Abstract
Objective
Ankle arthrodesis (AA) is often fixed using cannulated screws. The irritation from metalwork is a relatively common complication, but there is no consensus regarding the need to remove the screws on a systematic basis. The aim of this study was to determine (1) the proportion of screws removed after AA and (2) whether predictors of screw removal could be identified.
Methods
This PRISMA-compliant systematic review was part of a larger previous protocol registered on the PROSPERO platform. Multiple databases were searched including studies in which patients undergone AA using screws as exclusive fixation method were followed. Data were harvested regarding the cohort, the study design, the surgical technique, the nonunion and complication rate at the longest follow-up. Risk of bias was assessed using the modified Coleman Methodology Score (mCMS).
Results
Forty-four series of patients from thirty-eight studies (1990 ankles, 1934 patients) were selected. The average follow-up was 40.8 months (range 12–110). In all studies, hardware was removed due to symptoms reported by patients and related to the screws. The pooled proportion of removal of metalwork was 3% (95% CI 2–4). The pooled proportion of fusion was 96% (95%CI 95–98), while the pooled proportion of complications and reoperations (excluding the removal of metalwork) stood at 15% (95% CI 11–18) and 3% (95% CI 2–4), respectively. The mean mCMS (50.8 ± 8.1, range 35–66) revealed only an overall fair quality of studies. The univariate analysis and the multivariate model showed that the year of publication (R = − 0.004; p = 0.01) and the number of screws (R = 0.08; p = 0.01) were associated with the screw removal rate. Specifically, we found that over time the removal rate decreased by 0.4% per year and that the use of three screws instead of two reduced the risk of removal of metalwork by 8%.
Conclusions
In this review, removal of metalwork after ankle arthrodesis using cannulated screws was needed in 3% of cases at an average follow-up of 40.8 months. It was indicated only in case of symptoms related to soft tissue irritation from screws. The use of three screws was paradoxically related to a reduced risk of removal of screws as compared to two-screw constructs.
Level of evidence
Level IV, systematic review of Level IV.
Keywords: Ankle, Arthrodesis, Fusion, Screws, Fibular graft, Union
Introduction
Ankle Arthrodesis (AA) is a reliable option to treat end-stage ankle osteoarthritis resistant to conservative approaches [1–6]. To date, ankle replacement is gaining space in the foot and ankle field with new implants showing improved survival rates as compared to a few years ago, nevertheless AA remains the main choice in patients with history of ankle infection, significant tibiotalar deformity, poor bone quality or other contraindication to joint replacement [1–3]. Multiple fixation methods are available to stabilize the tibiotalar joint (screws, plates, external fixators or a combination of them) [2, 7–11] with no evidence of superiority of a method over one other. Among these methods, cannulated screws can be used in different number (two, three or less frequently more) and configuration (parallel or crossed) [12–15]. Furthermore, the use of a lateral fibular graft may offer additional biological and mechanical support to the arthrodesis [13], being therefore advocated by some authors.
Once the fusion has been achieved, the metalwork may be either removed or left in place. On a side, the systematic removal of screws may help reduce the risk of soft-tissue irritation at the price of risking further complications due to a second operation (e.g., infection, intraoperative fracture, nerve injury, etc.). On the other side, it may be suggested that the screws should be left in place and removed only in case of pain or discomfort reported by the patient. To date, there is no consensus in this field, therefore surgeons will generally make decisions based on their personal experience rather than on clear evidence.
In this study, we aimed to review the current literature to determine (1) the weighted proportion of screws removed after AA and (2) whether predictors of screw removal could be identified. Based on common experience, we hypothesized that the risk of removal of screws would be low and that a greater number of screws would lead to a higher risk of metalwork irritation.
Methods
Protocol and registration
This systematic review followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement and was part of a larger protocol prospectively registered in the PROSPERO database (CRD42022322784).
Eligibility criteria
The inclusion criteria were as follows: studies reporting data after AA (open or arthroscopically assisted) stabilized using only screws in patients aged between 18 and 85 years; clear description of the surgical technique with one or more statements about the number of screws used; studies including a sample size larger than 10 ankles; assessment of radiographic results through pre- and postoperative weightbearing standardized radiographs; reporting complications and reoperations after AA; minimum follow-up of 12 months; randomized, quasi-randomized, prospective and retrospective cohort studies, case series, technical notes; published in English; full text availability either online either after direct contact with the authors.
Exclusion criteria were the following: studies reporting results after AA stabilized using other methods (nail, external fixator, plate, hybrid constructs); data on skeletally immature patients; case reports, biomechanical studies, cadaveric studies, expert opinions, letters to the editor, studies on animals and instructional courses. Narrative or systematic reviews were also excluded from this study, but references were double checked to identify potential eligible studies.
Information sources and search
Pubmed, Embase, Cochrane Library and Scopus databases were searched from the earliest entries through November 20, 2022 with the following key words and Boolean operators: ((ankle) AND (arthrodes*)) OR ((ankle) AND (fusion)). Additional studies were identified in the bibliographies of articles. Two reviewers (AI and SS) independently screened the results of the research, then the full text of eligible studies was analyzed. Disputes were resolved by the senior author (AB). Unpublished studies and gray literature were not considered.
Data charting and items
Data were charted independently by two investigators (AI and AS) using an Excel sheet. Data were harvested regarding the cohort, the study design, the surgical technique and the outcome after the procedure. The primary outcome of this study was the need of removal of screws at the longest follow-up. The fusion rate, the complication rate and the need of reoperation (excluding the removal of metalwork) were the secondary outcomes.
Risk of bias
The modified Coleman Methodology Score (mCMS) was used to assess the quality of studies included, as in previous foot and ankle literature [16, 17], ranging from 0 to 100. Two investigators performed the mCMS assessment twice (AI and AC), with an interval of 10 days, then discussed the scores when more than a two-point difference was present, until consensus was reached. A score higher than 85 was considered excellent, good from 70 to 84, moderate from 50 to 69 and poor when less than 50 [16, 17].
Synthesis of results
Baseline data were reported as average value, standard deviation (SD) or 95% confidence interval (95% CI) and range values (minimum and maximum). A proportional meta-analysis was run to pool data regarding the rate of screw removal, fusion, nonunion, complication and reoperation. The ‘metaprop’ command was used to compute 95% CI using the score statistic and the exact binomial method and incorporate the Freeman-Tukey double arcsine transformation of proportions. Heterogeneity among studies was assessed through the Higgins’ I2 statistic and a random-effect model was applied in all cases.
Univariate linear regression was run to test demographics (sample size, sex, age), characteristics of the study (year of publication, mCMS, Level of Evidence (LoE) and length of follow-up) and type of surgery (arthroscopic or open procedure, number of screws used, configuration of screws, use of graft) against the need of screw removal. The association between variables (considering a continuous dependent variable) was tested through Pearson’s coefficient correlation (for continuous independent variables) and Wilcoxon rank-sum test (for categorical independent variables). For categorical independent variables where more than two categories were expected a Kruskal–Wallis test was used. A multivariate model was then used including all those variables significantly associated to the removal rate at the univariate analysis. Dummy variables were generated to handle categorical variables in the regression analysis. Parameters with P values < 0.05 were considered statistically significant in the final model. All analyses were performed using STATA statistical software package (Version 16.0, StataCorp, 2019).
Results
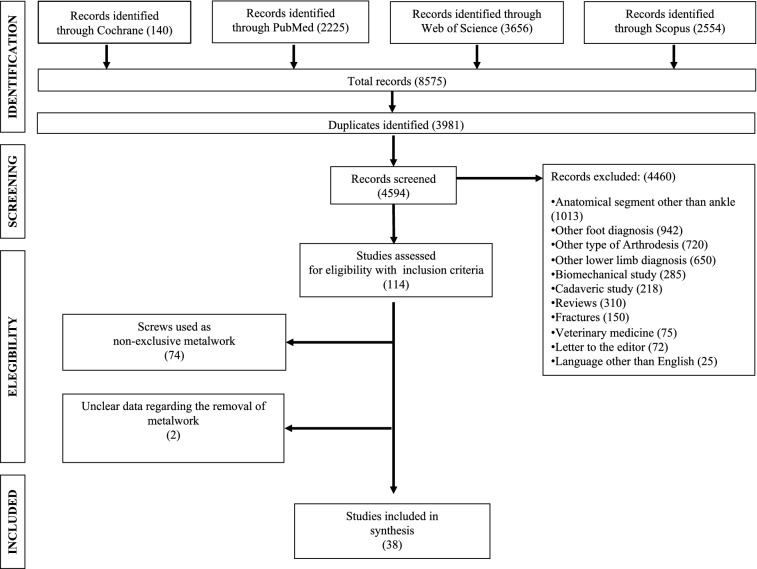
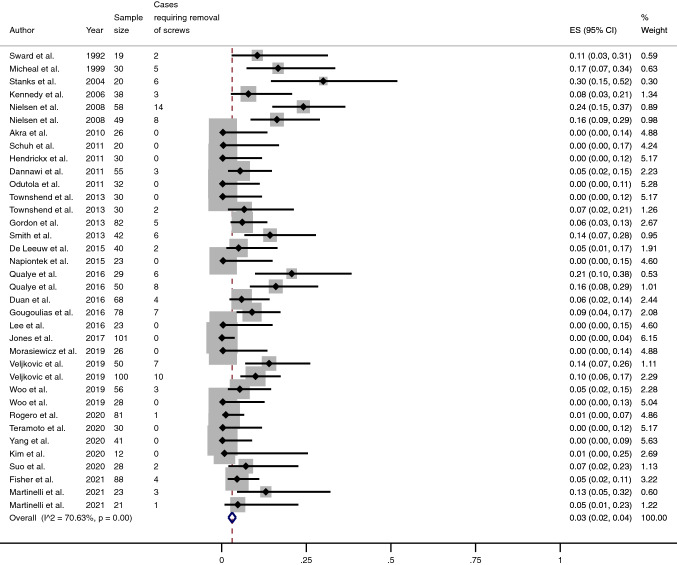
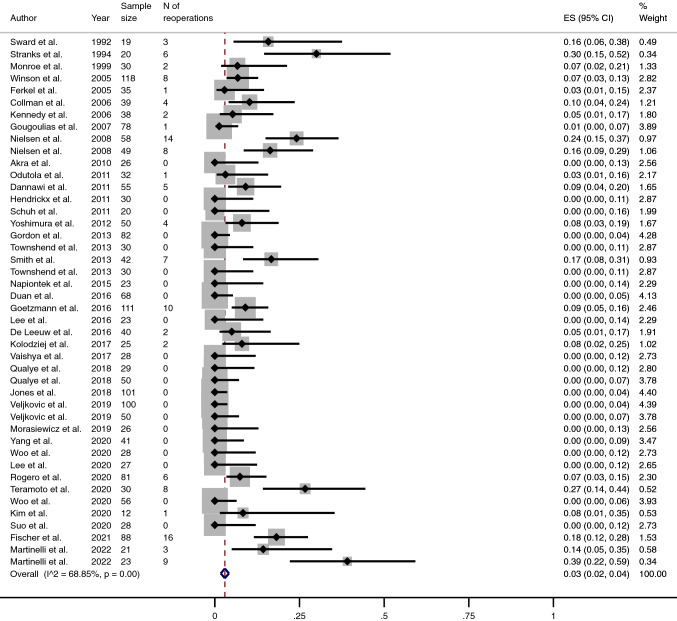
Forty-four series of patients from thirty-eight studies (1990 ankles, 1934 patients) were selected (Tables 1 and 2) (Fig. 1) [1, 3, 5, 12, 15, 18–50]. The average follow-up was 40.8 months (range 12–110). In all studies, hardware was removed due to symptoms reported by patients and related to the screws. The non-weighted screw removal rate was 7% (range 0–30), but the pooled proportion of removal of metalwork was 3% (95% CI 2–4) (Fig. 2).
Table 1.
Main characteristics of studies included in this review
| Characteristics of studies included |
Mean (SD) | Range (min – max) |
|---|---|---|
| Sample size (ankles), N | 45.2 (26.7) | 12–118 |
| Sample size (patients), N | 43.9 (26.2) | 12–116 |
| Age, y | 56.4 (5.8) | 43 -70 |
| Sex, % female | 42.7 (14) | 17–67 |
| mCMS | 50.8 (8) | 35–66 |
mCMS modified Coleman Methodology Score
Table 2.
Surgical details from studies included in this review
| Surgical details | (%) |
|---|---|
| Arthroscopic procedure |
Y: 47 N: 53 |
| Graft |
Y: 16 N: 84 |
| Number of screws |
< 3: 79 3: 21 |
| Orientation |
Crossed: 43 Parallel: 32 Variable: 25 |
Fig. 1.
Flow chart for studies included in this systematic review
Fig. 2.
Meta-analysis of the proportion of removal of screws in patients undergone Ankle Arthrodesis fixed using cannulated screws. Output generated by the Stata procedure metaprop
Predictors of outcome
The univariate analysis suggested that the rate of removal of screws was associated with the year of publication of the study (R = − 0.48; p = < 0.001) and with the number of screws used for the arthrodesis (p = 0.004). The multivariate model confirmed that both these variables were significantly associated with the need of screw removal (R = − 0.004; p = 0.01 for the year of publication and R = 0.08; p = 0.01 for the number of screws). Specifically, we found that over time the removal rate decreased by 0.4% per every year passed by (Fig. 3) and that the use of three screws instead of two reduced the risk of removal of metalwork by 8%.
Fig. 3.
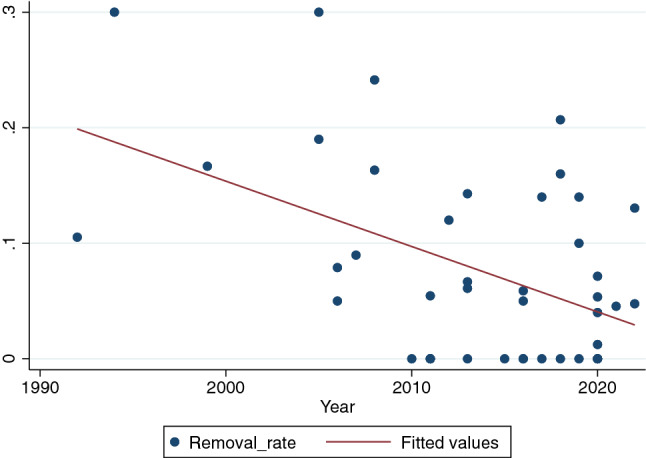
Scatter diagram illustrating the negative correlation between the year of publication of studies included in this review (x axis) and the rate of screw removal reported in each study (y axis, where 0.01 corresponds to 1%) (R = − 0.48; p = < 0.001)
Secondary outcomes
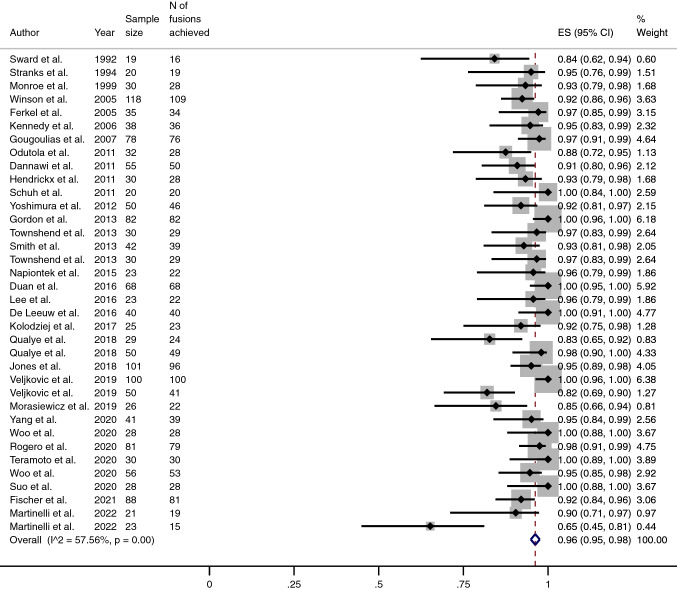
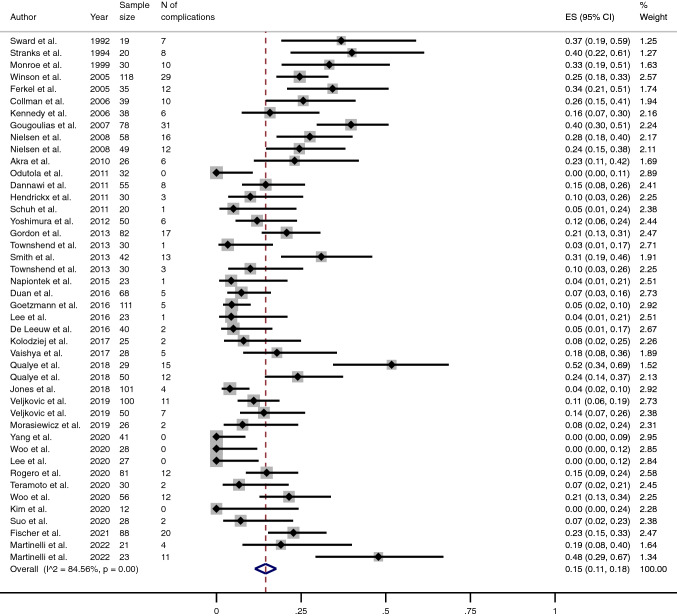
The pooled proportion of fusion was 96% (95% CI 95–98) (Fig. 4), while the pooled proportion of complications and reoperations (excluding the removal of metalwork) stood at 15% (95% CI 11–18) and 3% (95% CI 2–4) (Table 3) (Figs. 5 and 6), respectively. The mean mCMS (50.8 ± 8.1, range 35–66) revealed only an overall fair quality of studies.
Fig. 4.
Meta-analysis of the proportion of fusions achieved in patients undergone Ankle Arthrodesis fixed using cannulated screws. Output generated by the Stata procedure metaprop
Table 3.
Main outcomes from studies included in this review, reported both as non-weighted and pooled proportion
| Outcome | Non-weighted proportion | Pooled proportion (%) | ||
|---|---|---|---|---|
| Mean | 95% CI | Mean | 95% CI | |
| Removal rate | 7.6 | 5–10 | 5 | 4–7 |
| Non Union rate | 7.1 | 4.9–9.3 | 4 | 3–5 |
| Fusion Rate | 92.8 | 90.6–95 | 96 | 95–98 |
| Complication rate | 16.9 | 12.6–21.1 | 15 | 11–18 |
| Reoperation rate | 8.1 | 5.1–11 | 3 | 2–4 |
Fig. 5.
Meta-analysis of the proportion of complications in patients undergone Ankle Arthrodesis fixed using cannulated screws. Output generated by the Stata procedure metaprop
Fig. 6.
Meta-analysis of the proportion of reoperations (excluding removal of metalwork) in patients undergone Ankle Arthrodesis fixed using cannulated screws. Output generated by the Stata procedure metaprop
Discussion
The main finding of this study was that on a cohort of almost 2000 osteoarthritic ankles undergone ankle arthrodesis stabilized using cannulated screws the removal of metalwork was always performed because of soft tissue irritation related to the screws and was finally required in 3% of cases. Excluding the removal of metalwork, the pooled rate of complications was 15% but a second surgery was necessary only in 3% of cases at a 40-month mean follow-up.
Regarding predictors of removal of metalwork, both the univariate and multivariate analysis suggested a negative correlation between the year of publication and the removal of screws, with a reduction in terms of removal rate by 4% every 10 years. This would possibly reflect a reduced risk of irritation from metalwork with the advancement of technology in materials, screw designs and surgical techniques. One could argue that the use of headless screws might play a key role in this scenario, however we’d like to emphasize that out of thirty-eight studies included in this review only two papers by Odutola et al. [30] and Kolodziej et al. [40] reported the use of headless screws [30]. In their papers, the authors have demonstrated that this type of metalwork may reduce the risk of removal at 0% but with a nonunion rate standing at 8–12% which is considered high if compared with other series. Interestingly, the authors have reported a cost of 1285 pounds sterling per every case of metalwork removal in the United Kingdom, which the physician should take into account when discussing this type of procedures.
On a pathophysiological basis, we would have expected to find a correlation between a greater number of screws and a greater risk of removal of metalwork due to the increased total space occupied by the screw heads. We were surprised to see that in this review using three screws instead of two might be a protective element against the risk of removal of metalwork. In our opinion, this could be theoretically due to two reasons: first, the use of two screws may potentially lead to a more frequent use of washers which often do not seat completely on the cortical bone and may possibly lead to irritate surrounding soft tissues; second, the use of a third screw could incentivize the surgeon to place more carefully (and maybe in a more appropriate position) the first two since some room has to be left for the third one. To the best of our knowledge, no other study has analyzed this aspect so far, therefore, a comparison with previous literature was not possible. We advocate that a robust approach taking into accounts potential confounders should be mandatory in future studies to draw conclusions on risk factors for a second surgery after AA.
In our opinion, the final pooled removal rate at 3% represented an average value between a group of studies with greater figures and the fifteen cohorts in which a 0% removal rate was reported [1, 26–28, 30, 31, 35, 37, 39, 40, 42, 43, 45, 47, 48]. Such a low rate probably explains why most surgeons feel that removal of metalwork should not be advised as a routinary procedure. Of note, the pooled proportion of patients requiring removal of metalwork was much lower than the simple non-weighted mathematical average of different studies (7%), which suggests that larger studies tend to report a reduced need to remove the metalwork. On the balance, the relationship between a low risk of irritation from metalwork and all the risks inherently related to surgery leads most surgeons to remove screws only in symptomatic patients. The mean follow-up at 40 months was probably appropriate since in our experience the irritation produced by metalwork generally presents quite early during the first months or years after surgery (except in case of delayed breakage of screws).
Finally, it should be highlighted that, in the majority of studies here included, the conventional follow-up of fused ankles was carried out using standard radiographic imaging, while computed tomography was requested only in selected cases. Due to inherent biases related to radiographs (superimposition of bones, rotation of the source or of the foot, experience of the operator, etc.) [51–56] it would be difficult to extract accurate data about the position of the screw head, the orientation of screws and their entry point as variables potentially related to the risk of soft tissue irritation. In patients complaining of postoperative pain potentially related to metalware irritation the use of recently introduced cone beam weight bearing computed tomography [51–56] could help obtain such information along with data on the fusion of the arthrodesis site and the alignment of the ankle, both important for a correct assessment of the patient during his follow-up.
This study is not without limitations. First, although we included only studies performing ankle arthrodesis using cannulated screws, we acknowledge that the surgical technique adopted by different authors was heterogeneous (in terms of number of screws, metalwork positioning, use of arthroscopy and grafting etc.) which may weaken the strength of our findings. Also, the average quality of studies was only fair as demonstrated by the mCMS and all of them had a retrospective design with a Level of Evidence at III of IV. Third, the removal of metalwork was never considered a primary outcome in the studies selected, which may be considered a potential source of bias.
Conclusion
In this review, removal of metalwork after ankle arthrodesis using cannulated screws was needed in 3% of cases and was indicated only in case of symptoms related to irritation from metalwork. The pooled fusion rate after ankle arthrodesis using cannulated screws stood at 96%. These data could be useful in clinical practice to counsel patients correctly in the pre-operative setting. We also demonstrated that the need of removal of metalwork is progressively reducing as the time passes by and that using three screws instead of two to fix the tibiotalar fusion site might lead to a reduced risk of metalwork removal. Further studies are needed to confirm or disprove the findings of this review.
Author contributions
AI: Selection of studies, interpretation of results, writing of the manuscript, revision of the manuscript. AS: Study design, interpretation of results, writing of the manuscript, revision of the manuscript. SS: Study design, interpretation of results, writing of the manuscript, revision of the manuscript. AC: Study design, interpretation of results, writing of the manuscript, revision of the manuscript. AC: Study design, interpretation of results, writing of the manuscript, revision of the manuscript. MM: Study design, interpretation of results, writing of the manuscript, revision of the manuscript. AB: Study design, selection of studies, statistical analysis, interpretation of results, writing of the manuscript, revision of the manuscript.
Funding
Open access funding provided by Università degli Studi di Napoli Federico II within the CRUI-CARE Agreement. No funding has been provided for the current work.
Data availability
Data of this study can be made available upon request.
Declarations
Conflict of interest
Authors declare no conflict of interest directly or indirectly related to this work.
Ethics approval
The Institutional Research Ethics Committee has confirmed that no ethical approval was required for this systematic review and meta-analysis.
Consent to participate and to publish
Not needed for this systematic review and meta-analysis.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Antonio Izzo, Email: izzoantonio1992@gmail.com.
Arianna Sgadari, Email: arianna.sgadari@gmail.com.
Salvatore Santagata, Email: doc.santagatasalvatore92@gmail.com.
Antonio Coviello, Email: antonio_coviello@live.it.
Andrea Cozzolino, Email: andrea.cozzolino@hotmail.it.
Massimo Mariconda, Email: maricond@unina.it.
Alessio Bernasconi, Email: alessio.bernasconi@unina.it.
References
- 1.Yang TC, Tzeng YH, Wang CS, et al. Arthroscopic ankle arthrodesis provides similarly satisfactory surgical outcomes in ankles with severe deformity compared with mild deformity in elderly patients. Arthroscopy. 2020;36:2738–2747. doi: 10.1016/J.ARTHRO.2020.05.036. [DOI] [PubMed] [Google Scholar]
- 2.Mehdi N, Bernasconi A, Laborde J, Lintz F. Comparison of 25 ankle arthrodeses and 25 replacements at 67 months’ follow-up. Orthop Traumatol Surg Res. 2019;105:139–144. doi: 10.1016/j.otsr.2018.10.014. [DOI] [PubMed] [Google Scholar]
- 3.Quayle J, Shafafy R, Khan MA, et al. Arthroscopic versus open ankle arthrodesis. Foot Ankle Surg. 2018;24:137–142. doi: 10.1016/J.FAS.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 4.Pfahler M, Krödel A, Tritschler A, Zenta S. Role of internal and external fixation in ankle fusion. Arch Orthop Trauma Surg. 1996;115:146–148. doi: 10.1007/BF00434542. [DOI] [PubMed] [Google Scholar]
- 5.Fischer S, Klug A, Faul P, et al. Superiority of upper ankle arthrodesis over total ankle replacement in the treatment of end-stage posttraumatic ankle arthrosis. Arch Orthop Trauma Surg. 2022;142:435–442. doi: 10.1007/S00402-020-03714-X. [DOI] [PubMed] [Google Scholar]
- 6.Suda AJ, Richter A, Abou-Nouar G, et al. Arthrodesis for septic arthritis of the ankle: risk factors and complications. Arch Orthop Trauma Surg. 2016;136:1343–1348. doi: 10.1007/S00402-016-2520-Y. [DOI] [PubMed] [Google Scholar]
- 7.Ogut T, Glisson RR, Chuckpaiwong B, et al. External ring fixation versus screw fixation for ankle arthrodesis: a biomechanical comparison. Foot Ankle Int. 2009;30:353–360. doi: 10.3113/FAI.2009.0353. [DOI] [PubMed] [Google Scholar]
- 8.Betz MM, Benninger EE, Favre PP, et al. Primary stability and stiffness in ankle arthrodes-crossed screws versus anterior plating. Foot Ankle Surg. 2013;19:168–172. doi: 10.1016/J.FAS.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 9.Clifford C, Berg S, McCann K, Hutchinson B. A biomechanical comparison of internal fixation techniques for ankle arthrodesis. J Foot Ankle Surg. 2015;54:188–191. doi: 10.1053/J.JFAS.2014.06.002. [DOI] [PubMed] [Google Scholar]
- 10.van den Heuvel SBM, Penning D, Schepers T. Open ankle arthrodesis: a retrospective analysis comparing different fixation methods. J Foot Ankle Surg. 2022;61:233–238. doi: 10.1053/J.JFAS.2021.07.012. [DOI] [PubMed] [Google Scholar]
- 11.van den Heuvel SBM, Doorgakant A, Birnie MFN, et al. Open ankle arthrodesis: a systematic review of approaches and fixation methods. Foot Ankle Surg. 2021;27:339–347. doi: 10.1016/J.FAS.2020.12.011. [DOI] [PubMed] [Google Scholar]
- 12.Rogero RG, Fuchs DJ, Corr D, et al. ankle arthrodesis through a fibular-sparing anterior approach. Foot Ankle Int. 2020;41:1480–1486. doi: 10.1177/1071100720946740. [DOI] [PubMed] [Google Scholar]
- 13.Heifner JJ, Monir JG, Reb CW. Impact of bone graft on fusion rates in primary open ankle arthrodesis fixated with cannulated screws: a systematic review. J Foot Ankle Surg. 2021;60:802–806. doi: 10.1053/J.JFAS.2021.02.006. [DOI] [PubMed] [Google Scholar]
- 14.Valiyev N, Demirel M, Hürmeydan ÖM, et al. The effects of different screw combinations on the initial stability of ankle arthrodesis. J Am Podiatr Med Assoc. 2021 doi: 10.7547/20-241. [DOI] [PubMed] [Google Scholar]
- 15.Yoshimura I, Kanazawa K, Takeyama A, et al. The effect of screw position and number on the time to union of arthroscopic ankle arthrodesis. Arthroscopy J Arthrosc Relat Surg. 2012;28:1882–1888. doi: 10.1016/j.arthro.2012.06.019. [DOI] [PubMed] [Google Scholar]
- 16.Bernasconi A, Sadile F, Smeraglia F, et al. Tendoscopy of Achilles, peroneal and tibialis posterior tendons: An evidence-based update. Foot Ankle Surg. 2018;24:374–382. doi: 10.1016/j.fas.2017.06.004. [DOI] [PubMed] [Google Scholar]
- 17.Izzo A, Vallefuoco S, Basso MA, et al. Role of lateral soft tissue release in percutaneous hallux valgus surgery: a systematic review and meta-analysis of the literature. Arch Orthop Trauma Surg. 2022 doi: 10.1007/S00402-022-04693-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sward L, Hughes JS, Howell CJ, Colton CL. Posterior internal compression arthrodesis of the ankle. J Bone Jt Surg Br. 1992;74:752–756. doi: 10.1302/0301-620X.74B5.1527128. [DOI] [PubMed] [Google Scholar]
- 19.Stranks G, Cecil T, Jeffery I. Anterior ankle arthrodesis with cross-screw fixation. A dowel graft method used in 20 cases. J Bone Jt Surg Br. 1994;76:943–946. doi: 10.1302/0301-620X.76B6.7983124. [DOI] [PubMed] [Google Scholar]
- 20.Monroe MT, Beals TC, Manoli A. Clinical outcome of arthrodesis of the ankle using rigid internal fixation with cancellous screws. Foot Ankle Int. 1999;20:227–231. doi: 10.1177/107110079902000404. [DOI] [PubMed] [Google Scholar]
- 21.Ferkel RD, Hewitt M. Long-term results of arthroscopic ankle arthrodesis. Foot Ankle Int. 2005;26:275–280. doi: 10.1177/107110070502600402. [DOI] [PubMed] [Google Scholar]
- 22.Winson IG, Robinson DE, Allen PE. Arthroscopic ankle arthrodesis. J Bone Jt Surg Br. 2005;87:343–347. doi: 10.1302/0301-620X.87B3.15756. [DOI] [PubMed] [Google Scholar]
- 23.Collman DR, Kaas MH, Schuberth JM. Arthroscopic ankle arthrodesis: factors influencing union in 39 consecutive patients. Foot Ankle Int. 2006;27:1079–1085. doi: 10.1177/107110070602701214. [DOI] [PubMed] [Google Scholar]
- 24.Kennedy JG, Hodgkins CW, Brodsky A, Bohne WH. Outcomes after standardized screw fixation technique of ankle arthrodesis. Clin Orthop Relat Res. 2006;447:112–118. doi: 10.1097/01.BLO.0000203480.04174.0E. [DOI] [PubMed] [Google Scholar]
- 25.Nielsen KK, Linde F, Jensen NC. The outcome of arthroscopic and open surgery ankle arthrodesis: a comparative retrospective study on 107 patients. Foot Ankle Surg. 2008;14:153–157. doi: 10.1016/J.FAS.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 26.Akra GA, Middleton A, Adedapo AO, et al. Outcome of ankle arthrodesis using a transfibular approach. J Foot Ankle Surg. 2010;49:508–512. doi: 10.1053/J.JFAS.2010.07.004. [DOI] [PubMed] [Google Scholar]
- 27.Schuh R, Hofstaetter J, Krismer M, et al. Total ankle arthroplasty versus ankle arthrodesis. Comparison of sports, recreational activities and functional outcome. Int Orthop. 2012;36:1207–1214. doi: 10.1007/S00264-011-1455-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hendrickx RPM, Kerkhoffs GMMJ, Stufkens SAS, et al. Ankle fusion using a 2-incision, 3-screw technique. Oper Orthop Traumatol. 2011;23:131–140. doi: 10.1007/S00064-011-0015-0. [DOI] [PubMed] [Google Scholar]
- 29.Dannawi Z, Nawabi DH, Patel A, et al. Arthroscopic ankle arthrodesis: are results reproducible irrespective of pre-operative deformity? Foot Ankle Surg. 2011;17:294–299. doi: 10.1016/J.FAS.2010.12.004. [DOI] [PubMed] [Google Scholar]
- 30.Odutola AA, Sheridan BD, Kelly AJ. Headless compression screw fixation prevents symptomatic metalwork in arthroscopic ankle arthrodesis. Foot Ankle Surg. 2012;18:111–113. doi: 10.1016/J.FAS.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 31.Townshend D, di Silvestro M, Krause F, et al. Arthroscopic versus open ankle arthrodesis: a multicenter comparative case series. J Bone Jt Surg Am. 2013;95:98–102. doi: 10.2106/JBJS.K.01240. [DOI] [PubMed] [Google Scholar]
- 32.Gordon D, Zicker R, Cullen N, Singh D. Open ankle arthrodeses via an anterior approach. Foot Ankle Int. 2013;34:386–391. doi: 10.1177/1071100713477385. [DOI] [PubMed] [Google Scholar]
- 33.Smith JT, Chiodo CP, Singh SK, Wilson MG. Open ankle arthrodesis with a fibular-sparing technique. Foot Ankle Int. 2013;34:557–562. doi: 10.1177/1071100713477617. [DOI] [PubMed] [Google Scholar]
- 34.de Leeuw PAJ, Hendrickx RPM, van Dijk CN, et al. Midterm results of posterior arthroscopic ankle fusion. Knee Surg Sports Traumatol Arthrosc. 2016;24:1326–1331. doi: 10.1007/S00167-015-3975-Z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Napiontek M, Jaszczak T. Ankle arthrodesis from lateral transfibular approach: analysis of treatment results of 23 feet treated by the modified Mann’s technique. Eur J Orthop Surg Traumatol. 2015;25:1195–1199. doi: 10.1007/S00590-015-1663-9. [DOI] [PubMed] [Google Scholar]
- 36.Duan X, Yang L, Yin L. Arthroscopic arthrodesis for ankle arthritis without bone graft. J Orthop Surg Res. 2016 doi: 10.1186/S13018-016-0490-Y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Goetzmann T, Molé D, Jullion S, et al. Influence of fixation with two vs. three screws on union of arthroscopic tibio-talar arthrodesis: comparative radiographic study of 111 cases. Orthop Traumatol Surg Res. 2016;102:651–656. doi: 10.1016/J.OTSR.2016.03.015. [DOI] [PubMed] [Google Scholar]
- 38.Gougoulias NE, Agathangelidis FG, Parsons SW. Arthroscopic ankle arthrodesis. Foot Ankle Int. 2007;28:695–706. doi: 10.3113/FAI.2007.0695. [DOI] [PubMed] [Google Scholar]
- 39.Lee HJ, Min WK, Kim JS, et al. Transfibular ankle arthrodesis using burring, curettage, multiple drilling, and fixation with two retrograde screws through a single lateral incision. J Orthop Surg (Hong Kong) 2016;24:101–105. doi: 10.1177/230949901602400123. [DOI] [PubMed] [Google Scholar]
- 40.Kolodziej L, Sadlik B, Sokolowski S, Bohatyrewicz A. Results of arthroscopic ankle arthrodesis with fixation using two parallel headless compression screws in a heterogenic group of patients. Open Orthop J. 2017;11:37–44. doi: 10.2174/1874325001711010037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vaishya R, Azizi AT, Agarwal AK, Vijay V. Arthroscopic assisted ankle arthrodesis: a retrospective study of 32 cases. J Clin Orthop Trauma. 2017;8:54–58. doi: 10.1016/J.JCOT.2016.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jones CR, Wong E, Applegate GR, Ferkel RD. Arthroscopic ankle arthrodesis: a 2–15 year follow-up study. Arthroscopy. 2018;34:1641–1649. doi: 10.1016/J.ARTHRO.2017.11.031. [DOI] [PubMed] [Google Scholar]
- 43.Morasiewicz P, Dejnek M, Orzechowski W, et al. Clinical evaluation of ankle arthrodesis with Ilizarov fixation and internal fixation. BMC Musculoskelet Disord. 2019 doi: 10.1186/S12891-019-2524-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Veljkovic AN, Daniels TR, Glazebrook MA, et al. Outcomes of total ankle replacement, arthroscopic ankle arthrodesis, and open ankle arthrodesis for isolated non-deformed end-stage ankle arthritis. J Bone Jt Surg Am. 2019;101:1523–1529. doi: 10.2106/JBJS.18.01012. [DOI] [PubMed] [Google Scholar]
- 45.Woo BJ, Lai MC, Ng S, et al. Clinical outcomes comparing arthroscopic vs open ankle arthrodesis. Foot Ankle Surg. 2020;26:530–534. doi: 10.1016/J.FAS.2019.06.004. [DOI] [PubMed] [Google Scholar]
- 46.Lee DY, Kyung MG, Cho YJ, et al. A modified transfibular technique of ankle arthrodesis using partial fibular resection and onlay bone graft. PLoS ONE. 2020 doi: 10.1371/JOURNAL.PONE.0241141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Teramoto A, Nozaka K, Kamiya T, et al. Screw internal fixation and ilizarov external fixation: a comparison of outcomes in ankle arthrodesis. J Foot Ankle Surg. 2020;59:343–346. doi: 10.1053/J.JFAS.2019.09.012. [DOI] [PubMed] [Google Scholar]
- 48.Kim JB, Lee BJ, Jung D, et al. Comparing outcomes of the ankle arthrodesis by using two different materials via a transfibular approach. Acta Ortop Bras. 2020;28:55–59. doi: 10.1590/1413-785220202802223986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Suo H, Fu L, Liang H, et al. End-stage ankle arthritis treated by ankle arthrodesis with screw fixation through the transfibular approach: a retrospective analysis. Orthop Surg. 2020;12:1108–1119. doi: 10.1111/OS.12707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Martinelli N, Bianchi A, Raggi G, et al. Open versus arthroscopic ankle arthrodesis in high-risk patients: a comparative study. Int Orthop. 2022;46:515–521. doi: 10.1007/S00264-021-05233-9. [DOI] [PubMed] [Google Scholar]
- 51.Richter M, Seidl B, Zech S, Hahn S. PedCAT for 3D-imaging in standing position allows for more accurate bone position (angle) measurement than radiographs or CT. Foot Ankle Surg. 2014;20:201–207. doi: 10.1016/J.FAS.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 52.Lintz F, de Netto C, C, Barg A, , et al. Weight-bearing cone beam CT scans in the foot and ankle. EFORT Open Rev. 2018;3:278–286. doi: 10.1302/2058-5241.3.170066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Richter M, de Cesar NC, Lintz F, et al. The Assessment of Ankle Osteoarthritis with Weight-Bearing Computed Tomography. Foot Ankle Clin. 2022;27:13–36. doi: 10.1016/J.FCL.2021.11.001. [DOI] [PubMed] [Google Scholar]
- 54.Burssens A, Peeters J, Buedts K, et al. Measuring hindfoot alignment in weight bearing CT: A novel clinical relevant measurement method. Foot Ankle Surg. 2016;22:233–238. doi: 10.1016/j.fas.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 55.Zhang JZ, Lintz F, Bernasconi A, Zhang S. 3D Biometrics for Hindfoot alignment using weightbearing computed tomography. Foot Ankle Int. 2019 doi: 10.1177/1071100719835492. [DOI] [PubMed] [Google Scholar]
- 56.Bernasconi A, de Cesar Netto C, Barg A, et al. AAFD: conventional radiographs are not Enough! i Need the third dimension. Tech Foot Ankle Surg. 2019 doi: 10.1097/BTF.0000000000000234. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data of this study can be made available upon request.