Abstract
The World Health Organization- endorsed Robson Ten Group Classification System (TGCS) is a standard reporting mechanism for cesarean birth, yet this approach is not widely adopted in the US.
Objective:
Describe the application and utility of the TGCS to compare hospital-level cesarean births rates, for use in quality improvement and benchmarking.
Methods:
We conducted a descriptive, secondary data analysis of the Consortium on Safe Labor dataset using data from 228,438 women’s births, from 2002–2008, in 12 sites across the United States. We stratified births into 10 mutually exclusive groups and calculated within group proportions of group size and cesarean birth rates for between-hospital comparisons of cesarean birth, trial of labor after cesarean (TOLAC), and labor induction utilization.
Results:
There is variation in use of cesarean birth, labor induction, and trial of labor after cesarean across the 12 sites.
Conclusion:
The TGCS provides a method for between-hospital comparisons, particularly for revealing usage patterns of labor induction, TOLAC, and cesarean birth. Adoption of the TGCS in the US would provide organizations and quality improvement leaders with an effective benchmarking tool to assist in reducing the use of cesarean birth and increasing the support of trial of labor after cesarean.
Keywords: Cesarean birth, quality improvement, induction of labor, trial of labor after cesarean
Precis:
The Robson Ten Group Classification System, endorsed by the World Health Organization, provides quality improvement leaders with a clinically meaningful tool for evaluating cesarean birth utilization in US hospitals.
INTRODUCTION
While cesarean birth can be a life-saving intervention, the rise in use in the United States (US) over the last 40 years has not been associated with better outcomes for childbearing women or neonates. With cesarean birth rates in the US at 30% of all births,1 safely reducing the incidence of cesarean birth is a priority among public health and perinatal quality leaders.2 Determination of the appropriate level of cesarean birth can be difficult, so comparison of rates across birth facilities aids the understanding of relatively appropriate care.
In the US, reduction of cesarean birth has focused on two groups most susceptible to over-use of cesarean birth among the larger birthing population: nulliparous women with a term, singleton, vertex (NTSV) pregnancy and those with a previous cesarean birth who desire trial of labor after cesarean (TOLAC) with a current pregnancy.3,4 Comparisons of NTSV rates between birth facilities has some value and various risk-adjusted metrics have been proposed to permit appropriate comparisons of perinatal outcomes by facility.5 However, reporting or benchmarking using NTSV or TOLAC rates does not provide a comprehensive picture of patient factors associated with higher use of cesarean birth within a facility. In the US, low risk births occur in community hospitals and tertiary centers and high-risk births typically occur in tertiary centers, eliciting concerns that between facility comparisons are flawed by an inability to account for the acuity of the patient population in the facility. A reporting system that provides a description of a low-risk cesarean birth rate in the context of cesarean birth rates for an entire cohort of childbearing women is desirable for understanding the differences both in patient populations and clinical practices between hospitals. This additional information could more appropriately guide facility-level efforts toward achieving optimal use of cesarean birth.
The Robson Ten-Group Classification System (TGCS) is recommended by the World Health Organization (WHO) as a reliable and clinically relevant classification tool for evaluating and comparing cesarean birth utilization over time, between hospitals, or across geographic regions.6 The TGCS is inclusive of all women who give birth and uses 6 obstetric variables to classify all births into ten mutually exclusive groups. The variables include: (1) parity, (2) previous cesarean section, (3) onset of labor, (4) number of fetuses, (5) gestational age, and (6) fetal lie and presentation. The ten groups are defined in Table 1. Subgroups (2a and 4a) are commonly created to further stratify women according to additional clinically relevant factors, also outlined in Table 1.
Table 1.
Ten-Group Classification System
| 1 | Nulliparous women with a single cephalic pregnancy, ≥ 37 weeks gestation in spontaneous labor |
| 2a | Nulliparous women with a single cephalic pregnancy, ≥ 37 weeks gestation who had labor induced |
| 2b | Nulliparous women with a single cephalic pregnancy, ≥37 weeks gestation who were delivered by cesarean section before labor |
| 3 | Multiparous women without a previous uterine scar, with a single cephalic pregnancy, ≥37 weeks gestation in spontaneous labor |
| 4a | Multiparous women without a previous uterine scar, with a single cephalic pregnancy, ≥37 weeks gestation who had labor induced |
| 4b | Multiparous women without a previous uterine scar, with a single cephalic pregnancy, ≥ 37 weeks gestation who were delivered by cesarean section before labor |
| 5 | All multiparous women with at least one previous uterine scar, with a single cephalic pregnancy ≥37 weeks gestation |
| 6 | All nulliparous women with a single breech pregnancy |
| 7 | All multiparous women with a single breech pregnancy, including women with previous uterine scar |
| 8 | All women with multiple pregnancies, including women with previous uterine scars |
| 9 | All women with a single pregnancy with a transverse or oblique lie, including women with previous uterine scars |
| 10 | All women with a single cephalic pregnancy < 37 weeks gestation, including women with previous uterine scars |
The TGCS provides hospitals and healthcare facilities with a reporting system by which to judge the use of cesarean birth.7–9 Comparison of hospitals and systems with the TGCS helps to identify where difference in cesarean rates are less likely due to differences in patient-specific risk factors and more likely due to differences in hospital-level care management. Birth facility may be a stronger predictor of risk for cesarean birth than maternal factors. In a study of 1,373 hospitals from 2009–2010, the between-hospital variation in risk was 0.14 (95% CI, 0.12 to 0.15), a variation not attributable to maternal factors.10,11 The WHO expects that facilities that use the TGCS can:
Identify and analyze the groups of women which contribute most and least to overall cesarean section rates.
Compare practice in these groups of women with other units who have more desirable results and consider changes in practice.
Assess the effectiveness of strategies or interventions targeted at optimizing the use of cesarean section.
Assess the quality of care and of clinical management practices by analyzing outcomes by groups of women.
Assess the quality of the data collected and raise staff awareness about the importance of this data, interpretation, and use.6
While the TGCS has been widely used globally, there are fewer studies using this classification system with US birth data.12–14 Previous studies using the TGCS in the US have used birth certificate data to investigate trends over time and provide a reference point for benchmarking, though not specific to individual hospitals or systems.15 The purpose of this study was to demonstrate feasibility of the TGCS for quality improvement by providing hospital-level comparisons of cesarean birth utilization in a sample of US childbearing women.
The authors recognize that not all birthing people are women. However, women/woman is used throughout the manuscript to be consistent with the sample population in the dataset and the language of the WHO Robson Classification Implementation Manual6.
METHODS
In this secondary data analysis, the TGCS was applied to the Consortium on Safe Labor (CSL) dataset. The CSL dataset includes births in the US between 2002–2008 in 12 sites located in multiple geographic regions of the US and with varied capabilities; academic, community teaching, and community non-teaching hospitals.16,17 There were 228,562 births to 208,695 women reported in the CSL dataset. We excluded from analysis any birth with missing or incomplete data in one of the 6 key variables used for stratification, resulting in the exclusion of 124 births (0.05%). The final analysis includes 228,438 births. We chose existing CSL variables consistent with TGCS classifications for (1) parity (nulliparous or multiparous), (2) previous cesarean, (3) onset of labor (spontaneous or induced), (4) number of fetuses (singleton or multiple), (5) gestational age (<37 weeks or ≥37 weeks), and (6) fetal lie (oblique or transverse) and presentation (cephalic), we assigned all births in the CSL to one of the 10 mutually exclusive groups (Figure 1). We then differentiated births by birth site for between facility comparisons.
Figure 1.
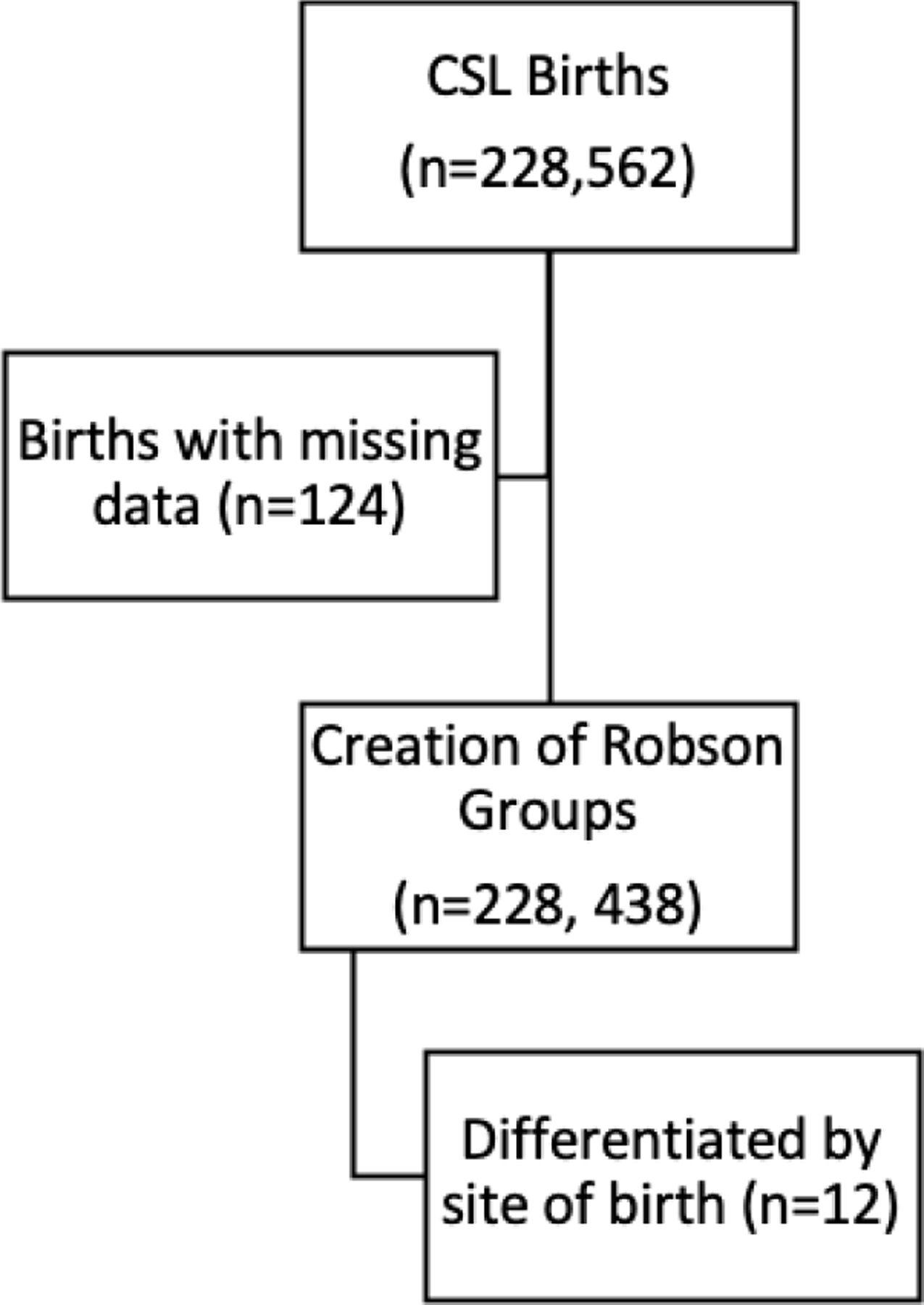
Sample selection
A within-group analysis was completed identifying (1) size of each group in relation to the overall population within the site (Group size (%)= n of women in the group/total N women delivered in the hospital *100), (2) the rate of cesarean delivery within each group (Group cesarean rate (%)= n of cesarean birth in the group/ total N of women in the group *100), and (3) the relative contribution of each groups’ cesarean birth rate to the overall cesarean rate (Relative contribution (%) = n of cesarean in the group/ total N of cesarean birth in the hospital *100). The WHO implementation guide, in addition to prior published work, contains additional detail on reporting and interpretation of results.6,18,19
RESULTS
Results are reported by the 10 groups across sites in Table 2. Because the intent of this paper is to describe the utility of the TGCS, results will be reported by group, with relational and contextual benchmarks to aid in interpretation.
Table 2.
TGCS Results Across 12 Sites (N=228,438)
| Site | A | B | C | D | E | F | G | H | I | J | K | L | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Births (n) | 20,779 | 50,320 | 12,637 | 6,420 | 7,877 | 20,329 | 14,667 | 27,869 | 7,749 | 23,141 | 18,392 | 18,258 | |
| Cesarean Births (%) | 20.5 | 22.0 | 23.6 | 24.2 | 25.4 | 28.8 | 28.8 | 31.6 | 34.6 | 34.9 | 35.0 | 44.3 | |
|
| |||||||||||||
|
Group 1 ≥37wks Nulliparous Singleton Cephalic Spontaneous Labor |
Group Sizea (%) | 21.1 | 20.6 | 21.1 | 12.1 | 23.6 | 23.0 | 17.5 | 18.9 | 19.5 | 13.0 | 12.4 | 6.5 |
| Cesarean Rateb (%) | 15.0 | 15.8 | 13.0 | 12.2 | 17.1 | 17.5 | 18.4 | 20.3 | 22.0 | 16.0 | 18.0 | 27.5 | |
| Contribution to overall ratec (%) | 3.2 | 3.3 | 2.3 | 1.5 | 4.0 | 4.0 | 3.2 | 3.8 | 4.3 | 2.1 | 2.2 | 1.8 | |
|
| |||||||||||||
|
2a ≥37wks Nulliparous Singleton Cephalic Induced Labor |
Group Size (%) | 9.2 | 10.0 | 10.1 | 18.5 | 8.6 | 10.3 | 14.7 | 14.7 | 11.9 | 16.8 | 27.0 | 23.5 |
| Cesarean Rate (%) | 34.8 | 20.2 | 28.4 | 25.5 | 32.1 | 34.9 | 36.5 | 36.0 | 40.2 | 33.2 | 29.2 | 42.1 | |
| Contribution to overall rate (%) | 3.2 | 2.0 | 2.9 | 4.7 | 2.8 | 3.6 | 5.4 | 5.3 | 4.8 | 5.6 | 7.8 | 9.9 | |
|
| |||||||||||||
|
2b ≥37wks Nulliparous Singleton Cephalic Prelabor Cesarean |
Group Size (%) | 1.0 | 0.1 | 0.4 | 0.5 | 0.9 | 1.0 | 2.0 | 1.0 | 1.3 | 2.0 | 3.7 | 1.9 |
| Cesarean Rate (%) | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | |
| Contribution to overall rate (%) | 1.0 | 0.1 | 0.4 | 0.5 | 0.9 | 1.0 | 2.0 | 1.0 | 1.3 | 2.0 | 3.7 | 1.9 | |
|
| |||||||||||||
|
3 ≥37wks Multiparous Singleton Cephalic Spontaneous Labor |
Group Size (%) | 39.0 | 25.3 | 26.5 | 19.9 | 31.0 | 27.4 | 23.0 | 22.1 | 23.0 | 17.1 | 15.3 | 13.8 |
| Cesarean Rate (%) | 2.4 | 3.6 | 2.5 | 3.8 | 3.9 | 3.3 | 3.8 | 7.2 | 4.2 | 3.7 | 3.2 | 7.3 | |
| Contribution to overall rate (%) | 0.9 | 0.9 | 0.7 | 0.8 | 1.2 | 0.9 | 0.9 | 1.6 | 1.0 | 0.6 | 0.5 | 1.0 | |
|
| |||||||||||||
|
4a ≥37wks Multiparous Singleton Cephalic Induced Labor |
Group Size (%) | 9.3 | 21.0 | 9.9 | 17.6 | 10.2 | 9.4 | 18.1 | 14.0 | 12.3 | 15.4 | 15.3 | 17.7 |
| Cesarean Rate (%) | 7.8 | 2.7 | 10.0 | 5.6 | 4.0 | 7.8 | 5.9 | 9.2 | 7.5 | 7.3 | 6.1 | 16.5 | |
| Contribution to overall rate (%) | 0.7 | 0.6 | 1.0 | 1.0 | 0.4 | 0.7 | 1.0 | 1.3 | 0.9 | 1.1 | 0.9 | 2.9 | |
|
| |||||||||||||
|
4b ≥37wks Multiparous Singleton Cephalic Prelabor Cesarean |
Group Size (%) | 0.6 | 0.1 | 0.5 | 0.4 | 0.9 | 0.8 | 1.0 | 0.8 | 0.6 | 1.3 | 0.8 | 0.9 |
| Cesarean Rate (%) | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | |
| Contribution to overall rate (%) | 0.6 | 0.1 | 0.5 | 0.4 | 0.9 | 0.8 | 1.0 | 0.8 | 0.6 | 1.3 | 0.8 | 0.9 | |
|
| |||||||||||||
|
5 ≥ 37wks Multiparous Singleton Cephalic w/previous Uterine scar |
Group Size (%) | 9.4 | 11.0 | 10.3 | 11.5 | 11.2 | 11.4 | 11.1 | 11.3 | 13.3 | 11.7 | 12.2 | 14.1 |
| Cesarean Rate (%) | 62.0 | 80.5 | 62.4 | 68.7 | 78.3 | 78.9 | 89.2 | 81.6 | 84.8 | 88.9 | 85.9 | 97.4 | |
| Contribution to overall rate (%) | 5.9 | 8.8 | 6.4 | 7.9 | 8.8 | 9.0 | 9.9 | 9.2 | 11.3 | 10.4 | 10.5 | 13.7 | |
|
| |||||||||||||
|
6 All Nulliparous Singleton Breech |
Group Size (%) | 1.1 | 1.4 | 1.6 | 1.0 | 0.0 | 1.9 | 0.3 | 1.6 | 1.7 | 1.2 | 2.4 | 1.7 |
| Cesarean Rate (%) | 96.9 | 94.8 | 87.0 | 98.4 | 0.0 | 99.7 | 84.8 | 94.0 | 94.6 | 98.6 | 100 | 95.0 | |
| Contribution to overall rate (%) | 1.1 | 1.3 | 1.4 | 1.0 | 0.0 | 1.9 | 0.3 | 1.5 | 1.6 | 1.2 | 2.4 | 1.7 | |
|
| |||||||||||||
|
7 All Multiparous Single Breech incl. w/previous Uterine scar |
Group Size (%) | 1.4 | 1.5 | 2.5 | 1.3 | 0.0 | 1.7 | 0.3 | 1.8 | 1.6 | 1.6 | 1.0 | 2.3 |
| Cesarean Rate (%) | 89.8 | 93.2 | 91.0 | 96.3 | 0.0 | 100 | 88.0 | 92.6 | 90.1 | 95.0 | 98.3 | 91.5 | |
| Contribution to overall rate (%) | 1.2 | 1.4 | 2.3 | 1.2 | 0.0 | 1.7 | 0.3 | 1.7 | 1.4 | 1.5 | 1.0 | 2.1 | |
|
| |||||||||||||
|
8 All Multiple including w/ previous Uterine scars |
Group Size (%) | 0.9 | 1.9 | 2.5 | 2.1 | 1.7 | 3.2 | 2.2 | 2.3 | 2.0 | 2.8 | 2.9 | 2.2 |
| Cesarean Rate (%) | 61.1 | 66.4 | 47.0 | 59.3 | 59.6 | 63.2 | 63.0 | 68.3 | 78.4 | 73.9 | 77.8 | 81.2 | |
| Contribution to overall rate (%) | 0.5 | 1.3 | 1.2 | 1.3 | 1.0 | 2.0 | 1.4 | 1.6 | 1.6 | 2.0 | 2.3 | 1.8 | |
|
| |||||||||||||
|
9 All Singleton Transverse or oblique incl. w/ previous Uterine scars |
Group Size (%) | 0.0 | 0.1 | 0.4 | 0.1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.4 | 0.2 | 0.0 | 0.4 |
| Cesarean Rate (%) | 0.0 | 94.4 | 93.3 | 100 | 0.0 | 0.0 | 0.0 | 0.0 | 100 | 98.2 | 0.0 | 98.6 | |
| Contribution to overall rate (%) | 0.0 | 0.1 | 0.3 | 0.1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.4 | 0.2 | 0.0 | 0.4 | |
|
| |||||||||||||
|
10 <37wks Singleton Cephalic Incl. w/ previous Uterine scars |
Group Size (%) | 5.7 | 7.9 | 14.1 | 15.0 | 9.4 | 9.7 | 9.6 | 10.4 | 12.7 | 16.4 | 7.1 | 13.0 |
| Cesarean Rate (%) | 34.2 | 28.6 | 26.6 | 26.1 | 30.4 | 29.6 | 35.1 | 32.4 | 44.0 | 40.5 | 40.5 | 44.0 | |
| Contribution to overall rate (%) | 1.9 | 2.3 | 3.7 | 4.0 | 2.9 | 2.9 | 3.4 | 3.4 | 5.6 | 6.7 | 2.9 | 5.7 | |
These totals and percentages come from the data in the table.
Group size (%) = n of women in the group / total N women delivered in the hospital x 100
Group CS rate (%) = n of CS in the group / total N of women in the group x 100
Relative contribution (%) = n of CS in the group / total N of CS in the hospital x 10011
Each reporting mechanism is useful in the overall understanding use of cesarean birth rates and will be explained for each group. Three proportions are reported for each group: 1) The relative size of the group is helpful for distinguishing women who enter labor spontaneously, have induced labor, or a prelabor cesarean birth at each site. Differences in group sizes within a site provide an epidemiological portrait of the population as well as insights into clinical practice in the site. 2) Within group cesarean birth rates identify the proportion of women who underwent cesarean birth for each TGCS group and represents differences in clinical practice between sites. 3) Relative contribution is a proportion of the overall cesarean rate, indicates how the within group rate affected a particular sites’ overall rate, and represents differences in clinical practice between sites.
Overall Cesarean Birth Rate
Overall cesarean birth rates across the 12 sites ranged from 20.5% to 44.3%. Seven of the 12 sites had overall cesarean birth rates less than 30%, at or below the mean cesarean birth rate across the CSL (30.5%).16 The overall cesarean rate is slightly less than the overall rate of cesarean birth in the US at the time (32.3%), and with less variation than that of a nationwide study which reported 10-fold variation.20–21 A US population-based study from 2005–2014 reported an overall cesarean birth rate of 31.6%.22 The WHO multi-country survey reported the cesarean birth rate worldwide was 31.2% and in high Human Development Index countries was 40%.23
Group 1: Nulliparous women with a single cephalic pregnancy, ≥37 weeks gestation in spontaneous labor
The proportion of births in group 1 ranged across sites from 23% to as few as 6.5%, and there was a two-fold difference of rates of cesarean birth from 12.2% to 27.5%. A population-based study in the US reported group size at 17% and a 12.3% cesarean birth rate for women in group 1. It has been suggested that cesarean rates of 10% are achievable in this population.6
Group 2a: Nulliparous women with a single cephalic pregnancy, ≥37 weeks gestation who had induced labor
Group size for 2a ranged from 9.2% to 27% of births. Cesarean birth rates in the group ranged from 20.2 to 42.1%, and the relative contribution of births to women who were induced ranged from 2.1% to 11.9%, with higher proportions indicating the significant role that cesarean births to nulliparous women with induced labor contributed to overall cesarean rates. In the nationwide sample, group size was consistently around 8% over a 10-year period, and cesarean birth rates of 25%.22
Group 2b: Nulliparous women with a single cephalic pregnancy, ≥37 weeks gestation who were delivered by cesarean section before labor
Prelabor cesarean births occurred at low rates; range 0.08–3.7% (mean 1.3%, mode 1.9%). Hehir, et al22, reported prelabor cesarean births occurred for 3% of the population of nulliparous women over a 10-year period.
Group 3: Multiparous women without a previous uterine scar, with a single cephalic pregnancy, ≥37 weeks gestation in spontaneous labor
There was variation in births to women in group 3 from a high of 39% to as few as 13.8%. Cesarean birth rates ranged from 2.4–7.3%. Worldwide, the proportion of multiparous women in spontaneous labor decreased to 25% in 2011, down from 28.9% in 2008.23 Across the US, women in group 3 were 31.0% of the population, and rate of cesarean birth was 4.4%.22 Group 3 is expected to have a lesser influence on overall cesarean rate and most of 12 sites had cesarean rates consistent with expected rates around 2–3%,24 though 2 sites had cesarean rates near 7% in this group.
Group 4a: Multiparous women without a previous uterine scar, with a single cephalic pregnancy, ≥37 weeks gestation who had labor induced
Group size for induced multiparous women ranged from 9.9% to 18.6% of the birthing population, and cesarean birth rates ranged from 2.7%−16.5% for women who had previously given birth vaginally. This is consistent with a nationwide average of 12.6% group size with 8.1% cesarean section rate6.
Group 4b: Multiparous women without a previous uterine scar, with a single cephalic pregnancy, ≥37 weeks gestation who were delivered by cesarean section before labor
Prelabor cesarean births among multiparous women were a very small proportion of the population across sites in the CSL (0.1–1.3%) and contributed little to overall cesarean rates.
Group 5: All multiparous women with at least one previous uterine scar, with a single cephalic pregnancy, ≥37 weeks gestation
This group represents the population of women eligible for TOLAC and potential subsequent VBAC. Group sizes were consistent across the 12 sites, ranging from 9.4–14.1% of the sample. Cesarean rates to women in Group 5 ranged from 62–97%, which provides us with some information about how a facility might approach their management of TOLAC/VBAC. Sites with cesarean rates cesarean rates of 90% and higher likely reflect sites that are unsupportive of TOLAC, and sites near 70% are more likely to offer women an opportunity to labor and attempt vaginal birth. VBAC in many sites were consistent with reported US average of near 70% success for women who attempt trial of labor after cesarean.25
Repeat cesarean births are the largest contributor to overall cesarean rates in all sites; contribution to the overall cesarean birth rate ranged from 5.9–13.7%, with most sites having between 8–10% contribution to the overall rate. In the US population as a whole, 10.3% of childbearing women have experienced prior cesarean delivery.26 From 2005–2014, percentage of obstetric population with a prior cesarean rose from 11.2 to 12.2%, and the cesarean birth rate among these women was 87.8%.6
Groups 6–9: Women with abnormal fetal lie or multiple pregnancies
Births to women in these groups were near or equal to 100% cesarean birth rates. Additionally, these groups have smaller, as expected, contributions to overall cesarean rates. Births to women in groups 6–9 are predictable across the population. The size of group 9 should be less than 1%6, groups 6 and 7 combined should be 3–4%, and group 8 should be 1.5–2%, and was consistent with the reported data in other CSL studies.
Group 10: All women with a single cephalic pregnancy <37 weeks gestation, including women with previous scars
Across sites in the CSL, the rate of preterm birth, group 10, ranged from 5.7% to 16.4%, which is consistent with the description of sites reported as a mix of community and tertiary hospitals, with varying capability and patient acuity. The size of group 10 can be indicative of the level of acuity of a facility, where more at-risk births are likely to take place. In the 10-year US population study, the preterm birth rate was 10%, and cesarean birth rates 37.9%.6 Preterm birth cesarean rates in this study ranged from 26.6 to 44%.
DISCUSSION
This analysis provides an example of how perinatal safety and quality leaders can apply the TGCS for categorizing data for benchmarking. Our assessment of the feasibility of applying the TGCS with this project is: (1) TGCS is easy to apply to a large, existing dataset, as data available within the dataset did not require data transformation. (2) The information provided by the TGCS demonstrated its utility in assessing cesarean use both within a single facility and across birth facilities. (3) The TGCS demonstrates how the overall cesarean rate is affected by the subpopulations. (4) The criteria are useful for demonstrating variation in the use of labor induction, prelabor cesarean birth, and TOLAC between facilities.
The TGCS has practical applicability in the US. Perinatal quality leaders could consider using the TGCS to compare cesarean birth rates between labor and birth units within the same health system or geographic region, as a reporting system for evaluating the effectiveness of interventions, for use in an audit and feedback strategy27, to further explore the populations for whom there are more cesarean births occurring, and to identify the specific features of the clinical setting which attribute to overuse of cesarean birth. For example, some individual hospitals may have midwives integrated into their care. Previous work this team conducted using this same dataset demonstrated that the presence of midwives was associated with differences in use of labor interventions and lower use of cesarean birth.28–30 Variation in rates of cesarean birth should spur perinatal leaders and quality managers to conduct further investigation into the aspects of clinical practice that drive these differences.
Use of Labor Induction
Accurately capturing use of labor induction and cesarean sections among groups 2a and 4a is an important part of a comprehensive benchmarking strategy. Labor induction rates have risen all around the world.23 In the US, labor induction rose from 9.5% to 23.2% of births over the last 20 years.31 In this analysis, sites with higher rates of labor induction in nulliparous women (Groups 2a, 8.6–26.9%), also demonstrated higher rates of labor induction in multiparous women (Group 4a, 9.3–18.1%). Cesarean birth rates in women who were induced were higher than rates for women who enter labor spontaneously (Groups 2a and 4a). In similar TGCS studies, institutional variation in cesarean birth was proportional to group size of spontaneously laboring women.32 In another TGCS study, women in group 2a (induced labor) were almost twice as likely to require a cesarean as those in group 1 (spontaneous labor) (26.2% vs 13.2%).6 However, this phenomenon could change with time. Since publication of a large, randomized control trial supporting routine use of 39-week labor induction, it is likely that there will be a larger proportion of women in groups 2a and 4a.33 Information on use of labor induction from this study will be valuable as a historical reference when observing changes that will likely occur in coming years.
Limitations
The age of the data makes the current clinical applicability somewhat limited because there have been many changes to quality indicators, clinical practice, and clinical recommendations. However, as a demonstration of the TGCS application, this study provides historical information that can be used now to assist in understanding the change over time.
CONCLUSION
Our study piloted the TGCS in a well-known and respected dataset and noted variation in cesarean birth, labor induction, TOLAC, and preterm birth across 12 sites. Within each site, the TGCS demonstrated how groups contributed to the overall cesarean birth rate. The TGCS was easily employed to stratify the sample population using obstetric variables that are routinely collected on admission for labor and birth by facilities around the globe. The TGCS proves a useful tool for quality improvement as it permits comparisons across units, hospitals, health systems, and countries, pre- and post-intervention, or over time. Uniform classifications allow comparisons among similar patient populations, and there is clinical relevance in the interpretation.
Continued efforts are needed to reduce cesarean births in the US. Birth facilities need more detailed information to understand the drivers of cesarean birth, tailor clinical interventions, and provide risk-appropriate care to childbearing women. This analysis illustrates the areas where individual sites can focus their quality improvement efforts to improve cesarean birth rates.
ACKNOWLEDGEMENTS
The Consortium on Safe Labor was supported by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, through a contract (Contract No. HHSN267200603425C).
The data included in this paper were obtained from the Consortium on Safe Labor, supported by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health. Institutions involved in the Consortium include, in alphabetical order: Baystate Medical Center, Springfield, MA; Cedars-Sinai Medical Center Burnes Allen Research Center, Los Angeles, CA; Christiana Care Health System, Newark, DE; Georgetown University Hospital, MedStar Health, Washington, DC; Indiana University Clarian Health, Indianapolis, IN; Intermountain Healthcare and the University of Utah, Salt Lake City, Utah; Maimonides Medical Center, Brooklyn, NY; MetroHealth Medical Center, Cleveland, OH.; Summa Health System, Akron City Hospital, Akron, OH; The EMMES Corporation, Rockville MD (Data Coordinating Center); University of Illinois at Chicago, Chicago, IL; University of Miami, Miami, FL; and University of Texas Health Science Center at Houston, Houston, Texas. The authors alone are responsible for the views expressed in this manuscript, which does not necessarily represent the decisions or the stated policy of the NICHD. We would like to thank the Principal Investigators that conducted the original Consortium of Safe Labor study as well as the NICHD for funding the study and NICHD DASH for providing us with the data.
Dr. Ellen L. Tilden received support from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and National Institutes of Health Office of Research on Women’s Health, Oregon BIRCWH Scholars in Women’s Health Research Across the Lifespan (K12HD043488‐14).
Dr. Julia C. Phillippi received support from a Vanderbilt University Medical Center Faculty Research Scholars Award and was supported by grant number K08HS024733 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Dr. Nicole S. Carlson received support by grant number 1K01NR016984–01 from the National Institutes of Health, National Institute of Nursing Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Abbreviations:
- WHO
World Health Organization
- TGCS
Robson Ten-Group Classification System
- CS
Cesarean Section
- NTSV
Nulliparous, Term, Singleton, Vertex
- US
United States
- CSL
Consortium for Safe Labor
- NICHD
National Institute of Child Health and Human Development
- IOL
Induction of Labor
- TOLAC
Trial of Labor after Cesarean
- VBAC
Vaginal Birth After Cesarean
Contributor Information
Denise Colter Smith, College of Nursing, University of Colorado, Aurora CO.
Julia C. Phillippi, Vanderbilt University School of Nursing, Nashville TN.
Ellen L. Tilden, Oregon Health Sciences University Schools of Nursing and Medicine, Portland OR.
Nancy K. Lowe, College of Nursing, University of Colorado, Aurora CO.
Nicole S. Carlson, Emory University School of Nursing, Atlanta GA.
Jeremy L. Neal, Vanderbilt University School of Nursing, Nashville TN.
Rachel Blankstein Breman, University of Maryland, School of Nursing, Baltimore, MD.
References
- 1.Martin JA, Hamilton BE, Osterman MJ, Driscoll AK. Births: Final data for 2018 2019; [PubMed]
- 2.ACOG Committee on Obstetric Practicelo. ACOG Committee Opinion No. 745: Mode of Term Singleton Breech Delivery: Interim Update. Obstet Gynecol August 2018. 2018;132(2):e60–63. [DOI] [PubMed] [Google Scholar]
- 3.Main EK, Moore D, Farrell B, et al. Is there a useful cesarean birth measure? Assessment of the nulliparous term singleton vertex cesarean birth rate as a tool for obstetric quality improvement. American Journal of Obstetrics & Gynecology 2006;194(6):1644–1651. [DOI] [PubMed] [Google Scholar]
- 4.Spong CY, Berghella V, Wenstrom KD, Mercer BM, Saade GR. Preventing the first cesarean delivery: summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, and American College of Obstetricians and Gynecologists Workshop. Obstetrics and gynecology 2012;120(5):1181–93. doi: 10.1097/AOG.0b013e3182704880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American College of Obstetricians and Gynecologists, Society for Maternal-Fetal Medicine. Obstetric care consensus no. 2: Levels of maternal care. Obstet Gynecol 2015;125(2):502–15. doi: 10.1097/01.AOG.0000460770.99574.9f [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization. Robson classification: implementation manual 2017.
- 7.Robson MS. Classification of caesarean section. Fetal and Maternal Medicine Review 2001;12(1):23–39. doi: 10.1017/s0965539501000122 [DOI] [Google Scholar]
- 8.Robson MS. The 10-Group Classification System–a new way of thinking. American Journal of Obstetrics & Gynecology 2018;219(1):1–4. doi: 10.1016/j.ajog.2018.05.026 [DOI] [PubMed] [Google Scholar]
- 9.Rossen J, Lucovnik M, Eggebø TM, et al. A method to assess obstetric outcomes using the 10-Group Classification System: a quantitative descriptive study. BMJ open 2017;7(7):e016192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shaw D, Guise J-M, Shah N, et al. Drivers of maternity care in high-income countries: can health systems support woman-centred care? The Lancet 2016;388(10057):2282–2295. [DOI] [PubMed] [Google Scholar]
- 11.Kozhimannil KB, Arcaya MC, Subramanian S. Maternal clinical diagnoses and hospital variation in the risk of cesarean delivery: analyses of a National US Hospital Discharge Database. PLoS Med 2014;11(10):e1001745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Betrán AP, Gulmezoglu AM, Robson M, et al. WHO Global Survey on Maternal and Perinatal Health in Latin America: classifying caesarean sections. journal article. Reproductive Health October 29 2009;6(1):18. doi: 10.1186/1742-4755-6-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roberge S, Dubé E, Blouin S, Chaillet N. Reporting Caesarean Delivery in Quebec Using the Robson Classification System. J Obstet Gynaecol Can: JOGC = Journal d’obstetrique et gynecologie du Canada : JOGC 2017;39(3):152–156. [DOI] [PubMed] [Google Scholar]
- 14.Vogel JP, Betrán AP, Vindevoghel N, et al. Use of the Robson Classification to assess caesarean section trends in 21 countries: a secondary analysis of two WHO multicountry surveys. The Lancet Global Health 2015;3(5):e260–e270. doi: 10.1016/S2214-109X(15)70094-X [DOI] [PubMed] [Google Scholar]
- 15.Hehir MP, Ananth CV, Siddiq Z, Flood K, Friedman AM, D’Alton ME. Cesarean delivery in the United States 2005 through 2014: a population-based analysis using the Robson 10-Group Classification System. American Journal of Obstetrics & Gynecology 2018; [DOI] [PubMed]
- 16.Zhang J, Troendle J, Reddy UM, et al. Contemporary cesarean delivery practice in the United States. Am J Obstet Gynecol Oct 2010;203(4):326.e1–326.e10. doi: 10.1016/j.ajog.2010.06.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang J, Landy HJ, Branch DW, et al. Contemporary patterns of spontaneous labor with normal neonatal outcomes. Obstetrics and gynecology 2010;116(6):1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Robson M, Murphy M, Byrne F . Quality assurance: The 10-Group Classification System (Robson classification), induction of labor, and cesarean delivery. International Journal of Gynecology & Obstetrics 2015;131:S23–S27. doi: 10.1016/j.ijgo.2015.04.026 [DOI] [PubMed] [Google Scholar]
- 19.World Health Organization. Robson classification: example of Robson report table with interpretation 2017.
- 20.Martin JA, Hamilton BE, Ventura SJ, et al. Births: final data for 2009. National vital statistics reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System 2011;60(1):1–70. [PubMed] [Google Scholar]
- 21.Kozhimannil KB, Law MR, Virnig BA. Cesarean delivery rates vary tenfold among US hospitals; reducing variation may address quality and cost issues. Health Aff (Millwood) 2013;32(3):527–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hehir MP, Ananth CV, Siddiq Z, Flood K, Friedman AM, D’Alton ME. Cesarean delivery in the United States 2005 through 2014: a population-based analysis using the Robson 10-Group Classification System. Am J Obstet Gynecol Jul 2018;219(1):105.e1–105.e11. doi: 10.1016/j.ajog.2018.04.012 [DOI] [PubMed] [Google Scholar]
- 23.Vogel JP, Betrán AP, Vindevoghel N, et al. Use of the Robson classification to assess caesarean section trends in 21 countries: a secondary analysis of two WHO multicountry surveys. The Lancet Global Health 2015;3(5):e260–e270. [DOI] [PubMed] [Google Scholar]
- 24.Robson M, Hartigan L, Murphy M. Methods of achieving and maintaining an appropriate caesarean section rate. Best Practice & Research Clinical Obstetrics & Gynaecology 2013/April/01/ 2013;27(2):297–308. doi: 10.1016/j.bpobgyn.2012.09.004 [DOI] [PubMed] [Google Scholar]
- 25.Grobman WA, Lai Y, Landon MB, et al. Can a prediction model for vaginal birth after cesarean also predict the probability of morbidity related to a trial of labor? American journal of obstetrics and gynecology 2009;200(1):56. e1–56. e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Osterman MJ, Martin JA. Trends in low-risk cesarean delivery in the United States, 1990–2013. National Vital Statistics Reports National Center for Health Statistics; 2014;63(6). Accessed ACCESS DATE? [PubMed] [Google Scholar]
- 27.Scarella A, Chamy V, Sepúlveda M, Belizán JM. Medical audit using the Ten Group Classification System and its impact on the cesarean section rate. European Journal of Obstetrics & Gynecology and Reproductive Biology 2011/February/01/ 2011;154(2):136–140. doi: 10.1016/j.ejogrb.2010.09.005 [DOI] [PubMed] [Google Scholar]
- 28.Neal JL, Carlson NS, Phillippi JC, et al. Midwifery presence in United States medical centers and labor care and birth outcomes among low‐risk nulliparous women: A Consortium on Safe Labor study. Birth 2019;46(3):475–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carlson NS, Neal JL, Tilden EL, et al. Influence of midwifery presence in United States centers on labor care and outcomes of low‐risk parous women: A Consortium on Safe Labor study. Birth 2019;46(3):487–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smith DC, Phillippi JC, Lowe NK, et al. Using the Robson 10‐group classification system to compare cesarean birth utilization between US centers with and without midwives. J Midwifery Womens Health 2020;65(1):10–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Osterman MJ, Martin JA. Recent declines in induction of labor by gestational age. NCHS Data Brief Jun 2014;(155):1–8. [PubMed] [Google Scholar]
- 32.Brennan DJ, Robson MS, Murphy M, O’herlihy C. Comparative analysis of international cesarean delivery rates using 10-group classification identifies significant variation in spontaneous labor. American journal of obstetrics and gynecology 2009;201(3):308. e1–308. e8. [DOI] [PubMed] [Google Scholar]
- 33.Grobman WA, Rice MM, Reddy UM, et al. Labor induction versus expectant management in low-risk nulliparous women. New England Journal of Medicine 2018;379(6):513–523. [DOI] [PMC free article] [PubMed] [Google Scholar]


