Abstract
Purpose
The purpose of this study is to systematically review multiligament knee injury (MLKI) outcome studies to determine definitions of arthrofibrosis (AF) and provide information about incidence, management as well as potential risk factors.
Methods
A systematic literature search was performed (PubMed and Cochrane library) following the PRISMA guidelines of operatively treated MLKI (Schenck II–IV) studies reporting the incidence of AF. Twenty-five studies met the inclusion criteria. Injury pattern, timing of surgery, surgical technique, treatment of AF, rehabilitation programs and PROMS were inquired. Risk of bias and quality of evidence were assessed using the Coleman methodological score.
Results
Twenty-five studies with a total of 709 patients with a mean age of 33.6 ± 4.8 years were included and followed 47.2 ± 32.0 months. The majority of studies (22/25) used imprecise and subjective definitions of AF. A total of 86 patients were treated for AF, resulting in an overall prevalence of 12.1% (range 2.8–57.1). Higher-grade injuries (Schenck III–IV), acute treatment and ROM (range of motion) limiting rehabilitation programs were potential risk factors for AF. The time from index surgery to manipulation anesthesia (MUA) and arthroscopic lysis of adhesions (LOA) averaged at 14.3 ± 8.8 and 27.7 ± 12.8 weeks. Prior to MUA and LOA, the ROM was 51.7° ± 23.5 and 80.2° ± 17.0, resulting in a total ROM gain after intervention of 65.0° ± 19.7 and 48.0° ± 10.6, respectively; with no reports of any complication within the follow-up. The overall methodological quality of the studies was poor as measured by the Coleman score with average 56.3 ± 12.5 (range 31–84) points.
Conclusions
AF is a common but poorly defined complication particularly in high-grade MLKI. Early postoperative and intensified physiotherapy is important to reduce the risk of AF. MUA and LOA are very effective treatment options and result in good clinical outcome. Prospective studies with bigger study population are needed to optimize treatment algorithms of further patients after MLKI.
The protocol of this systematic review has been prospectively registered with PROSPERO (CRD42021229187, January 4th, 2021).
Keywords: Knee, Multiligament knee injury, Knee dislocation, Arthrofibrosis, Stiffness, Systematic review
Introduction
Multiple-ligament injuries of the knee (MLKI) are rare (0.02–0.2% of all orthopedic injuries), but often devastating in nature as they are potentially limb-threatening, given the possibility of concomitant popliteal artery injuries with amputations being described in up to 25.0% [6, 9, 26, 45].
Historically, these injuries have been managed conservatively in the acute phase due to the reported high risk of arthrofibrosis (AF) [12, 23]. In the last decades, there has been a strong trend toward surgical management of such injuries, since recent studies provided evidence of worse functional outcomes, persisting instability and contracture in patients managed non-operatively [50, 67, 71]. However, there are many controversies with regard to type and timing of the surgical management [7, 60]. Strategies range from early to late surgery and repair to reconstruction and one- to two-stage procedures [7].
Commonly reported complications after MLKI surgery include wound infection, deep venous thrombosis and AF [23, 53], with MLKI having a much greater risk of complication compared to single ligament injuries [5, 9, 16, 71]. The overall complication rate ranges from 6.0% to 75.0% and is directly linked to number of injured ligaments [3, 9, 13, 86]. With rates up to 57.0%, AF is the most common complication and often requires interventional treatment [7, 43, 59, 64, 72, 76]. It has long been recognized but definitions widely vary and treatment guidelines are still lacking. Histopathologically, AF is caused by prolonged expression of inflammatory cytokines, migration of myofibroblasts, resulting in increased scar tissue and eventually leading to clinically apparent loss of motion of the knee [11, 82]. This extensive scar tissue is used in the concept of ligament bracing in a sense of “guided arthrofibrosis” for treating acute knee dislocations [25].
In addition to extensive injuries and complicated surgeries [59], several factors are assumed to increase the risk of stiffness such as injury of two or more ligaments, repair of medial sided structures and acute surgery within 3 weeks [9, 13, 41]. Protection of repaired or reconstructed structures, e.g., by means of bracing, restrictions of weight bearing and/or range of motion are still considered important to enable healing of these structures. Likewise, a good balance between protective measures and early enforced rehabilitation, assuming to potentially decrease the likelihood of AF, is of crucial importance [52]. Several protocols have already published recommendations, aiming to minimize the risk of AF such as staged, delayed surgery or the use of a hinged external fixator [2, 5, 49, 84]. However, to date, there is still no consensus on the best surgical procedure and rehabilitation program following MLKI surgery to avoid AF.
The purpose of this study is to systematically review MLKI outcome studies to determine definitions of AF and provide information about incidence, management and potential risk factors of this complication. We hypothesized that AF is inconsistently defined and more severely MLKI and acute surgery result in higher rates of AF. Furthermore, the treatment of AF is mainly operative and shows good results.
Materials and methods
Search criteria
A search for relevant studies that met prespecified inclusion criteria was conducted by two independent reviewers (H.F. and L.K.) on August 31st, 2021, through the two major electronic databases PubMed and Cochrane library.
The search strategy included the two following keyword searches:
"knee dislocation" OR "multiligament* knee injury*" OR "Tibiofemoral dislocation" OR "multiligament knee reconstruction" OR "multiligament-injured knee."
("anterior cruciate ligament" OR acl OR pcl OR "posterior cruciate ligament") AND ("stiffness" OR "range of motion deficits" OR "ROM deficits" OR "arthrofibrosis") AND ("reconstruction" OR "treatment" OR "surgery" OR "repair").
Both keyword searches were merged carefully afterward. Search terms, if possible, were mapped to relevant MeSH terms and subject headings. A supplementary search of the reference list of relevant articles was also conducted. The study was performed as a systematic review of the current literature following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) guidelines [58]. The protocol of this systematic review has been prospectively registered with PROSPERO (CRD42021229187, January 4th, 2021).
Study selection
In a first step, title and abstract of each study were evaluated to meet inclusion criteria (see Table 1).
Table 1.
Study Inclusion and Exclusion Criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
| Report of AF or stiffness following MLKI requiring interventional treatment like lysis of adhesions (LOA) or manipulation under anesthesia (MUA) | Articles that have investigated the outcome of conservatively treated injuries or studies older than 1990s |
| MLKI defined as the disruption of at least both cruciate ligaments (Schenck grade II–IV) | Reports on guidelines, technique articles, reviews or systematic reviews |
| Adult female and male patients | Complex fracture dislocation, such as tibial fracture and/or distal femur fracture requiring open reduction and internal fixation |
| Full texts available in English or German language |
Schenck I injuries are very common and differentiate from higher-grade injuries in terms of trauma mechanisms, treatment and outcome. On the other hand, Schenck V injuries are rare but often need complex internal fixation and are rather heterogeneous among themselves, since the description of fracture-dislocation injuries is often limited. As non-operative therapy is reserved for individual rare cases [15, 18, 22, 38, 67, 83] and data of MLKI are very inhomogeneous, this review focuses particularly on operatively treated knee dislocations with at least two torn cruciate ligaments without reported fracture dislocations.
Noticeably, studies including Schenck I or V injuries, where an individual analysis of Schenck II–IV injuries was possible, were also included. In cases where the review of the title and abstract did not clearly indicate whether a study was suitable for inclusion, the full-text article was analyzed. Two reviewers (H.F. and L.K.) independently evaluated the selected articles for meeting the inclusion criteria. The decision to include or exclude the study was made based on a group consensus. Any deviations from consensus were discussed and resolved as a group. Additionally, all references from the included studies were reviewed and reconciled to verify that no relevant articles were missing.
Data extraction
Two independent reviewers (H.F. and L.K.) performed data extraction in duplicates and used a form specifically designed for this review. The following data were extracted from each study: Number of participants included average age of participants, time of follow-up, injury pattern (Schenck Classification), surgical technique, timing of surgery, postoperative rehabilitation program and PROMS (Lysholm and IKDC Score). Furthermore, rate of AF, distribution and timing of LOA/MUA, range of motion (ROM) before and ROM gain after LOA/MUA were considered in the analysis.
Study quality assessment
The rating of evidence level based on Wright et al. [88] was used for this review. The quality of the studies was assessed using the Coleman methodological score [8], which was developed to assess the quality of primary studies in terms of risk of bias and applicability concerns. The total score can range from 0 to 100, and higher scores are indicative of absence of bias and confounding factors. The final score was categorized as excellent (85–100 points), good (70–84 points), fair (50–69 points) and poor (< 50 points) [56]. Each included study was assigned a score independently by the two reviewers (H.F. and L.K). Disagreements between the evaluators were resolved by consensus, with a third evaluator (M.K.) being called in, when consensus could not be reached.
Statistical analysis
Statistical analysis was performed using SPSS 15.0 software (SPSS Inc., Chicago, IL). Because of limitations in reporting (lack of availability AF/Stiffness) as well as heterogeneity between studies, a meta-analysis was not be performed. For descriptive purposes, the rate of AF (weighting based on the study sample size), averages for time to LOA/MUA, total ROM before and total ROM gain after LOA/MUA were calculated from the study summary data. The interrater reliabilities were obtained to assess the agreement among the two observers (H.F. and L.K.) for determining the Coleman score. Cohen’s kappa was evaluated between the average scores. A p value of less than 0.05 was considered significant.
Results
Literature selection
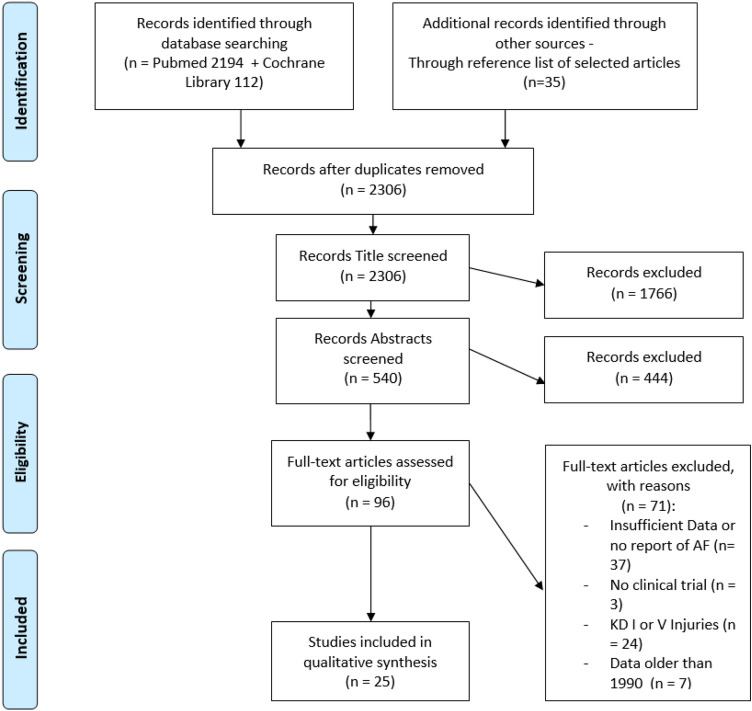
A total of 2341 articles were identified, after removal of duplicates (n = 35), 2,06 titles and abstracts were screened for eligibility (see Fig. 1). After exclusion of 2210 articles through screening, 96 remaining articles underwent a full-text analysis by the reviewers to evaluate matching of inclusion and exclusion criteria (see Table 1). Any discrepancies were mutually resolved. Ultimately, 25 articles were included, assessed and underwent a quality review.
Fig. 1.
Preferred Reporting Items for Systematic Reviews (PRISMA) flowchart demonstrating the article selection process
Study characteristics
In total, the studies included 709 patients after surgical treatment of MLKI, of whom 12.1% (n = 86) were diagnosed with postoperative AF. The average age of included patients was 33.6 ± 4.8 years with a mean follow-up of 47.2 ± 32.0 months. According to the classification by Schenck, there were 8.5% (n = 55) grade II, 44.0% (n = 285) grade IIIM, 31.4% (n = 203) grade IIIL and 16.1% (n = 104) grade IV injuries (n = 62 undefined Schenck II–IV injuries).
Definition
Overall, 22 of 25 studies used subjective definitions that can be divided into three subgroups: (1) Eight studies described AF solely as requirement of interventions like MUA/LOA. (2) Six studies referred to AF as “stiffness” and (3) eight studies referred to different manifestations of limited motion (flexion/extension loss).
Talbot, Richter and Jokela et al. [41, 70, 81] used objective cutoffs and defined AF as < 90° of flexion after 4 weeks; > 20° flexion loss to the contralateral side; knee extension deficiency of more than 10 degrees and flexion deficiency more than 20 degrees, respectively. To achieve simplification and comparability in this review, we defined AF, if not explicitly defined otherwise by the author, as requirement of additional manipulative treatments like LOA and MUA Table 2.
Table 2.
Characteristics of included studies (n = 25)
| Author | Year | Type of study | Level of evidence | Mean age (range) | Patients | Mean follow-up (mo) | Schenck classification | Surgical technique | Time to surgery (acute/staged/chronic) |
Lysholm (range) | IKDC | Coleman score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Shapiro et al. [76] | 1995 | Retrospective case series | IV | 26.6 | 7 | 51.4 | II–IV | ACL/PCL reconstruction with allografts; collaterals repair | Acute: 9.6 days (5–14) | 74.7 (34–93) | n/a | 31 |
| Wascher et al. [84] | 1999 | Retrospective case series | IV | 27.5 (14–51) | 13 | 38.4 (24–54) |
IIIM: 54% IIIL: 46% |
ACL/PCL reconstruction; collaterals repair |
69% Acute: 11 days 31% Chronic: 11 months |
88.0 (42–100) |
B 50.0% C 42.0% D 8.0% |
38 |
| Yeh et al. [89] | 1999 | Retrospective case series | IV | 37.8 (16–65) | 23 | 27.2 ± 7.86 |
IIIM: 57% IIIL: 30% IV: 13% |
Reconstruction of PCL (autograft + 1allograft); No ACL repair; Collaterals repair | Acute: 11.5 ± 5 days | 84.1 (79–93) | n/a | 49 |
| Ohkoshi al. [62] | 2002 | Retrospective case series | IV | 28.7 (18–27) | 8 | 40.1 ±16.7 |
IIIM: 67% IIIL: 33% |
ACL/PCL reconstruction (autograft and artificial ligament); collaterals reconstruction (Autograft) |
Staged: 1: 12.8 ± 5.3 days 2. 3.8 ± 1.1 months (after achieving sufficient ROM) |
n/a |
B 77.8% C 22.2% |
43 |
| Harner al. [22] | 2004 | Retrospective cohort study | III | 28.4 | 31 | > 24.0 | III | ACL/PCL reconstruction (allograft); collaterals reconstruction (allograft) or repair |
Acute: 12 days (5–21) Chronic: 6.5 months (5 weeks–22 months) |
87.0 ± 12.7 |
B 35.0% C 39.0% D 26.0% |
54 |
| Talbot et al. [81] | 2004 | Retrospective case series | IV | 28.5 (15–73) | 20 | 27.4 |
II: 5% IIIM: 43% IIIL: 48% IV: 5% |
ACL/PCL repair and augmentation with LARS; collaterals repair and if necessary Augmentation with LARS | Acute: 11 days | 71.7 ± 18 | n/a | 57 |
| Bin et al. [5] | 2007 | Retrospective case series | IV | 30.4 (20–51) | 14 | 88.9 (35–110) |
IIIM: 47% IIIL: 33% IV: 20% |
ACL/PCL reconstruction with allo/autograft; MCL repair or conservative; LCL repair or reconstruction |
Staged: 1: < 2 Weeks to injury 2. After full ROM (3-6monts) |
87.6 |
A 20.0% B 53.0% C 27.0% |
50 |
| Ibrahim et al. [34] | 2008 | Retrospective case series | IV | 27.3 (17–45) | 20 | 53.0 (36–96) |
IIIM: 75% IIIL: 25% |
ACL/PCL reconstruction (autograft); collaterals reconstruction with LARS | Acute: 2–3 weeks |
97–80: 95% 78–79: 5% |
B 45.0% C 45.0% D 10.0% |
54 |
| Lo et al. [51] | 2009 | Prospective clinical trail | III | 33 (19–48) | 11 | 55.0 (36–78) | II–III | ACL/PCL reconstruction (autograft); MCL repair; PLC reconstruction (autograft) | Chronic: 76 days (30–150) | 88.0 ± 5.8 | A + B 82.0% | 70 |
| Engebretsen et al. [13] | 2009 | Prospective cohort study | III | 33 (12–82) | 85 | Minimum 24.0 (25.2–118.8) |
II: 6% IIIM: 49% IIIL: 32% IV: 10 12% |
ACL/PCL reconstruction (auto-/allograft, collaterals repair or reconstruction |
Acute 60%: 1–2 weeks Chronic 40%: > 2 weeks |
81.0 (42–100) | 64.0 ± 20.0 | 83 |
| Ranger et al. [69] | 2011 | Retrospective case series | IV | 38.5 | 71 | 24–96 |
II: 4% IIIL: 39% IIIM: 41% IV: 16% |
All structures repair and reconstruction with LARS (ligament augmentation and reconstruction system) | Acute: 10.8 days (± 8) | 78.5 ± 18.5 | 67.9 ± 19.9 | 55 |
| Ibrahim et al. [35] | 2013 | Retrospective case series | IV | 26.4 (18–48) | 20 | 44.0 (24–52) | IIIL | ACL/PCL reconstruction (autograft/LARS); PLC reconstruction (autograft) | Acute: 15–21 days |
95–80 90% 75–79 10% |
B 45.0% C 45.0% D 10.0% |
49 |
| Piontek et al. [68] | 2013 | Retrospective cohort study | III | 36.0 | 11 | 27.0 ± 4 |
II: 64% IIIM: 36% |
All structures reconstruction (autograft) | Chronic: > 6 months |
100–98 54.6% 97–93 45.4% |
A 36.4% B 54.6% C 9.0% |
66 |
| Werner et al. [87] | 2014 | Retrospective case series | IV | 35.0 | 65 | 144.0 |
IIIM: 49% IV: 51% |
ACL reconstruction; PCL reconstruction in 63%; medial: 25% conservative, 18% repair and 57% reconstruction | Acute: < 3 weeks |
KD IIIM: 88.0 KD IV: 67.0 |
n/a | 60 |
| Heitmannet al. [25] | 2014 | Prospective case series | III | 33.0 (18–60) | 8 | 11.8 (10–15) | III–IV | ACL/PCL repair and bracing; MCL repair | Acute: 5 days (4–7) | 85.3 (62–99) | 75.7 (52.9–94.3) | 65 |
| Richter et al. [70] | 2014 | Retrospective case series | IV | 28.0 (16–39) | 8 | 72 (24–134.4) | IIIM | ACL/PCL reconstruction (allograft); MCL reconstruction (allograft) |
25% acute 75% chronic |
81.0 (58–100) |
B 57.0% C 29.0% D 14.0% |
52 |
| Kohl et al. [46] | 2015 | Prospective case series | III | 33.4 (17–56) | 35 | 25.9 (12–42) |
III: 74.3% IV: 25.7% |
ACL repair and augmentation (dynamic intraligamentary stabilization); PCL repair; collaterals repair or combined reconstruction (autograft) | Acute: < 2 days | 90.8 (81–95) |
B 83.0% C 17.0% |
63 |
| Angelini et al. [1] | 2015 | Retrospective case series | IV | 29.3 | 14 | 49.4 |
IIIM 14% IIIL 64% IV 22% |
All ligaments reconstruction (allografts); hinged external fixateur for 6 weeks postoperative | Chronic: 2.5 months (0.5–3) | 81.5 (49–95) |
B 71.0% C 21.0% D 8.0% |
48 |
| Khakha et al. [43] | 2016 | Retrospective cohort study | III | 36.5 (19–65) | 36 | 121.2 (84–228) | II–IV | ACL/PCL reconstruction (auto-/allograft) with LARS; collaterals reconstruction or repair | Acute: 12 days (1–21) | 80.0 (57–91) |
A 3.0% B 56.0% C 36.0% D 8.0% |
55 |
| Huax et al. [30] | 2016 | Retrospective case series | IV | 38.8 | 16 | 57.6 ± 15.6 |
IIIM 17% IIIL 22% IV 50% V 11% |
All ligaments repair | Acute: 5–10 days | 87.5 ± 7.7 | n/a | 60 |
| Sundararajan et al. [80] | 2018 | Retrospective cohort study | IV | 39.0 (17–74) | 45 | 36.0 (24–72) |
IIIM 69% IIIL 31% |
ACL/PCL reconstruction (autograft); collaterals repair or reconstruction; MCL mostly conservative |
78% acute-subacute: < 6 weeks 11% subacute: (6–12 weeks) 11% chronic: (3 months-6 months) |
87.7 | 74.7 | 58 |
| Heitmann et al. [24] | 2019 | Prospective multicenter study | II | 34.2 (18–60) | 69 | 14.0 |
IIIM 35% IIIL 54% IV 12% |
ACL/PCL repair and bracing; collaterals repair | Acute: 7.3 ± 1.6 days | 81.0 ± 15.5 |
A 13.0% B 19.0% C 32.0% D 13.0% |
84 |
| Jokela et al. [41] | 2020 | Retrospective cohort study | III | prox: 39.0 (21–64) distal 49.0 (17–67) | 25 |
Prox/mid: 98 (40–145) distal: 66 (24–82) |
IIIM | ACL/PCL reconstruction; MCL (proximal/midsubstance) conservative; MCL (distal) repair/reconstruction | Acute: 19 days (5–38) |
prox/mid: 88 (57–99) distal: 75 (40–100) |
prox/mid: 80.0 (57–99) distal: 62.0 (39–87) |
62 |
| Rosteius et al. [75] | 2021 | Retrospective Cohort Study | III | 38.3 | 27 | 18.1 ± 12.1 |
IIIM 22% IIIL 33% IV 45% |
All ligaments repair and bracing | Acute | 81.5 ± 10.4 | n/a | 63 |
| Goyal et al. [19] | 2021 | Retrospective case series | IV | 33.5 | 27 | 24.0 |
II 30% IIIM 41% IIIL 22% IV 7% |
All ligaments reconstruction (autograft) | Chronic: 14.6 ± 5.9 weeks | 50.4 ± 11.7 | 62.8 ± 5.1 | 66 |
Age, follow-up, time to surgery and subjective scores (Lysholm, IKDC) are stated in mean ± standard deviation (range). Results of PROMS (Lysholm and IKDC Score) are stated in points (0–100) or are qualified as “normal” (A), “nearly normal” (B), “abnormal” (C) or “severely abnormal” (D). Acute surgery is defined as surgery within < 3 weeks after trauma
ACL Anterior cruciate ligament, PCL posterior cruciate ligament, MCL medial collateral ligament, LCL lateral collateral ligament, PLC posterolateral corner, prox proximal, athro arthroscopically assisted
Prevalence
In total there were 86 cases of AF in 709 knees, which was equivalent to 12.1% (Table 3). The highest rate of AF was described by Shapiro et al. (57.1%) [76] and lowest by Khak et al. (2.8%) [43]. In both studies, MLKI were treated acutely (< 3 weeks) and reconstruction of both cruciate ligaments with concomitant repair or reconstruction of collateral ligaments was performed.
Table 3.
Summary of AF cases from included studies divided into subgroups
| Parameter | Total | Acute treatment | Chronic treatment [1, 19, 51, 68] | Mixed acute and chronic treatment [70, 80, 84] | Staged treatment [5, 62] | ACL/PCL repair [24, 25, 30, 46, 69, 75, 81] | ACL/PCL reconstruction | ROM week 1–3 allowed ≥ 90° | ROM week 1–3 allowed < 90°[5, 13, 25, 30, 35, 76, 84, 89] |
|---|---|---|---|---|---|---|---|---|---|
| Number of studies | 25 | 16 | 4 | 3 | 2 | 7 | 18 | 11 | 8 |
| Total number of patients | 709 | 558 | 63 | 66 | 22 | 246 | 463 | 267 | 186 |
| AF in % (n) | 12.1 (86) | 12.7 (71) | 9.5 (6) | 7.6 (5) | 18.2 (4) | 14.2 (35) | 11.0 (51) | 11.6 (31) | 14.0 (26) |
Subgroups include timing of surgery (acute, chronic and staged), surgical technique (repair or reconstruction of cruciate ligaments) and early postoperative rehabilitation (ROM restriction greater or under 90° Flexion at week 0–2 postoperatively)
Risk factors
Injury pattern
There was a trend toward higher rates of AF in Schenck III and IV injuries (Table 4). This was especially supported by Huax et al. [30], where all knees with AF had Schenck IV injuries. Also, Schenck II injuries [22] tended to have lower rates compared to Schenck III–IV injuries. On the other hand, Axibal et al. [3] could not find an increased rate comparing Schenck I–IV injuries, whereas PCL reconstruction was associated with stiffness. Engebretsen et al. [13] described a trend toward medial sided injuries. This could not be confirmed when dividing patients into subgroups based on Schenck’s Classification (Table 4). In accordance, Richter [70] and Jokela [41] et al. found no increased rates in Schenck IIIM injuries.
Table 4.
Cases of AF grouped by Schenck Classification
| Schenck grade | Total number of patients (author) | Number of cases with AF (rate in %) |
|---|---|---|
| II | 31 (Harner) | 4 (12.9) |
| IIIM | 33 (Richter, Jokela) | 3 (9.1) |
| IIIL | 23 (Okoshi, Ibrahim) | 5 (21.7) |
| IV | 9 (Huax) | 3 (33.3) |
Timing of surgery
Injuries treated after an initial non-operative rehabilitation (> 3 weeks) tended to develop lower rates of AF with 9.5% compared to injuries treated surgically in the acute phase with 12.7% (Table 3). However, the highest prevalence of AF was found after staged treatment algorithms with 18.0%. Harner and Patterson et al. [22, 65] provided evidence that primarily acutely treated patients required MUA.
Surgical technique
The distinction between repair (14.2%) and reconstruction (11.0%) of the torn cruciate ligaments showed a slight trend toward lower rates in the reconstruction group (Table 3).
Rehabilitation
There was a trend showing an increased rate of AF (14.0% vs. 11.6%) in studies compelling a more strict rehabilitation program with postoperative ROM allowed ≤ 90° within the first three postoperative weeks (Table 3).
Treatment of AF
The time from index surgery to MUA or LOA in the included studies averaged at 14.3 ± 8.8 (range 5–30) and 27.7 ± 12.8 (range 4–52) weeks, respectively. AF was mostly treated surgically by LOA (78.5%) and less often with MUA (21.5%). The total ROM before MUA and LOA was 51.7° ± 23.5 (range 30–90) and 80.2° ± 17.0 (range 60–113), resulting in total ROM gain of 65.0° ± 19.7 (range 22–65) and 48.0° ± 10.6 (range 33–60), respectively. There was no report of any complications after MUA/LOA (Table 5).
Table 5.
Summary of collected data concerning the prevalence
| Author | AF in % (n) | Time to MUA in weeks | Time to LOA in weeks | ROM before MUA | ROM before LOA | ROM gain after MUA | ROM gain after LOA |
|---|---|---|---|---|---|---|---|
| Shapiro et al | 57.1 (4) | 6.5 | 26.0 | 30° | 60° | 100° | 59° |
| Wascher et al | 15.4 (2) | – | 36.9 | – | 95° | – | 35° |
| Yeh et al | 13.0 (3) | – | 13.0 | – | n/a | – | n/a |
| Ohkoshi et al | 12.5 (1) | 5.0 | – | 90° | – | 40° | n/a |
| Harner et al | 12.9 (4) | 9.7 | 30.0 | n/a | n/a | 55 | n/a |
| Talbot et al | 10.0 (2) | – | 4.0 | – | n/a | – | n/a |
| Bin et al | 21.4 (3) | – | n/a | – | 113° | – | n/a |
| Ibrahim et al | 15.0 (3) | – | n/a | – | n/a | – | n/a |
| Lo et al | 9.1 (1) | – | 21.7 | – | 75° | – | 33° |
| Engebretsen et al | 6.0 (5) | n/a | n/a | n/a | n/a | n/a | n/a |
| Ranger et al | 19.7 (14) | – | n/a | – | n/a | – | n/a |
| Ibrahim et al | 20.0 (4) | – | n/a | – | n/a | – | n/a |
| Piontek et al | 9.1 (1) | – | 52.1 | – | n/a | – | n/a |
| Werner et al | 15.4 (10) | – | n/a | – | n/a | – | n/a |
| Heitmann et al.2014 | 12.5 (1) | – | n/a | – | n/a | – | n/a |
| Richter et al | 12.5 (1) | n/a | – | n/a | – | n/a | – |
| Kohl et al | 5.7 (2) | – | n/a | – | 73° | n/a | 53° |
| Angelini et al | 7.1 (1) | 30.4 | n/a | 35° | – | 65° | – |
| Khakha et al | 2.8 (1) | n/a | - | n/a | – | n/a | – |
| Huax et al | 18.8 (3) | 20.0 | 39.0 | n/a | n/a/ | n/a | n/a |
| Sundararajan et al | 4.5 (2) | – | n/a | – | 65° | - | 60° |
| Heitmann et al.2019 | 11.6 (8) | n/a | n/a | n/a | n/a | n/a | n/a |
| Jokela et al | 8.0 (2) | – | – | – | – | – | – |
| Rosteius et al | 18.5 (5) | – | 26.9 | – | n/a | – | n/a |
| Goyal et al | 11.1 (3) | n/a | – | n/a | – | n/a | - |
| Mean Total ± SD (range) | 12.1 (2.8–57.1) | 14.3 ± 8.8 (5–30) | 27.7 ± 12.8 (4–52) | 51.7° ± 23.5 (30–90) | 80.2° ± 17.0 (60–113) | 65.0° ± 19.7 (40–100) | 48.0° ± 10.6 (33–60) |
AF. Additionally, the distribution of MUA and LOA, time from index surgery to MUA/LOA, total ROM before and total ROM gain after MUA/LOA (at final follow-up) are shown
“n/a” indicates no data available, while "-” indicates no reported cases in the selected study;
Reporting quality and assessment of bias
Among the included studies, 15 were retrospective case series, five retrospective cohort studies and five prospective studies (Table 2).
The most common reasons for deduction in the Coleman score were study size < 60 patients (22/25 studies), absence of randomized controlled studies (25/25), retrospective collection of data (21/25 studies) and completion of assessment by subjects with minimal investigator assistance (24/25). The overall mean Coleman score of all included studies was 56.2 ± 12.5 points. Scores ranged from 84 to 31 points, showing a trend for better scores in more recent studies. Overall three studies were rated as good (12.0%), 16 as fair (64.0%) and 6 as poor (24.0%).
The interrater agreement was kappa = 0.922 (p < 0.001), implying a nearly perfect agreement between the two independent assessors (H.F. and L.K.) [47].
Discussion
Primary findings of this review demonstrate that (1) AF is a poorly defined condition with lack of consistency in the literature. (2) The absolute risk of AF across all studies was 12.1%. (3) Potential risk factors for AF are knee dislocation, higher-grade injuries (Schenck III and IV), acute treatment and ROM limiting rehabilitation programs. (4) Treatment of AF was mostly done by LOA (78.5%). (5) MUA and LOA were performed at an average of 14.3 and 27.7 weeks, respectively, and are safe and easy methods which yield good results. (6) The overall methodological quality of the studies was poor as measured by the Coleman score.
Our results confirm a recent meta-analysis by Kim et al. [45], who showed in an analysis of 21 studies pooled rates of AF to be 11.2%. However, Kim included studies with disruption of at least 2 of the 4 major knee ligaments and provided no further information about risk factors and treatment options.
Definition
There is a great inconsistency in defining AF in the included studies and literature in general [12, 82]. Ekhtiari et al. [12] came to similar results in a systematic review focusing on AF following ACL reconstruction and endorsed a homogenous definition and treatment guidelines for AF.
The terms “arthrofibrosis,” “stiffness” and “loss of motion” are often confusing, misleading and used synonymously. In the literature, complications concerning loss of motion, regardless of histopathological origin, time after surgery or, treatment responsiveness, are most commonly referred to as stiffness or AF [12, 57]. There are many classifications regarding motion loss [21, 40, 70, 77], but none does consider the multimodality of this condition.
It is worth mentioning that early ROM deficiencies within 3 months postoperatively are another entity, since these are often caused by postoperative swelling, pain or potential ROM restrictions given by the surgeon [61]. They can often be successfully treated by intensive physiotherapy and rarely need interventions like MUA/LOA [61]. Other factors like mechanical blockage (e.g., malposition of drilling tunnels, obstructive endobuttons, heterotopic ossifications) and infection also lead to loss of motion and are important differential diagnosis of AF. Hence, we propose a simply applicable objective clinical definition of AF including (1) motion loss defined by Shelbourne’s original classification [77], (2) occurrence > 3 months postoperatively, (3) absence of mechanical blockage or infection and (4) insufficient improvement of ROM by aggressive physiotherapy.
Injury pattern
In terms of injury pattern, a trend toward higher rates of AF in Schenck III–IV injuries was detected. This is supported by an epidemiology study, where a doubling of the 6-month incidence of MUA after combined ACL and collateral ligament reconstruction (1.8%), concomitant arthroscopic ACL and PCL reconstruction (4.1%), and combined ACL, PCL and collateral ligament reconstruction (8.0%) was shown [85]. Injuries with three or more ligaments requiring operative intervention and knee dislocation were shown to be associated with stiffness [9, 21], whereas others could not detect a correlation with the knee dislocation grade and postoperative motion loss [32]. Engebretsen et al. [13] suspected medial sided injuries to be associated with higher rates of AF, which is supported by a large retrospective study where mostly Schenck IIIM injuries required LOA [27]. However, this trend could not be supported by our results as well as by a large study of La Prade et al., who included surgically treated patients with at least two major knee ligaments torn [48]. A reason for this inconsistency could be the heterogeneity of the studies, e.g., in terms of surgical technique and rehabilitation; however, lateral injuries may require more complex surgery than medial sided injuries (e.g., reconstruction of the posterolateral corner) and therefore result in higher rates of AF.
A possible explanation for more severe injuries to have higher rates of AF is extensive soft tissue damage resulting in greater inflammatory reaction and longer operation time.
Surgical technique
Our data suggest a minor difference between reconstruction and repair of torn cruciate ligaments favoring reconstruction, which could be explained by the connection between acute treatment and repair, resulting in higher rates of AF.
Other aspects in surgical treatment like procedure time, technique of reconstruction or repair were unrewarding to investigate since the included studies showed great heterogeneity and provided scarce information.
Interestingly, allografts tolerate long periods of immobilization better than autografts and minimization of autografts taken from the injured knee is described to decrease the risk of AF [54, 73]. Another recently published study showed that prolonged procedure time (> 300 min), PCL reconstruction and shorter time to surgery were particular risk factors [3]. Taken together the impact of the surgical technique remains elusive, but allografts and short surgery time, minimizing the soft tissue damage, might prevent the development of AF.
Timing of surgery
Many studies and systematic reviews advocate that acute surgery yields overall better results [22, 28, 44, 50, 79] and delayed surgery (after 2–3 weeks) decreases the risk of AF [14, 50], whereas others found that acute surgery was not associated with stiffness [21].
The included studies indicate a trend toward higher rates of AF in acutely treated MLKI. This is in line with a review, showing that the number of patients undergoing MUA or LOA for the treatment of joint stiffness is greater in both the staged and acute treatment groups compared with the chronic treatment group [59]. Similar results were presented with all patients requiring manipulation or surgery for AF, who had surgical repair in the acute phase but higher outcome scores compared with those receiving surgery later [48, 63]. These results are underlined by a study focusing on the complications after MLKI surgeries [64], which showed a significantly decreased risk of AF when time to surgery is delayed.
One possible explanation for lower AF rates in delayed surgery could be related to more extensive preoperative physical therapy, which could ultimately result in better postoperative ROM. Additionally, increased time from injury to surgery may allow for reduced inflammation and swelling in the knee as shown in ACL reconstruction surgery (ACLR) [33].
Hence, a staged procedure was proposed, which might combine the advantages of acute and chronic treatment [78]. Mainly, this means reconstruction/repair of the PCL and peripheral ligaments, while the ACL is reconstructed later or treated conservatively [39]. Surprisingly, we found the highest rates of AF (18.2%) within staged treatment. Noticeably, only two studies in this review [5, 62] conducted a staged treatment, with a small group of patients (n = 22), which may lead to relevant bias. Mook et al. [59] showed in a systematic review lower rates of flexion loss in staged treatment, but no difference in AF, apart from this pointing out the importance of distinguishing between simple flexion loss and AF. A review concluded that staged treatment simplified the operative process and operation time and therefore might decrease the rate of AF [39]. However, a study comparing acute and staged treatment could not detect a difference in postoperative ROM between acute and staged treatment [37].
We propose that best results are shown when surgery is performed as soon as the patient general condition allows them to actively participate in postoperative rehabilitation. Solely if ligament surgery is unavoidably delayed and stability is crucial (e.g., vascular injury, compartment syndrome, open major trauma, general condition), the knee should be stabilized within a hinged external fixator or hinged knee brace, thereby accepting potential motion loss [31, 55].
Rehabilitation
After MLKI surgery, a balance between the risk of recurrent laxity and the risk of AF must be found [20]. Aggressive motion exercise started too early might risk stretching or damaging the healing soft tissue. Accordingly, timing and intensity of postoperative rehabilitation play a crucial role in terms of final outcome [7, 9, 14, 71].
Our data provide evidence that a more aggressive rehabilitation may lead to lower rates of AF while the final outcome is unaffected.
In accordance, a systematic review discovered a difference in flexion loss among patients when compared on the basis of rehabilitation [59]. Within the acute treatment group, flexion loss of 10° was reported in 48.0% of those who were immobilized, compared with 28.0% of those who were allowed early mobilization. Encouragingly early rehabilitation was not associated with increased joint instability in acutely managed patient [59]. A recent review showed consistently improved outcomes after early postoperative physical therapy and range of motion [42]. Hoit et al. [29], however, were unable to demonstrate a difference between early and late knee rehabilitation with regard to knee stiffness, laxity or patient-reported outcomes, but it is worth mentioning they had a very limited study size of 36 participants.
Taken together there is evidence that aggressive postoperative rehabilitation leads to lower rates of AF, without altering patient-reported outcomes. Not to be forgotten treating residual laxity is often more challenging than AF [74].
Treatment of AF
Paulus et al. [66] proposed that early surgical intervention to treat AF is best. In the literature, AF is described to require surgical treatment in 29.0% of patients [7]. It was shown that the results of LOA procedure yield excellent motion gains and surgery should be performed sooner than six months after primary surgery to achieve best outcome [10]. Time from primary surgery to MUA and LOA in the included studies averaged at 14.3 and 27.7 weeks with LOA being performed in the majority of cases. Similarly in total knee arthroplasty, if MUA has not been performed within 3 months or is unsuccessful, LOA is recommended, because the risk of iatrogenic fracture during MUA increases [4]. It is assumed that similar treatment algorithms and outcomes can be assigned to knee ligament surgery [12]. When comparing MUA and LOA (with or without concurrent MUA), the final ROM is similar [17]. The greater ROM gain shown in MUA compared with LOA in this review might be due to the severely limited ROM in cases with MUA before the intervention. A differentiation between flexion and extension could not be performed due to the poor study situation. However, this is important since a loss of flexion is easier to treat and usually better tolerated [36].
Hughes et al. [32] noticed, in a retrospective case series, time from primary surgery to MUA/LOA was 13.7 weeks, with no distinction between MUA and LOA being made. These results are only comparable to a limited extent, since Hughes et al. included 61% KD I injuries. Furthermore, it was shown that motion loss in the early stages (1 month postoperatively) was treated mostly conservatively but in later stages (3–6 months) all cases were treated with MUA/LOA, thus emphasizing the importance of early and aggressive physical therapy if motion loss is encountered within the first 3 months postoperatively. Overall, MUA and LOA are safe and well established procedures which yield excellent results.
Limitations
First a limitation of this systematic review is reliance on data from Level III and IV evidence studies; this is due to a general lack of high level of evidence studies related to MLKI. The low methodological quality of the included studies, lack of control groups and of randomization limits the quality of our results. Secondly, there was an essential amount of heterogeneity within the patient characteristics, injury mechanism and surgical technique. Thirdly, the detected differences in AF especially in terms of surgical technique, timing and rehabilitation should be treated with caution, due to the slight differences in small number of cases. Additionally, the reporting of AF and outcomes was often inconsistent and poor, which affected our analysis. It is important to mention that none of the included studies made direct comparisons between groups with regard to AF. AF definition was mostly simplified (requirement of LOA/MUA) not considering the pathologies multimodality and fluent transition between loss of motion and AF. Moreover, many studies did not report about AF and had to be sorted out, resulting in a selection bias. For future investigations, larger prospective studies with higher methodological quality and detailed information about AF are needed.
Conclusion
AF is a common but poorly defined complication particularly in high-grade MLKI. Early postoperative and intensified physiotherapy is important to reduce the risk of AF. MUA and LOA are very effective treatment options and result in good clinical outcome. Prospective studies with bigger study population are needed to optimize treatment algorithms of further patients after MLKI.
Funding
Open Access funding enabled and organized by Projekt DEAL. No funding was received.
Declarations
Conflict of interest
No potential competing interest was reported by the authors.
Ethical approval
Ethics approval was not required for this systematic review.
Informed consent
Informed consent was not required for this systematic review.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Hendrik Fahlbusch, Email: h.fahlbusch@uke.de.
Lukas Krivec, Email: l.krivec@uke.de.
Sebastian Müller, Email: s.mueller@usb.ch.
Alonja Reiter, Email: a.reiter@uke.de.
Karl Heinz Frosch, Email: k.frosch@uke.de.
Matthias Krause, Email: m.krause@uke.de.
References
- 1.Angelini FJ, Helito CP, Bonadio MB, da Mota EARF, Pecora JR, Camanho GL. Surgical management of knee dislocations with ligament reconstruction associated with a hinged external fixator. Orthop Traumatol Surg Res. 2015;101:77–81. doi: 10.1016/j.otsr.2014.11.001. [DOI] [PubMed] [Google Scholar]
- 2.Angelini FJ, Helito CP, Bonadio MB, Guimarães TM, Barreto RB, Pécora JR, et al. External fixator for treatment of the sub-acute and chronic multi-ligament-injured knee. Knee Surg Sports Traumatol Arthrosc. 2015;23:3012–3018. doi: 10.1007/s00167-015-3719-0. [DOI] [PubMed] [Google Scholar]
- 3.Axibal DP, Yeatts NC, Hysong AA, Hong IS, Trofa DP, Moorman CT, 3rd, et al. Intraoperative and Early (90-Day) Postoperative Complications and Associated Variables with Multiligamentous Knee Reconstruction: 15-year Experience from a Single Academic Institution. Arthroscopy. 2021 doi: 10.1016/j.arthro.2021.05.027. [DOI] [PubMed] [Google Scholar]
- 4.Bawa HS, Wera GD, Kraay MJ, Marcus RE, Goldberg VM. Predictors of range of motion in patients undergoing manipulation after TKA. Clin Orthop Relat Res. 2013;471:258–263. doi: 10.1007/s11999-012-2591-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bin SI, Nam TS. Surgical outcome of 2-stage management of multiple knee ligament injuries after knee dislocation. Arthroscopy. 2007;23:1066–1072. doi: 10.1016/j.arthro.2007.05.008. [DOI] [PubMed] [Google Scholar]
- 6.Brautigan B, Johnson DL. The epidemiology of knee dislocations. Clin Sports Med. 2000;19:387–397. doi: 10.1016/s0278-5919(05)70213-1. [DOI] [PubMed] [Google Scholar]
- 7.Burrus MT, Werner BC, Griffin JW, Gwathmey FW, Miller MD. Diagnostic and management strategies for multiligament knee injuries: a critical analysis review. JBJS Rev. 2016 doi: 10.2106/JBJS.RVW.O.00020. [DOI] [PubMed] [Google Scholar]
- 8.Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports. 2000;10:2–11. doi: 10.1034/j.1600-0838.2000.010001002.x. [DOI] [PubMed] [Google Scholar]
- 9.Cook S, Ridley TJ, McCarthy MA, Gao Y, Wolf BR, Amendola A, et al. Surgical treatment of multiligament knee injuries. Knee Surg Sports Traumatol Arthrosc. 2015;23:2983–2991. doi: 10.1007/s00167-014-3451-1. [DOI] [PubMed] [Google Scholar]
- 10.Cosgarea AJ, DeHaven KE, Lovelock JE. The surgical treatment of arthrofibrosis of the knee. Am J Sports Med. 1994;22:184–191. doi: 10.1177/036354659402200206. [DOI] [PubMed] [Google Scholar]
- 11.Czamara A, Kuźniecow M, Królikowska A. Arthrofibrosis of the knee joint - the current state of knowledge. Literature review. Ortop Traumatol Rehabil. 2019;21:95–106. doi: 10.5604/01.3001.0013.1545. [DOI] [PubMed] [Google Scholar]
- 12.Ekhtiari S, Horner NS, de Sa D, Simunovic N, Hirschmann MT, Ogilvie R, et al. Arthrofibrosis after ACL reconstruction is best treated in a step-wise approach with early recognition and intervention: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2017;25:3929–3937. doi: 10.1007/s00167-017-4482-1. [DOI] [PubMed] [Google Scholar]
- 13.Engebretsen L, Risberg MA, Robertson B, Ludvigsen TC, Johansen S. Outcome after knee dislocations: a 2–9 years follow-up of 85 consecutive patients. Knee Surg Sports Traumatol Arthrosc. 2009;17:1013–1026. doi: 10.1007/s00167-009-0869-y. [DOI] [PubMed] [Google Scholar]
- 14.Fanelli GC, Edson CJ. Surgical treatment of combined PCL-ACL medial and lateral side injuries (global laxity): surgical technique and 2- to 18-year results. J Knee Surg. 2012;25:307–316. doi: 10.1055/s-0032-1326997. [DOI] [PubMed] [Google Scholar]
- 15.Fanelli GC, Edson CJ, Orcutt DR, Harris JD, Zijerdi D. Treatment of combined anterior cruciate-posterior cruciate ligament-medial-lateral side knee injuries. J Knee Surg. 2005;18:240–248. doi: 10.1055/s-0030-1248188. [DOI] [PubMed] [Google Scholar]
- 16.Fanelli GC, Orcutt DR, Edson CJ. The multiple-ligament injured knee: evaluation, treatment, and results. Arthroscopy. 2005;21:471–486. doi: 10.1016/j.arthro.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 17.Fitzsimmons SE, Vazquez EA, Bronson MJ. How to treat the stiff total knee arthroplasty?: a systematic review. Clin Orthop Relat Res. 2010;468:1096–1106. doi: 10.1007/s11999-010-1230-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Frosch KH, Preiss A, Heider S, Stengel D, Wohlmuth P, Hoffmann MF, et al. Primary ligament sutures as a treatment option of knee dislocations: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21:1502–1509. doi: 10.1007/s00167-012-2154-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goyal T, Paul S, Banerjee S, Das L. Outcomes of one-stage reconstruction for chronic multiligament injuries of knee. Knee Surg Relat Res. 2021;33:3. doi: 10.1186/s43019-020-00083-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gwathmey F, Shafique D, Miller M. Our approach to the management of the multiple-ligament knee injury. Operat Techniq Sports Med. 2010;18:235–244. [Google Scholar]
- 21.Hanley J, Westermann R, Cook S, Glass N, Amendola N, Wolf BR, et al. Factors associated with knee stiffness following surgical management of multiligament knee injuries. J Knee Surg. 2017;30:549–554. doi: 10.1055/s-0036-1593624. [DOI] [PubMed] [Google Scholar]
- 22.Harner CD, Waltrip RL, Bennett CH, Francis KA, Cole B, Irrgang JJ. Surgical management of knee dislocations. J Bone Joint Surg Am. 2004;86:262–273. doi: 10.2106/00004623-200402000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Hegyes MS, Richardson MW, Miller MD. Knee dislocation. Complications of nonoperative and operative management. Clin Sports Med. 2000;19:519–543. doi: 10.1016/s0278-5919(05)70222-2. [DOI] [PubMed] [Google Scholar]
- 24.Heitmann M, Akoto R, Krause M, Hepp P, Schöpp C, Gensior TJ, et al. Management of acute knee dislocations: anatomic repair and ligament bracing as a new treatment option-results of a multicentre study. Knee Surg Sports Traumatol Arthrosc. 2019;27:2710–2718. doi: 10.1007/s00167-018-5317-4. [DOI] [PubMed] [Google Scholar]
- 25.Heitmann M, Gerau M, Hötzel J, Giannakos A, Frosch KH, Preiss A. Ligament bracing–augmented primary suture repair in multiligamentous knee injuries. Oper Orthop Traumatol. 2014;26:19–29. doi: 10.1007/s00064-013-0263-2. [DOI] [PubMed] [Google Scholar]
- 26.Held M, Laubscher M, von Bormann R, Walters J, Roche S, Banderker A, et al. High rate of popliteal artery injuries and limb loss in 96 knee dislocations. SA Orthopaed J. 2016;15:72–76. [Google Scholar]
- 27.Hirschmann MT, Meier MD, Amsler F, Friederich NF. Long-term outcome of patients treated surgically for traumatic knee dislocation: does the injury pattern matter? Phys Sportsmed. 2010;38:82–89. doi: 10.3810/psm.2010.06.1786. [DOI] [PubMed] [Google Scholar]
- 28.Hohmann E, Glatt V, Tetsworth K. Early or delayed reconstruction in multi-ligament knee injuries: A systematic review and meta-analysis. Knee. 2017;24:909–916. doi: 10.1016/j.knee.2017.06.011. [DOI] [PubMed] [Google Scholar]
- 29.Hoit G, Rubacha M, Chahal J, Khan R, Ravi B, Whelan DB. Is there a disadvantage to early physical therapy after multiligament surgery for knee dislocation? a pilot randomized clinical trial. Clin Orthop Relat Res. 2021;479:1725–1736. doi: 10.1097/CORR.0000000000001729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hua X, Tao H, Fang W, Tang J. Single-stage in situ suture repair of multiple-ligament knee injury: a retrospective study of 17 patients (18 knees) BMC Musculoskelet Disord. 2016;17:41. doi: 10.1186/s12891-016-0894-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hughes JD, Lynch AD, Smith CN, Musahl V, Irrgang JJ. External fixation increases complications following surgical treatment of multiple ligament knee injuries. Knee Surg Sports Traumatol Arthrosc. 2022;30:161–166. doi: 10.1007/s00167-021-06508-9. [DOI] [PubMed] [Google Scholar]
- 32.Hughes JD, Lynch AD, Smith CN, Musahl V, Irrgang JJ. External fixation increases complications following surgical treatment of multiple ligament knee injuries. Knee Surg Sports Traumatol Arthrosc. 2021 doi: 10.1007/s00167-021-06508-9. [DOI] [PubMed] [Google Scholar]
- 33.Huleatt J, Gottschalk M, Fraser K, Boden A, Dalwadi P, Xerogeanes J, et al. Risk factors for manipulation under anesthesia and/or lysis of adhesions after anterior cruciate ligament reconstruction. Orthop J Sports Med. 2018;6:2325967118794490. doi: 10.1177/2325967118794490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ibrahim SA, Ahmad FH, Salah M, Al Misfer AR, Ghaffer SA, Khirat S. Surgical management of traumatic knee dislocation. Arthroscopy. 2008;24:178–187. doi: 10.1016/j.arthro.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 35.Ibrahim SA, Ghafar S, Salah M, Abo Alnas M, Al Misfer A, Farouk H, et al. Surgical management of traumatic knee dislocation with posterolateral corner injury. Arthroscopy. 2013;29:733–741. doi: 10.1016/j.arthro.2012.11.021. [DOI] [PubMed] [Google Scholar]
- 36.Irrgang JJ, Harner CD. Loss of motion following knee ligament reconstruction. Sports Med. 1995;19:150–159. doi: 10.2165/00007256-199519020-00006. [DOI] [PubMed] [Google Scholar]
- 37.Ishibashi Y, Kimura Y, Sasaki E, Sasaki S, Yamamoto Y, Tsuda E. Acute primary repair of extraarticular ligaments and staged surgery in multiple ligament knee injuries. J Orthopaedics Traumatol. 2020;21:18–18. doi: 10.1186/s10195-020-00557-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.James EW, Wolfe I, Marx RG. Results of treatment of the multiple ligament injured (Dislocated) Knee. Sports Med Arthrosc Rev. 2020;28:116–119. doi: 10.1097/JSA.0000000000000274. [DOI] [PubMed] [Google Scholar]
- 39.Jiang W, Yao J, He Y, Sun W, Huang Y, Kong D. The timing of surgical treatment of knee dislocations: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23:3108–3113. doi: 10.1007/s00167-014-3435-1. [DOI] [PubMed] [Google Scholar]
- 40.Jokela MA, Mäkinen TJ, Koivikko MP, Lindahl JM, Halinen J, Lindahl J. Treatment of medial-sided injuries in patients with early bicruciate ligament reconstruction for knee dislocation. Knee Surg Sports Traumatol Arthrosc. 2020 doi: 10.1007/s00064-020-00674-8,10.1007/s00167-020-06207-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jokela MA, Mäkinen TJ, Koivikko MP, Lindahl JM, Halinen J, Lindahl J. Treatment of medial-sided injuries in patients with early bicruciate ligament reconstruction for knee dislocation. Knee Surg Sports Traumatol Arthrosc. 2021;29:1872–1879. doi: 10.1007/s00167-020-06207-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Keeling LE, Powell SN, Purvis E, Willauer TJ, Postma WF. Postoperative rehabilitation of multiligament knee reconstruction: a systematic review. Sports Med Arthrosc Rev. 2021;29:94–109. doi: 10.1097/JSA.0000000000000308. [DOI] [PubMed] [Google Scholar]
- 43.Khakha RS, Day AC, Gibbs J, Allen S, Hill P, Hull J, et al. Acute surgical management of traumatic knee dislocations–Average follow-up of 10 years. Knee. 2016;23:267–275. doi: 10.1016/j.knee.2015.09.019. [DOI] [PubMed] [Google Scholar]
- 44.Kim SH, Han SJ, Park YB, Kim DH, Lee HJ, Pujol N. A systematic review comparing the results of early vs delayed ligament surgeries in single anterior cruciate ligament and multiligament knee injuries. Knee Surg Relat Res. 2021;33:1. doi: 10.1186/s43019-020-00086-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kim SH, Park YB, Kim BS, Lee DH, Pujol N. Incidence of associated lesions of multiligament knee injuries: a systematic review and meta-analysis. Orthop J Sports Med. 2021;9:23259671211010409. doi: 10.1177/23259671211010409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kohl S, Stock A, Ahmad SS, Zumstein M, Keel M, Exadaktylos A, et al. Dynamic intraligamentary stabilization and primary repair: a new concept for the treatment of knee dislocation. Injury. 2015;46:724–728. doi: 10.1016/j.injury.2014.10.012. [DOI] [PubMed] [Google Scholar]
- 47.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 48.LaPrade RF, Chahla J, DePhillipo NN, Cram T, Kennedy MI, Cinque M, et al. Single-stage multiple-ligament knee reconstructions for sports-related injuries: outcomes in 194 patients. Am J Sports Med. 2019;47:2563–2571. doi: 10.1177/0363546519864539. [DOI] [PubMed] [Google Scholar]
- 49.Levy BA, Dajani KA, Morgan JA, Shah JP, Dahm DL, Stuart MJ. Repair versus reconstruction of the fibular collateral ligament and posterolateral corner in the multiligament-injured knee. Am J Sports Med. 2010;38:804–809. doi: 10.1177/0363546509352459. [DOI] [PubMed] [Google Scholar]
- 50.Levy BA, Dajani KA, Whelan DB, Stannard JP, Fanelli GC, Stuart MJ, et al. Decision making in the multiligament-injured knee: an evidence-based systematic review. Arthroscopy. 2009;25:430–438. doi: 10.1016/j.arthro.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 51.Lo YP, Hsu KY, Chen LH, Wang CJ, Yeh WL, Chan YS, et al. Simultaneous arthroscopic reconstruction of the anterior and posterior cruciate ligament using hamstring and quadriceps tendon autografts. J Trauma. 2009;66:780–788. doi: 10.1097/TA.0b013e31815d9b88. [DOI] [PubMed] [Google Scholar]
- 52.Lynch AD, Chmielewski T, Bailey L, Stuart M, Cooper J, Coady C, et al. Current concepts and controversies in rehabilitation after surgery for multiple ligament knee injury. Curr Rev Musculoskelet Med. 2017;10:328–345. doi: 10.1007/s12178-017-9425-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Manske RC, Hosseinzadeh P, Giangarra CE. Multiple ligament knee injury: complications. N Am J Sports Phys Ther. 2008;3:226–233. [PMC free article] [PubMed] [Google Scholar]
- 54.Marom N, Ruzbarsky JJ, Roselaar N, Marx RG. Knee MLI injuries: common problems and solutions. Clin Sports Med. 2018;37:281–291. doi: 10.1016/j.csm.2017.12.011. [DOI] [PubMed] [Google Scholar]
- 55.Maslaris A, Brinkmann O, Bungartz M, Krettek C, Jagodzinski M, Liodakis E. Management of knee dislocation prior to ligament reconstruction: What is the current evidence? Update of a universal treatment algorithm. Eur J Orthop Surg Traumatol. 2018;28:1001–1015. doi: 10.1007/s00590-018-2148-4. [DOI] [PubMed] [Google Scholar]
- 56.Messner J, Papakostidis C, Giannoudis PV, Kanakaris NK. Duration of administration of antibiotic agents for open fractures: meta-analysis of the existing evidence. Surg Infect (Larchmt) 2017;18:854–867. doi: 10.1089/sur.2017.108. [DOI] [PubMed] [Google Scholar]
- 57.Millett PJ, Wickiewicz TL, Warren RF. Motion loss after ligament injuries to the knee. Part I: causes. Am J Sports Med. 2001;29:664–675. doi: 10.1177/03635465010290052401. [DOI] [PubMed] [Google Scholar]
- 58.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 59.Mook WR, Miller MD, Diduch DR, Hertel J, Boachie-Adjei Y, Hart JM. Multiple-ligament knee injuries: a systematic review of the timing of operative intervention and postoperative rehabilitation. J Bone Joint Surg Am. 2009;91:2946–2957. doi: 10.2106/JBJS.H.01328. [DOI] [PubMed] [Google Scholar]
- 60.Mosquera MF, Jaramillo A, Gil R, Gonzalez Y. Controversies in acute multiligamentary knee injuries (MLKI) J Exp Orthop. 2020;7:56. doi: 10.1186/s40634-020-00260-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Noyes FR, Berrios-Torres S, Barber-Westin SD, Heckmann TP. Prevention of permanent arthrofibrosis after anterior cruciate ligament reconstruction alone or combined with associated procedures: a prospective study in 443 knees. Knee Surg Sports Traumatol Arthrosc. 2000;8:196–206. doi: 10.1007/s001670000126. [DOI] [PubMed] [Google Scholar]
- 62.Ohkoshi Y, Nagasaki S, Shibata N, Yamamoto K, Hashimoto T, Yamane S. Two-stage reconstruction with autografts for knee dislocations. Clin Orthop Relat Res. 2002 doi: 10.1097/00003086-200205000-00024169-175. [DOI] [PubMed] [Google Scholar]
- 63.Owens BD, Neault M, Benson E, Busconi BD. Primary repair of knee dislocations: results in 25 patients (28 knees) at a mean follow-up of four years. J Orthop Trauma. 2007;21:92–96. doi: 10.1097/BOT.0b013e3180321318. [DOI] [PubMed] [Google Scholar]
- 64.Patel NK, Lian J, Nickoli M, Vaswani R, Irrgang JJ, Lesniak BP, et al. Risk factors associated with complications after operative treatment of multiligament knee injury. Orthop J Sports Med. 2021;9:2325967121994203–2325967121994203. doi: 10.1177/2325967121994203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Patterson BM, Agel J, Swiontkowski MF, Mackenzie EJ, Bosse MJ. Knee dislocations with vascular injury: outcomes in the Lower Extremity Assessment Project (LEAP) Study. J Trauma. 2007;63:855–858. doi: 10.1097/TA.0b013e31806915a7. [DOI] [PubMed] [Google Scholar]
- 66.Paulos LE, Rosenberg TD, Drawbert J, Manning J, Abbott P. Infrapatellar contracture syndrome. An unrecognized cause of knee stiffness with patella entrapment and patella infera. Am J Sports Med. 1987;15:331–341. doi: 10.1177/036354658701500407. [DOI] [PubMed] [Google Scholar]
- 67.Peskun CJ, Whelan DB. Outcomes of operative and nonoperative treatment of multiligament knee injuries: an evidence-based review. Sports Med Arthrosc Rev. 2011;19:167–173. doi: 10.1097/JSA.0b013e3182107d5f. [DOI] [PubMed] [Google Scholar]
- 68.Piontek T, Ciemniewska-Gorzela K, Szulc A, Naczk J, Wardak M, Trzaska T, et al. Arthroscopically assisted combined anterior and posterior cruciate ligament reconstruction with autologous hamstring grafts-isokinetic assessment with control group. PLoS One. 2013;8:e82462. doi: 10.1371/journal.pone.0082462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ranger P, Renaud A, Phan P, Dahan P, De Oliveira E, Jr., Delisle J, Evaluation of reconstructive surgery using artificial ligaments in 71 acute knee dislocations. Int Orthop. 2011;35:1477–1482. doi: 10.1007/s00264-010-1154-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Richter D, Wascher DC, Schenck RC., Jr A novel posteromedial approach for tibial inlay PCL reconstruction in KDIIIM injuries: avoiding prone patient positioning. Clin Orthop Relat Res. 2014;472:2680–2690. doi: 10.1007/s11999-014-3557-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Richter M, Bosch U, Wippermann B, Hofmann A, Krettek C. Comparison of surgical repair or reconstruction of the cruciate ligaments versus nonsurgical treatment in patients with traumatic knee dislocations. Am J Sports Med. 2002;30:718–727. doi: 10.1177/03635465020300051601. [DOI] [PubMed] [Google Scholar]
- 72.Robertson A, Nutton RW, Keating JF. Dislocation of the knee. J Bone Joint Surg Br. 2006;88:706–711. doi: 10.1302/0301-620X.88B6.17448. [DOI] [PubMed] [Google Scholar]
- 73.Rodríguez-Merchán EC, De la Corte-Rodríguez H. Complications of surgical reconstruction of multiligament injuries of the knee joint: diagnosis, prevention and treatment. EFORT Open Rev. 2021;6:973–981. doi: 10.1302/2058-5241.6.210057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Romeyn RL, Jennings J, Davies GJ. Surgical treatment and rehabilitation of combined complex ligament injuries. NAJSPT. 2008;3:212–225. [PMC free article] [PubMed] [Google Scholar]
- 75.Rosteius T, Jettkant B, Rausch V, Lotzien S, Königshausen M, Schildhauer TA, et al. Anatomical repair and ligament bracing of Schenck III and IV knee joint dislocations leads to acceptable subjective and kinematic outcomes. Knee Surg Sports Traumatol Arthrosc. 2021;29:4188–4197. doi: 10.1007/s00167-021-06501-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Shapiro MS, Freedman EL. Allograft reconstruction of the anterior and posterior cruciate ligaments after traumatic knee dislocation. Am J Sports Med. 1995;23:580–587. doi: 10.1177/036354659502300511. [DOI] [PubMed] [Google Scholar]
- 77.Shelbourne KD, Patel DV, Martini DJ. Classification and management of arthrofibrosis of the knee after anterior cruciate ligament reconstruction. Am J Sports Med. 1996;24:857–862. doi: 10.1177/036354659602400625. [DOI] [PubMed] [Google Scholar]
- 78.Shelbourne KD, Pritchard J, Rettig AC, McCarroll JR, Vanmeter CD. Knee dislocations with intact PCL. Orthop Rev. 1992;21(607–608):610–601. [PubMed] [Google Scholar]
- 79.Smith JH, Belk JW, Friedman JL, Dragoo JL, Frank RM, Bravman JT, et al. Predictors of mid- to long-term outcomes in patients experiencing a knee dislocation: a systematic review of clinical studies. J Knee Surg. 2021 doi: 10.1055/s-0041-1723762. [DOI] [PubMed] [Google Scholar]
- 80.Sundararajan SR, Sambandam B, Rajagopalakrishnan R, Rajasekaran S. Comparison of KD3-M and KD3-L multiligamentous knee injuries and analysis of predictive factors that influence the outcomes of single-stage reconstruction in KD3 injuries. Orthop J Sports Med. 2018;6:2325967118794367. doi: 10.1177/2325967118794367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Talbot M, Berry G, Fernandes J, Ranger P. Knee dislocations: experience at the Hôpital du Sacré-Coeur de Montréal. Can J Surg. 2004;47:20–24. [PMC free article] [PubMed] [Google Scholar]
- 82.Usher KM, Zhu S, Mavropalias G, Carrino JA, Zhao J, Xu J. Pathological mechanisms and therapeutic outlooks for arthrofibrosis. Bone research. 2019;7:9–9. doi: 10.1038/s41413-019-0047-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Vicenti G, Solarino G, Carrozzo M, De Giorgi S, Moretti L, De Crescenzo A, et al. Major concern in the multiligament-injured knee treatment: a systematic review. Injury. 2019;50(Suppl 2):S89–s94. doi: 10.1016/j.injury.2019.01.052. [DOI] [PubMed] [Google Scholar]
- 84.Wascher DC, Becker JR, Dexter JG, Blevins FT. Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation. Results using fresh-frozen nonirradiated allografts. Am J Sports Med. 1999;27:189–196. doi: 10.1177/03635465990270021301. [DOI] [PubMed] [Google Scholar]
- 85.Werner BC, Cancienne JM, Miller MD, Gwathmey FW. Incidence of manipulation under anesthesia or lysis of adhesions after arthroscopic knee surgery. Am J Sports Med. 2015;43:1656–1661. doi: 10.1177/0363546515578660. [DOI] [PubMed] [Google Scholar]
- 86.Werner BC, Gwathmey FW, Jr, Higgins ST, Hart JM, Miller MD. Ultra-low velocity knee dislocations: patient characteristics, complications, and outcomes. Am J Sports Med. 2014;42:358–363. doi: 10.1177/0363546513508375. [DOI] [PubMed] [Google Scholar]
- 87.Werner BC, Hadeed MM, Gwathmey FW, Jr, Gaskin CM, Hart JM, Miller MD. Medial injury in knee dislocations: what are the common injury patterns and surgical outcomes? Clin Orthop Relat Res. 2014;472:2658–2666. doi: 10.1007/s11999-014-3483-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Joint Surg Am. 2003;85:1–3. [PubMed] [Google Scholar]
- 89.Yeh WL, Tu YK, Su JY, Hsu RW. Knee dislocation: treatment of high-velocity knee dislocation. J Trauma. 1999;46:693–701. doi: 10.1097/00005373-199904000-00023. [DOI] [PubMed] [Google Scholar]