Abstract
Background:
A foodborne disease outbreak among wedding attendees from Makunsar village, Palghar district, Maharashtra state, India, was reported on February 18, 2018.
Objectives:
The outbreak investigation was conducted to find out the epidemiology of the outbreak and to identify the etiologic agent and risk factors.
Methods:
A case–control study was carried out, where cases (patients), controls, and food handlers were interviewed and leftover foods were collected for culture. A case was defined as a person having vomiting or diarrhea (i.e., ≥3 loose stools within 24 h) who attended the wedding ceremony at Makunsar village, Palghar district, Maharashtra, on February 18, 2018. Attack rate and odds ratio (OR) were calculated with 95% confidence intervals (CIs).
Results:
Out of 75 cases, 63% were female. Altogether, forty-two (56%) cases were hospitalized, and later on, all of them were discharged from hospital without any mortality. About 93%, 68%, 43%, and 41% of the cases reported with vomiting, nausea, abdominal pain, and diarrhea, respectively. The median incubation period was found to be 4 h (range: 2–8 h). Eating gaajar halwa (carrot pudding) was significantly associated with illness (OR: 12.8; 95% CI: 3.5–46). Gaajar halwa is prepared with khoa, a perishable milk product. The gaajar halwa culture yielded no growth.
Conclusion:
The case-patients’ clinical presentation and incubation period were consistent with enterotoxin-producing Staphylococcus aureus as the probable etiologic agent. The epidemiologic investigation identified the probable etiologic agent and food source in a low-resource community setting. Community food handlers were educated on food preparation hygiene and safe storage measures to prevent future outbreaks.
Keywords: Foodborne diseases, gaajar halwa, India, outbreak investigation, Staphylococcus aureus, vomiting
Introduction
Foodborne diseases are a public health problem worldwide. The World Health Organization estimated that 600 million foodborne disease cases and 420,000 deaths occurred worldwide in 2010.[1] Despite vast underreporting in India, 554 acute diarrheal disease outbreaks, including 242 foodborne disease outbreaks, were reported during 2017.[2] Most foodborne outbreaks are not investigated because of a lack of resources and training, and etiologic agents and food sources are rarely identified or reported.
On February 18, 2018, the Palghar District Surveillance Unit in Maharashtra state generated an early warning signal after two primary health centers reported clusters of acute diarrheal disease cases. The district surveillance team initiated an investigation to find out the epidemiology of the foodborne diseases along with to identify the etiologic agent and risk factors.
Materials and Methods
Case finding
A case was defined as a person having vomiting or diarrhea (i.e., ≥3 loose stools within 24 h) who attended a wedding ceremony at Makunsar village, Palghar district, Maharashtra, on February 18, 2018. Records at two health facilities were also scrutinized to identify more cases in Makunsar and two nearby villages.
Case–control study
A case–control study was conducted with one control per case, to identify potential food sources for the outbreak. Controls were wedding attendees and neighbors of cases from the same village, who were not ill. Cases (patients) and controls were interviewed using a semi-structured questionnaire to collect data on sociodemographic characteristics, food consumption at the wedding, time of illness onset, clinical presentation and outcomes, and treatment history.
Environmental assessment
The host of the wedding ceremony and the relatives from Makunsar village were interviewed to explore food safety and hygiene practices during the event. Food handlers from Makunsar village were also interviewed to find out the cooking process and food storage practices during community gatherings. Food samples of gaajar halwa, paneer, and dal rice that remained after the wedding ceremony were collected and were sent to the state health laboratory for Salmonella, Shigella, Staphylococcus aureus, Bacillus cereus, and Vibrio cholerae testing.
Data analysis
Data were analyzed using Epi Info™ software, version 7.1 developed by Centers for Disease Control and Prevention, Atlanta, Unites States of America (USA) (available at http://www.cdc.gov/epiinfo).[3] Categorical data were expressed in proportions, while continuous data were expressed in median. Association between food items eaten and occurrence of acute illness was calculated overall and separately for different sexes. Exposure to different food items eaten and calculated odds ratios (ORs) with 95% confidence intervals (CIs) were compared between themselves. A P value 0.05 or less was considered as statistically significant.
Ethical considerations
The investigation was a public health response to an outbreak as part of the India Epidemic Intelligence Service Programme, undertaken with the purpose to identify the source of spread for immediate control of outbreak and intended for benefit of the community at large. Ethical approval is not applicable as part of public health response. The investigation did not involve any human laboratory sample collection for research purposes, and there were no invasive investigations or medical interventions/experiments. Ethical principles and guidelines as laid down by the Indian Council of Medical Research were maintained during the outbreak response: the investigation was aimed at achieving public good (beneficence) and collective welfare (solidarity); no harm was done to any individual (nonmaleficence); fair, honest, and transparent (accountability and transparency); and participants’ data were de-identified prior to analysis (confidentiality).
Results
Descriptive study
Altogether 75 cases were identified without any mortality. About forty-seven (63%) cases (patients) were female. The median age of cases was 38 years (range: 4–85 years). All 75 cases had eaten lunch at the wedding and reported illness between 3 and 10 p.m. on the same day [Figure 1]. The wedding lunch was served from 12 to 5 p.m. on February 18. The median incubation period for illness was 4 h (range: 2–10 h). The attack rate was 13% (75/600) among the wedding guests.
Figure 1:
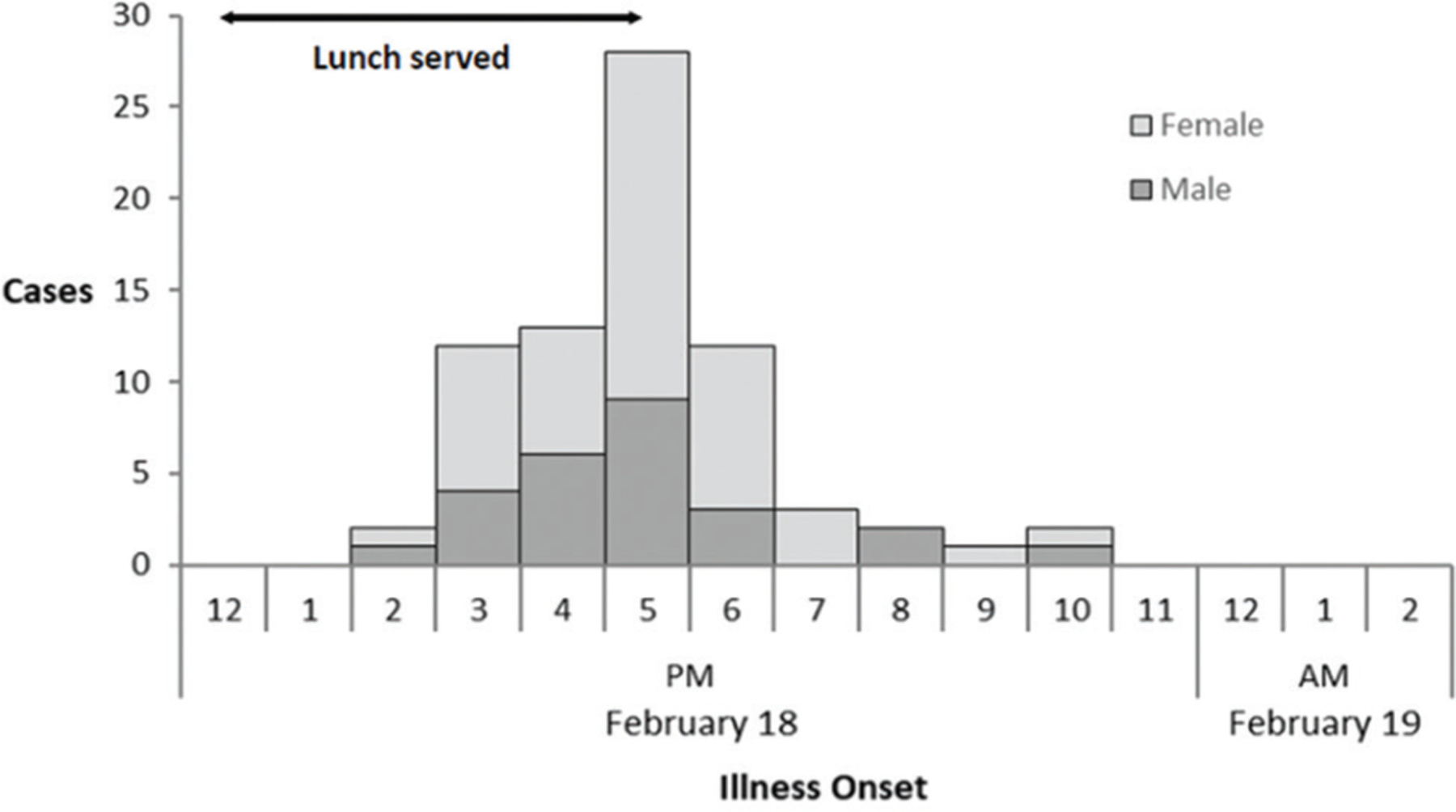
Epidemic curve of 75 foodborne disease cases by time of illness onset among wedding attendees in Makunsar village, Palghar district, Maharashtra, India, on February 18–19, 2018.
Of the 75 cases, 92% (69) reported vomiting, 67% (50) reported nausea, and 43% (32) and 41% (31) cases complained of abdominal pain and diarrhea, respectively. Seventy-four (99%) cases sought medical care from two health facilities. Out of the 74 cases who sought medical care, 57% (42) of them were admitted and all were discharged within 12 h after admission. Cases were treated with oral rehydration solution (62 [84%]), injectable antiemetics (65 [88%]), oral antibiotics (56 [76%]), and intravenous rehydration fluids (23 [31%]). No stool specimens were sent for laboratory testing.
Case–control study
Overall, 59 cases and 59 controls were enrolled in the case–control study as case: control as 1:1. Only consumption of gaajar halwa (carrot pudding) was found to be associated with illness (OR: 12.8) [Table 1]. In stratified analysis by sex, association of eating gaajar halwa with illness was found to be much higher among females (OR: 23.1) compared to males (OR: 7.7) [Table 2].
Table 1:
Comparison of lunch items eaten among cases and controls during a wedding in Makunsar village, Palghar district, Maharashtra state, India, on February 18, 2018
| Food or drink | Percentage of cases exposed* (n=59) | Percentage of controls exposed (n=59) | Odds ratio (95% CI) |
|---|---|---|---|
| Gaajar halwa | 95 | 59 | 12.8† (3.6–46) |
| Paneer | 76 | 68 | 1.5 (0.7–3.4) |
| Dal rice | 98 | 90 | 6.5 (0.8–56) |
| Water | 73 | 85 | 0.5 (0.2–1.2) |
| Papad | 58 | 68 | 0.6 (0.3–1.4) |
| Pickle | 29 | 34 | 0.8 (0.4–1.7) |
| Okra fry | 51 | 65 | 0.6 (0.3–1.2) |
| Green salad | 47 | 69 | 0.4 (0.2–0.8) |
| Kothimbir vadi | 41 | 66 | 0.3 (0.2–0.7) |
| Poori aloo | 32 | 61 | 0.3 (0.1–0.6) |
| Pineapple juice | 14 | 34 | 0.3 (0.1–0.8) |
| Cabbage | 7 | 19 | 0.3 (0.1–1.1) |
Persons who ate selected food or drink items.
Bold text indicates statistical significance. CI: Confidence interval
Table 2:
Comparison of lunch items stratified by sex among cases and controls during a wedding in Makunsar village, Palghar district, Maharashtra state, India, on February 18, 2018
| Food or drink | Percentage of cases exposed* (n=34) | Females percentage of controls exposed (n=34) | Odds ratio (95% CI) | Percentage of cases exposed (n=25) | Males percentage of controls exposed (n=25) | Odds ratio (95%CI) |
|---|---|---|---|---|---|---|
| Gaajar halwa | 97 | 59 | 23.1† (2.8–189) | 92 | 60 | 7.7 (1.5–40) |
| Paneer | 68 | 68 | 1.0 (0.4–2.8) | 88 | 68 | 3.4 (0.8–15) |
| Dal rice | 97 | 94 | 2.1 (0.2–24) | 96 | 81 | 5.9 (0.6–54) |
| Water | 71 | 79 | 0.6 (0.2–1.9) | 76 | 92 | 0.3 (0.0–1.5) |
| Papad | 59 | 68 | 0.7 (0.2–1.8) | 56 | 68 | 0.6 (0.2–1.9) |
| Pickle | 26 | 44 | 0.4 (0.2–1.2) | 32 | 20 | 1.9 (0.5–6.8) |
| Okra fry | 53 | 68 | 0.5 (0.2–1.4) | 48 | 60 | 0.6 (0.2–1.8) |
| Green salad | 35 | 71 | 0.2 (0.1–0.6) | 64 | 68 | 0.8 (0.3–2.7) |
| Kothimbir vadi | 32 | 62 | 0.3 (0.1–0.7) | 52 | 72 | 0.4 (0.1–1.3) |
| Poori aloo | 24 | 62 | 0.2 (0.1–0.5) | 44 | 60 | 0.5 (0.1–1.6) |
| Pineapple juice | 12 | 35 | 0.2 (0.1–0.9) | 16 | 32 | 0.4 (0.1–1.5) |
| Cabbage | 3 | 15 | 0.2 (0.0–1.6) | 12 | 24 | 0.4 (0.1–1.2) |
Persons who ate selected food or drink items.
Bold text indicates statistical significance. CI: Confidence interval
Environmental investigation
The wedding caterer cooked the food in a temporary kitchen in an open space near the wedding host’s house. Raw food and water were procured from the local market. The food handlers did not practice regular handwashing after handling raw food, after using washrooms, or after touching food preparation surfaces.
The wedding caterer reported that gaajar halwa was prepared the evening before the wedding with raw carrots, sugar, and milk cooked together on medium heat until the milk evaporated. The carrot mixture was stored at room temperature for approximately 12 h. Before the wedding lunch, khoa, a perishable milk product, was added to the carrot mixture and cooked on low heat until the khoa melted. The gaajar halwa was served warm at the wedding. Five kilograms of khoa had been procured a day before the wedding from an unauthorized local vendor and refrigerated. No information was available about the source of the raw milk or pasteurization. The date of preparation of the khoa was also uncertain. We were unable to screen food handlers for illness or assess temporary kitchen operations. No pathogens (i.e., Salmonella, Shigella, S. aureus, B. cereus, and V. cholerae) were isolated from the food samples of gaajar halwa, paneer, or dal rice that were tested.
Discussion
A point-source foodborne disease outbreak was investigated at a wedding lunch that was associated with eating gaajar halwa (carrot pudding) prepared from khoa, a perishable milk product. The clinical presentation and short incubation period were consistent with heat-stable enterotoxin-producing S. aureus as the etiological agent. Because toxin testing for S. aureus is not readily available in India and many other low-resource settings, we relied on the epidemiologic findings to identify the probable etiologic agent.[4,5] The association between eating gaajar halwa and illness was stronger in women compared to men. In most of the community gatherings in rural India, including weddings, women eat after men. Women might have received a higher dose of enterotoxin if the gaajar halwa was kept for a longer duration of time after preparation or women might have eaten larger quantities of gaajar halwa than men. The onset of illness did not differ between women and men. Khoa is a perishable milk product that is widely used across the Indian subcontinent as a base for sweets. Khoa is conducive to bacterial growth due to the high nutritive value and high water activity.[6] S. aureus can grow in khoa under a wide range of conditions.[6,7] In addition, higher microbial loads have been detected in milk products from local vendors compared to registered dairies in India.[8] Many unauthorized small-scale vendors sell milk products that do not meet food safety regulations for the treatment and storage of milk.[8] Foodborne diseases from locally prepared milk products, such as khoa, are common because milk is often not pasteurized, not refrigerated, and not prepared in hygienic conditions.[6,8] Foodborne outbreaks where S. aureus is implicated as the etiologic agent are usually due to food handlers; food is contaminated during preparation due to unhygienic practices. The investigation of foodborne outbreaks provides an opportunity to identify gaps in food safety controls across the food supply chain.[9,10] The district surveillance response team did not include representation from the food safety department for this outbreak investigation. They should be included and involved in future foodborne outbreak investigations to facilitate traceback of the source food through the supply chain, testing of food and environmental samples by the state laboratory, and for providing food safety education for both vendors and consumers.
The findings are subject to several limitations. Wedding guests might not have accurately recalled the lunch foods they ate when interviewed several days after the event. We could only test three foods that were left from the wedding for common foodborne pathogens; the state health laboratory did not have the capacity to test for enterotoxins. Finally, we were unable to assess food preparation practices or test the khoa.
Conclusion
This point-source foodborne disease outbreak associated with eating gaajar halwa at a wedding underscores the importance of timely epidemiologic investigations to identify the responsible food source and probable etiologic agent and to inform local public health actions. We conducted an educational session for community members and food handlers on hygiene practices and food safety measures to prevent future outbreaks.
Acknowledgments
We thank Dr. CS Aggarwal of National Centre for Disease Control, Delhi, for his support with the investigation. We also acknowledge the help and support of District Surveillance Unit and Public Health Department, Palghar district, Maharashtra.
We sincerely thank the village accredited social health activists and study participants for their cooperation throughout the investigation.
Financial support and sponsorship
This public health activity was conducted by the India Epidemic Intelligence Service (EIS) Programme at the request of the Government of Maharashtra. The National Centre for Disease Control receives funding support for the India EIS Programme through cooperative agreement no. NU2GGH001904GH10-1001 from the U.S. Centers for Disease Control and Prevention, Center for Global Health, Division of Global Health Protection.
Footnotes
Conflicts of interest
There are no conflicts of interest.
Epidemic Intelligence Service Programme Working Group: Samir V. Sodha, MD, MPH, Resident Advisor, Division of Global Health Protection, U.S. Centers for Disease Control and Prevention, New Delhi, India; Akshay Khandare, Taluka Health Officer, Health Department, Zilla Parishad (District Council), Palghar, Maharashtra, India; Sujeet Kumar Singh, MBBS, MD, Director, National Centre for Disease Control, New Delhi, India; Pradeep Khasnobis, MBBS, Joint Director, National Centre for Disease Control, New Delhi, India
References
- 1.World Health Organization. WHO Estimates of the Global Burden of Foodborne Diseases. Foodborne Disease Burden Epidemiology Reference Group 2007–2015 Available from: https://apps.who.int/iris/bitstream/handle/10665/199350/9789241565165_eng.pdf. [Last accessed on 2018 Mar 06].
- 2.National Centre for Disease Control Food-Borne Diseases and Food Safety in India New Delhi; 2011. Available from: www.ncdc.gov.in/writereaddata/linkimages/OCT-NOV_098132922884.pdf. [Last accessed on 2018 Aug 22]. [Google Scholar]
- 3.Dean AG, Arner TG, Sunki GG, Friedman R, Lantinga M, Sangam S, et al. Epi Info™, a database and statistics program for public health professionals. Atlanta, Georgia: Centers for Disease Control and Prevention; 2011.
- 4.Vo TH, Nguyen DV, Le LT, Phan LT, Nuorti JP, Minh NN. Applying standard epidemiological methods for investigating foodborne disease outbreak in resource-poor settings: Lessons from Vietnam. J Food Prot 2014;77:1229–31. [DOI] [PubMed] [Google Scholar]
- 5.Viazis S, Beal JK, Monahan C, Lanier WA, Kreil KR, Melka DC, et al. Investigation and regulatory enforcement actions in response to an outbreak of Salmonella Bredeney infections linked to peanut butter. Open Forum Infect Dis 2015;2:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhatnagar P, Khan AA, Jain M, Kaushik S, Jain S. Microbiological study of khoa sold in Chambal region (Madhya Pradesh): A case study. Indian J Microbiol 2007;47:263–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sohal S, Blank G, Lewis M. Survival and growth of selected microorganisms in khoa during preparation and storage. J Food Saf 1993;13:195–208. [Google Scholar]
- 8.Karthikeyan N, Pandiyan C. Microbial quality of khoa and khoa based milk sweets from different sources. Intern Food Res J 2013;20:1443–7. Available from: http://www.ifrj.upm.edu.my/20(03)2013/60 IFRJ 20(03)2013 Karthikeyan (342).pdf. [Last accessed on 2018 Oct 15]. [Google Scholar]
- 9.Ameme DK, Abdulai M, Adjei EY, Afari EA, Nyarko KM, Asante D. Food borne disease outbreak in a resource-limited setting: A tale of missed opportunities and implications for response. Pan Afr Med J 2016;8688:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ajlouni S, Gaungoo Y. Enforcement of food legislation and its impact on food safety: A case study on food law enactment in Mauritius. Adv Microbiol 2018;8:101–24. [Google Scholar]


