Abstract
BACKGROUND
Advanced surgical techniques, such as total laparoscopic hysterectomy, are often challenging to acquire beyond fellowship training programs for practicing obstetrician-gynecologists. A lack of formative data currently exist for continuing medical education programs, limiting our understanding of how improvement in surgical skills and training programs occur.
OBJECTIVE
This study aimed to investigate how practicing obstetrician-gynecologists acting as trainees experience a program that aims to teach them total laparoscopic hysterectomy, and to assess whether their surgical skills improve according to data from formative assessment tools and qualitative data from open-ended survey questions and in-depth interviews.
STUDY DESIGN
We report a process analysis of formative data collected during a pilot implementation trial of a surgical training program targeting practicing obstetrician-gynecologists. Eleven consultant obstetrician-gynecologists and 4 experienced surgical mentors participated in 4 hospitals in Queensland, Australia. Total laparoscopic hysterectomy was performed in 700 patients over the course of the study. A total laparoscopic hysterectomy surgical mentorship training program of 10 training days with up to 3 total laparoscopic hysterectomy procedures per day was performed. Both the obstetrician-gynecologists and the surgical mentor completed a formative assessment questionnaire analyzing the trainee's performance after each surgical procedure. Mentors were formatively assessed by the Structured Training Trainer Assessment Report (STTAR) and at the completion of the study by the mini-STTAR, a summative assessment of quality of mentorship. Obstetrician-gynecologists, mentors, hospital leaders, and surgical administrative staff participated in qualitative interviews about the training program.
RESULTS
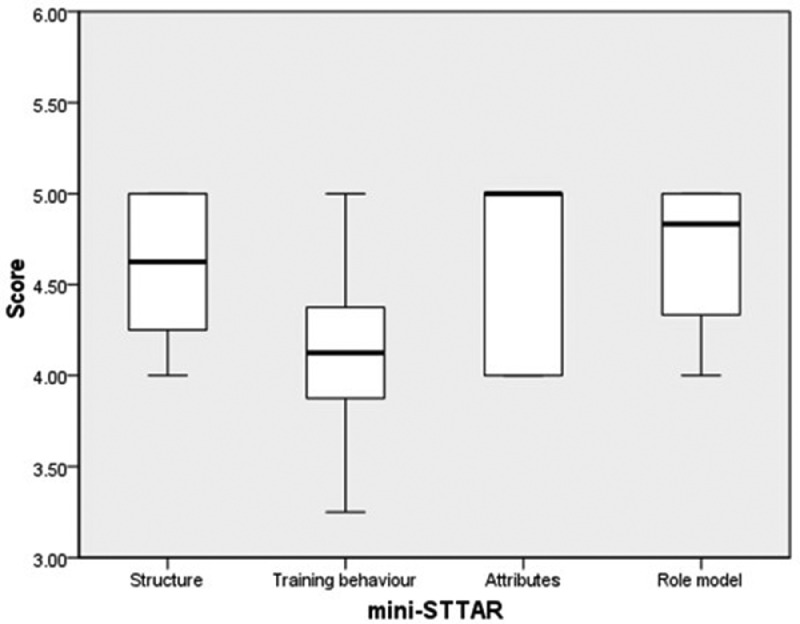
Over time, there was a demonstrated improvement in trainee performance reported by both mentors and trainees in all competency assessment tool domains as the case number increased, with mentors consistently rating trainees’ performance higher than the trainees themselves. Most trainees were satisfied with their mentor in all 31 areas during formative assessment, and at the end of the training, structure, attributes, and role modeling were all rated high (average score >4.5; range, 3.79–5.00), whereas training behavior was rated slightly lower at 4.1 (range, 3.79–4.45). Qualitative interviews demonstrated that the trainees found the training to be a beneficial, hands-on experience.
CONCLUSION
Formative assessment clearly documented improvement in surgical skills during a total laparoscopic hysterectomy training program for consultant obstetrician-gynecologists.
Key words: continuing medical education, gynecology, hysterectomy, laparoscopy, mentoring, surgical education
AJOG Global Reports at a Glance.
Why was this study conducted?
Fully trained consultants often face challenges in acquiring additional surgical skills that were not originally taught to them in their training, especially beyond fellowship training.
Key findings
Review of literature shows that only a very small evidence base exists regarding successful professional development programs and continuing medical education activities to improve surgical skills in faculty obstetrician and gynecologist (O&G) consultants.
What does this add to what is known?
The findings of this training program are valuable given the recognized gaps in the literature. The experiences and skill acquisition of consultant O&G surgeons throughout a surgical training program were evaluated using qualitative data and formative assessment tools to inform future programs beyond traditional training.
Introduction
According to the classic Halstedian apprenticeship model,1 obstetrician-gynecologists (O&Gs) acquire surgical skills by observing others, performing these skills under supervision in practice, and subsequently teaching them to new trainees. Once O&Gs are fully trained consultants, acquiring additional surgical skills beyond the fellowship training program that are originally not taught during their training is often challenging. Continuing medical education (CME) often involves passive learning activities such as lectures, online modules, short workshops during conferences, animal laboratories or cadaver training, but not hands-on surgical training.2,3
Therefore, CME activities are often insufficient to acquire and practice new surgical skills. Evidence shows that the effectiveness of CME interventions is greater with increasing interactivity, number and variety of educational methods, and greater length of intervention,2 including for the acquisition, maintenance, and retention of surgical and procedural skills.3 In some surgical specialties, including obstetrics and gynecology, the greater use of laparoscopy has led to a shift in surgical CME toward simulation.4 Simulation training is beneficial because it allows trainees to acquire skills in a controlled setting of a simulated surgical situation before practicing on patients. However, CME surgical simulation courses are often brief and do not reflect the complexity of major laparoscopic procedures such as total laparoscopic hysterectomy (TLH). Neither the Halstedian apprenticeship model nor short simulation courses address the challenge of acquiring new surgical skills and maintaining them after O&Gs become consultants.
To establish whether novel ways of surgical CME have emerged in the field of obstetrics and gynecology, a review of the literature was conducted, using the search terms included in Additional File 1. Intervention studies focusing on surgical skills acquisition, maintenance, or faculty training, wherein at least 5 O&Gs participated were eligible. The review discovered 9 studies, as summarized in Table 1. Only 2 studies investigated TLH training6,10 whereas 2 others investigated TLH along with other laparoscopic surgical procedures.8,13 Overall, 4 were short-term workshops1,11, 12, 13 and 5 were long-term (from 1 month to 5 years) preceptorship training programs.6, 7, 8, 9, 10 All included studies measured success of the skills training before and after intervention, using assessment tools such as the Objective Structured Assessment of Technical Skills (OSATS)6,11,13 or the Fundamentals of Laparoscopic Surgery (FLS) scale.9 Only 4 studies6,10,11,13 used formative assessment tools throughout the training to tailor the program to the trainees. Four studies5,7,10,13 collected qualitative data from the trainees about their opinions on the training. The qualitative data were collected at various times in these 4 studies, from baseline to the evaluation phase of the training programs. For example, formative assessment was used to improve workshops between sessions in Berkowitz et al5 (2017). In Crouss et al7 (2021), formative tools elicited barriers to performing a certain procedure at baseline. Leung et al10 (2013) and Stefanidis et al13 (2016) used qualitative interviews to evaluate participants’ program satisfaction.
Table 1.
Literature review
| Author | # of preceptors/coaches (gyn) | # of trainees (gyn) | Location | Procedure | Program completion % | Training description | Length of intervention | Number of interventions | Primary outcomes measured | Formative assessment conducted/learning curve? | Qualitative data? | Main results/conclusions |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Berkowitz et al,5 2018 | Unknown | 22 (22) | 1 academic tertiary hospital, United States | TAH | 88% | Surgical skills workshop for TAH | 2 h | 2 separate workshops | Pre/posttest (25 item knowledge test) about steps of TAH+focus group analyses | No | Yes, focus group comments were used and applied for future workshops. | An increase in knowledge of critical TAH surgical steps and analyses identified the need for increased review and training demonstrations of TAH and recommended continued offering of the workshops. |
| Briët et al,6 2010 | 2 | 11 (11) | 8 hospitals (1 university hospital and 7 regional hospitals), Netherlands | TLH | 100% | 1. Instructional video 2. Surgical skills workshop 3. Surgery w/ visiting surgeon present 4. Surgery w/out visiting surgeon |
2 y | 166 patients (83 patients with visiting surgeon+83 after) | OSATS Learning Curve during training+complications during/after competence achieved | Yes | No | “Nine of 11 gynecologists reached the competence score of at least 28 points during the study” AND “The concept of a visiting surgeon for on-site coaching and monitoring of established gynecologists during the learning curve of an advanced laparoscopic procedure using Objectively Structured Assessment of Technical Skills is feasible” |
| Crouss et al,7 2021 | Unknown | 9 (9) | 1 tertiary hospital in the United States | LAVH | NA | 1. Resident education workshops 2. Faculty workshops 3. Surgical mentorship for faculty |
1 mo | 18 cases under surgical mentorship (698 hysterectomies analyzed) | Preintervention survey+demographic, clinical, and outcome data pre/postintervention | No | Yes, anonymous survey indicated the most common barriers to vaginal hysterectomies. | “Postintervention, the proportion of vaginal hysterectomies was higher” AND “Implementation of a multiple-tier intervention was associated with an increase in vaginal hysterectomies.” |
| Cundiff and Geoffrion,8 2016 | 3 pre → 8 post | 33 (33)a | 2 tertiary hospitals, Canada | MIH (LH or VH) | unknown | 1. Interested surgeons submit request 2. Preceptor and trainee are scheduled for cases 3. Trainee is analyzed by preceptor using OSATS 4. Once trainee is determined to be competent by preceptor, they are placed on 1-y probationary period 5. Outcomes are reviewed and recredentialing is based on outcomes |
5 y | Unknown preceptor cases (mean 470 cases per y analyzed) | Longitudinal proportion of surgeons performing MIH, the proportion of MIH to TAH, and proportion of resident LH teaching cases |
No | No | The proportion of surgeons performing 50% of hysterectomies as MIH steadily increased in the first 5 y after implementation. The proportion of resident LH teaching cases increased with a similar rise in the proportion of MIH cases. Contrasting the experience between 2 hospitals revealed that having OR time dedicated to MIH cases provided significantly better results. |
| Hafford et al,9 2013 | NA | 99 (8) | 4 academic hospitals, United States | FLS certification | 73% | 1. Orientation + questionnaire + FLS skills pretests 2. Scores reviewed w/ participants 3. 2-mo period of self-study and practice of manual skills w/ proctors available upon request 4. FLS certification examination (skills+cognitive) 5. Remediation and certification retest 6. Posttest questionnaires |
2 mo | NA | Preintervention and postintervention FLS testing data+questionnaires about curriculum | No | No | 73% completed the entire curriculum, 33% failed baseline skills assessment (3 of them gynecologists). At certification, skills performance had improved. One surgeon (1.3%) failed the skills certification, and 9 (11.8%) failed the cognitive examination (2 of whom were gynecologists). This study demonstrated that FLS certification for practicing surgeons and proficiency verification is feasible. FLS certification may be necessary to ensure surgeon competency. |
| Leung et al,10 2013 | 3 | 9 (9) | 1 tertiary hospital, Australia | TLH | 100% | 1. ½-day weekly training session with a coach for 4 wk following the format of briefing, intraoperative teaching, and debriefing Evaluation component based on OREEM |
1 mo each over 2 y and 8 mo | 51 encounters | Postintervention evaluations (7 based on OREEM) | Yes | Yes | “There was a high degree of satisfaction among participants in the program…Participants felt they gained confidence and improved their surgical skill as a result of the program. The descriptive feedback validated the structured encounter template in facilitating the learning and teaching environment in the operating room. Most participants expressed an intention to adopt a more structured approach in their surgical teaching.“ |
| Palter et al,11 2016 | 1 | 20 (9) | 1 tertiary academic hospital, Canada | Laparoscopic suturing | 90% | 1. Pretest on a box trainer 2. Either conventional or coaching intervention 3. Postintervention test |
1 h | 2 | Comparing pre- and postintervention OSATS scores between intervention groups | Yes | No | “Comparing the pre- and postintervention scores within both groups, there was an improvement in technical proficiency in the peer coaching group, yet none in the conventional training group” AND “This trial demonstrates that a structured peer coaching program can facilitate faculty surgeons learning a novel procedure.” |
| Rossitto et al,12 2012 | unknown | 120 (120) | 1 single institution, Rome, Italy | Box trainer laparoscopic training | 95% | 1. 3-d course w/ box trainer and coaching 2. Live surgery 3. Self-assessment questionnaire |
3 d | NA | Comparing pre- and postintervention questionnaires on the intervention feedback and laparoscopic knowledge | No | No | “The subjective assessment showed an immediate improvement of motor skills.” AND “Laparoscopic training course can improve both theoretical knowledge and motor skills. Such courses result in a short-term subjective improvement.” |
| Stefanidis et al,13 2016 | 3 | 32 (14) | 6 hospitals, United States | TLH (colectomy+cholecystectomy for non-gyn) | 100% | 1. Surgeons recorded a video operating 2. Videos reviewed by an expert and deficiencies identified 3. Surgeons attended a 4.5-h coaching session to target deficiencies |
4.5 h |
1 | Identifying the technical and nontechnical skills most commonly deficient and analyzing the improvement during the coaching session using NOTSS, OSATS, satisfaction surveys | Yes | Yes | “Most surgeons appropriately accomplished some of the objectives of the distraction scenario,...but no participating surgeon was able to achieve expert levels…Participants perceived the coaching sessions as highly valuable.” |
FLS, Fundamentals of Laparoscopic Surgery; gyn, gynecologist; LAVH, laparoscopically assisted vaginal hysterectomy; LH, laparoscopic hysterectomy; MIH, minimally invasive hysterectomy; NA, not applicable; NOTSS, Non-Technical Skills for Surgeons; OR, operating room; OREEM, Operating Room Educational Environment Measure; OSATS, Objective Structured Assessment of Technical Skills; TAH, total abdominal hysterectomy; TLH, total laparoscopic hysterectomy; VH, vaginal hysterectomy.
Reflects the number of gynecologists listed at participating hospitals, although it is unknown how many participated in the program.
Magalski. Experience of practicing obstetrician-gynecologists in a surgical training program. Am J Obstet Gynecol Glob Rep 2023.
This review of literature shows that only a small evidence base exists of successful professional development programs to improve surgical skills in O&G consultants. The lack of formative data from the training programs limits our understanding of how improvement in surgical skill occurs, how trainees perceive training programs and mentoring by the trainers, and what could be improved to enhance their training experience. This study aims to answer some of these evidence gaps by reporting formative data from a surgical training program of TLH for O&G consultants, along with qualitative survey and interview data.
Materials and Methods
This trial was approved by the Royal Brisbane and Women's Hospital Human Research Ethics Committee (Approval HREC/16/QRBW/564) and received site-specific approval by all participating hospitals (NCT03617354). Study participants (practicing O&Gs and medical staff participating in interviews) provided written informed consent. Given that Human Research Ethics Committee approval was obtained, and practicing O&G surgeons (which we herein call participating specialist trainees) were the research participants, patients receiving a hysterectomy were not required to provide informed consent.
This study was part of the Implementation of Minimally Invasive Hysterectomy (IMAGINE) surgical training program for O&G consultants in Queensland, Australia. The primary aim of this pilot trial was to reduce the proportion of patients who receive a total abdominal hysterectomy (TAH) by increasing the proportion of those who may receive a TLH instead.14 Briefly, the training program encompassed multiple sequential steps, as described previously within the published protocol,14 including the introduction of operation theater requirements, explanation of training session, and checking of equipment. Then the surgical mentor supervised the participating specialist trainees in patient positioning and discussed the equipment, setup, and port placement. The surgical mentor acted as the primary surgeon for the first operation and as surgical assistant for the subsequent operations. The involvement of the surgical mentors decreased with the increasing familiarity of participating specialist trainees with the TLH technique. In each hospital, 10 training days were offered with up to 3 TLH procedures performed per day. Surgical outcome results showed that the rate of TLH increased 2-fold during the intervention and remained 12% higher after the intervention.15
Inclusion criteria
Participating specialist trainees were eligible if they were Fellows of the Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) (specialists), competent in laparoscopic surgery (such as laparoscopic ovarian cystectomy without complexity, laparoscopically assisted vaginal hysterectomy [uterine artery taken vaginally] without complexity, and excision of stage 2 endometriosis, oophorectomy, or removal of an ectopic pregnancy), and willing to complete the surgical training program.
To assess the surgical laparoscopic skills of the participating specialist trainees at baseline, an unedited, deidentified video recording of a laparoscopic ovarian cystectomy, oophorectomy, or salpingectomy was assessed by experienced surgical mentors using the Global Operative Assessment of Laparoscopic Skills (GOALS) screening tool. No further baseline data were provided to the surgical mentors. The GOALS tool was used to establish if participating specialist trainees had sufficient skills required to train in TLH in 5 domains, including depth perception, bimanual dexterity, efficiency, tissue handling, and autonomy at baseline.16 Each domain was scored from 1 to 5, with 1, 3, and 5 indicating a descriptive performance task of each domain; for example, for depth perception, 1=constantly overshoots and 5=accurately directs instruments (Additional File 2; Supplemental Table 1). Participating specialist trainees also completed a self-reported questionnaire at the start of the training to assess the reason they wanted to participate in the training program and the main barriers they faced with regard to implementing TLH. Surgical mentors provided a one-on-one session with each participating specialist trainee to initiate the training program, explain study procedures, and demonstrate how to use the database for recording adverse events. All surgical mentors and participating specialist trainees were provided with a copy of the operating procedures and a training manual that describes the practical steps necessary to implement the program. All surgical mentors attended the Train the Trainer workshop by Lapco to standardize their approach to mentoring.17
To be eligible as surgical mentors, they had to be senior laparoscopic surgeons experienced in TAH and TLH with a minimum of 100 TLH procedures, and to have completed a Train the Trainer workshop by the Lapco team.17 The mentors had to have no previous working or personal relationship with the surgical trainees. Each hospital was assigned a surgical mentor, who remained the same throughout the intervention.
Formative assessment of training participating specialist trainees and mentors
During the training, formative assessment was conducted using a tool developed for colorectal laparoscopic surgery and adapted for TLH (Additional File 2; Supplemental Table 2).18 Five skills were assessed for each TLH performed, including exposure, vascular and structure, mobilization, finalizing surgery, and overall performance. A total of 12 consecutive surgical steps were assessed within these 5 key skills. Each step was scored from 1 (“Not performed, step had to be done by trainer”) to 6 (“Proficient performance, could not be better”). Both the participating specialist trainees and the surgical mentors completed the formative assessment questionnaire after each surgical procedure separately. This allowed the participating specialist trainees to identify their strengths and weaknesses and target areas for improvement. It also allowed the surgical mentor to adapt their coaching style by focusing in the next operation on steps that required improvement. Participating specialist trainees completed a questionnaire before and after the training program, reporting their demographic characteristics and satisfaction with the training program.
Evaluation of mentors
Four surgical mentors delivered the TLH training program to the 11 participating specialist trainees at 4 hospitals. Two assessment tools were used to assess the formative and summative quality of the surgical mentoring, including:
-
1.
The formative Structured Training Trainer Assessment Report (STTAR) adapted from Wyles et al19 was completed by the participating specialist trainees; 31 skill assessment criteria of good mentoring were grouped into 3 primary areas of set, dialogue, and closure. Each assessment item was rated from 1 (“Did not happen but should have been done”) to 5 (“Happened perfect amount” or “Not applicable”). We recoded the surgical mentor assessment score by combining 1 and 2 as “Not happy,” 3 and 4 as “Neutral,” and 5 as “Happy with the mentor's performance” (Additional File 2; Supplemental Table 3).
-
2.
Another self-reported questionnaire and the mini-STTAR18 were completed by the participating specialist trainees at the end of the training program to report their overall satisfaction with the program; 21 items were evaluated and categorized into 4 key attributes—structure, training behavior, attributes, and role model (Additional File 2; Supplemental Table 4). Each item was rated from 1 (“strongly disagree”) to 5 (“strongly agree”), with 4 of the items being reverse-coded.
Interviews
We interviewed 3 mentors, 8 participating specialist trainees, and 6 other clinical staff members, including theater nurses, theater booking officers, and anesthetists (average interview, 15 minutes; range, 4–23 minutes). The questions asked about perceived barriers and enablers of the training program and potential improvements. Software NVivo 12 (Lumivero, Denver, CO) was used to analyze the verbatim transcripts. Transcripts were read and reread by 2 researchers independently (C.V.S. and C.H.). The interview questions were used as a priori codes, and additional codes were developed using deductive content analysis. Using a framework approach, themes were then extracted, and compared between the 2 researchers.
Statistical analyses
Descriptive statistical methods were used to summarize survey responses and the formative and summative assessment reports from participating specialist trainees and mentors. The internal consistency of each assessment scale was calculated using the Cronbach alpha. Bland–Altman plots were used to assess whether participating specialist trainees and mentors differed consistently in their formative assessment scores,20 and a linear regression model was used to determine differences in the assessment scores by the trainees and mentors. The comparative skill assessment data were visually presented using box plots.
Results
Characteristics of the participating specialist trainees
Of the 11 participating specialist trainees, 8 (72%) were female, and all were familiar with laparoscopic surgery to conduct diagnostic assessments, ovarian cystectomies, or ectopic pregnancy clearances. According to the GOALS baseline assessment, trainees had excellent depth perception and autonomy when conducting laparoscopy for these procedures, but scores were lower for bimanual dexterity, efficiency, and tissue handling (Additional File 2; Supplemental Figure 1). The most common reasons for participating in the training program reported by the participating specialist trainees at baseline were lack of own surgical skills (72%; 8/11), lack of surgical mentoring (54%; 6/11), and not wanting to be a burden (54%; 6/11).
Formative assessment of trainees by trainees and mentors
In line with the increase of surgical training case numbers, and as the training program progressed, trainee performance improved (Figure 1). The average scores for each of the individual skills rated by mentors and trainees were grouped by case numbers 1 to 3, 4 to 6, 7 to 9, and ≥10, as presented in Table 2. The “exposure” subscale was consistently the best-performing skill area for the participating specialist trainees, whereas the “overall performance” subscale was rated lowest. As shown in the Bland–Altman plot (Supplemental Figure 2), mentors consistently rated the trainees higher than participating specialist trainees themselves by 0.14 points. For example, the mentors’ rating of how well the participating specialist trainees achieved “exposure” increased from 5.09 to 5.84, whereas the same skill rating by participating specialist trainees improved from 4.86 to 5.82 (Table 2).
Figure 1.
Formative assessment by mentors and O&Gs
A, Formative assessment by mentors. B, Formative assessment by O&Gs themselves.
O&G, obstetrician-gynecologist.
Magalski. Experience of practicing obstetrician-gynecologists in a surgical training program. Am J Obstet Gynecol Glob Rep 2023.
Table 2.
Formative assessment of mentors and obstetrician-gynecologists
| Exposure |
Vascular and structures |
Mobilization |
Finalizing surgery |
Overall performance |
|||
|---|---|---|---|---|---|---|---|
| Participant Type | Case groupa | Number of completed questionnaire | Mean (SD) | ||||
| Mentor | 1-3 | 33 | 5.09 (0.74) | 4.32 (0.94) | 4.21 (1.02) | 4.12 (0.75) | 3.82 (1.10) |
| 4-6 | 33 | 5.39 (0.62) | 4.84 (0.95) | 4.42 (1.09) | 4.77 (0.77) | 3.70 (2.13) | |
| 7-9 | 24 | 5.25 (0.72) | 4.56 (0.72) | 4.33 (0.87) | 4.63 (0.50) | 3.58 (1.84) | |
| ≥10 | 14 | 5.84 (0.36) | 5.33 (0.75) | 5.00 (1.04) | 5.00 (0.59) | 4.64 (1.73) | |
| Overall | 104 | 5.32 (0.66) | 4.68 (0.92) | 4.41 (1.03) | 4.56 (0.75) | 3.84 (1.74) | |
| Trainee | 1-3 | 33 | 4.86 (0.74) | 4.09 (1.07) | 4.06 (1.14) | 3.88 (0.95) | 3.48 (1.37) |
| 4-6 | 33 | 5.19 (0.68) | 4.64 (1.04) | 4.30 (1.13) | 4.53 (0.84) | 3.79 (1.69) | |
| 7-9 | 24 | 5.29 (0.63) | 4.60 (0.82) | 4.33 (0.92) | 4.48 (0.70) | 2.79 (2.55) | |
| ≥10 | 14 | 5.82 (0.36) | 5.34 (0.65) | 5.14 (0.95) | 4.69 (0.69) | 4.21(2.32) | |
| Overall | 104 | 5.19 (0.71) | 4.55 (1.02) | 4.35 (1.10) | 4.36 (0.90) | 3.52 (1.95) | |
Overall reliability: Cronbach alpha: 0.93. For mentors: Cronbach alpha: 0.93. For trainees: Cronbach alpha: 0.93.
Trainees and mentors individual consecutive cases were split into four surgical groups.
Magalski. Experience of practicing obstetrician-gynecologists in a surgical training program. Am J Obstet Gynecol Glob Rep 2023.
Formative assessment of mentor
Table 3 and Figure 2 demonstrate the evaluation of the mentors’ teaching skills by the participating specialist trainees for 100 of the training cases. Most participating specialist trainees were satisfied with their mentor, including mentors being rated as “patient” (99/100), “non-threatening” (99/100), “excellent role model” (99/100), and “overall an excellent trainer” (73/100). According to the participating specialist trainees’ assessment scores of “not happy” or “neutral,” mentoring skills most in need of improvement involved the mentor being “controlling” (28/99), “taking over” (23/98), “questioning” (23/99), and “pushing the trainee out of their comfort zone” (20/100).
Table 3.
Formative assessment of the 4 mentors by the obstetrician-gynecologists for 100 cases completed during the training program
| Skills | Skills assessment criteria | Not happy | Neutral | Happy | Not applicable |
|---|---|---|---|---|---|
| Set | 1. Determines background knowledge | 2 | 12 | 81 | 5 |
| 2. Defines aims | 4 | 9 | 82 | 5 | |
| 3. Discusses case-specific information | 1 | 14 | 82 | 3 | |
| 4. Aligns agenda (n=99) | 2 | 7 | 82 | 6 | |
| 5. Establishes ground rules | 0 | 14 | 80 | 6 | |
| 6. Communicates with team | 0 | 1 | 96 | 2 | |
| 7. Ensures patient safety (n=98) | 0 | 3 | 92 | 3 | |
| Dialogue | 8. Guiding/deconstructing (eg, “the next step is...”) (n=99) | 0 | 11 | 88 | 0 |
| 9. Directions (eg, “ok, move your grasper to… go in a bit...”) (n=97) | 0 | 9 | 88 | 0 | |
| 10. Questioning (eg, “what would you do next”?) (n=99) | 6 | 17 | 76 | 0 | |
| 11. Clarifying (eg, “why are you doing that?”) (n=99) | 5 | 14 | 80 | 0 | |
| 12. Encouragement/praise (n=98) | 1 | 4 | 93 | 0 | |
| 13. Informing (eg, general information about disease/setup) (n=99) | 0 | 16 | 80 | 3 | |
| 14. Corrective feedback (eg, “if you grab that you'll get better traction”) | 0 | 5 | 95 | 0 | |
| 15. Warning (eg, “if you do that you may injure the small bowel”) | 1 | 19 | 77 | 3 | |
| 16. Controlling (eg, “stop”) (n=99) | 1 | 27 | 69 | 2 | |
| 17. Pushes trainee/takes them out of their comfort zone | 4 | 16 | 77 | 3 | |
| 18. Calm | 1 | 0 | 99 | 0 | |
| 19. Patient | 1 | 0 | 99 | 0 | |
| 20. Comfortable in silence (n=99) | 1 | 1 | 97 | 0 | |
| 21. Nonthreatening | 1 | 0 | 99 | 0 | |
| 22. Communicates clearly (n=99) | 1 | 0 | 98 | 0 | |
| 23. Takes over (n=98) | 0 | 23 | 69 | 6 | |
| Closure | 24. Critiques performance | 2 | 4 | 94 | 0 |
| 25. Asks trainee's opinion | 0 | 9 | 90 | 0 | |
| 26. Encourages reflection | 1 | 6 | 92 | 1 | |
| 27. Honest | 0 | 2 | 98 | 0 | |
| 28. Approachable | 0 | 0 | 100 | 0 | |
| 29. Seeks feedback | 4 | 8 | 87 | 1 | |
| 30. Behaves like an excellent role model | 0 | 1 | 99 | 0 | |
| 31. Develops learning point agreement (n=99) | 1 | 4 | 94 | 0 | |
| Overall is an excellent trainer (n=84) | Agree, n=11 (13.1) Strongly agree, n=73 (86.9) |
||||
Total items: 31. Reliability: Cronbach alpha: 0.848.
Magalski. Experience of practicing obstetrician-gynecologists in a surgical training program. Am J Obstet Gynecol Glob Rep 2023.
Figure 2.
Mini-STTAR domain ratings of the training mentor completed by trainees*
*N=11.
O&G, obstetrician-gynecologist; STTAR, Structured Training Trainer Assessment Report.
Magalski. Experience of practicing obstetrician-gynecologists in a surgical training program. Am J Obstet Gynecol Glob Rep 2023.
At the end of the training, the mentors’ structure, attributes, and role modeling were all rated high (average score >4.5; range, 3.79–5.00), whereas training behavior was lower at 4.1 (range, 3.79–4.45) (Figure 2). Details of the scoring system are provided in Additional File 2 and Supplemental Table 4.
Trainee and other medical staff interviews
The benefits of the IMAGINE training program identified by participating specialist trainees included: hands-on, supportive teaching style; positive learning experience; completion within their own hospital setting; and benefits to patients. Overall, most would recommend the training program to others and believe it should be implemented in other hospitals: “I think laparoscopic hysterectomy is going to be the gold standard type of hysterectomy in the coming years.” They appreciated the stepwise guidance by trainers, with more support at the beginning, and opportunity to operate independently at the end. The hands-on approach throughout the program helped to solidify their didactic learning experiences: “In a course, you normally observe. You don't do anything.”
After the first day of the trial, immediate patient outcomes were noticed: “Even after the first IMAGINE day, where most of the operations took 3 hours and then patients went home the next day. I mean, that was fantastic.” The participating specialist trainees were enthusiastic to transfer their skills onto their registrars: “We really enjoyed it [the training] because we really thought that there was a need for us to train, so that then we can train our surgeon trainees.”
Barriers identified included region-related issues, trial implementation issues, and insufficient eligible patients. In regional hospital settings, they reported sometimes low continuity of theater team when trying to roster the same staff during TLH training. Other implementation issues included logistic issues, such as delays with ordering supplies and equipment.
Suggestions for improving the training included: (1) implementing anonymous feedback, given that the trainees were required to hand in their evaluations to the mentor themselves; (2) the need for further educational opportunities after the training is completed; (3) inclusion of registrars as surgical trainees in the program; (4) improved allocation of number of surgical trainees, to fit number of patients to ensure sufficient opportunities to practice; (5) more opportunities for reflection with other participants in the training program to share experiences; and (6) training resources such as videos of the trainers conducting TLH in their own hospitals, to prepare the surgical trainees regarding expectations.
Mentor interviews
Benefits identified by mentors included the involvement of highly engaged participating specialist trainees. Barriers to participating identified by mentors included the high time commitment required for them to provide the training, difficulties with administrative trial procedures, and inconvenience of traveling to rural areas, including limited flight options. Mentors also identified that there were not enough surgical cases for some participants. Suggestions for improving training included providing trainee resources for use after the trial (eg, videos that they can refer back to) and increasing the number of mentors at each hospital from 1 to 2.
Comment
Principal findings
The objective of the IMAGINE pilot trial was to formally test a surgical training model to equip O&G consultants with the surgical skills to provide TLH as an alternative to TAH. This study showed that implementation of a 10-week training program for practicing O&G consultants in their own hospital is feasible and safe, improved their skills as self-reported by the participating specialist trainees and reported by mentors, and led to an increase in the proportion of hysterectomies completed laparoscopically. The rate of TLH increased 2-fold during the intervention and remained 12% higher after the intervention, as previously reported.15 The outcomes of this report add to the experiences of specialist trainees and mentors in a surgical training program. The formative assessment tools were useful for understanding the progression of skill acquisition over time, and the potential self-criticism or lack of self-confidence of participating specialist trainees regarding their skills, given that they rated their own skills consistently lower than their mentors did.
Our review demonstrated a lack of research on the topic of surgical skill acquisition in CME in the field of obstetrics and gynecology. The review discovered that only 9 studies investigated the acquisition and maintenance of surgical skills in specialists after training. Out of those 9, only 2 studies investigated the acquisition of advanced laparoscopic skills for TLH specifically,6,10 whereas 2 others investigated TLH along with other laparoscopic surgical procedures.8,13 Similarly to this study, the 9 examined studies all demonstrated some improvement in mentees’ surgical skills with their interventions. Comparing the qualitative data, Leung et al10 (2013) similarly reported high satisfaction with their coaching intervention, with comments stating improvement of confidence and surgical skills. Stefanidis et al13 (2016) used blinded group sessions where deidentified videos were reviewed as a group. The qualitative data revealed that participants found the anonymity and group discussion valuable for reviewing others’ mistakes and successes.13 This aligns with the qualitative data from this study suggesting the option of anonymous evaluation and more opportunities to reflect as a group. Given the lack of research on this topic, this study adds valuable data that could be used in the planning of future training programs.
Clinical implications
Before the start of the training programs, trainees already had excellent depth perception and autonomy but lacked bimanual dexterity, efficiency, and tissue handling. The formative assessment showed that exposure was consistently the best-performing skill area for the participating specialist trainees, whereas overall performance was rated the lowest. This indicates that these skills seem to take longer than others in their uptake and will require added focus in future training programs.
Regarding the formative assessment of the mentors, participating specialist trainees reported that mentoring was not as effective when the mentor was controlling or took over the surgery, and that they appreciated a calm, patient, and approachable mentor. Participating specialist trainees strongly agreed that their surgical mentors were excellent during 73 out of 100 rated cases. At the end of the training according to the mini-STTAR, the mentors’ skills regarding providing structure, good mentoring attributes, and role modeling were rated higher than their overall training behavior. This indicates that more investigation needs to be done on how to improve mentors’ teaching practices and behavior in the theater to facilitate a better learning environment for acquiring new skills as a consultant. The qualitative data collected provided some insights on how to improve future training programs, including ascertaining an optimal case load for each training participant and making it easy for mentors to undertake their demanding tasks by reducing their administrative burden as much as possible.
Limitations
The limitations of this study include the potential for response bias given that the formative assessment of the mentor by the trainee was often conducted in the presence of the mentor. The trainees might have feared that a negative assessment of the mentor could have affected the working relationship. This could be reflected in the observation that the mini-STTAR completed at the end of the training program demonstrated a lower rating of training behavior compared with the formative assessment of the mentors during the program.
Conclusion
This study suggests that the model of training consultant O&Gs in their own hospital is valuable, and could be implemented in a larger-scale training program with more participants and mentors, as well as transferred for the training of skills other than TLH. This is important as the pace of innovation in surgery increases and more O&Gs require upskilling while practicing their profession.
Acknowledgments
We thank the Implementation of Minimally Invasive Hysterectomy (IMAGINE) project managers at the Queensland Centre for Gynaecological Cancer, including Anne Hughes, BSc and Trudi Cattley, BAppSc.
Footnotes
A.O. reports grants, personal fees, and other funding from SurgicalPerformance Pty Ltd, and grants from Medtronic. A.O. also reports consultancy fees from Baxter Healthcare Australia and New Zealand and AstraZeneca Australia, not directly related to the subject of this article. In addition, A.O. has a trademark licensed to SurgicalPerformance Pty Ltd. The other authors report no conflict of interest.
This work was supported by research grants totaling >$1 million AUD. This included the National Health and Medical Research Council (NHMRC) Partnership Project for Better Health grant (1145961) and the Cherish Women's Cancer Foundation. M.J. was supported by an NHMRC Translating Research into Practice Fellowship (1151021). The work has received an unrestricted grant from Medtronic as an industry partner, which also provided in-kind support for equipment. This work received seed funding from Metro North Hospital and Health Service and from the Australian Centre For Health Services Innovation (AusHSI). The funders did not have any role in the conduct of the study or reporting of outcomes.
This trial was approved by the Royal Brisbane and Women's Hospital Human Research Ethics Committee (approval number HREC/16/QRBW/564) and received site-specific approval by all participating hospitals (NCT03617354). Study participants (obstetrician-gynecologists, those who participated in interviews) provided written informed consent. Given that Human Research Ethics Committee approval was obtained, and practicing obstetrician-gynecologist surgeons were the research participants, patients receiving a hysterectomy were not required to provide informed consent.
Cite this article as: Magalski GR, Obermair A, Hanna GB, et al. Experience of practicing obstetrician-gynecologists in a surgical training program in total laparoscopic hysterectomy. Am J Obstet Gynecol Glob Rep 2023;XX:x.ex–x.ex.
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.xagr.2023.100249.
Appendix. Supplementary materials
References
- 1.Romero P, Günther P, Kowalewski KF, et al. Halsted's “See One, Do One, and Teach One” versus Peyton's Four-Step Approach: a Randomized Trial for Training of Laparoscopic Suturing and Knot Tying. J Surg Educ. 2018;75:510–515. doi: 10.1016/j.jsurg.2017.07.025. [DOI] [PubMed] [Google Scholar]
- 2.Cervero RM, Gaines JK. The impact of CME on physician performance and patient health outcomes: an updated synthesis of systematic reviews. J Contin Educ Health Prof. 2015;35:131–138. doi: 10.1002/chp.21290. [DOI] [PubMed] [Google Scholar]
- 3.Moulton CE, Dubrowski A, Macrae H, Graham B, Grober E, Reznick R. Teaching surgical skills: what kind of practice makes perfect?: a randomized, controlled trial. Ann Surg. 2006;244:400–409. doi: 10.1097/01.sla.0000234808.85789.6a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gorman PJ, Meier AH, Rawn C, Krummel TM. The future of medical education is no longer blood and guts, it is bits and bytes. Am J Surg. 2000;180:353–356. doi: 10.1016/s0002-9610(00)00514-6. [DOI] [PubMed] [Google Scholar]
- 5.Berkowitz LR, James K, Petrusa E, York-Best C, Kaimal AJ. New challenges for a core procedure: development of a faculty workshop for skills maintenance for abdominal hysterectomy. J Surg Educ. 2018;75:942–946. doi: 10.1016/j.jsurg.2017.12.007. [DOI] [PubMed] [Google Scholar]
- 6.Briët JM, Mourits MJ, Kenkhuis MJ, van der Zee AG, de Bock GH, Arts HJ. Implementing an advanced laparoscopic procedure by monitoring with a visiting surgeon. J Minim Invasive Gynecol. 2010;17:771–778. doi: 10.1016/j.jmig.2010.05.011. [DOI] [PubMed] [Google Scholar]
- 7.Crouss T, Sharma S, Smith D, Hunter K, Perry R, Lipetskaia L. Vaginal hysterectomy rates before and after implementation of a multiple-tier intervention. Obstet Gynecol. 2021;137:641–647. doi: 10.1097/AOG.0000000000004318. [DOI] [PubMed] [Google Scholar]
- 8.Cundiff GW, Geoffrion R. An assessment of the continuing surgical Education Program, a surgical preceptor program for faculty members. J Obstet Gynaecol Can. 2016;38:1053–1060. doi: 10.1016/j.jogc.2016.09.005. [DOI] [PubMed] [Google Scholar]
- 9.Hafford ML, Van Sickle KR, Willis RE, et al. Ensuring competency: are fundamentals of laparoscopic surgery training and certification necessary for practicing surgeons and operating room personnel? Surg Endosc. 2013;27:118–126. doi: 10.1007/s00464-012-2437-7. [DOI] [PubMed] [Google Scholar]
- 10.Leung Y, Salfinger S, Tan JJ, Frazer A. The introduction and the validation of a surgical encounter template to facilitate surgical coaching of gynaecologists at a metropolitan tertiary obstetrics and gynaecology hospital. Aust N Z J Obstet Gynaecol. 2013;53:477–483. doi: 10.1111/ajo.12116. [DOI] [PubMed] [Google Scholar]
- 11.Palter VN, Beyfuss KA, Jokhio AR, Ryzynski A, Ashamalla S. Peer coaching to teach faculty surgeons an advanced laparoscopic skill: a randomized controlled trial. Surgery. 2016;160:1392–1399. doi: 10.1016/j.surg.2016.04.032. [DOI] [PubMed] [Google Scholar]
- 12.Rossitto C, Gagliardi ML, Fagotti A, Fanfani F, Gallotta V, Scambia G. Teaching and training in laparoscopic surgery: experience of Catholic Laparoscopy Advanced Surgery School in the basic gynecological surgery. Arch Gynecol Obstet. 2012;285:155–160. doi: 10.1007/s00404-011-1940-8. [DOI] [PubMed] [Google Scholar]
- 13.Stefanidis D, Anderson-Montoya B, Higgins RV, et al. Developing a coaching mechanism for practicing surgeons. Surgery. 2016;160:536–545. doi: 10.1016/j.surg.2016.03.036. [DOI] [PubMed] [Google Scholar]
- 14.Obermair A, Armfield NR, Graves N, et al. How to train practising gynaecologists in total laparoscopic hysterectomy: protocol for the stepped-wedge IMAGINE trial. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2018-027155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Obermair A, Hanna GB, Gebski V, et al. Feasibility and Safety of a Surgical Training Program in Total laparoscopic hysterectomy: results of a pilot trial. Aust NZ J Obstet Gynaecol. In press. [DOI] [PubMed]
- 16.Vassiliou MC, Feldman LS, Andrew CG, et al. A global assessment tool for evaluation of intraoperative laparoscopic skills. Am J Surg. 2005;190:107–113. doi: 10.1016/j.amjsurg.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 17.Lapco. Lapco Consultancy. 2023. Available at: https://www.lapco-international.com/. Accessed January 23, 2023.
- 18.Miskovic D, Ni M, Wyles SM, et al. Is competency assessment at the specialist level achievable? A study for the national training programme in laparoscopic colorectal surgery in England. Ann Surg. 2013;257:476–482. doi: 10.1097/SLA.0b013e318275b72a. [DOI] [PubMed] [Google Scholar]
- 19.Wyles SM, Miskovic D, Ni Z, et al. Development and implementation of the Structured Training Trainer Assessment Report (STTAR) in the English National Training Programme for laparoscopic colorectal surgery. Surg Endosc. 2016;30:993–1003. doi: 10.1007/s00464-015-4281-z. [DOI] [PubMed] [Google Scholar]
- 20.Doğan NÖ. Bland-Altman analysis: a paradigm to understand correlation and agreement. Turk J Emerg Med. 2018;18:139–141. doi: 10.1016/j.tjem.2018.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.