Abstract
Purpose
Electric bicycles (e-bikes) achieve higher speeds than pedal bicycles, but few studies have investigated the impact on injury rates specific to the pediatric population. Utilizing the National Electronic Injury Surveillance System (NEISS), we compared rates of pediatric injury for e-bikes, bicycles, and gas-engine bicycles (mopeds) from 2011 to 2020.
Methods
Descriptive and bivariate inferential analyses were performed upon NEISS estimates of e-bike, bicycle, and moped injuries in children aged 2–18 years. Analyses were stratified by patient age and helmet usage. The Mann-Kendall test of trends was used.
Results
We identified 3945 e-bike, 23,389 moped, and 2.05 million bicycle injuries. Over time, the incidence of injury increased for e-bikes (Kendall's τ=0.73, p = 0.004), decreased for pedal bicycles (Kendall's τ= − 0.91, p = 0.0003), and did not change for mopeds (Kendall's τ = 0.06, p = 0.85). Males accounted for 82.5 % of e-bike injuries. The age group most commonly affected by e-bike injury (44.3 %) was 10–13 years old. The proportion of injuries requiring hospitalization was significantly higher for e-bikes (11.5 %), compared to moped and bicycle (7.0 and 4.8 %, respectively, p < 0.0001). In cases where helmet use or absence was reported, 97.3 % of e-bike riders were without a helmet at the time of injury, compared to 82.1 % of pedal bicycle riders and 87.2 % of moped riders.
Conclusions
The rate of pediatric e-bike injuries increased over the study period. Compared to riders on pedal bicycles or mopeds, children on e-bikes had infrequent helmet use and increased rate of hospitalization. These findings suggest that attention to e-bike safety and increasing helmet usage are important to public health among the pediatric population.
Level of evidence
IV.
Keywords: Bicycle trauma, Pediatric injury, Electric bicycles, E-bike, Motorized bicycle
Highlights
-
•What is currently known about this topic?
-
•E-bikes cause serious injuries in children and adults, previously shown in single institution studies.
-
•National trends in pediatric e-bike injuries are unknown.
-
•Helmet usage helps prevent serious brain and facial injuries, and the usage rates on e-bikes are not known.
-
•
-
•What new information is contained in this article?
-
•Pediatric e-bike injuries increased during 2011-2020, while bicycle injuries decreased.
-
•E-bike injuries in children more frequently required hospital admission or transfer compared to pedal bicycle injuries.
-
•Helmet status was infrequently reported in this dataset.
-
•More research is needed to determine the frequency of helmet use with e-bikes.
-
•
Introduction
Electric bicycles (e-bikes) are an increasingly common choice for recreation and commuting, with an estimated 500,000 sold in 2020 in the United States (US), and sales expected to continue to rise [1]. Reasons for the increase include zero emissions, more bicycle infrastructure, higher cost of gasoline, and lower travel cost compared to gas-powered vehicles [2]. In the Netherlands, e-bike trips have been found to replace not just conventional bicycle trips, but in some cases commuting trips that would otherwise have been made in automobiles [3]. E-bikes are capable of reaching 20 mph without pedal assistance, and are not regulated as motor vehicles under US law [4]. Because maximum e-bike speeds (approximately 30 miles per hour (mph)) can exceed those attainable by traditional pedal bicycles [5,6], these e-bikes are a subject of increasing public health concern, for riders as well as pedestrians.
A nation-wide study of injuries due to e-bikes and electric scooters across all age groups demonstrated that e-bike accidents were more likely to result in hospitalization, internal injury, and concussion, compared to pedal bicycle accidents [7]. Since e-bikes can achieve higher speeds with less effort than traditional pedal bicycles, and pediatric riders may not wear helmets, significant injuries, including facial fractures and intracranial hemorrhage, are common among the pediatric population [8,9].
A single-center study conducted in 2015 demonstrated increased rates of intraabdominal injury and higher injury severity scores (ISS) among children using e-bikes compared to pedal bicycles [10]. Similar findings of higher ISS, as well as more multisystem trauma, were demonstrated in another single-center study focusing on 2015–2017 pediatric data [11]. To date, there is a paucity of national data specific to e-bike injuries in children. This study aims to use data from the National Electronic Injury Surveillance System (NEISS) to compare pediatric injuries incurred on e-bikes vs. pedal bicycles. We hypothesized that the frequency and severity of pediatric e-bike injuries had increased over time. Therefore, we compared two time periods, 2011–2015 and 2016–2020. Additional comparisons between pediatric users of e-bikes and mopeds (gasoline-powered bicycles) were made to address the gap in published research on injury associated with e-bike use in children, which has not included a comparison of e-bikes vs. mopeds, despite similarities in the demographics of users [7].
Material and methods
Data source
The NEISS is a nationally representative probability sample of approximately 100 hospital emergency departments, including approximately 20 pediatric emergency departments, geographically distributed throughout the US and its territories [12]. NEISS data is collected by the Consumer Products Safety Commission (CPSC) and is used to generate national estimates of injury frequency related to specific consumer product categories and sub-categories. The data collected by emergency departments and reported to NEISS include age, race, ethnicity, gender, date of injury, injury diagnosis, anatomic region of injury, admission to the hospital, and circumstances related to injury. This project was deemed exempt by the Children's Hospital Orange County Institutional Review Board, with a waiver of consent granted due to use of a deidentified national database. It was not appropriate or possible to involve patients or the public in the design, or conduct, or reporting, or dissemination plans of our research.
Inclusion/exclusion criteria
Reports of injuries that occurred during the period from 2011 to 2020 in individuals 2–18 years of age were identified from NEISS using the consumer product codes for “Bicycles and Accessories (Excluding All Terrain Bicycles)” (5040) and “Mopeds or Powered Bicycles” (3215). Presence of the terms “motor” and “electric” in the narrative field was used to differentiate electric-powered bicycles from gas-powered “mopeds.” Only records with statistical weights in the appropriate NEISS field were included. Statistical weights were used to generate population estimates related to frequency of injury related to demographic and clinical variables. Complete data for other variables related to anatomic site or nature of injury were not used as a criterion for exclusion, as patients with partial data could still contribute to variable-specific estimates.
Study variables
The variables examined included: patient age (continuous variable); age categorized as 2–5 years, 6–9 years, 10–13 years, and 14–18 years; gender; race; ethnicity; year of injury (aggregated into 5-year blocks as 2011–201 or 2016–2020); month of injury; anatomic site of injury (upper extremity, lower extremity, head and neck, face, trunk, or other); diagnosis (hemorrhage, dental injury, avulsion, dislocation, concussion, laceration, contusion, puncture, fracture, other). Presence or absence of the following characteristics was assessed as binary variables: concussion, fracture, internal injury, discharge from the emergency department. Narrative text was used to determine whether the individual used a protective device (helmet) at the time of injury. Data recorded in NEISS were complete across all sampled instances except for variables tracking Hispanic ethnicity, blood alcohol testing, drug testing, secondary diagnosis, and injury to second anatomic site. Hispanic ethnicity was excluded from this study due to the large proportion on missingness.
Statistical analysis
National estimates of pediatric two-wheeled vehicle injury were generated by applying sample weights developed by the NEISS. Estimates were created by multiplying an observation by the sample weight and summing within a given category. NEISS recommendations for national estimates require the restriction of results for groups with <20 actual cases, as the size of sample at this level may suffer from instability. If there is a coefficient of variation >33 % or an estimate generated that is <1200, NEISS states that these estimates may also be unstable. For this study, estimates were restricted based upon coefficient of variation and the number of actual cases observed. As this analysis was both exploratory and descriptive, estimates of 1200 that were contained within an estimate's 95 % confidence interval were also included. For comparison of frequency by strata, the chi-square test of independence was used. The Mann-Kendall test of trend was used to test the hypothesis of whether the frequency of injury estimates was distributed randomly, or whether an alternative hypothesis that injury estimates followed a monotonic trend over time should be considered. Missing data was excluded from all bivariate inferential statistical analysis. Alpha values <0.05 were considered statistically significant. Kendall's Tau is reported along with Mann-Kendall p-values, to describe concordance/discordance between measures of time and estimated frequency of injury. R statistical programming language (Vienna, Austria) 4.03 was used for all analyses.
Results
Patient characteristics
The relative distribution of e-bike, pedal bicycle, and moped use as the cause of injury varied significantly across age groups (p < 0.0001, Table 1). Over a 10-year period (2011–2020), e-bikes were estimated to injure 3945 children between the ages of 2–18 years treated in emergency departments in the US. Most e-bike injuries (82.5 %) occurred in male patients, and the average age of injury was 12.1 years. The number of pediatric injuries due to conventional bicycle use was estimated at 2,048,826 between 2011 and 2020. Most conventional bicycle injuries 1,451,240 (70.8 %) occurred in male patients. The average age of pediatric bicycle injury was 7.3 years. There were 23,300 pediatric injuries estimated for gas-powered two-wheeled vehicles classified as “mopeds” from 2011 to 2020, with males accounting for 69.6 % (16,298 estimated cases) and average age of 14.6 years.
Table 1.
Estimated distribution of demographics by vehicle type.
| Characteristic | Electric bicycle |
Moped |
Bicycle |
p-Value | |||
|---|---|---|---|---|---|---|---|
| Estimate | 95 % CI | Estimate | 95 % CI | Estimate | 95 % CI | ||
| Age | <0.0001 | ||||||
| 2–5 years | 680 (17.2 %) | 433–927 | 2845 (13.1 %) | 2088–3601 | 291,204 (14.2 %) | 177,214–405,195 | |
| 6–10 years | 421 (10.6 %) | 274–569 | 5560 (25.6 %) | 4180–6940 | 581,131 (28.3 %) | 366,066–796,195 | |
| 10–13 years | 1747 (44.3 %) | 673–1509 | 1411 (6.50 %) | 904–1917 | 665,564 (32.4 %) | 431,548–899,580 | |
| 14–18 years | 1091 (27.6 %) | 1217–2276 | 11,874 (54.7 %) | 8668–15,080 | 510,925 (24.9 %) | 353,636–668,214 | |
| Sex | <0.0001 | ||||||
| Male | 3257 (82.5 %) | 2227–4288 | 16,298 (69.6 %) | 11,809–20,786 | 1,451,240 (70.8 %) | 940,921–1,961,559 | |
| Female | 687 (17.4 %) | 378–997 | 7091 (30.3 %) | 5289–8894 | 597,585 (29.1 %) | 386,169–809,001 | |
| Race | <0.0001 | ||||||
| Native American | 112 (2.84 %) | 89–135 | 153 (0.65 %) | 126–179 | 11,395 (0.55 %) | 9055–13,735 | |
| African American | 651 (16.5 %) | 386–915 | 3248 (13.8 %) | 2277–42,220 | 216,430 (10.5 %) | 106,516–326,344 | |
| Not stated | 1002 (25.4 %) | 613–1392 | 8464 (36.1 %) | 5628–11,299 | 606,737 (29.6 %) | 397,822–815,653 | |
| Other | 191 (4.84 %) | 88–293 | 390 (1.66 %) | 227–553 | 14,695 (0.71 %) | 90,793–203,097 | |
| White | 1987 (50.3 %) | 1465–2509 | 11,117 (47.5 %) | 9096–13,138 | 1,046,073 (51.0 %) | 720,897–1,371,250 | |
| Ethnicity | NA | ||||||
| Non-Hispanic | 620 (39.4 %) | 383–857 | 2703 (50.6 %) | 2046–3360 | 115,604 (37.5 %) | 67,496–163,712 | |
| Hispanic | 180 (11.4 %) | 99–260 | 152 (2.85 %) | 75–229 | 25,900 (8.4 %) | 12,673–39,126 | |
| Not stated | 773 (49.1 %) | 476–1070 | 2478 (46.4 %) | 1827–3129 | 165,994 (53.9 %) | 106,330–225,658 | |
CI, confidence interval.
Change in rate of injury over time
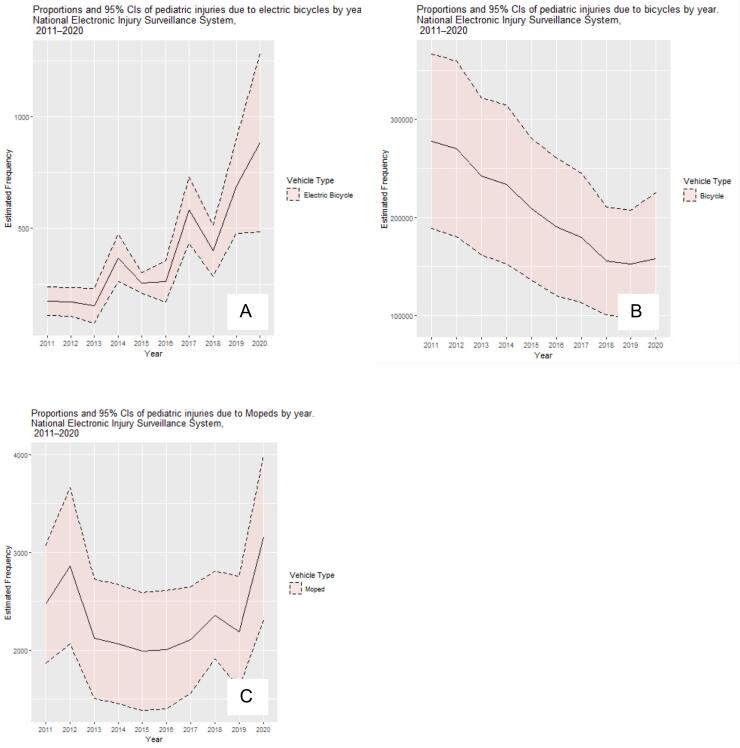
The rate of injury associated with e-bike use increased from 2011 to 2020 (Mann-Kendall p = 0.004, tau = 0.73, Fig. 1A), while the rate of injury associated with pedal bicycle use decreased over the same period (Kendall's tau = −0.91 p = 0.0003, Fig. 1B). There was no significant correlation between moped injury frequency and time (Kendall's Tau = 0.06, p = 0.48, Fig. 1C).
Fig. 1.
Frequency of injury by year and vehicle type. (A) E-bike, (B) Pedal bicycle, (C) moped.
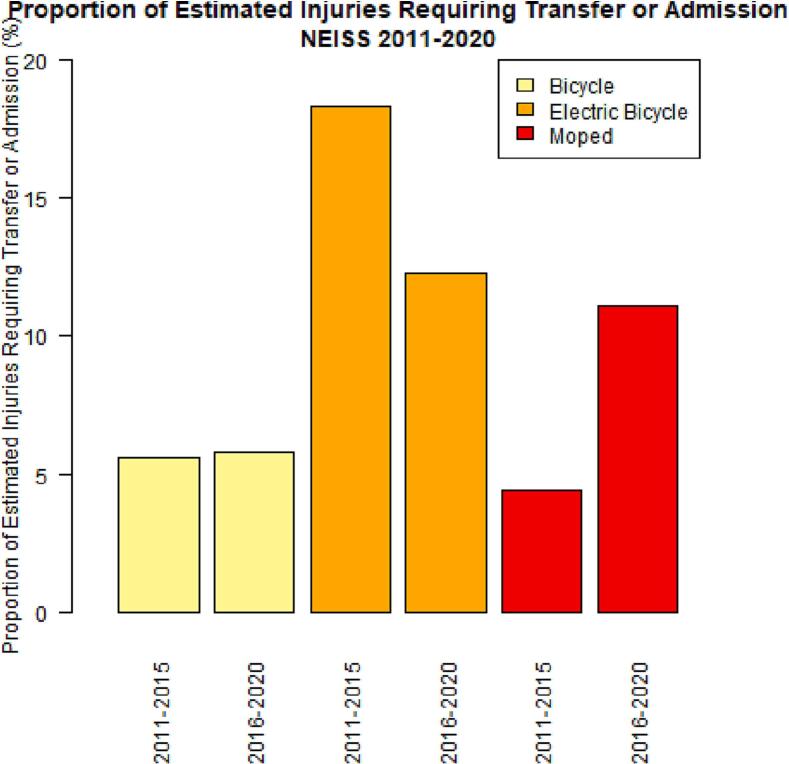
Overall, severity of injury defined as hospital hold/admission or transfer was estimated at 455 (11.5 %), with the remaining patients treated at the emergency department and released. When we compared the rate of injury requiring transfer or admission between the first and second halves of the study period (2011–2015 vs. 2016–2020, respectively), by vehicle type, we observed a decrease from 18.3 % to 12.2 % for e-bikes, an increase from 5.1 % to 5.7 % for pedal bicycles, and an increase from 4.0 % to 11.0 % for mopeds (p < 0.0001, Fig. 2).
Fig. 2.
Proportion of injuries requiring hospital transfer or admission, by vehicle type.
Injury characteristics
The most prevalent injuries among patients with e-bike injury were laceration (18.1 %), fracture (21.4 %), internal injury (14.6 %), and concussion (4.4 %) (Table 2). The anatomic sites most affected were head/neck/face (34.9 %), lower extremity (36 %), upper extremity (23.8 %), and trunk 204 (5.1 %). Most e-bike injuries (with reported location) took place on surface streets 2158 (54.7 %), with other common areas being at home (13.6 %), public areas (2 %), and sporting complexes (0.3 %).
Table 2.
Proportion of vehicle-specific injuries requiring admission or transfer during the period from 2011 to 2020.
| Bicycle |
E-bike |
Moped |
p-Value⁎ | ||||
|---|---|---|---|---|---|---|---|
| 2011–2015 | 2016–2020 | 2011–2015 | 2016–2020 | 2011–2015 | 2016–2020 | ||
| Treated and released | 1,169,029 (94.8 %) | 786,514 (94.2 %) | 919 (81.8 %) | 2474 (87.7 %) | 10,991(95.5 %) | 10,492 (88.9 %) | <0.0001 |
| Admitted or transferred | 63,514 (5.1 %) | 48,330 (5.7 %) | 205 (18.3 %) | 345 (12.2 %) | 509 (4.4 %) | 1306 (11.0 %) | |
p-Value for e-bike proportion of admission/transfer compared to bicycle and moped.
Pedal bicycle riders were found to have injury related to contusion (25.4 %), laceration (21.5 %), fracture (20 %), and concussion (3.0 %). Site of injury was most commonly reported as upper extremity (34.1 %), head/neck/face (31.4 %), lower extremity (25 %), and trunk (8.4 %). Location where the injury occurred was documented as on the street (29.8 %), at home (18.9 %), or not reported 808,627 (39.4 %). Of the 5.1 % with reported helmet status, 82.1 % reported no helmet use at the time of injury.
In moped riders, the injuries observed with the greatest frequency were contusion (33.6 %), fracture (17.6 %), strain (10.2 %), internal injury (9.8 %), and concussion (4.8 %). The anatomic sites most affected were lower extremity (38.1 %), upper extremity (29.4 %), head/neck/face (24.1 %), and trunk (5.2 %). The most common locations for moped injuries were the street (60.7 %), unknown (23.5 %), and at home 2445 (10.4 %). Helmet use was detected in review of narrative for moped injury in 7.1 % of estimated cases. Of those with reported helmet status, 87.2 % were reported to be without a helmet when injured.
Internal injuries were more common among injuries due to e-bikes (14.6 %), compared to bicycles (8.5 %) and mopeds (9.8 %) (p < 0.0001). The same was true of fractures (e-bike, 21.4 %; bicycle, 20.0 %; moped, 17.8 %) (p < 0.0001). Powered two-wheeled vehicles (mopeds and e-bikes) had significantly higher proportions of lower extremity injury than bicycles (e-bike, 36 %; bicycle, 25 %; moped, 38.1 %; p < 0.0001). In contrast, bicycles and e-bikes had a higher proportion of head/neck/face injury (31.4 % and 34.9 %, respectively), compared to mopeds (24.1 %, p < 0.0001). Upper extremity injuries were observed more frequently in moped and bicycle riders (29.4 % and 34.1 %, respectively), compared to e-bikes (23.8 %, p < 0.0001). E-bike riders reported the largest proportion of secondary injury and second anatomic site (17.8 %) compared to moped (12.0 %) and bicycle (4.5 %) (Supplemental Table 1).
The proportion of injuries requiring admission, hold, or transfer were significantly higher among e-bike associated injury (11.5 %) when compared to moped and bicycle (7.0 and 4.8 %, respectively, p < 0.0001). There was 2.4 times greater odds of severe injury for e-bikes compared to pedal bicycles (OR 2.4, 95 % CI 2.1–2.6, p < 0.0001). When comparing e-bike with moped, there was 1.7 times increased odds of severe injury (OR = 1.71, 95 % CI = 1.5–1.9, p < 0.0001). Given the small number of cases with data on helmet status, statistical comparison was not possible.
Discussion
This study of pediatric e-bike injuries from 2011 to 2022 using the NEISS database demonstrates that, in the US, pediatric e-bike–related injuries are uncommon compared to bicycle- and moped-related injuries. Importantly, the rate of e-bike injury among children increased during the study period. The results of subgroup analysis showed that 2-wheeled vehicle injury was most associated with e-bike use in children 14–18 years of age, but with pedal bike use in those 10–13 years of age. Similarly, DiMaggio et al. found that the overall age group distribution for pedal bicycle injuries skewed notably younger than that for e-bike injuries.
While the overall incidence of pediatric e-bike injury increased from 2011–2015 to 2016–2020, the incidence of pedal bicycle-related injury in children decreased over the same period. A decline in pediatric bicycle injury was also demonstrated in a US national study from 2006 to 2012 [13]. Additional information will be necessary to determine whether the decline in the rate of pediatric bicycle injury is correlated with the increase in e-bike injury, which would suggest that children likely to exhibit high-risk behavior were shifting to the use of e-bikes instead of pedal bicycles.
E-bikes have an important role to play in expanding the transportation options for, while providing an opportunity for physical activity in the pediatric population. In most US states, the legal age for driving a car or motorcycle is 16 years, and many areas of the country do not have robust public transit systems. While six US states require a license to drive an e-bike, the remainder do not [14]. We hypothesize that e-bikes are filling a transportation gap for the pediatric population, particularly adolescents, because most states do not require a license, the cost is less than a car, and insurance is not needed. Parents may support use of e-bikes, which supply a small amount of electric motor assistance while providing a fun way for children to exercise. One small study of adults showed that the intensity of exercise while riding an e-bike, as measured by heart rate above resting, was significant but less intensive than for pedal bicycles [15].
E-bikes represent a good option for outdoor exercise in the pediatric population, but use may result in serious injury. Our review of NEISS data showed that, although the proportion of pediatric e-bike injuries requiring transfer or admission decreased from 18.3 % in 2011–2015 to 12.2 % in 2016–2020 (Fig. 2), injury requiring transfer or admission was more common for e-bike injuries than for moped- or bicycle-related injuries throughout the study period. Concussions and internal injuries were also more common for e-bike injuries compared to bicycle injuries. These findings are concordant with the findings of a single-institution pediatric study conducted in Israel, which demonstrated higher ISS and more frequent loss of consciousness among injured e-bike riders compared to pedal bike riders [16]. However, a single-center study conducted in Switzerland reported that e-bike injury patterns were similar to those observed for pedal bicycles but not motorcycles [17]. In addition, DiMaggio et al. found that rates of concussion and fracture across all age groups were higher for bicycles compared to e-bikes; however, the study notes that rates of internal injury were greater for e-bikes than for pedal bicycles [7]. These differences between studies may reflect methodological differences, such as study population. Hypotheses to explain our finding of more severe injuries with e-bikes specific to children include issues related to speed as well as behavior. E-bikes achieve higher average speeds than pedal bicycles [16]. Although e-bikes are legally speed limited in many states, assisted speed can reach 28 mph, and consumer modifications may lead to even higher speeds [14]. Furthermore, e-bike riders have been shown to violate traffic rules at similarly high rates to pedal bicycle riders, e.g. wrong-way riding rate >40 % and 25–30 % compliance with red light signals [18].
Higher rates of head injury have been observed in e-bike compared to pedal bike injuries [19]. Helmets help to reduce the severity of head injuries and are recommended by the American Academy of Pediatrics and the American College of Surgeons [[20], [21], [22], [23]]. In this study, we found a 4.44 % rate of concussion among e-bike–related injuries. In their study of users across all ages, DiMaggio et al. reported a concussion rate of 0.5 % among e-bike users. [7] This difference between studies may reflect the fact that helmet status was missing for over 90 % of cases in the current study. The high rate of missingness in this dataset likely leads to unstable estimates, and the true rate of helmet use remains unknown. Another limitation is that the helmet data was drawn from narrative report, which may have resulted in reporting bias. For cases in which helmet use or absence was reported, only 2.65 % of e-bike riders were wearing helmets (Supplementary Table 1). In contrast, one study of pediatric bicyclists struck by cars and treated at a single US institution demonstrated a 12 % rate of helmet use [24]. On the other extreme, a single-institution study from Australia that relied upon interviews to determine status found that 75 % of children who were injured on bicycles were wearing helmets [25]. Accurate reporting and improved data availability are essential for the study of helmet usage and head injury in e-bike riders, as this may represent a substantial opportunity to augment public health. In the meantime, continued attention to e-bike safety and helmet use are recommended across age groups.
The NEISS dataset represents a probability sample rather than a national registry; therefore, injury estimates may be inaccurate, as NEISS only captures information on patients who sought treatment in emergency departments. There were also limitations surrounding the narrative provided, as narrative input was not standardized, and some categories (e.g., helmet use) had missing data. The methodology applied to free text narrative data to identify presence and absence of helmet at time of injury was exploratory in nature. For all vehicle categories, over 90 % of cases did not report the presence or absence of a helmet anywhere in the narrative field. NEISS reports would benefit from a discrete field in which helmet use or other protective devices are reported. An additional weakness of using free text to define helmet use is that there may be bias in reporters towards those that do not use helmets. This study provides a benefit in reporting upon the extent of missingness in this field, and the need for improved reporting on the use of protective devices.
The relatively small sample of e-bike injuries observed during 2011–2020 resulted in unstable estimates for categories within the pediatric e-bike injury group. While the number of e-bike injuries reported in NEISS between 2011 and 2020 was limited, the number of estimated injuries grew each year with a positive monotonic trend. Thus, future studies of pediatric e-bike injury using NEISS will be able to provide greater certainty in terms of national injury estimates in the pediatric population. Further studies should also utilize other data sources including the Trauma Quality Improvement Program database, which will include more granular data. To facilitate further research, a new International Classifications of Disease (ICD) code should be created specifically for e-bike injuries, as was done for standing electric scooters in ICD10. Finally, a mandatory data collection field for helmet status should be included in all relevant databases, given the findings on helmet usage for prevention of severe injury and the recommendations of professional societies [[20], [21], [22], [23]]. Furthermore, NEISS data is not generalizable outside of the US, where usage patterns, infrastructure, and transportation systems differ, and there may be regional differences that are not accounted for in the present study. Methodological improvements will be necessary to increase the accuracy of data collected on helmet usage and injuries.
A popular mode of transportation among the pediatric population, e-bike usage is increasing. The incidence of pediatric injuries due to e-bikes increased during the period from 2011 to 2020, while the rate of injuries related to use of pedal bicycles decreased. E-bike injuries in children tend to be more severe than pedal bicycle injuries, requiring hospital admission or transfer more frequently. Public, governmental, and healthcare provider attention to pediatric safety on e-bikes, and particularly to increasing helmet usage, is imperative to improving pediatric public health.
The following are the supplementary data related to this article.
Estimated distribution of injury characteristics.
Previous communication
This abstract was presented as a poster at the 2022 Western Pediatric Trauma Conference in Sonoma, CA, US on July 14, 2022.
Funding sources statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval statement
This study was completed with institutional IRB approval. All items on STROBE checklist were completed.
CRediT authorship contribution statement
Study conception and design: Laura Goodman, Yigit Guner, Jeffry Nahmias, John Schomberg, Saeed Awan, David Gibbs, Mary Maginas, Elizabeth Wallace
Data acquisition: John Schomberg
Analysis and data interpretation: John Schomberg, Laura Goodman
Drafting of the manuscript: Laura Goodman, John Schomberg
Critical revision: Zoe Birnbaum, Jeff Nahmias, Mary Maginas, Elizabeth Wallace, Saeed Awan, David Gibbs, Yigit Guner, Olivia Vukcevich.
Declaration of competing interest
The authors have no competing interests to declare.
References
- 1.Surico J. New York Times; 08 Nov 2021. The popularity of e-bikes isn't slowing down. [Google Scholar]
- 2.Weiss M., Dekker P., Moro A., et al. On the electrification of road transportation - a review of the environmental, economic, and social performance of electric two-wheelers. Transp Res D Transp Environ. 2015;41:348–366. doi: 10.1016/j.trd.2015.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.de Haas M., Kroesen M., Chorus C., et al. E-bike user groups and substitution effects: evidence from longitudinal travel data in the Netherlands. Transportation. 2021;49(3):815–840. [Google Scholar]
- 4.U.S. Government Printing Office . In: Public Law No: 107-319 to amend the Consumer Product Safety Act to provide that low-speed electric bicycles are consumer products subject to such Act. Congress US, editor. 2002. p. 116. [STAT. 2776] [Google Scholar]
- 5.Hu W., Marcius C.R. New York Times; 10/11/2021. As e-scooters and e-bikes proliferate, safety challenges grow. [Google Scholar]
- 6.Toll M. Believe it or not, this US-built fast e-bike hits 45 mph and 80 miles of range 2019. https://electrek.co/2019/03/25/hpc-scout-pro-electric-bicycle-fast/ Available from: [updated 03/25/2019]
- 7.DiMaggio C.J., Bukur M., Wall S.P., et al. Injuries associated with electric-powered bikes and scooters: analysis of US consumer product data. Inj Prev. 2020;26(6):524–528. doi: 10.1136/injuryprev-2019-043418. [DOI] [PubMed] [Google Scholar]
- 8.Gross I., Weiss D.J., Eliasi E., et al. E-bike-related trauma in children and adults. J Emerg Med. 2018;54(6):793–798. doi: 10.1016/j.jemermed.2017.12.012. [DOI] [PubMed] [Google Scholar]
- 9.Karepov Y., Kozyrev D.A., Benifla M., et al. E-bike-related cranial injuries in pediatric population. Child’s Nervous Syst. 2019;35(8):1393–1396. doi: 10.1007/s00381-019-04146-8. [DOI] [PubMed] [Google Scholar]
- 10.Capua T., Glatstein M., Hermon K., et al. A comparison of manual versus electric bicycle injuries presenting to a pediatric emergency department. Rambam Maimonides Med J. 2019;10(3) doi: 10.5041/RMMJ.10370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Botton I.N., Takagi D., Shlez A., et al. Road accidents in children involving light electric vehicles cause more severe injuries than other similar vehicles. Eur J Pediatr. 2021;180(11):3255–3263. doi: 10.1007/s00431-021-04089-w. [DOI] [PubMed] [Google Scholar]
- 12.Division of Hazard and Injury Data Systems U.S. Consumer Product Safety Commission NEISS The National Electronic Injury Surveillance System: a tool for researchers 2021. https://www.cpsc.gov/s3fs-public/pdfs/blk_media_2000d015.pdf Available from:
- 13.Wheeler-Martin K., Mooney S.J., Lee D.C., et al. Pediatric emergency department visits for pedestrian and bicyclist injuries in the US. Inj Epidemiol. 2017;4(1):31. doi: 10.1186/s40621-017-0128-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Conference of State Legislatures State electric bicycle laws | a legislative primer. https://www.ncsl.org/research/transportation/state-electric-bicycle-laws-a-legislative-primer.aspx Available from: [updated 02/24/2021]
- 15.Hoj T.H., Bramwell J.J., Lister C., et al. Increasing active transportation through e-bike use: pilot study comparing the health benefits, attitudes, and beliefs surrounding e-bikes and conventional bikes. JMIR Public Health Surveill. 2018;4(4) doi: 10.2196/10461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Avrahamov-Kraft E., Yulevich A., Sweed Y. Pediatric electrical bicycle road accidents. Eur J Pediatr Surg. 2022;32(1):120–126. doi: 10.1055/s-0041-1741545. [DOI] [PubMed] [Google Scholar]
- 17.Sporri E., Halvachizadeh S., Gamble J.G., et al. Comparison of injury patterns between electric bicycle, bicycle and motorcycle accidents. J Clin Med. 2021;10(15) doi: 10.3390/jcm10153359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Langford B.C., Chen J., Cherry C.R. Risky riding: naturalistic methods comparing safety behavior from conventional bicycle riders and electric bike riders. Accid Anal Prev. 2015;82:220–226. doi: 10.1016/j.aap.2015.05.016. [DOI] [PubMed] [Google Scholar]
- 19.Trichinopoly Krishna S., Roberts S., Dardis R. Electrically assisted pedal cycles: is new legislation required to mitigate increased head injury risk? Br J Neurosurg. 2021;35(5):629–632. doi: 10.1080/02688697.2021.1940846. [DOI] [PubMed] [Google Scholar]
- 20.American Academy of Pediatrics . 2021. TIPP—bicycle safety: myths and facts. [Google Scholar]
- 21.American College of Surgeons . 2014. Statement on bicycle safety and the promotion of bicycle helmet use. [PubMed] [Google Scholar]
- 22.Hasjim B.J., Grigorian A., Schubl S.D., et al. Helmets protect pediatric bicyclists from head injury and do not increase risk of cervical spine injury. Pediatr Emerg Care. 2022;38(1):e360–e364. doi: 10.1097/PEC.0000000000002290. [DOI] [PubMed] [Google Scholar]
- 23.Høye A. Bicycle helmets – to wear or not to wear? A meta-analyses of the effects of bicycle helmets on injuries. Accid Anal Prev. 2018;117:85–97. doi: 10.1016/j.aap.2018.03.026. [DOI] [PubMed] [Google Scholar]
- 24.Strotmeyer S.J., Behr C., Fabio A., et al. Bike helmets prevent pediatric head injury in serious bicycle crashes with motor vehicles. Inj Epidemiol. 2020;7(Suppl. 1):24. doi: 10.1186/s40621-020-00249-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ong J.S., Soundappan S.V., Adams S., et al. Helmet use in bicycles and non-motorised wheeled recreational vehicles in children. J Paediatr Child Health. 2018;54(9):968–974. doi: 10.1111/jpc.13925. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Estimated distribution of injury characteristics.