Abstract
Due to its advantages over open surgery and conventional laparoscopy, uptake of robot-assisted surgery has rapidly increased. It is important to know whether the existing open or laparoscopic skills of robotic novices shorten the robotic surgery learning curve, potentially reducing the amount of training required. This systematic review aims to assess psychomotor skill transfer to the robot in clinical and simulated settings. PubMed, EMBASE, Cochrane Library and Scopus databases were systematically searched in accordance with PRISMA guidelines from inception to August 2021 alongside website searching and citation chaining. Article screening, data extraction and quality assessment were undertaken by two independent reviewers. Outcomes included simulator performance metrics or in the case of clinical studies, peri- and post-operative metrics. Twenty-nine studies met the eligibility criteria. All studies were judged to be at high or moderate overall risk of bias. Results were narratively synthesised due to heterogeneity in study designs and outcome measures. Two of the three studies assessing open surgical skill transfer found evidence of successful skill transfer while nine of twenty-seven studies evaluating laparoscopic skill transfer found no evidence. Skill transfer from both modalities is most apparent when advanced robotic tasks are performed in the initial phase of the learning curve but quality and methodological limitations of the existing literature prevent definitive conclusions. The impact of incorporating laparoscopic simulation into robotic training curricula and on the cost effectiveness of training should be investigated.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11701-022-01492-9.
Keywords: Open surgery, Laparoscopic, Robotics, Simulation, Skill transfer
Introduction
Robotic surgery has experienced a rapid increase in uptake, with a four-fold increase in the number of robot-assisted operations performed over the last decade [1]. The continuing favourability of robot-assisted surgery (RAS) is due to the numerous advantages it possesses over open surgery and conventional laparoscopy such as faster learning curves, eradication of the fulcrum effect and the ability to mirror the movements of the wrist and hand [2]. Furthermore, when compared to open procedures, RAS operations have resulted in more favourable patient-centred outcomes such as significantly decreased blood loss, length of hospital stay, transfusion rates [3] and lower post-operative pain medication use [4].
Therefore, as experienced surgeons switch to robot-assisted operations to capitalise on its advantages, it is now a priority to address the training needs of current and future surgeons. It is clinically important to know how far existing skills transfer for safe robot-assisted operations on patients, and whether prior open or laparoscopic experience complicates or complements the robotic skill acquisition process. There are also implications for surgical trainees undergoing robotic training, based solely on the acquisition of robot-specific technical skills. Simulation forms the initial stage of robotic skills training due to its convenience, efficiency and provision of safe training posing no risk to patients [5]. Robotic simulators are more expensive [6] and less available than laparoscopic simulators [7, 8], so establishing whether skills learnt on laparoscopic simulators transfer to the extent that less time is needed on robotic simulators may optimise the use of such limited resources.
It might be expected that open surgical experience translates into enhanced robot-assisted performances as knowledge of the anatomy and approaches associated with operating in a particular region may aid in mastering the robotic form of the operation. Similarly, given that laparoscopic surgeons are well versed in fundamental minimally invasive techniques and accustomed to manoeuvring instruments through an indirect field of view, they might be well equipped with transferable skills to augment their robotic skills. This review aims to assess the transfer of open and laparoscopic psychomotor skills (gained through surgical simulation or operative experience) to the robot, evaluating their impact on the robotic learning curve. Successful crossover of skills across the various modalities would not only result in surgeons being able to operate across a range of settings but may optimise their training in terms of duration and cost effectiveness.
Methods
Design
A systematic review assessing the transfer of open and laparoscopic skills to robotic surgery was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [9]. A review protocol was prospectively designed and registered on the International Prospective Register of Systematic Reviews (PROSPERO) database (CRD42021231235) [10].
Eligibility criteria
Studies involving medical students, surgical trainees and consultant surgeons (expert surgeons) were included, with exclusion of any study involving non-medical participants. Eligible interventions included assessed performances of robotic tasks or procedures after undergoing laparoscopic training or having prior laparoscopic or open surgical experience. Comparators included control participants (no open or laparoscopic experience) or robotically trained participants. Outcomes included measures of task performance in operative or simulated settings, with studies not assessing the impact of skill transfer in statistical terms being excluded. Randomised controlled trials, non-randomised comparative studies, cohort studies and observational studies evaluating skill transfer were included. Review articles, editorials, letters to the editor and conference abstracts were excluded. A restriction on language was imposed, with only studies written in English being included.
Search strategy
The PubMed, EMBASE, Cochrane Library and Scopus databases were systematically searched from their inception to August 2021. A combination of free-text terms and medical subject headings (MeSH) was used in the searches. For PubMed and the Cochrane Library, the search strategy ‘(laparoscop* OR open OR Laparoscopy[mesh] OR Minimally Invasive Surgical Procedures[mesh]) AND (robot* OR Robotic Surgical Procedures[mesh]) AND (transfer*)’ was used. For Embase, ‘((laparoscop* OR open) AND robot* AND transfer*)’ was used, while ‘((laparoscop* OR open) AND surg* AND robot* AND transfer*)’ was employed for Scopus. The Google Scholar search engine was employed in combination with website searching and citation chaining to find relevant grey literature.
Study selection and screening
Initial screening of article titles and abstracts was performed by two independent reviewers (BC and MSAA). Duplicates were removed and the full text of articles which passed this initial screening process was then assessed for eligibility against the inclusion criteria. Disagreements over inclusion or exclusion were referred to a third reviewer (AA).
Data extraction and risk of bias assessment
Data extraction was performed by two independent reviewers using a pre-defined, standardised form. Any disagreements were resolved by a third reviewer. Data extracted included study characteristics such as author, publication date, study type and study population, as well as study outcome measures and results. All included studies were assessed for risk of bias by two independent reviewers using the Cochrane risk-of-bias tool for randomised trials (RoB 2) [11] and the Risk Of Bias In Non-Randomised Studies of Interventions (ROBINS-I) tool [12]. Disagreement was resolved by referral to a third reviewer.
Data synthesis
It was not possible to undertake a meta-analysis due to heterogeneity in study design and outcome measures. Thus, results were narratively synthesised in accordance with PRISMA [9] and Synthesis without meta-analysis (SWiM) [13] guidelines.
Results
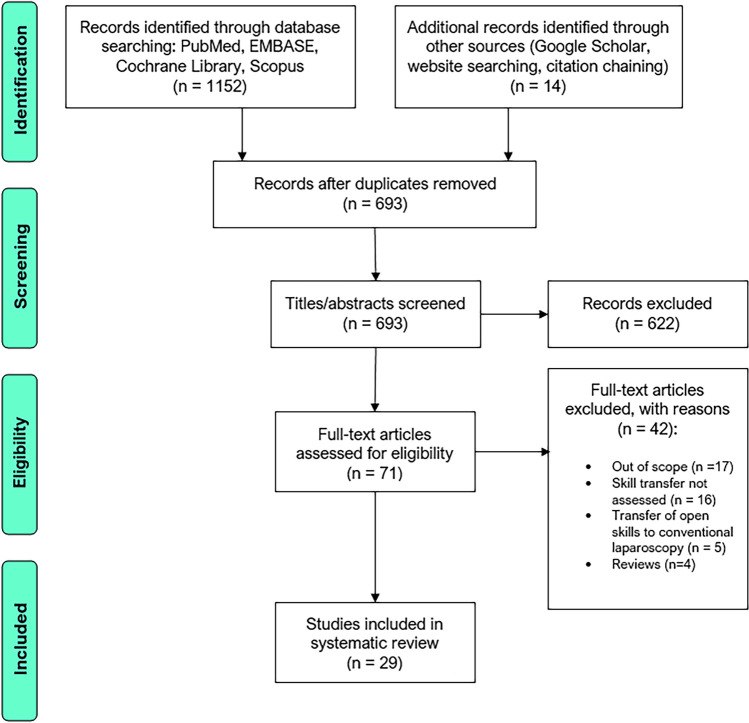
One thousand one hundred and fifty-two records were identified through database searching and fourteen additional records were identified through a search of the grey literature and citations. After deduplication, 693 studies were eligible for title and abstract screening with 622 studies being excluded, leaving 71 studies for full-text screening (Fig. 1). Forty-two studies were then excluded after full-text screening. Thus, 29 studies were included for narrative synthesis.
Fig. 1.
PRISMA flow diagram
Characteristics of included studies
The characteristics of the included studies are displayed in Tables 1 and 2. Of the studies included were 9 randomised controlled trials [20, 21, 23, 24, 27, 32, 33, 38, 42] (RCTs), 15 prospective cohort studies [15, 16, 22, 25, 26, 28–31, 34–37, 39, 41], 2 non-randomised controlled trials [18, 40], 1 retrospective cohort study [17], 1 uncontrolled before-and-after study [19] and 1 prospective single-surgeon study [14]. The publication dates of the included studies ranged from 2003 to 2020. All studies had a small sample size ranging from the results of 1 surgeon [14] to 21 participants [30]. Study participants included medical students, surgical trainees of all levels of training and expert surgeons. Robotic systems used in studies included the da Vinci Surgical System (Intuitive Surgical, Sunnyvale, CA), the Mimic dV-Trainer (Mimic Technologies Inc., Seattle, Washington), the RoSS surgical simulator (Simulated Surgical Systems, Williamsville, New York) and the Senhance Surgical System (TransEnterix Inc., Morrisville, NC).
Table 1.
Characteristics of included studies assessing skills transfer in clinical settings
| Study author, year | Skill transfer assessed | Specialty, country | Participants | Procedure(s) | Comparison group(s) |
|---|---|---|---|---|---|
| Ahlering et al. [14], 2003 | Open → R | Urology, USA | 1 Urological oncologist (open exp. only) | 45 robot-assisted lap. radical prostatectomy | None |
| Eddib et al. [15], 2013 | Lap.→ R | Gynaecology, USA | 64 cases performed by advanced lap. surgeons (lap. hysterectomy exp.) | Robot-assisted lap. hysterectomy | 72 cases performed by intermediate lap. surgeons (no lap. hysterectomy exp.) |
| Kilic et al. [16], 2012 | Lap. → R | Gynaecology, USA | 7 Gynaecology residents with ≥ 3 lap. experiences |
Vaginal cuff closure with either: robotic suturing with intracorporeal knot tying Lap. suturing with extracorporeal knot tying |
6 Gynaecology residents with ≤ 2 lap. experiences |
| IK. Kim et al. [17], 2014 | Lap. → R | Colorectal surgery, South Korea | First 100 consecutive cases performed by 1 surgeon (exp. of > 300 lap. colorectal operations) | Robot-assisted low anterior resection for rectal cancer | First 100 consecutive cases performed by 1 surgeon (exp. of < 30 lap. colorectal operations) |
exp. experience, lap. laparoscopic, R. robotic
Table 2.
Characteristics of included studies assessing skill transfer in simulated settings
| Study author, year | Skill transfer | Participants | Task sequence | Comparison group(s) |
|---|---|---|---|---|
| Anderberg et al. [18], 2010 | Lap. → R | 10 medical students (SN) performing tasks with conv. lap. first then on the da Vinci robot |
Repeated 4 times on each platform: Grab the Needle Continuous Suturing Tie a knot |
10 medical students (SN) performing tasks with the robot first then with conv. lap |
| Angell et al. [19], 2013 | Lap. → R | 14 medical students (SN) |
Spiral cutting exercise using da Vinci robot 1 month lap. training (no robotic exposure) Repeat spiral cutting exercise on da Vinci robot and on lap. box trainer |
None |
| Ashley et al. [20], 2019 | Lap. → R | 15 medical students (SN) trained on a lap. simulator and assessed on robotic simulator (RoSS) |
Balloon Grasp and Ball Drop tasks on RoSS, and Peg Transfer and Ball Drop tasks on lap. simulator Participants randomised to either lap. simulator or RoSS and perform Ball Drop 10 times Perform Ball Drop with the unpractised modality |
16 medical students (SN) trained on RoSS and assessed on lap. simulator |
| Blavier et al. [21], 2007 | Lap. → R | 40 medical students (SN) performing tasks with conv. lap. before switching to the da Vinci robot, or vice versa | Needle Guidance task | Medical students performing task with the robot first, then with conv. lap |
| Cumpanas et al. [22], 2017 | Open → R | 10 trainee surgeons (> 2 years of open surgical exp. only) |
3 repetitions on da Vinci Skills Simulator of: Peg Board Level 1 (easy) Energy Dissection Level 2 (intermediate) Suture Sponge Level 3 (difficult) |
15 final year medical students (SN) |
| Davila et al. [23], 2017 | Lap. → R | 9 surgical trainees (RN with limited lap. exp.) trained on lap. simulator then assessed on the da Vinci robot |
3 consecutive attempts each of Intracorporeal Knot Tying and Peg Transfer tasks performed on the robot Participants undergo 4 1-h training sessions in their assigned training modality Robotic skills then reassessed with the same two tasks |
88888surgical trainees receiving no training 10 surgical trainees trained on da Vinci Skills Simulator |
| Feifer et al. [24], 2010 | Lap. → R |
5 medical students (SN) undergo ProMIS (Haptica, Ireland) practice 5 medical students (SN) undergo LapSim (Surgical Science, Sweden, AB) practice 5 medical students (SN) undergo ProMIS and LapSim training |
Baseline evaluation on da Vinci robot with Peg Transfer, Pattern Cutting, Intracorporeal Suturing and Cannulation Participants undergo practice on assigned platform Reassessed on da Vinci robot |
5 medical students (SN) undergo no lap. training |
| Finnerty et al. [25], 2016 | Lap. → R | 28 surgical residents (RN with varying lap. experience ranging from 1 to 750 cases logged) |
1 trial on da Vinci robot of: Match Board Energy Dissection Suture Sponge |
8 medical students (SN) |
| Hagen et al. [26], 2009 | Lap. → R | 16 lap. trained fellows or senior surgeons |
10 repetitions on da Vinci robot of: Rubber Ring Placement Suturing with Knot Tying Needle Guidance |
18 medical students or residents (LN) |
| Hassan et al. [27], 2015 | Lap. → R | 15 medical students and junior residents (SN) performing tasks with conv. lap. first then on da Vinci robot |
5 repetitions on each platform of: Pick and Place Thread the Ring |
15 medical students and junior residents (SN) performing tasks with R. lap. first then with conv. lap |
| Jayaraman et al. [28], 2010 | Lap. → R | Lap. exp. surgeon (RN) | Each participant performed 10 lap. and 10 robotic choledochojejunostomies on ex vivo model consisting of porcine livers with contiguous intestines |
Surgeon with R. and lap. exp Surgeon with only basic lap. exp |
| Kim et al. [29], 2014 | Lap. → R | 10 lap. exp. surgeons (RN) |
Bead Transfer, Ring Insertion onto Cone, and Suturing with Knot Tying tasks performed on both lap. and da Vinci robotic platforms Tasks repeated after an 8-week interval |
10 LN medical students |
| Kowalewski et al. [30], 2018 |
Open → R Lap. → R |
25 surgeons (varying levels of open and lap. exp.) |
1 repetition each on da Vinci robot of: Peg Board Pick and Place Thread the Rings Suture Sponge |
37 medical students (SN) |
| McVey et al. [31], 2016 | Lap. → R | 32 trainees with varying levels of lap. exp |
Participants undergo 4 week robotic surgery course Assessed pre- and post-course on R. and lap. platforms: Peg Transfer Intracorporeal Suturing and Knot Tying |
Comparisons performed in analysis based on baseline lap. skill score |
| Moncayo et al. [32], 2019 | Lap. → R | 6 medical students (SN) performing tasks on the lap. platform first then on the R. platform |
Repeated 5 times on each platform: Thread the Ring Transfer the Plot |
6 medical students (SN) performing tasks on the R. platform first then on the lap. platform |
| Obek et al. [33], 2005 | Lap. → R | 10 medical students (SN) assessed with robotics first, undergo conv. lap. training then reassessed with robotics |
Intracorporeal Knot Tying performed on assigned pre-training platform Knot Tying practiced with assigned training method Knot Tying reassessed on pre-training platform |
10 medical students (SN) assessed with conv. lap. first, undergo R. training then reassessed with conv. lap |
| Panait et al. [34], 2014 | Lap. → R | 14 lap. exp. surgery residents (RN) |
Tasks performed on lap. platform first and then on R. platform (after a 24 h interval): Peg Transfer (easiest task) Circle Cutting (intermediate) Intracorporeal Suturing (hardest task) |
14 medical students with minimal lap. exp. and no R. exp |
| Passerotti et al. [35], 2015 | Lap. → R | 12 lap. exp. surgeons (RN) |
Performed in 5 consecutive, weekly training sessions on both the lap. and robotic platforms: Peg Transfer Precision Cutting Suturing with Intracorporeal Knot Tying |
31 SN |
| Pimentel et al. [36], 2018 | Lap. → R | 20 lap. exp. surgeons (RN) |
4 repetitions on da Vinci-Trainer of the following sequence: Peg Board 2 Ring and Rail 1 Suture Sponge 1 |
20 first-year surgical residents with minimal lap. and no robotic exp |
| Teishima et al. [37], 2012 | Lap. → R | 10 lap. exp. urologic surgeons (RN) |
4 repetitions on da Vinci-Trainer of: Pick and Place Peg Board Rope Walk Energy Dissection Suture Sponge Thread the Rings |
13 lap. inexp. urologic surgeons (RN) |
| Thomaier et al. [38], 2017 | Lap. → R | 20 medical students (SN) practice on lap. simulator |
Baseline evaluation of Peg Transfer on lap. simulator and Peg Board 1 on robotic simulator Participants then undergo practice session on assigned platform Reassessed performing the Peg Transfer task on both simulators |
20 medical students (SN) practice on robotic simulator |
| Tillou et al. [39], 2016 | Lap. → R | 20 senior residents, registrars and attending surgeons (lap. trained) |
To ensure progressive learning, the following task sequence was used on da Vinci Skills simulator: Camera Targeting 1 & 2 Ring Walk 1 & 2 Suture Sponge 1 & 2 Energy Switching 1 and Dissection Participants could only start next task upon scoring ≥ 80% in previous one |
8 junior residents (with no formal lap. training) 2 experienced robotic surgeons |
| Vurgun et al. [40], 2020 | Lap. → R |
6 medical students (SN) undergo 20 min of lap. training 6 medical students (SN) undergo 40 min of lap. training |
Participants undergo assigned lap. training Participants then complete Rope Passing and Ball Placement tasks on Laparo Advance box trainer (Laparo LLC, Wroclaw, Poland) and then similar tasks on Senhance robotic simulator (Senhance Surgical System & Kroton LLC, Warsaw, Poland) |
11 medical students (SN) receive no lap. training |
| Yoo et al. [41], 2015 | Lap. → R | 11 lap. exp. surgeons (no robotic experience) |
1 trial on da Vinci-trainer of: Pick and Place Peg Board Match Board |
14 medical students (SN) |
| Zihni et al. [42], 2016 | Lap. → R | 26 RN |
Tasks performed 3 times each on each platform (Robotic/Lap.). Platform and task order randomised: Peg Transfer Pattern Cutting Intracorporeal Suturing |
Comparisons made on platform order |
conv. lap. conventional laparoscopy, exp. experience, inexp. inexperienced, lap. laparoscopic, LN laparoscopic naïve, R robotic, RCT randomised controlled trial, RN robotics naïve, SN surgically naïve
Risk of bias
The results of the risk of bias assessment are depicted in Appendices 1 and 2. Two studies were assessed to have low risk of bias [23, 38] while nineteen studies were judged to have some concerns over risk of bias. Eight studies were deemed to be at high overall risk of bias.
Findings
The heterogeneity in study design, participants, interventions and outcome measures prevented the undertaking of a meta-analysis so the results were narratively synthesised, categorised into the type of setting and then into either transfer of open skills or transfer of laparoscopic skills.
Real-time skills transfer
Four studies [14–17] evaluated skill transfer in the clinical setting (Table 3). One study [14] demonstrated the successful transfer of open skills to robotic prostatectomy, describing an experienced open surgeon (with robotic experience of a day’s training course and two cadaveric procedures) achieving a 4-h proficiency after just 12 patients. All outcomes were satisfactory and equivalent to the performances of ‘expert’ surgeons who had experience of over 100 robotic procedures.
Table 3.
Main results of included studies assessing skill transfer in clinical settings
| Study author, year | Relevant outcome measures | Statistical analysis | Key findings | Skill transfer demonstrated? |
|---|---|---|---|---|
| Ahlering et al. [14], 2003 |
Operative time, time of completion of each operative step EBL Hb drop Length of hospital stay Resection margin status Continence and potency |
Not reported |
4-h proficiency achieved after 12 cases Satisfactory outcomes in all metrics |
Yes—successful transfer of open surgical skills |
| Eddib et al. [15], 2013 |
Total operative time, console time, closing time, procedure time EBL Hb drop Length of hospital stay Pain medication use Complications |
Student’s t test |
Lap. exp. vs lap inexp. surgeons: Mean procedure time: 121 vs 174 min (p < 0.05) Mean console time: 70 vs 119 min (p < 0.05) Mean EBL: 64 vs 84 ml (p = 0.3) Mean Hb drop: 1.7 vs 1.33 (p = 0.2) Pain medication use: 74.9 vs 68.8 mg morphine (p = 0.83) Length of stay: 1.07 vs 1.35 days (p = 0.29) |
Advanced lap. experience only significantly impacted length of procedure but no other variables |
| Kilic et al. [16], 2012 | Suture time | t test |
Lap. exp. surgeons: significant time reduction from laparoscopy to the robot (457 ± 158 s vs 337 ± 235 s, p = 0.02) LN participants: non-significant time reduction (p = 0.5) No significant differences between lap. exp. and LN mean suturing times on either platform (laparoscopy: p = 0.009, robot: p = 0.5) |
Yes—previous lap. experience improves the robotic surgery learning curve |
| Kim et al. [17], 2014 |
Operative time Conversion rate to open surgery Time to first flatus Time to soft diet resumption Length of hospital stay Post-operative morbidity or mortality Complications Resection margin status |
Pearson’s Chi-squared test Fisher’s exact test Student’s t test Moving average method |
Less exp. surgeon had shorter operation time (272.6 ± 121.8 vs 344.0 ± 59.7 min, p < 0.001) Lap. exp. surgeon’s patients had shorter hospital stays (8.7 ± 3.7 vs 12.7 ± 12.9 days, p = 0.003) and less time to soft diet resumption (3.4 ± 1.4 vs 6.5 ± 5.6 days, p < 0.001) Bowel motility: no significant difference in time to first flatus (p = 0.462) |
No—substantial previous lap. experience does not translate into superior performances |
EBL estimated blood loss, exp. experienced, Hb haemoglobin, inexp. inexperienced, lap. laparoscopic, LN laparoscopic-naïve
Three studies [15–17] assessed the transfer of laparoscopic skills to robotic surgery in the clinical setting. Eddib et al. [15] evaluated robot-assisted laparoscopic hysterectomy performances with the only significant difference reported being that the advanced laparoscopic surgeons had a shorter mean procedure time (121 vs 174 min, p < 0.05) with comparable performances in all other metrics. Kilic et al. [16] also reported time reductions for laparoscopically trained participants, concluding that prior laparoscopic experience contributes to an improved robotic surgery learning curve in the context of vaginal cuff closure. In contrast, IK. Kim et al. [17] evaluated the first 100 robot-assisted rectal cancer resections performed by a highly experienced laparoscopic surgeon and a surgeon with limited laparoscopic experience, finding comparable results overall.
Simulated setting
Table 4 illustrates the findings of the studies assessing skill transfer in the simulated setting. Two studies [22, 30] assessed the transfer of open skills to robotic surgery, with both using the da Vinci Skills Simulator. Cumpanas et al.’s [22] cohort study found no significant difference in the overall performance of open surgeons and surgical novices on the basic robotic task of Peg Board (80 vs 78%, p = 0.5) but as task complexity increased, the open surgeons performed significantly better. Conversely Kowalewski et al. [30] found no significant differences in the performances of open surgical novices, intermediates and experts on the Peg Board, Pick and Place and Suture Sponge tasks, with novices outperforming experts on the Thread the Ring task.
Table 4.
Main results of included studies assessing skill transfer in simulated settings
| Study author, year | Relevant outcome measures | Statistical analysis | Key findings | Skill transfer demonstrated? |
|---|---|---|---|---|
| Anderberg et al. [18], 2010 |
‘Grab the needle’ time ‘Continuous suturing’ time ‘Tie a knot’ time Damage to skin pad Number of times needle dropped Number of times thread torn |
Wilcoxon’s signed rank test for paired samples Mann–Whitney U test of two independent samples |
Grab the needle: no significant differences Continuous suturing: R. lap. last (conv. lap. first) outperformed R. lap. first group (144 ± 70 vs 216 ± 123 s, p = 0.049) Tying a knot: R. lap last (conv. lap first) outperformed R. lap first group (91 ± 35 vs 152 ± 94 s, p = 0.004) |
Yes—successful lap. skill transfer for advanced task |
| Angell et al. [19], 2013 |
Time to complete exercise Errors in technique |
Student’s t test |
Statistically significant improvement in mean time (9.04 vs 16.72 min p = 0.0002) and errors (3.57 vs 6.21 errors, p = 0.02) for robotic performance before and after laparoscopic training After laparoscopic training, task was completed faster (p < 0.001) and with fewer errors (p < 0.01) robotically compared to laparoscopically despite no robotic training |
Yes—successful lap. skill transfer |
| Ashley et al. [20], 2019 | Time to complete exercise |
Two-sample t test Paired t test Fisher’s exact test or Chi-squared test for categorical data |
Degree of improvement was not significantly better than 2 rounds of practice on the practiced modality (p = 0.98) | No evidence of lap. skill transfer |
| Blavier et al. [21], 2007 |
Performance score Error score Ambidexterity score |
Repeated measures analysis of variance Newman–Keuls test for post hoc comparisons |
After change to the alternate platform, performance decreased reaching the same score as the 1st trial indicating no skill transfer | No evidence of lap. skill transfer |
| Cumpanas et al. [22], 2017 |
Overall percentage score Time to complete exercise Objects dropped Number of times instrument out of view Economy of motion Instrument collisions Misapplied energy time Excessive instrument force Master workspace |
Two-tailed paired t test |
Peg Board: open surgeons achieved better economy of motion (145 vs 167 cm, p = 0.012) and drops (0.18 vs 0.66, p = 0.013) scores with SN achieving better master workspace (9 vs 11, p = 0.016) Energy dissection: open surgeons significantly outperformed SN in all metrics except master workspace where they achieved a worse score than SN (16.3 vs 15, p = 0.03) Suture Sponge: open surgeons significantly outperformed SN in all metrics except master workspace where they achieved a similar score to SN (8.1 vs 8.4, p = 0.3) |
Yes—more open surgical skill transfer occurs as task complexity increases |
| Davila et al. [23], 2017 | Performance score (based on time taken and number of errors) | One-way analysis of covariance (ANCOVA) |
Intracorporeal Knot Tying scores improved significantly after FLS training compared to dVSS (p = 0.018) and no training (p = 0.005) Peg Transfer scores improved significantly after FLS training compared to no training (p = 0.01) |
Yes—successful lap. skill transfer |
| Feifer et al. [24], 2010 |
ProMIS performance score LapSim performance score |
Mann–Whitney U test |
Significant performance improvement in all 4 robotic tasks were identified in the dual training group (p < 0.05) Participants in the no training group performed worse in all tasks and showed no significant performance improvement |
Yes—successful lap. skill transfer |
| Finnerty et al. [25], 2016 |
Performance score Economy of motion Time to complete Instrument collisions Master workspace range Critical errors Instruments out of view Excessive instrument force Missed targets Object drops Misapplied energy time |
Fisher’s exact test and Chi-squared test Student’s t test and Mann–Whitney U test Logistic and linear regressions |
Matchboard and Energy Dissection median scores did not significantly differ between groups (p = 0.27 and 0.99 respectively) Senior surgical residents achieved the highest median Suture Sponge score (p = 0.039) Suture Sponge performance significantly correlated with number of lap. cases logged during residency (p = 0.005, r2 = 0.21) |
Yes—increased lap. skill transfer seen for advanced task |
| Hagen et al. [26], 2009 | Time to complete exercise | t-test | Lap. exp. participants achieved a better robotic task performance than lap. novices (p < 0.05) | Yes—lap. exp. correlates with robotic skill |
| Hassan et al. [27], 2015 |
Time to complete exercise Object drops Instrument collisions Number of times instrument out of view Excessive instrument force |
Mann–Whitney U test of two independent samples |
Pick and Place: mean time on robotic platform was 41 s without previous lap. exp. vs 35 s with lap. exp. (p = 0.2) Thread the Ring: no significant difference in mean time on robotic platform for no previous lap. exp. vs those with exp. (212 vs 216 s (p = 0.66)) |
No evidence of lap. skill transfer |
| Jayaraman et al. [28], 2010 |
Procedure time Complications Number of bites for front and back wall Anastomotic integrity |
Student’s t test Chi-squared test |
Lap exp. surgeon rapidly overcame his learning curve for the R. procedure (36.8 ± 5.8 vs. 24.7 ± 0.6 min, p = 0.02) and achieved plateau after 3 cases Increased minimally invasive surgical exp. correlated with decreased probability of anastomotic leak |
Yes—lap. exp. contributed to rapid achievement of proficiency and better anastomosis |
| Kim et al. [29], 2014 | Time to complete each exercise |
Mean values calculated for continuous data Fisher’s exact test or Chi-squared test for categorical data |
Robotic tasks were performed better and faster by lap. exp. participants compared to lap. novices but only ‘suturing and knot tying’ task achieved statistical significance (p = 0.011 in 1st trial, p = 0.003 in 2nd trial) | Yes—successful lap. skill transfer for advanced task |
| Kowalewski et al. [30], 2018 |
Overall performance score Time to complete each exercise Economy of motion Instrument collisions Excessive instrument force Instruments out of view Master workspace range Object drops Missed targets |
Analysis of variance (ANOVA) Kruskal–Wallis test for non-parametric data |
Thread the Ring task: both open and lap. novices outperformed experts (p = 0.002 and p = 0.004, respectively) No significant differences between groups for the Peg Board, Pick and Place and Suture Sponge tasks |
No evidence of either open or lap. skill transfer |
| McVey et al. [31], 2016 |
Time to complete each exercise Global rating score using Likert scale provided by two blinded experts |
Paired sample t test Wilcoxon matched-pairs test ANOVA |
Baseline lap. task time of trainees on Intracorporeal Suturing with Knot Tying (ISKT) task correlated with post-robotic performances of Peg Transfer (r = 0.480) and ISKT time (r = 0.529, p < 0.01) | Yes—successful lap. skill transfer for advanced task |
| Moncayo et al. [32], 2019 |
Time to complete each exercise Objective Structured Assessment of Technical Skills (OSATS) |
Paired t test Wilcoxon test Mann–Whitney U test |
Thread the Ring task: transfer of laparoscopic skills to robotic skills was statistically significant (p = 0.01) Transfer the Plot task: no statistically significant transfer effect was seen (p = 0.96) |
Yes—successful lap. skill transfer for advanced task |
| Obek et al. [33], 2005 | Overall performance score | Paired t test for within-group comparison t test |
Post-training scores increased significantly from 57.4 to 81.8 for the lap. trained group (p = 0.02) and from 27.4 to 66.1 for the R. trained group (p = 0.04) Statistically significant decrease in error score in the lap. trained group, from 42.1 to 16.2 (p = 0.02) |
Yes—evidence of incomplete lap. skill transfer |
| Panait et al. [34], 2014 | Overall performance score | Paired t test | Lap. exp. trainees achieved similar robotic and laparoscopic scores for Circle Cutting (64 ± 9 vs 69 ± 15, p > 0.05) and Intracorporeal Suturing tasks (95 ± 3 vs 92 ± 10, p > 0.05) | Yes—lap. skill transfer demonstrated for more advanced tasks |
| Passerotti et al. [35], 2015 | Time to complete each exercise |
Statistical models created using generalised estimating equations with Poisson’s marginal distribution and link logarithmic function Interactions between the variables were assessed using Bonferroni multiple or post hoc comparison |
Peg Transfer: lap. exp. and novice participants both achieved learning curve plateau after 3rd session although exp. participants had a lower average completion time than novices at every corresponding session (p < 0.01) Precision cutting: lap. exp. participants achieved learning curve plateau after 2nd session, novices after 4th session. Exp. participants had a lower average completion time than novices at every corresponding session (p < 0.01) Simple suturing with intracorporeal knot tying: lap. exp. participants showed no improvement from the first to last sessions (p = 0.50) but completed the task faster than novice participants at every corresponding session |
Yes – lap. skill transfer demonstrated, most evident in the advanced tasks |
| Pimentel et al. [36], 2018 |
Overall performance score Time to complete exercise Object drops Economy of motion Excessive instrument force Instrument collisions Instruments out of view Master workspace range Missed targets |
Mann–Whitney U test Friedman test |
No statistically significant difference in overall score between lap. exp. and LN for all tasks: Peg Board 2 (p = 0.57), Ring and Rail 1 (p = 0.113), Suture Sponge 1 (p = 0.67) | No evidence of lap. skill transfer |
| Teishima et al. [37], 2012 |
Overall performance score Time to complete exercise Critical errors Number of drops Economy of motion Excessive instrument force Instrument collisions Master workspace range |
Mann–Whitney U test Wilcoxon test |
No significant differences between groups for Pick and Place, Peg Board, Rope Walk, Thread the Rings and Energy Dissection tasks Participants with more lap. exp. performed significantly better in the 2nd (p = 0.0236) and 3rd trials (p = 0.0043) of Suture Sponge than less exp. counterparts but no significant difference in 4th trial (p = 0.1068) |
Yes—limited evidence of lap. skill transfer |
| Thomaier et al. [38], 2017 |
Time to complete exercise Error rate Mimic da Vinci-trainer motion metrics Modified global rating score |
Student’s t test |
Decrease in mean completion time for lap. trained group (120 vs 167 s, p = 0.004) R. trained group had significantly faster (p < 0.001) and better robotic task performance with higher global rating scale scores (p = 0.006) compared to the lap. trained group |
Yes—successful but incomplete lap. skill transfer |
| Tillou et al. [39], 2016 |
Performance index Time to complete exercise Instrument collisions Economy of movement Excessive instrument force Instruments out of view Workspace size |
Dunn’s multiple comparisons test |
No significant differences between junior and senior resident scores and the scores of attending surgeons (p = 0.45) Attending surgeons needed more exercise repetitions than registrars (p = 0.024) |
No evidence of lap. skill transfer |
| Vurgun et al. [40], 2020 |
Time to complete exercise Clutch use Errors (number of ball drops, instruments out of view, interruptions requiring manual adjustments) |
Pearson Chi-squared test Independent-samples Kruskal–Wallis test |
Ball placement task: no significant differences between groups for any metric Rope Passing task: no significant differences between groups for any metric |
No evidence of lap. skill transfer |
| Yoo et al. [41], 2015 |
Overall performance score Time to complete exercise Number of drops Economy of motion Instruments out of view Excessive instrument force Instrument collisions Master workspace range |
Independent-sample t test Mann–Whitney U test |
No significant differences between overall scores of lap exp. participants and SN on Pick and Place (67.55 vs 75.71%, p = 0.337), Peg Board (51.36 vs 41.56%, p = 0.239) and Match Board (43.30 vs 42.31%, p = 0.706) tasks Lap exp. participants scored significantly better in the number of instrument collisions (4.11 ± 2.98 vs. 1.18 ± 1.60, p = 0.016), and the number of drops (2.67 ± 1.80 vs. 1.00 ± 1.01, p = 0.028), |
No significant evidence of lap. skill transfer |
| Zihni et al. [42], 2016 |
Time to complete exercise Errors per trial (EPT) |
Unpaired Student’s t test |
Lap. trained group made more errors on the robotic Pattern Cutting task (1.86 vs 1.03 EPT, p = 0.02) No significant differences between the groups for Peg Transfer or Intracorporeal Suturing |
No evidence of lap. skill transfer |
conv. lap. conventional laparoscopy, dVSS da Vinci Surgical System, exp. experience, FLS Fundamentals of Laparoscopic Surgery, lap. laparoscopic, LN laparoscopic naïve, R robotic, RN robotics naïve, SN surgically naïve
Twenty-four studies [18–21, 23–42] evaluated the transfer of laparoscopic skills to robotic surgery in the simulated setting. Thomaier et al. [38] assessed the performance of a basic robotic task (Peg Transfer) by surgical novices trained on either a laparoscopic or a robotic simulator, reporting that the laparoscopic trained group successfully transferred their skills to the robot with the mean time to complete the robotic task decreasing from baseline (167 vs 120 s, p = 0.004) with significant improvements in the global rating composite score and instrument collisions score. The transfer is incomplete, however, as the laparoscopic trained group were outperformed on the robotic platform by the robot trained group.
Three studies [24, 26, 35] reported successful skill transfer in both basic and advanced tasks. Hagen et al. [26] found that laparoscopically trained surgeons significantly outperformed laparoscopically naïve participants on ring placement, suturing with knot tying and needle guidance tasks, concluding that laparoscopic experience is a strong predictor of robotic performance. Feifer et al. [24] described significant performance improvements in all robotic tasks (Peg Transfer, Cutting, Intracorporeal Knot Tying and Cannulation) for surgical novices who had received dual training on augmented reality (ProMIS) and virtual reality (LapSim) laparoscopic simulators, with no significant improvements observed in those who had received no training and fewer significant improvements in participants who had trained on either simulator alone.
Ten studies [18, 19, 23, 25, 28, 29, 31–34] found that laparoscopic skill transfer was most evident when advanced surgical tasks such as intracorporeal knot tying or suturing were performed. In an RCT conducted by Davila et al. [23], the mean score improvement for robotic intracorporeal knot tying was greatest for inexperienced surgical trainees who had undergone 4 weeks of laparoscopic training compared to those who instead received 4 weeks of robotic training (82.2 vs 40.5 points, p = 0.018). In accordance with the findings of Davila et al., Panait et al.’s [34] cohort study reported that performances on the robot equalled those on the laparoscopic platform as the complexity of tasks increased thereby demonstrating transfer of skills.
Finnerty et al. [25] echoed these findings, reporting a statistically significant correlation between the number of laparoscopic operations logged by surgical trainees and performance on an advanced robotic task only (Suture Sponge) (p = 0.005, r2 = 0.21). Jayaraman et al.’s [28] study also reported that increased minimally invasive surgical experience correlated with a decreased likelihood of anastomotic leak when performing the complex task of suturing a biliary-enteric anastomosis in robotic choledochojejunostomies on a porcine model.
McVey et al.’s [31] cohort study found that baseline laparoscopic task time of surgical trainees on the advanced Intracorporeal Suturing with Knot Tying (ISKT) task, but not the basic Peg Transfer (PT) task, correlated with post-robotic training performances of both Peg Transfer and ISKT time. In a similar fashion, Moncayo et al. [32] described significant skill transfer for laparoscopically trained students to the confined space of the simulated paediatric robotic platform for the advanced Thread the Ring task (p = 0.01) but not for the basic Transfer the Plot task (p = 0.96). Obek et al. [33] evaluated the performances of laparoscopically trained students on the advanced knot tying robotic task, reporting that their composite score significantly increased after training (43% improvement, p = 0.02) with a significant decrease in error score (16.2 vs 42.1, p = 0.02) thereby demonstrating skill transfer to the robot.
In contrast, nine studies [20, 21, 27, 30, 36, 39–42] found no evidence of skill transfer in either basic or advanced tasks. Tillou et al.’s [39] study involved assessment of the more advanced task of suturing alongside basic tasks such as camera manipulation and Endowrist handling, finding comparable performances across all tasks between laparoscopically experienced surgeons and laparoscopically naïve trainees thereby signifying a complete lack of skill transfer. Similarly, Zihni et al. [42] found no evidence of laparoscopic skill transfer in both basic and advanced robotic tasks, noting that prior performance of the Pattern Cutting task on the laparoscopic platform appeared to impede subsequent performance of the task on the robot. Teishima et al. [37] reported significantly better overall Suture Sponge scores in the initial trials for laparoscopic experts compared to surgeons with less experience but by the fourth trial, there was no significant difference in scores (59.1 ± 19.5 vs 49.1 ± 7.0, p = 0.1068) suggesting that laparoscopic experience only confers an advantage in the initial phase of the robotic learning curve.
Discussion
Robotic training curricula consist of multiple modalities aiming to develop the necessary cognitive and psychomotor skills for safe robotic surgical practice. These modalities include dry and wet laboratory training, virtual reality simulation and online lectures [43]. Skill transfer from robotic virtual reality simulation to the operative environment has been demonstrated, thereby indicating its integral role in training curricula [44]. This review aimed to evaluate the presence of crossover from a trainee’s open or laparoscopic skills as any such skill transfer might accelerate the robotic training process and also result in greater availability of expensive robotic simulators to other trainees as less time is spent in the simulation phase. The results of the 29 included studies found conflicting evidence relating to the transfer of open and laparoscopic skills to robotic surgery in both clinical and simulated settings.
Successful open surgical skill transfer to the robotic clinical setting was demonstrated with satisfactory peri- and post-operative outcomes achieved in the absence of any laparoscopic experience [14]. However, the findings of the studies conducted in the simulated setting confirm the current view in surgical practice that open surgical skill transfer of any extent is insufficient in itself to enable a direct transition to robotic surgical practice in the absence of any systematic robotic training; one study found no evidence of any skill transfer [30] while the other reported skill transfer only for advanced robotic tasks [22].
Laparoscopic surgical experience only translates into reduced robotic procedure time in the clinical setting, with no significant improvement in other metrics [15, 16]. One study [17] contrarily reported that the surgeon with the least laparoscopic experience had a significantly shorter mean operative time but acknowledged confounders such as differing specimen extraction and anastomosis techniques between the surgeons which might have affected procedure time. Successful laparoscopic skill transfer does occur in the simulated setting, most notably when advanced robotic tasks are performed [37] although some studies did observe a transfer effect for basic tasks as well [23, 24, 26, 35, 38]. Substantial laparoscopic experience is not essential for successful skill transfer to occur as six studies [18, 19, 24, 32, 33, 38] reported a transfer effect in surgical novices following their completion of short laparoscopic training courses.
Thus, for both open and laparoscopic modalities, several studies suggested a possible correlation between task complexity and the extent of skill transfer. This is consistent with the high construct validity (ability to differentiate between experts and novices) associated with advanced robotic tasks such as Suture Sponge [45], so any superiority in the performances of open or laparoscopically experienced participants would be most evident in these tasks. Cumpanas et al. [22] attributed open surgeons’ extensive prior experience in guiding the needle from different angles when performing suturing as the reason for the transfer effect seen but noted that this inclination to reproduce their usual open surgery hand movements on the robotic console resulted in a worse master workspace score (a metric representing the virtual space used by the instruments during task performance). In contrast, Pimentel et al. [36] reported significantly better master workspace scores for laparoscopic surgeons as they are accustomed to manoeuvring instruments in a confined space which suggests that, unlike open surgical experience, prior laparoscopic experience enhances efficiency of movement on the robotic platform.
As described for open surgery [22], another reason for the laparoscopic transfer effect observed on advanced tasks may include an existing skillset of needle driving developed through repetitive practice and experience which predisposes laparoscopically trained participants to a more precise performance on the robot [25, 26, 29]. Two studies [24, 33] also conjectured that laparoscopic training facilitates the development of visual cues associating knot tension with suture resistance, thus preparing the participant for the loss of haptic feedback on the robotic platform but this is contrary to existing literature which reported that the perception of haptic feedback on the robot is similar between novices and laparoscopic surgeons [46].
There may be a preliminary period in which laparoscopically trained subjects transitioning to robotics adopt a conservatory strategy with camera and instrument movements [21] as they ‘unlearn’ certain laparoscopic-associated acquisitions [39] such as adjustment for the fulcrum effect [41] to adapt to the robotic console. This could explain why, for studies in which a progressively difficult task sequence was employed, performances improved as task complexity increased because the initial basic robotic tasks may serve to prime and enable modification of the laparoscopic skillset to the robot. This, therefore, implicates a role for systematic robotic training to include both basic and advanced tasks regardless of a surgeon’s prior laparoscopic experience.
Limitations
Limitations to the review findings include the low quality of certain studies, small sample sizes and low number of task repetitions assessed in some of the included studies. Reporting of outcomes also varied between studies, thus preventing a meta-analysis of results, with some studies electing to use time and score measurements only which precludes comprehensive assessment of surgical performance [47]. Confounders for laparoscopic skill transfer studies such as open surgical experience [22, 29] and video gaming experience [48] were inconsistently reported with variation in the definition of ‘laparoscopically experienced’; having more than 3 previous laparoscopic experiences constituted ‘experienced’ in one study [16] whereas participants with up to 750 laparoscopic cases logged were classed as ‘experienced’ in another [25]. At review level, the exclusion of non-English language studies may have increased the risk of language bias. However, strengths of the review include its comprehensive search strategy of numerous databases, adherence to the PRISMA [9] and SWiM [13] checklists, thorough quality assessment and its nature as the first systematic review investigating skill transfer of these modalities.
Implications for research and/or practice
All studies in the simulated setting assessed only the initial phase of the robotic surgery learning curve where skill transfer is most evident [37], so increasing the numbers of trials up to the acquisition of proficiency [23] in future studies would enable evaluation of skill transfer in the context of the whole learning curve. Given the reported additive mechanism by which a combination of virtual reality and augmented reality simulators enhance robotic performances [24], high-quality randomised controlled trials evaluating their impact on the robotic surgery learning curve are warranted especially as they can be adapted for use with robotic training modules [24] which may enable development of more cost-effective robotic surgery training curricula. Some studies also evaluated a robotic transfer effect to laparoscopy [20, 27, 32, 33, 38, 42] with contradictory findings, so further investigation of the impact of concomitantly teaching open, laparoscopic and robotic skills on trainee performances across the various modalities may aid in the development of more effective curricula to accelerate skill acquisition. Cohort studies with larger groups of surgeons in the intraoperative setting will enable more confident conclusions to be drawn regarding open and laparoscopic skill transfer in the clinical setting.
Regarding clinical practice, although all clinical studies [14–17] concluded that robotic skills can be acquired in the absence of any laparoscopic experience, open and laparoscopic training remains an essential part of robust surgical training. Robotic surgeons still employ laparoscopic skills such as pneumoperitoneum creation and adhesiolysis to facilitate port insertion [49], and they must be well-versed in open surgical techniques given the rates of conversion from robotic to open being as high as 9.2% for nephroureterectomy, for example [50]. Undergoing concomitant training across all modalities enables trainees to become more clinically skilled surgeons, able to safely and effectively undertake a variety of procedures thereby increasing the range of care they can provide. With results suggesting that laparoscopic skill transfer occurs in the initial phase of the learning curve, there is need for individually tailored curricula correlating with the level of laparoscopic expertise the trainee has.
Conclusion
Skill transfer from both modalities appears to be most apparent when advanced robotic tasks are performed in the initial phase of the learning curve but quality and methodological limitations of the existing literature prevent definite conclusions from being drawn. The impact of incorporating laparoscopic simulation into robotic training curricula on all phases of the robotic surgery learning curve and on the cost effectiveness of training should be investigated.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contributions
Baldev Chahal planned the review, performed the search strategies, extracted the data and wrote the manuscript. Mohammad S.A. Amin acted as second reviewer and contributed to writing the manuscript. Abdullatif Aydin acted as third reviewer, aided in planning of the review, and edited and reviewed the final manuscript. Kelly Ong, Azhar Khan, Muhammad S. Khan, Kamran Ahmed and Prokar Dasgupta provided revisions to the content of the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declarations
Conflict of interest
Baldev Chahal, Abdullatif Aydin, Mohammad S.A. Amin, Kelly Ong, Azhar Khan, Muhammad S. Khan and Kamran Ahmed have no conflicts of interest or financial ties to disclose. Prokar Dasgupta declares financial ties with Proximie and MysteryVibe.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lam K, Clarke J, Purkayastha S, Kinross JM. Uptake and accessibility of surgical robotics in England. Int J Med Rob Comput Assist Surg. 2021;17(1):e2174. doi: 10.1002/rcs.2174. [DOI] [PubMed] [Google Scholar]
- 2.Lanfranco AR, Castellanos AE, Desai JP, Meyers WC. Robotic surgery: a current perspective. Ann Surg. 2004;239(1):14–21. doi: 10.1097/01.sla.0000103020.19595.7d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cao L, Yang Z, Qi L, Chen M. Robot-assisted and laparoscopic vs open radical prostatectomy in clinically localized prostate cancer: perioperative, functional, and oncological outcomes: a Systematic review and meta-analysis. Medicine (Baltimore) 2019;98(22):e15770. doi: 10.1097/MD.0000000000015770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Skupin PA, Stoffel JT, Malaeb BS, Barboglio-Romo P, Ambani SN. Robotic versus open ureteroneocystostomy: is there a robotic benefit? J Endourol. 2020;34(10):1028–1032. doi: 10.1089/end.2019.0715. [DOI] [PubMed] [Google Scholar]
- 5.Brook N, Dell’Oglio P, Barod R, Collins J, Mottrie A. Comprehensive training in robotic surgery. Curr Opin Urol. 2019;29(1):1–9. doi: 10.1097/MOU.0000000000000566. [DOI] [PubMed] [Google Scholar]
- 6.Moglia A, Ferrari V, Morelli L, Ferrari M, Mosca F, Cuschieri A. A systematic review of virtual reality simulators for robot-assisted surgery. Eur Urol. 2016;69(6):1065–1080. doi: 10.1016/j.eururo.2015.09.021. [DOI] [PubMed] [Google Scholar]
- 7.Li MM, George J. A systematic review of low-cost laparoscopic simulators. Surg Endosc. 2017;31(1):38–48. doi: 10.1007/s00464-016-4953-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hertz AM, George EI, Vaccaro CM, Brand TC. Head-to-head comparison of three virtual-reality robotic surgery simulators. JSLS J Soc Laparoendosc Surg. 2018;22(1):e201700081. doi: 10.4293/JSLS.2017.00081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;2009(339):b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chahal B, Aydin A. The transfer of open and laparoscopic surgical skills to robotic surgery: a systematic review PROSPERO 2021 CRD42021231235. Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021231235, Accessed 15 Mar 2021
- 11.Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng H-Y, Corbett MS, Eldridge SM, Hernán MA, Hopewell S, Hróbjartsson A, Junqueira DR, Jüni P, Kirkham JJ, Lasserson T, Li T, McAleenan A, Reeves BC, Shepperd S, Shrier I, Stewart LA, Tilling K, White IR, Whiting PF, Higgins JPT. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 12.Sterne JAC, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hróbjartsson A, Kirkham J, Jüni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schünemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JPT. ROBINS-I: a tool for assessing risk of bias in non-randomized studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. 2020;368:l6890. doi: 10.1136/bmj.l6890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ahlering TE, Skarecky D, Lee D, Clayman RV. Successful transfer of open surgical skills to a laparoscopic environment using a robotic interface: initial experience with laparoscopic radical prostatectomy. J Urol. 2003;170(5):1738–1741. doi: 10.1097/01.ju.0000092881.24608.5e. [DOI] [PubMed] [Google Scholar]
- 15.Eddib A, Jain N, Aalto M, Hughes S, Eswar A, Erk M, et al. An analysis of the impact of previous laparoscopic hysterectomy experience on the learning curve for robotic hysterectomy. J Robot Surg. 2013;7(3):295–299. doi: 10.1007/s11701-012-0388-6. [DOI] [PubMed] [Google Scholar]
- 16.Kilic GS, Walsh TM, Borahay M, Zeybek B, Wen M, Breitkopf D. Effect of residents' previous laparoscopic surgery experience on initial robotic suturing experience. ISRN Obstet Gynecol. 2012;2012:569456. doi: 10.5402/2012/569456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim IK, Kang J, Park YA, Kim NK, Sohn SK, Lee KY. Is prior laparoscopy experience required for adaptation to robotic rectal surgery? Feasibility of one-step transition from open to robotic surgery. Int J Colorectal Dis. 2014;29(6):693–699. doi: 10.1007/s00384-014-1858-2. [DOI] [PubMed] [Google Scholar]
- 18.Anderberg M, Larsson J, Kockum CC, Arnbjörnsson E. Robotics versus laparoscopy—an experimental study of the transfer effect in maiden users. Ann Surg Innov Res. 2010;4:1–6. doi: 10.1186/1750-1164-4-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Angell J, Gomez MS, Baig MM, Abaza R. Contribution of laparoscopic training to robotic proficiency. J Endourol. 2013;27(8):1027–1031. doi: 10.1089/end.2013.0082. [DOI] [PubMed] [Google Scholar]
- 20.Ashley CW, Donaldson K, Evans KM, Nielsen B, Everett EN. Surgical cross-training with surgery naive learners: implications for resident training. J Surg Educ. 2019;76(6):1469–1475. doi: 10.1016/j.jsurg.2019.06.015. [DOI] [PubMed] [Google Scholar]
- 21.Blavier A, Gaudissart Q, Cadiere GB, Nyssen AS. Comparison of learning curves and skill transfer between classical and robotic laparoscopy according to the viewing conditions: implications for training. Am J Surg. 2007;194(1):115–121. doi: 10.1016/j.amjsurg.2006.10.014. [DOI] [PubMed] [Google Scholar]
- 22.Cumpanas AA, Bardan R, Ferician OC, Latcu SC, Duta C, Lazar FO. Does previous open surgical experience have any influence on robotic surgery simulation exercises? Wideochirurgia I Inne Techniki Maloinwazyjne. 2017;12(4):366–371. doi: 10.5114/wiitm.2017.72320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Davila DG, Helm MC, Frelich MJ, Gould JC, Goldblatt MI. Robotic skills can be aided by laparoscopic training. Surg Endosc Other Intervent Techn. 2017;32:1–6. doi: 10.1007/s00464-017-5963-5. [DOI] [PubMed] [Google Scholar]
- 24.Feifer A, Al-Almari A, Kovacs E, Delisle J, Carrier S, Anidjar M. Randomized controlled trial of virtual reality and hybrid simulation for robotic surgical training. J Urol. 2010;183(4):e423. doi: 10.1111/j.1464-410X.2010.10060.x. [DOI] [PubMed] [Google Scholar]
- 25.Finnerty BM, Afaneh C, Aronova A, Fahey TJ, Zarnegar R. General surgery training and robotics: are residents improving their skills? Surg Endosc. 2016;30(2):567–573. doi: 10.1007/s00464-015-4240-8. [DOI] [PubMed] [Google Scholar]
- 26.Hagen ME, Wagner OJ, Inan I, Morel P. Impact of IQ, computer-gaming skills, general dexterity, and laparoscopic experience on performance with the da Vinci® surgical system. Int J Med Rob Comput Assist Surg. 2009;5(3):327–331. doi: 10.1002/rcs.264. [DOI] [PubMed] [Google Scholar]
- 27.Hassan SO, Dudhia J, Syed LH, Patel K, Farshidpour M, Cunningham SC, et al. Conventional laparoscopic vs robotic training: which is better for Naive users? A randomized prospective crossover study. J Surg Educ. 2015;72(4):592–599. doi: 10.1016/j.jsurg.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 28.Jayaraman S, Quan D, Al-Ghamdi I, El-Deen F, Schlachta CM. Does robotic assistance improve efficiency in performing complex minimally invasive surgical procedures? Surg Endosc. 2010;24(3):584–588. doi: 10.1007/s00464-009-0621-1. [DOI] [PubMed] [Google Scholar]
- 29.Kim HJ, Choi G-S, Park JS, Park SY. Comparison of surgical skills in laparoscopic and robotic tasks between experienced surgeons and novices in laparoscopic surgery: an experimental study. Ann Coloproctol. 2014;30(2):71–76. doi: 10.3393/ac.2014.30.2.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kowalewski KF, Schmidt MW, Proctor T, Pohl M, Wennberg E, Karadza E, et al. Skills in minimally invasive and open surgery show limited transferability to robotic surgery: results from a prospective study. Surg Endosc. 2018;32(4):1656–1667. doi: 10.1007/s00464-018-6109-0. [DOI] [PubMed] [Google Scholar]
- 31.McVey R, Goldenberg MG, Bernardini MQ, Yasufuku K, Quereshy FA, Finelli A, et al. Baseline laparoscopic skill may predict baseline robotic skill and early robotic surgery learning curve. J Endourol. 2016;30(5):588–593. doi: 10.1089/end.2015.0774. [DOI] [PubMed] [Google Scholar]
- 32.Moncayo S, Compagnon R, Caire F, Grosos C, Bahans C, Ilhero P, et al. Transition effects from laparocscopic to robotic surgery skills in small cavities. J Rob Surg. 2019;14:525–530. doi: 10.1007/s11701-019-01024-y. [DOI] [PubMed] [Google Scholar]
- 33.Obek C, Hubka M, Porter M, Chang L, Porter JR. Robotic versus conventional laparoscopic skill acquisition: implications for training. J Endourol Endourol Soc. 2005;19(9):1098–1103. doi: 10.1089/end.2005.19.1098. [DOI] [PubMed] [Google Scholar]
- 34.Panait L, Shetty S, Shewokis PA, Sanchez JA. Do laparoscopic skills transfer to robotic surgery? J Surg Res. 2014;187(1):53–58. doi: 10.1016/j.jss.2013.10.014. [DOI] [PubMed] [Google Scholar]
- 35.Passerotti CC, Franco F, Bissoli JCC, Tiseo B, Oliveira CM, Buchalla CAO, et al. Comparison of the learning curves and frustration level in performing laparoscopic and robotic training skills by experts and novices. Int Urol Nephrol. 2015;47(7):1075–1084. doi: 10.1007/s11255-015-0991-3. [DOI] [PubMed] [Google Scholar]
- 36.Pimentel M, Cabral RD, Costa MM, Neto BS, Cavazzola LT. Does previous laparoscopic experience influence basic robotic surgical skills? J Surg Educ. 2018;75(4):1075–1081. doi: 10.1016/j.jsurg.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 37.Teishima J, Hattori M, Inoue S, Ikeda K, Hieda K, Miyamoto K, et al. Impact of laparoscopic experience on the proficiency gain of urologic surgeons in robot-assisted surgery. J Endourol. 2012;26(12):1635–1638. doi: 10.1089/end.2012.0308. [DOI] [PubMed] [Google Scholar]
- 38.Thomaier L, Orlando M, Abernethy M, Paka C, Chen CCG. Laparoscopic and robotic skills are transferable in a simulation setting: a randomized controlled trial. Surg Endosc. 2017;31(8):3279–3285. doi: 10.1007/s00464-016-5359-y. [DOI] [PubMed] [Google Scholar]
- 39.Tillou X, Collon S, Martin-Francois S, Doerfler A. Robotic surgery simulator: elements to build a training program. J Surg Educ. 2016;73(5):870–878. doi: 10.1016/j.jsurg.2016.04.008. [DOI] [PubMed] [Google Scholar]
- 40.Vurgun N, Vongsurbchart T, Myszka A, Richter P, Rogula T. Medical student experience with robot-assisted surgery after limited laparoscopy exposure. J Robot Surg. 2020;15:443–450. doi: 10.1007/s11701-020-01129-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yoo B, Kim J, Cho J, Shin J, Lee D, Kwak J, et al. Impact of laparoscopic experience on virtual robotic simulator dexterity. J Minim Access Surg. 2015;11(1):68–71. doi: 10.4103/0972-9941.147696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zihni A, Ge T, Ray S, Wang R, Liang Z, Cavallo JA, et al. Transfer and priming of surgical skills across minimally invasive surgical platforms. J Surg Res. 2016;206(1):48–52. doi: 10.1016/j.jss.2016.06.026. [DOI] [PubMed] [Google Scholar]
- 43.Azadi S, Green IC, Arnold A, Truong M, Potts J, Martino MA. Robotic surgery: the impact of simulation and other innovative platforms on performance and training. J Minim Invasive Gynecol. 2021;28(3):490–495. doi: 10.1016/j.jmig.2020.12.001. [DOI] [PubMed] [Google Scholar]
- 44.Schmidt MW, Köppinger KF, Fan C, Kowalewski KF, Schmidt LP, Vey J, Proctor T, Probst P, Bintintan VV, Müller-Stich BP, Nickel F. Virtual reality simulation in robot-assisted surgery: meta-analysis of skill transfer and predictability of skill. BJS Open. 2021;5(2):zraa066. doi: 10.1093/bjsopen/zraa066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lyons C, Goldfarb D, Jones SL, Badhiwala N, Miles B, Link R, et al. Which skills really matter? Proving face, content, and construct validity for a commercial robotic simulator. Surg Endosc. 2013;27(6):2020–2030. doi: 10.1007/s00464-012-2704-7. [DOI] [PubMed] [Google Scholar]
- 46.Hagen ME, Meehan JJ, Inan I, Morel P. Visual clues act as a substitute for haptic feedback in robotic surgery. Surg Endosc. 2008;22(6):1505–1508. doi: 10.1007/s00464-007-9683-0. [DOI] [PubMed] [Google Scholar]
- 47.Hernandez JD, Bann SD, Munz Y, Moorthy K, Datta V, Martin S, et al. Qualitative and quantitative analysis of the learning curve of a simulated surgical task on the da Vinci system. Surg Endosc. 2004;18(3):372–378. doi: 10.1007/s00464-003-9047-3. [DOI] [PubMed] [Google Scholar]
- 48.Hvolbek AP, Nilsson PM, Sanguedolce F, Lund L. A prospective study of the effect of video games on robotic surgery skills using the high-fidelity virtual reality RobotiX simulator. Adv Med Educ Pract. 2019;10:627–634. doi: 10.2147/AMEP.S199323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sridhar AN, Briggs TP, Kelly JD, Nathan S. Training in robotic surgery-an overview. Curr Urol Rep. 2017;18(8):58. doi: 10.1007/s11934-017-0710-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Khanna A, Campbell SC, Murthy PB, Ericson KJ, Nyame YA, Abouassaly R. Unplanned conversion from minimally invasive to open kidney surgery: the impact of robotics. J Endourol. 2020;34(9):955–963. doi: 10.1089/end.2020.0357. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.