Summary
Background
Laparoscopic surgery remains limited in low-resource settings. We aimed to examine its use in Mexico and determine associated factors.
Methods
By querying open-source databases, we conducted a nationwide retrospective analysis of three common surgical procedures (i.e., cholecystectomies, appendectomies, and inguinal hernia repairs) performed in Mexican public hospitals in 2021. Procedures were classified as laparoscopic based on ICD-9 codes. We extracted patient (e.g., insurance status), clinical (e.g., anaesthesia technique), and geographic data (e.g., region) from procedures performed in hospitals and ambulatories. Multivariable analysis with random forest modelling was performed to identify associated factors and their importance in adopting laparoscopic approach.
Findings
We included 97,234 surgical procedures across 676 public hospitals. In total, 16,061 (16.5%) were performed using laparoscopic approaches, which were less common across all procedure categories. The proportion of laparoscopic procedures per 100,000 inhabitants was highest in the northwest (22.2%, 16/72) while the southeast had the lowest (8.3%, 13/155). Significant factors associated with a laparoscopic approach were female sex, number of municipality inhabitants, region, anaesthesia technique, and type of procedure. The number of municipality inhabitants had the highest contribution to the multivariable model.
Interpretation
Laparoscopic procedures were more commonly performed in highly populated, urban, and wealthy northern areas. Access to laparoscopic techniques was mostly influenced by the conditions of the settings where procedures are performed, rather than patients' non-modifiable characteristics. These findings call for tailored interventions to sustainably address equitable access to minimally invasive surgery in Mexico.
Funding
None.
Keywords: Appendectomy, Cholecystectomy, Global surgery, Health disparities, Inguinal hernia repair, Minimally invasive surgery
Research in context.
Evidence before this study
In high-income countries (HICs), laparoscopic surgery is preferred for most frequently performed intra-abdominal procedures. This approach is favoured over open techniques because of reduced postoperative complications, shorter length of hospitalisation, and faster return to daily activities. These benefits are potentially more important in low-resource settings in which a reduction in opportunity cost is substantial in the setting of possibly catastrophic or impoverishing expenditure. However, laparoscopic surgery remains unavailable for many people living in low- and middle-income countries (LMICs), where it is estimated that only 2% of the population can access affordable minimally-invasive surgical services. We must assess whether a population has access to laparoscopic surgery to address context-related challenges and develop national policies to promote the sustainability of minimally invasive procedures. This question has not been answered in Latin America, as evidence reporting the availability of laparoscopic surgery in the region is limited.
Added value of this study
As the third-largest country and second-largest economy in Latin America, Mexican public policies hold the potential to impact others and prompt similar change throughout the region. Our research utilised hospital and municipal-based data to cross-sectionally determine nationwide access to the three most common laparoscopic procedures, as well as geographic predictors for their implementation. We found that laparoscopy was employed less frequently compared to open technique overall and in all Mexican regions and states. It represented 32% (13,560/42,317), 5.6% (2298/41,174), and 1.5% (203/13,743) of cholecystectomies, appendectomies, and inguinal herniorrhaphy, respectively. Conversely, studies in HICs reported higher percentages of laparoscopy implementation, reaching 94% in cholecystectomies and 93% in appendectomies. Furthermore, a random forest model was used to determine the contribution of each variable in the adoption of laparoscopic techniques. This analysis shows that the conditions of the localities where procedures were performed were more predictive of the use of laparoscopy than were patients’ individual non-modifiable characteristics. These results show that assertive policymaking at the regional, state, and municipal levels could have a significant impact on improving access to minimally invasive surgery in Mexico.
Implications of all the available evidence
Latin America is a highly complex region. Its culturally diverse population, growing economies, and constant political change perpetuate inequalities within the region. At the national level, Mexico demonstrates some of the greatest disparities noted worldwide. Based on the Gini index 45.4, it is ranked 27th in the world for income inequality and economic concentration. Despite the benefits of minimally invasive surgery, our findings suggest that the open technique remains the most available surgical approach in the Mexican public health system. Laparoscopic techniques are more commonly used in highly populated, urban, and northern areas. Future work is needed to understand context-specific barriers to accessing minimally invasive procedures in Mexico.
Introduction
The laparoscopic approach has become preferred for many common intra-abdominal procedures such as appendectomy, cholecystectomy, and inguinal hernia repairs.1,2 In high-income countries (HICs), this approach is favoured over open operations due to reduced infection rates and blood loss, improved postoperative pain, shorter hospitalisation, and faster return to daily activities.2,3 However, laparoscopic surgery remains largely unavailable in low- and middle-income countries (LMICs), where only 2% of the population can access affordable minimally-invasive surgical services.3,4 Within LMICs, these services are predominantly accessible to higher-income patients, while the poor and marginalised are left with limited access.2,5 This is unfortunate, as minimally invasive surgery is associated with a decreased risk of wound infections and blood loss, which is relevant as many low-resource facilities lack blood banks and advanced sanitation resources.3 Furthermore, laparoscopic procedures can play a pivotal role in locations where a return to economic activity and reduced length of hospitalisation are imperative. Reduced postoperative complications, shorter length of hospitalisation, and faster return to daily activities are potentially more important in low-resource settings in which a reduction in opportunity cost is substantial in the setting of possibly catastrophic or impoverishing expenditure.3,6,7
To develop national policies for sustainable minimally invasive surgery, an assessment of the population's access to laparoscopic surgery is first required. The current evidence has explored the availability of minimally invasive surgery primarily in HICs, while little has been reported about its access in LMICs, including Latin America, preventing countries from analysing their local context and identifying facilitators and barriers.8 As the second-largest country by population and economy in Latin America, Mexico exerts a powerful potential for impacting public policies in the region.9 Therefore, a deeper understanding of the issue in Mexico can generate insights that might apply to other Latin American countries and LMICs with similar characteristics and disparities.
In this study, we sought to examine the nationwide access to laparoscopic surgery in Mexican public hospitals across three common laparoscopic procedures and determine the association between the adoption of laparoscopic techniques and geographic, demographic, and clinical factors.
Methods
Study design
We reported this study following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.10 We conducted a retrospective analysis of surgeries performed in Mexican public hospitals by using open-source nationwide-level data from the Procedimientos and Egresos Hospitalarios databases.11 Both databases provide health data from public hospitals administered by the Mexican Ministry of Health (Secretaria de Salud), which represent approximately one-third of the country's total number of hospitals.12 While Procedimientos captures aggregated geographical and resource-related data about surgeries performed at hospitals and ambulatories, Egresos Hospitalarios provides de-identified data concerning in-hospital surgical operations at the patient and clinical levels.
We extracted data from 2021, as this was the most recent complete year from which we could retrieve information. We queried the databases and used their entry identification codes to track demographic, clinical, and geographical information about surgical procedures. Additionally, we extracted the number of inhabitants from included municipalities from the latest 2020 National Census available from the Mexican Institute of Statistics and Geography (Instituto Nacional de Estadística y Geografía, INEGI).13
Eligibility criteria
We included laparoscopic and open procedures using the International Classification of Diseases Procedure Codes (ICD-9-PCS) for cholecystectomy, appendectomy, and inguinal hernia repair (Supplementary Material S1). This was the most recent ICD code version available in the databases. Procedures not identified as laparoscopic were considered open. There was no information regarding the conversion of laparoscopic procedures to an open approach. In case the codes did not match with ICD-9-PCS, manual analysis was conducted to identify missing procedure codes and extract data (Supplementary Material S1). For the purposes of this study, we excluded robotic cases due to the limited availability of surgical robots within the Mexican public health sector.14
Proportions of laparoscopic procedures were adjusted to 100,000 inhabitants. Estimates of the evaluated population by state were obtained by summing the number of inhabitants of municipalities where procedures were performed. Each state was mapped using Excel version 2212 (© Geonames, Microsoft, TomTom, 2023).
Laparoscopic versus open approach to the included procedures was the primary outcome of interest. Analysed factors included demographic, clinical, and geographic features. Concerning demographic factors, we extracted data on patients' age, sex, self-identification with indigenous ethnicity, and insurance status. Clinical variables included procedure type (i.e., cholecystectomy, appendectomy, and hernia inguinal repair), anaesthesia technique, and length of hospitalisation in days. According to the Mexican Official Anaesthesiology Norm, general anaesthesia was defined as the administration of injected or inhaled medication, resulting in complete patient unconsciousness and unresponsiveness. Regional anaesthesia was characterised as the injection of local anaesthetics into specific nerves or nerve bundles, blocking sensation and motor function in the supplied anatomical area. Local anaesthesia was described as a loss of sensation and motor function restricted to a specific operative area. Lastly, combined anaesthesia was considered to be the simultaneous use of general and regional anaesthesia techniques.15 Based on these definitions, we excluded anaesthesia-related data from 1247 procedures classified in the categories of “not undergoing anaesthesia”, “sedation”, or “unspecified technique”. We presumed these data were a product of miscategorisation during data collection.
We also extracted hospital characteristics, particularly their geographic location (i.e., municipality, state, and region), whether they were situated in urban or rural areas, level of care (i.e., primary, secondary, and tertiary), number of hospital beds, number of surgeons, number of anaesthesiologists, and population density at the municipality level.
Statistical analysis
Categorical variables were summarised using frequency with percentages. Continuous variables were summarised by means and standard deviations or medians and interquartile ranges, depending on whether the variable followed or departed from the normal distribution, respectively. Due to privacy protection and confidentiality, we did not report cells with less than or equal to 10 individuals for sociodemographic data extracted from Egresos Hospitalarios.16 We purposefully selected variables available on the queried databases for the univariable and multivariable analyses. As independent demographic factors, we included patients' age, sex, indigenous identity, and insurance status. Clinical factors encompassed procedure type (i.e., cholecystectomy, appendectomy, and inguinal hernia repair) and anaesthesia technique (i.e., general, regional, local, and combined). Accounted geographical factors included rural or urban settings, the Mexican region, and the municipality's population where the procedure happened. The variable addressing the municipality population was log-transformed. We converted the insurance variable from categorical to dichotomous by combining “government,” “employment,” and “other” as the category representing insured patients, and “none” and “missing” as the category representing uninsured patients. For dichotomous variables whose categories were “Yes” and “No,” we adopted the “No” category as reference. For all other categorical variables, we selected as reference category the one with the highest number of laparoscopic procedures reported.
We used logistic regression to conduct the univariable and multivariable analyses and assess the association between factor and outcome variables. We did not use any threshold to include variables in the multivariable model. Hence, we incorporated all variables from the univariable analysis into the multivariable model. We also performed a random forest model, a Machine Learning-based method, to identify the importance of each variable used in the multivariable analysis. We conducted this analysis to provide a ranking of factors, which is impossible by only considering P-values from the multivariable model, for building a predictive model. The Variable Importance Plot is created to incorporate this information in the Results section. Missing data were handled by complete case analysis. Results were reported with 95% confidence intervals (CIs), and two-sided P-values <0.05 were considered statistically significant. All analyses were performed in Stata17 (Statacorp LLC; College Station, TX) and R (version 4.0.3).
Ethical aspects
This project was submitted to the Institutional Review Board of the Harvard Faculty of Medicine and considered non-human subjects research (protocol # IRB23-0178).
Role of the funding source
The present study had no source of funding.
Results
Descriptive analysis
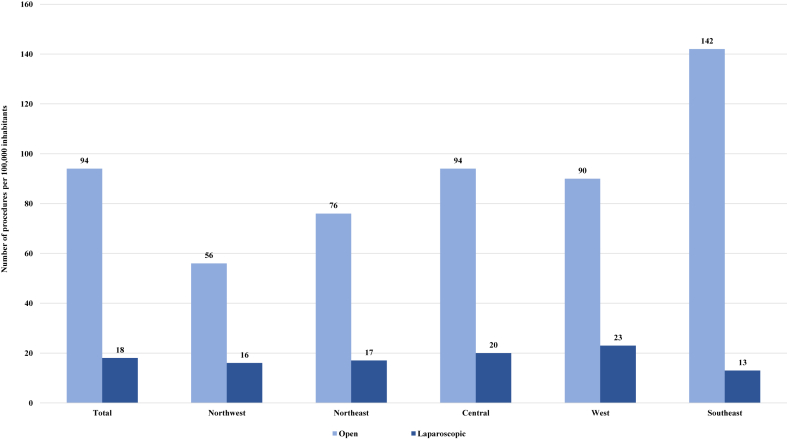
By retrieving data from the Procedimientos database, we included 97,234 registered surgical procedures performed at the hospital and ambulatory levels across all 32 Mexican states, including Ciudad de México. In total, 81,173 (83.4%) and 16,061 (16.5%) procedures were performed using open and laparoscopic techniques, respectively (Supplementary Material S2). Adjusting by the population from assessed municipalities, 94 open and 18 laparoscopic procedures were performed per 100,000 inhabitants (Table 1). The most common procedure was cholecystectomy (49 per 100,000 inhabitants), followed by appendectomy (47 per 100,000 inhabitants) and inguinal hernia repair (15 per 100,000 inhabitants). Across procedures, the laparoscopic technique was less commonly utilised compared to open techniques (Table 1, Supplementary Material S2).
Table 1.
Procedure techniques across Mexican regions and states adjusted by 100,000 inhabitants according to Procedimientos 2021.
| Evaluated population (%) | All procedures totals (per 100,000 inhabitants) |
Cholecystectomy (per 100,000 inhabitants) |
Appendectomy (per 100,000 inhabitants) |
Inguinal hernia repair (per 100,000 inhabitants) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Open | Laparoscopic | Total | Open | Laparoscopic | Total | Open | Laparoscopic | Total | Open | Laparoscopic | Total | ||
| All regions | 86,314,503 | 94 | 18 | 112 | 33 | 16 | 49 | 45 | 3 | 48 | 15 | 0 | 15 |
| Northwest | 13,266,633 | 56 | 16 | 72 | 18 | 13 | 31 | 28 | 2 | 30 | 10 | 0 | 10 |
| Baja California | 3,769,020 (28.4) | 37 | 8 | 45 | 9 | 7 | 16 | 24 | 1 | 24 | 5 | 0 | 5 |
| Baja California Sur | 798,447 (6) | 72 | 12 | 84 | 25 | 5 | 30 | 43 | 6 | 49 | 10 | 0 | 10 |
| Chihuahua | 3,218,130 (24.3) | 64 | 14 | 78 | 23 | 13 | 36 | 31 | 1 | 33 | 10 | 0 | 10 |
| Sinaloa | 2,978,282 (22.4) | 61 | 26 | 87 | 18 | 24 | 42 | 27 | 2 | 29 | 18 | 0 | 18 |
| Sonora | 2,502,754 (18.9) | 64 | 18 | 82 | 22 | 15 | 37 | 34 | 3 | 37 | 11 | 1 | 12 |
| Northeast | 10,741,085 | 76 | 17 | 93 | 32 | 15 | 47 | 32 | 3 | 34 | 12 | 0 | 12 |
| Cohauila de Zaragoza | 2,715,496 (25.3) | 52 | 13 | 65 | 22 | 12 | 34 | 22 | 1 | 23 | 8 | 0 | 8 |
| Durango | 1,530,518 (14.2) | 88 | 7 | 95 | 33 | 6 | 39 | 36 | 1 | 37 | 19 | 0 | 19 |
| Nuevo León | 1,326,476 (12.3) | 61 | 45 | 106 | 8 | 39 | 47 | 42 | 7 | 48 | 11 | 0 | 11 |
| San Luis Potosi | 1,918,679 (17.9) | 104 | 15 | 119 | 50 | 10 | 60 | 38 | 6 | 43 | 15 | 0 | 15 |
| Tamaulipas | 3,249,916 (30.3) | 82 | 15 | 97 | 39 | 14 | 53 | 30 | 2 | 32 | 12 | 0 | 12 |
| Central | 28,335,221 | 94 | 20 | 114 | 29 | 15 | 44 | 50 | 4 | 54 | 15 | 0 | 15 |
| Ciudad de México | 8,744,636 (30.9) | 67 | 28 | 95 | 14 | 21 | 35 | 42 | 7 | 49 | 10 | 1 | 10 |
| Guerrero | 1,880,892 (6.6) | 124 | 8 | 132 | 34 | 7 | 41 | 77 | 1 | 78 | 13 | 0 | 13 |
| Hidalgo | 1,045,288 (3.7) | 242 | 53 | 295 | 92 | 51 | 143 | 107 | 3 | 110 | 42 | 0 | 42 |
| México | 10,981,818 (38.7) | 80 | 12 | 92 | 30 | 12 | 42 | 37 | 1 | 38 | 13 | 0 | 13 |
| Morelos | 1,081,094 (3.8) | 116 | 12 | 128 | 30 | 3 | 33 | 80 | 8 | 81 | 6 | 0 | 6 |
| Puebla | 4,186,662 (14.8) | 116 | 19 | 135 | 35 | 11 | 46 | 57 | 8 | 65 | 24 | 0 | 24 |
| Tlaxcala | 414,831 (1.5) | 249 | 35 | 284 | 60 | 34 | 94 | 142 | 1 | 144 | 47 | 0 | 47 |
| West | 18,276,032 | 90 | 23 | 113 | 29 | 21 | 50 | 42 | 2 | 44 | 19 | 0 | 19 |
| Aguascalientes | 1,112,255 (6.1) | 79 | 50 | 129 | 19 | 43 | 62 | 44 | 6 | 50 | 17 | 0 | 17 |
| Colima | 464,384 (2.5) | 141 | 8 | 149 | 53 | 5 | 58 | 69 | 3 | 71 | 19 | 0 | 19 |
| Guanajuato | 5,678,651 (31.1) | 76 | 25 | 101 | 21 | 22 | 43 | 39 | 2 | 41 | 16 | 1 | 17 |
| Jalisco | 4,565,480 (25) | 81 | 25 | 106 | 24 | 23 | 47 | 37 | 1 | 38 | 21 | 0 | 21 |
| Michoacán | 3,073,203 (16.8) | 117 | 13 | 131 | 52 | 10 | 63 | 41 | 3 | 44 | 24 | 0 | 24 |
| Nayarit | 847,839 (4.6) | 101 | 15 | 116 | 30 | 15 | 45 | 55 | 0 | 55 | 16 | 0 | 16 |
| Querétaro | 1,510,840 (8.3) | 66 | 27 | 93 | 7 | 25 | 33 | 48 | 2 | 49 | 11 | 0 | 11 |
| Zacatecas | 1,023,380 (5.6) | 138 | 14 | 152 | 58 | 13 | 71 | 56 | 1 | 57 | 24 | 0 | 24 |
| Southeast | 15,695,532 | 142 | 13 | 155 | 59 | 11 | 70 | 63 | 2 | 64 | 21 | 0 | 21 |
| Campeche | 772,164 (4.9) | 149 | 14 | 163 | 64 | 13 | 77 | 66 | 0 | 66 | 19 | 0 | 19 |
| Chiapas | 3,191,624 (20.3) | 175 | 4 | 179 | 70 | 4 | 74 | 84 | 0 | 84 | 22 | 0 | 22 |
| Oaxaca | 1,604,896 (10.2) | 201 | 1 | 202 | 77 | 1 | 78 | 95 | 1 | 96 | 28 | 0 | 28 |
| Quintana-Roo | 1,713,418 (10.9) | 68 | 15 | 84 | 21 | 13 | 34 | 39 | 2 | 41 | 8 | 0 | 8 |
| Tabasco | 2,402,598 (15.3) | 126 | 5 | 131 | 70 | 4 | 74 | 42 | 1 | 42 | 15 | 0 | 15 |
| Veracruz | 4,754,299 (30.3) | 138 | 12 | 150 | 57 | 9 | 66 | 55 | 3 | 58 | 25 | 0 | 25 |
| Yucatán | 1,256,533 (8) | 122 | 70 | 192 | 39 | 65 | 104 | 64 | 5 | 69 | 18 | 0 | 18 |
Caption: Percentages have been approximated to one decimal place and may not sum up to 100%.
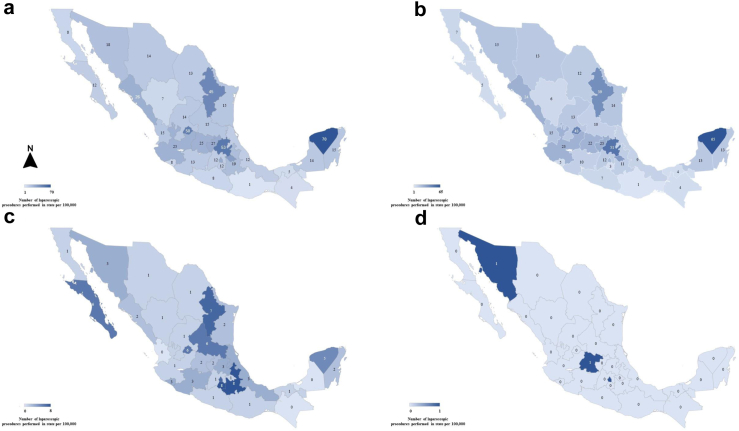
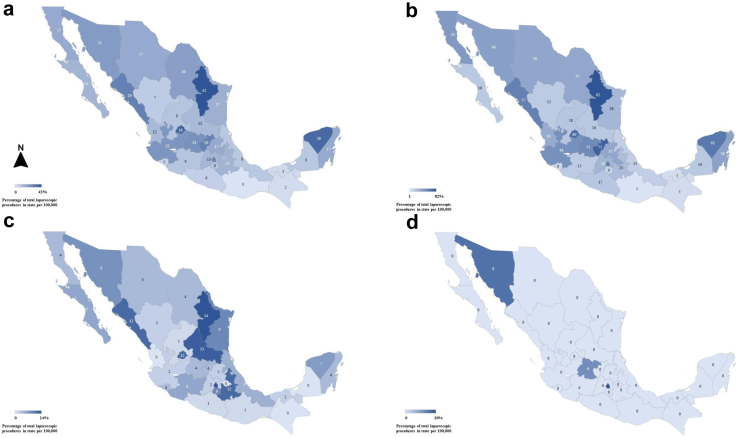
The proportion of laparoscopic operations was highest in the northwest (16 of 72 procedures per 100,000 inhabitants) while the southeast had the lowest (13 of 155 procedures per 100,000 inhabitants), as shown in Fig. 1. Analysis per Mexican state identified that Nuevo León (45 of 106 procedures per 100,000 inhabitants) and Oaxaca (1 of 202 procedures per 100,000 inhabitants) demonstrated the highest and lowest proportion of laparoscopic procedures, respectively (Fig. 2, Fig. 3).
Fig. 1.
Proportion of total laparoscopic procedures per 100,000 inhabitants by region. This series of graphs shows the number of open and laparoscopic procedures per 100,000 inhabitants by region.
Fig. 2.
Number of laparoscopic procedures per 100,000 inhabitants by state for a) total, b) cholecystectomy, c) appendectomy, and d) inguinal hernia repair operations. This series of graphs shows the number of laparoscopic procedures adjusted per 100,000 inhabitants by state for a) total, b) cholecystectomy, c) appendectomy, and d) inguinal hernia repair operations. The states of Mexico that reside within the dark blue area have higher percentages of laparoscopic procedures, compared to areas in light blue that have lower percentages.
Fig. 3.
Proportion of laparoscopic procedures per 100,000 inhabitants by state for a) total, b) cholecystectomy, c) appendectomy, and d) inguinal hernia repair operations. This series of graphs shows the proportion of laparoscopic procedures adjusted per 100,000 inhabitants by state for a) total, b) cholecystectomy, c) appendectomy, and d) inguinal hernia repair operations. Proportions were obtained dividing the number of laparoscopic procedures by the total number of procedures per examined category. The states of Mexico that reside within the dark blue area have higher percentages of laparoscopic procedures, compared to areas in light blue that have lower percentages.
Procedures were performed across 676 Mexican public hospitals, comprising 50,368 surgical beds (Table 2). Most hospitals were located in the central (29.1%, 197/676), southeast (27.8%, 188/676), and west (20.2%, 137/676) regions. Of the 676 assessed hospitals, 31 (4.5%) served rural areas, and 668 (98.8%) were secondary or tertiary centres. The northwest (4, IQR = 6), northeast (4, IQR = 7), and central (4, IQR = 7) regions had the highest median number of surgeons per hospital. The northwest (6, IQR = 7) and central regions (6, IQR = 9) had the highest median number of anaesthesiologists per hospital. In contrast, the southeast had the lowest median number of surgeons (3, IQR = 3) and anaesthesiologists per hospital (4, IQR = 4).
Table 2.
Hospital characteristics across Mexican regions and states according to Procedimientos 2021.
| Total population (%) | Evaluated population (%) | Hospitals (%) | Rural hospitals (%) | Urban hospitals (%) | Secondary and tertiary hospitals (%) | Total number of beds (%) | Surgeons–median (IQR) | Anesthesiologists–median (IQR) | |
|---|---|---|---|---|---|---|---|---|---|
| Total | 126,014,024 | 86,314,503 | 676 | 31 | 645 | 668 | 50,368 | 4 (5) | 5 (7) |
| Northwest | 14,281,119 | 13,266,633 | 74 | 0 | 74 | 71 | 5794 | 4 (6) | 6 (7) |
| Baja California | 3,769,020 (26.4) | 3,769,020 (28.4) | 8 (10.8) | 0 (0) | 8 (10.8) | 8 (11.3) | 1025 (17.7) | 7.5 (15.5) | 11.5 (9) |
| Baja California Sur | 798,447 (5.6) | 798,447 (6) | 7 (9.5) | 0 (0) | 7 (9.5) | 5 (7) | 399 (6.9) | 4 (5) | 4 (4) |
| Chihuahua | 3,741,869 (26.2) | 3,218,130 (24.3) | 22 (29.7) | 0 (0) | 22 (29.7) | 21 (29.6) | 1605 (27.7) | 3.5 (6) | 5.5 (6) |
| Sinaloa | 3,026,943 (21.2) | 2,978,282 (22.4) | 22 (29.7) | 0 (0) | 22 (29.7) | 22 (31) | 1461 (25.2) | 4 (4) | 4 (8) |
| Sonora | 2,944,840 (20.6) | 2,502,754 (18.9) | 15 (20.3) | 0 (0) | 15 (20.3) | 15 (21.1) | 1304 (22.5) | 5 (7) | 6 (5) |
| Northeast | 17,113,853 | 10,741,085 | 80 | 0 | 80 | 77 | 6119 | 4 (7) | 5 (7) |
| Cohauila de Zaragoza | 3,146,771 (18.4) | 2,715,496 (25.3) | 16 (20) | 0 (0) | 16 (20) | 15 (19.5) | 932 (15.2) | 4.5 (5) | 5 (5) |
| Durango | 1,832,650 (10.7) | 1,530,518 (14.2) | 15 (18.7) | 0 (0) | 15 (18.7) | 15 (19.5) | 933 (15.2) | 2 (3) | 2.5 (3) |
| Nuevo León | 5,784,442 (33.8) | 1,326,476 (12.3) | 8 (10) | 0 (0) | 8 (10) | 8 (10.4) | 900 (14.7) | 4 (6) | 4 (17.5) |
| San Luis Potosi | 2,822,255 (16.5) | 1,918,679 (17.9) | 15 (18.7) | 0 (0) | 15 (18.7) | 14 (18.2) | 1306 (21.3) | 4 (5) | 4 (6) |
| Tamaulipas | 3,527,735 (20.6) | 3,249,916 (30.3) | 26 (32.5) | 0 (0) | 26 (32.5) | 25 (32.4) | 2048 (33.5) | 3.5 (8) | 6 (8) |
| Central | 42,723,663 | 28,335,221 | 197 | 19 | 178 | 197 | 16,659 | 4 (7) | 6 (9) |
| Ciudad de México | 9,209,944 (21.6) | 8,744,636 (30.9) | 34 (17.3) | 0 (0) | 34 (19.1) | 34 (17.2) | 5820 (34.9) | 14.5 (18) | 15.5 (15) |
| Guerrero | 3,540,685 (8.3) | 1,880,892 (6.6) | 19 (9.6) | 1 (5.3) | 18 (10.1) | 19 (9.6) | 1173 (7) | 3 (6) | 6 (7) |
| Hidalgo | 3,082,841 (7.2) | 1,045,288 (3.7) | 17 (8.6) | 3 (15.8) | 14 (7.9) | 17 (8.6) | 1076 (6.5) | 4 (2) | 5 (4) |
| Estado de México | 16,992,418 (39.8) | 10,981,818 (38.7) | 56 (28.4) | 10 (52.6) | 46 (25.8) | 56 (28.4) | 4801 (28.8) | 5 (8) | 7 (9) |
| Morelos | 1,971,520 (4.6) | 1,081,094 (3.8) | 11 (5.6) | 0 (0) | 11 (6.2) | 11 (5.6) | 735 (4.4) | 5 (7) | 7 (8) |
| Puebla | 6,583,278 (15.4) | 4,186,662 (14.8) | 50 (25.4) | 4 (21) | 46 (25.8) | 50 (25.4) | 2368 (14.2) | 2.5 (3) | 4 (5) |
| Tlaxcala | 1,342,977 (3.1) | 414,831 (1.5) | 10 (5.1) | 1 (5.3) | 9 (5.1) | 10 (5.1) | 686 (4.1) | 7 (3) | 5.5 (7) |
| West | 26,646,990 | 18,276,032 | 137 | 4 | 133 | 135 | 10,670 | 3 (5) | 5 (7) |
| Aguascalientes | 1,425,607 (5.3) | 1,112,255 (6.1) | 6 (4.4) | 0 (0) | 6 (4.5) | 6 (4.4) | 510 (4.8) | 6.5 (10) | 10.5 (10) |
| Colima | 731,391 (2.7) | 464,384 (2.5) | 4 (2.9) | 0 (0) | 4 (3) | 4 (3) | 358 (3.4) | 6 (6) | 8.5 (10) |
| Guanajuato | 6,166,934 (23.1) | 5,678,651 (31.1) | 36 (26.3) | 0 (0) | 36 (27.1) | 36 (26.7) | 2587 (24.2) | 3 (6) | 7 (8) |
| Jalisco | 8,348,151 (31.3) | 4,565,480 (25) | 31 (22.6) | 0 (0) | 31 (23.3) | 31 (23) | 2890 (27.1) | 3.5 (7) | 4 (4) |
| Michoacán | 4,748,846 (17.8) | 3073,203 (16.8) | 32 (23.4) | 3 (75) | 29 (21.8) | 31 (23) | 2133 (20) | 4 (3) | 5 (5) |
| Nayarit | 1,235,456 (4.6) | 847,839 (4.6) | 8 (5.8) | 1 (25) | 7 (5.2) | 8 (5.9) | 441 (4.1) | 2.5 (1) | 4 (2.5) |
| Querétaro | 2,368,467 (8.9) | 1,510,840 (8.3) | 7 (5.1) | 0 (0) | 7 (5.2) | 6 (4.4) | 1072 (10) | 6 (18) | 7 (32) |
| Zacatecas | 1,622,138 (6.1) | 1,023,380 (5.6) | 13 (9.5) | 0 (0) | 13 (9.7) | 13 (9.6) | 679 (6.4) | 2 (6) | 4 (8) |
| South-east | 25,248,399 | 15,695,532 | 188 | 8 | 180 | 187 | 11,126 | 3 (3) | 4 (4) |
| Campeche | 928,363 (3.7) | 772,164 (4.9) | 8 (4.2) | 1 (12.5) | 7 (3.9) | 8 (4.3) | 589 (5.3) | 3.5 (3.5) | 4.5 (2.5) |
| Chiapas | 5,543,828 (22) | 3,191,624 (20.3) | 39 (20.7) | 1 (12.5) | 38 (21.1) | 39 (20.8) | 2058 (18.5) | 4 (3) | 4 (8) |
| Oaxaca | 4,132,148 (16.4) | 1,604,896 (10.2) | 43 (22.9) | 1 (12.5) | 42 (23.3) | 43 (23) | 1943 (17.5) | 4 (2) | 4 (3) |
| Quintana-Roo | 1,857,985 (7.3) | 1,713,418 (10.9) | 8 (4.2) | 0 (0) | 8 (4.4) | 8 (4.3) | 750 (6.7) | 5.5 (7.5) | 6.5 (6.5) |
| Tabasco | 2,402,598 (9.5) | 2,402,598 (15.3) | 22 (11.7) | 2 (25) | 20 (11.1) | 22 (11.8) | 1493 (13.4) | 2 (3) | 5 (5) |
| Veracruz | 8,062,579 (31.9) | 4,754,299 (30.3) | 59 (31.4) | 3 (37.5) | 56 (31.1) | 58 (31) | 3308 (29.7) | 3 (4) | 3 (4) |
| Yucatán | 2,320,898 (9.2) | 1,256,533 (8) | 9 (4.8) | 0 (0) | 9 (5) | 9 (4.8) | 985 (8.9) | 4 (6) | 5 (6) |
Caption: Percentages have been approximated to one decimal place and may not sum up to 100%.
Based on the data from Egresos Hospitalarios, we analysed a sample of 28,837 in-hospital procedures to understand the demographic, geographic, and clinical characteristics of patients undergoing included procedures (Table 3). In this sample, 23,760 (82.3%) and 5077 (17.6%) procedures were performed using open and laparoscopic techniques, respectively. The mean age of patients who underwent a laparoscopic procedure was 37 years (SD = 16) compared to 32 years (SD = 19) among open procedures. Additionally, the percentage of female patients undergoing a laparoscopic procedure was higher (76.4%, 3879/5077) in comparison to men. 2.5% (708/28,837) of included patients self-identified as indigenous. Laparoscopic procedures were performed at a higher percentage in uninsured patients (52.7%, 2678/5077) when compared to open procedures (48.8%, 11,592/23,760). In contrast, open procedures presented a larger percentage of patients with government-provided insurance (35.4%, 8415/23,760) compared to laparoscopic procedures (30.6%, 1552/5077).
Table 3.
Demographic, geographic and clinical characteristics of procedure techniques according to procedures registered in Egresos Hospitalarios 2021.
| Procedures (n = 28 837) | Open (n = 23 760) | Laparoscopic (n = 5077) | |
|---|---|---|---|
| Age (%) | |||
| Mean (SD) | 33 (22) | 32 (19) | 37 (16) |
| Sex (%) | |||
| Male | 12,176 (42.2) | 10,979 (46.2) | 1197 (23.6) |
| Female | 16,657 (57.8) | 12,778 (53.8) | 3879 (76.4) |
| Missing | 4 (0) | 3 (0) | 1 (0) |
| Indigenous ethnicity (%) | |||
| Yes | 708 (2.5) | 627 (2.6) | 81 (1.6) |
| No | 28,129 (97.5) | 23,133 (97.4) | 4996 (98.4) |
| Insurance (%)a | |||
| None | 14,270 (49.5) | 11,592 (48.8) | 2678 (52.7) |
| Government | 9967 (34.6) | 8415 (35.4) | 1552 (30.6) |
| Employment | 125 (0.4) | 89 (0.4) | 36 (0.7) |
| Other | 185 (0.6) | 160 (0.7) | 25 (0.5) |
| Missing | 4290 (14.9) | 3504 (14.7) | 786 (15.5) |
| Region (%) | |||
| Northwest | 2620 (9.1) | 2039 (8.6) | 581 (11.4) |
| Northeast | 2897 (10) | 2257 (9.5) | 640 (12.6) |
| Central | 10,065 (34.9) | 8324 (35) | 1741 (34.3) |
| West | 6178 (21.4) | 4848 (20.4) | 1330 (26.2) |
| Southeast | 6645 (23) | 5978 (25.2) | 667 (13.1) |
| Missing | 432 (1.5) | 314 (1.3) | 118 (2.3) |
| Hospital (%) | |||
| Urban | 27,569 (95.6) | 22,668 (95.4) | 4901 (96.5) |
| Rural | 1268 (4.4) | 1092 (4.6) | 176 (3.5) |
| Municipality population percentile (%) | |||
| <25% | 7193 (24.9) | 6720 (26.4) | 923 (18.2) |
| 25%–75% | 14,699 (51) | 12,625 (53.1) | 2074 (40.8) |
| >75% | 6945 (24.1) | 4865 (20.5) | 2080 (41) |
| Anaesthesia technique (%) | |||
| General | 9950 (34.5) | 6726 (28.3) | 3224 (63.5) |
| Regional | 16,510 (57.2) | 15,092 (63.5) | 1418 (27.9) |
| Local | 188 (0.6) | 139 (0.6) | 49 (1) |
| Combined | 942 (3.3) | 843 (3.5) | 99 (2) |
| Missing | 1247 (4.3) | 960 (4) | 287 (5.6) |
| Procedure type (%) | |||
| Cholecystectomy | 12,290 (42.6) | 7992 (33.6) | 4298 (84.7) |
| Appendectomy | 12,687 (44) | 11,972 (50.4) | 715 (14.1) |
| Inguinal hernia repair | 3860 (13.4) | 3796 (16) | 64 (1.2) |
| Days of hospitalization | |||
| Median (IQR) | 2 (3) | 2 (3) | 2 (1) |
Cells containing less than or equal to 10 patients were hidden to ensure privacy protection and confidentiality. Percentages have been approximated to one decimal place and may not sum up to 100%.
Laparoscopic procedures were less frequent in municipalities with smaller population sizes, particularly those below the 25th percentile (18.2%, 923/5077). The most common anaesthesia technique among laparoscopic procedures was general anaesthesia (63.5%, 3224/5077), whereas regional anaesthesia prevailed among open procedures (63.5%, 15,092/23,760). A subanalysis of this sample across the three procedure categories (i.e., cholecystectomy, appendectomy, inguinal hernia repair) is provided in Table 4.
Table 4.
Characteristics of procedures performed across cholecystectomy, appendectomy and inguinal hernia repair based on procedures registered in Egresos Hospitalarios 2021.
| Number of procedures (%) | Age–Mean (SD) | Sex (%)a |
Indigenous ethnicity (%)a | Insurance (%)a |
Rural hospital (%) | Urban hospital (%) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | None | Government | Employment | ||||||
| Total | 28,837 | 33 (22) | 12,176 | 16,657 | 708 | 14,270 | 9967 | 125 | 1268 | 27,569 |
| Open | 23,760 (82.4) | 32 (19) | 10,979 (90.2) | 12,778 (76.7) | 627 (88.6) | 11,592 (81.2) | 8415 (84.4) | 89 (71.2) | 1092 (86.1) | 22,668 (82.2) |
| Laparoscopic | 5077 (17.6) | 37 (16) | 1197 (9.8) | 3879 (23.3) | 81 (11.4) | 2678 (18.8) | 1552 (15.6) | 36 (28.8) | 176 (13.9) | 4901 (17.8) |
| Cholecystectomy | 12,290 | 40 (15) | 2309 | 9980 | 298 | 6053 | 4351 | 66 | 538 | 11,752 |
| Open | 7992 (65) | 40 (15) | 1507 (65.3) | 6485 (65) | 230 (77.2) | 3728 (61.6) | 3126 (71.9) | 32 (48.5) | 390 (72.5) | 7602 (64.7) |
| Laparoscopic | 4298 (35) | 39 (15) | 802 (34.7) | 3495 (35) | 68 (22.8) | 2325 (38.4) | 1225 (28.1) | 34 (51.5) | 148 (27.5) | 4150 (35.3) |
| Appendectomy | 12,687 | 23 (16) | 6844 | 5841 | 284 | 6253 | 4341 | 37 | 538 | 12,149 |
| Open | 11,972 (94.4) | 23 (16) | 6503 (95) | 5467 (93.6) | — | 5943 (95) | 4030 (92.8) | 35 (94.6) | 510 (94.8) | 11,462 (94.4) |
| Laparoscopic | 715 (5.6) | 26 (17) | 341 (5) | 374 (6.4) | — | 310 (5) | 311 (7.2) | 2 (5.4) | 28 (5.2) | 687 (5.6) |
| Inguinal hernia repair | 3860 | 45 (22) | 3023 | 836 | 126 | 1964 | 1275 | 22 | 192 | 3668 |
| Open | 3796 (98.3) | 45 (22) | 2969 (98.2) | — | — | 1921 (97.8) | 1259 (98.8) | 22 (100) | 192 (100) | 3604 (98.3) |
| Laparoscopic | 64 (1.7) | 51 (15) | 54 (1.8) | — | — | 43 (2.2) | 16 (1.2) | 0 | 0 (0) | 64 (1.7) |
Percentages have been approximated to one decimal place and may not sum up to 100%.
Cells containing less than or equal to 10 patients were hidden to ensure privacy protection and confidentiality.
Univariable analysis
The outputs of the univariable analysis are shown in Table 5. Geographical characteristics positively associated with laparoscopic procedures were increasing municipalities’ population density (OR 1.48, 95% CI 1.44–1.51) and operating in urban areas (OR 1.34, 95% CI 1.14–1.58, compared to rural areas). Conversely, the central (OR 0.86, 95% CI 0.81–0.90) and southeast regions (OR 0.79, 95% CI 0.77–0.81) had a negative association with the outcome of a procedure being laparoscopic, using the northwest region as reference.
Table 5.
Univariable analysis for use of laparoscopic technique according to procedures registered in Egresos Hospitalarios 2021.
| Variable | ORa | 95% CIa | P-value |
|---|---|---|---|
| Age | 1.012 | 1.010, 1.013 | <0.001 |
| Sex | |||
| Male | — | — | |
| Female | 2.784 | 2.597, 2.985 | <0.001 |
| Indigenous ethnicity | |||
| Yes | 0.598 | 0.473, 0.755 | <0.001 |
| No | — | — | |
| Insurance | |||
| Yes | 0.811 | 0.760, 0.865 | <0.001 |
| No | — | — | |
| Procedure type | |||
| Cholecystectomy | — | — | |
| Appendectomy | 0.111 | 0.102, 0.120 | <0.001 |
| Hernia inguinal repair | 0.177 | 0.156, 0.200 | <0.001 |
| Rural vs Urban | |||
| Rural | — | — | |
| Urban | 1.341 | 1.140, 1.577 | <0.001 |
| Region | |||
| Northwest | — | — | |
| Northeast | 0.995 | 0.876, 1.130 | 0.940 |
| Central | 0.856 | 0.812, 0.903 | <0.001 |
| West | 0.987 | 0.951, 1.024 | 0.501 |
| Southeast | 0.791 | 0.767, 0.815 | <0.001 |
| Anesthesia technique | |||
| General | — | — | |
| Regional | 0.196 | 0.182, 0.209 | <0.001 |
| Local | 0.902 | 0.809, 1.007 | 0.067 |
| Combined | 0.703 | 0.667, 0.741 | <0.001 |
| Municipality population | 1.475 | 1.436, 1.514 | <0.001 |
Caption: For the univariable model, we used the binary variable (if the procedure was laparoscopic or open) as the dependent variable. The glm() function from R software was used to run all univariable logistic regression models. P-values <0.05 in bold indicates statistically significant values.
OR = Odds Ratio, 95% Confidence Intervals (95% CI).
Regarding clinical factors, laparoscopic procedures had a negative association with appendectomies (OR 0.11, 95% CI 0.1–0.12) and inguinal hernia repair (OR 0.18, 95% CI 0.16–0.20) in comparison to cholecystectomies; and application of regional (OR 0.2, 95% CI 0.18–0.21) and combined anaesthesia (OR 0.7, 95% CI 0.67–0.74) in relation to general anaesthesia.
Demographic factors that presented a positive association with laparoscopic procedures were age (OR 1.01, 95% CI 1.010–1.013), being female (OR 2.78, 95% CI 2.6–3.0), and not reporting Indigenous ethnicity (OR 0.6, 95% CI 0.48–0.75). Additionally, patients with government-provided insurance were negatively associated with the performance of laparoscopic procedures (OR 0.81, 95% CI 0.76–0.86).
Multivariable analysis
On the multivariable analysis (Table 6), the geographical characteristics that remained positively associated with laparoscopic procedures were the municipalities’ population density (OR 1.36, 95% CI 1.32–1.40); and whether surgeries were conducted in urban areas (OR 1.3, 95% CI 1.06–1.61). Furthermore, the southeast was negatively associated with laparoscopic operations (OR 0.48, 95% CI 0.41–0.55) while the northeast (OR 1.37, 95% CI 1.17–1.6) and west (OR 1.56, 95% CI 1.35–1.8) were positively associated.
Table 6.
Multivariable analysis for use of laparoscopic technique according to procedures registered in Egresos Hospitalarios 2021.
| Variable | ORa | 95% CIa | P-value |
|---|---|---|---|
| Age | 1.001 | 0.999, 1.003 | 0.404 |
| Sex | |||
| Male | — | — | |
| Female | 1.262 | 1.154, 1.380 | <0.001 |
| Indigenous ethnicity | |||
| Yes | 1.695 | 1.288, 2.206 | <0.001 |
| No | — | — | |
| Insurance | |||
| Yes | 0.883 | 0.811, 0.960 | 0.004 |
| No | — | — | |
| Procedure type | |||
| Cholecystectomy | — | — | |
| Appendectomy | 0.105 | 0.095, 0.117 | <0.001 |
| Hernia inguinal repair | 0.036 | 0.027, 0.047 | <0.001 |
| Rural vs Urban | |||
| Rural | — | — | |
| Urban | 1.301 | 1.060, 1.605 | 0.013 |
| Region | |||
| Northwest | — | — | |
| Northeast | 1.370 | 1.174, 1.599 | <0.001 |
| Central | 0.994 | 0.868, 1.140 | 0.933 |
| West | 1.563 | 1.355, 1.805 | <0.001 |
| Southeast | 0.477 | 0.412, 0.554 | <0.001 |
| Anesthesia technique | |||
| General | — | — | |
| Regional | 0.225 | 0.208, 0.244 | <0.001 |
| Local | 1.095 | 0.737, 1.610 | 0.648 |
| Combined | 0.253 | 0.200, 0.317 | <0.001 |
| Municipality Population | 1.360 | 1.317, 1.404 | <0.001 |
| Goodness-of-fit: McFadden's R2 | 0.29 |
Caption: For the multivariable model, we used the binary variable (if the procedure was laparoscopic or open) as the dependent variable. The glm() function from R software was used to run the multivariable logistic regression models. The multivariable model was developed based on all the variables used in the univariable models. We did not use any threshold value in P-values for each of the variables of the univariable models to be included in the multivariable model. P-values <0.05 in bold indicates statistically significant values.
Goodness-of-fit: McFadden's R2 = 0.29. Hosmer–Lemeshow Good of Fit Test: Chi-squared = 92.147, df = 8, P-value <0.001.
OR = Odds Ratio, 95% Confidence Intervals (95% CI).
In regard to clinical factors, laparoscopic technique remained negatively associated with appendectomies (OR 0.1, 95% CI 0.09–0.12) and inguinal hernia repair (OR 0.04, 95% CI 0.03–0.05) when compared to cholecystectomies. Additionally, the laparoscopic approach had a negative association with regional (OR 0.22, 95% CI 0.21–0.24) and combined anaesthesia (OR 0.25, 95% CI 0.20–0.32) compared to general anaesthesia.
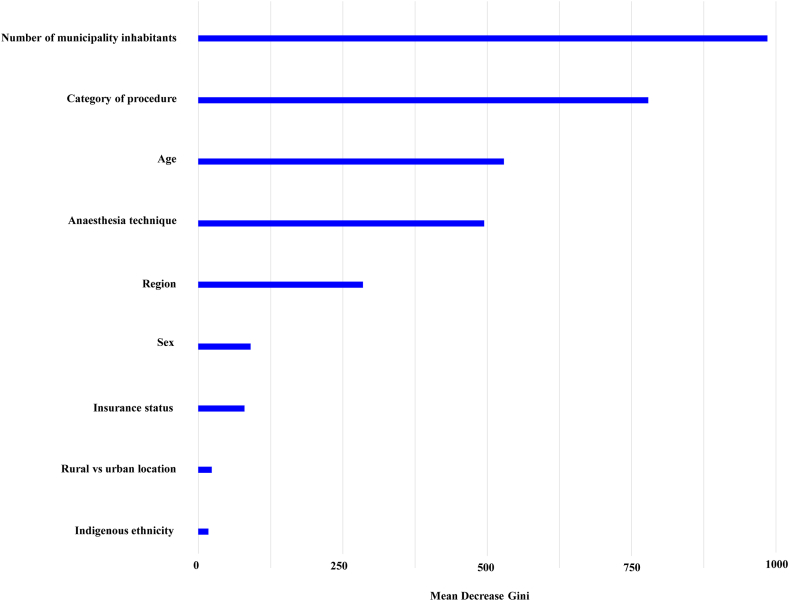
Finally, female sex (OR 1.26, 95% CI 1.15–1.38, as opposed to male) and being covered by government-provided insurance (OR 0.88, 95% CI 0.81–0.96) held a positive and negative association with laparoscopic technique, respectively. Moreover, reporting Indigenous ethnicity (OR 1.69, OR 1.29–2.21) was positively associated with adoption of the laparoscopic approach. Age was found to be a non-significant factor (OR 1.002, 95% CI 1.000–1.004). The contributions of each variable in the multivariable analysis are represented in Fig. 4. Further information on the random forest implementation and results can be found in Supplementary Material S3.
Fig. 4.
Variable Importance Plot to assess importance of each of the variables in the Random Forest Model. Outputs of the random forest model, ranking each variable in terms of importance to the multivariable model. Mean Decrease Gini is a measure of variable importance based on the Gini impurity index.
Discussion
Although minimally invasive surgery is the approach of choice for many surgical conditions in HICs, such services are limited in LMICs.1,2,8 By considering three common procedures as proxies, our study reports on the prevalence of laparoscopic procedures in Mexico's public health system, corresponding to only 16.5% of analysed surgeries. We found that laparoscopic procedures prevailed in highly populated urban municipalities and in the wealthier northwest region, with a high concentration of surgeons and anaesthesiologists. Most importantly, our study provides insights into the geographic, demographic, and clinical factors influencing access to laparoscopic procedures in Mexico. We identified that factors that determined the use of laparoscopy were more related to the conditions of the localities where procedures occurred than the patients' non-modifiable characteristics. These results show that assertive policymaking at the regional, state, and municipal levels could significantly improve access to minimally invasive surgery in Mexico.
In our study, the volume of laparoscopic procedures was significantly associated with population density and regional characteristics. The central region, the most populated area in Mexico and where the country's capital is located, had the highest number of laparoscopic procedures.13 Such a result reflects the trends concerning the distribution of minimally invasive procedures in Mexico. Until 2012, more than 30% of all minimally invasive procedures were performed in the capital, which concentrated 39.8% of the country's surgical productivity at that time.17 In accordance, the states of Ciudad de México and Estado de México performed the highest number of laparoscopic procedures across the country in 2015.18 Interestingly, the northwest, the least populated region, had the largest proportion of laparoscopic procedures performed. However, as the northwest has three of its five states amongst the highest GDP per capita holders, this finding demonstrates the need to contextualise the socioeconomic background of the population.13
Besides outlining regional disparities, we demonstrated that resource-allocation barriers can influence the availability of laparoscopic surgery. In our study, only 4.5% of hospitals that performed laparoscopic procedures were based in rural areas. Furthermore, the proportion of laparoscopic procedures decreased in regions where the median for surgeons and anaesthesiologists per hospital was low. In Mexico, less populated settings are associated with being rural, economically dependent on agriculture, and scarce in basic public services, including medical, sanitary, and hygiene services.19 While analysing the economic implications of our findings exceeds the scope of this study, minimally invasive surgery can play a relevant role in low-resource settings, as these are most vulnerable to catastrophic health expenditure and may benefit from the lower morbidity associated with a laparoscopic approach.3,6, 7, 8 By extending the evidence base on the availability of laparoscopic procedures, our study highlights the need to expand access to these surgeries through investments in infrastructure and personnel.
We observed that a greater number of female patients underwent a laparoscopic procedure than male patients. This could be attributed to the characteristics of our sample, as cholecystectomies were the most common procedure performed laparoscopically and gallbladder pathologies are more prevalent among women.20 In addition, our finding is corroborated by a similar study that utilised national data from 2015 and identified that 79% of the patients who underwent laparoscopic procedures in Mexico's public hospitals were female.18 Whereas multiple studies have shown a higher prevalence of gallbladder disease in female patients, men frequently present with complicated cholecystitis. Factors such as higher rates of severe fibrosis, anatomical anomalies, and the need for more experienced laparoscopic operative teams may contribute to a general preference for open surgery in male patients.20,21 Nonetheless, the lower proportion of procedures in men may suggest the necessity for laparoscopic training programs to strengthen practice regarding advanced and complicated procedures within operative teams, which can be enhanced through simulations, exchange programs, telemedicine, and intraoperative practice.8
In early 2020, Mexico achieved universal health coverage through the Institute of Health for Well-being (INSABI). Under the new legislation, the former insurance registration system was entirely abandoned, and all one needed to receive medical care through INSABI was proof of Mexican citizenship.22 Thus, we found that most patients undergoing surgical procedures in the public health system had either registered for federal government insurance (34.5%) or had not (49.4%) and were covered by INSABI. Nonetheless, those without registered insurance receive services from a system considered second-tier in terms of quality and where tertiary-care hospitals are less accessible.23 In our study, only patients with had employment-based insurance were more likely to undergo laparoscopic procedures (51.5%). The laparoscopic approach was less commonly used for all other insurance status across all procedure categories. Employment-based insurance is associated with a higher patient socioeconomic status, compared to government insurance, often indicative of poverty. These patients may reside in wealthier areas, proximal to better-equipped public hospitals and be more likely to defray associated out-of-pocket expenses.24, 25, 26
Despite the implementation of universal health coverage, only 1.6% of laparoscopic procedures were performed in Indigenous patients, and the technique was less commonly used in this population across all procedure categories. However, in contrast to the available literature, our multivariable analysis evidenced that reporting Indigenous ethnicity was paradoxically positively associated with adoption of the laparoscopic approach (OR 1.69, OR 1.29–2.21). While racial disparities in access to minimally invasive surgery have not been analysed in LMICs, studies in HICs demonstrate that racially minoritised patients are less likely to receive laparoscopic operations than an open surgical approach.27,28
Concerning the adoption of a laparoscopic technique across the three procedure categories, we observed the highest and lowest prevalence in cholecystectomies (49 per 100,000 inhabitants) and inguinal hernia repairs (15 per 100,000 inhabitants). While the expansion of laparoscopic operative care of gallbladder disease in LMICs has resulted in shorter recovery time and hospital stay, reduced wound infection rate, and lower overall costs, even in HICs, the initial enthusiasm for laparoscopic inguinal hernia repairs has been challenged by similar surgical outcomes, lower costs, and a shorter learning curve associated with the open approach.29,30 This study was not able to explore these associations.
Our results showed that general anaesthesia was the most common technique among laparoscopic procedures. Because awake patients generally do not tolerate pneumoperitoneum well, laparoscopic procedures are standardly performed under general anaesthesia.31 Interestingly, 27.9% of included laparoscopic procedures were conducted under regional anaesthesia. Usually, this technique has been limited to patients at high risk for general anaesthesia and, in HICs, its use remains controversial for patients without severe comorbidities.32,33 Due to its greater affordability, cost-effectiveness, and safety, regional anaesthesia has been more commonly observed in low-resource settings to perform laparoscopic operations.34 Yet, further research is needed to demonstrate if conducting laparoscopic procedures under regional anaesthesia generates equal or improved patient outcomes in comparison to the administration of general anaesthesia. Additionally, the plan of anaesthesia technique is associated with but does not necessarily factor in the surgical approach decision-making. The direction of this relationship may be opposite, as the type of anaesthesia could be decided based on the hospital's anaesthesia capacity, as well as the planned surgical approach.
Given the generated findings, our study outlines some takeaways policymakers should consider to improve access to laparoscopic procedures in Mexico. We demonstrated that operations that underwent a laparoscopic approach were most prevalent in urban municipalities and the country's northern regions. These findings highlight the potential need to incorporate required equipment and infrastructure in health facilities and geographically decentralise where laparoscopic procedures take place. However, as previously reported in the literature, the lack of financial resources often constitutes a main barrier to implementing laparoscopic machines.35 Hence, policymakers should consider partnerships and business models that reduce costs and optimise laparoscopic equipment's cost-effectiveness.35,36 Accordingly, providing adequate training for surgeons is fundamental to increasing the number of laparoscopic procedures. Suitable educational options include implementing institutional partnerships, sponsoring fellowships, and structuring training programs at the local, regional, and national levels.36
Limitations
This study is not without limitations. We analysed data from the hospitals from the Mexican Ministry of Health, the Secretaria de Salud, and did not include other public health sector hospitals namely the Mexican Institute of Social Security (Instituto Mexicano del Seguro Social, IMSS) and the Institute of Security and Social Service of State Workers (Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado, ISSSTE). We also did not include laparoscopic procedures in private hospitals, where we expect a higher prevalence. Additionally, private hospitals may exhibit a stronger association between patient insurance status and the use of laparoscopic techniques due to potential financial incentives and differential access to technological resources that may be more standardised and regulated by government policies in public hospitals. As we utilised secondary data sources, limitations regarding data entry quality were present, such as missing or incomplete data. Due to data availability, we could only track and analyse demographic and clinical variables for a sample of the procedures. We also lacked information on other factors that could have influenced the observed differences between the prevalences of laparoscopic and open procedures. These include the availability of and access to laparoscopic equipment and the surgeon's preference for a given approach and degree of training in laparoscopic techniques. Additionally, we used a 2021 dataset as this was the most recent complete year from which we could retrieve information. We had to complement it with 2020 geographic information, as this was the year when the latest Mexican National Census was held. While analysing previous years exceeds the scope of our present work, a study using 2015 data from Egresos Hospitalarios reported higher volumes of laparoscopic procedures compared to our findings.18 We recognize that data from 2021 may have been affected by the COVID-19 pandemic. Lastly, our results are based on a single country and may not be generalisable. In spite of these limitations, our study illustrates access to minimally invasive surgery at a national level in a large country with broad socioeconomic disparities that might be similar to other LMICs, especially in Latin America.
Conclusion
Despite the benefits of minimally invasive surgery, our findings suggest that the open technique remains the most common surgical approach in the Mexican public health system. Laparoscopic procedures are more commonly performed in highly populated, urban, and wealthy northern areas, accounting for higher numbers of anaesthesiologists and surgeons per hospital. Due to disparities in resource provision across Mexico, access to laparoscopic techniques is mostly influenced by the conditions of the settings where procedures are performed, such as the number of municipality inhabitants, rather than patients' non-modifiable characteristics, such as sex and Indigenous ethnicity. These findings call for tailored, multilevel interventions to address equitable access to minimally invasive surgery in Mexico sustainably.
Contributors
MBA and TUL conceived the study. MBA, LNC, and TUL coordinated the study, acquired and verified the data. MBA, LNC, and TUL designed the study. MBA and LNC prepared the figures and tables. MBA and LNC wrote the first draft report. MBA, LNC, and TD contributed to the analysis. MBA, LNC, TD, DDV, SKH, MZ, AV, SJ, GAA, and TUL contributed to the interpretation. MBA, LNC, DDV, SKH, MZ, AV, SJ, GAA, and TU edited the report. All authors critically reviewed the paper, approved the final version, and decided to submit the manuscript.
Data sharing statement
All data used in these analyses are publicly available from the Mexican National Ministry of Health and the Mexican Institute of Statistics and Geography.
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
None.
Acknowledgements
The authors would like to acknowledge the following sources of funding that are supporting their academic endeavours: Fundação Maria Emília Pedreira Feire de Carvalho (LNC), Fundação Estudar (LNC), the Swedish Research Council Grant 2022–00208 (MZ), the Swedish governmental funding of clinical research (ALF YF00054-MZ) and the Swedish Doctor's Association (SLS-971600-MZ). These institutions played no role in the conceptualization, design, data collection, data analysis, and writing of the manuscript.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lana.2023.100556.
Appendix A. Supplementary data
Supplementary Material
References
- 1.Varela J.E., Nguyen N.T. Disparities in access to basic laparoscopic surgery at U.S. academic medical centers. Surg Endosc. 2011;25(4):1209–1214. doi: 10.1007/s00464-010-1345-y. [DOI] [PubMed] [Google Scholar]
- 2.Wood K.L., Haider S.F., Bui A., Leitman I.M. Access to common laparoscopic general surgical procedures: do racial disparities exist? Surg Endosc. 2020;34(3):1376–1386. doi: 10.1007/s00464-019-06912-w. [DOI] [PubMed] [Google Scholar]
- 3.Rosenbaum A.J., Maine R.G. Improving access to laparoscopy in low-resource settings. Ann Glob Health. 2019;85(1):114. doi: 10.5334/aogh.2573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Price R., Sergelen O., Unursaikhan C. Improving surgical care in Mongolia: a model for sustainable development. World J Surg. 2013;37(7):1492–1499. doi: 10.1007/s00268-012-1763-1. [DOI] [PubMed] [Google Scholar]
- 5.Tatebe L.C., Gray R., Tatebe K., Garcia F., Putty B. Socioeconomic factors and parity of access to robotic surgery in a county health system. J Robot Surg. 2018;12(1):35–41. doi: 10.1007/s11701-017-0683-3. [DOI] [PubMed] [Google Scholar]
- 6.Wilkinson E., Aruparayil N., Gnanaraj J., Brown J., Jayne D. Barriers to training in laparoscopic surgery in low- and middle-income countries: a systematic review. Trop Doct. 2021;51(3):408–414. doi: 10.1177/0049475521998186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mishra A., Bains L., Jesudin G., Aruparayil N., Singh R., Shashi Evaluation of gasless laparoscopy as a tool for minimal access surgery in low-to middle-income countries: a phase II noninferiority randomized controlled study. J Am Coll Surg. 2020;231(5):511–519. doi: 10.1016/j.jamcollsurg.2020.07.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chao T.E., Mandigo M., Opoku-Anane J., Maine R. Systematic review of laparoscopic surgery in low- and middle-income countries: benefits, challenges, and strategies. Surg Endosc. 2016;30(1):1–10. doi: 10.1007/s00464-015-4201-2. [DOI] [PubMed] [Google Scholar]
- 9.The World Inequality Report 2022 presents the most up-to-date & complete data on inequality worldwide. https://wir2022.wid.world/ [cited 2023 Jan 22]. Available from:
- 10.von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 11.SINBA cubos dinámicos. http://sinaiscap.salud.gob.mx:8080/DGIS/ [cited 2022 Oct 20]. Available from:
- 12.Roa L., Moeller E., Fowler Z., et al. Assessment of diagnostics capacity in hospitals providing surgical care in two Latin American states. eClinicalMedicine. 2020;29–30 doi: 10.1016/j.eclinm.2020.100620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Census of population and housing. 2020. https://en.www.inegi.org.mx/programas/ccpv/2020/ [cited 2023 Jan 22]. Available from: [Google Scholar]
- 14.Secin F.P., Coelho R., Monzó Gardiner J.I., et al. Robotic surgery in public hospitals of Latin-America: a castle of sand? World J Urol. 2018;36(4):595–601. doi: 10.1007/s00345-018-2227-5. [DOI] [PubMed] [Google Scholar]
- 15.NORMA Oficial Mexicana NOM-006-SSA3-2011, Para la práctica de la anestesiología. https://www.dof.gob.mx/normasOficiales/4677/SALUD/SALUD.htm [cited 2023 Apr 18]. Available from:
- 16.Requirements for publishing with HCUP data. https://www.hcup-us.ahrq.gov/db/publishing.jsp [cited 2023 Jan 29]. Available from:
- 17.Guerrero-Aguirre J., Ortiz-Barrón S., Castillo-Arriaga R., Salazar-Lozano C. La cirugía de invasión mínima: antecedente histórico; presente y perspectivas futuras en el ISSSTE. Rev Espec Méd-Quirúrgicas. 2014;19(3):375–386. [Google Scholar]
- 18.Chávez-Saavedra G., Lara-Lona E., Hidalgo-Valadez C., Romero-Salinas N., Méndez-Sashida G.J. Experiencia en procedimientos laparoscópicos en México durante 2015: ¿dónde estamos? Cir Cir. 2019;87(3) doi: 10.24875/CIRU.18000562. https://www.cirugiaycirujanos.com/frame_esp.php?id=143 [cited 2023 Apr 18] Available from: [DOI] [PubMed] [Google Scholar]
- 19.MacGregor G., Teresa M. Desarrollo y distribución de la población urbana en México. Investig Geogr. 2003;(50):77–91. [Google Scholar]
- 20.Shilling Bailey K., Marsh W., Daughtery L., Hobbs G., Borgstrom D. Gender disparities in the presentation of gallbladder disease. Am Surg. 2019;85(8):830–833. [PubMed] [Google Scholar]
- 21.Akcakaya A., Okan I., Bas G., Sahin G., Sahin M. Does the difficulty of laparoscopic cholecystectomy differ between genders? Indian J Surg. 2015;77(S2):452–456. doi: 10.1007/s12262-013-0872-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ramos-De la Medina A., Torres-Cisneros J.R. La cirugía como problema de salud pública en México y el concepto de cirugía global. Cir Gen. 2020;42(1):57–60. [Google Scholar]
- 23.Vazquez-Narvaez K.G., Garcia-Campos D.E. Perioperative medicine in Mexico. Int Anesthesiol Clin. 2022;60(1):80–83. doi: 10.1097/AIA.0000000000000345. [DOI] [PubMed] [Google Scholar]
- 24.Mehta R., Sahara K., Merath K., et al. Insurance coverage type impacts hospitalization patterns among patients with hepatopancreatic malignancies. J Gastrointest Surg. 2020;24(6):1320–1329. doi: 10.1007/s11605-019-04288-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gutiérrez J.P., Heredia-Pi I., Hernández-Serrato M.I., Pelcastre-Villafuerte B.E., Torres-Pereda P., Reyes-Morales H. Desigualdades en el acceso a servicios, base de las políticas para la reducción de la brecha en salud. Salud Publica Mex. 2019;61(6):726. doi: 10.21149/10561. [DOI] [PubMed] [Google Scholar]
- 26.Ratnapradipa K.L., Lian M., Jeffe D.B., et al. Patient, hospital, and geographic disparities in laparoscopic surgery use among surveillance, Epidemiology, and end results–medicare patients with colon cancer. Dis Colon Rectum. 2017;60(9):905–913. doi: 10.1097/DCR.0000000000000874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ranjit A., Chaudhary M.A., Jiang W., et al. Disparities in receipt of a laparoscopic operation for ectopic pregnancy among TRICARE beneficiaries. Surgery. 2017;161(5):1341–1347. doi: 10.1016/j.surg.2016.09.029. [DOI] [PubMed] [Google Scholar]
- 28.Ranjit A., Sharma M., Romano A., et al. Does universal insurance mitigate racial differences in minimally invasive hysterectomy? J Minim Invasive Gynecol. 2017;24(5):790–796. doi: 10.1016/j.jmig.2017.03.016. [DOI] [PubMed] [Google Scholar]
- 29.Wells K.M., Lee Y.J., Erdene S., et al. Expansion of laparoscopic cholecystectomy in a resource limited setting, Mongolia: a 9-year cross-sectional retrospective review. Lancet. 2015;385(Suppl 2):S38. doi: 10.1016/S0140-6736(15)60833-9. [DOI] [PubMed] [Google Scholar]
- 30.Haladu N., Alabi A., Brazzelli M., et al. Open versus laparoscopic repair of inguinal hernia: an overview of systematic reviews of randomised controlled trials. Surg Endosc. 2022;36(7):4685–4700. doi: 10.1007/s00464-022-09161-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vretzakis G., Bareka M., Aretha D., Karanikolas M. Regional anesthesia for laparoscopic surgery: a narrative review. J Anesth. 2014;28(3):429–446. doi: 10.1007/s00540-013-1736-z. [DOI] [PubMed] [Google Scholar]
- 32.Sinha R., Gurwara A.K., Gupta S.C. Laparoscopic cholecystectomy under spinal anesthesia: a study of 3492 patients. J Laparoendosc Adv Surg Tech A. 2009;19(3):323–327. doi: 10.1089/lap.2008.0393. [DOI] [PubMed] [Google Scholar]
- 33.Sinha R., Gurwara A.K., Gupta S.C. Laparoscopic surgery using spinal anesthesia. JSLS. 2008;12(2):133–138. [PMC free article] [PubMed] [Google Scholar]
- 34.Bajwa S.S., Kulshrestha A. Anaesthesia for laparoscopic surgery: general vs regional anaesthesia. J Minim Access Surg. 2016;12(1):4. doi: 10.4103/0972-9941.169952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schwartz M., Jeng C.J., Chuang L.T. Laparoscopic surgery for gynecologic cancer in low- and middle-income countries (LMICs): an area of need. Gynecol Oncol Rep. 2017;20:100–102. doi: 10.1016/j.gore.2017.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zadey S., Mueller J., Fitzgerald T.N. Improving access to laparoscopic surgery in low- and middle-income countries. JAMA Surg. 2022;157(9):844. doi: 10.1001/jamasurg.2022.2675. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material