Abstract
We examine whether women’s social proximity to Zika during the Zika epidemic predicts intentions to avoid a pregnancy because of the COVID-19 pandemic either directly or indirectly via subjective assessments of the pandemic. We apply path models on unique microdata from Brazil, the country most affected by Zika and an epicenter of COVID-19, to understand whether a novel infectious disease outbreak left lasting imprints shaping fertility intentions during a subsequent novel infectious disease outbreak. Findings show that Zika social proximity is associated with fertility intentions through an indirect path related to subjective assessment of the COVID-19 pandemic. These findings emerged regardless of whether a woman herself had or suspected she had Zika and speak to the transformative consequences of novel infectious disease outbreaks that go beyond mortality and health.
Keywords: fertility, COVID-19 pandemic, fertility intentions, Brazil
Introduction
The COVID-19 pandemic generated tremendous uncertainty and worry about SARS-CoV-2 infection and its health, social, and economic consequences. During periods of macro-structural uncertainty and worry such as those brought on by novel infectious disease outbreaks, people may revise their intentions about whether and when to have (more) children. As individuals navigate the uncertainty and lack of knowledge that initially accompanies novel infectious disease outbreaks, their prior experiences with other recent novel infectious disease crises might consciously or unconsciously serve as a frame of reference for shaping their subjective assessments about subsequent novel infectious disease outbreaks. In turn, these assessments might influence their fertility intentions during the subsequent outbreak—especially during the early stages of a new novel disease crisis, when uncertainty about the new disease is high.
To investigate this possibility, we examine whether women’s experiences during the Zika epidemic in Brazil—the country with the highest prevalence of the Zika virus (ZIKV)—predict intentions to avoid a pregnancy because of the Covid-19 pandemic, directly or indirectly, via subjective assessments of the pandemic—perceived risk of contracting COVID-19, worry about pregnancy and fetal complications due to Covid-19, and fertility attitudes about pregnancy during COVID-19. We operationalize women’s experiences during the Zika epidemic by their social proximity to Zika, a novel composite measure encompassing who they know and how many people they know who had Zika or microcephaly, a congenital fetal abnormality caused by Zika infection in utero. The social proximity to Zika measure is rooted in previous research that finds that social networks are important determinants of fertility dynamics (Kohler 2000). We argue that this key role of social proximity to one disease can extend to epidemics of other diseases. We hypothesize a scarring effect such that women who experienced greater social proximity to Zika are more likely to intend to avoid pregnancy, either by postponing or forgoing pregnancy altogether, because of the COVID-19 pandemic. We further hypothesize that subjective assessments about the virus and pandemic mediate the ways in which social proximity to a prior epidemic shapes intention to avoid a pregnancy in a subsequent outbreak of a different novel infectious disease.
To examine whether social proximity to disease in one novel infectious disease outbreak has scarring effects on fertility intentions in a subsequent outbreak of a successive novel infectious disease, we focus on Brazil, the epicenter of the 2015 to 2017 ZIKV epidemic. Three years later, Brazil was again an epicenter of another novel infectious disease outbreak, with among the highest case and death counts of COVID-19 in the world (as of May 2023; Johns Hopkins Coronavirus Resource Center 2021). Navigating fertility intentions during the Zika epidemic became especially fraught for women once scientists established that ZIKV can cause serious birth defects, including microcephaly and other types of congenital Zika syndrome (CZS; Brasil et al. 2016; Rasmussen et al. 2016). Although COVID-19 does not present the same kinds of risk as ZIKV, pregnant women are at higher risk of developing severe illness from COVID-19 (Centers for Disease Control and Prevention 2021), and there is evidence of increases in stillbirth, preterm birth (Khalil et al. 2020), and maternal mortality particularly in low- and middle-income countries during the COVID-19 pandemic (Diniz, Brito, and Rondon 2022; Maza-Arnedo et al. 2022). Although ZIKV and SARS-CoV-2 are distinct viruses, they both transmitted novel infectious diseases that generated high levels of individual and societal uncertainty and worry. Thus, women in places affected by the Zika epidemic are again managing fertility intentions in contexts of high uncertainty and worry, this time coupled with heightened social and economic instability brought on by the COVID-19 pandemic.
Using structural path models and unique population-level probabilistic data from 3,996 women ages 18 to 34, we examine whether social proximity to Zika is associated with fertility intentions to postpone or forgo pregnancy because of the pandemic, directly or indirectly, via subjective assessments about the COVID-19 pandemic. In doing so, this study makes at least three contributions to the literature. First, it advances knowledge on the fertility implications of the COVID-19 pandemic by examining subjective assessments that underlie the fertility decision-making process. Although there is empirical evidence of the effects of the pandemic on fertility intentions (Kahn et al. 2021; Luppi, Arpino, and Rosina 2020), with a few exceptions (Manning et al. 2022), most prior research has been limited to descriptive accounts of the association between the pandemic and fertility intentions and to the use of nonprobabilistic samples, which restricts the generalizability of their findings. Our study extends beyond descriptive work by examining some of the mechanisms that might explain how the pandemic shapes fertility intentions. The second contribution is evidence that the fertility consequences of novel infectious disease outbreaks may transcend a single epidemic. To the best of our knowledge, no research has considered fertility intentions across more than one epidemic in response to experiences with the disease within one’s social network. The third contribution stems from our granular measure of social proximity to disease. Previous studies focusing on fertility outcomes during epidemics have operationalized proximity to disease by calculating rates of confirmed cases of the disease or another measure of exposure at an aggregate level of geography, such as the municipality or region (Lucas 2013; Rangel et al. 2020; Terceira et al. 2003). We argue that accounting for social proximity to both confirmed and suspected cases at the individual level is crucial because such proximity can shape subjective assessments such as perceptions of and worry about the risk and consequences of the disease.
Fertility Intentions
Fertility intentions are a fundamental component of women’s reproductive decision-making processes. Fertility intentions encompass individuals’ personal preferences and goals regarding having (more) children, ideal family size, pregnancy timing, and use of contraception and fertility treatments (Bongaarts 2001; Hayford and Agadjanian 2019; Hin et al. 2011; Miller 1995; Perugini and Bagozzi 2001). In this article, we focus specifically on the intention to avoid pregnancy because of the COVID-19 pandemic. Our measure of pregnancy avoidance intentions captures both quantum and tempo elements of intentions—that is, whether an individual intends to forgo having any (additional) children because of the COVID-19 pandemic (quantum) or whether they intend to postpone pregnancy because of the COVID-19 pandemic (tempo). We maintain that the processes through which social proximity to Zika influences fertility intentions because of the COVID-19 pandemic will likely operate similarly for intentions to postpone and intentions to forgo childbearing because both types of intentions capture a desire to avoid pregnancy. However, to account for the possibility of differences in the processes, we disaggregate pregnancy avoidance intentions into intentions to postpone and intentions to forgo pregnancy.
Although fertility intentions can serve as a predictor of fertility behaviors (Yeatman, Trinitapoli, and Garver 2020), there can also be notable discordance between fertility intentions and behaviors at both the individual and aggregate levels (Bongaarts 2001). Regardless of whether they translate into fertility behavior, fertility intentions are in themselves important foci of study because they reflect social and health structures (Bachrach and Morgan 2013) and differences in women’s real and perceived autonomy over their reproductive lives. Fertility intentions are dynamic and sensitive to changes in people’s lives (Bachrach and Morgan 2013; Barber 2001), including macro-level changes (Bhrolcháin and Beaujouan 2011; Sennott and Yeatman 2018; Towriss et al. 2020; Trinitapoli and Yeatman 2018; Yeatman, Sennott, and Culpepper 2013) such as large-scale novel infectious disease outbreaks, and micro-level social interactions (Rossier and Bernardi 2009). In this article, we examine how a macro-level event—the Zika epidemic—manifested at the micro level in women’s social networks in ways that influenced their fertility intentions during a subsequent macro-level novel infectious disease outbreak—the COVID-19 pandemic. We next discuss the theoretical reasons for linking social proximity to Zika to fertility during the COVID-19 pandemic.
Social Proximity to Disease as a Predictor of Fertility Intentions across Epidemics
Although there are studies on fertility behavioral responses to macro-level shocks such as economic crises (Sobotka, Skirbekk, and Philipov 2011), natural disasters (Nobles, Frankenberg, and Thomas 2015), and wars (Agadjanian and Prata 2002; Lindstrom and Berhanu 1999), there is comparatively little research on the sensitivity of fertility intentions to degree of exposure to epidemics of novel infectious diseases. The few exceptions are studies that focus on how diagnosis of an infectious disease shapes fertility preferences (Hayford, Agadjanian, and Luz 2012; Yeatman 2009).
Extrapolating from research on fertility behavior in response to degree of exposure to public health shocks, we argue that women’s degree of social proximity to disease during a public health crisis, particularly a novel infectious disease outbreak, can be an important predictor of fertility intentions in a subsequent novel infectious disease outbreak. We define social proximity to disease as the number of people that an individual personally knows that has had a confirmed or suspected case of Zika or a confirmed case of microcephaly. Our conceptualization of social proximity to disease as a predictor of fertility intentions stems from the idea that women’s evaluations of the relative risks and benefits of childbearing during a novel infectious disease outbreak likely hinge in part on the ways in which they have experienced a previous outbreak at the micro level in their own social networks. This assumption is rooted in literature documenting social network effects on fertility intentions and attitudes and risk perceptions of disease. Knowing about other people’s, particularly family and household members’ (Kohler, Behrman, and Watkins 2007), experiences with the disease can make the abstract threat of an unfamiliar virus a more concrete reality in a similar way that a bereavement operates (Verdery et al. 2020). This experience of social proximity to disease might in turn serve as an anchor that guides one’s fertility intentions in a subsequent novel infectious disease crisis, especially in the early stages when information about the new disease is limited and uncertainty is high.
The core theoretical ideas about social proximity 1 (i.e., degree of exposure to or experiences with) to macro-structural shocks have been applied in prior studies investigating impacts on fertility behaviors but less so to studies focusing on fertility intentions. Moreover, previous studies using population-level data tend to operationalize risk or proximity to disease by calculating rates of confirmed cases of the disease or another measure of exposure at an aggregate level of geography, such as the municipality, state, or region (Lucas 2013; Rangel et al. 2020; Terceira et al. 2003). To the best of our knowledge, no research has considered how experiences with a novel infectious disease within one’s own social network shape fertility intentions across consecutive novel disease outbreaks. In defining social proximity to disease on a more granular level than previous studies—as the number of people that an individual personally knows that has had a confirmed or suspected case of Zika or a confirmed case of microcephaly—we build the argument that this level of detail about both confirmed and suspected cases in an individual’s social network is important because it can shape the complex sociopsychological mechanisms, including subjective assessments regarding the disease, which in turn might shape fertility intentions during outbreaks.
Regarding the sensitivity of fertility intentions to COVID-19, emerging research suggests that the pandemic is associated with revised fertility intentions. In their multicountry study, Luppi Arpino, and Rosina (2020) found evidence of postponement or abandonment of fertility plans with variation across countries and individual characteristics. Malicka, Mynarska, and Świderska (2021) also found evidence of changes to fertility intentions related to changes in socioeconomic and health conditions; Kahn et al. (2021) reported a similar pattern among women in New York City. Zhu et al. (2020) found that in Shanghai, forgoing childbearing plans was associated with health concerns.
While these studies provide a sense of changing fertility intentions in response to the COVID-19 pandemic, none of these studies considered back-to-back public health crises, nor have they reflected on individuals’ social proximity to an epidemic. We contend that it is possible to measure individuals’ social proximity to a previous epidemic and that such experiences of proximity can impact fertility intentions during a subsequent crisis. We further argue that it is possible that the association between social proximity to a previous epidemic and fertility intentions during a subsequent public health crisis is mediated by subjective assessments of the ongoing crisis.
Pathways Linking Social Proximity to Disease to Fertility Intentions across Epidemics: The Role of Subjective Assessments
We posit that social proximity to a novel disease in the aftermath of a previous epidemic works primarily through indirect pathways to shape fertility intentions in a subsequent novel infectious disease crisis. Given the time lag between the Zika epidemic and the COVID-19 pandemic, we do not hypothesize direct pathways linking social proximity to Zika and fertility intentions during the COVID-19 pandemic. Instead, we argue that social proximity to disease in a previous epidemic might indirectly shape fertility intentions by conditioning one’s subjective assessments of the subsequent epidemic regarding the virus risk—perceived risk of contracting COVID-19 and worry about pregnancy and fetal complications due to COVID-19—and normative attitudes on childbearing—fertility attitudes about pregnancy during COVID-19.
In the context of uncertainty brought on by a newly discovered disease, people’s experiences with a previous novel infectious disease crisis might inform the cognitive schema through which they form attitudes and intentions about childbearing during this new public health shock (Johnson-Hanks 2014). Greater social proximity to disease in a previous epidemic, in this case, Zika, might shape the subjective assessments of risk and worry about the current disease, in this case, COVID-19, which ultimately shape fertility intentions.
Greater social proximity to Zika might increase one’s risk perceptions of contracting COVID-19 or worry about fetal complications due to COVID-19. In turn, these heightened negative subjective assessments of risk and worry about COVID-19 might be associated with normative attitudes that support avoiding pregnancy during the COVID-19 pandemic, ultimately shaping personal intentions to avoid pregnancy during the pandemic. In addition, greater social proximity might be associated with in-creased risk perception and worry if it makes people concerned about the potential burden of care brought on by the health consequences of the disease, which in turn might influence women to intend to avoid pregnancy, particularly if resources are constrained. Indeed, the prospective burden of caring for a child with CZS may have been a motivation to reduce childbearing during the Zika epidemic, driving down birth rates (Marteleto et al. 2020; Rangel et al. 2020).
On the other hand, it is also possible that women’s proximity to a previous public health crisis that brought extreme societal uncertainty and risk translates into intention to have (more) children if they view childbearing as a mechanism to reduce personal or societal uncertainty (Friedman, Hechter, and Kanazawa 1994). For example, amid crises associated with high mortality, a desire to replace lost children can also lead to an intention for more children (Nobles et al. 2015) as a strategy to deal with the uncertainty regarding child survival (Trinitapoli and Yeatman 2011). And research on fertility intentions during the pandemic has documented that at least some women intended to have children sooner because of COVID-19 (Zimmerman et al. 2022).
We also consider fertility attitudes as an important component of subjective assessments during the pandemic. As such, fertility attitudes can be predictors of fertility intentions (Miller 1994, 1995) among reproductive-age women across back-to-back novel infectious disease outbreaks. Fertility attitudes encompass one’s thinking about others’ fertility through normative ideas about broader societal expectations and values around childbearing. Normative ideas about childbearing can be encoded through prescriptive norms, or expectations of appropriate behaviors that convey “what individuals should do” (Bicchieri 2005; Horne and Mollborn 2020; Riley et al. 2021; Shakya, Weeks, and Christakis 2019), and through descriptive norms, which emerge from the prevalence of individual or collective behaviors in a defined geographical location (i.e., what individuals actually do; Bernardi 2013; Horne and Mollborn 2020; Torche and Abufhele 2021). Thus, although related to fertility intentions, fertility attitudes differ from intentions in that attitudes are subjective norms that guide intentions and behaviors through positive or negative evaluations of performing the behavior (Ajzen 1991) and intentions refer to conscious (Fishbein and Ajzen 2010) and unconscious (Bachrach and Morgan 2013) commitments to perform an action. Fertility attitudes can be useful for understanding how norms and expectations shape individuals’ personal fertility intentions.
Thus, we investigate the links between social proximity to disease, subjective assessments, and fertility intentions to offer important insights into women’s cognitive schemas and decision-making processes around fertility during back-to-back novel infectious disease outbreaks (Manning et al. 2022)
Research Questions and Hypotheses
We examine three research questions:
Research Question 1: Is social proximity to Zika associated with fertility intentions during the COVID-19 pandemic?
Hypothesis 1: We hypothesize that the direct path between social proximity to Zika and fertility intentions will be weak or nonexistent mainly because of the time lag between the Zika epidemic and the COVID-19 epidemic.
Research Question2: Does social proximity to Zika work through subjective assessments of the pandemic, including perceived risk of infection, worry about COVID-19 complications, and attitudes about pregnancy during the pandemic, to shape fertility intentions during the COVID-19 pandemic?
Hypothesis 2: We hypothesize that social proximity to Zika influences fertility intentions indirectly through subjective assessments of the pandemic. Individuals who experienced greater proximity to Zika might prompt respondents to assess their personal risks for COVID differently than those who experienced less social proximity to Zika.
Research Question 3: Are the paths mediating the association between social proximity to Zika and fertility intentions due to the COVID-19 pandemic different based on intentions to postpone versus intentions to forgo pregnancy during COVID-19?
Hypothesis 3: We hypothesize that the processes of postponing versus forgoing childbearing during the COVID-19 pandemic operate similarly, that is, through the indirect path of subjective assessments of the pandemic.
Data and Methods
Data
Data for this study come from the first wave of the Demographic Consequences of Epidemics Project (DeCodE Project), an ongoing, annual panel study on the implications of novel infectious disease outbreaks on women’s reproductive lives in Pernambuco—one of the poorest states in Brazil and the state that was most severely affected by recent public health shocks, including Zika in 2015–2017 and COVID-19 since 2020.
Between May and October 2020, the DeCodE Project conducted the first wave of data collection using surveys with 3,996 women, ages 18 to 34. To recruit a probabilistic sample of women living in Area Code 81, we used random-digit dialing (RDD) with a dual frame design, drawing on a sampling base of more than 19 million randomly generated cell phone numbers from Brazil’s government concession. Brazilian census data (Instituto Brasileiro de Geografía e Estatística 2021) found that 94 percent and 88 percent of women in the target age group own a cell phone in the metropolitan region of Recife and in the state of Pernambuco, respectively. 2
Surveys were conducted using phone interviews (≈25 minutes in duration), with interviewers using an Institutional Review Board-approved script to confirm respondent consent. Surveys were conducted in Portuguese, and bilingual study staff and the principal investigator translated the questionnaire. All interviews were recorded for supervision and quality control. The Institutional Review Board at the University of Texas at Austin and at the Brazilian National Commission for Research Ethics approved this study.
Analytical Sample and Variables
We focused our analysis on women who were not pregnant at the time of the interview (N = 3,890). We model three outcome variables measuring intention to avoid a pregnancy because of the COVID-19 pandemic. All three outcomes are derived from survey questions that asked respondents who reported wanting a(nother) child whether they changed their mind about the desired timing of their pregnancy because of the COVID-19 pandemic (i.e., postponing) and asked respondents who reported not wanting a(nother) child if they changed their mind about wanting a(nother) child because of the COVID-19 pandemic (i.e., forgoing). The first measure combines all women who intend to avoid a pregnancy because of COVID-19, either by intending to postpone or forgo pregnancy altogether. The reference category for the models with this outcome includes women who intend a pregnancy now/within the next six months and those who intend to postpone or forgo a pregnancy for reasons other than the pandemic. We conducted sensitivity analyses that separated the reference group and found results consistent with models that combined the reference group into one category.
The next two outcomes separate intentions to avoid a pregnancy because of the COVID-19 pandemic into intentions to postpone and intentions to forgo pregnancy. Postponing because of the pandemic captures respondents who report they want a(nother) child in the future but changed their intended fertility timing to get pregnant at a later time (six months or longer) because of the COVID-19 pandemic. Forgoing because of the pandemic captures respondents who report not intending a(nother) child in the future because of the COVID-19 pandemic. The reference group for the models measuring postponement because of the pandemic is postponing a pregnancy for reasons other than the pandemic. The reference group for the models measuring forgoing because of the pandemic is forgoing a pregnancy altogether for reasons other than the pandemic.
The focal independent variable is a social proximity to Zika index, which summarizes whether the respondent herself, family and household members, and/or their children and partners had a suspected or confirmed Zika infection; the overall number of people they know with a suspected or confirmed case; and whether they know any child with CZS. Indices constructed using items in Table 1 through sum scores, principal components, and factor analysis are highly correlated (rs = .96–.99). Simple sum score of binary indicators showed the strongest association with Zika exposure correlates such as household water shortage. A high level of social proximity to Zika is unrelated to education (mean difference = .02, p = .60) or income (r = .004, p = .79).
Table 1.
Weighted Descriptive Statistics (N = 3,890).
| M/% | SD | Range | |
|---|---|---|---|
| Zika proximity index | 2.05 | 1.46 | 0–5 |
| Perceived likelihood of contracting COVID-19 | 3.49 | 1.52 | 1–5 |
| Worried/extremely worried pregnancy-fetal COVID-19 complications | 82.7% | ||
| All women should avoid pregnancy during pandemic | 4.11 | 1.36 | 1–5 |
| Changed mind regarding intention to postpone or forgo pregnancy because of COVID-19 pandemic | 23.5% | ||
| Does not want another child | 32.3% | ||
| Has a child | 51.7% | ||
| Age 18–26 | 52.9% | ||
| Race (non-White) | 69.8% | ||
| Completed high school or less | 68.5% | ||
| Lives in metro Recife | 43.5% | ||
| Income category (1–7) | 4.06 | 1.62 | 1–7 |
| Married or lives with partner | 44.1% | ||
| Zika proximity index items | |||
| Knows at least one person who had Zika (confirmed or suspected) | 70.8% | ||
| Someone in respondent's household or family had suspected or confirmed case | 42.3% | ||
| Knows at least five people who had Zika | 36.9% | ||
| Knows any children with microcephaly | 26.7% | ||
| Suspected or confirmed case | 22.2% | ||
Source: Demographic Consequences of Epidemics Project data; sample of nonpregnant women.
We include three indicators of subjective assessments of the COVID-19 pandemic: (1) perceived risk of contracting COVID-19, (2) worry about pregnancy or fetal complications due to COVID-19, and (3) attitude toward pregnancy during the COVID-19 pandemic. COVID-19 risk perception is a self-assessment of the likelihood of infection measured through a 5-point scale (1 = very small chance, 5 = very large chance). Worry about pregnancy and fetal complications because of COVID-19 is a 5-point scale coded as a dichotomous variable due to low variability (0 = no worry, 1 = any worry). Pregnancy attitudes during the COVID-19 pandemic—whether respondents believe that all women should avoid childbearing during the pandemic—is measured through a 5-point scale (1 = strongly disagree, 5 = strongly agree). Additional covariates included in the models are age, race, education, income, living with partner, living in the metropolitan state capital area, and has at least one child.
Methods
To test for direct and indirect associations (i.e., mediation) between social proximity to Zika and fertility intentions during COVID-19, we conducted path models in Mplus version 8.2. We estimated three main models and several sensitivity analyses. In all models, we tested a direct path from Zika social proximity to changing fertility intentions because of COVID-19 and an indirect path through the following mediators: perceived probability of COVID-19 infection, worry about pregnancy/fetal complications due to COVID-19, and attitudes about pregnancy during the pandemic. We used maximum likelihood robust estimation to account for the dichotomous nature of the outcome variables, and we employed full information maximum likelihood estimation to handle missing values (Enders 2013). All models included raked sampling weights.
Estimates in the path models are interpreted like regression coefficients, although a path model uses covariance matrix to estimate associations between variables simultaneously. Indirect paths are useful for examining the mechanisms through which a process operates. For example, we hypothesize that it is not simply enough for a woman to have social proximity to Zika to change her mind about her childbearing intentions. The social proximity to Zika only influences these decisions inasmuch as the experience of social proximity prompts her to consider her subjective assessments of COVID-19, that is, the likelihood that she would contract COVID, the extent to which she would worry about the pregnancy complications due to COVID, and the attitudes she holds about whether women should avoid pregnancy during the pandemic. In other words, there is no direct influence of social proximity to Zika on childbearing intentions during the COVID pandemic; there is only an (indirect) influence through how Zika proximity prompts her to evaluate and interpret risk during the pandemic.
Results
The descriptive statistics in Table 1 show that about three-fourths of the respondents know at least one person who had a suspected or confirmed case of Zika during the epidemic (70.8 percent). Regarding additional measures of social proximity to Zika, 42.3 percent of the respondents had someone in their household or family with a suspected or confirmed case of Zika. Approximately a third of the sample (36.9 percent) knew at least five people who had Zika, and approximately one-fourth (26.7 percent) knew at least one child with microcephaly. Finally, 22.2 percent of the women we interviewed suspected or confirmed a Zika diagnosis. Combined, these statistics reflect the high prevalence of Zika and the pervasiveness of microcephaly in the state of Pernambuco.
Approximately half of the sample (51.7 percent) are mothers, and 44.1 percent are married or cohabiting with a partner. Regarding COVID-19, most women in our sample were worried or extremely worried about pregnancy or fetal COVID-19 complications. About a fourth of the women interviewed (23.5 percent) reported a change in their fertility intentions directly due to COVID-19 in 2020. We next show results of path models to further understand this perceived change in fertility intentions that resulted in women either postponing or forgoing childbearing because of COVID.
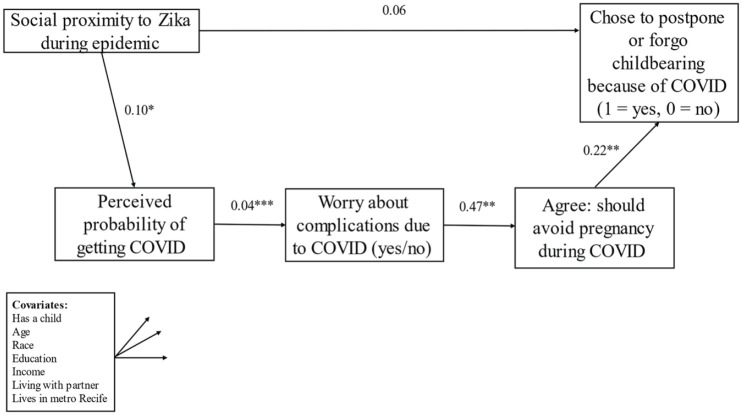
Figure 1, which shows the results from the path models, indicates that greater social proximity to Zika during the Zika epidemic was not directly associated with a greater likelihood of intending to postpone or forgo pregnancy because of COVID-19 during the first year of the pandemic (b = 0.06, odds ratio [OR] = 1.06, p < n.s.).
Figure 1.
Path model predicting change in fertility intentions because of COVID-19 (N = 3,890).
Note: Akaike information criterion = 91,163.75; Bayesian information criterion = 91,721.44.
*p < .05. **p < .01. ***p < .001.
Testing indirect paths via subjective assessments in Figure 1 elucidated how social proximity to Zika influenced women’s subjective assessments of the pandemic, which ultimately predicted their intention to avoid a pregnancy because of COVID-19. Greater social proximity to Zika during the Zika epidemic was associated with a higher likelihood of perceiving a higher risk of infection of COVID-19 (b = 0.10, p < .05), which, in turn, predicted a higher likelihood of worry about pregnancy and fetal complications due to COVID-19 (b = 0.04 p < .001). Greater worry about COVID infection, in turn, predicted stronger agreement that all women should avoid pregnancy during the COVID-19 pandemic (b = 0.47 p < .01). Stronger agreement that all women should avoid pregnancy during the COVID-19 pandemic predicted a higher likelihood of intending to postpone or forgo pregnancy because of the COVID-19 pandemic (b = .22, OR = 1.24, p < .05). The associations between each subjective assessment provide evidence for a sequence of women’s scarring that links two back-to-back novel infectious disease outbreaks that women have experienced to fertility intentions.
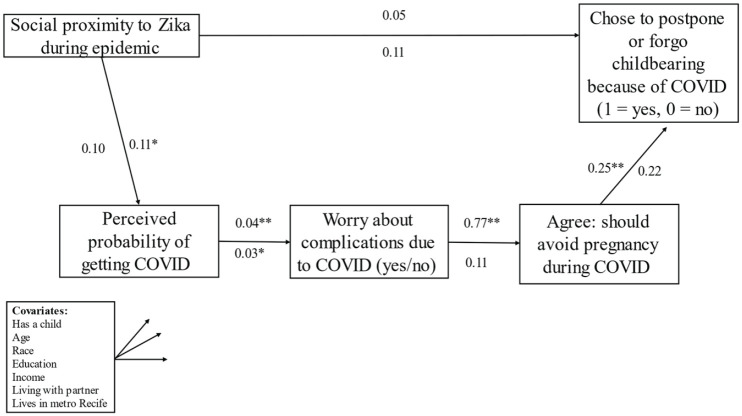
We next disaggregated changes in fertility intentions into intention to forgo versus intention to postpone childbearing because of COVID-19 (Figure 2). Overall findings from Figure 2 suggest that the sequence of subjective assessments linking social proximity to Zika to fertility intentions during COVID-19 generally operates similarly for intentions to postpone and intentions to forgo pregnancy. The magnitude of most of the paths for the subjective assessments is similar for intentions to postpone and intentions to forgo. However, the significance levels differ; the paths predicting intentions to postpone are all statistically significant, whereas most of the paths predicting intentions to forgo do not reach statistical significance. The most prominent difference between intentions to postpone versus intentions to forgo pregnancy because of COVID is the association between worry about pregnancy and/or fetal complications due to COVID and fertility attitudes, with a large coefficient magnitude for intentions to postpone pregnancy (b = 0.77, p < .01) that is negligible for intentions to forgo pregnancy altogether (b = 0.11, p = n.s.).
Figure 2.
Path model predicting childbearing intentions for women intending to postpone pregnancy (above line, n = 2,289) and women intending to forgo pregnancy (below line, n = 1,219).
Note: Akaike information criterion = 53,735.42 (27,738.24); Bayesian information criterion = 54,245.95 (28,192.66).
The numbers in parentheses represents the fit statistics for the model for forgoing pregnancy.
*p < .05. **p < .01.
Sensitivity analyses by age, race, socioeconomic status levels, age, motherhood status, marital union status, and children’s age are shown in Table 2. Results from disaggregated models by these characteristics follow a general similar trend to results shown in Figure 1—while there is no direct path between social proximity to Zika and fertility intentions during COVID-19, there is an indirect path between social proximity to Zika and fertility intentions during COVID-19 that is moderated by subjective assessments of the pandemic.
Table 2.
Direct, Indirect, and Total Paths from Zika Proximity to Fertility Intentions due to the COVID-19 Pandemic.
| Proximity → Fertility Intentions Total Direct |
Proximity → Risk Perception | Risk Perception → Worry | Worry → Attitude | Attitude → Fertility Intentions | |
|---|---|---|---|---|---|
| White (n = 1,150) |
0.09 | 0.01 | 0.04* | 0.74** | 0.26* |
| Non-White (n = 2,735) |
0.05 | 0.14** | 0.04*** | 0.37 | 0.21 |
| Younger: 18–26 (n = 1,597) |
0.16 | 0.11 | 0.03 | 0.56* | 0.21 |
| Older: 27–34 (n = 2,293) |
-0.03 | 0.10* | 0.05*** | 0.37* | 0.28** |
| High education (n = 1,833) |
0.07 | 0.08 | 0.03* | 0.55** | 0.41*** |
| Low education (n = 2,053) |
0.09 | 0.10 | 0.04*** | 0.41 | 0.16 |
| In union (n = 1,829) |
0.04 | 0.09 | 0.04*** | 0.25 | 0.22* |
| Single/not in union (n = 2,061) |
0.09 | 0.13* | 0.04* | 0.58* | 0.21 |
| Has child < 6 years old (n = 1,227) |
0.14 | 0.06 | 0.03** | 0.27 | 0.13 |
| No child < 6 years old (n = 663) |
-0.21 | 0.23** | 0.03 | 0.23 | 0.04 |
| No children (n = 1,972) |
0.10 | 0.10 | 0.05** | 0.62* | 0.37** |
Source: Demographic Consequences of Epidemics Project data; weighted sample of nonpregnant women.
Note: Direct path reports the path from Zika proximity to postponing/forgoing fertility. Indirect path reports the mediated path from Zika proximity to postponing/forgoing through perceived probability of COVID-19 infection, worry about pregnancy-fetal complications due to COVID-19, and beliefs women should avoid pregnancy during the pandemic. Full sample reports models for postponing/forgoing childbearing combined (analogous to Figure 1).
We estimate further sensitivity analyses to ensure that the Zika social proximity index is not also capturing COVID-19 social proximity. The correlation between the Zika social proximity index and an analogous COVID-19 social proximity index is only 0.22. Additional models in which we control for a COVID-19 social proximity index show substantively similar results to those presented here.
Discussion and Conclusion
With the COVID-19 pandemic occurring only three years after the Zika epidemic ended, women of childbearing age in places heavily affected by the 2015–2017 Zika epidemic, such as Brazil, navigated fertility during back-to-back novel infectious disease outbreaks surrounded by high levels of uncertainty and fear. With scientists predicting an “era of pandemics” characterized by a global rise in novel infectious diseases (The Lancet Planetary Health 2021), the occurrence of consecutive outbreaks may increase, with transformative impacts on how individuals everywhere navigate major life decisions such as pregnancy.
Our study used unique population-level probabilistic microdata from Brazil, the country most affected by the Zika epidemic and an epicenter of the COVID-19 pandemic, to demonstrate a scarring effect of one novel infectious disease outbreak to another that operates through subjective assessments of the subsequent crisis, COVID-19. A woman’s social proximity to Zika during the Zika epidemic indirectly predicts fertility intentions three years later, during the COVID-19 pandemic, through subjective assessments. These results show generally similar patterns for intentions to postpone and intentions to forgo pregnancy, although only the paths predicting intentions to postpone remain statistically significant, even after controlling for parity and alternative analytical strategies considering differential selection to Zika social proximity.
Broadly, our findings speak to the transformative consequences of novel infectious disease outbreaks that go beyond mortality and health. This study extends emerging descriptions of pandemic-induced changes in fertility intentions to underscore the subjective assessments explaining them and contribute to building knowledge on the importance of psychosocial factors in explaining fertility during the pandemic (i.e., Manning et al. 2022). Our results have important general implications for understanding the scarring effects of novel infectious disease epidemics and the importance of social proximity to a novel infectious disease and specific implications for understanding individual- and population-level consequences of successive novel infectious disease epidemics for women’s pregnancy intentions and potentially, for fertility rates. We discuss each of these implications in turn and in correspondence with the study’s hypotheses.
First, our findings provide evidence of a scarring effect across outbreaks that operates via women’s subjective assessments of COVID-19. Our findings provide support for Hypotheses 1 and 2, which posited, respectively, no direct effects of social proximity to Zika on fertility intentions but indirect effects through subjective assessments. Results show that the path between social proximity to a previous epidemic and fertility intentions during the subsequent epidemic is mediated by subjective assessments of the subsequent crisis. More than three years since the Zika epidemic ended, women who had greater social proximity to the disease during the epidemic perceived a greater risk of infection with COVID-19, were more likely to be worried about fetal and birth complications from COVID-19, and were more likely to believe that all women should avoid pregnancy during the pandemic. These subjective assessments ultimately were associated with a higher likelihood to intend to avoid childbearing because of the COVID-19 pandemic. Had the COVID-19 pandemic not occurred or had it occurred many years after Zika, the impacts of the Zika epidemic might have begun to fade. However, the COVID-19 pandemic appears to have triggered a sense of risk and worry about another novel infectious disease and about childbearing during that new public health crisis that is linked to women’s experiences during the previous epidemic. This finding suggests that the effects of epidemics can spill over from one novel infectious disease outbreak to another.
Second, our results show that social proximity to Zika is an important predictor of women's risk perceptions, worry, and fertility attitudes during a subsequent public health crisis. Whereas prior studies often capture exposure to a disease at a macro level and over a single outbreak, our measure drills down to the more proximate level of women’s social networks in a previous novel infectious disease outbreak. We argue that personally knowing people who have had Zika shapes women’s perceptions of the risks of novel infectious diseases and worries about the consequences for pregnancy likely because novel infectious diseases are more real to them and less of an abstract and distant threat that they hear about in the news. Our results show that social proximity to Zika—whether confirmed or suspected—matters in concrete ways for how women perceive infection risks and worry about pregnancy and fetal complications, which, in turn, shape fertility attitudes and fertility intentions during the COVID-19 pandemic. Our study suggests that collecting data about social proximity to infectious diseases across multiple outbreaks and social networks could be central for understanding how individuals perceive public health risks and how they modify their fertility intentions in response.
Even in the absence of a public health crisis, fertility intentions are often wrapped in at least some worry due to the risks inherent in pregnancy, childbirth, and childrearing. Social proximity to Zika during the epidemic is associated with a heightened likelihood of pregnancy worries during the COVID-19 pandemic. A third key point is that these compounding subjective assessments about novel diseases during consecutive outbreaks could translate into higher levels of stress and adverse mental health during pregnancy, which can also be associated with deleterious pregnancy and birth outcomes similar to the ones found regarding other shocks (Torche and Echevarría 2011).
Fourth, our results point to the potential consequences of the COVID-19 pandemic on fertility behavior in a below replacement level fertility, middle-income, and highly urban and unequal country. As emerging evidence points to fertility decline at least in high-income countries (Kearney and Levine 2020), our ability to distinguish between intentions to postpone versus intentions to forgo pregnancy provides insight into whether observed changes in fertility rates following the pandemic might represent tempo or quantum effects. Supporting Hypothesis 3, we find that the logical sequence of the path between social proximity to Zika and fertility intentions works similarly for postponing and forgoing pregnancy—through subjective assessments of COVID-19—but that only the paths predicting intentions to postpone are statistically significant. This points to a combination of potential tempo and quantum effects if most women are able to fulfill their fertility intentions through fertility rates. There has been some evidence of quantum effects (Sobotka et al. 2023) but not much on tempo effects of the pandemic.
The COVID-19 pandemic has reshaped our world in profound and unequal ways. Drawing evidence from a prior novel infectious disease outbreak, our study showed that the Zika epidemic has left scars that influence fertility intentions years later via subjective assessments. The long-lasting effect of public health crises on fertility rates depends on whether these intentions become reality, but they may leave scars that impact intentions for years to come.
Author Biographies
Leticia J. Marteleto, PhD, is a professor in the Department of Sociology and the Population Studies Center at the University of Pennsylvania. Her research has focused on the connections between social stratification, fertility, and reproductive processes in Latin America and Africa. She has been directing a large-scale data collection study focusing on the consequences of the Zika and COVID-19 public health crises on women’s reproductive trajectories in Brazil.
Molly Dondero is an assistant professor in the Department of Sociology at the American University. Her research focuses on how immigration, race/ethnicity, social class, and place contribute to population-level inequality in health and well-being in the United States and Latin America. She holds a PhD in sociology with a specialization in demography from the University of Texas at Austin.
Andrew Koepp is doctoral candidate in human development and family sciences and a predoctoral trainee at the Population Research Center at the University of Texas at Austin. He studies how educational and family contexts support children’s development and learning.
Whereas previous studies often use the term “exposure” to disease, we use the term “social proximity” to make it clear that we are referring to the people an individual knows who has had a confirmed or suspected case of Zika and not to an individual’s pathogenic exposure to Zika.
We used a dual frame sample design in which 70 percent of the sample was selected through a list-assisted RDD procedure and 30 percent was selected at random from a commercial database. In the RDD frame, we used the available 1,000 banks dedicated to cell phones in the target area code of 81, as informed by the telecommunications authority in Brazil. We then stratified these numbers into three strata. The first two strata were based on region (Stratum 1: metropolitan region of Recife; Stratum 2: nonmetropolitan region Recife) using the location of the plurality of the listed phones, while the third stratum contained those for whom the 1,000 bank did not have any listed cell phone number. The sample was allocated proportionately to the number of 1,000 banks from each stratum. Within Strata 1 and 2, the 1,000 banks were selected with probabilities proportionate to the number of listed phones, and within Stratum 3, they were selected at random. All phone numbers were sampled from the selected 1,000 banks for a total of approximately 3,000,000 phone numbers. More details of the sampling and study procedures are available from authors.
Footnotes
Funding: This research was funded by Grant R01HD091257, Reproductive Responses to the Zika Virus Epidemic in Brazil, awarded to PI L. J. Marteleto by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. This research was also supported by Grants P2CHD042849 and T32HD007081, Population Research Center, awarded to the PRC at The University of Texas at Austin by the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
ORCID iDs: Leticia J. Marteleto  https://orcid.org/0000-0003-4234-0129
https://orcid.org/0000-0003-4234-0129
Molly Dondero  https://orcid.org/0000-0002-2732-3075
https://orcid.org/0000-0002-2732-3075
Andrew Koepp  https://orcid.org/0000-0002-6976-8507
https://orcid.org/0000-0002-6976-8507
References
- Agadjanian Victor, Prata Ndola. 2002. “War, Peace, and Fertility in Angola.” Demography 39(2):215–31. doi: 10.1353/dem.2002.0013. [DOI] [PubMed] [Google Scholar]
- Ajzen Icek. 1991. “The Theory of Planned Behavior.” Theories of Cognitive Self-Regulation 50(2):179–211. doi: 10.1016/0749-5978(91)90020-T. [DOI] [Google Scholar]
- Bachrach Christine A., Morgan S. Philip. 2013. “A Cognitive–Social Model of Fertility Intentions.” Population and Development Review 39(3):459–85. doi: 10.1111/j.1728-4457.2013.00612.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber Jennifer S.2001. “Ideational Influences on the Transition to Parenthood: Attitudes toward Childbearing and Competing Alternatives.” Social Psychology Quarterly 64(2):101–27. doi: 10.2307/3090128. [DOI] [Google Scholar]
- Bernardi Laura. 2013. “From Mothers to Daughters: Intergenerational Transmission of Fertility Norms.” Pp. 165–81 in The Social Meaning of Children and Fertility Change in Europe, edited by Ellingsaeter A. L., Jensen A.-M., Lie M.London: Routledge. [Google Scholar]
- Bhrolcháin Máire Ní, Beaujouan Éva. 2011. “Uncertainty in Fertility Intentions in Britain, 1979-2007.” Vienna Yearbook of Population Research 9:99–129. [Google Scholar]
- Bicchieri Cristina. 2005. “The Rules We Live by.” Pp. 1–54 in The Grammar of Society, edited by Bicchieri C.Cambridge: Cambridge University Press. [Google Scholar]
- Bongaarts John. 2001. “Fertility and Reproductive Preferences in Post-transitional Societies.” Population and Development Review 27:260–81. [Google Scholar]
- Brasil Patrícia, Pereira José P., Moreira M. Elisabeth, Ribeiro Nogueira Rita M., Damasceno Luana, Wakimoto Mayumi, Rabello Renata S., et al. 2016. “Zika Virus Infection in Pregnant Women in Rio de Janeiro.” New England Journal of Medicine 375(24):2321–34. doi: 10.1056/NEJMoa1602412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. 2021. “Pregnant People: At Increased Risk for Severe Illness from COVID-19.” https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/pregnant-people.html.
- Diniz Debora, Brito Luciana, Rondon Gabriela. 2022. “Maternal Mortality and the Lack of Women-Centered Care in Brazil during COVID-19: Preliminary Findings of a Qualitative Study.” The Lancet Regional Health – Americas 10:100239. doi: 10.1016/j.lana.2022.100239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders Craig K.2013. “Dealing with Missing Data in Developmental Research.” Child Development Perspectives 7(1):27–31. doi: 10.1111/cdep.12008. [DOI] [Google Scholar]
- Fishbein Martin, Ajzen Icek. 2010. Predicting and Changing Behavior: The Reasoned Action Approach. New York, NY: Psychology Press. doi: 10.4324/9780203838020. [DOI] [Google Scholar]
- Friedman Debra, Hechter Michael, Kanazawa Satoshi. 1994. “A Theory of the Value of Children.” Demography 31(3):375–401. doi: 10.2307/2061749. [DOI] [PubMed] [Google Scholar]
- Hayford Sarah R., Agadjanian Victor. 2019. “Spacing, Stopping, or Postponing? Fertility Desires in a Sub-Saharan Setting.” Demography 56(2):573–94. doi: 10.1007/s13524-018-0754-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayford Sarah R., Agadjanian Victor, Luz Luciana. 2012. “Now or Never: Perceived HIV Status and Fertility Intentions in Rural Mozambique.” Studies in Family Planning 43(3):191–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hin Saskia, Gauthier Anne, Goldstein Joshua, Bühler Christoph. 2011. “Fertility Preferences: What Measuring Second Choices Teaches Us.” Vienna Yearbook of Population Research 9:131–56. [Google Scholar]
- Horne Christine, Mollborn Stefanie. 2020. “Norms: An Integrated Framework.” Annual Review of Sociology 46(1):467–87. doi: 10.1146/annurev-soc-121919-054658. [DOI] [Google Scholar]
- Instituto Brasileiro de Geografía e Estatística. 2021. “Pesquisa Nacional Por Amostra de Domicílios Contínua - PNAD.” Retrieved March30, 2022. https://www.ibge.gov.br/estatisticas/sociais/educacao/17270-pnad-continua.html?edicao=27138&t=oque-e
- Johns Hopkins Coronavirus Resource Center. 2021. “Brazil: Overview.” https://coronavirus.jhu.edu/region/brazil.
- Johnson-Hanks Jennifer. 2014. “Waiting for the Start: Flexibility and the Question of Convergence.” Pp. 23–40 in Ethnographies of Youth and Temporality: Time Objectified, edited by Dalsgaard A. L., Frederiksen M. D., Højlund S., Meinert L.Philadelphia, PA: Temple University Press. [Google Scholar]
- Kahn Linda G., Trasande Leonardo, Liu Mengling, Mehta-Lee Shilpi S., Brubaker Sara G., Jacobson Melanie H.2021. “Factors Associated with Changes in Pregnancy Intention among Women Who Were Mothers of Young Children in New York City Following the COVID-19 Outbreak.” JAMA Network Open 4(9):e2124273. doi: 10.1001/jamanetworkopen.2021.24273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kearney Melissa S., Levine Phillip. 2020. “The Coming COVID-19 Baby Bust: Update.” Brookings (blog), December17. https://www.brookings.edu/blog/up-front/2020/12/17/the-coming-covid-19-baby-bust-update/.
- Khalil Asma, Dadelszen Peter von, Draycott Tim, Ugwumadu Austin, O’Brien Pat, Magee Laura. 2020. “Change in the Incidence of Stillbirth and Preterm Delivery during the COVID-19 Pandemic.” Journal of the American Medical Association 324(7):705–706. doi: 10.1001/jama.2020.12746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohler Hans-Peter. 2000. “Social Interactions and Fluctuations in Birth Rates.” Population Studies 54(2):223–37. doi: 10.1080/713779084. [DOI] [Google Scholar]
- Kohler Hans-Peter, Behrman Jere R., Watkins Susan C.2007. “Social Networks and HIV/AIDS Risk Perceptions.” Demography 44(1):1–33. doi: 10.1353/dem.2007.0006. [DOI] [PubMed] [Google Scholar]
- The Lancet Planetary Health. 2021. “A Pandemic Era.” The Lancet Planetary Health 5(1):e1. doi: 10.1016/S2542-5196(20)30305-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindstrom David P., Berhanu Betemariam. 1999. “The Impact of War, Famine, and Economic Decline on Marital Fertility in Ethiopia.” Demography 36(2):247–61. doi: 10.2307/2648112. [DOI] [PubMed] [Google Scholar]
- Lucas Adrienne M.2013. “The Impact of Malaria Eradication on Fertility.” Economic Development and Cultural Change 61(3):607–31. doi: 10.1086/669261. [DOI] [Google Scholar]
- Luppi Francesca, Arpino Bruno, Rosina Alessandro. 2020. “The Impact of COVID-19 on Fertility Plans in Italy, Germany, France, Spain, and the United Kingdom.” Demographic Research 43:1399–412. doi: 10.4054/DemRes.2020.43.47. [DOI] [Google Scholar]
- Malicka Izabela, Mynarska Monika, Świderska Joanna. 2021. “Perceived Consequences of the COVID-19 Pandemic and Childbearing Intentions in Poland.” Journal of Family Research 33(3):674–702. doi: 10.20377/jfr-666. [DOI] [Google Scholar]
- Manning Wendy D., Guzzo Karen Benjamin, Longmore Monica A., Giordano Peggy C.2022. “Cognitive Schemas and Fertility Motivations in the US during the COVID-19 Pandemic.” Vienna Yearbook of Population Research 20:1. doi: 10.1553/populationyearbook2022.res1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marteleto Letícia J., Guedes Gilvan, Coutinho Raquel Z., Weitzman Abigail. 2020. “Live Births and Fertility Amid the Zika Epidemic in Brazil.” Demography 57(3):843–72. doi: 10.1007/s13524-020-00871-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maza-Arnedo Fabian, Paternina-Caicedo Angel, Sosa Claudio G., de Mucio Bremen, Rojas-Suarez José, Say Lale, Cresswell Jenny A., et al. 2022. “Maternal Mortality Linked to COVID-19 in Latin America: Results from a Multi-country Collaborative Database of 447 Deaths.” The Lancet Regional Health – Americas 12:100269. doi: 10.1016/j.lana.2022.100269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller Warren B.1994. “Childbearing Motivations, Desires, and Intentions: A Theoretical Framework.” Genetic, Social, and General Psychology Monographs 120(2):223–58. [PubMed] [Google Scholar]
- Miller Warren B.1995. “Childbearing Motivation and Its Measurement.” Journal of Biosocial Science 27(4):473–87. doi: 10.1017/S0021932000023087. [DOI] [PubMed] [Google Scholar]
- Nobles Jenna, Frankenberg Elizabeth, Thomas Duncan. 2015. “The Effects of Mortality on Fertility: Population Dynamics after a Natural Disaster.” Demography 52(1):15–38. doi: 10.1007/s13524-014-0362-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perugini Marco, Bagozzi Richard P.2001. “The Role of Desires and Anticipated Emotions in Goal-Directed Behaviours: Broadening and Deepening the Theory of Planned Behaviour.” British Journal of Social Psychology 40(1):79–98. doi: 10.1348/014466601164704. [DOI] [PubMed] [Google Scholar]
- Rangel Marcos A., Nobles Jenna, Hamoudi Amar. 2020. “Brazil’s Missing Infants: Zika Risk Changes Reproductive Behavior.” Demography 57(5):1647–80. doi:10.1007/s13524-020-00900-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen Sonja A., Jamieson Denise J., Honein Margaret A., Petersen Lyle R.2016. “Zika Virus and Birth Defects—Reviewing the Evidence for Causality.” New England Journal of Medicine 374(20):1981–87. doi: 10.1056/NEJMsr1604338. [DOI] [PubMed] [Google Scholar]
- Riley Amy Henderson, Moeller Patrick, Ramolia Shivani, Stevens Sarah, Pengele Maurice, Chembe Shadrick, Hampande Douglas, et al. 2021. “Measuring Family Planning Norms in Zambia: A Mixed Methods Vignette Study.” African Journal of Reproductive Health 25(5):37–48. [DOI] [PubMed] [Google Scholar]
- Rossier Clémentine, Bernardi Laura. 2009. “Social Interaction Effects on Fertility: Intentions and Behaviors.” European Journal of Population / Revue Europénne de Démographie 25(4):467–85. doi: 10.1007/s10680-009-9203-0. [DOI] [Google Scholar]
- Sennott Christie, Yeatman Sara. 2018. “Conceptualizing Childbearing Ambivalence: A Social and Dynamic Perspective.” Journal of Marriage and Family 80(4):888–901. doi: 10.1111/jomf.12489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shakya Holly B., Weeks John R., Christakis Nicholas A.2019. “Do Village-Level Normative and Network Factors Help Explain Spatial Variability in Adolescent Childbearing in Rural Honduras?” SSM - Population Health 9:100371. doi: 10.1016/j.ssmph.2019.100371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobotka Tomáš, Skirbekk Vegard, Philipov Dimiter. 2011. “Economic Recession and Fertility in the Developed World.” Population and Development Review 37(2):267–306. doi: 10.1111/j.1728-4457.2011.00411.x. [DOI] [PubMed] [Google Scholar]
- Sobotka Tomáš, Zeman Kryštof, Jasilioniene Aiva, Winkler-Dworak Maria, Brzozowska Zuzanna, Alustiza-Galarza Ainhoa, Németh László, et al. 2023. “Pandemic Roller-Coaster? Birth Trends in Higher-Income Countries during the COVID-19 Pandemic.” Population and Development Review. doi: 10.1111/padr.12544. [DOI] [Google Scholar]
- Terceira Nicola, Gregson Simon, Zaba Basia, Mason Peter. 2003. “The Contribution of HIV to Fertility Decline in Rural Zimbabwe, 1985-2000.” Population Studies 57(2):149–64. doi: 10.1080/0032472032000097074. [DOI] [PubMed] [Google Scholar]
- Torche Florencia, Abufhele Alejandra. 2021. “The Normativity of Marriage and the Marriage Premium for Children’s Outcomes.” American Journal of Sociology 126(4):931–68. [Google Scholar]
- Torche Florencia, Echevarría Ghislaine. 2011. “The Effect of Birthweight on Childhood Cognitive Development in a Middle-Income Country.” International Journal of Epidemiology 40(4):1008–18. doi: 10.1093/ije/dyr030. [DOI] [PubMed] [Google Scholar]
- Towriss Catriona A., Beguy Donatien, Wringe Alison, Hussein Barwako Hassan, Timæus Ian M.2020. “Planning a Family in Nairobi’s Informal Settlements: Results of a Qualitative Study.” Journal of Biosocial Science 52(2):286–99. doi: 10.1017/S0021932019000452. [DOI] [PubMed] [Google Scholar]
- Trinitapoli Jenny, Yeatman Sara. 2011. “Uncertainty and Fertility in a Generalized AIDS Epidemic.” American Sociological Review 76(6):935–54. doi: 10.1177/0003122411427672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trinitapoli Jenny, Yeatman Sara. 2018. “The Flexibility of Fertility Preferences in a Context of Uncertainty: Flexibility of Fertility Preferences in a Context of Uncertainty.” Population and Development Review 44(1):87–116. doi: 10.1111/padr.12114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verdery Ashton M., Smith-Greenaway Emily, Margolis Rachel, Daw Jonathan. 2020. “Tracking the Reach of COVID-19 Kin Loss with a Bereavement Multiplier Applied to the United States.” Proceedings of the National Academy of Sciences 117(30):17695–701. doi: 10.1073/pnas.2007476117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeatman Sara. 2009. “HIV Infection and Fertility Preferences in Rural Malawi.” Studies in Family Planning 40(4):261–76. doi: 10.1111/j.1728-4465.2009.00210.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeatman Sara, Sennott Christie, Culpepper Steven. 2013. “Young Women’s Dynamic Family Size Preferences in the Context of Transitioning Fertility.” Demography 50(5):1715–37. doi: 10.1007/s13524-013-0214-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeatman Sara, Trinitapoli Jenny, Garver Sarah. 2020. “The Enduring Case for Fertility Desires.” Demography 57(6):2047–56. doi: 10.1007/s13524-020-00921-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Huaping, Wang Lin, Fang Chengzhi, Peng Sicong, Zhang Lianhong, Chang Guiping, Xia Shiwen, et al. 2020. “Clinical Analysis of 10 Neonates Born to Mothers with 2019-NCoV Pneumonia.” Translational Pediatrics 9(1):51–60. doi: 10.21037/tp.2020.02.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman Linnea A., Karp Celia, Thiongo Mary, Gichangi Peter, Guiella Georges, Gemmill Alison, Moreau Caroline, et al. 2022. “Stability and Change in Fertility Intentions in Response to the COVID-19 Pandemic in Kenya.” PLOS Global Public Health 2(3):e0000147. doi: 10.1371/journal.pgph.0000147. [DOI] [PMC free article] [PubMed] [Google Scholar]