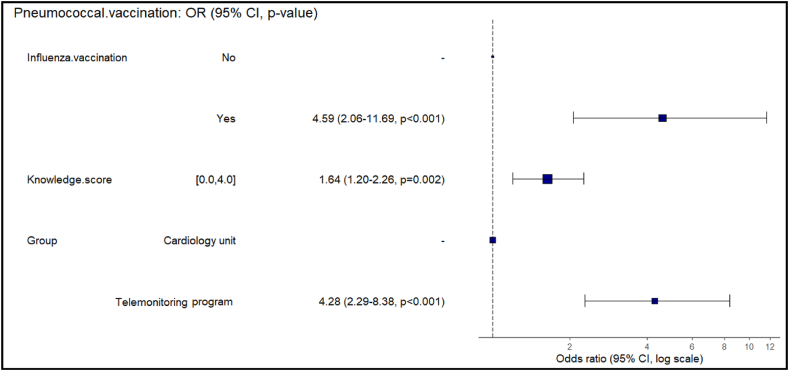
Being male (OR 2.55, p = 0.003) or older patients (OR 2.46, p = 0.011 for patients aged 61 to 74 years; OR 4.27, p < 0.001 for patients over 74 years), having completed the pneumococcal vaccination (OR 4.34, p = 0.001) and a high score on the knowledge questionnaire (OR 1.62, p = 0.001) are factors associated with a better rate of vaccination against influenza (Fig. 1). The telemonitoring program also appears to be a positive factor for influenza vaccination, although it is not significant (OR 1.71, p = 0.074). By contrast, a good medication compliance (OR 1.90, p = 0.369) does not seem to influence influenza vaccination.
Fig. 1.
Multivariate analysis of variables associated with influenza vaccination. (Multivariable logistic regression analysis was performed between influenza vaccine status and gender, age, pneumococcal vaccination, medication compliance, knowledge score, patient's group (cardiology unit or telemonitoring). These variables were those with a p-value <0.2 in univariate analysis. Finally, variables retained were selected using a backward stepwise selection procedure (Akaike Information Criterion).
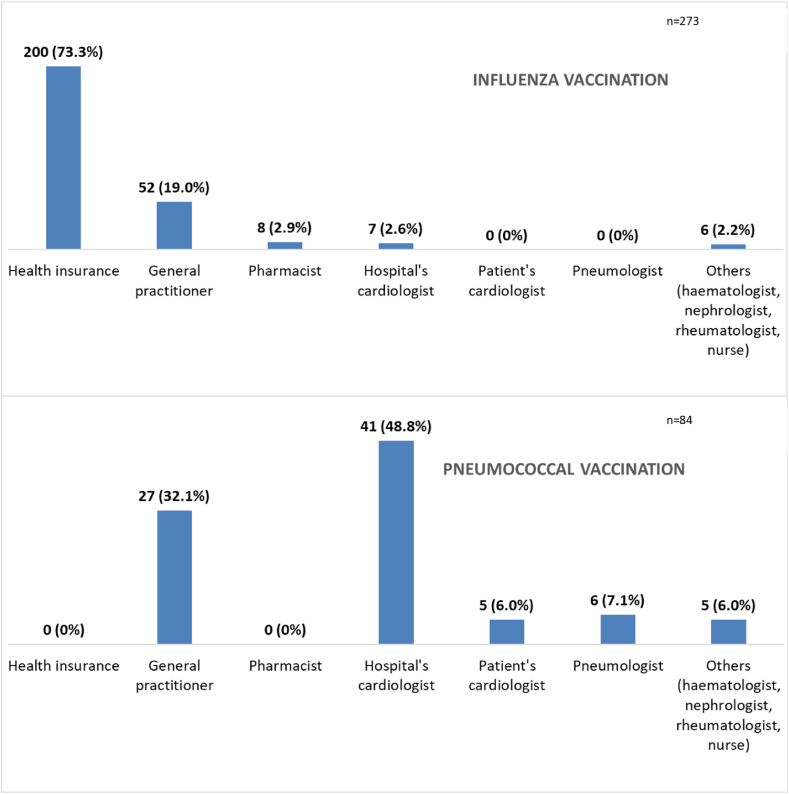
Being vaccinated against influenza (OR 4.59, p < 0.001), having a high knowledge score (OR 1.64, p = 0.002) and being telemonitored (OR 4.28, p < 0.001) are associated with a better vaccination against pneumococcus (Fig. 2).
Fig. 2.
Multivariate analysis of variables associated with pneumococcal vaccination. (Multivariable logistic regression analysis was performed between pneumococcal vaccination status and influenza vaccination, knowledge score and patient's group. These variables were those with a p-value <0.2 in univariate analysis. Finally, variables retained were selected using a backward stepwise selection procedure (Akaike Information Criterion).
3.6. Ways of patients getting information on vaccination
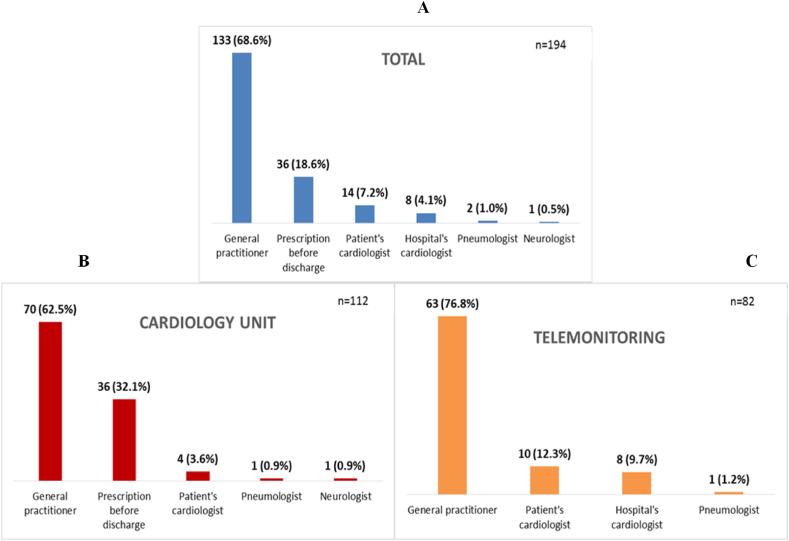
Among the patients who were informed about the necessity of vaccination, information had been provided to them mostly by health insurance (73.3%, n = 200) and their GP (19.0%, n = 52) for influenza and by their cardiologist (54.8%, n = 46) and GP (32.1%, n = 27) for the pneumococcal vaccination (Fig. 3).
Fig. 3.
Way in which patients were informed of the need of vaccination.
3.7. Ways of achieving vaccination
Considering all non-vaccinated patients against influenza or pneumococcus (n = 233), 50.6% patients wishing to be vaccinated (n = 118), 32.2% patients considering the possibility of being vaccinated (n = 75) and 17.2% refused to be vaccinated after the pharmaceutical team has informed them of the need to be vaccinated against influenza and pneumococcus because of their heart failure (n = 40). The main reasons for refusal were lack of interest in vaccines due to ineffectiveness (34.8%), fear of adverse effects (31.9%) and vaccine excipients (15.9%).
Among unvaccinated patients who consider vaccination (n = 194), 68.6% wanted to be vaccinated by their GP (n = 133) and 7.2% wanted to be vaccinated by their cardiologist (n = 14) (Fig. 4A). 32.1% of patients in the cardiology units’ group wanted a prescription at discharge after pharmaceutical intervention during their hospital stay (n = 36) (Fig. 4B). More than 3/4 of patients in telemonitoring program wanted a prescription by their GP (76.9%, n = 63) (Fig. 4C).
Fig. 4.
Preference of unvaccinated patients regarding the health care provider wanted to perform vaccination. (Fig. 4A: all patients; Fig. 4B: patients in cardiology; Fig. 4C: patients in telemonitoring program).
4. Discussion
Vaccination is still the most effective way to reduce morbidity and mortality from infections, especially for patients with chronic diseases. Indeed, similarly to HF, vaccination against influenza is recommended in patients with COPD, to decrease all-cause mortality [17] and in diabetic patients, to decrease hospitalisations and deaths [18,19]. Importantly, both influenza and pneumococcal vaccination have been shown to reduce mortality in haemodialysis patients [20]. Despite this benefit, this study shows that the vaccination coverage of HF patients 1/remains insufficient, 2/is associated with some characteristics of the patients such as the vaccination knowledge or telemonitoring programs, 3/could be improved if more often integrated in the systematic management program.
Vaccination coverage is largely insufficient. This is particularly true regarding pneumococcus with only 22.1% of vaccination, as underlined in another French study, with only 9.1% (on 673 patients) of HF outpatients vaccinated against pneumococcus [21]. Patients in telemonitoring program seem to be more vaccinated for influenza (OR 1.71, p = 0.074) and are significantly more vaccinated for pneumococcus (OR 4.28, p < 0.001) than patients in cardiology units, which could involve better management of HF. Indeed, these patients benefit from therapeutic education interviews and a follow-up by a caregiver team dedicated to this telemonitoring program who monitored the patients and thus allowing a better global management. Also, other physicians including GP but also other cardiologists could be involved in the program, allowing various ways of education. Consistently, these patients are more aware of the factors of HF exacerbation, such as infections, which can be prevented by vaccination. However, there was no difference in the knowledge score about vaccination between the two groups. During the educational interviews, we presume that the importance of vaccinations to avoid HF complications is more frequently discussed than more technical and specific information about vaccines.
The impact of telemonitoring remains a matter of debate. In a meta-analysis including 15 studies conducted between 2003 and 2013, home telemonitoring interventions (especially automated device-based telemonitoring and mobile telemonitoring) reduced the relative risk of all-cause mortality and HF-related hospitalisations compared with usual care [22]. Here, our telemonitoring system is close to the program developed in the OSICAT trial [23]. The primary endpoint was negative in this trial (preventing all-cause deaths or unplanned hospitalisations), but the analyses suggested that some subgroups of patients could draw more benefit, especially the patients with more symptoms, the patients more adherent to the program or the most isolated. New ESC guidelines considered non-invasive telemonitoring for patients with HF in order to reduce the risk of recurrent cardiovascular and HF hospitalisations and cardiovascular death [9].
Lack of awareness among health professionals also leads to a lack of awareness among patients regarding the need to be vaccinated. Actually, only 17% of patients refuse to be vaccinated after being informed of the benefits of vaccination for them. The higher vaccination rate for influenza than for pneumococcus may be explained first by better knowledge about this infection. Indeed, almost half of the patients answered correctly to the question about influenza, compared to only 19% for the question about pneumococcus. Knowledge was found to be the only factor positively influencing both influenza and pneumococcal vaccination. This demonstrates the importance of patient education in their own care.
The better vaccination coverage for influenza can also be attributed to the presence of an annual vaccination campaign from the French medical insurance for HF patients or over 65 years old that does not exist for pneumococcus. Approximately three quarters of patients who were informed of the need for influenza vaccination were informed by the French national health insurance. Older patients tend to be more vaccinated against influenza (OR 2.46, p = 0.011 for patients aged 61 to 74 years; OR 4.27, p < 0.001 for patients over 74 years), which can also be explained by the vaccination campaign, as patients over 65 years of age receive an annual influenza vaccination voucher. Thus, simple patient information could be enough to improve vaccination coverage. It therefore seems more relevant to focus on awareness of vaccination and the need to carry out vaccination rather than on technical aspects and the way vaccines work. Similar measures used for pneumococcal vaccination could drastically increase pneumococcal vaccination coverage and thus reduce the number of hospitalisations or deaths. Indeed, communication campaigns to promote vaccines and the multiplication of means to do this, increase vaccination coverage [24], and it is estimated that about 2000 deaths are avoided each year in France thanks to flu vaccination [25]. There is however no data for HF patients.
Other options can also be considered to improve vaccination coverage, such as the use of a computerised vaccination management application for general practitioners (electronic shared medical records with notifications for GP's), the simplification of the vaccination process (diversification of the locations of vaccination and the professionals authorised to vaccinate) and the updating of health professionals' knowledge on vaccination guidelines [26].
We notice that patients who received either the influenza or pneumococcal vaccine are more likely to have received the other vaccine. This seems to demonstrate that patients vaccinated against a disease are generally in favour of any type of vaccination and supports the idea that better information on the need for vaccination would improve vaccination coverage. We can therefore also assume that patients vaccinated against influenza and pneumococcus would be more susceptible to receive the Sars-Cov-2 vaccine and inversely.
About two thirds of patients wanted to be vaccinated by their GP, who thus play a major role in their global care. According to a study investigating the patients’ point of view about preventive care in Switzerland, preventive care should be the mission of their GP (84.1%) and they consider him/her to be the best source of information in this domain (83.4%). About 72% of them consider they are very well or well informed about immunization [27].
Each healthcare professional has a role to play in promoting vaccination in order to inform the patient. The hospital admission, specifically when a patient has a complication of HF, is an opportunity to consider the prevention of acute HF and to prevent it through vaccination. Hospital health professionals (doctors, nurses, pharmacists) can play an important role in the vaccination of HF patients. Indeed, among unvaccinated patients, more than 80% wanted or were considering vaccination and approximately one-third of hospitalized patients wish to have a vaccine prescription at discharge on the advice of the pharmaceutical team. In a US study including patients vaccinated against influenza, pneumococcal vaccination coverage was better when influenza vaccination was performed by a pharmacist compared to standard care. The pharmacist asked patients about their risk of pneumococcal disease (e.g., age, smoking status, co-morbid conditions) and recommended vaccination if any risk was identified [28]. In another study looking at the influenza vaccination coverage of patients with rheumatoid arthritis, it was demonstrated that a multimodal implementation strategy including patient recalls, a nurse providing vaccines, and physician reminders resulted in an increase in the vaccination coverage from 48.5% to 62.6% [29]. This demonstrates once again that the more sources of information on vaccination there are, the better the vaccination coverage. As such, the promotion of vaccination can be carried out by all health professionals in charge of a patient in order to increase the chances of its implementation.
Different measures can be derived from the data of this study that will presumably help to increase vaccination coverage of patients with HF. Presumably, these will include inclusion in a managed care program (as recommended by the guidelines), increasing awareness of vaccination in the hospital and during ambulatory care, and providing easy access to vaccination through the general practitioner as well as all other health professionals.
In summary, this study shows that it’s crucial to improve educational and organisational aspects in order to reinforce awareness and accessibility to vaccination.
4.1. Study limitations
Our observational study also has some limitations. This was a monocentric study, so conducting the study in other hospitals would have provided a larger sample size and avoided possible prescriber bias. This is limited by inclusions of patients followed in the telemonitoring program which cover a large part of our geographical region.
The age and the stage of the HF were not collected in this study because of the difficulty to collect this information, but we didn't recruit patients admitted for the first HF exacerbation.
The rate of hospitalisation for pulmonary infection appears to be low compared with the literature [5]. This may be explained by the difficulty in collecting the etiology of the cardiac exacerbation responsible for the hospitalisation from the medical records.
Finally, the knowledge score was set up arbitrarily according to our experience as there is no standardised knowledge questionnaire on vaccination. When a question was confusing and the patient had questions about it, the pharmacist conducting the interview guided the patient by giving him explanations. This study was conducted prior to the availability of COVID vaccines in France. It is possible that patients’ perception of vaccination has changed since the introduction of the COVID vaccines.
5. Conclusion
Influenza and pneumococcal vaccination coverage of HF patients are still largely insufficient. This remains essential to improve, as patients with HF are likely to draw major benefits (fewer exacerbations lead to less admissions and readmissions and lower mortality).
Improving patients' knowledge about vaccination is an independent factor for better vaccination coverage and could then be a powerful approach to improve the situation. To this purpose, it is crucial to educate health professionals and to carry out public health campaigns about the benefits of vaccinations. The medical team, including the clinical pharmacist by his dedicated time during medication reconciliation may play a major role in the management of hospitalized patients as well as GP's as local actors.
Author contribution statement
Adrien Maire, Nicolas Chapet: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Wrote the paper.
S. Aguilhon, M. Rigoni, Betty Mathieu, Yohan Audurier, Cyril Breuker, Gaëlle de Barry, Anne Jalabert, Florence Leclercq, Jean-Luc Pasquié: Analyzed and interpreted the data.
Laugier Marie Lucie, P. Laffont-Lozes: Performed the experiments.
François Roubille, Audrey Castet-Nicolas: Conceived and designed the experiments; Analyzed and interpreted the data; Wrote the paper.
Data availability statement
Data will be made available on request.
Institutional review board statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of Montpellier University Hospital (protocol code IRB-MTP_2020_07_202000541 approved on July 16, 2020).
Informed consent statement
Informed consent was obtained from all subjects involved in the study.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Roubille Francois reports a relationship with Pfizer Inc that includes: consulting or advisory. CHAPET Nicolas reports a relationship with Pfizer Inc that includes: consulting or advisory.
Contributor Information
Adrien Maire, Email: adrien219.maire@laposte.net.
Nicolas Chapet, Email: n-chapet@chu-montpellier.fr.
Marie-Lucie Laugier, Email: lmarielucie@yahoo.fr.
Paul Laffont-Lozes, Email: paul.laffontlozes@chu-nimes.fr.
Mélinda Rigoni, Email: melinda.rigoni@gmail.com.
Betty Mathieu, Email: betty-mathieu@chu-montpellier.fr.
Yohan Audurier, Email: yaudurier@chicacr.fr.
Cyril Breuker, Email: c-breuker@chu-montpellier.fr.
Gaëlle de Barry, Email: g-de_barry@chu-montpellier.fr.
Anne Jalabert, Email: a-jalabert@chu-montpellier.fr.
Florence Leclercq, Email: f-leclercq@chu-montpellier.fr.
Jean-Luc Pasquié, Email: jl-pasquie@chu-montpellier.fr.
François Roubille, Email: f-roubille@chu-montpellier.fr.
Audrey Castet-Nicolas, Email: audrey-castet@chu-montpellier.fr.
Appendices.
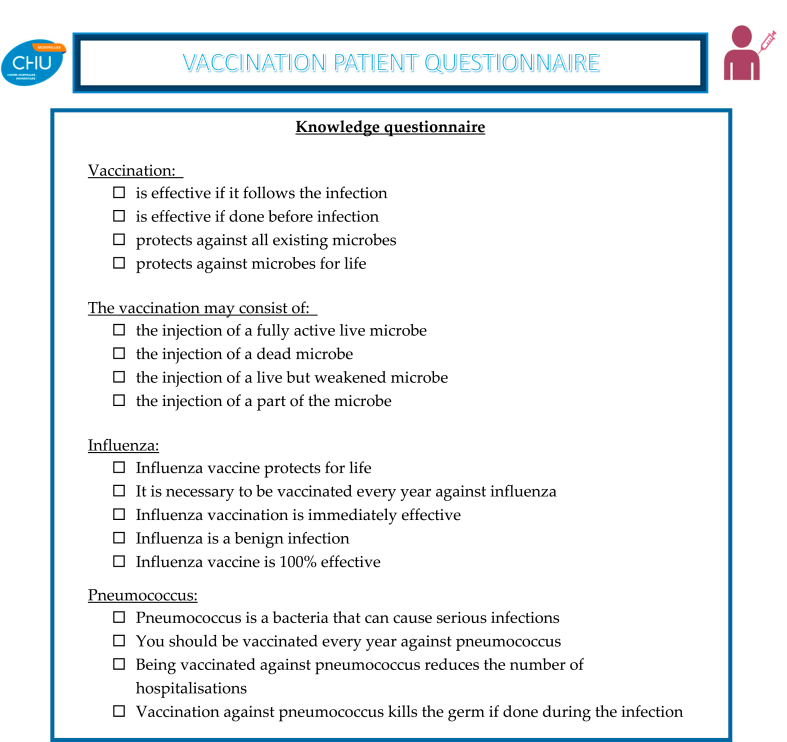
Appendix A. Vaccination patient questionnaire
| Influenza Vaccination | OR (95% CI, p-value) | |
|---|---|---|
| Gender | Male | 1.64 (0.97–2.77, p = 0.063) |
| Age | [61–74] | 2.00 (1.10–3.67, p = 0.024) |
| Age | [> 74] | 2.44 (1.29–4.66, p = 0.006) |
| Pneumococcal vaccination | Yes | 6.30 (2.94–15.65, p < 0.001) |
| LVEF | HFrEF | 0.99 (0.61–1.59, p = 0.952) |
| Medication compliance | Good | 3.18 (0.84–12.06, p = 0.081) |
| Medication compliance | Moderate | 1.31 (0.35–4.90, p = 0.677) |
| History of hospitalisation for pulmonary infection | 1.81 (0.82–4.41, p = 0.164) | |
| Knowledge score | 1.63 (1.26–2.13, p < 0.001) | |
| Group | Telemonitoring program | 1.76 (1.09–2.87, p = 0.021) |
Appendix B. Univariate analysis of variables associated with influenza vaccination
LVEF: Left Ventricular Ejection Fraction HFrEF: Heart failure with reduced ejection fraction.
| Pneumococcal Vaccination | OR (95% CI, p-value) | |
|---|---|---|
| Gender | Male | 0.82 (0.46–1.50, p = 0.510) |
| Age | [61–74] | 1.57 (0.79–3.24, p = 0.208) |
| Age | [> 74] | 0.81 (0.37–1.78, p = 0.589) |
| Influenza vaccination | Yes | 6.30 (2.94–15.65, p < 0.001) |
| LVEF | HFrEF | 1.39 (0.81–2.39, p = 0.234) |
| Medication compliance | Good | 7499610.33 (0.00-NA, p = 0.983) |
| Medication compliance | Moderate | 2879850.37 (0.00-NA, p = 0.984) |
| History of hospitalisation for pulmonary infection | 1.24 (0.52–2.71, p = 0.610) | |
| Knowledge score | 1.81 (1.36–2.46, p < 0.001) | |
| Group | Telemonitoring program | 4.58 (2.52–8.71, p < 0.001) |
Appendix C. Univariate analysis of variables associated with pneumococcal vaccination
LVEF: Left Ventricular Ejection Fraction HFrEF: Heart failure with reduced ejection fraction.
References
- 1.Mosterd A., Hoes A.W. Clinical epidemiology of heart failure. Heart. 2007;93(9):1137–1146. doi: 10.1136/hrt.2003.025270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maggioni A.P., Dahlström U., Filippatos G., Chioncel O., Leiro M.C., Drozdz J., et al. EURObservationalResearch programme : regional differences and 1-year follow-up results of the heart failure pilot survey (ESC-HF pilot) Eur. J. Heart Fail. 2013;15(7):808–817. doi: 10.1093/eurjhf/hft050. [DOI] [PubMed] [Google Scholar]
- 3.Bhatt A.S., DeVore A.D., Hernandez A.F., Mentz R.J. Can vaccinations improve heart failure outcomes. JACC (J. Am. Coll. Cardiol.) : Heart Fail. 2017;5(3):194–203. doi: 10.1016/j.jchf.2016.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alon D., Stein G.Y., Korenfeld R., Fuchs S. Predictors and outcomes of infection-related hospital admissions of heart failure patients. PLoS One. 2013;8(8) doi: 10.1371/journal.pone.0072476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fonarow G., Abraham W., Albert N., Stough W., Gheorghiade M., Greenberg B., et al. Factors identified as precipitating hospital admissions for heart failure and clinical outcomes. Arch. Intern. Med. 2008;168(8):847. doi: 10.1001/archinte.168.8.847. [DOI] [PubMed] [Google Scholar]
- 6.Calendrier des vaccinations et recommandations vaccinales . 2019. (Ministère des solidarités et de la santé)(consulted on december 2019) [Google Scholar]
- 7.HAS – Guide du parcours de soins/Insuffisance cardiaque – Juin. 2014. [Google Scholar]
- 8.Stratégie de vaccination contre le Sars-Cov-2 - Actualisation des facteurs de risque de formes graves de la Covid-19 et des recommandations sur la stratégie de priorisation des populations à vacciner. 2021. https://www.has-sante.fr/jcms/p_3240117/fr/strategie-de-vaccination-contre-le-sars-cov-2-actualisation-des-facteurs-de-risque-de-formes-graves-de-la-covid-19-et-des-recommandations-sur-la-strategie-de-priorisation-des-populations-a-vacciner 2 mars). Haute Autorité de Santé. consulted on. [Google Scholar]
- 9.McDonagh T.A., Metra M., Adamo M., Gardner R.S., Baumbach A., Böhm M., et al. European Heart Journal; 2021. 2021 ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure. Published. [DOI] [PubMed] [Google Scholar]
- 10.Vardeny O., Claggett B., Udell J.A., Packer M., Zile M., Rouleau, et al. Influenza vaccination in patients with chronic heart failure. JACC (J. Am. Coll. Cardiol.) : Heart Fail. 2016;4(2):152–158. doi: 10.1016/j.jchf.2015.10.012. [DOI] [PubMed] [Google Scholar]
- 11.Influenza Vaccine to Prevent Adverse Vascular Events – IVVE. Presented by Dr. Mark Loeb at the American College of Cardiology Annual Scientific Session. ACC 2022); Washington, DC: 2022. April 3. [Google Scholar]
- 12.Girerd N., Chapet N., Roubille C., Roncalli J., Salvat M., Mouquet F., et al. Vaccination for respiratory infections in patients with heart failure. J. Clin. Med. 2021;10(19):4311. doi: 10.3390/jcm10194311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lipsky B.A. Risk factors for acquiring pneumococcal infections. Arch. Intern. Med. 1986;146(11):2179–2185. doi: 10.1001/archinte.146.11.2179. [DOI] [PubMed] [Google Scholar]
- 14.Boey L., Bosmans E., Ferreira L.B., Heyvaert N., Nelen M., Smans L., et al. Vaccination coverage of recommended vaccines and determinants of vaccination in at-risk groups. Hum. Vaccines Immunother. 2020;16(9):2136–2143. doi: 10.1080/21645515.2020.1763739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Girerd X., Hanon O., Anagnostopoulos K., Ciupek C., Mourad J.J., Consoli S. Evaluation de l'observance du traitement antihypertenseur par un questionnaire : mise au point et utilisation dans un service spécialisé. Presse Med. 2001:1044–1048. [PubMed] [Google Scholar]
- 16.Ponikowski P., Voors A.A., Anker S.D., Bueno H., Cleland J.G.F., Coats A.J.S., et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2016;37(27):2129–2200. doi: 10.1093/eurheartj/ehw128. [DOI] [PubMed] [Google Scholar]
- 17.Schembri S., Morant S., Winter J.H., MacDonald T.M. Influenza but not pneumococcal vaccination protects against all-cause mortality in patients with COPD. Thorax. 2009;64(7):567–572. doi: 10.1136/thx.2008.106286. [DOI] [PubMed] [Google Scholar]
- 18.Vamos E.P., Pape U.J., Curcin V., Harris M.J., Valabhji J., Majeed A., et al. Effectiveness of the influenza vaccine in preventing admission to hospital and death in people with type 2 diabetes. Can. Med. Assoc. J. 2016;188(14):E342–E351. doi: 10.1503/cmaj.151059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lau D., Eurich D.T., Majumdar S.R., Katz A., Johnson J.A. Effectiveness of influenza vaccination in working-age adults with diabetes : a population-based cohort study. Thorax. 2013;68(7):658–663. doi: 10.1136/thoraxjnl-2012-203109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bond T.C., Spaulding A.C., Krisher J., McClellan W. Mortality of dialysis patients according to influenza and pneumococcal vaccination status. Am. J. Kidney Dis. 2012;60(6):959–965. doi: 10.1053/j.ajkd.2012.04.018. [DOI] [PubMed] [Google Scholar]
- 21.Kopp A., Mangin O., Gantzer L., Lekens B., Simoneau G., Ravelomanantsoa M., et al. Pneumococcal vaccination coverage in France by general practitioners in adults with a high risk of pneumococcal disease. Hum. Vaccines Immunother. 2020;17(1):162–169. doi: 10.1080/21645515.2020.1756669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kitsiou S., Paré G., Jaana M. Effects of home telemonitoring interventions on patients with chronic heart failure : an overview of systematic reviews. J. Med. Internet Res. 2015;17(3):e63. doi: 10.2196/jmir.4174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Galinier M., Roubille F., Berdague P., Brierre G., Cantie P., Dary P., et al. Telemonitoring versus standard care in heart failure : a randomised multicentre trial. Eur. J. Heart Fail. 2020;22(6):985–994. doi: 10.1002/ejhf.1906. [DOI] [PubMed] [Google Scholar]
- 24.Yoo B.K., Holland M.L., Bhattacharya J., Phelps C.E., Szilagyi P.G. Effects of mass media coverage on timing and annual receipt of influenza vaccination among medicare elderly. Health Serv. Res. 2010;45(5p1):1287–1309. doi: 10.1111/j.1475-6773.2010.01127.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vaccination contre la grippe saisonnière. 2021. https://www.ameli.fr/pharmacien/exercice-professionnel/services-patients/vaccination-grippe-saisonniere Ameli. consulted on. [Google Scholar]
- 26.Berrada S., Caroff N., Navas D., Moret L., Huon J. Comment améliorer la couverture vaccinale en France ? Étude qualitative auprès de professionnels de santé. Ann. Pharm. Fr. 2021;79(1):77–85. doi: 10.1016/j.pharma.2020.09.004. [DOI] [PubMed] [Google Scholar]
- 27.Cohidon C., Imhof F., Bovy L., Birrer P., Cornuz J., Senn N. Patients' and general practitioners' views about preventive care in family medicine in Switzerland : a cross-sectional study. J. Prev. Med. Pub. Heal. 2019;52(5):323–332. doi: 10.3961/jpmph.19.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Taitel M., Cohen E., Duncan I., Pegus C. Pharmacists as providers : targeting pneumococcal vaccinations to high risk populations. Vaccine. 2011;29(45):8073–8076. doi: 10.1016/j.vaccine.2011.08.051. [DOI] [PubMed] [Google Scholar]
- 29.Valerio V., Bazan M.C., Wang M., Mazer B.D., Pineau C.A., Hazel E.M., et al. A multimodal intervention increases influenza vaccine uptake in rheumatoid arthritis. Clin. Rheumatol. 2020;40(2):575–579. doi: 10.1007/s10067-020-05435-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.