Abstract
Inherited and acquired coagulopathy are frequently associated with major bleeding in severe trauma, cardiac surgery with cardiopulmonary bypass, and postpartum hemorrhage. Perioperative management is multifactorial and includes preoperative optimization and discontinuation of anticoagulants and antiplatelet therapy in elective procedures. Prophylactic or therapeutic use of antifibrinolytic agents is strongly recommended in guidelines and has been shown to reduce bleeding and need for allogeneic blood administration. In the context of bleeding induced by anticoagulants and/or antiplatelet therapy, reversal strategies should be considered when available. Targeted goal-directed therapy using viscoelastic point-of-care monitoring is increasingly used to guide the administration of coagulation factors and allogenic blood products. In addition, damage control surgery, which includes tamponade of large wound areas, leaving surgical fields open, and other temporary maneuvers, should be considered when bleeding is refractory to hemostatic measures.
The pathophysiology of bleeding in patients after trauma, major surgery, and postpartum hemorrhage is multifactorial, and includes hypovolemia, hypothermia, metabolic acidosis, hemodilution, thrombocytopenia, platelet dysfunction, coagulation factor deficit, fibrinolysis, and activation of inflammatory pathways.1,2 Pre-existing hemostatic defects due to oral anticoagulants (vitamin K antagonists [VKAs], factor IIa or Xa inhibitors) and antiplatelet therapy (aspirin, adenosine diphosphate P2Y12 receptor inhibitors) are often present in bleeding patients. The management of perioperative bleeding includes evaluating the bleeding risk, the effects of surgery on hemostasis, administration of transfusional therapies, factor concentrates, or other measures based on point-of-care coagulation testing and their limitations.3 After major postoperative hemorrhage and resuscitation, patients transition from a hemorrhagic to a prothrombotic phenotype due to hypercoagulability associated with the acute phase responses and therapies administered.4 This can be exacerbated by physicians’ reluctance to start venous thromboembolic prophylaxis after a bleeding episode. Optimizing hemostatic balance is critical for perioperative physicians, and requires understanding of hemostasis and therapeutic approaches.
This clinical focus review will discuss the definitions and pathophysiology of clinical bleeding in three major domains, trauma, cardiac surgery with cardiopulmonary bypass (CPB), and postpartum hemorrhage; describe evolving therapeutic approaches to manage bleeding conditions that occur commonly in each of these clinical settings; and provide summary tables for the clinician’s reference.
General Considerations
Perioperative bleeding can occur from surgical and nonsurgical causes, or a combination of both. Drug-induced coagulopathy and/or platelet inhibition are important risk factors in patients treated with anticoagulants or antiplatelet therapy, and perioperative management should be individualized based on the reduced risk of bleeding as a benefit of interrupting those medications versus increased risk of thrombosis as a result of such discontinuation. Nonsurgical bleeding manifests as generalized but often diffuse bleeding at sites remote from the surgical field. This type of bleeding, often referred to as oozing or diffuse microvascular bleeding, is typically due to coagulopathy and platelet dysfunction. Coagulopathy can result from a single factor but often a combination of factors, including hemorrhage, metabolic acidosis, hypocalcemia, hypothermia, coagulation factor deficiency (inherited or acquired) or inappropriate replacement, hepatic dysfunction, hyperfibrinolysis, or disseminated intravascular coagulation (DIC).5 In addition, bleeding can be observed in the presence of thrombocytopenia or platelet dysfunction. Severe bleeding may trigger transfusion of red blood cells, which still involves the risk of viral infection and is associated with the risk of transfusion-related immunomodulation, thus promoting nosocomial infections and other immune responses.6,7 Massive hemorrhage contributes to 4% of malpractice claims in the United States, with a high percentage of cases in which anesthesia care was judged to be inappropriate.8 Of note, claims are highest in obstetrics (30%); however, risk factors, failure of early recognition, and delayed communication of a developing hemorrhagic emergency contribute to the complications.
Definition of Severe Bleeding
The most severe complication of perioperative hemorrhage is hypovolemic shock. Classification of acute hypovolemia as defined by the American College of Surgeons (Chicago, Illinois) includes four levels corresponding to less than 15% (class I), 15 to 30% (class II), 31 to 40% (class III), and greater than 40% (class IV) blood volume loss.9 Shock occurs when the blood loss creates oxygen debt, end-organ dysfunction, and ultimately death if not effectively treated in a timely fashion.
Multiple tools to standardize bleeding assessment have been reported. As examples, the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS) defines major bleeding as the need for four or more erythrocyte units within 24 h in the first postoperative week, whereas the International Society on Thrombosis and Haemostasis (Carrboro, North Carolina) defines major bleeding as more than two erythrocyte units in the same timeframe.10 The universal definition of perioperative bleeding, which monitors nine independent events related to perioperative bleeding within a five-level classification system, has been well-validated for the prediction of bleeding complications after adult cardiac surgery (table 1).11,12 The same applies for the European Coronary Artery Bypass Graft Bleeding Severity Grade.12 The universal definition of perioperative bleeding score revealed a high predictive value for 28-day mortality of patients of the large randomized Transfusion Avoidance in Cardiac Surgery (TACS) trial.12
Table 1.
Bleeding Categories According to Consensus-based Bleeding Scores in Cardiac Surgery
Although there are many definitions of severe or life-threatening bleeding, each differs in the timeframe and volume of blood products administered and whether the response activates a massive transfusion protocol. The need for consensus-based definitions is evident from the variable quantification of bleeding and inconsistent timing of when scoring occurs. This challenge was the topic of a recent consensus conference that recommended primary outcomes for clinical trials evaluating hemostatic blood products and agents in patients with bleeding.13,14 Summary recommendations addressed multiple scenarios including trauma, cardiac surgery/mechanical circulatory support, and inherited bleeding disorders.
Identifying Procedures and Patients with High Bleeding Risk
The bleeding risk is often estimated based on the surgical or interventional procedure performed. In this context, various specialty societies have categorized their procedures as low, intermediate, high, and uncertain bleeding risks.
Extremity trauma is considered low or high bleeding risk, depending on the extent, while hip, pelvis, and acetabular fractures are defined as high bleeding risk events. Different models and scores exist for identifying patients who may require massive transfusion after trauma. The models are mostly based on hemodynamic, physiologic, laboratory, injury patterns and severity, mechanism, and demographic triggers.15 The Trauma-associated Severe Hemorrhage score was developed based on analysis of data from severely injured patients with blunt trauma from the multicenter civilian trauma registry database of the German Trauma Society (Berlin, Germany).15,16 This score was measured by seven independent but weighted variables (table 2). The range of values was 0 to 28, and each point corresponded to a percentage risk of massive transfusion. Most of these parameters can be determined within 15 min in high-quality centers. The high performance of the score was reflected in an area under curve of 0.892 (95% CI, 0.879 to 0.905) in the development cohort and 0.887 (95% CI, 0.864 to 0.910) in the validation cohort. Massive transfusion was required in more than 90% of cases with a Trauma-associated Severe Hemorrhage score greater than 16.
Table 2.
Trauma-associated Severe Hemorrhage Score
Cardiac surgery is associated with high bleeding risk, especially in reoperations, major aortic surgery, multiple procedures with prolonged CPB times, implantation of ventricular assist devices, and transplantation after previous sternotomy or ventricular assist device implant.17 In the Papworth Bleeding Risk-Score, the type of surgery and patient-related factors were combined.18 However, the focus of this score is coronary artery bypass graft and valve surgery. The recent Association of Cardiothoracic Anaesthetists perioperative risk of blood transfusion score developed by the Association of Cardiothoracic Anaesthesia and Critical Care (United Kingdom) to predict the PeriOperative Risk of blood Transfusion (PORT) in cardiac surgery is more complex and is extrapolated from a large national database.19 This score uses age greater than 70 yr, gender, body surface area, categorized hemoglobin, creatinine and Euroscore, and type of surgery (coronary artery bypass grafting or valve surgery, combination of both, or other type of surgery). Of note, the development of a bleeding score in postpartum hemorrhage did not yield a satisfactory discriminative value.20 However, the Association of Women’s Health, Obstetrics and Neonatal Nurses (Washington, D.C.) hemorrhage risk assessment tool predicted clinically relevant composite morbidity.21
Further, pre-existing patient-related factors associated with an increased risk of procedural bleeding have been extensively studied in patients undergoing percutaneous coronary intervention and cardiac surgery.14,22–24 The identified factors include age 75 yr or greater, renal disease, liver disease, active cancer, laboratory findings including anemia/thrombocytopenia, and emergency procedures. Even though these data cannot be easily extrapolated to all operative settings, they might be considered in the preoperative risk evaluation of the patient.
Pathophysiology of Coagulation Abnormalities in Specific Circumstances: Trauma, Cardiac Surgery, and Postpartum Hemorrhage
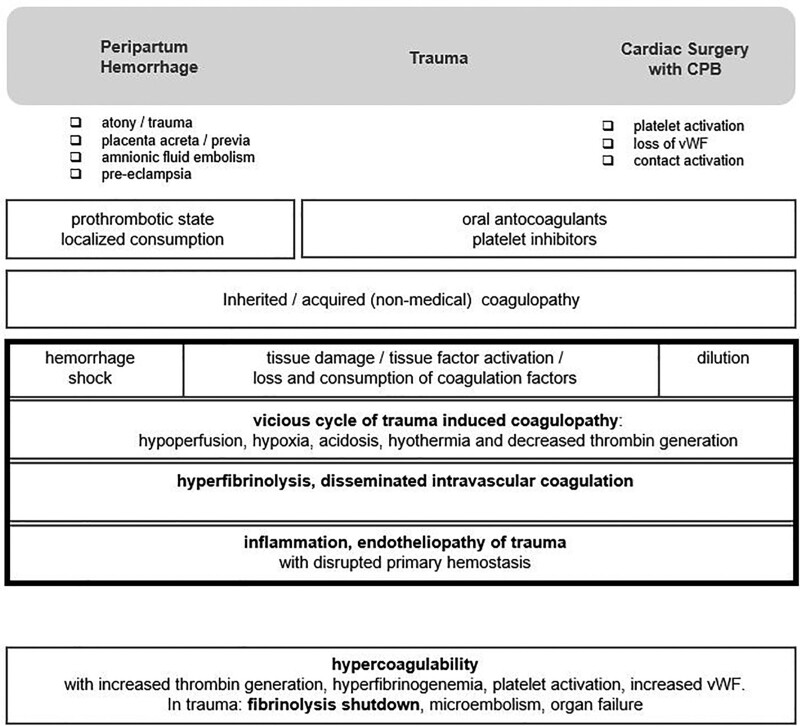
The early understanding of the classical coagulation cascade and operationalization of this knowledge have contributed to the development of plasma-based assays for coagulation factor levels. However, the partial thromboplastin time (PTT) and the international normalized ratio (INR) are not able to predict bleeding, as these assays were never developed with this specific goal, but to examine hemostatic defects in patients identified as hemophiliacs.25 A more modern understanding of the interrelated roles of the vascular endothelium, tissue factor activity and regulation, platelet function and signaling, and the contribution of immunoinflammatory factors led to a revision of the concept of coagulation cascade to a cell-based model with further specification into the steps of initiation, amplification, propagation, and stabilization, which have implications for therapeutic targets (fig. 1).26–29 Approaches to identifying and managing bleeding risk continue to be explored and refined and will have significant impact on its management over time.
Fig. 1.
Common pathophysiology pathways of postpartum hemorrhage, trauma, and cardiac surgery and related therapy strategies. vWF, von Willebrand factor.
Trauma
Uncontrolled posttraumatic bleeding has been reported to cause 25% of all injury-related deaths, and 40 to 80% of potentially preventable early traumatic deaths, with later mortality typically due to a hypercoagulable state and multiorgan failure. Trauma-induced coagulopathy describes a multifactorial coagulopathy arising from the interaction of hemorrhagic shock, tissue injury, and time from injury.30 Trauma-induced coagulopathy may manifest as hypocoagulability, and variably evolve to contribute along with metabolic acidosis and hypothermia as a component of traumatic hemorrhage, forming the lethal triad.
Early trauma-induced coagulopathy (less than 6 h) is seen in massively hemorrhaging patients with shock due to poor hemostatic control and clot formation compared to late trauma-induced coagulopathy (more than 24 h), which is a hypercoagulable state leading to thromboses, acute lung injury, and multiorgan failure. Risk factors for developing or worsening trauma-induced coagulopathy include situational and patient-related factors of older age, use of oral anticoagulants, severe tissue injury, penetrating trauma, traumatic brain injury, systemic shock and hypoperfusion, metabolic acidosis, long prehospital times, hypothermia, and dilutional crystalloid resuscitation fluids. Notably, DIC is related to but distinct from trauma-induced coagulopathy. DIC reveals systemic, unbridled clotting that is often promoted by the expression of tissue factor on several cell surfaces, whereas in the early period of trauma-induced coagulopathy, tissue factor facilitates clot formation at the sites of endothelial injury. However, the late trauma-induced prothrombotic and antifibrinolytic phenotype of trauma-induced coagulopathy is reminiscent of certain phenotypes of DIC.31 Both conditions are clarified by the International Society on Thrombosis and Haemostasis and have recently been reviewed in detail.30
The pathophysiologic response to tissue injury and hemorrhagic shock, along with the impact of resuscitation, generate an imbalanced activation of procoagulant and anticoagulant factors, endothelial injury, platelet dysfunction, fibrinolysis, and immune responses.32 Multiple mechanisms contribute to trauma-induced coagulopathy, including hemorrhagic shock, which causes endogenous stimulation of tissue plasminogen activator release from the endothelium, activated protein C, and decreased levels of plasminogen activator inhibitor-1. In addition, tissue injury potentiates trauma-induced coagulopathy through endothelial disruption by activation of tissue factor, platelets, and generation of damage-associated molecular patterns. After traumatic injury, prothrombotic microparticles are released, causing endothelial dysfunction, loss of barrier function, increased leukocyte adhesion, coagulopathy with micro- and macrothrombi, and multiorgan failure, referred to as “endotheliopathy of trauma.”30 This coagulopathy is characterized by loss of endothelial glycocalyx, sustained endothelial exocytosis of von Willebrand factor multimers, and platelet dysfunction. Animal models provide evidence that endotheliopathy and lung injury are apparent more than 3 h after injury, but recover by 24 h.33 The coagulopathic manifestation of trauma is bleeding requiring transfusional factors and procoagulant therapies to restore hemostatic function, especially in concordance with damage control surgery.34 Fibrinogen, a critical hemostatic protein, is often the initial factor to reach critically low levels and requires repletion as part of resuscitation.35 Proposed mechanisms include coagulation activation–induced consumption, degradation by hyperfibrinolysis, and dilution by volume replacement.36 Red blood cells are also critical components of hemostatic function on primary hemostasis, as the physical dispersion of platelets in the microcirculation toward the subendothelial surface promotes endothelial interaction.37,38 According to ex vivo and in vitro data, higher hematocrit values (greater than 25 to 30%) improve interaction.
Dysregulated fibrinolysis is also a potential concern in traumatic injury.30,39 Hyperfibrinolysis is initiated after trauma due to excessive tissue plasminogen activator from vascular endothelium presumed to be from Weibel–Palade bodies. Hyperfibrinolysis is then suppressed by a surge of plasminogen activator inhibitor-1 enhanced by resuscitation lasting for approximately 12 h, called fibrinolytic shutdown, which is pathologic if it continues longer than 24 h. A more protracted shutdown is associated with delayed mortality from traumatic brain injury and multiorgan failure compared with the hyperfibrinolysis seen in hemorrhagic deaths.
Early or late trauma-induced coagulopathy is not effectively diagnosed with a specific laboratory profile. The transition from the hypocoagulable to hypercoagulable state usually occurs within 2 h. Risk factors include evidence of excessive clot strength and continued fibrinolytic shutdown assessed by viscoelastic hemostatic assays. The contribution of ongoing thromboinflammatory pathophysiology is poorly understood but likely also impacts outcomes.40
Cardiac Surgery with CPB
CPB generates well-described hemostatic activation and acquired coagulopathy that can be complicated by life-threatening bleeding. Up to 10% of cardiac surgical patients will experience major bleeding, and 20 to 40% will receive transfusions, especially if the procedure is a reoperation or complex procedure, or is complicated by numerous other patient and procedural-related factors.14,24,41–43
The etiology of CPB coagulopathy is multifactorial and complex,2,42,44 and may result from interrelated factors. First, hemodilution from CPB circuit prime immediately reduces all factors in the blood, including coagulation factors, inhibitors, and activation biomarkers by 30 to 40%. Second, whole blood loss from surgical bleeding can result in acquired coagulopathy, consumption, and loss of coagulation factors and fibrinogen. Third, tissue factor release into the circulation from exposure to surgical trauma and air activates consumption of coagulation factors and platelets as well as increased fibrinolysis. Fourth, contact activation of the hemostatic system due to the nonendothelial circuit components depletes coagulation factors.1 If not otherwise contraindicated, systemic heparin is commonly administered as the standard systemic anticoagulant during CPB to bind and activate antithrombin and inhibit thrombin formation. However, thrombin is resistant to the effects of heparin when it is bound to soluble and circuit-bound fibrin, thus necessitating high-intensity dosing of heparin for circuit anticoagulation. Fifth, hyperfibrinolysis from CPB stimulation of endothelial cell release of tissue plasminogen activator leads to plasmin generation, fibrinolysis, and clot lysis. Conversely, a hypofibrinolytic state can also occur postoperatively as plasminogen activator inhibitor-1 variably increases into the first postoperative day, predisposing some patients to thrombosis instead of hemorrhage.1 Sixth, reduced platelet count and function arise from platelet binding via glycoprotein-IIb/IIIa receptors to fibrinogen bound to the CPB circuit. CPB also stimulates platelet activation via protease-activated receptor-1 and -4. Excess plasmin also can partially inactivate platelets through cleavage of their glycoprotein-Ib receptor. Seventh, inflammation may be exacerbated by multiple mechanisms. Surgical trauma and the CPB circuit may upregulate inflammatory cytokines, which cause coagulation factor activation and dysregulated fibrinolysis. A systemic inflammatory response and a procoagulant state also result from activation of neutrophils and monocytes, increasing tissue factor expression while decreasing protein C activity. Factor XII and contact activation contribute to bradykinin release and complement activation, and propagate the systemic inflammatory response.45 Pericardial blood also contains activated leukocytes, high levels of tissue factor, and cell-derived microparticles generated from multiple cell types and can contribute to a procoagulant state.1 Residual heparinization from systemic administration during CPB that is not adequately reversed with protamine or heparin rebound after administration can contribute to bleeding. Of note, protamine given in higher dosages than necessary to reverse actual heparin concentrations impairs coagulation.46 This condition is the basis for measuring heparin levels when using a protamine titration assay such as the Hepcon heparin management system (Medtronic, USA). Clinically, titrated protamine dosing appears to translate in reduced postoperative blood loss and transfusion rates.46 Thus, potential aggregate mechanisms contributing to inadequate hemostasis after separation from CPB in a bleeding patient may include disturbances in platelet function and thrombin generation, factor depletion, hypofibrinogenemia, and hyperfibrinolysis.42
Examples of efforts to minimize hemostatic activation and better preserve normal hemostatic mechanisms after CPB have incorporated procedural changes (washed cardiotomy blood), circuit modifications (miniaturization, heparin-bonding), and antifibrinolytic or anti-inflammatory pharmacologic adjuncts, all with varying implementation and impact.1,42,47–49 A combined early and ongoing approach to reduce hemostatic activation and its downstream consequences may result in fewer thromboinflammatory-related contributions to patient morbidity and mortality after CPB.
Postpartum Hemorrhage
Bleeding at the time of childbirth is a frequent, challenging, and often devastating clinical emergency. Postpartum hemorrhage is defined as blood loss exceeding 500 ml with vaginal delivery, or 1,000 ml with cesarian section. Major postpartum hemorrhage is classified as moderate (1,000 to 2,000 ml) and severe (greater than 2,000 ml). Massive postpartum hemorrhage is defined as bleeding of greater than 2,500 ml, a hemoglobin drop of more than 4 g/dl, transfusion of five or more erythrocyte units, or the need for an invasive procedure or coagulopathy treatment. Massive postpartum hemorrhage occurs in approximately 6 of 1,000 deliveries and contributes to up to 50% of maternal deaths worldwide.50,51
The hemostatic changes associated with postpartum hemorrhage are somewhat different from those of acute trauma or cardiac surgery using CPB.52,53 The type, severity, timing, and onset of coagulopathy vary depending on the etiology of postpartum hemorrhage.54 The coagulopathy of postpartum hemorrhage is multifactorial and includes dilutional coagulopathy, localized consumption, DIC, and increased fibrinolysis.50 Dilutional coagulopathy occurs when postpartum hemorrhage losses are replaced with crystalloid and colloid. Localized consumption may occur in the placenta and uterus from placental abruption or retained/adherent placenta. Classic systemic DIC is not typical of postpartum hemorrhage but can be associated with amniotic fluid embolus, infection/sepsis, retained fetal remnants, and severe cases of placental abruption and pre-eclampsia propagated by placental release of tissue factor. Blood loss may be minimal until DIC consumes the coagulation reserve.51–53
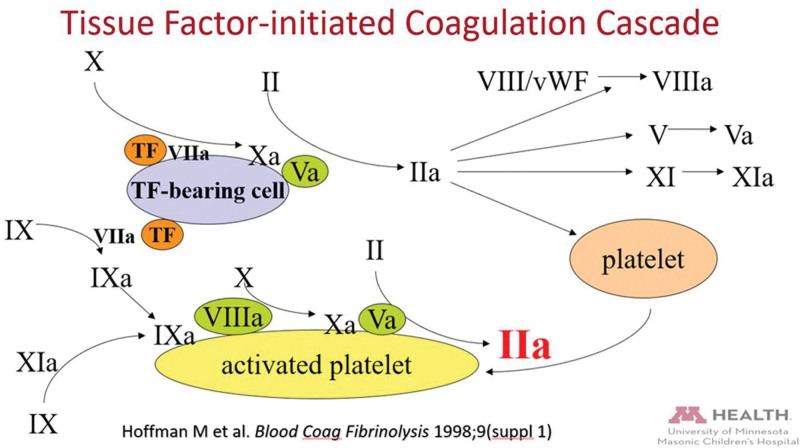
Mechanistic underpinnings of coagulopathy in postpartum hemorrhage are widely variable in etiology and severity.51 Uterine atony and surgical/genital tract trauma-induced bleeding are not accompanied by significant coagulopathy, even with relatively large blood loss, unless a predominantly dilutional late coagulopathy evolves. Varying degrees of localized consumption may occur with the development of large intrauterine clots. Placental abruption may be accompanied by severe and abrupt DIC from the significant release of tissue factor from the damaged placenta and uterus. Although the fibrinogen levels decline, after abruption, major factor deficiencies not initially observed may ultimately be severe despite minimal initial localized blood loss. Severe and rapid DIC associated with amniotic fluid emboli is likely triggered by amniotic fluid tissue factor. Thrombosis of pulmonary blood vessels and severe systemic inflammatory response can provoke catastrophic deterioration. Massive hemorrhage with DIC follows within 4 h in 40% of the initial survivors.55 Pre-eclampsia is a major cause of maternal and fetal morbidity and mortality from DIC, with macroscopic fibrin deposits and multiorgan failure in severe cases.56 Vascular endothelial cell damage or activation, including placental ischemia, exacerbate the normal prothrombotic balance of pregnancy.56,57 Localized consumption can progress to systemic consumption, hypocoagulability, and increased risk of postpartum hemorrhage (fig. 2).
Fig. 2.
Schematic model of normal hemostasis. CPB, cardiopulmonary bypass; vWF, von Willebrand factor. From Hofmann M et al., Blood Coag Fibrinolysis 1998; 9(suppl 1), modified by the University of Minnesota.
Mild Inherited and Acquired Coagulation Disorders
Detection of Mild Inherited Bleeding Disorders
Massive hemorrhagic diathesis can be caused by disorders of primary hemostasis (von Willebrand disease, platelet disorders), secondary hemostasis (hemophilia A and B), and disturbance of the fibrinolytic system, connective tissue, or vascular formation.58,59 These conditions are mostly diagnosed before adulthood. However, less severe disorders might have gone undiagnosed and contribute to unexpected bleeding in major surgery. The first step in the diagnostic approach is quantifying bleeding symptoms resulting from minor hemostatic challenges, including dental extraction, minor surgery or trauma, epistaxis, or menorrhagia. The bleeding assessment tool of the International Society on Thrombosis and Haemostasis can be used for adults and children.60 A severity score is calculated, and for patients at increased risk (score 4 or greater in men, 6 or greater in women, 2 or greater in children), this examination should be followed by a systematic diagnostic laboratory workup.
In patients with an increased bleeding risk of major surgery, it is important to identify these potential inherited bleeding disorders. The activated PTT is often prolonged in factor deficiencies such as hemophilia A and B, hemophilia C, sometimes in von Willebrand disease (as domains of this macromolecule bind and protect factor VIII) in rare isolated factor deficiencies and in dys- or hypofibrinogenemia.61 However, prolongation of the activated PTT is also observed in common conditions that are usually not associated with increased bleeding, such as deficiencies of the contact activation factors (e.g., factor XII) and anticardiolipin antibodies due to antiphospholipid syndrome.59 Preoperative bleeding risk evaluation with the International Society on Thrombosis and Haemostasis bleeding assessment tool and laboratory testing with prothrombin time and activated PTT do not accurately detect mild bleeding disorders in patients undergoing elective surgery.62 In a study of 1,502 surgical patients, 5.5% had a positive questionnaire and/or abnormal coagulation test results for PTT/INR. None of these patients reported major bleeding.62 However, even when combining the questionnaire with more extensive laboratory testing including thrombin time, euglobulin lysis time to assess fibrinolysis, and the Platelet Function Analyzer-100 (USA) in vitro bleeding time to assess primary hemostasis, results remained unsatisfactory.63 In only 8.8% of patients with reported bleeding symptoms, hemostatic abnormalities were found, while in 10.5% of patients without reported bleeding symptoms, test results were abnormal. In this regard, the diagnostic workup revealed a high specificity but low sensitivity.
Despite limitations, a thorough clinical assessment and detailed questionnaire for bleeding symptoms should be considered with critical scoring patients, and evaluation by a hematologist may be helpful. For such patients, algorithms for the diagnosis of mild and moderate inherited bleeding disorders have been proposed, including the current system of the European Hematology Association (The Hague, The Netherlands).60 Other algorithms with a substantially different laboratory workup, particular in the first stage, and early genotyping have also been suggested.58,64 In case of a substantial coagulation system abnormality, guidelines suggest perioperative management should be provided in concert with a hematologist.
Drug-related, Acquired Coagulation Disorders
In the aging multimorbid population, an increasing number of patients are on oral antiplatelet agents, anticoagulants, especially the new direct oral anticoagulants, or combined therapy.65,66 Urgent surgery in patients treated with intravenous therapy such as direct thrombin inhibitors (argatroban or bivalirudin) or antiplatelet agents also plays a role, particularly in patients requiring urgent cardiac surgery. Agent-specific timing for discontinuation of the anticoagulant or antiplatelet drug is reported in pharmacologic studies and guidelines.67–76 Nevertheless, individual thrombotic risk of the patients varies considerably, so that case-by-case evaluation should be considered. Particularly in patients with antiplatelet therapy after recent placement of coronary artery stents, discontinuation of therapy should be discussed interdisciplinary to weigh the potential risks of bleeding and (stent) thrombosis against each other.68 However, in patients with severe trauma or emergent cardiac surgical cases, residual anticoagulant effects may contribute to excessive bleeding. In this situation, specific or nonspecific reversal agents should be considered. In the context of cardiac surgery, extracorporeal devices can be implemented into the CPB to eliminate certain drugs. However, these strategies have not been validated in large prospective trials, and data are limited to in vitro settings, reports of small case series, or anecdotal case reports. Such strategies include hemofiltration for agents like bivalirudin or tirofiban or the hemadsorption of ticagrelor, rivaroxaban, edoxaban, and argatroban.77–81 Nevertheless, in severe trauma, with massive coagulopathy and residual drug effect, such elimination strategies might be considered within a damage control strategy after the patient has been transferred to the intensive care unit (ICU; table 3).
Table 3.
Antiplatelet Agents and Anticoagulants with Possible Reversal and Elimination Strategies
Standard and Advanced Laboratory Tests
Most national guidelines, including French Society of Anaesthesia and Intensive Care (Paris, France), British Committee for Standards in Haematology (London, United Kingdom), and American Society of Anesthesiologists (Schaumburg, Illinois), do not recommend routine preoperative coagulation testing due to the outlined limitations of standard laboratory tests to detect clinically relevant bleeding disorders, but favor the use of a preoperative bleeding assessment tools.82–85 It does remain usual practice in patients undergoing CPB procedures with high-dose heparinization86,87 that monitoring of adequate systemic anticoagulation is performed via the activated clotting time with target values typically greater than 480 s. However, activated clotting time assays like the activated PTT are measures of the contact pathway inhibition. Most clinically asymptomatic prolongations of the activated PTT are caused by low levels of coagulation factors XI, XII, or anticardiolipin antibodies.62 In this condition, even an adequately prolonged activated clotting time might underestimate the true heparin requirement to suppress tissue factor–associated hemostatic activation related to CPB. Using a tissue factor–based heparin monitoring device is a potential option for such patients.88 In the setting of cardiac surgery, heparin resistance, the need for high heparin doses (greater than 600 U/kg) to achieve the target activated clotting time value, is a major concern.86,87 Reasons for heparin resistance include antithrombin deficiency, hyperfibrinogenemia, and thrombocytosis.86,87,89 Preoperative knowledge of risk conditions for both increased in vitro sensitivity to heparin and heparin resistance may help to adjust the anticoagulation strategy or anticoagulation monitoring practice. Therefore, in this particular setting, preoperative monitoring of the activated PTT, antithrombin and fibrinogen values, and the platelet count are important information to obtain before surgery.
A detailed medication and symptomatic bleeding history should identify oral anticoagulant or antiplatelet drugs and their last intake. Laboratory tests can be used to monitor effects or residual effects on coagulation, which, particularly in patients with multiorgan dysfunction, may be present despite timely termination of drug intake. For example, the INR is the reference assay for warfarin and VKA therapy. Platelet function testing (e.g., impedance aggregometry) facilitates monitoring of preoperative antiplatelet drug effects.90 Preoperatively, direct oral anticoagulants (DOACs) can be monitored with specific calibrated assays or, in case of targeting factor Xa, with a global (uncalibrated) anti-Xa assay as a qualitative screening tool.71 Recent recommendations provided a pragmatic approach for DOAC monitoring.71
When the unconscious patient requires emergency surgery or when a thorough history or assessment is not possible, a qualitative screening of the coagulation system for inherited and acquired coagulation disorders can be helpful (table 4).71,91–93 Even given the limitations of available routine laboratory coagulation assays, such a protocol may be helpful to provide an initial assessment of the coagulation to screen for inherited coagulation disorders and/or potential use of anticoagulants.94–97 Limitations of laboratory tests, particularly in severe trauma, should be considered. This includes the fact that colloids and fibrinolysis may alter prothrombin time, activated PTT, and fibrinogen assays.98
Table 4.
Possible Rapid Screening Assays for Acquired and Inherited Coagulation Disorders in the Unconscious Patient
Perioperative Assessment of Hemostasis with Viscoelastic Tests
Despite the routine clinical use of standard coagulation tests in the perioperative setting, they do not predict bleeding.99 The in vitro sensitivity of different activated PTT reagents to detect certain clotting factor deficiencies is highly variable and differs depending on the deficient factor(s).100 In this regard, limitations are comparable to the prothrombin time method with significant variations in the activity of the activating tissue factor, which lead to the introduction of the INR to overcome this problem.98
Standard coagulation assays, including fibrinogen assays, are susceptible to fibrin split products, heparin, lipids, and hemodilution.98,101 A comparative study in cardiac surgical patients reported substantial differences among fibrinogen concentrations measured in six laboratories, all using different Clauss techniques, considered the reference laboratory method.101
Viscoelastic testing, especially thromboelastography and rotational thromboelastometry (ROTEM), provide insight into the status of the coagulation factors, fibrinogen action, platelet count, and fibrinolysis.102 However, viscoelastic tests are insensitive to the effects of oral antiplatelet agents on platelet function. These tests are increasingly used to rapidly evaluate the status of the coagulation system and guide hemostatic therapy102 and are recommended in recent guidelines for cardiac surgery and trauma as part of treatment algorithms.103–106 However, in obstetrics and postpartum hemorrhage, data are more sparse, and further research is needed.107,108
The main advantage of viscoelastic testing is the rapid turnaround time and availability of results,99 which are important in rapidly changing scenarios with massive transfusion, such as in cardiac surgery and severe trauma. Kaolin-activated thromboelastography is a heparin-sensitive assay in which kaolin is used to activate the intrinsic coagulation cascade. A corresponding fibrinogen assay is available in which platelet aggregation is inhibited. The rapid thromboelastography is tissue factor–activated, provides results relatively quickly, and is predominately used in patients with severe trauma.109 The commonly used tissue factor–activated ROTEM assays are sensitive to concentrations of coagulation factor VII.99 These assays thus reflect the effect of exogenous factor VII included in the four-factor prothrombin complex concentrates (PCCs) when administered for hemostatic resuscitation in cardiac surgery and severe trauma.99,110 Thromboelastography and ROTEM results also allow early detection of either hyperfibrinolysis or fibrinolytic shutdown, of particular importance in hemostasis management in severe trauma.102 Newly developed viscoelastic test systems still require validation of clinical efficacy in large clinical studies.102 The ClotPro system (enicor GmbH, Germany) is similar to the ROTEM technique, but offers a different portfolio of assays. The Quantra hemostasis analyzer (HemoSonics L.L.C., USA) uses the technique of sonorheometry.111 The TEG® 6s Hemostasis Analyzer System (Haemonetics Corporation, USA) uses a resonance method to measure clot viscoelasticity. The resulting graphical representation is nearly identical to that of thromboelastography. All new systems have recently been thoroughly reviewed.112
Several clinical trials have assessed the impact of using transfusion algorithms based viscoelastic hemostatic assays on bleeding and transfusion in different surgical and nonsurgical populations. A randomized monocentric trial in complex cardiac surgery compared transfusion protocols based on point-of-care monitoring with viscoelastic hemostatic assays and platelet function testing using impedance aggregometry with a protocol based on standard laboratory tests.113 The primary outcome was erythrocyte transfusion within 24 h of inclusion. The study was terminated early after inclusion of 50 patients in each arm because interim analysis showed a significantly higher red cell transfusion rate in the standard laboratory arm compared to the viscoelastic hemostatic assays arm (median [25th to 75th percentile], 5 [4 to 9] vs. 3 [2 to 6]; P < 0.001). The fact that highly significant results were obtained in such a complex scenario, in which only one actor was changed, after enrollment of only 100 patients is impressive. However, nearly 25% of patients in the conventional arm and 2% of patients in the viscoelastic hemostatic assays arm received recombinant activated factor VIIa, despite the fact that approximately 50% of patients in both groups had received fibrinogen concentrate and/or a four-factor PCC. In 2016, Karkouti et al. published the results of a pragmatic multicenter stepped-wedge cluster randomized controlled trial of a point-of-care–based transfusion algorithm in consecutive patients undergoing cardiac surgery with CPB at 12 hospitals.114 After a 1-month data collection at all participating hospitals, a transfusion algorithm incorporating point-of-care hemostatic testing was sequentially implemented at two hospitals at a time in 1-month intervals, with the implementation order randomly assigned. No other aspects of care were modified. Among the 7,402 patients studied, 3,555 underwent surgery during the control phase and 3,847 during the intervention phase. The trial intervention reduced rates of erythrocyte units, platelet transfusion, and major bleeding, but had no effect on other blood product transfusions or major complications. The authors conclude that their findings support the broader adoption of point-of-care hemostatic testing into clinical practice.
Although viscoelastic hemostatic assays have been studied in many retrospective studies in trauma patients, the number of prospective randomized trials is limited. The Implementing Treatment Algorithms for the Correction of Trauma-Induced Coagulopathy (ITACTIC) study was a multicenter, randomized controlled trial comparing outcomes in trauma patients who received empiric massive hemorrhage protocol augmented by either viscoelastic hemostatic assays or conventional coagulation testing.115 The nearly 400 patients in the intention-to-treat population were well-balanced with regard to demographics, injuries, and admission characteristics. The authors failed to demonstrate a benefit of using viscoelastic hemostatic assays. The literature on postpartum hemorrhage is also limited to retrospective studies. In a recent systematic review, the authors identified only two randomized controlled trials on thromboelastography or ROTEM use in obstetrics.107 ROTEM may be used to guide transfusion therapy for postpartum hemorrhage. Thromboelastography and ROTEM can detect the hypercoagulable changes associated with pregnancy and can help detect coagulopathy before and after labor in patients with pre-eclampsia.116 Variability between study protocols and results suggests the need for future large prospective high-quality studies with standardized protocols to investigate the utility of thromboelastography or ROTEM in assessing risk for thrombosis and hemorrhage as well as in guiding prophylaxis and treatment in obstetric patients.
Management Options to Treat Microvascular Bleeding and Reverse Coagulation Abnormalities
In the last decade, guidelines for perioperative bleeding report specific management algorithms and particularly emphasize the use of viscoelastic testing and the potential of targeted hemostatic resuscitation with coagulation factor concentrates.50,67,69,105,117 Strategies involved in the management of bleeding include controlled (e.g., cardiac or orthopedic surgery) and uncontrolled (e.g., trauma, postpartum hemorrhage) scenarios. While hypothermia is sometimes used as a neuroprotective mechanism under controlled circumstances, inadvertent hypothermia is associated with dysregulation of coagulation enzymes, platelet dysfunction, fibrinolysis, endothelial injury, and worse outcomes.118,119 Recent guidelines recommend early application of measures to reduce heat loss to achieve and maintain normothermia (Grade 1C) to optimize coagulation.105 Additionally, metabolic acidosis and hypocalcemia often present in uncontrolled hemorrhage and are each associated with increased coagulopathy, transfusion requirements, and mortality.120 Hypocalcemia has been found in approximately 50% of severely injured patients121 and the majority of massive transfusion recipients.120
Activation of the fibrinolytic system is an important component of excessive bleeding in trauma and surgery that leads to activation of the fibrinolytic pathway.122 Antifibrinolytic agents have been used extensively to prevent or treat fibrinolysis. The antifibrinolytic agents used are the lysine analogs, tranexamic acid, and epsilon aminocaproic acid. Landmark studies showing the effectiveness of tranexamic acid, as measured by a reduction of all-cause mortality or death due to severe bleeding, are the Clinical Randomization of an Antifibrinolyticin Significant Hemorrhage (CRASH) trials in severe trauma and brain injury and the World Maternal Antifibrinolytic (WOMAN) trial in postpartum hemorrhage.123–125 However, the performance and results of the large CRASH-2 study have been a subject of intensive controversial debate,126 as the reduction in mortality was subtle and transfusion rates in the treatment arm not reduced. It is noteworthy that only half of the patients were transfused, and only a small number of patients required surgery. In cardiac surgery, the Aspirin and Tranexamic Acid for Coronary Artery Surgery (ATACAS) trial showed a reduction of postoperative blood loss and the re-exploration rate in patients having received tranexamic acid compared to those without.127 However, treatment group patients undergoing open-heart surgery showed an increased rate of convulsive seizures, which, within the ongoing trial, resulted in a significant reduction of the dose from a 100 mg/kg bolus to a 50 mg/kg bolus. The mechanism of this dose-dependent effect of tranexamic acid, which is restricted to open-heart cardiac surgery, is a disinhibition of cerebral γ-aminobutyric acid receptors.128 In the most recent Outcome Impact of Different Tranexamic Acid Regimens in Cardiac Surgery with Cardiopulmonary Bypass (OPTIMAL) trial in cardiac surgery, established high-dose and low-dose tranexamic acid protocols have been compared.129 High-dose tranexamic acid (cumulative dose approximately 100 mg/kg) showed a modest increased efficacy, as measured by patients transfused with red blood cells, when compared to the low-dose protocol (cumulative dose approximately 20 mg/kg) and revealed noninferiority in the composite primary safety endpoint consisting of 30-day mortality, seizure, kidney dysfunction, and thrombotic events.129 However, this study included only patients who were not older than 70 yr, and the mean age in both groups was only 53 yr. In this regard, the elderly patient population, which potentially has a high intraoperative seizure risk, may not have been adequately represented, potentially limiting the validity of the results.
Based on current evidence, guidelines recommend the prophylactic administration of antifibrinolytic agents within 3 h of trauma or bleeding onset to reduce bleeding, transfusion, and mortality. Evidence that antifibrinolytics agents increase the risk of thrombotic complications is lacking. In trauma, there is a concern regarding fibrinolytic shutdown39 and the potential role of antifibrinolytic agent administration more than 3 h after the event. In cardiac surgery, optimal tranexamic acid dosing to balance efficacy and safety still needs further investigation.
In the presence of major bleeding and coagulopathy, current management strategy relies on the replacement of the blood volume lost with allogeneic transfusions and the missing coagulation factors. Particularly in severe trauma, following current guidelines, initial hemostatic resuscitation usually is performed by balanced ratios of red blood cells, fresh frozen plasma, (FFP), and platelets.130 However, during the last decade, goal-directed therapy based on coagulation monitoring has been increasingly used, and includes viscoelastic testing. This approach has also promoted the use of coagulation factors concentrates rather than whole blood or plasma. Although the use of factor concentrates remains the topic of debate, the rationale comes from the more specific and efficient replacement of the missing coagulation factors with those concentrates when compared to plasma or whole blood.131 It is indeed important to remember that plasma and whole blood contain only physiologic concentrations of coagulation factors, and therefore large volumes (greater than 20 to 30 ml/kg) are needed to obtain a significant improvement in plasma levels.132 Severe side effects, such as transfusion-related acute lung injury and transfusion-associated circulatory overload, are described.133 However, data for the efficacy and safety of this widely used practice and guideline recommended intervention are scant and diluted by the large proportion of studies with prophylactic FFP transfusions.134,135
Particularly in trauma, there is an ongoing debate about the use of fresh whole blood transfused within 24 h of donation, a strategy originating mainly in military medicine. A recent meta-analysis found no difference in mortality when comparing fresh whole blood to component therapy (odds ratio, 1.00; 95% CI, 0.65 to 1.55; P = 0.061).136 However, when only studies of the highest quality in terms of physiology and injury characteristics were included in the analysis, the adjusted odds ratio was 0.29 (95% CI, 0.13 to 0.58; P < 0.01). Another recent meta-analysis of studies in trauma and surgery patients found no difference in harm when comparing the two strategies.137 In addition to the off-label use of agents such as three-factor PCC, factor eight inhibitor bypassing activity (FEIBA), and recombinant activated factor VII, several new anticoagulant concentrates are now commercially available.
Fibrinogen, a critical hemostatic factor for clot formation in the management of perioperative bleeding in cardiac surgical patients, has been extensively studied. Fibrinogen is also the first factor to reach a critical level in the presence of bleeding.35 Normal fibrinogen concentrations are 200 to 400 mg/dl in the nonparturient, but can be greater than 400 mg/dl during the third trimester of pregnancy. Older guidelines suggested a transfusion trigger of 100 mg/dl of fibrinogen, while current European guidelines recommended levels of greater than 200 mg/dl. To achieve the target fibrinogen levels, 3 to 4 g fibrinogen concentrate, or 15 to 20 units cryoprecipitate, are recommended in the bleeding patient (tables 5 to 7).40,67,105,110,138–144
Table 5.
Trigger Values for Hemostatic Disturbances Based on Viscoelastic Point-of-care Results in the Bleeding Patient
Table 7.
Hemostatic Therapy in the Bleeding Patient According to Recent Guidelines/Recommendations
Table 6.
Trigger Values for Hemostatic Disturbances Based on Conventional Coagulation Test Results in the Bleeding Patient
In a small randomized controlled single-center trial in 61 patients undergoing major thoracic or thoracoabdominal aortic surgery, transfusion of fibrinogen concentrate to a very high threshold of maximum clot firmness of 22 mm in the functional fibrinogen assay of the ROTEM system was compared with placebo.113 The primary endpoint was the number of units of allogenic transfusions within 24 h after administration of study medication. The results were impressive: in the fibrinogen arm, the mean transfusion rate after administration of a median dose of 8 g fibrinogen was 2 U versus 13 in the placebo arm (P < 0.001). The protocol was reassessed in the large randomized evaluation of fibrinogen versus placebo in the complex cardiovascular surgery (REPLACE) trial, which enrolled 519 patients from 34 centers.145 However, in this study, fibrinogen concentrate was associated with an unexpected increase in allogenic blood transfusions compared to placebo (median [interquartile range], 5.0 [2 to 11] vs. 3.0 [0 to 7]; P = 0.026).
In another randomized controlled single-center trial of 116 high-risk cardiac surgery patients, first-line fibrinogen supplementation with the same high fibrinogen threshold was compared to placebo.146 Fibrinogen supplementation with a median dose of 4 g resulted in a significantly lower primary endpoint of blood product transfusion rate (odds ratio, 0.40; 95% CI, 0.19 to 0.84; P = 0.015) and postoperative bleeding (median [interquartile range], 300 ml [200 to 400] vs. 355 ml [250 to 600]). Of note, only in the treatment arm could patients receive 7 U/kg of a four-factor PCC when the coagulation time in the extrinsically activated assay of ROTEM was less than 80 s.
In another single-center randomized controlled trial in 120 high-risk cardiac surgery patients, there was no significant difference in the primary outcome of intraoperative blood loss of a median 50 ml (interquartile range, 29 to 100 ml) versus 70 ml (interquartile range, 22 to 145 ml) when fibrinogen concentrations exceeded 2.5 mg/dl using fibrinogen concentrate compared with placebo.147
In a large randomized cardiac surgery clinical trial, patients with clinically significant bleeding and hypofibrinogenemia after cardiac surgery were randomized to receive either 4 g fibrinogen concentrate or 10 U cryoprecipitate within 24 h after CPB.148 The study confirmed fibrinogen concentrate was a safe and an effective alternative to cryoprecipitate for fibrinogen repletion. Although fibrinogen concentrate has been studied in the context of postpartum hemorrhage and trauma,149–152 there is currently a lack of robust evidence to provide strong recommendations regarding the use of fibrinogen concentrate as first line for fibrinogen supplementation in various perioperative bleeding situations, and further investigation is needed.
The three-factor PCCs are purified coagulation factor concentrates that include coagulation factors II, IX, and X. The approved indication of three-factor PCC is hemophilia B. The four-factor PCCs were continuously developed to antagonize effects of VKA therapy and include procoagulant factors II, VII, IX, and X and anticoagulant proteins C and S in variable concentrations. Some preparations include minimal antithrombin and heparin (table 8).110,153,154 The use of PCCs for urgent reversal of VKA effects is recommended in current guidelines.3 A meta-analysis showed that the four-factor PCCs are more effective when used in this indication than the three-factor PCCs.155 With the increased use of DOACs, PCCs are now also considered to treat the coagulopathy induced by those agents in trauma and surgical patients.156 Although PCCs are increasingly used off-label to treat acquired coagulopathy in trauma and surgical patients, the evidence remains poor.110 In a recently published trial,157 adult patients requiring coagulation factor replacement for bleeding during cardiac surgery were randomized to receive either PCC or FFP. Hemostatic effectiveness was defined as the administration of any hemostatic therapies from 60 min to 4 and 24 h after initiation of the intervention, the amount of allogeneic blood components administered within 24 h after the start of surgery, and avoidance of erythrocyte within 24 h after start of surgery. Hemostatic therapy was not required at the 4-hour time point for 80% in the PCC group and for 68% in the plasma group, nor at the 24-hour time point for 76% in the PCC group and for 66% patients in the plasma group (P = 0.28). The median numbers of units for 24-hour cumulative allogeneic transfusions were 6.0 in the PCC group and 14.0 units in the plasma group (P < 0.001). The authors concluded that further adequately powered studies are needed to determine whether PCC is a suitable substitute for mitigation of bleeding in cardiac surgery. In another study, administration of 15 U/kg of a four-factor PCC was compared with FFP in 100 patients with bleeding after CPB.158 Transfusion of PCC resulted in fewer erythrocyte transfusions after treatment, whereas overall intraoperative transfusion rates did not differ between groups. However, seven of the patients in the PCC groups versus none in the FFP group were not transfused by the end of the first postoperative day. A recent meta-analysis of larger propensity-matched observational studies evaluated the use of PCC, with or without additional use of FFP, in patients with severe trauma. Compared to FFP only, the use of PCC resulted in improved survival, clinical recovery, and reduced transfusions without, however, increasing thromboembolic events.159 New recommendations of the American Heart Association (Dallas, Texas) and American Stroke Association (Dallas, Texas) indicate that four-factor PCC rather than FFP should be first-line therapy in anticoagulated patients with spontaneous intracerebral hemorrhage.160 This might impact therapeutic considerations for patients with traumatic brain jury and a similar condition. Further studies are needed to investigate procoagulant interactions between various hemostatic components and the potential for thromboembolic complications. The Factors in Initial Resuscitation of Severe Trauma 2 (FiiRST-2) trial will determine the impact of fibrinogen concentrate and PCC used together as an early hemostatic therapy in bleeding trauma patients, as compared with the standard massive transfusion protocol that infuses one plasma unit for every one or two erythrocyte units.161 This trial will provide efficacy data on the number of allogenic blood products transfused, coagulation tests, and clinical and safety endpoints.
Table 8.
Coagulation Factors Outside the Indication of Inherited Coagulation Disorders
Strategies for Uncontrollable Microvascular Bleeding
In patients with severe bleeding who do not respond to conventional therapy and local hemostatic materials,68 other potent clotting factor concentrates such as recombinant activated factor VII, the factor VIII inhibitor bypassing activity complex, which contains clotting factors II, IX, X, and activated factor VII, or concentrates of clotting factor XIII have been reported. Although recombinant factor VIIa is indicated for hemophilia with inhibitors, acquired hemophilia, patients with congenital factor VII deficiency, Glanzmann thrombocytopenia, and in Europe in postpartum hemorrhage,162,163 multiple studies report the off-label use in bleeding unresponsive to other hemostatic therapy.163 Although studies report efficacy in cardiac surgery,164 most studies reporting its use are retrospective observational reports of patients having received multiple transfusions and other therapeutic agents for refractory bleeding.163 A prospective analysis of 4,468 nonhemophilia subjects (4,119 patients and 349 healthy volunteers), arterial thromboembolic events of factor VIIa patients versus placebo were 5.5% versus 3.2%, but venous thromboembolic events were similar (5.3% vs. 5.7%).165 Nevertheless, rates of thrombosis were higher in patients older than 65 yr (9% vs. 4%) and particularly high in those older than 75 yr (11% vs. 4%). A large dataset in cardiac surgery, trauma, and postpartum hemorrhage is available from the New Zealand Hemostasis Registry.166 In this dataset, reduction or cessation of bleeding was reported in 74% of patients, and in approximately 11% of patients, thromboembolic complications were observed.166
The standard approved dose of recombinant activated factor VII for hemophiliac patients is 90 µg/kg. However, in cardiac surgery, a lower dose of 20 to 40 µg/kg has been recommended.140 Results of more recent observational studies might indicate that an even lower dosage of approximately 13 µg/kg is effective in reducing bleeding without being associated with increased thromboembolic or renal complications.167
In a large randomized placebo-controlled multicenter study in cardiac surgery, replenishing factor XIII levels with recombinant factor XIII given after CPB had no effects on transfusion rates and need for reoperation.168 In a larger retrospective study in trauma patients, low factor XIII levels after hospital admission correlated with an adverse clinical course of patients.169 Replacement of factor XIII levels with factor XIII concentrate failed to reduce transfusion demands. Further clinical studies are needed to clarify the population, dosing interval, and outcomes if using these agents for uncontrollable bleeding.
The concept of leaving an abdomen or chest temporarily open is a modification of the concept of damage control surgery.170 In patients with intractable bleeding, the large wound areas are tamponaded or “packed,” and further hemostatic resuscitation is performed in the ICU.170 In cardiovascular surgery with uncontrollable bleeding, this strategy may be used after ventricular assist device implantation, type A aortic dissection, and surgery for ruptured abdominal aortic aneurysm.171–173 Abdominal packing for 24 to 48 h is also an option after hysterectomy in case of severe bleeding associated with postpartum hemorrhage.174 The potential benefits of such a strategy are the reduction of active bleeding via local compression and tamponade, better preservation of temperature in the ICU, and avoidance or reduction of ongoing massive transfusion or presumably critical dosages of powerful coagulation factor concentrates, which involve the risk of thromboembolism. This strategy has to be balanced against the risk of infection and necessity of continued mechanical ventilation.
Diagnostic and Therapeutic Strategies in Severe Coagulopathy: Limits of Current Evidence
Despite the demonstrated benefits on transfusion requirement, routine use of viscoelastic testing has not been proven to improve important clinical outcomes such as morbidity and mortality.175 However, the impressive results achieved in a single center in cardiac surgery using a point-of-care monitoring-based transfusion algorithm remain controversial.113 The extremely high dose of recombinant activated factor VII in this study raises the question of the extent to which center-specific effects influenced the study results. Although thromboelastography and ROTEM have been widely used for years, it remains unclear why the trigger values for hemostatic interventions vary between international recommendations and in different clinical scenarios (table 5). Limited evidence based on the few well-conducted, adequate multicenter trials most likely contributes to this observation. This lesson must be kept in mind when validating the new viscoelastic hemostatic assay systems that have recently been introduced.
It is important to attempt to reconcile laboratory results obtained with newer diagnostic techniques that are often discordant with established methods. Single data points from isolated laboratory tests cannot describe the entirety of the hemostatic balance, and we should attempt to harmonize information from different coagulation monitoring platforms to better understand the pathophysiology of the individual patient. Similarly, different technologies, such as the new and established viscoelastic tests, should ideally be correlated to evaluate the impact and results of different studies to provide better quality evidence.
The potential limitations of the current evidence with potent hemostatic agents become apparent when considering the results of randomized controlled trials of fibrinogen concentrates in cardiac surgery. The impressive results of the first monocentric pilot study with a very high threshold in aortic surgery could not be confirmed in the subsequent large multicenter study. The results of the smaller studies at individual centers in patients considered to be at particular risk of bleeding are contradictory. The use of different fibrinogen thresholds may have contributed to this observation. However, looking at the clinical endpoints in these studies, such as intraoperative blood loss, which was a median of 50 versus 70 ml in one study, and postoperative blood loss, which was a median of 300 versus 350 ml in the other study, it is reasonable to assume that the bleeding risk of patients was not as high as assumed. In both studies, transfusion rates and the number of allogeneic blood transfusions were very low. Furthermore, it remains unclear why only in the treatment arm of one of these studies was an additional PCC used. Although this criterion was not met by any patient in the study group, the potential for dilution of the study results is evident. The future of fresh whole blood transfusion remains to be seen. In addition to efficacy and safety considerations, such a strategy will require fundamental changes in blood donation and storage logistics.
Reliable data from well-designed trials are the key to increase valid, clinically relevant evidence. However, we consider elementary conditions that should be acknowledged in the design and conduct of such studies. A successful prospective clinical trial should be designed in a multicenter setting to mitigate center-specific effects, with appropriate inclusion criteria for patients at substantially increased bleeding risk. It should contain a feasible trial intervention to assure high compliance, a feasible transfusion algorithm, and harmonization of management strategies to assess meaningful clinical endpoints with timely recruitment of sufficient numbers of study patients to meet power calculations.13,14,176
However, severe coagulopathy leading to excessive microvascular bleeding is a multifactorial condition in which numerous elements are involved in establishing and maintaining the very complex hemostatic balance. It thus is challenging to propose that one single intervention, even when performed within the setting of a well-designed randomized controlled multicenter trial, will finally achieve the goal of adequate hemostasis to safely reduce bleeding and transfusion needs and their associated morbidity and mortality risks. In this regard, we consider that results of clinical studies available to date need to be implemented in complex multimodal diagnostic and therapeutic algorithms, comparable to those recently published by the Society of Cardiac Anesthesiologists (East Dundee, Illinois), for optimizing coagulation and clinical decision-making.140
Conclusions
Severe disorders of the hemostatic system can lead to uncontrollable bleeding. Given the increasing use of antiplatelets and anticoagulants, perioperative management of these acquired coagulation disorders is crucial, requiring optimal timing for discontinuation of therapy, monitoring of potential residual drug effects, and targeted reversal strategies for bleeding management. In contrast to standard anticoagulation testing, modern point-of-care viscoelastic systems provide rapid information on whole blood coagulation that includes fibrinogen, platelets, and fibrinolysis. Transfusion thresholds based on results of these assays are increasingly being incorporated into current guidelines of national and international societies. Important elements of hemostatic resuscitation are antifibrinolytic therapy, replacement of clotting factors and fibrinogen, platelets, and RBC transfusions. In trauma, the optimal timing of antifibrinolytic therapy, and in cardiac surgery, the optimal tranexamic acid dosage, need to be further defined. In addition to therapy with FFP, four-factor PCC and fibrinogen concentrates play an increasingly important role when clotting factor and fibrinogen stores are depleted. Despite increasing reports of interventions with factor concentrates, the results of randomized clinical trials in the aforementioned areas of hemostatic resuscitation are still pending. The role of fresh donated whole blood in hemostatic resuscitation needs further investigation.
Viewing the complexity of coagulopathy and efficacy of intervention options, evidence from adequately conducted randomized clinical trials need to be implemented into multimodal algorithms for patient blood management. These algorithms need to be validated and further developed in appropriate multicenter trials and monitored against large registry databases.
Research Support
Support was provided solely from institutional and/or departmental sources.
Competing Interests
Dr. Steiner reports the following: advisory committee for Octapharma (Paramus, New Jersey), DSMB for PumpKIN trial, hemostasis education for Medtronic (Dublin, Ireland), and U.S. Department of Defense contract “Chilled Platelet Study in Cardiac Surgery (CHIPS)” (Washington, D.C.). Dr. Ghadimi reports the following: research grant support from the International Anesthesia Research Society (San Francisco, California) and Octapharma. Dr. Levy reports the following: advisory committees for Instrumentation Labs (Bedford, Massachusetts), Merck (Rahway, New Jersey), and Octapharma. The other authors declare no competing interests.
Footnotes
This article is featured in “This Month in Anesthesiology,” page A1.
Contributor Information
Gabor Erdoes, Email: juditgabor@mac.com;gabor.erdoes@insel.ch.
David Faraoni, Email: David.Faraoni@bcm.edu.
Andreas Koster, Email: AKoster@hdz-nrw.de.
Marie E. Steiner, Email: stein083@umn.edu.
Kamrouz Ghadimi, Email: kamrouz.ghadimi@duke.edu.
Jerrold H. Levy, Email: jerrold.levy@duke.edu.
References
- 1.Sniecinski RM, Chandler WL: Activation of the hemostatic system during cardiopulmonary bypass. Anesth Analg. 2011; 113:1319–33 [DOI] [PubMed] [Google Scholar]
- 2.Despotis GJ, Avidan MS, Hogue CW, Jr.: Mechanisms and attenuation of hemostatic activation during extracorporeal circulation. Ann Thorac Surg. 2001; 72:S1821–31 [DOI] [PubMed] [Google Scholar]
- 3.Ghadimi K, Levy JH, Welsby IJ: Prothrombin complex concentrates for bleeding in the perioperative setting. Anesth Analg. 2016; 122:1287–300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Levy JH, Dutton RP, Hemphill JC, 3rd, Shander A, Cooper D, Paidas MJ, Kessler CM, Holcomb JB, Lawson JH, Hemostasis Summit Participants: Multidisciplinary approach to the challenge of hemostasis. Anesth Analg. 2010; 110:354–64 [DOI] [PubMed] [Google Scholar]
- 5.Adelborg K, Larsen JB, Hvas AM: Disseminated intravascular coagulation: Epidemiology, biomarkers, and management. Br J Haematol. 2021; 192:803–18 [DOI] [PubMed] [Google Scholar]
- 6.Carson JL, Grossman BJ, Kleinman S, Tinmouth AT, Marques MB, Fung MK, Holcomb JB, Illoh O, Kaplan LJ, Katz LM, Rao SV, Roback JD, Shander A, Tobian AA, Weinstein R, Swinton McLaughlin LG, Djulbegovic B, Clinical Transfusion Medicine Committee of the AABB: Red blood cell transfusion: A clinical practice guideline from the AABB*. Ann Intern Med. 2012; 157:49–58 [DOI] [PubMed] [Google Scholar]
- 7.Rohde JM, Dimcheff DE, Blumberg N, Saint S, Langa KM, Kuhn L, Hickner A, Rogers MA: Health care-associated infection after red blood cell transfusion: A systematic review and meta-analysis. JAMA. 2014; 311:1317–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dutton RP, Lee LA, Stephens LS, Posner KL, Davies JM, Domino KB: Massive hemorrhage: A report from the anesthesia closed claims project. Anesthesiology. 2014; 121:450–8 [DOI] [PubMed] [Google Scholar]
- 9.Kortbeek JB Al Turki SA Ali J Antoine JA Bouillon B Brasel K Brenneman F Brink PR Brohi K Burris D Burton RA Chapleau W Cioffi W, Collet e Silva Fde S, Cooper A Cortes JA Eskesen V Fildes J Gautam S Gruen RL Gross R Hansen KS Henny W Hollands MJ Hunt RC, Jover Navalon JM, Kaufmann CR Knudson P Koestner A Kosir R Larsen CF Livaudais W Luchette F Mao P McVicker JH Meredith JW Mock C Mori ND Morrow C Parks SN Pereira PM Pogetti RS Ravn J Rhee P Salomone JP Schipper IB Schoettker P Schreiber MA Smith RS Svendsen LB Taha W van Wijngaarden-Stephens M Varga E Voiglio EJ Williams D Winchell RJ Winter R: Advanced trauma life support, 8th edition, the evidence for change. J Trauma. 2008; 64:1638–50 [DOI] [PubMed] [Google Scholar]
- 10.Schulman S, Kearon C; Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis: Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost. 2005; 3:692–4 [DOI] [PubMed] [Google Scholar]
- 11.Dyke C, Aronson S, Dietrich W, Hofmann A, Karkouti K, Levi M, Murphy GJ, Sellke FW, Shore-Lesserson L, von Heymann C, Ranucci M: Universal definition of perioperative bleeding in adult cardiac surgery. J Thorac Cardiovasc Surg. 2014; 147:1458–1463.e1 [DOI] [PubMed] [Google Scholar]
- 12.Bartoszko J, Wijeysundera DN, Karkouti K, Callum J, Rao V, Crowther M, Grocott HP, Pinto R, Scales DC, Achen B, Brar S, Morrison D, Wong D, Bussieres JS, de Waal T, Harle C, de Medicis E, McAdams C, Syed S, Tran D, Waters T; Transfusion Avoidance in Cardiac Surgery Study Investigators: Comparison of two major perioperative bleeding scores for cardiac surgery trials: Universal definition of perioperative bleeding in cardiac surgery and European Coronary Artery Bypass Grafting Bleeding Severity Grade. Anesthesiology. 2018; 129:1092–100 [DOI] [PubMed] [Google Scholar]
- 13.Spinella PC, El Kassar N, Cap AP, Kindzelski AL, Almond CS, Barkun A, Gernsheimer TB, Goldstein JN, Holcomb JB, Iorio A, Jensen DM, Key NS, Levy JH, Mayer SA, Moore EE, Stanworth SJ, Lewis RJ, Steiner ME; Hemostasis Trials Outcomes Working Group: Recommended primary outcomes for clinical trials evaluating hemostatic blood products and agents in patients with bleeding: Proceedings of a National Heart Lung and Blood Institute and US Department of Defense Consensus Conference. J Trauma Acute Care Surg. 2021; 91:S19–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Levy JH, Faraoni D, Almond CS, Baumann-Kreuziger L, Bembea MM, Connors JM, Dalton HJ, Davies R, Dumont LJ, Griselli M, Karkouti K, Massicotte MP, Teruya J, Thiagarajan RR, Spinella PC, Steiner ME: Consensus statement: Hemostasis trial outcomes in cardiac surgery and mechanical support. Ann Thorac Surg. 2022; 113:1026–35 [DOI] [PubMed] [Google Scholar]
- 15.El-Menyar A, Mekkodathil A, Abdelrahman H, Latifi R, Galwankar S, Al-Thani H, Rizoli S: Review of existing scoring systems for massive blood transfusion in trauma patients: Where do we stand? Shock. 2019; 52:288–99 [DOI] [PubMed] [Google Scholar]
- 16.Yucel N, Lefering R, Maegele M, Vorweg M, Tjardes T, Ruchholtz S, Neugebauer EA, Wappler F, Bouillon B, Rixen D; Polytrauma Study Group of the German Trauma Society: Trauma Associated Severe Hemorrhage (TASH)-Score: Probability of mass transfusion as surrogate for life threatening hemorrhage after multiple trauma. J Trauma. 2006; 60:1228–36; discussion 1236–7 [DOI] [PubMed] [Google Scholar]
- 17.Petrou A, Tzimas P, Siminelakis S: Massive bleeding in cardiac surgery. Definitions, predictors and challenges. Hippokratia. 2016; 20:179–86 [PMC free article] [PubMed] [Google Scholar]
- 18.Vuylsteke A, Pagel C, Gerrard C, Reddy B, Nashef S, Aldam P, Utley M: The Papworth Bleeding Risk Score: A stratification scheme for identifying cardiac surgery patients at risk of excessive early postoperative bleeding. Eur J Cardiothorac Surg. 2011; 39:924–30 [DOI] [PubMed] [Google Scholar]
- 19.Klein AA, Collier T, Yeates J, Miles LF, Fletcher SN, Evans C, Richards T, Contributors: The ACTA PORT-score for predicting perioperative risk of blood transfusion for adult cardiac surgery. Br J Anaesth. 2017; 119:394–401 [DOI] [PubMed] [Google Scholar]
- 20.Gillissen A, van den Akker T, Caram-Deelder C, Henriquez D, Nij Bijvank SWA, Bloemenkamp KWM, Eikenboom J, van der Bom JG: Predictive value of a bleeding score for postpartum hemorrhage. Res Pract Thromb Haemost. 2019; 3:277–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Colalillo EL, Sparks AD, Phillips JM, Onyilofor CL, Ahmadzia HK: Obstetric hemorrhage risk assessment tool predicts composite maternal morbidity. Sci Rep. 2021; 11:14709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Urban P, Mehran R, Colleran R, Angiolillo DJ, Byrne RA, Capodanno D, Cuisset T, Cutlip D, Eerdmans P, Eikelboom J, Farb A, Gibson CM, Gregson J, Haude M, James SK, Kim HS, Kimura T, Konishi A, Laschinger J, Leon MB, Magee PFA, Mitsutake Y, Mylotte D, Pocock S, Price MJ, Rao SV, Spitzer E, Stockbridge N, Valgimigli M, Varenne O, Windhoevel U, Yeh RW, Krucoff MW, Morice MC: Defining high bleeding risk in patients undergoing percutaneous coronary intervention. Circulation. 2019; 140:240–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Karkouti K, Wijeysundera DN, Beattie WS, Callum JL, Cheng D, Dupuis JY, Kent B, Mazer D, Rubens FD, Sawchuk C, Yau TM; Reducing Bleeding in Cardiac Surgery (RBC) Research Group: Variability and predictability of large-volume red blood cell transfusion in cardiac surgery: A multicenter study. Transfusion. 2007; 47:2081–8 [DOI] [PubMed] [Google Scholar]
- 24.Pettersson GB, Martino D, Blackstone EH, Nowicki ER, Houghtaling PL, Sabik JF, 3rd, Lytle BW: Advising complex patients who require complex heart operations. J Thorac Cardiovasc Surg. 2013; 145:1159–1169.e3 [DOI] [PubMed] [Google Scholar]
- 25.Dzik WH: The James Blundell Award Lecture 2006: Transfusion and the treatment of haemorrhage: Past, present and future. Transfus Med. 2007; 17:367–74 [DOI] [PubMed] [Google Scholar]
- 26.Hoffman M, Monroe DM, 3rd, Roberts HR: Activated factor VII activates factors IX and X on the surface of activated platelets: Thoughts on the mechanism of action of high-dose activated factor VII. Blood Coagul Fibrinolysis. 1998; 9(suppl 1):S61–5 [PubMed] [Google Scholar]
- 27.Roberts HR, Monroe DM, White GC: The use of recombinant factor VIIa in the treatment of bleeding disorders. Blood. 2004; 104:3858–64 [DOI] [PubMed] [Google Scholar]
- 28.Frederick R, Pochet L, Charlier C, Masereel B: Modulators of the coagulation cascade: Focus and recent advances in inhibitors of tissue factor, factor VIIa and their complex. Curr Med Chem. 2005; 12:397–417 [DOI] [PubMed] [Google Scholar]
- 29.Vojacek JF: Should we replace the terms intrinsic and extrinsic coagulation pathways with tissue factor pathway? Clin Appl Thromb Hemost. 2017; 23:922–7 [DOI] [PubMed] [Google Scholar]
- 30.Moore HB, Gando S, Iba T, Kim PY, Yeh CH, Brohi K, Hunt BJ, Levy JH, Draxler DF, Stanworth S, Gorlinger K, Neal MD, Schreiber MA, Barrett CD, Medcalf RL, Moore EE, Mutch NJ, Thachil J, Urano T, Thomas S, Scarlatescu E, Walsh M; Subcommittees on Fibrinolysis Disseminated Intravascular Coagulation, and Perioperative and Critical Care Thrombosis and Hemostasis: Defining trauma-induced coagulopathy with respect to future implications for patient management: Communication from the SSC of the ISTH. J Thromb Haemost. 2020; 18:740–7 [DOI] [PubMed] [Google Scholar]
- 31.Moore EE, Moore HB, Kornblith LZ, Neal MD, Hoffman M, Mutch NJ, Schochl H, Hunt BJ, Sauaia A: Trauma-induced coagulopathy. Nat Rev Dis Primers. 2021; 7:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Meizoso JP, Dudaryk R, Mulder MB, Ray JJ, Karcutskie CA, Eidelson SA, Namias N, Schulman CI, Proctor KG: Increased risk of fibrinolysis shutdown among severely injured trauma patients receiving tranexamic acid. J Trauma Acute Care Surg. 2018; 84:426–32 [DOI] [PubMed] [Google Scholar]
- 33.Barry M, Trivedi A, Vivona LR, Chui J, Pathipati P, Miyazawa B, Pati S: Recovery of endotheliopathy at 24 hours in an established mouse model of hemorrhagic shock and trauma. Shock. 2022; 58:313–20 [DOI] [PubMed] [Google Scholar]
- 34.Jenkins DH, Rappold JF, Badloe JF, Berseus O, Blackbourne L, Brohi KH, Butler FK, Cap AP, Cohen MJ, Davenport R, DePasquale M, Doughty H, Glassberg E, Hervig T, Hooper TJ, Kozar R, Maegele M, Moore EE, Murdock A, Ness PM, Pati S, Rasmussen T, Sailliol A, Schreiber MA, Sunde GA, van de Watering LM, Ward KR, Weiskopf RB, White NJ, Strandenes G, Spinella PC: Trauma hemostasis and oxygenation research position paper on remote damage control resuscitation: Definitions, current practice, and knowledge gaps. Shock. 2014; 41(suppl 1):3–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hiippala ST, Myllyla GJ, Vahtera EM: Hemostatic factors and replacement of major blood loss with plasma-poor red cell concentrates. Anesth Analg. 1995; 81:360–5 [DOI] [PubMed] [Google Scholar]
- 36.Hayakawa M: Dynamics of fibrinogen in acute phases of trauma. J Intensive Care. 2017; 5:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Weisel JW, Litvinov RI: Red blood cells: The forgotten player in hemostasis and thrombosis. J Thromb Haemost. 2019; 17:271–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Boneu B, Fernandez F: The role of the hematocrit in bleeding. Transfus Med Rev. 1987; 1:182–5 [DOI] [PubMed] [Google Scholar]
- 39.Moore HB, Moore EE, Neal MD, Sheppard FR, Kornblith LZ, Draxler DF, Walsh M, Medcalf RL, Cohen MJ, Cotton BA, Thomas SG, Leeper CM, Gaines BA, Sauaia A: Fibrinolysis shutdown in trauma: Historical review and clinical implications. Anesth Analg. 2019; 129:762–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stanworth SJ, Dowling K, Curry N, Doughty H, Hunt BJ, Fraser L, Narayan S, Smith J, Sullivan I, Green L; Transfusion Task Force of the British Society for Haematology: Haematological management of major haemorrhage: A British Society for Haematology Guideline. Br J Haematol. 2022; 198:654–67 [DOI] [PubMed] [Google Scholar]
- 41.Despotis GJ, Santoro SA, Spitznagel E, Kater KM, Cox JL, Barnes P, Lappas DG: Prospective evaluation and clinical utility of on-site monitoring of coagulation in patients undergoing cardiac operation. J Thorac Cardiovasc Surg. 1994; 107:271–9 [PubMed] [Google Scholar]
- 42.Bartoszko J, Karkouti K: Managing the coagulopathy associated with cardiopulmonary bypass. J Thromb Haemost. 2021; 19:617–32 [DOI] [PubMed] [Google Scholar]
- 43.Cholette JM, Faraoni D, Goobie SM, Ferraris V, Hassan N: Patient blood management in pediatric cardiac surgery: A review. Anesth Analg. 2018; 127:1002–16 [DOI] [PubMed] [Google Scholar]
- 44.Hofer J, Fries D, Solomon C, Velik-Salchner C, Ausserer J: A snapshot of coagulopathy after cardiopulmonary bypass. Clin Appl Thromb Hemost. 2016; 22:505–11 [DOI] [PubMed] [Google Scholar]
- 45.Kozik DJ, Tweddell JS: Characterizing the inflammatory response to cardiopulmonary bypass in children. Ann Thorac Surg. 2006; 81:S2347–54 [DOI] [PubMed] [Google Scholar]
- 46.Wang J, Ma HP, Zheng H: Blood loss after cardiopulmonary bypass, standard vs titrated protamine: A meta-analysis. Neth J Med. 2013; 71:123–7 [PubMed] [Google Scholar]
- 47.Wan S, LeClerc JL, Vincent JL: Inflammatory response to cardiopulmonary bypass: Mechanisms involved and possible therapeutic strategies. Chest. 1997; 112:676–92 [DOI] [PubMed] [Google Scholar]
- 48.Gorlinger K, Dirkmann D, Hanke AA: Potential value of transfusion protocols in cardiac surgery. Curr Opin Anaesthesiol. 2013; 26:230–43 [DOI] [PubMed] [Google Scholar]
- 49.Steiner ME, Despotis GJ: Transfusion algorithms and how they apply to blood conservation: The high-risk cardiac surgical patient. Hematol Oncol Clin North Am. 2007; 21:177–84 [DOI] [PubMed] [Google Scholar]
- 50.Collins P, Abdul-Kadir R, Thachil J; Subcommittees on Women’s Health Issues in Thrombosis and Haemostasis and on Disseminated Intravascular Coagulation: Management of coagulopathy associated with postpartum hemorrhage: Guidance from the SSC of the ISTH. J Thromb Haemost. 2016; 14:205–10 [DOI] [PubMed] [Google Scholar]
- 51.Collis RE, Collins PW: Haemostatic management of obstetric haemorrhage. Anaesthesia. 2015; 70(suppl 1):78-86. [DOI] [PubMed] [Google Scholar]
- 52.Collis R, Guasch E: Managing major obstetric haemorrhage: Pharmacotherapy and transfusion. Best Pract Res Clin Anaesthesiol. 2017; 31:107–24 [DOI] [PubMed] [Google Scholar]
- 53.Allard S, Green L, Hunt BJ: How we manage the haematological aspects of major obstetric haemorrhage. Br J Haematol. 2014; 164:177–88 [DOI] [PubMed] [Google Scholar]
- 54.Committee on Practice Bulletins-Obstetrics: Practice bulletin No. 183: Postpartum hemorrhage. Obstet Gynecol. 2017; 130:e168–86 [DOI] [PubMed] [Google Scholar]
- 55.Levi M: Pathogenesis and management of peripartum coagulopathic calamities (disseminated intravascular coagulation and amniotic fluid embolism). Thromb Res. 2013; 131:S32–4 [DOI] [PubMed] [Google Scholar]
- 56.Xu C, Li Y, Zhang W, Wang Q: Analysis of perinatal coagulation function in preeclampsia. Medicine (Baltimore). 2021; 100:e26482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Brenner B: Haemostatic changes in pregnancy. Thromb Res. 2004; 114:409–14 [DOI] [PubMed] [Google Scholar]
- 58.Boender J, Kruip MJ, Leebeek FW: A diagnostic approach to mild bleeding disorders. J Thromb Haemost. 2016; 14:1507–16 [DOI] [PubMed] [Google Scholar]
- 59.Lippi G, Franchini M, Montagnana M, Favaloro EJ: Inherited disorders of blood coagulation. Ann Med. 2012; 44:405–18 [DOI] [PubMed] [Google Scholar]
- 60.Rodeghiero F, Pabinger I, Ragni M, Abdul-Kadir R, Berntorp E, Blanchette V, Bodo I, Casini A, Gresele P, Lassila R, Leebeek F, Lillicrap D, Mezzano D, Noris P, Srivastava A, Tosetto A, Windyga J, Zieger B, Makris M, Key N: Fundamentals for a systematic approach to mild and moderate inherited bleeding disorders: An EHA consensus report. Hemasphere. 2019; 3:e286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ng C, Motto DG, Di Paola J: Diagnostic approach to von Willebrand disease. Blood. 2015; 125:2029–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ambaglio C, Zane F, Russo MC, Preti PS, Scudeller L, Klersy C, Gamba G, Squizzato A: Preoperative bleeding risk assessment with ISTH-BAT and laboratory tests in patients undergoing elective surgery: A prospective cohort study. Haemophilia. 2021; 27:717–23 [DOI] [PubMed] [Google Scholar]
- 63.Vries MJ, van der Meijden PE, Kuiper GJ, Nelemans PJ, Wetzels RJ, van Oerle RG, Lance MD, Ten Cate H, Henskens YM: Preoperative screening for bleeding disorders: A comprehensive laboratory assessment of clinical practice. Res Pract Thromb Haemost. 2018; 2:767–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sivapalaratnam S, Collins J, Gomez K: Diagnosis of inherited bleeding disorders in the genomic era. Br J Haematol. 2017; 179:363–76 [DOI] [PubMed] [Google Scholar]
- 65.Burnett AE, Barnes GD: A call to action for anticoagulation stewardship. Res Pract Thromb Haemost. 2022; 6:e12757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Grymonprez M, Simoens C, Steurbaut S, De Backer TL, Lahousse L: Worldwide trends in oral anticoagulant use in patients with atrial fibrillation from 2010 to 2018: A systematic review and meta-analysis. Europace. 2022; 24:887–98 [DOI] [PubMed] [Google Scholar]
- 67.Kozek-Langenecker SA, Ahmed AB, Afshari A, Albaladejo P, Aldecoa C, Barauskas G, De Robertis E, Faraoni D, Filipescu DC, Fries D, Haas T, Jacob M, Lance MD, Pitarch JVL, Mallett S, Meier J, Molnar ZL, Rahe-Meyer N, Samama CM, Stensballe J, Van der Linden PJF, Wikkelso AJ, Wouters P, Wyffels P, Zacharowski K: Management of severe perioperative bleeding: Guidelines from the European Society of Anaesthesiology: First update 2016. Eur J Anaesthesiol. 2017; 34:332–95 [DOI] [PubMed] [Google Scholar]
- 68.Pagano D, Milojevic M, Meesters MI, Benedetto U, Bolliger D, von Heymann C, Jeppsson A, Koster A, Osnabrugge RL, Ranucci M, Ravn HB, Vonk ABA, Wahba A, Boer C: 2017 EACTS/EACTA guidelines on patient blood management for adult cardiac surgery. Eur J Cardiothorac Surg. 2018; 53:79–111 [DOI] [PubMed] [Google Scholar]
- 69.Tibi P, McClure RS, Huang J, Baker RA, Fitzgerald D, Mazer CD, Stone M, Chu D, Stammers AH, Dickinson T, Shore-Lesserson L, Ferraris V, Firestone S, Kissoon K, Moffatt-Bruce S: STS/SCA/AmSECT/SABM update to the clinical practice guidelines on patient blood management. Ann Thorac Surg. 2021; 112:981–1004 [DOI] [PubMed] [Google Scholar]
- 70.Doshi R, Vadher A, Mithawala P, Shah P: Oral antiplatelets in primary and secondary prevention of myocardial infarction: A review. Ir J Med Sci. 2019; 188:453–67 [DOI] [PubMed] [Google Scholar]
- 71.Erdoes G, Martinez Lopez De Arroyabe B, Bolliger D, Ahmed AB, Koster A, Agarwal S, Boer C, von Heymann C: International consensus statement on the peri-operative management of direct oral anticoagulants in cardiac surgery. Anaesthesia. 2018; 73:1535–45 [DOI] [PubMed] [Google Scholar]
- 72.Aliter KF, Al-Horani RA: Thrombin inhibition by argatroban: Potential therapeutic benefits in COVID-19. Cardiovasc Drugs Ther. 2021; 35:195–203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gladwell TD: Bivalirudin: A direct thrombin inhibitor. Clin Ther. 2002; 24:38–58 [DOI] [PubMed] [Google Scholar]
- 74.Nutescu EA, Burnett A, Fanikos J, Spinler S, Wittkowsky A: Pharmacology of anticoagulants used in the treatment of venous thromboembolism. J Thromb Thrombolysis. 2016; 41:15–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tan KT, Lip GY: Fondaparinux. Curr Pharm Des. 2005; 11:415–9 [DOI] [PubMed] [Google Scholar]
- 76.Kondo K, Umemura K: Clinical pharmacokinetics of tirofiban, a nonpeptide glycoprotein IIb/IIIa receptor antagonist: Comparison with the monoclonal antibody abciximab. Clin Pharmacokinet. 2002; 41:187–95 [DOI] [PubMed] [Google Scholar]
- 77.Tripathi R, Morales J, Lee V, Gibson CM, Mack MJ, Schneider DJ, Douketis J, Sellke FW, Ohman EM, Thourani VH, Storey RF, Deliargyris EN: Antithrombotic drug removal from whole blood using haemoadsorption with a porous polymer bead sorbent. Eur Heart J Cardiovasc Pharmacother. 2022; 8:847–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Koster A, Warkentin H, von Dossow V, Morshuis M: Use of the CytoSorb(R) filter for elimination of residual therapeutic argatroban concentrations during heparinized cardiopulmonary bypass for heart transplantation. Perfusion. 2022; 26:2676591221093875 [DOI] [PubMed] [Google Scholar]
- 79.Koster A, Chew D, Merkle F, Gruendel M, Jurmann M, Kuppe H, Oertel R: Extracorporeal elimination of large concentrations of tirofiban by zero-balanced ultrafiltration during cardiopulmonary bypass: An in vitro investigation. Anesth Analg. 2004; 99:989–92 [DOI] [PubMed] [Google Scholar]
- 80.Koster A, Buz S, Krabatsch T, Dehmel F, Kuppe H, Hetzer R, Aronson S, Dyke CM: Effect of modified ultrafiltration on bivalirudin elimination and postoperative blood loss after on-pump coronary artery bypass grafting: Assessment of different filtration strategies. J Card Surg. 2008; 23:655–8 [DOI] [PubMed] [Google Scholar]
- 81.Koster A, Chew D, Grundel M, Hausmann H, Grauhan O, Kuppe H, Spiess BD: An assessment of different filter systems for extracorporeal elimination of bivalirudin: An in vitro study. Anesth Analg. 2003; 96:1316–9 [DOI] [PubMed] [Google Scholar]
- 82.Cosmi B, Alatri A, Cattaneo M, Gresele P, Marietta M, Rodeghiero F, Tripodi A, Ansaloni L, Fusari M, Taddei S; Italian Society for Haemostasis and Thrombosis: Assessment of the risk of bleeding in patients undergoing surgery or invasive procedures: Guidelines of the Italian Society for Haemostasis and Thrombosis (SISET). Thromb Res. 2009; 124:e6–12 [DOI] [PubMed] [Google Scholar]
- 83.Chee YL, Crawford JC, Watson HG, Greaves M: Guidelines on the assessment of bleeding risk prior to surgery or invasive procedures. British Committee for Standards in Haematology. Br J Haematol. 2008; 140:496–504 [DOI] [PubMed] [Google Scholar]
- 84.Bonhomme F, Ajzenberg N, Schved JF, Molliex S, Samama CM; French Anaesthetic and Intensive Care Committee on Evaluation of Routine Preoperative Testing; French Society of Anaesthesia and Intensive Care: Pre-interventional haemostatic assessment: Guidelines from the French Society of Anaesthesia and Intensive Care. Eur J Anaesthesiol. 2013; 30:142–62 [DOI] [PubMed] [Google Scholar]
- 85.American Society of Anesthesiologists Task Force on Perioperative Blood Management: Practice guidelines for perioperative blood management: An updated report by the American Society of Anesthesiologists Task Force on Perioperative Blood Management*. Anesthesiology. 2015; 122:241–75 [DOI] [PubMed] [Google Scholar]
- 86.Finley A, Greenberg C: Review article: Heparin sensitivity and resistance: Management during cardiopulmonary bypass. Anesth Analg. 2013; 116:1210–22 [DOI] [PubMed] [Google Scholar]
- 87.Levy JH, Connors JM: Heparin resistance - Clinical perspectives and management strategies. N Engl J Med. 2021; 385:826–32 [DOI] [PubMed] [Google Scholar]
- 88.Cankovic L, Steenwyk BL, McGiffin DC, Nielsen VG: Practical approach to anticoagulation for cardiopulmonary bypass in the patient with congenital prolonged activated partial thromboplastin time. Blood Coagul Fibrinolysis. 2008; 19:725–6 [DOI] [PubMed] [Google Scholar]
- 89.Koster A, Zittermann A, Schirmer U: Heparin resistance and excessive thrombocytosis. Anesth Analg. 2013; 117:1262. [DOI] [PubMed] [Google Scholar]
- 90.Aradi D, Komocsi A, Price MJ, Cuisset T, Ari H, Hazarbasanov D, Trenk D, Sibbing D, Valgimigli M, Bonello L; Tailored Antiplatelet Treatment Study Collaboration: Efficacy and safety of intensified antiplatelet therapy on the basis of platelet reactivity testing in patients after percutaneous coronary intervention: Systematic review and meta-analysis. Int J Cardiol. 2013; 167:2140–8 [DOI] [PubMed] [Google Scholar]
- 91.Ibrahim F, Calmette L, Layka A, Horellou MH, Mazoyer E, Gouin-Thibault I, Flaujac C: PT, aPTT, TT and the hemostatic safety threshold of dabigatran and rivaroxaban. Ann Biol Clin (Paris). 2016; 74:457–64 [DOI] [PubMed] [Google Scholar]
- 92.Taylor G, Osinski D, Thevenin A, Devys JM: Is platelet transfusion efficient to restore platelet reactivity in patients who are responders to aspirin and/or clopidogrel before emergency surgery? J Trauma Acute Care Surg. 2013; 74:1367–9 [DOI] [PubMed] [Google Scholar]
- 93.Favaloro EJ, Pasalic L, Lippi G: Towards 50 years of platelet function analyser (PFA) testing. Clin Chem Lab Med. 2022. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 94.Guay J, Faraoni D, Bonhomme F, Borel Derlon A, Lasne D: Ability of hemostatic assessment to detect bleeding disorders and to predict abnormal surgical blood loss in children: A systematic review and meta-analysis. Paediatr Anaesth. 2015; 25:1216–26 [DOI] [PubMed] [Google Scholar]
- 95.Favaloro EJ: Utility of the platelet function analyser (PFA-100/200) for exclusion or detection of von Willebrand disease: A study 22 years in the making. Thromb Res. 2020; 188:17–24 [DOI] [PubMed] [Google Scholar]
- 96.Karger R, Donner-Banzhoff N, Muller HH, Kretschmer V, Hunink M: Diagnostic performance of the platelet function analyzer (PFA-100) for the detection of disorders of primary haemostasis in patients with a bleeding history-A systematic review and meta-analysis. Platelets. 2007; 18:249–60 [DOI] [PubMed] [Google Scholar]
- 97.Alvikas J, Zenati M, Campwala I, Jansen JO, Hassoune A, Phelos H, Okonkwo DO, Neal MD: Rapid detection of platelet inhibition and dysfunction in traumatic brain injury: A prospective observational study. J Trauma Acute Care Surg. 2022; 92:167–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bates SM, Weitz JI: Coagulation assays. Circulation. 2005; 112:e53–60 [DOI] [PubMed] [Google Scholar]
- 99.Visweshwar N, Jaglal M, Patel A, Laber D, Sokol L: Should we integrate viscoelastic assays with standard coagulation screening? J Clin Pathol. 2021; 74:141–3 [DOI] [PubMed] [Google Scholar]
- 100.Toulon P, Eloit Y, Smahi M, Sigaud C, Jambou D, Fischer F, Appert-Flory A: In vitro sensitivity of different activated partial thromboplastin time reagents to mild clotting factor deficiencies. Int J Lab Hematol. 2016; 38:389–96 [DOI] [PubMed] [Google Scholar]
- 101.Solomon C, Baryshnikova E, Tripodi A, Schlimp CJ, Schochl H, Cadamuro J, Winstedt D, Asmis L, Ranucci M: Fibrinogen measurement in cardiac surgery with cardiopulmonary bypass: Analysis of repeatability and agreement of Clauss method within and between six different laboratories. Thromb Haemost. 2014; 112:109–17 [DOI] [PubMed] [Google Scholar]
- 102.Erdoes G, Koster A, Levy JH: Viscoelastic coagulation testing: Use and current limitations in perioperative decision-making. Anesthesiology. 2021; 135:342–9 [DOI] [PubMed] [Google Scholar]
- 103.Meco M, Montisci A, Giustiniano E, Greco M, Pappalardo F, Mammana L, Panisi P, Roscitano C, Cirri S, Donatelli F, Albano G: Viscoelastic blood tests use in adult cardiac surgery: Meta-analysis, meta-regression, and trial sequential analysis. J Cardiothorac Vasc Anesth. 2020; 34:119–27 [DOI] [PubMed] [Google Scholar]
- 104.Dias JD, Sauaia A, Achneck HE, Hartmann J, Moore EE: Thromboelastography-guided therapy improves patient blood management and certain clinical outcomes in elective cardiac and liver surgery and emergency resuscitation: A systematic review and analysis. J Thromb Haemost. 2019; 17:984–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Spahn DR, Bouillon B, Cerny V, Duranteau J, Filipescu D, Hunt BJ, Komadina R, Maegele M, Nardi G, Riddez L, Samama CM, Vincent JL, Rossaint R: The European guideline on management of major bleeding and coagulopathy following trauma: Fifth edition. Crit Care. 2019; 23:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Bugaev N, Como JJ, Golani G, Freeman JJ, Sawhney JS, Vatsaas CJ, Yorkgitis BK, Kreiner LA, Garcia NM, Aziz HA, Pappas PA, Mahoney EJ, Brown ZW, Kasotakis G: Thromboelastography and rotational thromboelastometry in bleeding patients with coagulopathy: Practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2020; 89:999–1017 [DOI] [PubMed] [Google Scholar]
- 107.Amgalan A, Allen T, Othman M, Ahmadzia HK: Systematic review of viscoelastic testing (TEG/ROTEM) in obstetrics and recommendations from the Women’s SSC of the ISTH. J Thromb Haemost. 2020; 18:1813–38 [DOI] [PubMed] [Google Scholar]
- 108.Dias JD, Butwick AJ, Hartmann J, Waters JH: Viscoelastic haemostatic point-of-care assays in the management of postpartum haemorrhage: A narrative review. Anaesthesia. 2022; 77:700–11 [DOI] [PubMed] [Google Scholar]
- 109.Einersen PM, Moore EE, Chapman MP, Moore HB, Gonzalez E, Silliman CC, Banerjee A, Sauaia A: Rapid thrombelastography thresholds for goal-directed resuscitation of patients at risk for massive transfusion. J Trauma Acute Care Surg. 2017; 82:114–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Erdoes G, Koster A, Ortmann E, Meesters MI, Bolliger D, Baryshnikova E, Martinez Lopez De Arroyabe B, Ahmed A, Lance MD, Ranucci M, von Heymann C, Agarwal S, Ravn HB: A European consensus statement on the use of four-factor prothrombin complex concentrate for cardiac and non-cardiac surgical patients. Anaesthesia. 2021; 76:381–92 [DOI] [PubMed] [Google Scholar]
- 111.Baryshnikova E, Di Dedda U, Ranucci M: A comparative study of SEER sonorheometry versus standard coagulation tests, rotational thromboelastometry, and multiple electrode aggregometry in cardiac surgery. J Cardiothorac Vasc Anesth. 2019; 33:1590–8 [DOI] [PubMed] [Google Scholar]
- 112.Volod O, Bunch CM, Zackariya N, Moore EE, Moore HB, Kwaan HC, Neal MD, Al-Fadhl MD, Patel SS, Wiarda G, Al-Fadhl HD, McCoy ML, Thomas AV, Thomas SG, Gillespie L, Khan RZ, Zamlut M, Kamphues P, Fries D, Walsh MM: Viscoelastic hemostatic assays: A primer on legacy and new generation devices. J Clin Med. 2022; 11:860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Weber CF, Gorlinger K, Meininger D, Herrmann E, Bingold T, Moritz A, Cohn LH, Zacharowski K: Point-of-care testing: A prospective, randomized clinical trial of efficacy in coagulopathic cardiac surgery patients. Anesthesiology. 2012; 117:531–47 [DOI] [PubMed] [Google Scholar]
- 114.Karkouti K, Callum J, Wijeysundera DN, Rao V, Crowther M, Grocott HP, Pinto R, Scales DC, Investigators T: Point-of-care hemostatic testing in cardiac surgery: A stepped-wedge clustered randomized controlled trial. Circulation. 2016; 134:1152–62 [DOI] [PubMed] [Google Scholar]
- 115.Baksaas-Aasen K, Gall LS, Stensballe J, Juffermans NP, Curry N, Maegele M, Brooks A, Rourke C, Gillespie S, Murphy J, Maroni R, Vulliamy P, Henriksen HH, Pedersen KH, Kolstadbraaten KM, Wirtz MR, Kleinveld DJB, Schafer N, Chinna S, Davenport RA, Naess PA, Goslings JC, Eaglestone S, Stanworth S, Johansson PI, Gaarder C, Brohi K: Viscoelastic haemostatic assay augmented protocols for major trauma haemorrhage (ITACTIC): A randomized, controlled trial. Intensive Care Med. 2021; 47:49–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Murray EKI, Murphy MSQ, Smith GN, Graham CH, Othman M: Thromboelastographic analysis of haemostasis in preeclamptic and normotensive pregnant women. Blood Coagul Fibrinolysis. 2018; 29:567–72 [DOI] [PubMed] [Google Scholar]
- 117.Vlaar APJ, Dionne JC, de Bruin S, Wijnberge M, Raasveld SJ, van Baarle F, Antonelli M, Aubron C, Duranteau J, Juffermans NP, Meier J, Murphy GJ, Abbasciano R, Muller MCA, Lance M, Nielsen ND, Schochl H, Hunt BJ, Cecconi M, Oczkowski S: Transfusion strategies in bleeding critically ill adults: A clinical practice guideline from the European Society of Intensive Care Medicine. Intensive Care Med. 2021; 47:1368–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Martini WZ: Coagulopathy by hypothermia and acidosis: Mechanisms of thrombin generation and fibrinogen availability. J Trauma. 2009; 67:202–8. discussion 208-9 [DOI] [PubMed] [Google Scholar]
- 119.Balmer JC, Hieb N, Daley BJ, Many HR, Heidel E, Rowe S, McKnight CL: Continued relevance of initial temperature measurement in trauma patients. Am Surg. 2022; 88:424–8 [DOI] [PubMed] [Google Scholar]
- 120.DeBot M, Sauaia A, Schaid T, Moore EE: Trauma-induced hypocalcemia. Transfusion. 2022; 62(suppl 1):S274–80 [DOI] [PubMed] [Google Scholar]
- 121.Moore HB, Tessmer MT, Moore EE, Sperry JL, Cohen MJ, Chapman MP, Pusateri AE, Guyette FX, Brown JB, Neal MD, Zuckerbraun B, Sauaia A: Forgot calcium? Admission ionized-calcium in two civilian randomized controlled trials of prehospital plasma for traumatic hemorrhagic shock. J Trauma Acute Care Surg. 2020; 88:588–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Levy JH, Koster A, Quinones QJ, Milling TJ, Key NS: Antifibrinolytic therapy and perioperative considerations. Anesthesiology. 2018; 128:657–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Franchini M, Mannucci PM: The never ending success story of tranexamic acid in acquired bleeding. Haematologica. 2020; 105:1201–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Shakur H, Roberts I, Bautista R, Caballero J, Coats T, Dewan Y, El-Sayed H, Gogichaishvili T, Gupta S, Herrera J, Hunt B, Iribhogbe P, Izurieta M, Khamis H, Komolafe E, Marrero MA, Mejia-Mantilla J, Miranda J, Morales C, Olaomi O, Olldashi F, Perel P, Peto R, Ramana PV, Ravi RR, Yutthakasemsunt S: Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): A randomised, placebo-controlled trial. Lancet. 2010; 376:23–32 [DOI] [PubMed] [Google Scholar]
- 125.WOMAN Trial Collaborators: Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with post-partum haemorrhage (WOMAN): An international, randomised, double-blind, placebo-controlled trial. Lancet. 2017; 389:2105–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Binz S, McCollester J, Thomas S, Miller J, Pohlman T, Waxman D, Shariff F, Tracy R, Walsh M: CRASH-2 study of tranexamic acid to treat bleeding in trauma patients: A controversy fueled by science and social media. J Blood Transfus. 2015; 2015:874920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Myles PS, Smith JA, Forbes A, Silbert B, Jayarajah M, Painter T, Cooper DJ, Marasco S, McNeil J, Bussieres JS, McGuinness S, Byrne K, Chan MT, Landoni G, Wallace S; ATACAS Investigators of the ANZCA Clinical Trials Network: Tranexamic acid in patients undergoing coronary-artery surgery. N Engl J Med. 2017; 376:136–48 [DOI] [PubMed] [Google Scholar]
- 128.Lecker I, Wang DS, Whissell PD, Avramescu S, Mazer CD, Orser BA: Tranexamic acid-associated seizures: Causes and treatment. Ann Neurol. 2016; 79:18–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Shi J, Zhou C, Pan W, Sun H, Liu S, Feng W, Wang W, Cheng Z, Wang Y, Zheng Z, Group OS: Effect of high- vs low-dose tranexamic acid infusion on need for red blood cell transfusion and adverse events in patients undergoing cardiac surgery: The OPTIMAL randomized clinical trial. JAMA. 2022; 328:336–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Holcomb JB, Tilley BC, Baraniuk S, Fox EE, Wade CE, Podbielski JM, del Junco DJ, Brasel KJ, Bulger EM, Callcut RA, Cohen MJ, Cotton BA, Fabian TC, Inaba K, Kerby JD, Muskat P, O’Keeffe T, Rizoli S, Robinson BR, Scalea TM, Schreiber MA, Stein DM, Weinberg JA, Callum JL, Hess JR, Matijevic N, Miller CN, Pittet JF, Hoyt DB, Pearson GD, Leroux B, van Belle G, Group PS: Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: The PROPPR randomized clinical trial. JAMA. 2015; 313:471–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Godier A, Greinacher A, Faraoni D, Levy JH, Samama CM: Use of factor concentrates for the management of perioperative bleeding: Guidance from the SSC of the ISTH. J Thromb Haemost. 2018; 16:170–4 [DOI] [PubMed] [Google Scholar]
- 132.Chowdary P, Saayman AG, Paulus U, Findlay GP, Collins PW: Efficacy of standard dose and 30 ml/kg fresh frozen plasma in correcting laboratory parameters of haemostasis in critically ill patients. Br J Haematol. 2004; 125:69–73 [DOI] [PubMed] [Google Scholar]
- 133.Jhaveri P, Bozkurt S, Moyal A, Belov A, Anderson S, Shan H, Whitaker B, Hernandez-Boussard T: Analyzing real world data of blood transfusion adverse events: Opportunities and challenges. Transfusion. 2022; 62:1019–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Stanworth SJ, Brunskill SJ, Hyde CJ, McClelland DB, Murphy MF: Is fresh frozen plasma clinically effective? A systematic review of randomized controlled trials. Br J Haematol. 2004; 126:139–52 [DOI] [PubMed] [Google Scholar]
- 135.Huber J, Stanworth SJ, Doree C, Fortin PM, Trivella M, Brunskill SJ, Hopewell S, Wilkinson KL, Estcourt LJ: Prophylactic plasma transfusion for patients without inherited bleeding disorders or anticoagulant use undergoing non-cardiac surgery or invasive procedures. Cochrane Database Syst Rev. 2019; 11:CD012745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Naumann DN, Boulton AJ, Sandhu A, Campbell K, Charlton W, Gurney JM, Martin MJ, Scorer T, Doughty H: Fresh whole blood from walking blood banks for patients with traumatic hemorrhagic shock: A systematic review and meta-analysis. J Trauma Acute Care Surg. 2020; 89:792–800 [DOI] [PubMed] [Google Scholar]
- 137.Geneen LJ, Brunskill SJ, Doree C, Estcourt LJ, Green L: The difference in potential harms between whole blood and component blood transfusion in major bleeding: A rapid systematic review and meta-analysis of RCTs. Transfus Med Rev. 2022; 36:7–15 [DOI] [PubMed] [Google Scholar]
- 138.Baksaas-Aasen K, Van Dieren S, Balvers K, Juffermans NP, Naess PA, Rourke C, Eaglestone S, Ostrowski SR, Stensballe J, Stanworth S, Maegele M, Goslings JC, Johansson PI, Brohi K, Gaarder C; TACTIC/INTRN Collaborators: Data-driven development of ROTEM and TEG algorithms for the management of trauma hemorrhage: A prospective observational multicenter study. Ann Surg. 2019; 270:1178–85 [DOI] [PubMed] [Google Scholar]
- 139.Munoz M, Stensballe J, Ducloy-Bouthors AS, Bonnet MP, De Robertis E, Fornet I, Goffinet F, Hofer S, Holzgreve W, Manrique S, Nizard J, Christory F, Samama CM, Hardy JF: Patient blood management in obstetrics: prevention and treatment of postpartum haemorrhage. A NATA consensus statement. Blood Transfus. 2019; 17:112–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Raphael J, Mazer CD, Subramani S, Schroeder A, Abdalla M, Ferreira R, Roman PE, Patel N, Welsby I, Greilich PE, Harvey R, Ranucci M, Heller LB, Boer C, Wilkey A, Hill SE, Nuttall GA, Palvadi RR, Patel PA, Wilkey B, Gaitan B, Hill SS, Kwak J, Klick J, Bollen BA, Shore-Lesserson L, Abernathy J, Schwann N, Lau WT: Society of Cardiovascular Anesthesiologists clinical practice improvement advisory for management of perioperative bleeding and hemostasis in cardiac surgery patients. Anesth Analg. 2019; 129:1209–21 [DOI] [PubMed] [Google Scholar]
- 141.Erdoes G, Koster A, Meesters MI, Ortmann E, Bolliger D, Baryshnikova E, Ahmed A, Lance MD, Ravn HB, Ranucci M, von Heymann C, Agarwal S: The role of fibrinogen and fibrinogen concentrate in cardiac surgery: An international consensus statement from the Haemostasis and Transfusion Scientific Subcommittee of the European Association of Cardiothoracic Anaesthesiology. Anaesthesia. 2019; 74:1589–600 [DOI] [PubMed] [Google Scholar]
- 142.Curry NS, Davenport R, Pavord S, Mallett SV, Kitchen D, Klein AA, Maybury H, Collins PW, Laffan M: The use of viscoelastic haemostatic assays in the management of major bleeding: A British Society for Haematology guideline. Br J Haematol. 2018; 182:789–806 [DOI] [PubMed] [Google Scholar]
- 143.Cannon JW, Khan MA, Raja AS, Cohen MJ, Como JJ, Cotton BA, Dubose JJ, Fox EE, Inaba K, Rodriguez CJ, Holcomb JB, Duchesne JC: Damage control resuscitation in patients with severe traumatic hemorrhage: A practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2017; 82:605–17 [DOI] [PubMed] [Google Scholar]
- 144.Sentilhes L, Vayssiere C, Deneux-Tharaux C, Aya AG, Bayoumeu F, Bonnet MP, Djoudi R, Dolley P, Dreyfus M, Ducroux-Schouwey C, Dupont C, Francois A, Gallot D, Haumonte JB, Huissoud C, Kayem G, Keita H, Langer B, Mignon A, Morel O, Parant O, Pelage JP, Phan E, Rossignol M, Tessier V, Mercier FJ, Goffinet F: Postpartum hemorrhage: Guidelines for clinical practice from the French College of Gynaecologists and Obstetricians (CNGOF): In collaboration with the French Society of Anesthesiology and Intensive Care (SFAR). Eur J Obstet Gynecol Reprod Biol. 2016; 198:12–21 [DOI] [PubMed] [Google Scholar]
- 145.Rahe-Meyer N, Levy JH, Mazer CD, Schramko A, Klein AA, Brat R, Okita Y, Ueda Y, Schmidt DS, Ranganath R, Gill R: Randomized evaluation of fibrinogen vs placebo in complex cardiovascular surgery (REPLACE): A double-blind phase III study of haemostatic therapy. Br J Anaesth. 2016; 117:41–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Ranucci M, Baryshnikova E, Crapelli GB, Rahe-Meyer N, Menicanti L, Frigiola A; Surgical Clinical Outcome Research (SCORE) Group: Randomized, double-blinded, placebo-controlled trial of fibrinogen concentrate supplementation after complex cardiac surgery. J Am Heart Assoc. 2015; 4:e002066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Bilecen S, de Groot JA, Kalkman CJ, Spanjersberg AJ, Brandon Bravo Bruinsma GJ, Moons KG, Nierich AP: Effect of fibrinogen concentrate on intraoperative blood loss among patients with intraoperative bleeding during high-risk cardiac surgery: A randomized clinical trial. JAMA. 2017; 317:738–47 [DOI] [PubMed] [Google Scholar]
- 148.Callum J, Farkouh ME, Scales DC, Heddle NM, Crowther M, Rao V, Hucke HP, Carroll J, Grewal D, Brar S, Bussieres J, Grocott H, Harle C, Pavenski K, Rochon A, Saha T, Shepherd L, Syed S, Tran D, Wong D, Zeller M, Karkouti K, Group FR: Effect of fibrinogen concentrate vs cryoprecipitate on blood component transfusion after cardiac surgery: The FIBRES randomized clinical trial. JAMA. 2019; 322:1966–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Zaidi A, Kohli R, Daru J, Estcourt L, Khan KS, Thangaratinam S, Green L: Early use of fibrinogen replacement therapy in postpartum hemorrhage-A systematic review. Transfus Med Rev. 2020; 34:101–7 [DOI] [PubMed] [Google Scholar]
- 150.Ducloy-Bouthors AS, Mercier FJ, Grouin JM, Bayoumeu F, Corouge J, Le Gouez A, Rackelboom T, Broisin F, Vial F, Luzi A, Capronnier O, Huissoud C, Mignon A; FIDEL Working Group: Early and systematic administration of fibrinogen concentrate in postpartum haemorrhage following vaginal delivery: The FIDEL randomised controlled trial. BJOG. 2021; 128:1814–23 [DOI] [PubMed] [Google Scholar]
- 151.Innerhofer P, Fries D, Mittermayr M, Innerhofer N, von Langen D, Hell T, Gruber G, Schmid S, Friesenecker B, Lorenz IH, Strohle M, Rastner V, Trubsbach S, Raab H, Treml B, Wally D, Treichl B, Mayr A, Kranewitter C, Oswald E: Reversal of trauma-induced coagulopathy using first-line coagulation factor concentrates or fresh frozen plasma (RETIC): A single-centre, parallel-group, open-label, randomised trial. Lancet Haematol. 2017; 4:e258–71 [DOI] [PubMed] [Google Scholar]
- 152.Nascimento B, Callum J, Tien H, Peng H, Rizoli S, Karanicolas P, Alam A, Xiong W, Selby R, Garzon AM, Colavecchia C, Howald R, Nathens A, Beckett A: Fibrinogen in the initial resuscitation of severe trauma (FiiRST): A randomized feasibility trial. Br J Anaesth. 2016; 117:775–82 [DOI] [PubMed] [Google Scholar]
- 153.Neisser-Svae A, Hegener O, Gorlinger K: Differences in the biochemical composition of three plasma derived human fibrinogen concentrates. Thromb Res. 2021; 205:44–6 [DOI] [PubMed] [Google Scholar]
- 154.Grottke O, Levy JH: Prothrombin complex concentrates in trauma and perioperative bleeding. Anesthesiology. 2015; 122:923–31 [DOI] [PubMed] [Google Scholar]
- 155.Margraf DJ, Brown SJ, Blue HL, Bezdicek TL, Wolfson J, Chapman SA: Comparison of 3-factor versus 4-factor prothrombin complex concentrate for emergent warfarin reversal: A systematic review and meta-analysis. BMC Emerg Med. 2022; 22:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Hoffman M, Goldstein JN, Levy JH: The impact of prothrombin complex concentrates when treating DOAC-associated bleeding: A review. Int J Emerg Med. 2018; 11:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Karkouti K, Bartoszko J, Grewal D, Bingley C, Armali C, Carroll J, Hucke HP, Kron A, McCluskey SA, Rao V, Callum J: Comparison of 4-factor prothrombin complex concentrate with frozen plasma for management of hemorrhage during and after cardiac surgery: A randomized pilot trial. JAMA Netw Open. 2021; 4:e213936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Smith MM, Schroeder DR, Nelson JA, Mauermann WJ, Welsby IJ, Pochettino A, Montonye BL, Assawakawintip C, Nuttall GA: Prothrombin complex concentrate vs plasma for post-cardiopulmonary bypass coagulopathy and bleeding: A randomized clinical trial. JAMA Surg. 2022; 157:757–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Kao TW, Lee YC, Chang HT: Prothrombin complex concentrate for trauma induced coagulopathy: A systematic review and meta-analysis. J Acute Med. 2021; 11:81–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Greenberg SM, Ziai WC, Cordonnier C, Dowlatshahi D, Francis B, Goldstein JN, Hemphill JC, 3rd, Johnson R, Keigher KM, Mack WJ, Mocco J, Newton EJ, Ruff IM, Sansing LH, Schulman S, Selim MH, Sheth KN, Sprigg N, Sunnerhagen KS; American Heart Association/American Stroke Association: 2022 Guideline for the management of patients with spontaneous intracerebral hemorrhage: A guideline from the American Heart Association/American Stroke Association. Stroke. 2022; 53:e282–361 [DOI] [PubMed] [Google Scholar]
- 161.da Luz LT, Callum J, Beckett A, Hucke HP, Carroll J, Grewal D, Schwartz B, Peng H, Engels PT, Parry N, Petrosoniak A, Tien H, Nathens AB, Scales D, Karkouti K: Protocol for a multicentre, randomised, parallel-control, superiority trial comparing administration of clotting factor concentrates with a standard massive haemorrhage protocol in severely bleeding trauma patients: The FiiRST 2 trial (a 2020 EAST multicentre trial). BMJ Open. 2021; 11:e051003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Hedner U, Lee CA: First 20 years with recombinant FVIIa (NovoSeven). Haemophilia. 2011; 17:e172–82 [DOI] [PubMed] [Google Scholar]
- 163.Simpson E, Lin Y, Stanworth S, Birchall J, Doree C, Hyde C: Recombinant factor VIIa for the prevention and treatment of bleeding in patients without haemophilia. Cochrane Database Syst Rev. 2012; 3:CD005011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Gill R, Herbertson M, Vuylsteke A, Olsen PS, von Heymann C, Mythen M, Sellke F, Booth F, Schmidt TA: Safety and efficacy of recombinant activated factor VII: A randomized placebo-controlled trial in the setting of bleeding after cardiac surgery. Circulation. 2009; 120:21–7 [DOI] [PubMed] [Google Scholar]
- 165.Levi M, Levy JH, Andersen HF, Truloff D: Safety of recombinant activated factor VII in randomized clinical trials. N Engl J Med. 2010; 363:1791–800 [DOI] [PubMed] [Google Scholar]
- 166.Zatta A, McQuilten Z, Kandane-Rathnayake R, Isbister J, Dunkley S, McNeil J, Cameron P, Phillips L: The Australian and New Zealand Haemostasis Registry: Ten years of data on off-licence use of recombinant activated factor VII. Blood Transfus. 2015; 13:86–99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Sutherland L, Houchin A, Wang T, Wang S, Moitra V, Sharma A, Zorn T, 3rd, Flynn BC: Impact of early, low-dose factor VIIa on subsequent transfusions and length of stay in cardiac surgery. J Cardiothorac Vasc Anesth. 2022; 36:147–54 [DOI] [PubMed] [Google Scholar]
- 168.Karkouti K, von Heymann C, Jespersen CM, Korte W, Levy JH, Ranucci M, Sellke FW, Song HK: Efficacy and safety of recombinant factor XIII on reducing blood transfusions in cardiac surgery: A randomized, placebo-controlled, multicenter clinical trial. J Thorac Cardiovasc Surg. 2013; 146:927–39 [DOI] [PubMed] [Google Scholar]
- 169.Katzensteiner M, Ponschab M, Schochl H, Oberladstatter D, Zipperle J, Osuchowski M, Schlimp CJ: Factor XIII measurement and substitution in trauma patients after admission to an intensive care unit. J Clin Med. 2022; 11:4174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Roberts DJ, Bobrovitz N, Zygun DA, Kirkpatrick AW, Ball CG, Faris PD, Stelfox HT; Indications for Trauma Damage Control Surgery International Study Group: Evidence for use of damage control surgery and damage control interventions in civilian trauma patients: A systematic review. World J Emerg Surg. 2021; 16:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Stulak JM, Romans T, Cowger J, Romano MA, Haft JW, Aaronson KD, Pagani FD: Delayed sternal closure does not increase late infection risk in patients undergoing left ventricular assist device implantation. J Heart Lung Transplant. 2012; 31:1115–9 [DOI] [PubMed] [Google Scholar]
- 172.Lin CY, Wu MY, Tseng CN, Lee HF, Tsai FC: Delayed sternal closure for intractable bleeding after acute type A aortic dissection repair: Outcomes and risk factors analyses. J Cardiothorac Surg. 2022; 17:184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Smidfelt K, Nordanstig J, Wingren U, Bergstrom G, Langenskiold M: Routine open abdomen treatment compared with on-demand open abdomen or direct closure following open repair of ruptured abdominal aortic aneurysms: A propensity score-matched study. SAGE Open Med. 2019; 7:2050312119833501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Deffieux X, Vinchant M, Wigniolle I, Goffinet F, Sentilhes L: Maternal outcome after abdominal packing for uncontrolled postpartum hemorrhage despite peripartum hysterectomy. PLoS One. 2017; 12:e0177092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Serraino GF, Murphy GJ: Routine use of viscoelastic blood tests for diagnosis and treatment of coagulopathic bleeding in cardiac surgery: Updated systematic review and meta-analysis. Br J Anaesth. 2017; 118:823–33 [DOI] [PubMed] [Google Scholar]
- 176.Miskimins R, Pati S, Schreiber M: Barriers to clinical research in trauma. Transfusion. 2019; 59:846–53 [DOI] [PubMed] [Google Scholar]