Abstract
Background
Revision of well-fixed cementless femoral stems is a challenging and time-consuming aspect of revision hip arthroplasty. The Watson Extraction System (WES) is a novel, size-specific 3-D fabricated instrument that mimics the outer geometry of the implanted femoral stem. The device acts to cut circumferentially around the stem as it is impacted into place, effectively disrupting the bone-implant interface.
Methods
This is a retrospective review assessing the experience of 3 fellowship-trained adult reconstruction surgeons who used the WES to extract 10 well-fixed femoral stems during rTHA between 11/7/2020 and 11/7/2022. Outcomes and measures included: ability to remove the stem without a femoral osteotomy, femoral stem extraction time, incidence of femoral fracture, stem type used for reconstruction, blood loss, total surgical time, post-operative complications.
Results
No femoral osteotomies were required. The mean time for stem extraction was 7 min (range, 2–13), and there were 2 (20%) intra-operative femoral fractures. The stem type utilized for reconstruction included: 4 (40%) modular, tapered style stems, 3 (30%) antibiotic spacers, 2 (20%) primary style stems, and 1 (10%) ream and broach proximally porous stem. The mean blood loss was 425 ml (range, 200–800), total surgical time was 160 min (range, 107–232), and duration of follow-up was 7 months (range, 2–22 months).
Conclusion
The WES may mitigate the need for femoral osteotomy, reduce femoral stem extraction and overall intraoperative time, and decrease blood loss in rTHA. Further, reduced bone loss with use of this device may permit final reconstruction with a primary style stem.
Keywords: Revision total hip arthroplasty (rTHA), Extended trochanteric osteotomy (ETO), Femoral stem extraction, Operative time, Blood loss
1. Introduction
The number of primary and revision total hip arthroplasty (rTHA) cases continues to increase in the U.S1. A large nationwide study demonstrated a 36% increase in rTHAs from 36,898 in 2002 to 50,220 rTHA in 2014. The most common causes of revision were instability (18.3%), aseptic loosening (15.8%), and infection (11.6%)2,3. Implications on national healthcare costs and resources are substantial. Therefore, rTHA techniques and methods that improve efficiency while maintaining or improving patient outcomes is paramount. Extraction of a well-fixed femoral stem remains one of the most challenging aspects of rTHA and may result in significant femoral bone loss and even fracture if appropriate techniques are not employed. Further, known difficulty with removal of well-fixed femoral stems may bias the surgeon's operative strategy making the surgeon “socket-centric” when managing pathologies such as hip instability and periprosthetic joint infection (PPJI).
A variety of instruments and techniques to extract well-fixed femoral components have been reported and include the use of flexible osteotomes, high-speed burrs and k-wires4. Femoral osteotomies such the extended trochanteric osteotomy (ETO) is commonly employed to safely extract femoral stems when other “less invasive” methods have failed or are unrealistic4. While effective, an ETO requires a larger dissection, increases operative time and blood loss, and may still result in significant femoral bone loss. Although ETOs are generally met with reliable success the potential for trochanteric migration, iatrogenic fracture, malunion and non-union still exist5,6. A recent systematic review reported a 7% risk of non-union and a total perioperative complication rate of 8.1% for aseptic patients undergoing revision THA with ETO5.
The Watson Extraction System (WES) is a novel, three dimensional osteotome that mimics the outer geometry of the implanted femoral stem. The device acts to circumferentially cut around the stem as it is impacted into place, effectively disrupting the bone-implant interface. We are aware of only a single publication reporting the use of this device for rTHA in a small case series of 4 patients6. We intend to retrospectively evaluate the effectiveness and efficiency of the WES in extracting well fixed femoral stems during rTHA. We hypothesize that use of the WES will be more effective and efficient than historical controls and will negate the need for an osteotomy in most cases. Further, we expect its use will be associated with decreased operative times and blood loss compared to historical controls.
2. Material and methods
IRB approval was obtained prior to initiation of this study. Between November 2020 and November 2022, three fellowship-trained adult reconstruction surgeons at a single institution utilized the WES for stem extraction during rTHA for 10 consecutive cases. A retrospective chart review of each patient was performed to collect demographic and clinical data including any post-operative complications. Institutional hospital records were reviewed for intraoperative data including blood loss, intra-operative complications, operative time (Defined: incision to skin closure) and stem extraction time which was measured by the device representative (Defined: time of sizing for the first WES broach to removal of the stem). Additionally implant selection for femoral reconstruction was reviewed.
Of the ten cases performed, there were 8 men and 2 women with a mean age at time of surgery of 64 years (range, 46–73). Diagnosis for rTHA were the following: wear and osteolysis in two (20%), femoral loosening in one (10%), acetabular loosening in two (10%), and chronic PPJI in six (60%). Regarding the femoral stem removal in the setting of acetabular loosening, the patient presented with significant pain refractory to multimodal pain management for over six months without signs of implant loosening on imaging. However, the patient and the surgeon opted to pursue treatment with total revision of both components. Regarding the patient with femoral loosening, the patient had significant prolonged pain for over one year after initial THA and imaging suggestive of possible femoral loosening. A posterolateral approach was used in all cases. For PPJI cases, a single stage revision was performed in 3 cases and a two-stage revision in 3 cases. Staged revisions underwent implant resection, debridement, and implantation of a low friction antibiotic spacer.
The primary objective of this study is to evaluate the effectiveness of the WES to extract a well-fixed femoral stem safely and efficiently during rTHA. Primary outcomes included the ability to remove the stem without a femoral osteotomy, femoral stem extraction time and the incidence of intra-operative femoral fracture. Secondary outcome measures included blood loss, total surgical time, intra-operative and post-operative complications, and the stem type used for reconstruction. Additionally, post-operative radiographic analysis for implant position and fixation was performed.
2.1. Surgical technique
The following technique is a brief description of the WES and can be supplemented with a description published by Sagers et al.6. Importantly, the WES manufacturer can provide a variety of blade shapes and sizes; however, not all stem types have corresponding extraction blades. The device representative should be contacted and informed of the stem type and size in advance of the case. If this is unknown, the set does include sizing guides for intraoperative assessment.
The senior author's preference for rTHA is a posterolateral approach. The hip is dissected, and circumferential synovectomy performed. The hip is dislocated, and femoral head removed. The proximal femur is delivered into the center of the surgical site and the area surrounding the stem is debrided of remaining fibrous tissue and debris. To avoid levering and possible fracture, it is important to resect any prominent bone from the mesial aspect of the greater trochanter around the stem. Further, good visualization of the shoulder of the stem facilitates insertion the lateral blade down the contour of the stem (Fig. 1). Femoral stem ingrowth is confirmed by direct visualization of the bone-implant interface and high-speed burr may be utilized to further expose the interface. A physical template device is used intraoperatively to determine the size of the implanted femoral stem and identify which size and shape WES blade is needed. The lateral osteotome is carefully impacted into place over the lateral shoulder of the implant while gently directing the tip of the device towards the stem's lateral side (Fig. 1). Mallet impactions should be relatively gentle to permit the device to follow the bone-implant interface and not perforate the lateral cortex. Once the osteotome has been completely impacted into place, it is removed, and the medial osteotome is inserted at the calcar bone-implant interface. As this osteotome is carefully impacted into place, the tip is again guided toward the femoral stem using the blade handle to avoid calcar perforation and fracture. As the medial blade is impacted into place, the stem trunnion passes through a cutout in the blade to allow advancement to the tip of the stem distally (Fig. 2). After the medial blade is completely inserted, it is removed. The lateral and medial blades are impacted into place repeatedly until the stem is completely disengaged and easily removed by a stem extraction device. All blades mimic the outer geometry of the femoral stem and therefore will disrupt the bone-implant interface circumferentially and nearly completely (Fig. 3).
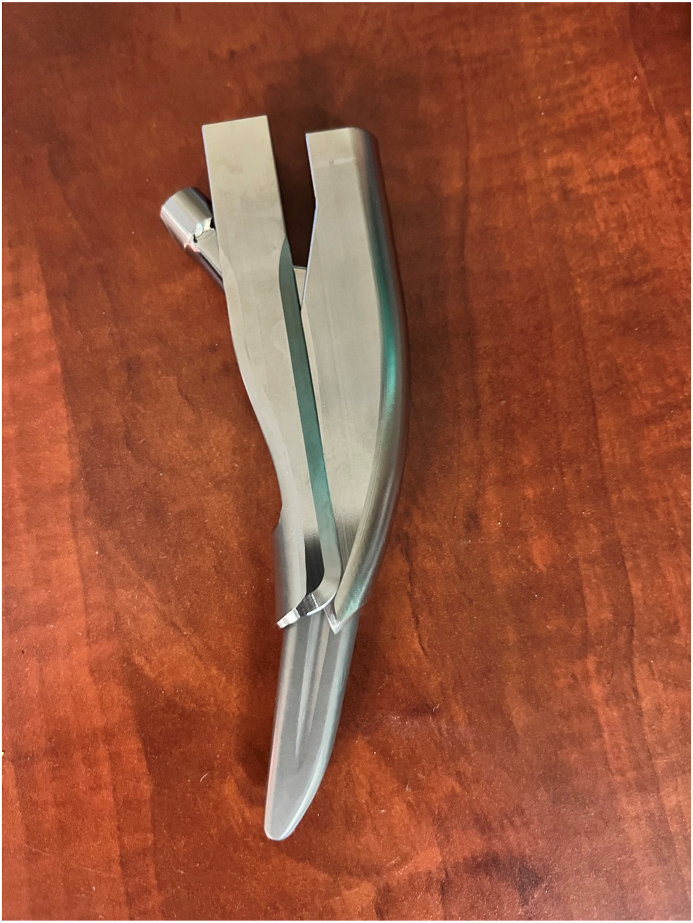
Fig. 1.
Legend: This is the lateral blade overlying a femoral stem, showing the path along the lateral portion of the femoral stem implant. Boney prominence should be resected from the medial trochanter to avoid levering and trochanter fracture. One should manually guide the tip of the osteotome toward the stem to avoid lateral cortical perforation.
Fig. 2.
Legend: This is the medial blade overlying a femoral stem, showing the path along the medial portion of the femoral stem implant. The tip of the blade should be gently directed toward the bone-implant interface.
Fig. 3.
Legend: This is a femoral stem implant with WES blades showing the full coverage of the outer edges around the entire stem.
3. Results
Our series included 10 cases with a mean follow-up was 7 months (range, 2–22 months). There was no need for a femoral osteotomy in any of the rTHA cases reviewed. The mean time for femoral stem extraction was 7 min (range, 2–13), and the mean total surgical time was 160 min (range, 107–232). The mean blood loss during surgery was 425 ml (range, 200–800). Mean operative time for single and two stage revision for PPJI was 194 min (range, 143–232) and 149 min (range, 115–172), respectively.
There were two (20%) intra-operative complications including one non-displaced calcar fracture and one non-displaced greater trochanter fracture. In the first case involving a 63 year-old man, a non-displaced fracture of the calcar was noted intra-operatively during revision in the setting of a long-standing PPJI. The fracture was treated with a single cable and healed uneventfully with no untoward post-operative sequelae. The operative time and blood loss in this case was 194 min and 800 ml, respectively. The second case involved a 46 year-old man during rTHA for PPJI in which an intra-operative non-displaced greater trochanter fracture went unnoticed until observed on immediate post-operative radiographs in the recovery unit. This was treated with abduction restrictions for 3 months and healed successfully without post-operative sequelae or re-operation at final follow-up. Surgical time and blood loss in this case was 232 min and 500 ml of blood loss. There was one (10%) post-operative complication in a 73 year-old man who underwent rTHA to a low friction spacer for chronic PPJI. Approximately 6 months later, he underwent a successful reimplantation with primary THA components but suffered two dislocations less than 6 months after reimplantation. Both dislocations were treated with closed reduction, and he has not dislocated again or required re-operation (Fig. 4a–c).
Fig. 4.
Legend: a) Right Hip AP view of the pre-operative THA implant, b) R Hip AP view of the post-operative low friction antibiotic spacer, c) R Hip AP view of the re-implanted rTHA implant.
There were no cases of radiographic loosening or stem migration at final follow-up and no post-operative infections or re-infections to date. The types of femoral stems removed, and final femoral implants used can be found in Table 1.
Table 1.
Demographics and results of all cases.
| Sex | Age | Reason for Revision | Approach | Blood Loss (mL) | Total Surgical Time (min) | Femoral Stem Extraction Time (min) | Intra-op Complications | Type of Stem Removed | Final Implant used | Immediate Post-op Complications |
|---|---|---|---|---|---|---|---|---|---|---|
| M | 63 | Chronic PPJI | Posterior | 400 | 143 | 10 | None | Dual Taper | Tri-taper | None |
| M | 73 | Chronic PPJI | Posterior | 400 | 207 | 5 | None | Short, chili pepper stem | Tri-taper | 2 closed dislocations |
| M | 64 | Acetabular Loosening | Posterior | 400 | 140 | 6 | none | Dual Taper | Modular, tapered | None |
| M | 60 | Femoral Loosening | Posterior | 400 | 107 | 13 | none | Dual Taper | Ream and broach, tapered stem | none |
| M | 69 | Chronic PPJI | Posterior | 200 | 160 | 3 | none | Dual Taper | Low friction spacer/cemented stem | none |
| M | 63 | Catastrophic failure of ceramic on ceramic with Wear and Osteolysis | Posterior | 800 | 194 | 8 | Non-displaced calcar fracture | Metaphyseal fitting, tapered stem | Modular, tapered | None |
| F | 67 | Wear and Osteolysis | Posterior | 300 | 130 | 2 | none | Dual Taper | Modular, tapered | none |
| F | 73 | Chronic PPJI | Posterior | 350 | 115 | 6 | none | Dual Taper | Low friction spacer/cemented stem | none |
| M | 46 | Chronic PPJI | Posterior | 500 | 232 | 5 | non-displaced greater trochanter fracture | Dual Taper | Modular, tapered | none |
| M | 58 | Chronic PPJI | Posterior | 500 | 172 | 10 | none | Dual Taper | Low friction spacer/cemented stem | none |
Notes: PPJI, Periprosthetic Joint Infection.
4. Discussion
Revision THA is associated with increased operative times and perioperative blood loss especially when extraction of a well-fixed femoral stem is required. Further, longer surgical times are a harbinger for increased length of hospital stay, increased rates of blood transfusions, prolonged recovery and periprosthetic infection. We anticipated that by reducing the time for stem extraction and mitigating the need for a femoral osteotomy, total operative time, blood loss and complications would be decreased. In our study of the WES, there were no cases in which femoral osteotomy was required to remove a well-fixed femoral stem. This resulted in a mean operative time of 160 min (range, 107–232) which compares favorably to reported rTHA operative times in current literature which ranges from 60 min to 661 minutes7, 8, 9, 10, 11, 12. Additionally, we observed less blood loss compared to historical controls. Mean intra-operative blood loss in our series was 425 ml (range, 200–800) which compares favorably to other reports ranging from 500 ml to 2000 ml7, 8, 9,13, 14, 15.
Notably, operative times during rTHA will vary depending on the diagnosis for revision. The mean operative time for all PPJI cases in our series was 172 min (range, 115–232). This was longer than the mean operative time of 143 min (range, 107–194) for aseptic cases. It is accepted that PPJI cases necessitate longer surgical times due to the need for thorough surgical debridement, irrigation and at times re-draping. Mean operative times for chronic PPJI have been reported to be between 129 and 247 min, depending on numerous factors such as one-stage vs two-stage, types of implants used, bone loss, among others15, 16, 17. Nonetheless, the average time for septic revisions in our series appears to be favorable to the current literature.
The reduced operative time in our series can be directly attributed to shorter femoral stem extraction times without the need of a femoral osteotomy. However, the duration of time to extract a well-fixed femoral stem is not routinely reported in the literature making a direct comparison of the WES to an ETO or other extraction techniques difficult. If total operative times are used as a surrogate for stem extraction times, this device appears to have an advantage over comparable techniques. Our average time for stem extraction using the WES was 7 min (range, 2 to 13). In a review article regarding the removal of well-fixed femoral stems, Laffosse et al. reports that attempts at femoral stem extraction should be reasonably kept under 30–45 minutes4. A recent study of 612 consecutive ETOs performed during rTHAs at a single academic institution showed a mean operative time of 221 ± 81 min (range, 71–661 min)10. Another study comprising 43 ETOs with additional horizontal and vertical cabling showed a mean operative time of 165 min (range, 120–270)11. Recently, Whittaker et al. compared 76 cases of rTHA with ETOs in the setting of PPJI against ETOs without PPJI, and the mean operative times were 222 min (range, 116–329) and 245 min (range, 126–358) respectively12.
In our series, the use of the WES resulted in less bone loss and frequently Paprosky Type 1 femoral deficiencies with preserved metaphyseal bone18. This enabled us to implant primary style stems (two tri-taper stems and one proximally porous tapered stem) in 30% of cases. Further when we include PPJIs, a primary or cemented stem (for low friction spacer) was used in 50% of cases. While we don't recommend using a primary stem for anything greater than a Paprosky type I deficiency, we do believe this observation has significant relevance and warrants further investigation.
Our experience of improved ease of stem removal, reduced operative times and diminished bone loss has resulted in an unanticipated benefit of the WES. Our center is now more likely to consider stem removal during pre-op planning, especially in scenarios of infection and instability. In short, we are less “socket-centric” in our planning. For instance, stem removal can be considered in a case of THA posterior instability with a mildly malpositioned socket and a stem in neutral position. Historically we may have planned for isolated socket revision to a more anteverted position. However, given our experience with the WES, we are now more likely to revise the femoral stem as well as the socket to optimize combined anteversion.
While there was a 30% combined intra- and post-operative complication rate in this series, only two were related to use of the WES. Both were non-displaced fractures of the proximal femur. One greater trochanter fracture treated conservatively, and one calcar fracture treated with a single cable. Neither patient suffered any long-term ramifications from the fracture. The one case of post-operative instability is not directly associated with use of the WES and further, post-operative work-up revealed abnormal spinal-pelvic mobility as the likely cause of his instability. In comparison, a meta-analysis with 1478 aseptic rTHAs requiring ETOs noted a perioperative complication rate of 8% (30/372; all intraoperative fractures) and postoperative complication rate was 5.7% (84/1478)5. The osteotomy nonunion rate was 7% and infection rate was 0.8% (12/1478). While we do recognize that our cohort of 10 patients is not powered for a direct comparison, we believe that further study of the WES is warranted.
We recognize that there are several inherent limitations to our study. First, we are reporting a retrospective review of a relatively small number of cases which is not equipped to definitively compare results of the WES to other interventions. However, given the novelty of this system and the potential future benefit for patients and surgeons during rTHA, we felt that our experience would contribute to future use of comparable devices. Second, the three surgeons in this study had different levels of experience using the WES which may have affected the results of this study. Third, most studies evaluating stem extraction techniques do not report the time for extraction alone making a direct comparison of the WES to other methods difficult. For best comparison, we chose to compare our mean total surgical times to historical controls with the assumption that our reduced operative times are related to the use of the WES. We cannot however confirm that other variables don't exist which may have resulted in shorter operative times in our series. Lastly, blood loss was assessed entirely intra-operatively and determined by the surgeon and anesthesia at the end of the case. Pre- and post-operative hemoglobin levels were not evaluated which limits the conclusions we can draw from blood loss and its clinical manifestation in our series.
5. Conclusion
Our study of the Watson Extraction System for stem extraction in 10 rTHAs is currently the largest series to date for such a device. We understand that use of any novel technology warrants careful investigation to evaluate its safety and efficacy before the arthroplasty community engages in widespread adoption. Our pilot experience is generally positive with observations of reduced stem extraction, intraoperative times, and decrease blood loss. Further, decreased bone loss permitted reconstruction with primary, bone preserving stems in some cases in our series. Further investigation is necessary to determine if our observations can be reliably reproduced.
Institutional ethical committee approval
This study was approved by the Institutional Review Board.
Funding/sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
Kevin Salomon: Investigation, Data curation, Formal Analysis, Writing - Original Draft. Victor Shen: Data curation, Writing – Original Draft. Alex Sullivan: Formal Analysis, Writing – Review & Editing. Christopher Grayson: Investigation, Writing - Review & Editing. Steven Lyons: Investigation, Writing - Review & Editing. Brian Palumbo: Conceptualization, Formal Analysis, Writing – Review & Editing, and Supervision.
Declaration of competing interests
Kevin Salomon, Victor Shen, Alex Sullivan, Christopher Grayson, Steven Lyons, and Brian Palumbo declare that they have no competing interests.
Informed consent
N/A.
Acknowledgments
N/A.
References
- 1.Kurtz S., et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 2.Bozic K.J., et al. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91(1):128–133. doi: 10.2106/JBJS.H.00155. [DOI] [PubMed] [Google Scholar]
- 3.Schwartz A.M., et al. Projections and epidemiology of revision hip and knee arthroplasty in the United States to 2030. J Arthroplasty. 2020;35(6s):S79–s85. doi: 10.1016/j.arth.2020.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Laffosse J.M. Removal of well-fixed fixed femoral stems. Orthop Traumatol Surg Res. 2016;102(1 Suppl):S177–S187. doi: 10.1016/j.otsr.2015.06.029. [DOI] [PubMed] [Google Scholar]
- 5.Malahias M.A., et al. Outcomes and risk factors of extended trochanteric osteotomy in aseptic revision total hip arthroplasty: a systematic review. J Arthroplasty. 2020;35(11):3410–3416. doi: 10.1016/j.arth.2020.07.034. [DOI] [PubMed] [Google Scholar]
- 6.Sagers K.M., et al. Removing well-fixed, collared and noncollared tapered hip stems without an extended trochanteric osteotomy using a novel stem removal system. Arthroplast Today. 2021;11:146–150. doi: 10.1016/j.artd.2021.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Manara J., et al. Prolonged operative time increases risk of blood loss and transfusion requirements in revision hip surgery. Eur J Orthop Surg Traumatol. 2020;30(7):1181–1186. doi: 10.1007/s00590-020-02677-4. [DOI] [PubMed] [Google Scholar]
- 8.Sershon R.A., et al. The optimal dosing regimen for tranexamic acid in revision total hip arthroplasty: a multicenter randomized clinical trial. J Bone Joint Surg Am. 2020;102(21):1883–1890. doi: 10.2106/JBJS.20.00010. [DOI] [PubMed] [Google Scholar]
- 9.Saito K., et al. Intraoperative hemorrhage in revision total hip arthroplasty: a retrospective single-center study. J Anesth. 2019;33(3):399–407. doi: 10.1007/s00540-019-02644-2. [DOI] [PubMed] [Google Scholar]
- 10.Abdel M.P., et al. Extended trochanteric osteotomy in revision total hip arthroplasty: contemporary outcomes of 612 hips. J Bone Joint Surg Am. 2021;103(2):162–173. doi: 10.2106/JBJS.20.00215. [DOI] [PubMed] [Google Scholar]
- 11.Huffman G.R., Ries M.D. Combined vertical and horizontal cable fixation of an extended trochanteric osteotomy site. J Bone Joint Surg Am. 2003;85(2):273–277. doi: 10.2106/00004623-200302000-00014. [DOI] [PubMed] [Google Scholar]
- 12.Whittaker M.J., et al. The impact of extended trochanteric osteotomy with cerclage fixation in revision total hip arthroplasty for prosthetic joint infection. J Arthroplasty. 2022 doi: 10.1016/j.arth.2022.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Peck J., et al. The effect of preoperative administration of intravenous tranexamic acid during revision hip arthroplasty: a retrospective study. J Bone Joint Surg Am. 2018;100(17):1509–1516. doi: 10.2106/JBJS.17.01212. [DOI] [PubMed] [Google Scholar]
- 14.Wang Q., et al. Intravenous tranexamic acid for reducing perioperative blood loss during revision hip arthroplasty: a retrospective study. Acta Orthop Traumatol Turcica. 2020;54(5):519–523. doi: 10.5152/j.aott.2020.19044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shi X., et al. The use of extended trochanteric osteotomy in 2-stage reconstruction of the hip for infection. J Arthroplasty. 2019;34(7):1470–1475. doi: 10.1016/j.arth.2019.02.054. [DOI] [PubMed] [Google Scholar]
- 16.Jämsen E., et al. Spacer prostheses in two-stage revision of infected knee arthroplasty. Int Orthop. 2006;30(4):257–261. doi: 10.1007/s00264-006-0102-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hsieh P.H., et al. Two-stage revision hip arthroplasty for infection: comparison between the interim use of antibiotic-loaded cement beads and a spacer prosthesis. J Bone Joint Surg Am. 2004;86(9):1989–1997. [PubMed] [Google Scholar]
- 18.Valle C.J., Paprosky W.G. Classification and an algorithmic approach to the reconstruction of femoral deficiency in revision total hip arthroplasty. J Bone Joint Surg Am. 2003;(Suppl 4):1–6. doi: 10.2106/00004623-200300004-00001. 85-A. [DOI] [PubMed] [Google Scholar]