Abstract
While care transitions influence quality of care, less work studies transitions between hospital units. We studied care transitions from the operating room (OR) to pediatric and adult intensive critical care units (ICU) using Systems Engineering Initiative for Patient Safety (SEIPS)-based process modeling. We interviewed twenty-nine physicians (surgery, anesthesia, pediatric critical care) and nurses (OR, ICU) and administered the AHRQ Hospital Survey on Patient Safety Culture items about handoffs, care transitions and teamwork. Care transitions are complex, spatio-temporal processes and involve work during the transition (i.e., handoff and transport) and preparation and follow up activities (i.e., articulation work). Physicians defined the transition as starting earlier and ending later than nurses. Clinicians in the OR to adult ICU transition without a team handoff reported significantly less information loss and better cooperation, despite positive interview data. A team handoff and supporting articulation work should increase awareness, improving quality and safety of care transitions.
Keywords: Process mapping, Care transition, Communication and coordination
1. INTRODUCTION
The publication of landmark reports, such as “Crossing the Quality Chasm: A New Health System for the 21st Century” (Institute of Medicine, 2001), brought attention to quality in health care. Handoff communication (i.e., the transfer of information, authority and responsibility for patient care, Abraham et al., 2014) is necessary to ensure safe, high quality care. Handoffs provide opportunities to detect and correct errors (Perry, 2004), but risk information loss, delays and decreased effectiveness/efficiency (Arora et al., 2009). Despite the 2006 National Patient Safety Goal by the Joint Commission to improve handoff communication, between 2009–2013 7149 instances of patient harm, including 1744 deaths, were attributed to communication failures (CRICO Strategies, 2015).
Some work has focused on improving care transitions with technology, particularly transitions between facilities (Marcotte et al., 2015) and across shifts (Arora et al., 2009). Less work has focused on transitions between different hospital inpatient units, i.e., intrahospital care transitions. We use care transition to include transport, handoff and other activities necessary to ensure the patients’ physical transition, with handoff referring to communication for exchanging information.
1.1. Intrahospital care transitions
Published research on intrahospital care transitions has focused on information to communicate, developing mnemonics and checklists to ensure information transfer during handoffs (Abraham et al., 2017). These transitions include transitions between physical locations and organizational units – signifying changes in care team, equipment, support staff, technology and work environment – and can be conceptualized as processes, i.e., “set[s] of interrelated or interacting activities…to deliver an intended result” (ISO, 2015), including important work outside of transport and handoff (Aase & Waring, 2020). Research with this conceptualization has focused on the operating room (OR) to intensive care unit (ICU) care transitions and provides a broader insight on how transitions occur. For example, in a failure modes and effects analysis, McElroy and colleagues (2015) observed and described the process of OR-to-ICU care transitions, identifying 37 major steps in the process; these steps were grouped into five basic steps:
Operation concludes;
OR preparation;
ICU preparation;
Physical transfer and settling;
Handoff communication and team disperses.
Other researchers have re-designed the OR to pediatric ICU (PICU) care transition of pediatric cardiac surgery patients (Agarwal et al., 2012; Catchpole et al., 2007; Craig et al., 2012). The redesigned processes began while the patient was in the OR when information was sent to the PICU, triggering preparation in both units before transport; the patient was stabilized in the PICU before an inter-professional handoff, with discussion of plans and questions. The redesigned processes improved:
Information flow (Agarwal et al., 2012; Catchpole et al., 2007; Craig et al., 2012)
Attentiveness and interruptions (Catchpole et al., 2007; Craig et al., 2012)
Errors (Catchpole et al., 2007)
Four clinical outcomes: cardiopulmonary resuscitation, placement on extracorporeal membrane oxygenation, need for mediastinal reexploration, and development of severe metabolic acidosis (Agarwal et al., 2012).
The redesigned processes use information on existing research and workshops with stakeholders (Craig et al., 2012), lessons from motorcar racing and aviation (Catchpole et al., 2007) and feedback from handoff participants (Agarwal et al., 2012). However, the studies did not describe the care transition process before the redesign nor how those practices were considered in the redesign. Lane-Fall and colleagues (2018; Ross Perfetti et al., 2020) conducted interviews and focus groups with clinicians participating in OR-to-ICU transitions to identify barriers and supporting factors. They identified barriers including time pressure, unclear expectations and lack of understanding of the information needs of others; the supporting factors included pre-notification of patient arrival to ICU team, presence of extra nurses upon patient arrival and predictable handoff format, in the existing care transition process. They combined this analysis with published literature to develop a standardized process for OR-to-ICU care transitions, with findings indicating improvements in teamwork and information transfer (Lane-Fall et al., 2016; Lane-Fall et al., 2020). Nonetheless, they too did not describe or analyze the existing process in detail, although their recent protocol does call for in-depth process analysis prior to implementing their tool (Lane-Fall et al., 2021). Their subsequent work has focused on interprofessional communication training (Massa et al., 2021), which – while important – may inadvertently increase workload of clinicians and contribute to the ongoing epidemic of clinician burnout (National Academies of Sciences, 2019).
1.2. Process mapping: integrating quality improvement science and human factors/ergonomics
Hignett and colleagues (2015) argue that the integration of quality improvement science (QIS) and human factors and ergonomics (HFE) is key to improving quality of care. Fundamentally, although defined in various ways, QIS is a set of strategies to increase quality, such as Plan-Do-Study-Act, Total Quality Improvement, Lean and Six Sigma. HFE is “the scientific discipline concerned with the understanding of interactions among humans and other elements of a system, and the profession that applies theory, principles, data and methods to design in order to optimize human well-being and overall system performance” (International Ergonomics Association (IEA), 2020). Both HFE and QSI identify a required change, apply various methods to describe the current situation and develop an intervention, which is implemented and evaluated before the cycle repeats (Hignett et al., 2015). We believe the overlap goes beyond the similarities identified by Hignett and colleagues (2015). For instance, process mapping is one of the strategies used in QIS, which also has a rich history in HFE (Huang & Gramopadhye, 2014; Jun et al., 2010; Lane et al., 2006; Siemieniuch & Sinclair, 2015; Wooldridge et al., 2017). Clearly understanding the current work situation, i.e., work system, before developing and implementing any interventions aimed to improve outcomes is necessary (Daniellou, 2005). Further, it is important to understand the work as it is done, not just as is prescribed or imagined by management (Hollnagel et al., 2015; Leplat, 1989). Process mapping approaches are one way to do this and are useful in identifying risks from various sources (Simsekler et al., 2018), a key element of quality improvement.
We have previously described the Systems Engineering Initiative for Patient Safety (SEIPS)-based process modeling method to clearly understand the work system and process. We demonstrated the application of SEIPS-based process modeling to three processes in primary care: previsit planning, patient outreach for panel management and checkout (Carayon & Wooldridge, 2020; Wooldridge et al., 2017). The SEIPS-based process modeling method builds on HFE tools for process modeling, incorporates sociotechnical system theory and represents all six work system elements: people, tasks, technologies, organization, physical environment and external environment (Carayon et al., 2006; Carayon et al., 2014; Carayon et al., 2020). The six work system elements and interactions between them must be addressed together, as they dictate how the process occurs and are key to designing new processes that result in improved outcomes for both patients and healthcare professionals (Berg, 1999).
SEIPS-based process maps are similar to swim-lane diagrams and flowcharts: columns represent physical locations and organizational units, while rows represent temporality (Carayon & Wooldridge, 2020; Wooldridge et al., 2017). Major steps are shown in boxes located in the cells created by the rows and columns; details about who performs tasks with what technologies are in those boxes. The process models can be used to describe processes to increase awareness in stakeholders (Schultz et al., 2007) and can be used to evaluate processes to identify opportunities for improvement (Wetterneck et al., 2006; Wooldridge et al., 2020).
1.3. Objective
In this study, we identify activities in the OR-to-PICU and OR-to-ICU care transitions associated with preparation, handoff and follow up activities using SEIPS-based process maps, comparing and contrasting the two processes. We explore process scope (i.e., beginning and end) from the perspective of the healthcare professionals involved in the care transitions. We focus on pediatric and adult trauma patients as trauma is the leading cause of death among children and adults aged one to 44 years old (Stewart et al., 2003). These patients are typically critical and unstable, and care transitions occur with additional time pressure and uncertainty due to the nature of trauma, increasing the complexity of the system and process (Wooldridge, Carayon, Hoonakker, et al., 2018).
2. METHODS
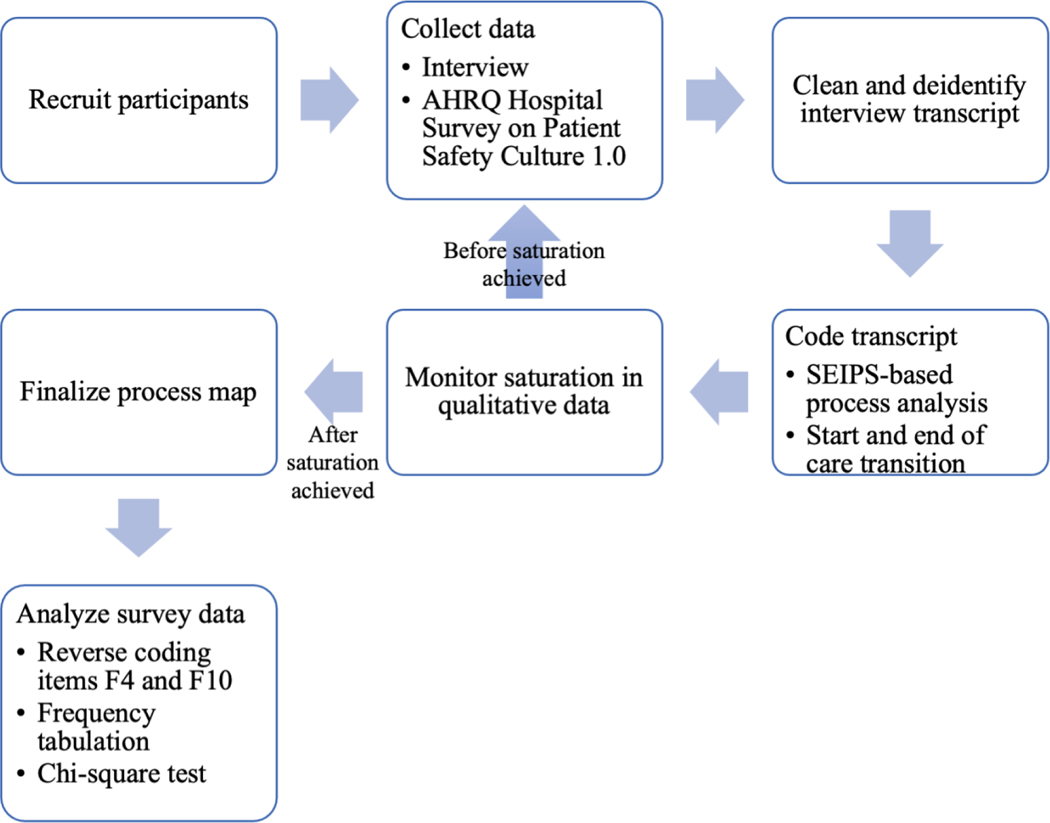
This study is part of a larger study on health information technology (IT) for teamwork and care transitions in pediatric trauma care (http://cqpi.wisc.edu/teamwork-and-care-transitions-in-pediatric-trauma/). Approval for this study was obtained from the IRB at the University of Wisconsin-Madison; approval for secondary data analysis was obtained from the IRB at the University of Illinois at Urbana-Champaign. Figure 1 provides an overview of the study methods.
Figure 1.
Flowchart of study methodology.
2.1. Setting and sample
This study was conducted at a medical center that includes a pediatric and adult hospital with a Level 1 trauma center in the midwestern United States. The pediatric hospital at the medical center has 111 beds, 8 pediatric operating rooms and a 21-bed PICU. In this PICU, the surgeons and a pediatric critical care medicine team are involved in patient care. The adult hospital at the medical center has 505 beds, 27 operating rooms and multiple ICUs; this study focuses on one 24-bed adult ICU where the surgeons and a critical care team, composed of surgeons and critical care anesthesiologists, are involved in patient care.
We used purposeful sampling (Patton, 2015) to select healthcare professionals to interview about the OR-to-PICU and OR-to-ICU care transitions, see table 1; participation was voluntary. Clinician members of our research team helped to identify healthcare professionals knowledgeable about the care transition process. All recruitment, data collection and analysis were done by HFE researchers with extensive field research experience. We approached clinicians via email, describing the purpose of our study and asking if they would be willing to participate in a less-than-one-hour interview and survey; all were willing to participate.
Table 1.
Sample (N=28)
| Profession | OR-to-PICU (N=15) | OR-to-ICU (N=13) |
|---|---|---|
| Physicians | Attending physicians: Anesthesiology - 1 Surgery - 1 Pediatric critical care - 1 Fellows Pediatric critical care - 2 Residents Anesthesiology - 1 Surgery - 2 |
Attending physicians: Anesthesiology* - 2 Surgery* - 1 Fellows Anesthesiology critical care - 1 Surgical critical care* - 1 Residents Anesthesiology* - 1 Surgery* - 2 |
| Advanced practice providers | Anesthetist - 1 | Anesthetist - 1 |
| Nurse | OR - 4 PICU - 2 |
OR - 2 Adult ICU - 2 |
Note:
denotes physicians who may practice in both the OR and adult ICU; these participants were asked if they provide care in both units, and if yes were asked about the transition from the perspective of providing care in the OR and the adult ICU.
2.2. Data collection
We conducted in-person semi-structured interviews with each healthcare professional, with follow-up questions to probe for more detailed information (Robson & McCartan, 2016). Each interview was conducted by one or two HFE researchers. The pediatric healthcare professionals were asked about the OR-to-PICU care transition; the adult healthcare professionals were asked about OR-to-ICU care transition. The adult surgery and anesthesiology interviewees were asked about the care transition from the perspective of being the physician in the OR and/or the physician in the ICU, based on the units in which they cared for the patient. For each care transition, researchers asked interviewees to identify the start and end of the care transition and describe the work system and process, including preparation and follow up, guided by the SEIPS model (Carayon et al., 2006; Carayon et al., 2014). We also elicited examples of good and bad transitions – i.e., when the patient’s care was not (or might have been) compromised and the transition went (or did not go) well from their perspective – and what made those go well or poorly, respectively. Interviewees were asked about the two most critical triaged levels of acuity upon emergency department (ED) arrival (Williams et al., 2011). The interview guides are available at: http://cqpi.wisc.edu/teamwork-and-care-transitions-in-pediatric-trauma/.
At the conclusion of the interview, each participant was asked to complete an eight-item survey that consisted of the four “teamwork across units” and four “handoffs and care transitions” items from the AHRQ Hospital Survey on Patient Safety Culture 1.0 (Sorra et al., 2018). The items detailing “shift changes” were worded instead as “transitions between units” as described by (Hoonakker et al., 2019).
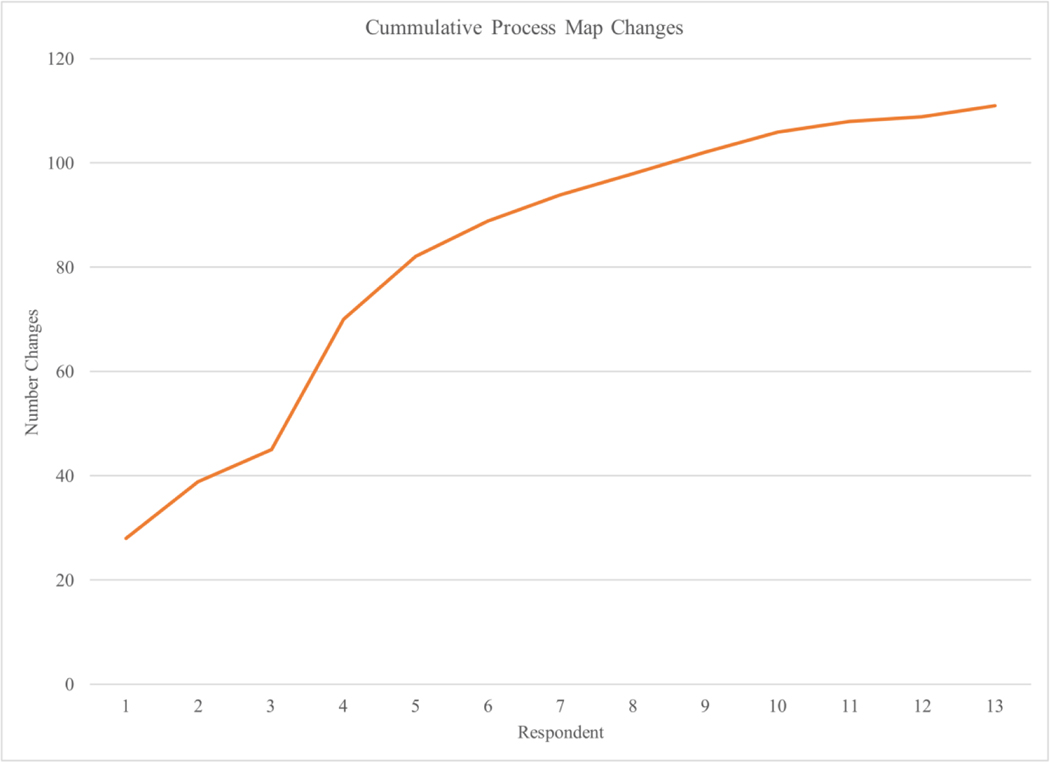
Nearly 22 hours of interviews were conducted (average: 46 minutes, range: 24 to 65 minutes). All interviews were audio-recorded and transcribed by a professional transcription service. After four interviews were conducted and deidentified, we iterated between data collection and analysis, monitoring when theoretical saturation (Glaser & Strauss, 1967) was reached by tracking the number of changes (e.g., additions and modifications) to the process map from each interview (see figure 2). In figure 2, we plot the cumulative number of changes by respondent – the changes from that specific interview plus all prior changes. There is a relatively sharp positive slope for each of the first five respondents, followed by a curve that gradually levels to approach a horizontal asymptote. The asymptote shows no new changes for each subsequent respondent, indicating we reached theoretical saturation. If additional clarification was needed, participants were contacted via email.
Figure 2.
Example of data saturation tracking: OR-to-ICU process map
2.3. Coding of interview transcripts
Transcripts were checked for accuracy and all identifying information was removed before we uploaded transcripts to Dedoose©, a web-based qualitative analysis software. The interviews were coded using a pre-determined coding scheme:
The specific care transition being discussed: OR-to-PICU or OR-to-ICU;
The trauma level designated upon arrival to the ED, following the Emergency Severity Index (ESI): Level 1 (highest level of acuity) and level 2 (lower level of acuity);
Description of the process and elements of the work system (Carayon et al., 2006; Carayon et al., 2014; Carayon et al., 2020).
Two HFE researchers independently coded one transcript and then met to review and resolve discrepancies. The same researchers then independently coded a second transcript and met to review discrepancies; at this point, there were minimal differences, and one researcher coded the remaining interview transcripts.
2.4. Creation of process maps
The coded excerpts were exported to Excel® by groups of each combination of transition and level (e.g., Level 1 OR-to-PICU, Level 2 OR-to-PICU). One researcher drafted the process maps in LucidChart© using the SEIPS-based process modeling method (Wooldridge et al., 2017). For each excerpt, the researcher identified which role(s) performed what task(s) with which technology(ies). Temporally relevant tasks related to the same goal and in the same location were grouped in the major steps shown in the boxes. When there were disagreements between interviewees, we relied on the description provided by the individual performing the work (i.e., the person in the role completing those tasks). Any outstanding questions were resolved through a consensus process with other HFE researchers. The process maps were reviewed by participating clinicians in a member-checking process; their feedback and suggestions were incorporated in revising the process maps.
2.5. Care transition start and end
Each interviewee’s response to the two questions about the start and end of the care transition were coded as process start or process end, respectively in Dedoose©. The responses were then exported to Excel® and reviewed by two HFE researchers to identify the step of the process mentioned. Responses were counted by profession (i.e., physician/APP or nurse) and whether the interviewee provided care in the OR, adult ICU or PICU (i.e., sending or receiving unit, respectively).
2.6. Survey data analysis
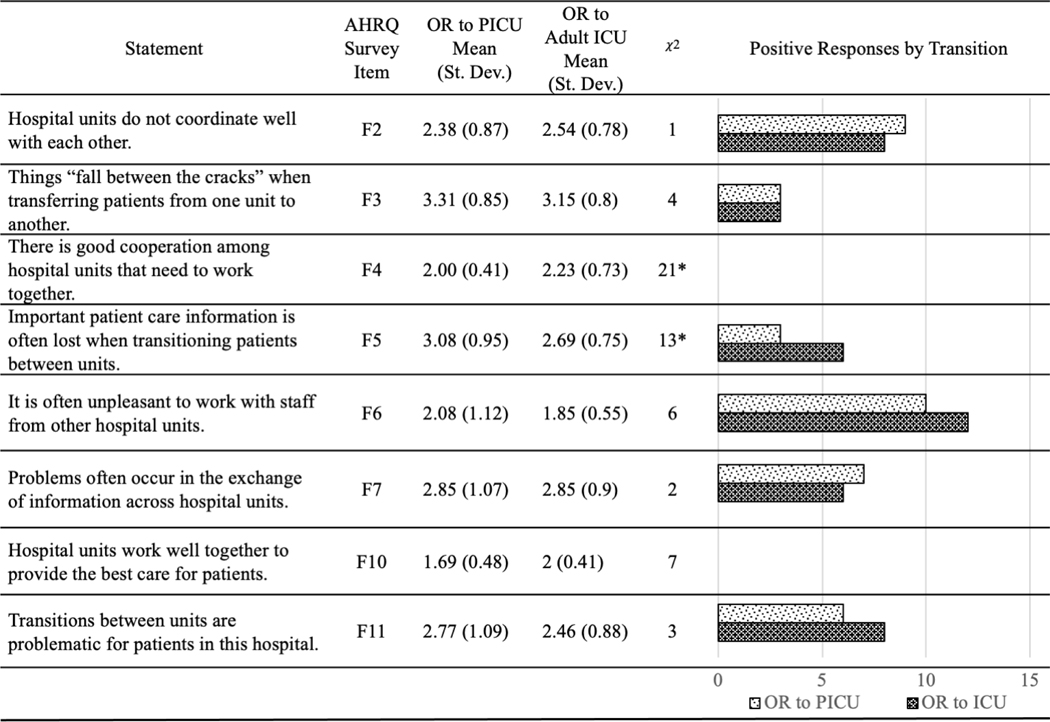
The means and standard deviations of responses to each item were calculated for the OR-to-ICU and OR-to-PICU transitions. Two questions (F4 and F10) were reverse coded for consistency in scale from positive to negative response across items, and chi-square tests were conducted to determine if the distributions of responses between the OR to PICU and OR to adult ICU groups for each question were different. Additionally, the frequency of positive responses (i.e., responses of 1 or 2 after reverse coding) for each group were tabulated and compared.
3. RESULTS
3.1. Process maps
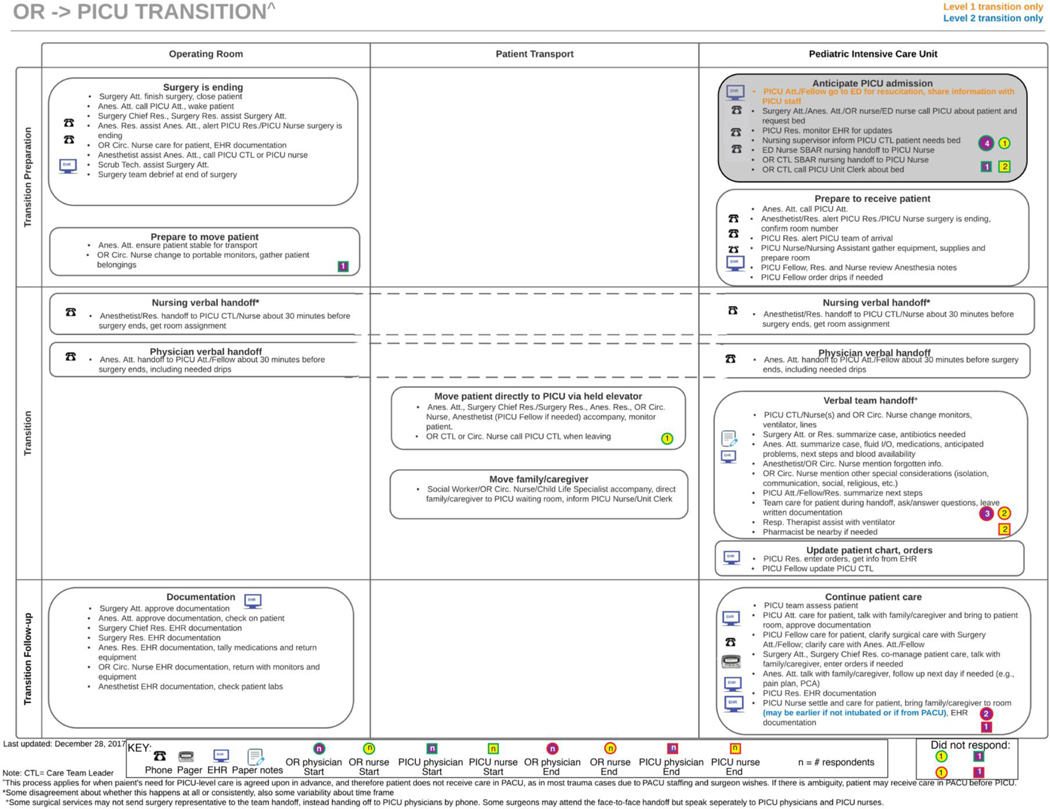
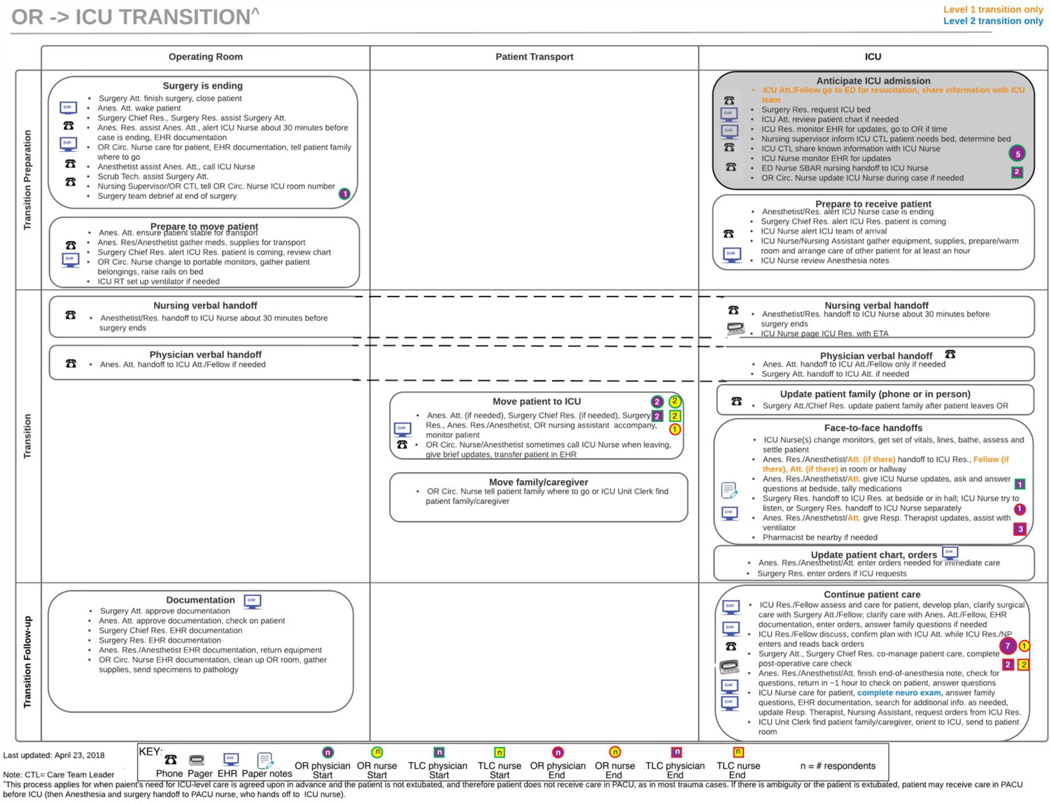
Table 2 shows guidelines we use to created SEIPS-based process maps and how we operationalized these guidelines in this study. Figures 3 shows the process map of the OR-to-PICU care transition and figure 4 shows the process map of the OR-to-ICU care transition.
Table 2.
Guidelines for creating process maps
| Guideline | Operationalization |
|---|---|
| 1. Represent temporal nature of process. | • Rows represent phases of care transition: transition preparation, transition and transition follow-up. • Time is represented moving down through the phases and roughly from left to right. |
| 2. Represent spatial nature of process (i.e., physical locations where work is performed). | • Columns represent physical locations: OR, PICU or ICU and the path of transport from OR to PICU or ICU. |
| 3. Clearly indicate distributed work. | • Tasks that are distributed spatially in the OR and PICU or ICU are represented with dashed lines connecting the boxes in each column. |
| 4. Highlight work completed in preparation for, but not necessarily part of, the process being modeled. | • Activities when the patient is still in the ED before transfer to the OR are in light grey. |
| 5. Distinguish and incorporate higher-level goals and specific tasks performed by individual(s). | • Each bulleted line in the activity box represents tasks completed by a unique group of roles. |
| 6. Show tools and technologies used for each task. | • The technologies used only in one bulleted line (task or tasks completed by the same group of roles) are represented with icons. • If a technology was used for every bulleted line in an activity box, the icon is to the right of the title of that box. |
| Represent variation in the process. | • There were differences in two and five bullet points between level 1 and level 2 patients for pediatric and adult care transitions, respectively; specific differences are highlighted by text color. |
Figure 3.
SEIPS-based process model of OR-to-PICU care transition.
Figure 4.
SEIPS-based process model of OR-to-ICU care transition.
The OR-to-PICU care transition has 12 activities (four preparation, six transition and two follow-up) and 55 groups of tasks (23 preparation, 18 transition and 14 follow-up). The OR-to-ICU care transition has 15 activities (four preparation, nine transition and two follow-up) and 58 groups of tasks (28 preparation, 18 transition and 12 follow-up). Twenty-three roles participate in the care transition process using four communication technologies in both care transitions. Many of the activities and specific tasks in both care transitions are similar. One major difference is that the OR-to-PICU care transition includes a team handoff between surgery, anesthesia and PICU team, including nurses and physicians. The handoff was described by a surgery resident as follows:
“[T]he nurses up there, as well as the [pediatric] ICU doctor team, receive the patient… the surgery handoff is a brief history of what happened to the patient, the injuries, what you did in the OR, and what the care plan is. And the anesthesia team then usually signs out.”
The handoffs in the OR-to-ICU transition are separate, occurring simultaneously between anesthesia and nursing and surgeon and ICU physician while others were settling the patient in the ICU room. An adult ICU nurse described the handoff as follows: “[A]nesthesia is usually trying to give their report…And then kind of off in the corner it will be the surgical resident with the [adult] ICU resident…giving like a report of the actual surgery and stuff” (adult ICU nurse).
3.2. Start and end of care transition process
The healthcare professionals involved in care transition have different perspectives on when the care transition starts and ends; responses are integrated on the process maps in figures 4 and 5 showing the profession and unit of the interviewee. While there was variation between interviewees, the first communication, or “that heads-up phone call” (PICU nurse), between the surgical team and PICU or ICU team was the most frequent step noted as the start of the care transition. Responses on the start of the transition ranged from when the patient arrives to the ED and as late as the handoff in the PICU or ICU. After the handoff and the receiving team is satisfied (i.e., gets to ask questions) and after the receiving team assumes care, described by an adult anesthesia attending as “achieving a stable set of vitals” after handoff, were mentioned most as the end of the care transition. Responses for when the transition ends ranged from when the patient arrives in the PICU or ICU and as late as after the surgery chief resident completes a post-operative check. The physicians and APPs, including trainee physicians, responded that the care transition starts earlier and ends later than the nurses.
Figure 5.
Survey items, average responses, χ2 and frequency of positive responses.
Notes: Possible survey responses 1=strongly disagree, 2=disagree, 3=neither, 4=agree, 5=strongly agree. Chi-square critical value for all tests = 11.1143. *denotes significantly different distribution of responses. Positive responses were 1 and 2, after questions F4 and F10 were reverse coded.
Table 3 shows how many interviewees responded that each transition starts or ends at specific pairs of steps by their profession and unit. Interviewees in the OR-to-PICU care transition, which involves the team handoff, were more similar in their start and end responses: there were only four combinations of process start and end responses. The participants in the OR-to-ICU care transition had a more varied response, with seven combinations of start and end given.
Table 3.
Start and end of care transition process
| Process | OR-to-PICU Frequency | OR-to-Adult ICU Frequency | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sender | Receiver | Sender | Receiver | |||||||
| Start | End | Physician | Nurse | Physician | Nurse | Physician | Nurse | Physician | Nurse | Total Frequency |
| Anticipate admission | Handoff | 2 | 1 | 2 | 1 | 6 | ||||
| Anticipate admission | Continue patient care | 2 | 1 | 5 | 1 | 9 | ||||
| Surgery is ending | Continue patient care | 1 | 1 | |||||||
| Prepare to move patient | Handoff | 1 | 1 | |||||||
| Move patient | Continue patient care | 1 | 1 | 2 | 4 | |||||
| Move patient | Move patient | 1 | 1 | |||||||
| Move patient | Handoff | 1 | 1 | 2 | 4 | |||||
| Handoff | Continue patient care | 1 | 1 | |||||||
| Not answered | Not answered | 1 | 1 | 2 | ||||||
3.3. AHRQ Hospital Survey on Patient Safety Transitions, Handoffs and Teamwork Across Units Differences
Figure 5 shows the statements for each item, the average and standard deviation of responses for the OR to PICU or ICU groups and the χ2 statistic; χ2c for each comparison was 11.143. The distribution for item F4 and F5 were significantly different between groups (i.e., χ2 > χ2c). Figure 5 also includes the frequency of positive responses to each item for each care transition, where positive responses indicate disagreement with statements that negatively impact patient safety. Neither OR-to-PICU nor OR-to-ICU participants responded positively to F4 (that there is good cooperation between hospital units) or F10 (that hospital units work well together). Some participants in the OR-to-ICU care transition responded that they neither agreed nor disagreed to F4 (i.e., selected 3 “neither”), indicating less disagreement with the statement than participants from the OR-to-PICU care transition, who all responded that they disagreed or strongly disagreed with F4. The participants from the OR-to-ICU transition had more positive responses to F5, indicating information was not lost during care transitions.
4. DISCUSSION
Our results show that OR-to-PICU and OR-to-ICU care transitions of trauma patients are complex, temporal processes involving many healthcare professionals, and include both physical transitions (i.e., transport) and cognitive transitions (i.e., handoffs). Clinicians involved in the care transition had varying perceptions of when the care transitions begin and end, perhaps explained by differing professional perspectives or their roles as sender or receiver. The care transition was often described as beginning when admission to the PICU or ICU was anticipated, i.e., first communication between surgical and PICU or ICU teams and ending when the PICU or ICU team continued patient care and assumed care after handoff. Clinicians participating in the handoff with the team handoff (OR-to-PICU) had a more similar understanding of process scope than did those in with separate handoffs (OR-to-ICU).
4.1. Comparison of OR to PICU and OR to ICU care transitions
The main difference between the two care transitions was how the handoffs were organized. The OR-to-PICU care transition included a verbal team handoff, including anesthesia, surgery and PICU physicians and nurses. Handoffs in the OR-to-ICU care transition were separate, with anesthesia and surgery residents providing information to the adult ICU resident and nurse separately. Handoffs, while important, are only a small part of the care transition process. The transition includes preparatory activities before the handoff (as early as immediately after a trauma patient arrives to the ED) and follow-up activities afterward (as late as a post-operative check completed by the surgery chief resident); these activities are specified in the process maps in figures 3 and 4. Examples of preparatory activities described by our participants include the debrief at the end surgery, calls between the OR and PICU or ICU and gathering supplies and equipment before the patient arrives to the PICU or ICU; examples of follow-up activities include completing documentation, returning medications and equipment to the OR, patient care activities in the PICU or ICU and updating family or caregivers of the patient. This idea is not new, since it has been described in previous research (Abraham et al., 2012; Agarwal et al., 2012; Catchpole et al., 2007; Craig et al., 2012; Haque et al., 2017; Matthews et al., 2002; McElroy, Collins, et al., 2015; McElroy, Macapagal, et al., 2015); in fact, early notification of ICU arrival is important in successful handoffs (Lane-Fall et al., 2018). However, these studies were less detailed in their description of the activities involved in preparation and follow-up. Here, we uniquely show that preparation includes communication and coordination (e.g., the early notification and information exchange prior to transport) as well as preparation activities in both units (e.g., gathering supplies or equipment and preparing team members).
While neither group in the OR-to-PICU or OR-to-ICU transition responded positively to the statements about good cooperation between hospital units and units working well together, the OR-to-ICU group responded significantly differently and more positively to the statement about information being lost when patients transition between hospital units (item F5, see figure 5), indicating less information loss than in the OR-to-PICU transition with a team handoff. The survey results were not expected – the only items with different responses were more positive for the OR-to-ICU transition, which did not include a team handoff. One possible, but unlikely, interpretation is that the team handoff had a negative impact, but based on literature emphasizing the importance of teams and teamwork to patient safety (Salas et al., 2008), this interpretation is not likely to be correct. A more likely explanation is that participating in the team-based handoff may have highlighted issues related to communication, coordination and cooperation between the hospital units because the handoffs increased interaction. The clinicians involved in the OR-to-PICU care transitions were made aware of developing failures during the team handoff, providing them the opportunity to recover from them. Unfortunately, the participants may have interpreted the awareness of developing failures as lack of success, rather than the team handoff working well to support avoiding and recovering from failure before patient harm occurs, i.e., a success. In other words, the team handoff resulted in increased recognition of problems that could exist in transitions and thus resulted in more negative responses to the survey (i.e., that information was lost during transitions), despite the benefits recognized by those same participants in the interview, such as:
“[I]f the patient’s on epi, and, you know, we say, don’t give fluid right now, just go up on epi, then maybe they’ll understand because of something that happened in the OR, whereas we would just have to re-explain everything [if it was not a team handoff]. So it’s just easier if they can kind of get the firsthand information as well.” [PICU nurse]
We argue that the team-based handoff likely increased awareness about the communication (or lack thereof) within the team as well as organizational awareness – awareness of how work of the individuals fit together in the overall care process (Schultz et al., 2007). We expect that increasing organizational awareness and improving communication will improve patient safety during care transitions in the long term. Future work could include studies designed specifically to investigate the impact of the team handoff on outcomes, including observed communication challenges, patient outcomes, organizational awareness, and individual clinician outcomes like satisfaction with the handoff. Interventions using SEIPS-based process mapping may also serve to increase organizational awareness, for example by helping the participating healthcare professionals understand their work as well as how and where their work fits in the overall care process and with the work of their colleagues. Further, HFE-based tools and projects are instrumental in highlighting the difference between task and activity (Leplat, 1989), also called work-as-imagined and work-as-done (Hollnagel et al., 2015).
4.2. Importance of articulation work in care transitions
The activities associated with the preparation and follow-up phases of the care transition can be thought of as articulation work (Berg, 1999; Gerson & Star, 1986) – work that enables other work (e.g., transport, handoff). Without these activities, the care transition will not be successful; failing to consider this articulation work in redesigning care transitions could have a negative impact on quality of care. Further, all activities impact the healthcare professionals involved in the care transition and are included in their workload; if disregarded, clinicians may still perform the communication and coordination work to ensure safe transitions for their patients. However, this could overburden the clinicians and result in poor worker outcomes (e.g., stress, burnout). This is an important reminder that we, as human factors experts, cannot simply design for one task (i.e., handoff tasks) – we must design for the process (Walker & Carayon, 2009). Improving the entire care transition process through careful, systems-based thinking should result in improved patient and worker outcomes (Waterson, 2009).
Many of the articulation work activities in the care transition process involved communication and coordination (e.g., anesthesia resident calling the PICU or ICU nurse before the surgical case ends), the handoffs, developing and clarifying the care plan. Some of this communication is asynchronous and distributed (e.g., through the EHR), some is synchronous and distributed (e.g., conducted by phone) while some is synchronous and collocated (e.g., face-to-face handoffs). Differences in communication due to synchronicity (i.e., synchronous or asynchronous), communication modality (e.g., phone, text, email, face-to-face) and if it is distributed or collocated are well documented (Fairbanks et al., 2007; Wooldridge, Carayon, Shaffer, et al., 2018). For example, when tasks were allocated between members of a primary care team synchronously, those tasks were more likely to be accepted and completed (Wooldridge, Carayon, Shaffer, et al., 2018). Future work should consider the spatio-temporal nature of communication involved in care transition processes.
Communication and coordination activities inherently include two or more individuals working towards a common goal, i.e., a safe care transition; in other words, they involve a team. These team communication activities can be conceptualized as team cognition (Cooke et al., 2013). Thus, team cognition theory could inform efforts to improve handoffs, e.g., by changing how we train medical professionals to communicate, facilitating interactions with and/or designing team-centric technology (Coppola & Gurses, 2021), co-location and other work system design choices. The team cognition approach also has implications for how we approach handoff research (Cooke et al., 2013); for example, we could measure team cognition during handoffs as part of evaluating interventions, facilitating real-time measurement to use in training or identify hazardous transitions.
4.3. Advancing SEIPS-based process modeling
In this study, we continued developing SEIPS-based process modeling by analyzing a complex process involving many people completing tasks distributed across space and time. We expanded our method to represent a larger number of tasks distributed over space and time than we had previously considered (Wooldridge, Carayon, Hoonakker, et al., 2018). Here, we also provide guidelines for others to develop these process models, with specific examples of how those guidelines can be operationalized (see table 2). In this study, we used interviews to collect data rather than combined interviews and observations; therefore, we relied on the description of the process provided by participants. Interestingly, participants did not include various IV pumps, monitors, poles, etc. in their description of the technology they use in the transition; instead, they focused on technologies to facilitate communication and coordination. In an observational study using a macroergonomic perspective, we would expect to identify additional technologies used, as well as issues related to the physical environment.
Process modeling has been used in other sectors to identify improvement opportunities by building an understanding of the system, as well as documenting current or planned processes to ensure understanding necessary for future improvement (Jun et al., 2009). Although we did not evaluate the transition by presenting data on work system barriers and facilitators, we were able to represent more specific details of the tasks on the process maps, eliminating additional tables in our first application (Wooldridge et al., 2017). Future work will address how to incorporate work system barriers and facilitators on the maps as part of process evaluation.
4.4. Limitations
This study was completed in one healthcare organization, necessarily limiting generalization beyond this organization. Although a generalizable description of the OR-to-PICU and OR-to-ICU care transition beyond this medical center was not the goal of this study, care transitions in urban or non-teaching hospitals may be very different.
We did not collect the patient and family perceptions of care transitions in this study. Trauma is, by definition, highly stressful; this presents challenges to data collection involving patients and their family: interviewing patients and their family immediately following the OR-to-PICU or OR-to-ICU care transition may not be appropriate, given the emotional challenges experienced by families. Retrospective data collection may be reasonable, but it may be several weeks before it is appropriate and feasible to talk with patients and their family, considering potentially long hospitalizations, inpatient or outpatient rehabilitation, etc. That lag could result in recall bias, particularly since patients and their families may not focus on care transitions. Future work should seek to find ways to incorporate the perspective of patients and their families or other caregivers.
5. CONCLUSION
Our study demonstrates that care transitions are complex processes distributed over time and space, involving many individuals; even though they occur frequently (i.e., are routine), they remain high risk. Care transitions include readily acknowledged work – handoffs and transport – as well as articulation work. As human factors professionals and systems engineers, we must account for articulation work because it impacts system performance and human well-being. Without considering the significant communication and coordination work done before and after handoff, we can overburden clinicians and staff, subjecting them to stress and burnout and contributing to poor patient outcomes due to inadequately coordinated transitions. Moving forward in the study and improvement of care transitions, we must consider the entire process through systems-based methodologies grounded in HFE. SEIPS-based process modeling is a useful tool to consider articulation work during process (re)design. HFE experts embedded in health care organizations could have substantial impact, in particular as they are trained to consider the entire system, not only person, and capture differences between task and activity (i.e., work-as-imagined and work-as-done). Clinicians could use the seven simple SEIPS tools to have positive impact as well (Holden & Carayon, 2021). Future work should incorporate the perspective of the patient and their family to shift to patient- and family-centered care as well as analyze system barriers and facilitators to inform care transition process redesign, with a focus on supporting team cognition and awareness while considering articulation work involved before and after handoffs.
Highlights.
SEIPS-based process modeling applies to higher complexity processes.
Articulation work can be highlighted with SEIPS-based process modeling.
Articulation work outside of handoffs is necessary for safe care transitions.
Team handoffs increased team members’ awareness of poor cooperation.
Physicians and nurses think of care transition scope differently.
6. ACKNOWLEGEMENTS
We would like to thank the study participants, as our research would not be possible without them.
8. FUNDING
This work was supported by the Agency for Healthcare Research and Quality [Grant No. R01 HS023837] and the Clinical and Translational Science Award (CTSA) program, through the National Institutes of Health National Center for Advancing Translational Sciences (NCATS), [Grant UL1TR002373]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
Footnotes
DECLARATION OF COMPETING INTEREST
The authors have no competing interests to disclose.
REFERENCES
- Aase K, & Waring J. (2020). Crossing boundaries: Establishing a framework for researching quality and safety in care transitions. Appl Ergon, 89, 103228. 10.1016/j.apergo.2020.103228 [DOI] [PubMed] [Google Scholar]
- Abraham J, Ihianle I, & Burton S. (2017). Exploring Information Seeking Behaviors in Inter-unit Clinician Handoffs International Symposium on Human Factors and Ergonomics in Health Care, [Google Scholar]
- Abraham J, Kannampallil T, & Patel VL (2014). A systematic review of the literature on the evaluation of handoff tools: implications for research and practice. J Am Med Inform Assoc, 21(1), 154–162. 10.1136/amiajnl-2012-001351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abraham J, Kannampallil TG, & Patel VL (2012). Bridging gaps in handoffs: A continuity of care based approach [Journal Article Research Support, Non-U.S. Gov’t Research Support, U.S. Gov’t, P.H.S.]. Journal of Biomedical Informatics, 45(2), 240–254. 10.1016/j.jbi.2011.10.011 [DOI] [PubMed] [Google Scholar]
- Agarwal HS, Saville BR, Slayton JM, Donahue BS, Daves S, Christian KG, Bichell DP, & Harris ZL (2012). Standardized postoperative handover process improves outcomes in the intensive care unit: A model for operational sustainability and improved team performance [Journal Article]. Critical Care Medicine, 40(7), 2109–2115. 10.1097/CCM.0b013e3182514bab [DOI] [PubMed] [Google Scholar]
- Arora VM, Manjarrez E, Dressler DD, Basaviah P, Halasyamani L, & Kripalani S. (2009). Hospitalist handoffs: A systematic review and task force recommendations. Journal of Hospital Medicine, 4(7), 433–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg M. (1999). Patient care information systems and health care work: A sociotechnical approach. Int J Med Inform, 55(2), 87–101. [DOI] [PubMed] [Google Scholar]
- Carayon P, Hundt AS, Karsh B-T, Gurses AP, Alvarado CJ, Smith M, & Brennan PF (2006). Work system design for patient safety: The SEIPS model. Qual Saf Health Care, 15(Supplement I), i50–i58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, Wetterneck TB, Rivera-Rodriguez AJ, Hundt AS, Hoonakker P, Holden R, & Gurses AP (2014). Human factors systems approach to healthcare quality and patient safety. Appl Ergon, 45(1), 14–25. 10.1016/j.apergo.2013.04.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, & Wooldridge AR (2020). Improving Patient Safety in the Patient Journey: Contributions from Human Factors Engineering. In Smith AE (Ed.), Women in Industrial and Systems Engineering: Key Advances and Perspectives on Emerging Topics (pp. 275–299). Springer International Publishing. 10.1007/978-3-030-11866-2_12 [DOI] [Google Scholar]
- Carayon P, Wooldridge AR, Hoonakker P, Hundt AS, & Kelly MM (2020). SEIPS 3.0: Human-centered design of the patient journey for patient safety. Appl Ergon, 84, 103033. 10.1016/j.apergo.2019.103033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catchpole K, De Leval MR, Mcewan A, Pigott N, Elliott MJ, Mcquillan A, Macdonald C, & Goldman AJ (2007). Patient handover from surgery to intensive care: using Formula 1 pit-stop and aviation models to improve safety and quality. Pediatric Anesthesia, 17(5), 470–478. [DOI] [PubMed] [Google Scholar]
- Cooke NJ, Gorman JC, Myers CW, & Duran JL (2013). Interactive team cognition. Cognitive science, 37(2), 255–285. [DOI] [PubMed] [Google Scholar]
- Coppola SM, & Gurses AP (2021). Remote Usability Testing of a Pediatric Trauma Dashboard. In Black NL, Neumann WP, & Noy I, Proceedings of the 21st Congress of the International Ergonomics Association (IEA 2021) Cham. [Google Scholar]
- Craig R, Moxey L, Young D, Spenceley NS, & Davidson MG (2012). Strengthening handover communication in pediatric cardiac intensive care. Pediatric Anesthesia, 22(4), 393–399. [DOI] [PubMed] [Google Scholar]
- CRICO Strategies. (2015). Malpractice risk in communication failures; 2015 Annual Benchmarking Report. The Risk Management Foundation of the Harvard Medical Institutions, Inc. [Google Scholar]
- Daniellou F. (2005). The French-speaking ergonomists’ approach to work activity: cross-influences of field intervention and conceptual models. Theoretical Issues in Ergonomics Science, 6(5), 409–427. 10.1080/14639220500078252 [DOI] [Google Scholar]
- Fairbanks RJ, Bisantz AM, & Sunm M. (2007). Emergency Department Communication Links and Patterns. Annals of Emergency Medicine, 50(4), 396–406. 10.1016/j.annemergmed.2007.03.005 [DOI] [PubMed] [Google Scholar]
- Gerson EM, & Star SL (1986). Analyzing due process in the workplace. ACM Transactions on Information Systems (TOIS), 4(3), 257–270. [Google Scholar]
- Glaser BG, & Strauss AL (1967). The Discovery of Grounded Theory: Strategies for Qualitative Research. Aldine. [Google Scholar]
- Haque SN, Østerlund CS, & Fagan LM (2017). What’s Ideal? A case study exploring handoff routines in practice. Journal of Biomedical Informatics, 65, 159–167. [DOI] [PubMed] [Google Scholar]
- Hignett S, Jones EL, Miller D, Wolf L, Modi C, Shahzad MW, Buckle P, Banerjee J, & Catchpole K. (2015). Human factors and ergonomics and quality improvement science: Integrating approaches for safety in healthcare. BMJ Quality & Safety 24(4), 1–5. 10.1136/bmjqs-2014-003623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holden RJ, & Carayon P. (2021). SEIPS 101 and seven simple SEIPS tools. BMJ Quality & Safety, bmjqs-2020–012538. 10.1136/bmjqs-2020-012538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollnagel E, Wears R, & Braithwaite J. (2015). Chapter 18: Why is work-as-imagined different from work-as-done? In Resilient Health Care, Volume 2: The Resilience of Everyday Clinical Work. Ashgate Publishing, Ltd. [Google Scholar]
- Hoonakker PLT, Wooldridge AR, Hose B-Z, Carayon P, Eithun B, Brazelton TB 3rd, Kohler JE, Ross JC, Rusy DA, Dean SM, Kelly MM, & Gurses AP (2019). Information flow during pediatric trauma care transitions: things falling through the cracks. Intern Emerg Med, 14(5), 797–805. 10.1007/s11739-019-02110-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y-H, & Gramopadhye AK (2014). Systematic engineering tools for describing and improving medication administration processes at rural healthcare facilities. Appl Ergon, 45(6), 1712–1724. 10.1016/j.apergo.2014.06.003 [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. (2001). Crossing the Quality Chasm: A New Health System for the 21st Century. National Academy Press. [PubMed] [Google Scholar]
- International Ergonomics Association (IEA). (2020). Definition and Application. Retrieved October 31, 2020 from http://www.iea.cc/whats/ [Record #9935 is using a reference type undefined in this output style.]
- Jun GT, Ward J, & Clarkson P. (2010). Systems modelling approaches to the design of safe healthcare delivery: ease of use and usefulness perceived by healthcare workers. Ergonomics, 53(7), 829–847. 10.1080/00140139.2010.489653 [DOI] [PubMed] [Google Scholar]
- Jun GT, Ward J, Morris Z, & Clarkson J. (2009). Health care process modelling: which method when? [Journal Article]. International Journal for Quality in Health Care, 21(3), 214–224. 10.1093/intqhc/mzp016 [DOI] [PubMed] [Google Scholar]
- Lane R, Stanton NA, & Harrison D. (2006). Applying hierarchical task analysis to medication administration errors. Appl Ergon, 37, 669–679. [DOI] [PubMed] [Google Scholar]
- Lane-Fall MB, Christakos A, Russell GC, Hose BZ, Dauer ED, Greilich PE, Hong Mershon B, Potestio CP, Pukenas EW, Kimberly JR, Stephens-Shields AJ, Trotta RL, Beidas RS, & Bass EJ (2021). Handoffs and transitions in critical care-understanding scalability: study protocol for a multicenter stepped wedge type 2 hybrid effectiveness-implementation trial. Implement Sci, 16(1), 63. 10.1186/s13012-021-01131-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane-Fall MB, Pascual J, Gutsche J, Di Taranti LJ, Buddai S, Barg F, & Fleisher L. (2016). Handoff standardization in two mixed surgical intensive care units improves teamwork and information exchange: preliminary findings from the Handoffs and Transitions in Critical Care (HATRICC) study. Anesthesia and Analgesia, [Google Scholar]
- Lane-Fall MB, Pascual JL, Massa S, Collard ML, Peifer HG, Di Taranti LJ, Linehan M, Fleisher LA, & Barg FK (2018). Developing a Standard Handoff Process for Operating Room–to-ICU Transitions: Multidisciplinary Clinician Perspectives from the Handoffs and Transitions in Critical Care (HATRICC) Study. The Joint Commission Journal on Quality and Patient Safety, 44(9), 514–525. https://doi.org/doi: 10.1016/j.jcjq.2018.02.004 [DOI] [PubMed] [Google Scholar]
- Lane-Fall MB, Pascual JL, Peifer HG, Di Taranti LJ, Collard ML, Jablonski J, Gutsche JT, Halpern SD, Barg FK, & Fleisher LA (2020). A Partially Structured Postoperative Handoff Protocol Improves Communication in 2 Mixed Surgical Intensive Care Units: Findings From the Handoffs and Transitions in Critical Care (HATRICC) Prospective Cohort Study. Ann Surg, 271(3), 484–493. 10.1097/sla.0000000000003137 [DOI] [PubMed] [Google Scholar]
- Leplat J. (1989). Error analysis, instrument and object of task analysis. Ergonomics, 32(7), 813–822. [Google Scholar]
- Marcotte L, Kirtane J, Lynn J, & McKethan A. (2015). Integrating health information technology to achieve seamless care transitions. Journal of Patient Safety, 11(4), 185–190. [DOI] [PubMed] [Google Scholar]
- Massa S, Wu J, Wang C, Peifer H, & Lane-Fall MB (2021). Interprofessional Training and Communication Practices Among Clinicians in the Postoperative ICU Handoff. The Joint Commission Journal on Quality and Patient Safety, 47(4), 242–249. 10.1016/j.jcjq.2020.12.004 [DOI] [PubMed] [Google Scholar]
- Matthews AL, Harvey CM, Schuster RJ, & Durso FT (2002). Emergency physician to admitting physician handovers: an exploratory study Human Factors and Ergonomics Society Annual Meeting, [Google Scholar]
- McElroy LM, Collins KM, Koller FL, Khorzad R, Abecassis MM, Holl JL, & Ladner DP (2015). Operating room to intensive care unit handoffs and the risks of patient harm. Surgery, 158(3), 588–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McElroy LM, Macapagal KR, Collins KM, Abecassis MM, Holl JL, Ladner DP, & Gordon EJ (2015). Clinician perceptions of operating room to intensive care unit handoffs and implications for patient safety: a qualitative study. The American Journal of Surgery, 210(4), 629–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, E., and Medicine,. (2019). Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being. https://nam.edu/clinicianwellbeingstudy [PubMed] [Google Scholar]
- Patton MQ (2015). Sampling, Qualitative (Purposeful). In The Blackwell Encyclopedia of Sociology. 10.1002/9781405165518.wbeoss012.pub2 [DOI] [Google Scholar]
- Perry SJ (2004). Transitions in care: Studying safety in emergency department signovers. Focus on Patient Safety, 7(2), 1–3. [Google Scholar]
- Robson C, & McCartan K. (2016). Real World Research (Fourth ed.). Wiley & Sons Ltd. [Google Scholar]
- Ross Perfetti A, Peifer H, Massa S, Di Taranti LJ, Choudhary M, Collard M, George D, Wang C, Beidas R, Barg FK, & Lane-Fall MB (2020). Mixing Beyond Measure: Integrating Methods in a Hybrid Effectiveness–Implementation Study of Operating Room to Intensive Care Unit Handoffs. Journal of Mixed Methods Research, 14(2), 207–226. 10.1177/1558689819844038 [DOI] [Google Scholar]
- Salas E, Wilson KA, Murphy CE, King H, & Salisbury M. (2008). Communicating, coordinating, and cooperating - When lives depend on it: Tips for teamwork. The Joint Commission Journal on Quality and Patient Safety, 34(6), 333–341. [DOI] [PubMed] [Google Scholar]
- Schultz K, Carayon P, Hundt AS, & Springman SR (2007). Care transitions in the outpatient surgery preoperative process: Facilitators and obstacles to information flow and their consequences. Cognition, Technology & Work, 9(4), 219–231. [Google Scholar]
- Siemieniuch CE, & Sinclair MA (2015). Methods in Systems Ergonomics. In Evaluation of Human Work (4th ed., pp. 855–879). CRC Press. [Google Scholar]
- Simsekler MCE, Ward JR, & Clarkson PJ (2018). Evaluation of system mapping approaches in identifying patient safety risks. International Journal for Quality in Health Care, 30(3), 227–233. 10.1093/intqhc/mzx176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorra J, Gray L, Streagle S, Famolaro T, Yount N, & Behm J. (2018). AHRQ Hospital Survey on Patient Safety Culture. (Prepared by Westat, under Contract No. 290–96-0004) (AHRQ publication, Issue. https://www.ahrq.gov/sops/surveys/hospital/index.html [Google Scholar]
- Stewart RM, Myers JG, Dent DL, Ermis P, Gray GA, Villarreal R, Blow O, Woods B, McFarland M, Garavaglia J, Root HD, & Pruitt BA Jr. (2003). Seven hundred fifty-three consecutive deaths in a level I trauma center: the argument for injury prevention. J Trauma, 54(1), 66–71. 10.1097/01.ta.0000046312.75231.74 [DOI] [PubMed] [Google Scholar]
- Walker J, & Carayon P. (2009). From tasks to processes: The case for changing health information technology to improve health care. Health Affairs, 28(2), 467–477. http://ezproxy.library.wisc.edu/login?url=http://proquest.umi.com/pqdweb?did=1672025341&Fmt=7&clientId=3751&RQT=309&VName=PQD [DOI] [PubMed] [Google Scholar]
- Waterson P. (2009). A critical review of the systems approach within patient safety research. Ergonomics, 52(10), 1185–1195. [DOI] [PubMed] [Google Scholar]
- Wetterneck TB, Skibinski KA, Roberts TL, Kleppin SM, Schroeder ME, Enloe M, Rough SS, Hundt AS, & Carayon P. (2006). Using failure mode and effects analysis to plan implementation of smart i.v. pump technology [Journal Article Research Support, N.I.H., Extramural Research Support, U.S. Gov’t, P.H.S. Review]. American Journal of Health-System Pharmacy, 63(16), 1528–1538. 10.2146/ajhp050515 [DOI] [PubMed] [Google Scholar]
- Williams D, Foglia R, Megison S, Garcia N, Foglia M, & Vinson L. (2011). Trauma activation: are we making the right call? A 3-year experience at a Level I pediatric trauma center. Journal of Pediatric Surgery, 46(10), 1985–1991. [DOI] [PubMed] [Google Scholar]
- Wooldridge AR, Carayon P, Hoonakker P, Hose B-Z, Eithun B, Brazelton T, Ross J, Kohler JE, Kelly MM, Dean SM, Rusy D, & Gurses AP (2020). Work system barriers and facilitators in inpatient care transitions of pediatric trauma patients. Appl Ergon, 85, 103059. 10.1016/j.apergo.2020.103059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wooldridge AR, Carayon P, Hoonakker P, Hose B-Z, Ross J, Kohler JE, Brazelton T, Eithun B, Kelly MM, Dean SM, Rusy D, Durojaiye A, & Gurses AP (2018). Complexity of the pediatric trauma care process: implications for multi-level awareness [journal article]. Cognition, Technology & Work. 10.1007/s10111-018-0520-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wooldridge AR, Carayon P, Hundt AS, & Hoonakker PLT (2017). SEIPS-based process modeling in primary care. Appl Ergon, 60, 240–254. 10.1016/j.apergo.2016.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wooldridge AR, Carayon P, Shaffer DW, & Eagan B. (2018). Quantifying the qualitative with epistemic network analysis: A human factors case study of task-allocation communication in a primary care team. IISE Transactions on Healthcare Systems Engineering, 8(1), 72–82. 10.1080/24725579.2017.1418769 [DOI] [PMC free article] [PubMed] [Google Scholar]