Abstract
Background
Some antiepileptic drugs but not others are useful in clinical practice for the prophylaxis of migraine. This might be explained by the variety of actions of these drugs in the central nervous system. The present review is part of an update of a Cochrane review first published in 2004, and previously updated (conclusions not changed) in 2007.
Objectives
To describe and assess the evidence from controlled trials on the efficacy and tolerability of valproate (valproic acid or sodium valproate or a combination of the two) for preventing migraine attacks in adult patients with episodic migraine.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL; The Cochrane Library 2012, Issue 12), PubMed/MEDLINE (1966 to 15 January 2013), MEDLINE In‐Process (current week, 15 January 2013), and EMBASE (1974 to 15 January 2013) and handsearched Headache and Cephalalgia through January 2013.
Selection criteria
Studies were required to be prospective, controlled trials of valproate taken regularly to prevent the occurrence of migraine attacks, to improve migraine‐related quality of life, or both.
Data collection and analysis
Two review authors independently selected studies and extracted data. For headache frequency data, we calculated mean differences (MDs) between valproate and comparator (placebo, active control, or valproate in a different dose) for individual studies and pooled these across studies. For dichotomous data on responders (patients with ≥ 50% reduction in headache frequency), we calculated odds ratios (ORs) and, in select cases, risk ratios (RRs); we also calculated numbers needed to treat (NNTs). We calculated MDs for Migraine Disability Assessment (MIDAS) scores. We also summarised data on adverse events from placebo‐controlled trials and calculated risk differences (RDs) and numbers needed to harm (NNHs).
Main results
Ten papers describing 10 unique trials met the inclusion criteria. Analysis of data from two trials (63 participants) showed that sodium valproate reduced headache frequency by approximately four headaches per 28 days as compared to placebo (MD ‐4.31; 95% confidence interval (CI) ‐8.32 to ‐0.30). Data from four trials (542 participants) showed that divalproex sodium (a stable combination of sodium valproate and valproic acid in a 1:1 molar ratio) more than doubled the proportion of responders relative to placebo (RR 2.18; 95% CI 1.28 to 3.72; NNT 4; 95% CI 2 to 11). One study of sodium valproate (34 participants) versus placebo supported the latter findings (RR for responders 2.83; 95% CI 1.27 to 6.31; NNT 3; 95% CI 2 to 9). There was no significant difference in the proportion of responders between sodium valproate versus flunarizine (one trial, 41 participants) or between divalproex sodium versus propranolol (one trial, 32 participants). Pooled analysis of post‐treatment mean headache frequencies in two trials (88 participants) demonstrates a slight but significant advantage for topiramate 50 mg over valproate 400 mg (MD ‐0.90; 95% CI ‐1.58 to ‐0.22). For placebo‐controlled trials of sodium valproate and divalproex sodium, NNHs for clinically important adverse events ranged from 7 to 14.
Authors' conclusions
Valproate is effective in reducing headache frequency and is reasonably well tolerated in adult patients with episodic migraine.
Plain language summary
Valproate for preventing migraine attacks in adults
Various medicines, collectively termed 'antiepileptics', are used to treat epilepsy. For several years, some of these drugs have also been used for preventing migraine attacks. For the present review, researchers in The Cochrane Collaboration reviewed the evidence about the effects of valproate (valproic acid or sodium valproate or a combination of the two) in adult patients (≥ 16 years of age) with 'episodic' migraine (headache on < 15 days per month). They examined research published up to 15 January 2013 and found 10 relevant studies. Compared with placebo, valproate reduced the frequency of migraine headaches by approximately four per month (two studies, 63 participants). Patients were also more than twice as likely to reduce the number of their migraine headaches by 50% or more with valproate than with placebo (five studies, 576 participants). Side effects associated with valproate were common but generally mild; valproate can, however, cause birth defects and so should be used with caution in women of childbearing age. Further research is needed comparing valproate with other active drugs used for preventing migraine attacks.
Background
Description of the condition
Migraine is a common and disabling health problem among children and predominantly young and middle‐aged adults. Surveys from the main regions of the world suggest that the global prevalence of migraine is 14.7% (18.8% among women and 10.7% among men) (GBD 2010 Study). This disorder results in significant disability and work loss, and several studies have addressed the issue of the costs of migraine. In one of the most recent publications, aggregate direct and indirect costs to society due to migraine among adults in the European Union were estimated to amount to 50 billion Euros (67 billion US dollars) annually, or about 1222 Euros (1634 US dollars) annually per sufferer (Linde 2012).
Description of the intervention
Drug therapy for migraine falls into two categories: acute and preventive. Acute therapy aims at the symptomatic treatment of the head pain and other symptoms associated with an acute attack of migraine. The primary goals of preventive treatment are to reduce attack frequency, severity, and duration. Moreover, such therapy is commonly employed in an attempt to improve responsiveness to acute treatment, enhance functional status, and reduce disability. Evidence‐based guidelines on the drug treatment of migraine have been developed and published by the European Federation of Neurological Societies (EFNS; Evers 2009). These guidelines suggest that prophylactic therapy should be considered for patients with migraine when quality of life, business duties, or school attendance are severely impaired; when the frequency of attacks is two or more per month; when there is a lack of response to acute drug treatment; and when frequent, very long, or uncomfortable auras occur.
This review considers the evidence for the efficacy and tolerability of valproate for preventing episodic migraine in adults. The prophylactic treatment of migraine in children is the subject of a separate Cochrane review (Victor 2003).
Valproic acid (2‐Propylpentanoic acid) was first synthesised in 1882 as analogue of valeric acid, found naturally in valerian. It is a liquid at room temperature, but it can be reacted with a base such as sodium hydroxide to form the salt sodium valproate, which is solid. Valproic acid, sodium valproate, or a mixture of the two (divalproex sodium according to United States Adopted Names (USAN), valproate semisodium according to WHO International Nonproprietary Name (INN) nomenclature) are marketed under various brand names and are collectively referred to as 'valproate' in this review.
Sodium valproate is rapidly absorbed, reaching peak plasma concentrations within one to four hours and thereafter remaining stable for four to 14 hours. After oral administration, 85% to 100% of the administered dose is absorbed. Half‐life is eight to 20 hours in most patients, but may occasionally be much longer. Renal impairment prolongs the half‐life. The relationship between dose, plasma concentration, and effect are incompletely understood. The equilibrium concentration is usually achieved after three to five days of treatment. Sodium valproate is highly protein bound (approximately 90%). The concentration in the cerebrospinal fluid is approximately 10% of plasma concentrations. Sodium valproate is extensively metabolised and excreted in the urine as conjugated metabolites.
How the intervention might work
We use the term 'antiepileptics' here to refer generally to those drugs in common use for the treatment of epilepsy. The pharmacological treatment of epilepsy can be traced back as far as 1857, but the period of greatest development of antiepileptics was between 1935 and 1960, when 13 drugs were developed and marketed (Porter 1992). In recent decades, renewed interest has led to the development of several novel antiepileptics which may confer advantages in tolerability (Dalkara 2012), and these are beginning to be used in migraine also.
The use of antiepileptics for the prophylactic treatment of migraine is theoretically warranted by several known modes of action which relate either to the general modulation of pain systems or more specifically to systems involved in the pathophysiology of migraine (Silberstein 2008; Wiffen 2010). The mechanisms of action of valproate include enhanced neurotransmission of GABA (by inhibiting GABA transaminase) and blockage of voltage‐gated sodium channels and T‐type calcium channels. More than 15 years ago, Cutrer and colleagues identified nine stages of the migraine attack at which valproate might potentially have a beneficial effect (Cutrer 1997), but it is still not possible to state with certainty which particular mode or modes of action of valproate are relevant to the prophylaxis of migraine.
Why it is important to do this review
Some antiepileptic drugs are marketed specifically for migraine prophylaxis, and divalproex sodium has been approved by the US Food and Drug Administration (FDA) for migraine prophylaxis since 1996. The EFNS (Evers 2009) and the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society (Silberstein 2012) list valproic acid among first‐line migraine prophylactics.
There is a fairly substantial body of evidence from controlled trials supporting the efficacy of many of the agents used for preventing migraine, yet such therapies are used by only a small percentage of patients with migraine — 3% to 12% in various studies (Clarke 1996; Edmeads 1993; Mehuys 2012). It is hoped that this review and others like it will increase awareness of migraine prophylactic treatment options and help to provide a systematic basis for making the best possible choice of such therapy in those individuals in need of it.
The present review is part of a series of reviews which, taken together, represent an update of a Cochrane review on 'Anticonvulsant drugs for migraine prophylaxis' (Chronicle 2004; Mulleners 2008; first published in 2004, and previously updated (conclusions not changed) in 2007). The old review has been split into four separate reviews for updating:
Topiramate for the prophylaxis of episodic migraine in adults (Linde 2013a)
Valproate (valproic acid or sodium valproate or a combination of the two) for the prophylaxis of episodic migraine in adults (the present review, Linde 2013b)
Gabapentin or pregabalin for the prophylaxis of episodic migraine in adults (Linde 2013c)
Antiepileptics other than gabapentin, pregabalin, topiramate, and valproate for the prophylaxis of episodic migraine in adults (Linde 2013d)
Objectives
To describe and assess the evidence from controlled trials on the efficacy and tolerability of valproate (valproic acid or sodium valproate or a combination of the two) for preventing migraine attacks in adult patients with episodic migraine.
Methods
Criteria for considering studies for this review
Types of studies
The International Headache Society (IHS) has provided a useful document setting out guidelines for the conduct of clinical trials in migraine, to which current investigators are encouraged to adhere (Tfelt‐Hansen 2012). This document was not used as the sole basis for considering studies in this review, as too many potentially informative past studies would likely have been excluded on methodological grounds. However, many of its recommendations have been used as a basis for what follows.
Included studies were required to be prospective, controlled trials of self administered valproate (valproic acid or sodium valproate or a combination of the two) taken regularly to prevent the occurrence of migraine attacks, to improve migraine‐related quality of life, or both. We included trials only if allocation to treatment groups was randomised or pseudo‐randomised (based on some non‐random process unrelated to the treatment selection or expected response). Blinding was not required. We excluded concurrent cohort comparisons and other non‐experimental designs.
Types of participants
Study participants were required to be adults (at least 16 years of age) and to meet reasonable criteria designed to distinguish migraine from tension‐type headache. If patients with both types of headache were included in a trial, results were required to be stratified by headache diagnosis. We did not require the use of a specific set of diagnostic criteria (eg, Ad Hoc Cttee 1962; IHS Cttee 1988; ICHD‐II 2004), but migraine diagnoses had to be based on at least some of the distinctive features of migraine, eg, nausea/vomiting, severe head pain, throbbing character, unilateral location, phono/photophobia, or aura. Secondary headache disorders had to be excluded using reasonable criteria.
We anticipated that some of the trials identified would include patients described as having mixed migraine and tension‐type headaches or combination headaches, and the protocol for this review described detailed procedures for dealing with such trials. In the end, no such precautions were necessary. We excluded studies evaluating treatments for chronic daily headache, chronic migraine, and transformed migraine. The reasons for this are: (a) the definition of chronic migraine is still heavily debated, and a revision of the 2004 IHS criteria for this condition has been proposed (Olesen 2006); (b) transformed migraine and chronic daily headache, although commonly used terms, are insufficiently validated diagnoses; (c) the separation of these conditions from headache due to medication overuse is not always clear in many studies; and (d) there is some evidence that suggests that chronic migraine may be more refractory to standard prophylactic treatment than episodic migraine. We explicitly excluded trials and treatment groups including only patients with tension‐type headache.
Types of interventions
Included studies were required to have at least one arm in which valproate (valproic acid or sodium valproate or combination of the two, without concomitant use of other migraine prophylactic treatment) was given regularly during headache‐free intervals with the aim of preventing the occurrence of migraine attacks, improving migraine‐related quality of life, or both. Acceptable comparator groups included placebo, no intervention, active drug treatment (ie, with proven efficacy, not experimental), the same drug treatment with a clinically relevant different dose, and non‐pharmacological therapies with proven efficacy in migraine. The analysis included only drugs and dosages that are commercially available.
We recorded any data reported on treatment compliance in the Characteristics of included studies table. After examination of these data, it did not seem necessary to stratify the analysis by compliance.
We anticipated that most trials would permit the use of medication for acute migraine attacks experienced during the trial period. We therefore recorded descriptions of trial rules concerning the use of acute medication in the Characteristics of included studies table whenever such information was provided. We did not otherwise model or adjust for this factor in our analysis.
Types of outcome measures
We collected and analysed trial data on headache frequency, responders (patients with ≥ 50% reduction in headache frequency), quality of life, and adverse events.
Search methods for identification of studies
Search strategies used in our earlier review (Chronicle 2004; Mulleners 2008) are detailed in Appendix 1 (last search date 31 December 2005). For the present update, trained information specialists developed detailed search strategies for each database searched (Appendix 2). The new searches overlapped the old searches by a full year to ensure complete coverage. The last search date for all updated searches was 15 January 2013.
Databases searched for this update were:
Cochrane Central Register of Controlled Trials (CENTRAL; The Cochrane Library 2012, Issue 12; years searched = 2005 to 2012);
MEDLINE (via OVID), 2005 to 15 January 2013;
MEDLINE In‐Process (via OVID), current week, 15 January 2013;
EMBASE (via OVID), 2005 to 15 January 2013.
Additional strategies for identifying trials included searching the reference lists of review articles and included studies, searching books related to headache, and consulting experts in the field. We attempted to identify all relevant published trials, irrespective of language. We handsearched two journals, Headache and Cephalalgia, in their entirety through January 2013.
Data collection and analysis
Selection of studies
Two of us independently screened titles and abstracts of studies identified by the literature search for eligibility. Papers that could not be excluded with certainty on the basis of information contained in the title and/or abstract were retrieved in full for screening. Disagreements were resolved through discussion. We retrieved papers passing this initial screening process, and two of us independently reviewed the full texts. Disagreements at the full‐text stage were resolved through internal discussion and, in a few cases, through correspondence with members of the editorial staff of the Cochrane Pain, Palliative and Supportive Care Review Group. We were not blinded to study investigators' names and institutions, journal of publication, or study results at any stage of the review.
The search strategy described above identified a large number of short conference and journal abstracts. The majority of these either (a) reported partial results of ongoing trials; (b) provided insufficient information on trial design or results; (c) were early reports of included studies; or (d) were reproductions of abstracts of papers published in full (for example, the journal Headache reproduces abstracts of interest to readers, and these are found by PubMed). We agreed that short abstracts of this kind would be excluded from consideration.
Data extraction and management
Two of us independently abstracted information on patients, methods, interventions, efficacy outcomes, and adverse events from the original reports onto specially designed, pre‐tested paper forms. Disagreements were again resolved through discussion.
We anticipated that trials would vary in length, that outcomes would be measured over various units of time (eg, number of attacks per two weeks versus number of attacks per four weeks), and that results would be reported for numerous different time points (eg, four‐week headache frequency at two months versus at four months). We attempted to standardise the unit of time over which headache frequency was measured at 28 days (four weeks) wherever possible. We recorded outcomes beginning four weeks after the start of treatment and continued through all later assessment periods. We made decisions about which time points to include in the final analysis once the data had been collected.
We anticipated that outcomes measured on a continuous scale (eg, headache frequency) would be reported in a variety of ways, eg, as mean pre‐treatment, post‐treatment, and/or change scores. Among change scores, we preferred the mean of within‐patient changes (from baseline to on‐treatment in a parallel‐group trial) over the change in group means because the first both results in a lower variance (taking into account the correlation between baseline and post‐treatment scores in each patient) and adjusts for imbalances in baseline headache frequencies, while the latter has only the second advantage. When neither type of change score was reported, we compared post–treatment means between groups, assuming that baseline data would be balanced due to randomisation. We anticipated that many trials would report group means, without reporting data on the variance associated with these means. In such cases, we attempted to calculate or estimate variances based on primary data, test statistics, and/or error bars in graphs.
When efficacy outcomes were reported in dichotomous form (success/failure), we required that the threshold for distinguishing between treatment success and failure be clinically significant; for example, we interpreted a ≥ 50% reduction in headache frequency as meeting this criterion. In such cases, we recorded, for each treatment arm, the number of patients included in the analysis and the number with each outcome.
The protocol for this review specified rules for dealing with outcome data reported on an ordinal scale (eg, for reduction in headache frequency: 0%, 1% to 24%, 25% to 49%, 50% to 74%, 75% to 99%, 100%) but, in fact, none of the included trials reported ordinal data for outcomes of interest.
We envisaged that the preferred methods of collecting and presenting data on quality of life would most likely be the Migraine‐Specific Questionnaire (MSQ) and the Medical Outcomes Study 36‐item Short‐Form Health Survey (SF‐36). However, other instruments and other types of outcomes related to quality of life (eg, work absenteeism) were not excluded a priori, and these data were kept under review before specifying rules for analysing outcome data in this domain.
We recorded the proportion of patients reporting adverse events for each treatment arm wherever possible. The identity and rates of specific adverse events were also recorded. We anticipated that reporting of adverse events would vary greatly across trials with regard to the terminology used, method of ascertainment, and classification of adverse events as drug‐related or not and as severe or not.
Assessment of risk of bias in included studies
We completed a 'Risk of bias' table for each study, using assessments of random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), and selective reporting (reporting bias). For new studies identified in the present update, two of us completed this assessment independently; for older studies, one of us performed the assessment and a second author reviewed and commented on it. Disagreements were resolved through discussion.
We also assessed the methodological quality of individual trials using the scale devised by Jadad and colleagues (Jadad 1996), operationalised as follows:
Was the study described as randomised? (1 = yes; 0 = no)
Was the method of randomisation well described and adequate? (0 = not described; 1 = described and adequate; ‐1 = described, but not adequate)
Was the study described as double‐blind? (1 = yes; 0 = no)
Was the method of double‐blinding well described and adequate? (0 = not described; 1 = described and adequate; ‐1 = described, but not adequate)
Was there a description of withdrawals and dropouts sufficient to determine the number of patients in each treatment group entering and completing the trial? (1 = yes; 0 = no)
Each trial thus received a score of 0 to 5 points, with higher scores indicating higher quality in the conduct or reporting of the trial. Two review authors scored the studies independently, and a consensus score was then arrived at through discussion. The consensus score is reported for each study in the Characteristics of included studies table and was not used as a weighting in statistical analyses.
Measures of treatment effect
The primary outcome considered for the efficacy analysis was headache frequency. Among headache frequency measures, we preferred number of migraine attacks to number of days with migraine. The latter measure confusingly incorporates attack duration into the measure of headache frequency. Moreover, attack duration is affected by the use of symptomatic medication, which is permitted in most trials. We also analysed headache frequency in terms of a responder rate, or the proportion of patients with a ≥ 50% reduction in headache frequency from pre‐ to post‐treatment.
As noted above (Data extraction and management), we kept patient‐reported quality of life data under review as studies were selected. There were no quality of life data available for rigorous analysis, but one study (Afshari 2012) reported Migraine Disability Assessment (MIDAS) scores.
The analysis considered only outcome data obtained directly from the patient and not those judged by the treating physician or study personnel. Efficacy data based on contemporaneous and timed (usually daily) recording of headache symptoms were preferred to those based on global or retrospective assessments.
In addition, we tabulated adverse events for each included study.
Unit of analysis issues
In the case of cross‐over trial designs, we anticipated that the data reported would normally not permit analysis of paired within‐patient data. We therefore analysed cross‐over trials as if they were parallel‐group trials, combining data from all treatment periods. If a carry‐over effect was found and data were reported by period, then the analysis was restricted to period‐one data only. In no trial were complete within‐patient data reported, so within‐patient improvement scores were not calculated.
Dealing with missing data
Where data were missing or inadequate, we attempted to obtain these data by correspondence with study authors.
Assessment of heterogeneity
We tested estimates of efficacy (both mean differences (MDs) and odds ratios (ORs)) for homogeneity. When significant heterogeneity was present, we made an attempt to explain the differences based on the clinical characteristics of the included studies. We did not statistically combine studies that were clinically dissimilar. However, when a group of studies with statistically heterogeneous results appeared to be clinically similar, we did combine study estimates. We performed all pooled analyses using a random‐effects model.
As a sensitivity analysis, we also planned to calculate a pooled effect estimate using a fixed‐effect model for major outcomes (headache frequency, responder rate, and any AE) when the random‐effects result was near‐significant (0.05 ≤ P ≤ 0.15) and the pooled studies were homogeneous (heterogeneity statistics: P > 0.15/I2 < 30%). Such a sensitivity analysis would evaluate whether conclusions might differ based on the statistical model used for pooling in situations where a fixed‐effect model might reasonably be considered instead of a random‐effects model. In fact, however, no such sensitivity analyses were warranted in the present review.
Data synthesis
We anticipated that continuous outcome measures of headache frequency would be reported on different and often incompatible scales. Although we attempted to standardise the extraction of headache frequency data to a 28‐day (four‐week) period, this was not possible in every case. In our previous review (Chronicle 2004; Mulleners 2008), we therefore analysed these data using the standardised mean difference (SMD, with 95% confidence intervals (CIs)) rather than the mean difference (MD). The introduction of change scores in the newly included studies for some of the reviews in this series necessitated a change in the analysis plan from SMDs to MDs. The latter also has the advantage of giving a result in clinically meaningful units (ie, x fewer migraines per 28 days).
We used dichotomous data meeting our definition of a clinically significant threshold to calculate odds ratios (ORs), with 95% CIs. Although we prefer ORs because of their statistical properties, some readers may find it simpler to interpret the clinical significance of our findings using risk ratios (RRs); we have therefore calculated RRs where appropriate. We additionally computed numbers needed to treat (NNTs), with 95% CIs, as the reciprocal of the risk difference (RD) versus placebo (McQuay 1998).
In the same way, we used data on the proportion of patients reporting adverse events to calculate RDs and numbers needed to harm (NNHs).
Subgroup analysis and investigation of heterogeneity
We undertook subgroup analyses by dose where possible. We considered further subgroup analyses by method of randomisation and by completeness of blinding, but did not undertake them because of insufficient data.
Results
Description of studies
Results of the search
The PubMed search strategy for our previous review (Chronicle 2004; Mulleners 2008) yielded 1089 potentially eligible citations, while the EMBASE and CENTRAL searches yielded 290 and 6952 citations, respectively. No additional citations were retrieved from the Cochrane Pain, Palliative & Supportive Care Trials Register or from other sources. After title and abstract screening, we obtained 58 published papers on antiepileptics for full‐text scrutiny. Of these, 22 (nine included, 13 excluded) investigated valproate.
The MEDLINE search strategy for the present update (from 2005 on) yielded 188 citations as possible candidates for the current series of reviews on antiepileptic drugs for migraine prophylaxis; the search of MEDLINE In‐Process identified an additional 20 citations. The EMBASE and CENTRAL updates identified 484 and 85 citations, respectively. Three additional study reports (all unpublished and all pertaining to gabapentin) were identified from other sources. After title and abstract screening, we obtained 37 published and three unpublished papers on antiepileptics for full‐text scrutiny. Of these, seven (one included, six excluded) investigated valproate.
Thus, for the present update, we reviewed a total of 29 papers on valproate at the full‐text screening stage. Of these, we included 10 papers and excluded 19.
Included studies
The 10 included papers reported data from 10 unique studies, including four trials of divalproex sodium (Freitag 2002; Kaniecki 1997; Klapper 1997; Mathew 1995) and six trials of sodium valproate (Afshari 2012; Hering 1992; Jensen 1994; Kinze 2001; Mitsikostas 1997; Shaygannejad 2006). Six trials compared valproate with placebo (Freitag 2002; Hering 1992; Jensen 1994; Kaniecki 1997; Klapper 1997; Mathew 1995), four compared valproate to active intervention (Afshari 2012; Kaniecki 1997; Mitsikostas 1997; Shaygannejad 2006), and one reported data that enabled dose comparisons of valproate (Kinze 2001).
Four trials (Hering 1992; Jensen 1994; Kaniecki 1997; Shaygannejad 2006) had a cross‐over design, whereas the other six trials had a parallel‐group design (Afshari 2012; Freitag 2002; Kinze 2001; Klapper 1997; Mathew 1995; Mitsikostas 1997).
The doses of valproate investigated in the 10 included trials ranged from 400 to 1500 mg/day. This can be compared to the range of doses used in epilepsy, which is 750 to 4000 mg/day.
The duration of the treatment phase of the included trials varied from eight to 12 weeks, with a mean of 11 weeks.
See the Characteristics of included studies for further details.
Excluded studies
Of the 29 papers obtained for full‐text scrutiny, 19 were excluded for reasons given in the Characteristics of excluded studies table. The most common reasons for exclusion were: no control group (five papers), comparator an experimental intervention (three papers), and review article (two papers).
Risk of bias in included studies
We scored methodological quality using the Jadad scale as indicated in the Assessment of risk of bias in included studies section, with a maximum attainable score of 5. The median quality score was 3.5 (mean 3.2; range 1 to 5).
Of 60 risk of bias items scored for the 10 studies, the majority of ratings were either 'unclear' (23 (38%)) or 'low' (20 (33%)) (Figure 1; Figure 2); we judged seven studies (Afshari 2012; Hering 1992; Jensen 1994; Kaniecki 1997; Kinze 2001; Klapper 1997; Mitsikostas 1997) as having a 'high' risk of bias for at least one item (Figure 2). One of these studies (Kinze 2001) was judged as having a high risk of bias for all six items assessed.
1.
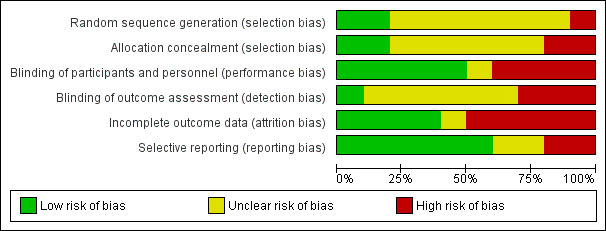
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
2.
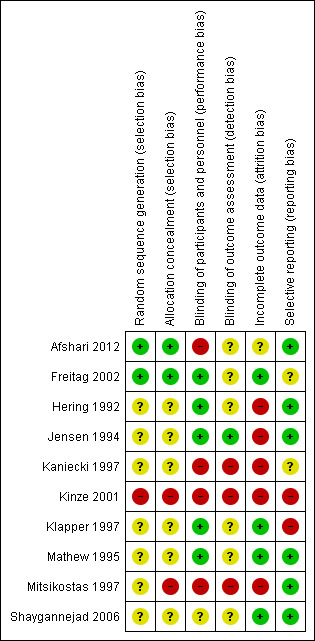
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Only two studies (Afshari 2012; Freitag 2002) provided an adequate methodological description (computer‐generated randomisation schedule) of how allocation sequences were generated (see the Characteristics of included studies table). Likewise, only Afshari 2012 and Freitag 2002 provided an adequate methodological description (preprinted medication code labels and sealed envelopes) of attempts to conceal allocation of intervention assignment (see the Characteristics of included studies table). A high risk of selection bias was valued for Kinze 2001 and Mitsikostas 1997 due to their open‐label design in combination with a lack of description of predefined randomisation schedules.
Blinding
Both participants and clinicians were blinded during the conduct of the majority of studies (7/10), and adequate methodological descriptions are reported for five of them (see Figure 2 and Characteristics of included studies table). Double‐blinding was typically achieved by packaging and labelling identical appearing tablets according to the randomisation codes. In Afshari 2012, there is no mention of identical appearing tablets, and it is thus possible that standard medication was provided by third party according to allocation label. We therefore judged this study as suffering from a high risk of performance bias. In Kaniecki 1997, even the stated single‐blinding is questionable, since divalproex, propranolol, and placebo had different appearances. Kinze 2001 and Mitsikostas 1997 were open‐label studies and therefore also had a high risk of performance bias. In Kaniecki 1997, the single investigator was not blinded until he reviewed the diaries for outcomes assessment. Since the sample of this study was small, and non‐completers were excluded from the analysis, he could possibly have recognised some of the participants and the interventions they were using. Remarkably, no paper clearly stated that the analyst was effectively blinded. The risk of detection bias in all studies is therefore unclear.
Incomplete outcome data
Only in four of the 10 studies was completeness of data adequately reported (Figure 2). Usually in these papers an intention‐to‐treat (ITT) analysis was applied (see the Characteristics of included studies table). We were particularly concerned about incomplete outcome data in Jensen 1994, Kaniecki 1997, Kinze 2001, and Mitsikostas 1997, which considered complete cases only, excluding the other participants from analysis. In addition, Hering 1992 does not report the size of the safety evaluable sample.
Selective reporting
We judged the risk of reporting bias as low in six of the 10 studies (Figure 2). Selective availability of data was encountered in Kaniecki 1997 (nocebo effect not reported, precluding calculation of NNHs), Kinze 2001 (inadequate reporting of adverse events), and Klapper 1997 (dose comparisons not possible, as insufficient data were provided).
Other potential sources of bias
Statistically significant results are more likely to be published than trials affirming a null result. This tendency for negative or inconclusive results to remain unpublished is inherently problematic also in the context of this review.
Effects of interventions
Methodological considerations
Significant statistical heterogeneity was evident across trials for both efficacy outcomes. The clinical similarity of trials was therefore examined to determine whether studies should be combined for statistical meta‐analysis. Although there was methodological variation as described above (Risk of bias in included studies), the included trials were fundamentally similar with regard to basic design, patients, and measures.
All doses reported below are given in terms of mg/day.
Valproate versus placebo
Divalproex sodium
None of the four trials comparing divalproex sodium with placebo (Freitag 2002; Kaniecki 1997; Klapper 1997; Mathew 1995) reported sufficient data for us to calculate mean differences (MDs) for headache frequency, our preferred outcome measure.
All four trials did, however, report data on responders. Analysis of these data showed, overall, that active treatment was significantly superior to placebo for this outcome (odds ratio (OR) 3.34; 95% confidence interval (CI) 1.46 to 7.67; 542 patients (one cross‐over study had 32 patients); Analysis 1.1). In clinical terms, the observed effect suggests that patients are approximately twice as likely to experience a ≥ 50% reduction in headache frequency with divalproex sodium as with placebo. Details are as follows:
1.1. Analysis.
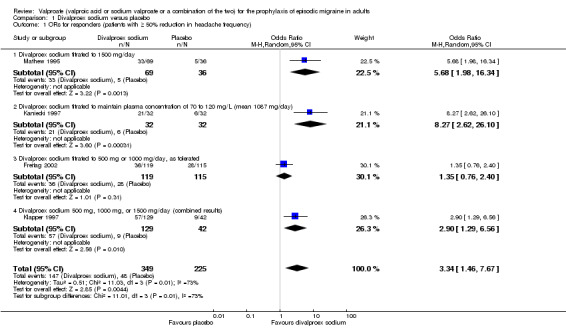
Comparison 1 Divalproex sodium versus placebo, Outcome 1 ORs for responders (patients with ≥ 50% reduction in headache frequency).
The proportion of responders with divalproex sodium was 42% (147/349; range: 30% to 66%);
The proportion of responders with placebo was 21% (48/225; range 14% to 24%);
The risk ratio (RR) for divalproex sodium versus placebo was 2.18 (95% CI 1.28 to 3.72; Analysis 1.2);
The number needed to treat (NNT) for divalproex sodium versus placebo was 4 (95% CI 2 to 11).
1.2. Analysis.
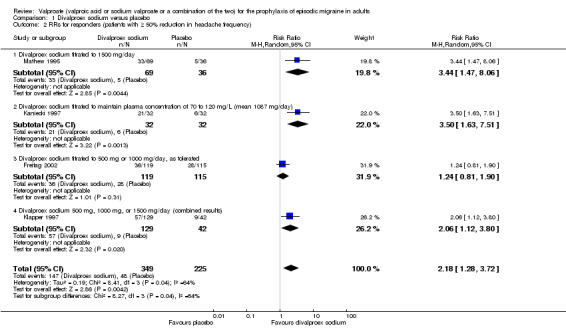
Comparison 1 Divalproex sodium versus placebo, Outcome 2 RRs for responders (patients with ≥ 50% reduction in headache frequency).
It is notable that the largest of the four studies analysed (Freitag 2002; 234 patients) found no significant difference between active treatment and placebo.
Sodium valproate
Two cross‐over trials of sodium valproate (Hering 1992; Jensen 1994; 63 patients) showed a significant reduction in headache frequency (per 28‐day period) in the active group compared to the placebo group (MD ‐4.31; 95% CI ‐8.32 to ‐0.30; Analysis 2.1). In clinical terms, the observed effect corresponds to a reduction in headache frequency of approximately four headaches per 28 days. The mean baseline headache frequency in the valproate group (reported only by Jensen 1994, and only for completers) was 6.1 headaches per 28 days.
2.1. Analysis.
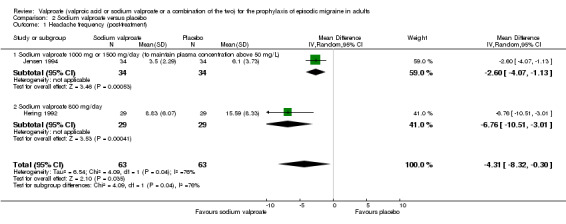
Comparison 2 Sodium valproate versus placebo, Outcome 1 Headache frequency (post‐treatment).
One cross‐over trial (Jensen 1994; 34 patients) reported data on responders; these showed that sodium valproate was significantly superior to placebo for this outcome (OR 4.67; 95% CI 1.54 to 14.14; Analysis 2.2). In clinical terms, the observed effect suggests that patients are nearly three times as likely to experience a ≥ 50% reduction in headache frequency with sodium valproate as with placebo. Details are as follows:
2.2. Analysis.
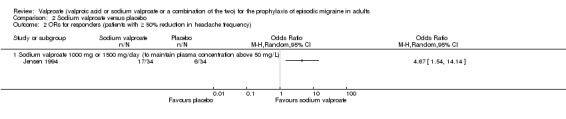
Comparison 2 Sodium valproate versus placebo, Outcome 2 ORs for responders (patients with ≥ 50% reduction in headache frequency).
The proportion of responders with sodium valproate was 50% (17/34);
The proportion of responders with placebo was 18% (6/34);
The RR for sodium valproate versus placebo was 2.83 (95% CI 1.27 to 6.31; Analysis 2.3);
The NNT for sodium valproate versus placebo was 3 (95% CI 2 to 9).
2.3. Analysis.
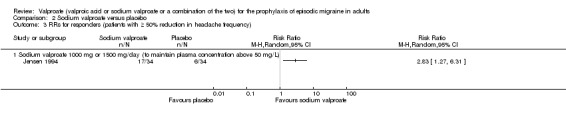
Comparison 2 Sodium valproate versus placebo, Outcome 3 RRs for responders (patients with ≥ 50% reduction in headache frequency).
Dose comparisons for sodium valproate
One parallel‐group trial (Kinze 2001) compared different doses of sodium valproate by measuring serum valproate concentrations. The study showed that lower (21 to 50 µg/ml) serum levels gave rise to slightly but significantly lower headache frequency than higher (> 50 µg/ml) serum levels (MD 0.80; 95% CI 0.24 to 1.36; 45 patients; Analysis 3.1). In clinical terms, the observed effect corresponds to a reduction in headache frequency of approximately one headache per 28 days in the lower versus the higher serum level group. The mean baseline headache frequency (reported only for the study population as a whole) was 3.5 headaches per 28 days.
3.1. Analysis.
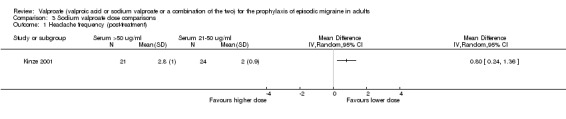
Comparison 3 Sodium valproate dose comparisons, Outcome 1 Headache frequency (post‐treatment).
Sodium valproate versus flunarizine
One parallel‐group trial (Mitsikostas 1997) compared sodium valproate with flunarizine. Data were insufficient for us to calculate MDs for headache frequency, our preferred outcome measure. There was no significant difference between sodium valproate and flunarizine in the proportion of responders (OR 1.07; 95% CI 0.28 to 4.12; 41 patients; Analysis 4.1).
4.1. Analysis.
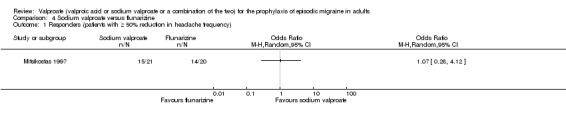
Comparison 4 Sodium valproate versus flunarizine, Outcome 1 Responders (patients with ≥ 50% reduction in headache frequency).
Divalproex sodium versus propranolol
A further (cross‐over) trial using an active comparator examined divalproex sodium versus propranolol (Kaniecki 1997). Data were insufficient for us to calculate MDs for headache frequency, our preferred outcome measure. There was no significant difference between treatments in the proportion of responders (OR 1.15; 95% CI 0.41 to 3.18; 32 patients; Analysis 5.1).
5.1. Analysis.
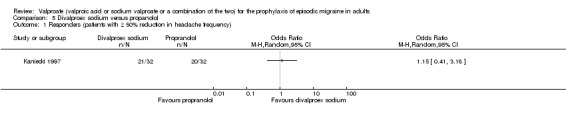
Comparison 5 Divalproex sodium versus propanolol, Outcome 1 Responders (patients with ≥ 50% reduction in headache frequency).
Sodium valproate versus topiramate
Two fairly small studies compared topiramate 50 mg with sodium valproate 400 mg. Afshari 2012 did not demonstrate a significant difference in mean headache frequency during treatment (MD ‐0.60; 95% CI ‐1.57 to 0.37; 56 participants; Analysis 6.1). On the basis of their statistical analysis, the authors of Shaygannejad 2006 found no significant differences in efficacy between the two drugs. However, our analysis of post‐treatment mean headache frequencies demonstrated a slight but significant advantage for topiramate over valproate (MD ‐1.20; 95% CI ‐2.16 to ‐0.24; 32 (cross‐over) participants; Analysis 6.1). The pooled results of these two studies indicate a significant difference between topiramate and sodium valproate, in favour of topiramate, for this outcome (MD ‐0.90; 95% CI ‐1.58 to ‐0.22; Analysis 6.1). In clinical terms, the observed effect corresponds to a reduction in headache frequency of approximately one headache per 28 days with topiramate versus sodium valproate. The median baseline headache frequency in the topiramate groups of the two trials was 6.1 headaches per 28 days (mean 6.1; range: 5.4 to 6.8). It should be noted that the doses used in these two studies are not those used in routine clinical practice for the management of migraine.
6.1. Analysis.
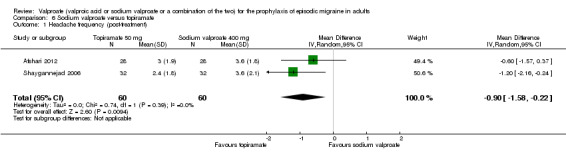
Comparison 6 Sodium valproate versus topiramate, Outcome 1 Headache frequency (post‐treatment).
Afshari 2012 was the only study to report data on migraine‐related disability. These data showed no significant difference in Migraine Disability Assessment (MIDAS) scores between sodium valproate and topiramate (MD ‐3.90; 95% CI ‐8.72 to 0.92; 56 participants; Analysis 6.2).
6.2. Analysis.
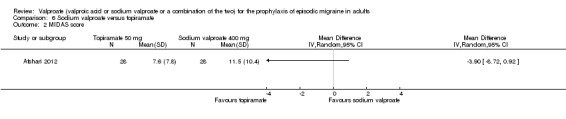
Comparison 6 Sodium valproate versus topiramate, Outcome 2 MIDAS score.
Safety
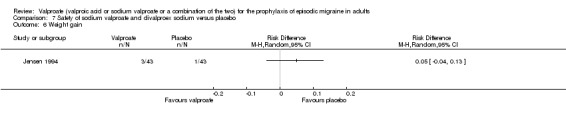
During the process of extracting safety data, it became clear that the range of adverse events and the method of their reporting varied very considerably from trial to trial. Because of the fundamental similarity of sodium valproate and divalproex sodium, safety data from trials of these drugs against placebo were analysed together. We calculated risk differences (RDs) for any adverse event (Analysis 7.1), and for the five specific adverse events we judged to be of greatest clinical importance, namely, asthenia/fatigue (Analysis 7.2), dizziness/vertigo (Analysis 7.3), nausea (Analysis 7.4), tremor (Analysis 7.5), and weight gain (Analysis 7.6). Numbers needed to harm (NNHs) (with 95% CIs) were as follows:
7.1. Analysis.
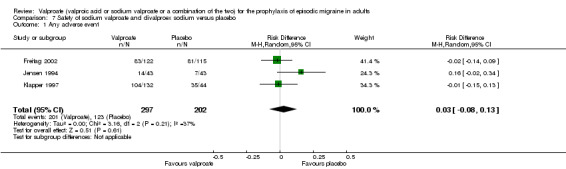
Comparison 7 Safety of sodium valproate and divalproex sodium versus placebo, Outcome 1 Any adverse event.
7.2. Analysis.
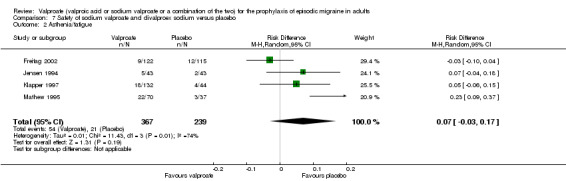
Comparison 7 Safety of sodium valproate and divalproex sodium versus placebo, Outcome 2 Asthenia/fatigue.
7.3. Analysis.
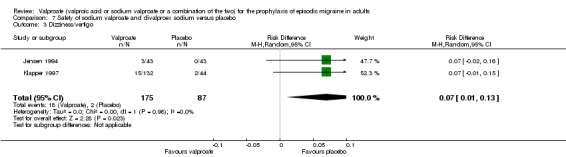
Comparison 7 Safety of sodium valproate and divalproex sodium versus placebo, Outcome 3 Dizziness/vertigo.
7.4. Analysis.
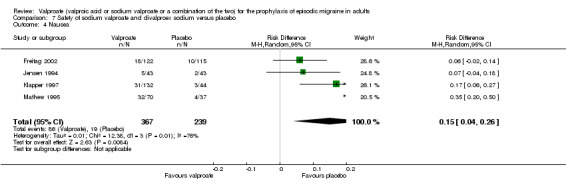
Comparison 7 Safety of sodium valproate and divalproex sodium versus placebo, Outcome 4 Nausea.
7.5. Analysis.
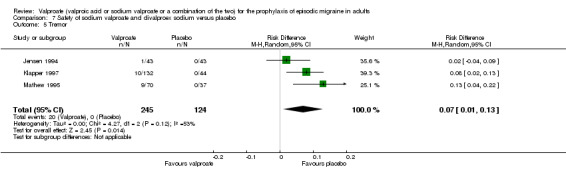
Comparison 7 Safety of sodium valproate and divalproex sodium versus placebo, Outcome 5 Tremor.
7.6. Analysis.
Comparison 7 Safety of sodium valproate and divalproex sodium versus placebo, Outcome 6 Weight gain.
Any adverse event: NNH not calculated, since 95% CI for RD includes zero.
Asthenia/fatigue: NNH not calculated, since 95% CI for RD includes zero.
Dizziness/vertigo: NNH 14 (8 to 100).
Nausea: NNH 7 (4 to 25).
Tremor: NNH 14 (8 to 100).
Weight gain: NNH not calculated, since 95% CI for RD includes zero.
Five of the six placebo‐controlled trials of sodium valproate or divalproex sodium reported unambiguous data on the percentage of patients in active treatment groups who withdrew because of adverse events. These percentages ranged from 8% to 19% (Freitag 2002, 8%; Jensen 1994, 9%; Kaniecki 1997, 11%; Klapper 1997, 19%; Mathew 1995, 13%), with a mean of 12% (median 11%).
Discussion
Summary of main results
Placebo‐controlled trials
Meta‐analysis of the studies included in this review suggests that valproate is efficacious for the prophylaxis of migraine. Mean headache frequency was significantly reduced (by approximately four headaches per month) with sodium valproate as compared to placebo (two studies contributed to this analysis, one of which reported a baseline frequency of six headaches per month). Furthermore, and perhaps of greater clinical relevance (though less informative scientifically), patients were more than twice as likely to have a ≥ 50% reduction in headache frequency with divalproex sodium than with placebo (four studies contributed to this analysis). Supporting the latter finding, one small study showed that patients were nearly three times as likely to experience a ≥ 50% reduction in headache frequency with sodium valproate as with placebo.
Dose comparisons
The data included did not demonstrate a direct dose‐response relationship.
Trials with active comparators
The four trials using active comparators found (a) no significant difference in efficacy between sodium valproate and flunarizine (Mitsikostas 1997); (b) no significant difference in efficacy between divalproex sodium and propranolol (Kaniecki 1997); and (c) a slight but significant advantage of topiramate over valproate (pooled results of Afshari 2012 and Shaygannejad 2006).
Safety
Valproate does not appear to give rise to an unexpectedly high rate of adverse events when used for migraine prophylaxis, although nausea is clearly a problem when trials of sodium valproate and divalproex sodium are considered together.
Overall completeness and applicability of evidence
The studies identified were sufficient to address all of the objectives of the review. Our analysis demonstrates that valproate is efficacious for preventing attacks in adult patients with episodic migraine, and these results fit into the context of current practice. The trials with active comparator are of relevance since all three comparators have demonstrable efficacy in the prophylaxis of migraine (Edvinsson 2010; Linde 2004; Reveiz‐Herault 2003).
Several important issues need to be taken into account in any assessment of the efficacy of a drug for migraine prophylaxis. Diagnostic criteria, baseline headache frequency, washout periods for previous medication, rules for rescue medication, and the statistical power of the comparison were handled very variably in the 10 included studies. As investigations of the efficacy of various agents become more commonplace, it seems increasingly important that scientists and clinicians are at least aware of the trial guidelines suggested by the International Headache Society (Tfelt‐Hansen 2012). Even if these guidelines cannot — for operational or scientific reasons — be adhered to in their entirety, they provide a useful consultative framework at the early stages of trial design.
Quality of the evidence
The identified body of evidence allows a robust conclusion of an overall superiority of valproate over placebo with regard to reduction of mean headache frequency (two trials, 126 participants) and the proportion of responders (five trials, 576 participants). These relatively straightforward results should be viewed with some caution. As usual in the context of clinical trials research, there is considerable heterogeneity in both headline results and general levels of analytic and statistical sophistication. It is fair to say that we faced several difficulties in deriving adequate information from the results of the 10 included studies. It is appropriate, therefore, to review a number of caveats. The largest trial of divalproex sodium (Freitag 2002) did not report sufficient data for us to calculate mean differences (MDs) for headache frequency (means were reported, but not standard deviations (SDs)), but the analysis reported by the study investigators demonstrated a statistically significant (P = 0.006) difference favouring active treatment over placebo for this outcome. The clinical relevance of this effect was, however, less compelling, as both the investigators' analysis and our own found no significant difference between treatments in the proportion of responders (patients with ≥ 50% reduction in headache frequency). The finding of Kinze 2001, that lower serum valproate levels produced lower headache frequency than higher serum levels, is somewhat counterintuitive, has not been replicated, and should be regarded as preliminary. It should be noted that all three trials with active comparator are potentially problematic for several reasons including lack of blinding. Further well‐designed trials of valproate against other active drugs and non‐pharmacological interventions are thus desirable.
Potential biases in the review process
Of 60 risk of bias items scored for the 10 studies, the majority of ratings were either 'unclear' (23 (38%)) or 'low' (20 (33%)) (Figure 1; Figure 2). As described in detail above (Risk of bias in included studies), we judged seven trials as having a 'high' risk of bias for at least one item, as follows: random sequence generation (Kinze 2001), allocation concealment (Kinze 2001; Mitsikostas 1997), blinding of participants and personnel (Afshari 2012; Kaniecki 1997; Kinze 2001; Mitsikostas 1997), blinding of outcome assessment (Kaniecki 1997; Kinze 2001; Mitsikostas 1997), incomplete outcome data (Hering 1992; Jensen 1994; Kaniecki 1997; Kinze 2001; Mitsikostas 1997), and/or selective reporting (Kinze 2001; Klapper 1997) (Figure 2). A strength of this review is that the methods used for searching and study selection make it highly likely that the absolute majority of relevant trial results in the public domain were identified. There is nevertheless an obvious risk that the reports of some trials may have been classified and thus remain unobtainable.
Agreements and disagreements with other studies or reviews
The overall conclusion in this review, that valproate is efficacious for preventing attacks in adult patients with episodic migraine, is well in line with guideline recommendations of the EFNS (Evers 2009) and the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society (Silberstein 2012).
Authors' conclusions
Implications for practice.
Bearing in mind the limitations invoked by the methodological and reporting issues mentioned above, this review nevertheless helps to provide a rational framework for the application of valproate for the preventive management of migraine headache in clinical practice. Valproate has been investigated in 10 independent clinical trials, the results of which are generally consistent. It can be concluded from this review that valproate is of proven efficacy in migraine prevention and is suitable for routine clinical use. It must be stressed, however, that this review does not provide definite evidence for the efficacy of valproate in the management of other aspects of the condition (eg, prodromal symptoms, aura symptoms). Likewise, the conclusions in this review cannot be extrapolated to chronic migraine, transformed migraine, or chronic daily headache. None of these conditions was considered for this review, as properly validated definitions are as yet lacking.
Although adverse events were reported by a large proportion of migraine patients treated with valproate, these were usually mild and of a non‐serious nature. Thus it can be concluded that valproate is reasonably well tolerated. One important caveat should be noted: valproate is known to be teratogenic (Morrell 2003), and appropriate caution must accordingly be used when prescribing to women of childbearing age.
Implications for research.
There is a need for more studies designed specifically to compare the efficacy or safety of valproate to other interventions with proven efficacy in the prophylaxis of migraine. Also needed are (a) better studies of dose versus effect; (b) studies of which patients do and do not respond, and why; (c) long‐term studies; and (d) studies post‐withdrawal of valproate after effective use for several months.
Future trialists should also be encouraged to follow the recommendations of the International Headache Society (Tfelt‐Hansen 2012) with regard to both trial design and reporting of data.
Little is definitely known about the mechanism of action of valproate in migraine prophylaxis. A considerable amount of basic science research in both animal models and human neuroscience laboratories will be necessary in order to discover which of the many potential actions of this drug are causative in the reduction of headache frequency.
What's new
| Date | Event | Description |
|---|---|---|
| 1 July 2016 | Review declared as stable | See Published notes. |
History
Review first published: Issue 6, 2013
| Date | Event | Description |
|---|---|---|
| 8 May 2014 | Amended | Minor edit made to numbers reported in Results of the search. |
| 20 June 2013 | New citation required but conclusions have not changed | Conclusions regarding valproate essentially unchanged. |
| 20 June 2013 | New search has been performed | Searches updated on 15 January 2013. One new included study added (Afshari 2012). |
| 26 August 2008 | Amended | Converted to new review format. |
| 11 May 2007 | New search has been performed | May 2007 (Issue 3, 2007):
|
Notes
An updated search in May 2016 identified two relevant studies (Chitsaz 2012 and Facco 2013). However, we did not identify any potentially relevant studies likely to change the conclusions. Therefore, this review has now been stabilised following discussion with the authors and editors. If appropriate, we will update the review if new evidence likely to change the conclusions is published, or if standards change substantially which necessitate major revisions.
Chitsaz, A., M. R. Najafi, et al. (2012). "Pizotifen in migraine prevention: A comparison with sodium valproate." Neurology Asia 17(4): 319‐324.
Facco, E., A. Liguori, et al. (2013). "Acupuncture versus valproic acid in the prophylaxis of migraine without aura: A prospective controlled study." Minerva Anestesiologica 79(6): 634‐642.
Acknowledgements
Professor EP Chronicle, PhD, sadly passed away on 9 February 2007. We wish to acknowledge Professor Chronicle's major contribution and tremendous effort in compiling all statistical analyses and much of the text of the original review on antiepileptics (Chronicle 2004; Mulleners 2008). Without his relentless dedication it would have never seen the light of day.
The protocol for the original review was developed while Dr Chronicle was a Visiting Scholar at the University of California, Berkeley. Dr Sally Hollis, Lancaster University, and Dr Kentaro Hayashi, University of Hawaii at Manoa, provided helpful advice on statistical matters. Several pharmaceutical companies kindly provided information about trials in progress.
We thank Ruth Foxlee, Jane Hayes, and Joanne Abbott for assistance in designing search strategies and running searches; Prof Timothy Steiner for editorial guidance; and Dr Rebecca Gray for editorial assistance and technical support.
Lifting The Burden: the Global Campaign against Headache and the International Headache Society provided financial support for the editorial process (see Sources of support).
Appendices
Appendix 1. Search strategies for the previous review
For the identification of studies considered for the original review and the 2007 update (Chronicle 2004; Mulleners 2008), detailed search strategies were developed for each database searched. These were based on the search strategy for PubMed, but revised appropriately for each database. The search strategies combined the subject searches described below with the Cochrane highly sensitive search strategy for RCTs current at the time (Alderson 2004). The subject searches used a combination of controlled vocabulary and free‐text terms based on the search strategy for PubMed presented below.
Databases searched were:
Cochrane Pain, Palliative & Supportive Care Trials Register;
Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library 2005, Issue 3);
PubMed 1966 to 31 December 2005;
EMBASE 1974 to 31 December 2005.
Additional strategies for identifying trials included searching the reference lists of review articles and included studies, searching books related to headache and consulting experts in the field. Two journals, Headache and Cephalalgia, were handsearched in their entirety, through April 2006.
Detailed descriptions of the subject search strategies used for PubMed, EMBASE, and CENTRAL are given below.
PubMed
Phase 1
#1 (randomized controlled trial [pt] OR controlled clinical trial [pt] OR randomized controlled trials [mh] OR random allocation [mh] OR double‐blind method [mh] OR single‐blind method [mh] OR clinical trial [pt] OR clinical trials [mh] OR ("clinical trial" [tw]) OR ((singl* [tw] OR doubl* [tw] OR trebl* [tw] OR tripl* [tw]) AND (mask* [tw] OR blind* [tw])) OR (placebos [mh] OR placebo* [tw] OR random* [tw] OR research design [mh:noexp] OR comparative study [mh] OR evaluation studies [mh] OR follow‐up studies [mh] OR prospective studies [mh] OR control* [tw] OR prospectiv* [tw] OR volunteer* [tw]) NOT (animals [mh] NOT human [mh]) Limits: Humans
Phase 2
#2 HEADACHE Field: MeSH Terms, Limits: Humans #3 HEADACHE DISORDERS Field: MeSH Terms, Limits: Humans #4 headache* OR migrain* OR cephalgi* OR cephalalgi* Field: All Fields, Limits: Humans #5 #2 OR #3 OR #4 Limits: Humans
Phase 3
#6 anticonvulsant* OR antiepileptic* OR acetazolamide OR carbamazepine OR chlormethiazole OR clobazam OR clonazepam OR clorazepate OR diazepam OR divalproex OR ethosuximide OR felbamate OR fosphenytoin OR gabapentin OR lamotrigine OR levetiracetam OR lidocaine OR lignocaine OR lorazepam OR mephobarbital OR methsuximide OR midazolam OR nitrazepam OR oxcarbazepine OR paraldehyde OR pentobarbital OR phenobarbital OR phenytoin OR primidone OR valproate OR tiagabine OR topiramate OR valproic OR vigabatrin OR zonisamide Field: All Fields, Limits: Humans #7 #1 AND #5 AND #6
EMBASE
#1 'migraine'/exp AND [embase]/lim #2 migrain* OR cephalgi* OR cephalalgi* AND [embase]/lim #3 headache*:ti #4 #1 OR #2 OR #3 #5 'anticonvulsive agent'/de AND [embase]/lim #6 anticonvulsant* OR antiepileptic* OR 'acetazolamide'/de OR 'carbamazepine'/de OR 'chlormethiazole'/de OR 'clobazam'/de OR 'clonazepam'/de OR 'clorazepate'/de OR 'diazepam'/de OR 'divalproex'/de OR 'ethosuximide'/de OR 'felbamate'/de OR fosphenytoin OR 'gabapentin'/de OR 'lamotrigine'/de OR 'levetiracetam'/de OR 'lidocaine'/de OR 'lignocaine'/de OR 'lorazepam'/de OR 'mephobarbital'/de OR 'methsuximide'/de OR 'midazolam'/de OR 'nitrazepam'/de OR 'oxcarbazepine'/de OR 'paraldehyde'/de OR 'pentobarbital'/de OR 'phenobarbital'/de OR 'phenytoin'/de OR 'primidone'/de OR 'valproate'/de OR 'tiagabine'/de OR 'topiramate'/de OR valproic OR 'vigabatrin'/de OR 'zonisamide'/de AND [embase]/lim #7 #5 OR #6 #8 #4 AND #7 #9 ((random*:ti,ab) OR (factorial*:ab,ti) OR (crossover*:ab,ti OR 'cross over':ab,ti OR 'cross over':ab,ti) OR (placebo*:ab,ti) OR ('double blind' OR 'double blind') OR ('single blind':ab,ti OR 'single blind':ab,ti) OR (assign*:ti,ab OR allocat*:ti,ab) OR (volunteer*:ab,ti) OR ('randomized controlled trial'/exp AND [embase]/lim) OR ('single blind procedure'/exp AND [embase]/lim) OR ('double blind procedure'/exp AND [embase]/lim) OR ('crossover procedure'/exp AND [embase]/lim)) NOT ((animal/ OR nonhuman/ OR 'animal'/de AND experiment/ AND [embase]/lim) NOT ((human/ AND [embase]/lim) AND (animal/ OR nonhuman/ OR 'animal'/de AND experiment/ AND [embase]/lim)) AND [embase]/lim) AND [embase]/lim #10 #8 AND #9
CENTRAL
(migrain* OR headache*) AND (randomized controlled trial OR controlled clinical trial) Field: All Fields
Appendix 2. Search strategies for this update
CENTRAL
#1 MeSH descriptor: [Migraine Disorders] explode all trees #2 (migrain* or cephalgi* or cephalalgi*) #3 #1 or #2 #4 MeSH descriptor: [Anticonvulsants] explode all trees #5 (anticonvulsant* or antiepileptic* or acetazolamide or carbamazepine or chlormethiazole or clobazam or clonazepam or clorazepate or diazepam or divalproex or ethosuximide or felbamate or fosphenytoin or gabapentin or lamotrigine or levetiracetam or lidocaine or lignocaine or lorazepam or mephobarbital or methsuximide or midazolam or nitrazepam or oxcarbazepine or paraldehyde or pentobarbital or phenobarbital or phenytoin or primidone or valproate or tiagabine or topiramate or valproic or vigabatrin or zonisamide or eslicarbazepine or lacosamide or perampanel or phenobarbitone or pregabalin or retigabine or rufinamide or stiripentol or *barbit*) #6 #4 or #5 #7 #3 and #6 (search limited to years 2005‐2012)
MEDLINE and MEDLINE In‐Progress (via Ovid)
exp Migraine Disorders/
(migrain* or cephalgi* or cephalalgi*).tw.
or/1‐2
exp Anticonvulsants/
(anticonvulsant* or antiepileptic* or acetazolamide or carbamazepine or chlormethiazole or clobazam or clonazepam or clorazepate or diazepam or divalproex or ethosuximide or felbamate or fosphenytoin or gabapentin or lamotrigine or levetiracetam or lidocaine or lignocaine or lorazepam or mephobarbital or methsuximide or midazolam or nitrazepam or oxcarbazepine or paraldehyde or pentobarbital or phenobarbital or phenytoin or primidone or valproate or tiagabine or topiramate or valproic or vigabatrin or zonisamide or eslicarbazepine or lacosamide or perampanel or phenobarbitone or pregabalin or retigabine or rufinamide or stiripentol or $barbit$).tw.
or/4‐5
3 and 6
randomized controlled trial.pt.
controlled clinical trial.pt.
randomized.ab.
placebo.ab.
clinical trials as topic.sh.
randomly.ab.
trial.ti.
or/8‐14
exp animals/ not humans.sh.
15 not 16
7 and 17
For MEDLINE: limited 18 to yr="2005 ‐Current" For MEDLINE In‐Process: searched current week on 15 January 2013
EMBASE (via Ovid)
exp Migraine/
(migrain* or cephalgi* or cephalalgi*).tw.
or/1‐2
exp Anticonvulsants/
(anticonvulsant* or antiepileptic* or acetazolamide or carbamazepine or chlormethiazole or clobazam or clonazepam or clorazepate or diazepam or divalproex or ethosuximide or felbamate or fosphenytoin or gabapentin or lamotrigine or levetiracetam or lidocaine or lignocaine or lorazepam or mephobarbital or methsuximide or midazolam or nitrazepam or oxcarbazepine or paraldehyde or pentobarbital or phenobarbital or phenytoin or primidone or valproate or tiagabine or topiramate or valproic or vigabatrin or zonisamide or eslicarbazepine or lacosamide or perampanel or phenobarbitone or pregabalin or retigabine or rufinamide or stiripentol or $barbit$).tw.
or/4‐5
3 and 6
random$.tw.
factorial$.tw.
crossover$.tw.
cross over$.tw.
cross‐over$.tw.
placebo$.tw.
(doubl$ adj blind$).tw.
(singl$ adj blind$).tw.
assign$.tw.
allocat$.tw.
volunteer$.tw.
Crossover Procedure/
double‐blind procedure.tw.
Randomized Controlled Trial/
Single Blind Procedure/
or/8‐22
(animal/ or nonhuman/) not human/
23 not 24
7 and 25
limit 26 to yr="2005 ‐Current"
Data and analyses
Comparison 1. Divalproex sodium versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 ORs for responders (patients with ≥ 50% reduction in headache frequency) | 4 | 574 | Odds Ratio (M‐H, Random, 95% CI) | 3.34 [1.46, 7.67] |
| 1.1 Divalproex sodium titrated to 1500 mg/day | 1 | 105 | Odds Ratio (M‐H, Random, 95% CI) | 5.68 [1.98, 16.34] |
| 1.2 Divalproex sodium titrated to maintain plasma concentration of 70 to 120 mg/L (mean 1087 mg/day) | 1 | 64 | Odds Ratio (M‐H, Random, 95% CI) | 8.27 [2.62, 26.10] |
| 1.3 Divalproex sodium titrated to 500 mg or 1000 mg/day, as tolerated | 1 | 234 | Odds Ratio (M‐H, Random, 95% CI) | 1.35 [0.76, 2.40] |
| 1.4 Divalproex sodium 500 mg, 1000 mg, or 1500 mg/day (combined results) | 1 | 171 | Odds Ratio (M‐H, Random, 95% CI) | 2.90 [1.29, 6.56] |
| 2 RRs for responders (patients with ≥ 50% reduction in headache frequency) | 4 | 574 | Risk Ratio (M‐H, Random, 95% CI) | 2.18 [1.28, 3.72] |
| 2.1 Divalproex sodium titrated to 1500 mg/day | 1 | 105 | Risk Ratio (M‐H, Random, 95% CI) | 3.44 [1.47, 8.06] |
| 2.2 Divalproex sodium titrated to maintain plasma concentration of 70 to 120 mg/L (mean 1087 mg/day) | 1 | 64 | Risk Ratio (M‐H, Random, 95% CI) | 3.5 [1.63, 7.51] |
| 2.3 Divalproex sodium titrated to 500 mg or 1000 mg/day, as tolerated | 1 | 234 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [0.81, 1.90] |
| 2.4 Divalproex sodium 500 mg, 1000 mg, or 1500 mg/day (combined results) | 1 | 171 | Risk Ratio (M‐H, Random, 95% CI) | 2.06 [1.12, 3.80] |
Comparison 2. Sodium valproate versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Headache frequency (post‐treatment) | 2 | 126 | Mean Difference (IV, Random, 95% CI) | ‐4.31 [‐8.32, ‐0.30] |
| 1.1 Sodium valproate 1000 mg or 1500 mg/day (to maintain plasma concentration above 50 mg/L) | 1 | 68 | Mean Difference (IV, Random, 95% CI) | ‐2.60 [‐4.07, ‐1.13] |
| 1.2 Sodium valproate 800 mg/day | 1 | 58 | Mean Difference (IV, Random, 95% CI) | ‐6.76 [‐10.51, ‐3.01] |
| 2 ORs for responders (patients with ≥ 50% reduction in headache frequency) | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Sodium valproate 1000 mg or 1500 mg/day (to maintain plasma concentration above 50 mg/L) | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 RRs for responders (patients with ≥ 50% reduction in headache frequency) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 Sodium valproate 1000 mg or 1500 mg/day (to maintain plasma concentration above 50 mg/L) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 3. Sodium valproate dose comparisons.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Headache frequency (post‐treatment) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 4. Sodium valproate versus flunarizine.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Responders (patients with ≥ 50% reduction in headache frequency) | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected |
Comparison 5. Divalproex sodium versus propanolol.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Responders (patients with ≥ 50% reduction in headache frequency) | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected |
Comparison 6. Sodium valproate versus topiramate.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Headache frequency (post‐treatment) | 2 | 120 | Mean Difference (IV, Random, 95% CI) | ‐0.90 [‐1.58, ‐0.22] |
| 2 MIDAS score | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 7. Safety of sodium valproate and divalproex sodium versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Any adverse event | 3 | 499 | Risk Difference (M‐H, Random, 95% CI) | 0.03 [‐0.08, 0.13] |
| 2 Asthenia/fatigue | 4 | 606 | Risk Difference (M‐H, Random, 95% CI) | 0.07 [‐0.03, 0.17] |
| 3 Dizziness/vertigo | 2 | 262 | Risk Difference (M‐H, Random, 95% CI) | 0.07 [0.01, 0.13] |
| 4 Nausea | 4 | 606 | Risk Difference (M‐H, Random, 95% CI) | 0.15 [0.04, 0.26] |
| 5 Tremor | 3 | 369 | Risk Difference (M‐H, Random, 95% CI) | 0.07 [0.01, 0.13] |
| 6 Weight gain | 1 | Risk Difference (M‐H, Random, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Afshari 2012.
| Methods | Prospective, randomised, double‐blind, parallel‐group trial. The study consisted of a 4‐week baseline period (possibly retrospective) and a prospective treatment period of 12 weeks Discontinuation rate: sodium valproate 22%, topiramate 30% Compliance (adherence) data: not available Rule for use of acute medication: during the acute attacks, patients were allowed to use acetaminophen, NSAIDs, ergotamine, triptans, and opioids. Dosing frequency not limited Methodological quality score: 3 |
|
| Participants | Inclusion: migraine with or without aura according to ICHD‐II; migraine onset at least 6 months prior to study and before age 50; migraine frequency 4 to 10 attacks per month; attacks separated by 48 h pain‐free interval. Ages 18 to 65. Non‐pregnant, non‐lactating, adequate contraception. Migraine prophylaxis withdrawn at least 1 month prior to study entry Exclusion: non‐migraine headaches; > 8 treatment days/month of ergots, NSAIDs, or triptans. No rule reported for exclusion of CDH. Other exclusions: alcohol/drug dependence. Hemiplegic, basilar, or ophthalmoplegic migraine. Serious medical conditions Setting: single‐centre Country: Iran Intention‐to‐treat analysis of 56 patients. Of these, 9 had migraine with aura and 47 migraine without aura (ie, not stated that some had both). 44 females and 12 males included in the ITT analysis; mean age among ITT participants treated with sodium valproate 29.2 ± 9.6; mean age among ITT participants treated with topiramate 32.1 ± 10.2. 36 allocated to receive sodium valproate; 40 allocated to receive topiramate |
|
| Interventions | Sodium valproate 400 mg/day versus topiramate 50 mg/day (12 weeks). Sodium valproate initiated with 200 mg/day for 1 week, thereafter 400 mg/day until study end. Dosing frequency not stated. Topiramate initiated with 25 mg/day for 1 week, thereafter 50 mg/day until study end. Dosing frequency not stated | |
| Outcomes | Headache frequency (4 weeks). Headache severity. Duration of episode. Weight. MIDAS at baseline and 8 weeks. HIT‐6 at baseline and 8 weeks. Responder rate Time point(s) considered in the review: last (third) month of double‐blind phase for frequency; entire double‐blind phase for MIDAS |
|
| Notes | A migraine attack persisting longer than 72 hours was counted as a new distinct migraine period. This outcome measure runs the risk of confounding reductions in migraine frequency with reductions in attack duration. Since it is unclear if the baseline was prospective, change scores from baseline were excluded from the analyses of this review. Complementary information requested by email (twice) and ordinary letter (once) but not provided by corresponding author Funders of the trial: Kermanshah University of Medical Sciences, Iran |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation schedule |
| Allocation concealment (selection bias) | Low risk | Medication prescribed with preprinted medication code labels |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Stated that both participants and clinicians were blinded by the use of preprinted medication code labels. However, there is no mention of equally appearing tablets. It is thus possible that standard medication was provided by third party according to allocation label |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 20 randomised patients did not contribute to the ITT analysis: 8 AEs; 10 lack of efficacy (whereof 8 were allocated to topiramate); 2 moved |
| Selective reporting (reporting bias) | Low risk | No suspicion of selective reporting of outcomes, time points, or analyses |
Freitag 2002.
| Methods | Prospective, randomised, double‐blind, parallel trial. 5 half‐lives washout period for previous migraine prophylactic medication. 4‐week baseline period. Duration of treatment: 2 weeks titration then 10 weeks stable dosage Discontinuation rate: dropout 17% for active treatment; 12% for placebo Compliance (adherence) data: compliance, defined as "generally took study drug as directed", 75% for active treatment, 74% for placebo Rule for use of acute medication: was permitted but restrictions not reported Methodological quality score: 5 |
|
| Participants | Inclusion: migraine according to ICHD‐I; migraine onset more than 6 months before screening; average of 2 or more attacks per month in the 3 months before screening Exclusion: secondary headaches were adequately excluded. Neither daily headache nor analgesic overuse headache were adequately excluded. Other exclusions: pregnancy, lactation, inadequate contraception, more than 15 headache days per month, cluster headache, previous adequate treatment with sodium valproate or divalproex sodium, significant CNS disorder, failed more than 2 adequate trials of migraine prophylactic medication Setting: multicentre Country: USA Intention‐to‐treat analysis of 237 migraine patients. 229 had had attacks without aura; 86 had had attacks with aura (since migraine onset). 187 females and 50 males; age range 16 to 69. 122 received active treatment and 115 received placebo |
|
| Interventions | Divalproex sodium versus placebo (12 weeks). Dosage titrated up to 1000 mg/day then maintained at 1000 mg/day for 10 weeks, or 500 mg/day if higher dose could not be tolerated (14% of active group) | |
| Outcomes | Number of migraine attacks per 28 days. Number of migraine days per 28 days Time point(s) considered in the review: entire 3‐month treatment phase |
|
| Notes | Funders of the trial: Abbott Laboratories | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation schedule, which assigned a unique series of randomised (in a 1:1 ratio) subject numbers to each centre, was computer‐generated by Abbott Laboratories Department of Clinical Statistics prior to study initiation |
| Allocation concealment (selection bias) | Low risk | The randomisation schedule was used by Abbott Laboratories Investigational Drugs Services Department to package and label the study medication containers. Randomisation was accomplished by instructing investigators to assign the subject numbers in ascending numerical sequence as subjects qualified for randomisation. Treatment assignments were provided to the clinical sites in sealed envelopes that could have been opened if needed in an emergency. The integrity of these envelopes was verified at each clinical monitoring visit |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Both clinicians and participants were blinded. Placebo tablets were identical (grey, ovaloid) to active tablets |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis includes all randomised participants |
| Selective reporting (reporting bias) | Unclear risk | The information is not sufficient to come up with precise enough estimates to include mean migraine frequency in this meta‐analysis. Only the 95% CI of the difference between (but not the SDs for) the changes in mean migraine frequency from baseline are given. The responder ratios are usable in this meta‐analysis |
Hering 1992.
| Methods | Prospective, randomised, double‐blind, single cross‐over trial. 2‐week washout period for previous migraine prophylactic medication. No baseline period. Total duration: 16 weeks Discontinuation rate: dropout 3.1% for active treatment; 6.3% for placebo Compliance (adherence) data: compliance assessed by pill count and blood valproate levels, but pill count data not reported Rule for use of acute medication: patients' normal analgesics permitted Methodological quality score: 4 |
|
| Participants | Inclusion: Ad Hoc Committee criteria; migraine onset more than 2 years prior to screening; at least 4 attacks per month for 2 years. No information about mixed or combination headaches Exclusion: secondary headaches were adequately excluded. It is not reported whether daily headaches were excluded. Analgesic overuse headaches were not adequately excluded. Other exclusions: contraindications to valproate, renal or hepatic abnormality, psychiatric disorder, pregnancy or reproductive intentions, change in use of oral contraception, alcohol or drug abuse, participation in another headache study, other chronic medication use Setting: single headache clinic Country: Israel 32 migraine patients participated. Demographic data available on the 29 who completed the trial. 4 had migraine with aura, and 25 migraine without aura. 23 females and 6 males; age range 18 to 54 years |
|
| Interventions | Sodium valproate versus placebo (8 weeks). Dosage: 800 mg/day | |
| Outcomes | Number of migraine attacks per 8 weeks. Sum of individual attack severity (1 to 3) per 8 weeks. Sum of individual attack duration (hours) per 8 weeks Time point(s) considered in the review: entire 8‐week treatment phase |
|
| Notes | Funders of the trial: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Description of method for random sequence generation is lacking |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Both clinicians and participants were blinded. Placebo had same appearance as verum |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | High risk | AEs reported but number of safety evaluable participants on each drug unclear |
| Selective reporting (reporting bias) | Low risk | No suspicion of selective reporting of outcomes, time points, or analyses |
Jensen 1994.
| Methods | Prospective, randomised, double‐blind, single cross‐over trial. Total duration 32 weeks. 4‐week medication‐free run‐in period; 12‐week treatment period; 4‐week washout period; 12‐week treatment period Discontinuation rate: dropout 21% Compliance (adherence) data: compliance data available only as mean blood valproate levels Rule for use of acute medication: patients' usual treatment permitted Methodological quality score: 4 |
|
| Participants | Inclusion: migraine according to ICHD‐I; migraine onset more than 1 year prior to study; 2 to 10 days with migraine per month Exclusion: secondary and daily headaches were adequately excluded. The criteria for excluding analgesic overuse headache were vague. Other exclusions: cluster headache, trigeminal neuralgia, other neurological or psychiatric disease, other migraine prophylaxis, drug dependency, previous participation in more than 2 migraine drug trials Setting: single headache clinic Country: Denmark 43 migraine patients participated; all had migraine without aura. 36 females and 7 males; allowed age range 18 to 70 years |
|
| Interventions | Sodium valproate versus placebo (12 weeks). Dosage either 1000 mg/day or 1500 mg/day to maintain plasma concentration above 50 mg/L | |
| Outcomes | Number of migraine days per 28 days. Intensity of headache (3‐point scale). Duration Time point(s) considered in the review: entire 12‐week treatment phase |
|
| Notes | Funders of the trial: Ercopharm Ltd Denmark | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Description of method for random sequence generation is lacking |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Both clinicians and participants were blinded. Dose adjustments (differentiation between 2 doses) were performed by independent investigators based on serum levels of sodium valproate. Placebo and verum tablets were apparently identical |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The term 'triple‐blind' presumably means that the statistician was blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Patients who dropped out after randomisation were excluded from statistical analysis |
| Selective reporting (reporting bias) | Low risk | No suspicion of selective reporting of outcomes, time points, or analyses |
Kaniecki 1997.
| Methods | Prospective, randomised, single‐blind, double cross‐over trial. 4‐week baseline period. Total duration: 32 weeks (4 weeks placebo, 12 weeks treatment, 4‐week washout, 12 weeks treatment) Discontinuation rate: dropout: 14% overall Compliance (adherence) data: compliance data available only as mean blood valproate levels Rule for use of acute medication: not reported Methodological quality score: 2 |
|
| Participants | Inclusion: migraine according to ICHD‐I; migraine onset more than 1 year prior to study; 2 to 8 attacks per month; maximum of 15 headache days per month. Patients unable to differentiate migraine from other headaches were not included Exclusion: secondary headaches, daily headaches, and analgesic overuse headache were adequately excluded. Other exclusions: participation in previous trials of valproate or propanolol, failure of more than 2 other migraine prophylactic agents, severe medical or psychiatric illness, alcohol or drug abuse, inadequate contraception Setting: single neurology clinic Country: USA 37 migraine patients participated; all had migraine without aura. 30 females and 7 males; allowed age range 18 to 65 |
|
| Interventions | Placebo (4 weeks) versus divalproex sodium (12 weeks) versus propranolol hydrochloride (12 weeks). Dosage titrated for 8 weeks to goals of 1500 mg/day for divalproex sodium and 180 mg/day for propranolol hydrochloride, followed by 4‐week maintenance period | |
| Outcomes | Number of migraine attacks per 28 days. Number of migraine days per 28 days Time point(s) considered in the review: entire 12‐week treatment phase for active treatment (valproate or propranolol); 4‐week treatment phase for placebo |
|
| Notes | Placebo tablets were continued throughout the trial Funders of the trial: Abbott Laboratories |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Description of method for random sequence generation is lacking |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Clinician not blinded. Placebo, divalproex, and propranolol had different appearances, so even single‐blinding is questionable |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | The single investigator was not blinded until he reviewed the diaries for outcomes assessment |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Patients who dropped out after randomisation were excluded from statistical analysis |
| Selective reporting (reporting bias) | Unclear risk | AEs not reported for placebo treatment |
Kinze 2001.
| Methods | Prospective, open‐label, parallel study of serum valproate levels. Baseline period of 1 to 3 months. Duration of treatment: unspecified titration period followed by 6 months stable dosage Discontinuation rate: dropout/loss to follow‐up: 7 of 52 patients Compliance (adherence) data: compliance assessed by serum valproate level in relation to dose Rule for use of acute medication: triptans and NSAIDS allowed, others not specified Methodological quality score: 1 |
|
| Participants | Inclusion: migraine according to ICHD‐I, migraine frequency of 2 to 5 attacks per month, sufficient therapy for acute attacks (not fully defined), age 18 or over Exclusion: secondary headaches were adequately excluded. No clear information on the exclusion of daily headache or analgesic overuse headache. Other exclusions: pregnancy, breast‐feeding, use of other migraine prophylaxis, history of liver disease or elevated liver enzymes, more than 10 days of tension‐type headache per month Setting: single outpatient headache clinic Country: Germany 52 patients recruited, 7 with aura and 45 without aura. 49 females and 3 males; mean age 45 years |
|
| Interventions | Patients received differing doses of sodium valproate depending upon their assignment to a physician. Efficacy of low (21 to 50 micrograms/ml) versus high (> 50 micrograms/ml) serum valproate levels was the focus of analysis. Dosage started at 150 mg/day and was titrated upwards to individualised target dose (maximum 1200 mg/day) | |
| Outcomes | Migraine frequency per month. Migraine days per month. Headache intensity. Use of acute medication Time point(s) considered in the review: last (sixth) month of stable dosage treatment phase |
|
| Notes | Funders of the trial: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Two participating physicians generally used doses up to 600 mg/day, whereas 2 others escalated up to 1200 mg/day without a predefined schedule |
| Allocation concealment (selection bias) | High risk | Study not blinded |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Study not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Results reflect a complete case analysis of 45 patients. Analysis was by serum valproate level; it was not reported whether patients assigned to the lower dose conditions were all in the low serum level group |
| Selective reporting (reporting bias) | High risk | Numerical information about adverse events not provided |
Klapper 1997.
| Methods | Prospective, randomised, double‐blind, parallel trial. Five half‐lives washout period. Total duration then 16 weeks. 4‐week single‐blind, placebo‐only baseline period. 12‐week treatment period Discontinuation rate: dropout: 25% of randomised participants Compliance (adherence) data: compliance data not reported Rule for use of acute medication: fewer than 3 times per week, but no information about permitted medications Methodological quality score: 4 |
|
| Participants | Inclusion: migraine according to ICHD‐I; migraine onset at least 6 months prior to study; at least 2 attacks per month for previous 3 months Exclusion: daily headaches and analgesic overuse headaches were adequately excluded. No information on the exclusion of secondary headaches is reported. Other exclusions: more than 15 days of non‐migrainous headache per month, migraine symptoms without headache, pregnancy, inadequate contraception for women, previous treatment with valproate, failure of more than 2 other migraine prophylactic agents, significant medical or psychiatric disorder, many concomitant medications Setting: multi‐centre Country: USA and Canada 176 migraine patients were randomised; 91% had had attacks without aura and 40% with aura. 157 females and 19 males; age range 17 to 76 |
|
| Interventions | Divalproex sodium 500 mg versus 1000 mg versus 1500 mg versus placebo (12 weeks). Dosage titrated for 4 weeks, then maintained for 8 weeks | |
| Outcomes | Number of headache days per 28 days. Number of migraine attacks per 28 days. Frequency of non‐migraine headaches Time point(s) considered in the review: entire 3‐month treatment phase |
|
| Notes | Funders of the trial: Abbott Laboratories | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Description of method for random sequence generation (1:1:1:1 ratio within each study centre) is lacking |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Single‐blind baseline phase followed by double‐blind experimental phase. Placebo tablets were matched to verum |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis includes all randomised participants who provided headache data during the double‐blind phase |
| Selective reporting (reporting bias) | High risk | Dose comparisons not possible, as insufficient data were provided |
Mathew 1995.
| Methods | Prospective, 2:1 randomised, double‐blind, parallel trial. 5 half‐lives washout period for previous migraine prophylactic medication. Total duration then 16 weeks: 4‐week single‐blind, placebo‐only baseline period. 4 weeks titration, then 8 weeks stable dosage Discontinuation rate: dropout 17% for active treatment, 14% for placebo Compliance (adherence) data: compliance data available only as mean blood valproate levels Rules for use of acute medication: reported as exclusions; analgesics and triptans permitted (but not daily) Methodological quality score: 4 |
|
| Participants | Inclusion: migraine according to ICHD‐I; migraine onset more than 6 months prior to study; 2 or more attacks per month for previous 3 months Exclusion: secondary headaches, daily headaches, and analgesic overuse headache were adequately excluded. Other exclusions: migraine symptoms without headache, significant other medical or psychiatric disorder, history of poor compliance, history of valproate use, women of childbearing potential, failure of more than 2 other migraine prophylactic agents Setting: multi‐centre Country: USA 107 migraine patients participated; 95% had had attacks without aura and 27% with aura. 83 females and 24 males; allowed age range 16 to 75 |
|
| Interventions | Divalproex sodium versus placebo (12 weeks). Dosage titrated to maintain plasma concentration at 70 to 120 mg/L. Mean dose 1087 mg/day | |
| Outcomes | Number of migraine attacks per 28 days. Number of migraine days per 28 days. Peak headache severity (0 to 4 scale). Headache duration (hours). Average analgesic use. Other composite measures Time point(s) considered in the review: entire 3‐month treatment phase |
|
| Notes | Funders of the trial: Abbott Laboratories | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Description of method for random sequence generation (2:1 ratio of verum to placebo within each centre) is lacking |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Single‐blind baseline phase (patient was blinded, clinician was not) followed by double‐blind treatment phase. Placebo tablets were identical in appearance to verum and dose‐adjusted in a similar fashion. An unblinded designee reviewed plasma concentrations and informed personnel at each clinic of the results in a blinded manner. For patients receiving placebo, sham valproate concentrations were reported by the unblinded designee according to an algorithm designed to maintain the blind |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Analyses were performed using all data from randomised patients |
| Selective reporting (reporting bias) | Low risk | No suspicion of selective reporting of outcomes, time points, subgroups, or analyses |
Mitsikostas 1997.
| Methods | Prospective, randomised, parallel trial. 4‐week baseline period. Duration of treatment: 4 weeks titration, then 4 weeks stable dosage Discontinuation rate: dropout 4.5% for active treatment; 9.1% for the comparison treatment Compliance (adherence) data: compliance was assessed for the active treatment group only by serum valproate concentrations Rule for use of acute medication: sumatriptan or anti‐inflammatory agents only Methodological quality score: 2 |
|
| Participants | Inclusion: migraine according to ICHD‐I; migraine onset at least 6 months before screening; at least 3 attacks per month for 6 months; negative brain CT scan. Mixed headaches (with episodic TTH) were included; subgroups cannot be distinguished Exclusion: secondary headaches, daily headaches, and analgesic overuse headache were adequately excluded. Other exclusions: other migraine prophylactic medication in last 6 months, study drug contraindications, hepatic or renal disorder, pregnancy or reproductive intention, chronic use of any other medication during study period Setting: single headache clinic Country: Greece 44 migraine patients participated; 9 with aura and 35 without. 31 females and 13 males; age range 15 to 60 years. 22 received active treatment and 22 received placebo |
|
| Interventions | Sodium valproate versus flunarizine (8 weeks). Dosage titrated up to valproate 1000 mg/day or flunarizine 10 mg/day and maintained for 4 weeks | |
| Outcomes | Number of migraine attacks per 28 days. Mean severity of attacks (0 to 10 scale). Mean attack duration (hours). Mean state of physical activity during attacks (0 to 100 scale). Average use of escape medication during 28 days (number of tablets) Time point(s) considered in the review: last (second) month of treatment phase |
|
| Notes | Funders of the trial: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Description of method for random sequence generation (1:1 ratio) is lacking |
| Allocation concealment (selection bias) | High risk | No blinding |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | This trial is described as double‐open, which appears equivalent to open‐label |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Participants not completing study were excluded from the analysis |
| Selective reporting (reporting bias) | Low risk | No suspicion of selective reporting of outcomes, time points, or analyses |
Shaygannejad 2006.
| Methods | Prospective, randomised, double‐blind, double cross‐over trial. 1‐month baseline period. Duration of treatment: 1 week titration, followed by 2 months stable dose of first drug. 2‐month washout, then 2‐month stable dose of second drug Discontinuation rate: no dropouts were recorded Compliance (adherence) data: compliance was reported as good, but no details or results of compliance measurement are given Rule for use of acute medication: unspecified analgesics allowed, but not more than once per day. No other details provided Methodological quality score: 3 |
|
| Participants | Inclusion: migraine according to ICHD‐I, migraine for at least 6 months prior to trial, migraine frequency 3 or more per month in the 3 months prior to trial Exclusion: no clear details given on the exclusion of secondary headache, daily headache, or analgesic overuse headache. Other exclusions: concurrent medical treatment; concurrent serious medical problems; other neurological disease; lactating or pregnant Setting: single neurology clinic Country: Iran Complete case analysis of 64 patients. Patients with and without aura recruited, but percentages not reported. 36 males and 28 females; age range 14 to 57 years |
|
| Interventions | Topiramate 50 mg/day versus sodium valproate 400 mg/day; repeat in cross‐over phase. Topiramate dose started at 25 mg/day and was incremented to 50 mg/day; sodium valproate was started at 200 mg/day and incremented to 400 mg/day | |
| Outcomes | Migraine frequency per month; migraine intensity; migraine duration Time point(s) considered in the review: last (second) month of stable dosage treatment phase |
|
| Notes | Study appears to use doses of both topiramate and valproate that are lower than normal clinical doses Funders of the trial: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Description of method for random sequence generation (1:1 ratio) is lacking |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Participants and clinician were blinded. Information lacking about how this was adequately achieved |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All enrolled patients completed treatment and were available for follow‐up |
| Selective reporting (reporting bias) | Low risk | No suspicion of selective reporting of outcomes, time points, subgroups, or analyses |
Abbreviations: AE = adverse event; CDH = chronic daily headache; CI = confidence interval; CNS = central nervous system; CT = computed tomography; h = hour; HIT‐6 = Headache Impact Test; ICHD‐I = International Classification of Headache Disorders, 1st Edition (IHS Cttee 1988); ICHD‐II = International Classification of Headache Disorders, 2nd Edition (ICHD‐II 2004); ITT = intention‐to‐treat; MIDAS = Migraine Disability Assessment; NSAIDs = non‐steroidal anti‐inflammatory drugs; SD = standard deviation; TTH = tension‐type headache
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Arnold 1998 | Review paper |
| Bartolini 2005 | Reports data on chronic migraine only |
| Bavrasad 2010 | Serious flaws including selective outcome reporting and concerns about data integrity |
| Blumenfeld 2008 | Comparator is experimental |
| Cutrer 2001 | Basic science paper |
| Erdemoglu 2000 | No control group |
| Fragoso 2003 | Letter to editor |
| Ghose 1998 | No control group |
| Green 2005 | Post hoc analysis of Klapper 1997 (included) |
| Keyvan 2009 | Unknown number of participants were children. Lack of usable outcome data |
| Klapper 1994 | No extractable data published |
| Krymchantowski 2011 | No randomisation |
| Lenaerts 1996 | No control group |
| Millan‐Guerrero 2007 | Comparator is experimental |
| Rothrock 1994 | No control group |
| Rothrock 1997 | Review paper |
| Silberstein 1993 | Conference abstract only |
| Sørensen 1988 | No control group |
| Togha 2008 | Comparator is experimental |
Differences between protocol and review
After reviewing the variety of methods used for calculating headache index, we decided that no systematic analysis of headache index data would be undertaken, for two principal reasons. First, rarely was sufficient information given to allow a clear understanding of how the index was calculated, and second, even when indexes were clearly described, they were not always useful — for example, because they confounded severity scores with frequency scores. Avoiding the use of headache index measures is consistent with the recommendations of the International Headache Society (Tfelt‐Hansen 2012).
After publication of the protocol, we decided not to extract trial data on pain intensity, duration of attacks, or associated symptoms of migraine (nausea, vomiting, photophobia, phonophobia). The reasons were that such information was rarely given, and that the methods used were not standardised.
Our methods for assessing and dealing with heterogeneity have evolved over time in line with changing Cochrane methods. The protocol for the original review specified that we would test estimates of efficacy for homogeneity, use a fixed‐effect model to combine homogenous estimates, and use a random‐effects model to combine estimates when a group of studies with statistically heterogeneous results appeared to be clinically similar. In the original review itself, and in the 2007 update (Chronicle 2004; Mulleners 2008), we in fact used a random‐effects model throughout for pooled analyses. In the present review, we again use a random‐effects model for pooling, but we have added a possible fixed‐effect sensitivity analysis in select cases; see Assessment of heterogeneity for details.
Contributions of authors
Prof Linde: Designing the review. Co‐ordinating the review. Data collection for the review. Screening search results. Organising retrieval of papers. Screening retrieved papers against eligibility criteria. Appraising quality of papers. Extracting data from papers. Writing to authors of papers for additional information. Providing additional data about papers. Data management for the review. Entering data into RevMan. Analysis of data. Interpretation of data. Providing a clinical perspective. Writing the review.
Dr Mulleners: Conceiving the review. Designing the review. Data collection for the review. Screening search results. Organising retrieval of papers. Screening retrieved papers against eligibility criteria. Appraising quality of papers. Extracting data from papers. Interpretation of data. Providing a clinical perspective.
Prof Chronicle: Performing previous work that was the foundation of the current review.
Assoc Prof McCrory: Analysis of data. Interpretation of data. Providing a methodological perspective. Providing general advice on the review.
Sources of support
Internal sources
No sources of support supplied
External sources
-
International Headache Society, UK.
Funding for administrative costs associated with editorial and peer review of the original and updated reviews
-
Lifting The Burden: the Global Campaign against Headache, UK.
Funding for administrative costs associated with editorial and peer review of the updated review
Declarations of interest
Prof Linde: During the process of preparing this review the author received a travel grant from Allergan in Sweden and was involved as an investigator in a clinical trial in Norway sponsored by AstraZeneca and comparing candesartan, propranolol, and placebo in the prophylaxis of migraine.
Dr Mulleners: The author was a paid consultant for the Merck Dutch Migraine Advisory Board and received a speaker's fee from Merck Sharp & Dohme Corp.
Prof Chronicle: Author deceased. During the process of preparing the original review the author was a paid consultant for Johnson & Johnson and NPS Pharmaceuticals in the USA.
Assoc Prof McCrory: During 2008, the author was a paid expert witness for the plaintiffs in a legal action against the manufacturer of Neurontin (gabapentin). In this capacity, he prepared a systematic review examining previously confidential research reports obtained from the manufacturer (through discovery), along with published trial reports of gabapentin for migraine prophylaxis, and testified at trial.
Stable (no update expected for reasons given in 'What's new')
References
References to studies included in this review
Afshari 2012 {published data only (unpublished sought but not used)}
- Afshari D, Rafizadeh S, Rezaei M. A comparative study of the effects of low‐dose topiramate versus sodium valproate in migraine prophylaxis. International Journal of Neuroscience 2012;122(2):60‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Freitag 2002 {published data only}
- Freitag FG, Collins SD, Carlson HA, Goldstein J, Saper J, Silberstein S, et al. A randomized trial of divalproex sodium extended‐release tablets in migraine prophylaxis. Neurology 2002;58(11):1652‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Hering 1992 {published data only}
- Hering R, Kuritzky A. Sodium valproate in the prophylactic treatment of migraine: a double‐blind study versus placebo. Cephalalgia 1992;12(2):81‐4. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Jensen 1994 {published data only}
- Jensen R, Brinck T, Olesen J. Sodium valproate has a prophylactic effect in migraine without aura: a triple‐blind, placebo‐controlled crossover study. Neurology 1994;44(4):647‐51. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kaniecki 1997 {published data only}
- Kaniecki RG. A comparison of divalproex with propanolol and placebo for the prophylaxis of migraine without aura. Archives of Neurology 1997;54(9):1141‐5. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kinze 2001 {published data only}
- Kinze S, Clauss M, Reuter U, Wolf T, Dreier JP, Einhaupl KM, et al. Valproic acid is effective in migraine prophylaxis at low serum levels: a prospective open‐label study. Headache 2001;41(8):774‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Klapper 1997 {published data only}
- Klapper J, on behalf of the Divalproex Sodium in Migraine Prophylaxis Study Group. Divalproex sodium in migraine prophylaxis: a dose‐controlled study. Cephalalgia 1997;17(2):103‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Mathew 1995 {published data only}
- Mathew NT, Saper JR, Silberstein SD, Rankin L, Markley HG, Solomon S, et al. Migraine prophylaxis with divalproex. Archives of Neurology 1995;52(3):281‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Mitsikostas 1997 {published data only}
- Mitsikostas DD, Polychronidis I. Valproate versus flunarizine in migraine prophylaxis: a randomized, double‐open, clinical trial. Functional Neurology 1997;12(5):267‐76. [MEDLINE: ] [PubMed] [Google Scholar]
Shaygannejad 2006 {published data only}
- Shaygannejad V, Janghorbani M, Ghorbani A, Ashtary F, Zakizade N, Nasr V. Comparison of the effect of topiramate and sodium valproate in migraine prevention: a randomized blinded crossover study. Headache 2006;46(4):642‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Arnold 1998 {published data only}
- Arnold G, Einhaupl KM. Valproic acid in the prophylactic treatment of migraine [Valproinsaure in der prophylaktischen Behandlung der Migräne]. Nervenarzt 1998;69(10):913‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Bartolini 2005 {published data only}
- Bartolini M, Silvestrini M, Taffi R, Lanciotti C, Luconi R, Capecci M, et al. Efficacy of topiramate and valproate in chronic migraine. Clinical Neuropharmacology 2005;28(6):277‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Bavrasad 2010 {published data only}
- Bavrasad R, Nejad SEM, Yarahmadi AR, Sajedi SI, Rahim F. Assessment of the middle dose of topiramate in comparison with sodium valproate for migraine prophylaxis: a randomized double‐blind study. International Journal of Pharmacology 2010;6(5):670‐5. [EMBASE: 2010449325] [Google Scholar]
Blumenfeld 2008 {published data only}
- Blumenfeld AM, Schim JD, Chippendale TJ. Botulinum toxin type A and divalproex sodium for prophylactic treatment of episodic or chronic migraine. Headache 2008;48(2):210‐20. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Cutrer 2001 {published data only}
- Cutrer FM. Antiepileptic drugs: how they work in headache. Headache 2001;41 Suppl 1:S3‐S10. [DOI] [PubMed] [Google Scholar]
Erdemoglu 2000 {published data only}
- Erdemoglu AK, Ozbakir S. Valproic acid in prophylaxis of refractory migraine. Acta Neurologica Scandinavica 2000;102(6):354‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Fragoso 2003 {published data only}
- Fragoso YD. Low dose of sodium divalproate for the treatment of migraine. MedGenMed [electronic resource]: Medscape General Medicine 2003;5(1):32. [MEDLINE: ] [PubMed] [Google Scholar]
Ghose 1998 {published data only}
- Ghose K, Niven B. Prophylactic sodium valproate therapy in patients with drug‐resistant migraine. Methods & Findings in Experimental & Clinical Pharmacology 1998;20(4):353‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Green 2005 {published data only}
- Green MW, Giordano S, Jiang P, Jafari M, Smith TB. Effect of divalproex on metabolic parameters is dose related in migraine prophylaxis. Headache 2005;45(8):1031‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Keyvan 2009 {published and unpublished data}
- Keyvan G, Abolfazl MB. Comparison of treatment effect of sodium valproate, propranolol and tricyclic antidepressants in migraine. Pakistan Journal of Biological Sciences 2009;12(15):1098‐101. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Klapper 1994 {published data only}
- Klapper JA. An open label cross‐over comparison of divalproex sodium and propanolol HCl in the prevention of migraine headaches. Headache Quarterly 1994;5(4):50‐3. [Google Scholar]
Krymchantowski 2011 {published data only}
- Krymchantowski AV, Jevoux CC. Topiramate vs divalproex sodium in the preventive treatment of migraine: a prospective "real‐world" study. Headache 2011;51(4):554‐8. [EMBASE: 2011188025] [DOI] [PubMed] [Google Scholar]
Lenaerts 1996 {published data only}
- Lenaerts M, Bastings E, Sianard J, Schoenen J. Sodium valproate in severe migraine and tension‐type headache: an open study of long‐term efficacy and correlation with blood levels. Acta Neurologica Belgica 1996;96(2):126‐9. [MEDLINE: ] [PubMed] [Google Scholar]
Millan‐Guerrero 2007 {published data only}
- Millan‐Guerrero RO, Isais‐Millan R, Barreto‐Vizcaino S, Rivera‐Castano L, Garcia‐Solorzano A, Lopez‐Blanca C, et al. Subcutaneous histamine versus sodium valproate in migraine prophylaxis: a randomized, controlled, double‐blind study. European Journal of Neurology 2007;14(10):1079‐84. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Rothrock 1994 {published data only}
- Rothrock JF, Kelly NM, Brody ML, Golbeck A. A differential response to treatment with divalproex sodium in patients with intractable headache. Cephalalgia 1994;14(3):241‐4. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Rothrock 1997 {published data only}
- Rothrock JF. Clinical studies of valproate for migraine prophylaxis. Cephalalgia 1997;17(2):81‐3. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Silberstein 1993 {published data only}
- Silberstein SD, Saper JR, Mathew NT. The safety and efficacy of divalproex sodium in the prophylaxis of migraine headache: a multicenter, double‐blind, placebo‐controlled trial. Headache 1993;33(5):264‐5. [Google Scholar]
Sørensen 1988 {published data only}
- Sørensen KV. Valproate: a new drug in migraine prophylaxis. Acta Neurologica Scandinavica 1988;78(4):346‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Togha 2008 {published data only}
- Togha M, Rahmat Jirde M, Nilavari K, Ashrafian H, Razeghi S, et al. Cinnarizine in refractory migraine prophylaxis: Efficacy and tolerability. A comparison with sodium valproate. Journal of Headache & Pain 2008;9(2):77‐82. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Ad Hoc Cttee 1962
- Ad Hoc Committee on the Classification of Headache of the National Institute of Neurological Diseases and Blindness. Classification of headache. JAMA 1962;179(9):717‐8. [Google Scholar]
Alderson 2004
- Alderson P, Green S, Higgins JPT, editors. Highly sensitive search strategies for identifying reports of randomized controlled trials in MEDLINE. Cochrane Reviewers' Handbook 4.2.2 [updated December 2003]; Appendix 5b. In: The Cochrane Library, Issue 1, 2004. Chichester, UK: John Wiley & Sons, Ltd.
Clarke 1996
- Clarke CE, MacMillan L, Sondhi S, Wells NE. Economic and social impact of migraine. QJM 1996;89(1):77‐84. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Cutrer 1997
- Cutrer FM, Limmroth V, Moskowitz MA. Possible mechanisms of valproate in migraine prophylaxis. Cephalalgia 1997;17(2):93‐100. [DOI] [PubMed] [Google Scholar]
Dalkara 2012
- Dalkara S, Karakurt A. Recent progress in anticonvulsant drug research: strategies for anticonvulsant drug development and applications of antiepileptic drugs for non‐epileptic central nervous system disorders. Current Topics in Medicinal Chemistry 2012;12(9):1033‐71. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Edmeads 1993
- Edmeads J, Findlay H, Tugwell P, Pryse‐Phillips W, Nelson RF, Murray TJ. Impact of migraine and tension‐type headache on life‐style, consulting behaviour, and medication use: a Canadian population survey. Canadian Journal of Neurological Sciences 1993;20(2):131‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Edvinsson 2010
- Edvinsson L, Linde M. New drugs in migraine treatment and prophylaxis: telcagepant and topiramate. Lancet 2010;376(9741):645‐55. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Evers 2009
- Evers S, Afra J, Frese A, Goadsby PJ, Linde M, May A, et al. European Federation of Neurological Societies. EFNS guideline on the drug treatment of migraine—revised report of an EFNS task force. European Journal of Neurology 2009;16(9):968‐81. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
GBD 2010 Study
- Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990‐2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2013;380(9859):2163‐96. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
ICHD‐II 2004
- Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders: 2nd edition. Cephalalgia 2004;24 Suppl 1:1‐160. [DOI] [PubMed] [Google Scholar]
IHS Cttee 1988
- Headache Classification Committee of the International Headache Society. Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalalgia 1988;8 Suppl 7:1‐96. [PubMed] [Google Scholar]
Jadad 1996
- Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary?. Controlled Clinical Trials 1996;17(1):1‐12. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Linde 2004
- Linde K, Rossnagel K. Propranolol for migraine prophylaxis. Cochrane Database of Systematic Reviews 2004, Issue 2. [DOI: 10.1002/14651858.CD003225.pub2] [DOI] [PubMed] [Google Scholar]
Linde 2012
- Linde M, Gustavsson A, Stovner LJ, Steiner TJ, Barré J, Katsarava Z, et al. The cost of headache disorders in Europe: the Eurolight project. European Journal of Neurology 2012;19(5):703‐11. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Linde 2013a
- Linde M, Mulleners WM, Chronicle EP, McCrory DC. Topiramate for the prophylaxis of episodic migraine in adults. Cochrane Database of Systematic Reviews 2013, Issue 6. [DOI: 10.1002/14651858.CD010610] [DOI] [PMC free article] [PubMed] [Google Scholar]
Linde 2013b
- Linde M, Mulleners WM, Chronicle EP, McCrory DC. Valproate (valproic acid or sodium valproate or a combination of the two) for the prophylaxis of episodic migraine in adults. Cochrane Database of Systematic Reviews 2013, Issue 6. [DOI: 10.1002/14651858.CD010611] [DOI] [PMC free article] [PubMed] [Google Scholar]
Linde 2013c
- Linde M, Mulleners WM, Chronicle EP, McCrory DC. Gabapentin or pregabalin for the prophylaxis of episodic migraine in adults. Cochrane Database of Systematic Reviews 2013, Issue 6. [DOI: 10.1002/14651858.CD010609] [DOI] [PMC free article] [PubMed] [Google Scholar]
Linde 2013d
- Linde M, Mulleners WM, Chronicle EP, McCrory DC. Antiepileptics other than gabapentin, pregabalin, topiramate, and valproate for the prophylaxis of episodic migraine in adults. Cochrane Database of Systematic Reviews 2013, Issue 6. [DOI: 10.1002/14651858.CD010608] [DOI] [PMC free article] [PubMed] [Google Scholar]
McQuay 1998
- McQuay H, Moore R. An Evidence‐based Resource for Pain Relief. Oxford: Oxford University Press, 1998. [Google Scholar]
Mehuys 2012
- Mehuys E, Paemeleire K, Hees T, Christiaens T, Bortel LM, Tongelen I, et al. Self‐medication of regular headache: a community pharmacy‐based survey. European Journal of Neurology 2012;19(8):1093‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Morrell 2003
- Morrell MJ. Reproductive and metabolic disorders in women with epilepsy. Epilepsia 2003;44 Suppl 4:11‐20. [DOI] [PubMed] [Google Scholar]
Olesen 2006
- Olesen J, Bousser M‐G, Diener H‐C, Dodick D, First M, Goadsby PJ, et al. Headache Classification Committee. New appendix criteria open for a broader concept of chronic migraine. Cephalalgia 2006;26(6):742‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Porter 1992
- Porter RJ, Meldrum BS. Antiepileptic drugs. In: Katzung BG editor(s). Basic and Clinical Pharmacology. 5th Edition. Norwalk, CT: Appleton & Lange, 1992:331‐49. [Google Scholar]
Reveiz‐Herault 2003
- Reveiz‐Herault L, Cardona AF, Ospina EG, Carrillo P. Effectiveness of flunarizine in the prophylaxis of migraine: a meta‐analytical review of the literature [Eficacia de flunaricina en la profilaxis de migrana: revision metaanalitica de la bibliografia]. Revista de Neurologia 2003;36(10):907‐12. [MEDLINE: ] [PubMed] [Google Scholar]
Silberstein 2008
- Silberstein S, Saper J, Berenson F, Somogyi M, McCague K, D'Souza J. Oxcarbazepine in migraine headache: a double‐blind, randomized, placebo‐controlled study. Neurology 2008;70(7):548‐55. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Silberstein 2012
- Silberstein SD, Holland S, Freitag F, Dodick DW, Argoff C, Ashman E, Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Evidence‐based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology 2012;78(17):1337‐45. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tfelt‐Hansen 2012
- Tfelt‐Hansen P, Pascual J, Ramadan N, Dahlöf C, D'Amico D, Diener HC, et al. International Headache Society Clinical Trials Subcommittee. Guidelines for controlled trials of drugs in migraine: third edition. A guide for investigators. Cephalalgia 2012;32(1):6‐38. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Victor 2003
- Victor S, Ryan S. Drugs for preventing migraine headaches in children. Cochrane Database of Systematic Reviews 2003, Issue 4. [DOI: 10.1002/14651858.CD002761] [DOI] [PubMed] [Google Scholar]
Wiffen 2010
- Wiffen PJ, Collins S, McQuay HJ, Carroll D, Jadad A, Moore RA. Anticonvulsant drugs for acute and chronic pain. Cochrane Database of Systematic Reviews 2010, Issue 1. [DOI: 10.1002/14651858.CD001133.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Chronicle 2004
- Chronicle EP, Mulleners WM. Anticonvulsant drugs for migraine prophylaxis. Cochrane Database of Systematic Reviews 2004, Issue 3. [DOI: 10.1002/14651858.CD003226.pub2] [DOI] [PubMed] [Google Scholar]
Mulleners 2008
- Mulleners WM, Chronicle EP. Anticonvulsants in migraine prophylaxis: a Cochrane review. Cephalalgia 2008;28(6):585‐97. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]


