Abstract
Background
Cognitive appraisals play a fundamental role in mental health outcomes following exposure to trauma. Appraisals influence emotional reactions, coping responses, and adaptation to stress and represent a modifiable factor that can serve as a central focus for intervention. Most studies have primarily focused on the role of dysfunctional cognitions in the persistence of posttraumatic stress disorder (PTSD). In this study, we extend research in this area by investigating the role of problem-solving appraisal, an adaptive cognitive strategy, in the association between stress and PTSD.
Methods
A total of 322 participants completed the Perceived Stress Scale, the problem-solving inventory (PSI), and the PTSD Checklist for DSM-5. Descriptive statistics were generated, and intercorrelations and mediation analysis were performed.
Results
Problem-solving confidence and personal control partially mediated the relationship between stress and PTSD. However, contrary to existing research, the approach-avoidance style, which is a subscale of the PSI, did not mediate the relationship between these variables.
Conclusion
Interventions for PTSD should incorporate a complementary focus on developing and increasing adaptive cognitions pertaining to personal control and confidence in problem-solving abilities. This could potentially form part of a broader process of rebuilding the individual's cognitive worldview following exposure to trauma.
Keywords: mediation, problem-solving appraisal, perceived stress, posttraumatic stress disorder, COVID-19, South Africa
Introduction
Empirical evidence compellingly suggests that cognitive appraisals play a pivotal role in mental health outcomes. Assessing and evaluating life events have significant implications for emotional responses, coping behaviors, and positive or negative adaptation to adverse events. 1 According to the seminal theory of stress and coping of Lazarus and Folkman, 1 cognitive appraisals in stress responses are divided into primary appraisals, which entail an immediate assessment of whether the stressor threatens one's well-being or goals, and secondary appraisals, which entail an evaluation of the individual's ability to cope with the stressor and the internal (e.g., sense of coherence) and external (e.g., financial resources and social support) resources available to them. Most research on cognitive appraisals has focused on the role of dysfunctional cognitions in the onset and maintenance of mental health disorders.2,3 For example, consistent findings have indicated that appraisals of loss of a vital investment (e.g., a romantic relationship or job opportunity) and of the self as being deficient and unworthy underlie depression, 4 whereas dysfunctional appraisals regarding one's ability to cope with or personally influence negative events are associated with the persistence of generalized anxiety disorder. 5 According to studies on suicidality,6,7 negative subjective appraisals of social problem-solving ability and negative perceptions of the availability of social support predict suicidal ideation. In posttraumatic stress disorder (PTSD), significant differences in appraisals have been found to account for the persistence of the disorder following exposure to traumatic events. 8 According to cross-sectional and prospective longitudinal studies of PTSD9,10 following exposure to different types of traumatic events, problematic appraisals of trauma and its sequelae, as well as perceptions of ongoing threat, perpetuate post-trauma symptomology. Negative appraisals of personal vulnerability and future harm have also been found to account for unique variances in PTSD. 11
Although many studies have explored negative appraisals, only a few studies have investigated the protective role of adaptive appraisals in mental health outcomes. Adaptive appraisals are not simply the absence of maladaptive cognitions but are rather specific thoughts and beliefs that positively influence outcomes. 3 According to the seminal study of Beck et al. 12 on cognitive therapy, psychological distress is determined by the interplay between negative appraisals of adverse events and positive appraisals of personal control (PC) and coping ability. The presence of positive or adaptive cognitions can help individuals tolerate negative appraisals or re-appraise situations in a way that facilitates coping. For example, benevolent religious re-appraisals of stressful circumstances, as a valuable learning opportunity, have been found to aid coping among young adults [8]. Empirical support for the role of adaptive appraisals has largely been derived from research on self-efficacy, which is defined as the belief that one can effectively cope with adverse events. Shahrour and Dardas 13 reported that self-efficacy significantly predicted psychological distress and acute stress disorder among nurses during the COVID-19 pandemic. Self-efficacy has also been reported to partially mediate the relationship between cyber-victimization and depression. 14 Luberto et al. 15 examined the relationship between mindfulness and emotional dysregulation and found that low coping self-efficacy predicted high emotional dysregulation among adults.
In this study, we investigated the role of self-appraised problem-solving ability in the relationship between stress and PTSD in a sample of South African university students. Self-appraised problem-solving ability refers to an individual's appraisal of their own ability to solve problems and effectively respond to stressors, and it entails a secondary appraisal process. 16 The majority of studies on the construct of problem-solving have focused on problem-solving ability, which refers to an individual's capacity to effectively and efficiently use internal and external resources to cope with stressors. Problem-solving ability entails both cognitive and behavioral processes including understanding the nature of the problem, generating and assessing possible solutions to the problem, evaluating the resources available to cope, and implementing strategies and assessing their effectiveness in managing the problem. Furthermore, existing studies17,18 have predominantly investigated the association between problem-solving ability and mental health or psychological adjustment, since deficits in this area confer a risk for depression, suicidality, and physical health problems. Comparatively fewer studies have investigated the role of self-appraised problem-solving ability in mental health outcomes. Furthermore, a significant portion of studies on problem-solving appraisal has been conducted in the late 20th century (i.e., 1970-1999), and there is a need for additional research in this area. For example, Elliott et al. 19 studied psychological adjustment following spinal cord injury and discovered that higher self-appraised problem-solving ability was associated with lower levels of depressive behavior and psychosocial impairment. Kerns et al. 20 investigated patients with chronic pain and reported that decreased self-appraised problem-solving ability was associated with increased pain, depression, and disability. In a study exploring the association between problem-solving skills and suicidality by examining the role of problem-solving appraisal, Dixon et al. 21 discovered that reduced problem-solving appraisal independently predicted suicidal ideation and hopelessness.
PTSD develops in response to exposure to traumatic events and is characterized by symptoms of intrusive re-experiencing (e.g., flashbacks and nightmares of the trauma), physiological hyper-arousal, changes in cognition and mood, and cognitive and behavioral avoidance strategies. 8 Evidence suggests that university students are at an increased risk of experiencing traumatic events, with exposure rates ranging from 48% to 95%, thus placing them at a risk of developing PTSD.22,23 In South Africa, McGowan and Kagee 24 investigated the prevalence of 14 potentially traumatic events among university students and discovered that approximately 90% of the sample reported exposure to 1 or more traumatic events in their lifetime. In a more recent study, Padmanabhanunni 25 reported a prevalence rate of 97.6% for trauma exposure among a sample of students. They reported that physical assault, transportation accidents, and sexual assault were the most common types of trauma. Bryant 26 reported that, despite the high prevalence of exposure to trauma, a significant proportion of the population did not develop PTSD. These findings highlight the potential role of adaptive appraisals that may confer protection by buffering the impact of dysfunctional cognitions or facilitating their re-appraisal. Furthermore, a core emotional response implicated in the persistence of PTSD is helplessness and powerlessness, which are evoked by appraisals of not being able to respond effectively (i.e., problem-solve) in the context of the traumatic event. 27 Hence, appraisals of problem-solving ability may be a central component in the persistence of the disorder and have implications for intervention. In this study, we hypothesize that the dimensions of problem-solving appraisal (problem-solving confidence (PSC), PC, and approach-avoidance style (AAS)—see “Instruments for descriptions”) would mediate the relationship between perceived stress and PTSD.
Methods
Participants and Procedure
The study sample consisted of 322 university students who chose to respond to an invitation that was sent to a randomly selected sample of 1500 students from a higher educational institution located in the Western Cape in South Africa. The response rate was 21.5%, which resulted in a margin of error of 5.31% (95% confidence interval [CI]). An electronic survey was conducted with the instruments described below using Google Forms and distributed to the participants for completion online. The majority of the sample were women (77%) who lived in an urban area (87.3%). The mean age of the sample was 26.01 years (SD = 10.19). Most of the participants were vaccinated against COVID-19 (86.6%), and 40.7% had experienced the loss of a family member due to COVID-19.
Instruments
The electronic survey included the perceived stress scale (PSS), 28 the problem-solving inventory (PSI), 29 and the PTSD Checklist for DSM-5 (PCL-5). 30 Given the length of the survey, only a brief demographic questionnaire was included.
The PSS is a 10-item measure of perceived stress that uses a 5-point scale ranging from 0 (Never) to 4 (Very often). A sample item is “In the last month, how often have you felt nervous and stressed?” Cohen 28 reported satisfactory reliability estimates (α = 0.84–0.86) in 3 different samples and provided evidence of validity through correlations between perceived stress and life-event scores and depressive and physical symptomatology, among other factors.
The PSI is a 32-item measure of participants’ appraisal of themselves as effective or ineffective problem-solvers. It uses a 6-point scale ranging from 1 (Strongly agree) to 6 (Strongly disagree). The PSI consists of 3 subscales: PSC, AAS, and PC. PSC refers to a participant's confidence in their problem-solving abilities (e.g., “I have the ability to solve most problems, even though initially no solution is immediately apparent”). AAS describes the general disposition to approach or avoid problem-solving tasks (e.g., “After I solve a problem, I do not analyze what went right and what went wrong”). PC describes a participant's belief in their control over their own behaviors and emotions while solving problems (e.g., “Sometimes I do not stop and take time to deal with my problems but just kind of muddle ahead”). In the PSI, high scores reflect self-appraised ineffective problem-solving. Heppner 29 reported an internal consistency coefficient of 0.90 for the total scale, with subscale reliabilities ranging between 0.72 and 0.85. Validity was also established through the relationship between problem-solving appraisal and a participant's rating of their problem-solving skills, as well as the ability of the PSI to differentiate between participants who had received training in problem-solving skills and those who had not. In South Africa, the reliability coefficients for the PSI range between 0.83 and 0.89.31–33
The PCL-5 is a 20-item assessment tool used to evaluate the severity and presence of PTSD symptoms. It is scored on a 5-point scale that ranges from 0 (not at all) to 4 (extremely). A sample item from the PCL-5 is “How much have you been bothered by repeated, disturbing dreams of the stressful experience?” Blevins et al. 30 reported estimates of internal consistency of 0.94 and 0.95 for 2 distinct samples of college students. They also provided evidence of validity through correlations between the PCL-5 and other measures of PTSD and depression. In South Africa, Padmanabhanunni and Wiid 34 reported an estimate of internal consistency of 0.93 for the PCL-5.
Ethics
This study was conducted in accordance with the guidelines outlined by the Declaration of Helsinki and was approved by the Humanities and Social Sciences Ethics Committee of the University of the Western Cape (ethics reference number: HS22/2/9, February 2022). Participation was voluntary, and no incentives were offered for participation. The participants completed the survey anonymously and provided informed consent on the landing page of the survey link.
Data Analysis
All statistical analyses were performed using IBM SPSS Statistics version 28 for Windows (IBM Corp., Armonk, NY, USA). Descriptive statistics (means and standard deviations), intercorrelations between study variables (Pearson's r), and estimates of internal consistency (α and ω) were examined, and a mediation analysis was conducted. Coefficient ω was obtained using the OMEGA macro in SPSS. 35 A mediation analysis was conducted using the PROCESS macro written by Hayes for SPSS. 36 The significance of the indirect effects of perceived stress on PTSD was evaluated using bootstrapped 95% CIs. The results indicated that gender and age were associated with perceived stress, problem-solving appraisal, and PTSD (as reported in the “Results” section). Therefore, they were included as covariates in the mediation analysis. A post-hoc power analysis specifying a medium effect size and α = 0.05 indicated that the achieved power was 0.99.
Results
Table 1 presents the descriptive statistics, reliabilities, and intercorrelations between the variables. All scales demonstrated satisfactory reliability (α and ω = 0.71–0.94). Perceived stress positively correlated with PTSD (r = 0.67, p < 0.001), PSC (r = 0.54, p < 0.001), AAS (r = 0.32, p < 0.001), and PC (r = 0.52, p < 0.001). Except for the correlation between perceived stress and AAS, all coefficients represented a large effect. However, the AAS represented a medium effect. Therefore, high levels of perceived stress were associated with high levels of PTSD. By contrast, high levels of perceived stress were associated with low confidence in problem-solving ability, an avoidant problem-solving style, and the absence of PC during problem-solving, with higher scores on the PSI reflecting more negative appraisals of problem-solving ability.
Table 1.
Intercorrelations, descriptive statistics, and reliabilities of the study variables.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1. Perceived stress | — | |||||
| 2. PTSD | 0.673** | — | ||||
| 3. PSC | 0.537** | 0.487** | — | |||
| 4. AAS | 0.323** | 0.285** | 0.595** | — | ||
| 5. PC | 0.512** | 0.507** | 0.530** | 0.504** | — | |
| 6. Problem-solving appraisal | 0.517** | 0.475** | 0.855** | 0.893** | 0.729** | — |
| Mean | 23.89 | 38.46 | 29.90 | 48.43 | 19.52 | 97.85 |
| SD | 6.28 | 18.98 | 8.37 | 10.59 | 4.99 | 20.25 |
| Alpha | 0.85 | 0.94 | 0.85 | 0.79 | 0.71 | 0.89 |
| Omega | 0.86 | 0.94 | 0.85 | 0.81 | 0.71 | 0.89 |
Abbreviations: AAS, approach-avoidance style; PSC, problem-solving confidence; PTSD, posttraumatic stress disorder; PC, personal control; SD, standard deviation.
** p < 0.001.
Significant gender differences were found for some variables. For instance, women reported higher levels of perceived stress (M = 24.25, SD = 6.14) than those reported by men (M = 22.26, SD = 6.47, t = 2.33, p = 0.02). Additionally, women reported lower levels of PC (M = 19.81, SD = 4.86) than those reported by men (M = 18.21, SD = 5.20, t = 2.37, p = 0.02). Age negatively correlated with all variables (perceived stress: r = −0.32, p < 0.001; PTSD: r = −0.29, p < 0.001; PSC: r = −0.31, p < 0.001; AAS: r = −0.22, p < 0.001; and PC: r = −0.33, p < 0.001).
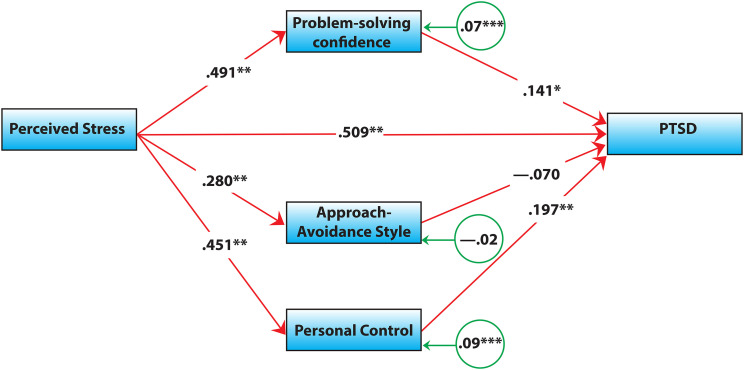
Table 2 presents the direct and indirect effects of perceived stress and the direct effects of the dimensions of problem-solving appraisal. All indirect effects, except for those of AAS, were significant:
- PSC partially mediated the relationship between perceived stress and PTSD (β = 0.07, 95% CI [0.04, 0.40]).
- PC partially mediated the relationship between perceived stress and PTSD (β = 0.09, 95% CI [0.11, 0.44]).
- AAS did not mediate the relationship between perceived stress and PTSD (β = −0.05, 95% CI [−0.17, 0.02]).
Table 2.
Direct and indirect effects of perceived stress and problem-solving appraisal on PTSD.
| Effect | B | SE | 95% CI | β | p |
|---|---|---|---|---|---|
| Direct effects | |||||
| Stress → PTSD | 0.72 | 0.06 | [0.59, 0.84] | 0.51 | <0.001 |
| Problem-solving appraisal → PTSD | 0.15 | 0.05 | [0.06, 0.24] | 0.16 | <0.001 |
| PSC → PTSD | 0.32 | 0.13 | [0.07, 0.57] | 0.14 | 0.013 |
| AAS → PTSD | −0.13 | 0.09 | [−0.30, 0.06] | −0.07 | 0.18 |
| PC → PTSD | 0.75 | 0.20 | [0.36, 1.14] | 0.20 | <0.001 |
| Indirect effects | |||||
| Stress → problem-solving appraisal → PTSD | 0.23 | 0.15 | [0.07, 0.38] | 0.08 | — |
| Stress → PSC → PTSD | 0.21 | 0.09 | [0.04, 0.40] | 0.07 | — |
| Stress → AAS → PTSD | −0.05 | 0.05 | [−0.17, 0.02] | −0.02 | — |
| Stress → PC → PTSD | 0.27 | 0.08 | [0.11, 0.44] | 0.09 | — |
Abbreviations: AAS, approach-avoidance style; PTSD, posttraumatic stress disorder; SE, standard error; CI, confidence interval; PC, personal control; PSC, problem-solving confidence.
The direct effects of PSC (β = 0.14, p = 0.013) and PC (β = 0.20, p < 0.001) on PTSD were significant. Figure 1 shows the results obtained using the PROCESS macro.
Figure 1.
Visual representation of the mediating role of problem-solving appraisal.
Note. All coefficients are standardized. The circles indicate indirect effects. ** p < 0.001; * p < 0.05; *** evaluated with 95% confidence intervaals (CIs).
Discussion
Dysfunctional cognitive appraisals have consistently been identified as strong predictors of psychological adjustment following exposure to trauma. 26 However, only a few studies have investigated the role of adaptive cognitive appraisals in the relationship between stress and PTSD. In this study, we addressed this gap by investigating the role of self-appraised problem-solving ability in the relationship between stress and PTSD in a sample of university students.
First, we discovered that PSC partially mediated the relationship between stress and PTSD. Negative cognitive appraisals of a traumatic event (e.g., appraisals related to self-blame) and post-traumatic stress symptomology (e.g., appraising flashbacks as indicative of a permanent change in cognitive functioning), as well as the reactions of other people (e.g., appraising other people as untrustworthy), play a central role in the development and persistence of PTSD. Negative appraisals evoke adverse emotional reactions (e.g., fear, shame, guilt, and sadness) and foster avoidance behaviors that ultimately impede the processing of the traumatic event and maintain a negative view of the self. 26 Hence, stronger beliefs and confidence in one's ability to solve a problem may generate an increased sense of agency in overcoming the impact of the trauma and mitigate the development of PTSD.
Previous research (e.g., Brown et al. 37 ) on self-efficacy suggests that individuals tend to draw on past experiences when attempting to solve problems. A similar process may occur during problem-solving appraisal. Evoking memories of successful prior attempts at problem-solving may increase the level of confidence and evoke positive emotions. According to the broaden-and-build theory of positive emotion of Fredrickson, 38 the experience of positive emotional states broadens momentary thought-action repertoires and weakens the grip of negative emotions on the individual, thus facilitating coping.
Second, we discovered that PC (i.e., the belief that one is in control of their behaviors and emotions) partially mediates the relationship between perceived stress and PTSD. The construct of PC is similar to that of perceived control, which has been extensively associated with physical and mental health outcomes.39,40 Perceived control plays a central role in PTSD. 8 Specifically, control over a post-trauma recovery process is associated with improved adjustment. 41 Theories of vulnerability (e.g., Gallagher et al. 42 ) suggest that diminished perceived control is a key aspect of negative emotional experiences. Appraisals of PC may confer confidence in the ability to recover following exposure to stressors, thus generating a positive outlook and buffering against PTSD.
Finally, we discovered that the AAS (i.e., the general disposition to approach or avoid problem-solving tasks) does not mediate the relationship between perceived stress and PTSD. However, this finding is in contrast to existing research,43,44 which has consistently linked avoidant coping to psychological distress. Generally, the use of cognitive and behavioral avoidance strategies has been implicated in the persistence of PTSD, as these strategies hinder the processing of traumatic events in memory. 8 One possible explanation for this finding is that PC may be the central mechanism influencing trauma-related outcomes. PC can enhance an individual's sense of agency, repertoire of coping strategies, and confidence in their ability to effectively cope with trauma-related cues, thereby ameliorating their PTSD symptoms. However, further longitudinal and qualitative studies are required to elucidate the associations among these variables. Qualitative studies on emotional regulation have reported that avoidance strategies (e.g., emotional suppression and distraction) can be effective in long-term adaptation. For example, Harnisch and Montgomery 45 reported that personal silencing (i.e., deciding not to speak about the trauma to significant others) and suppression of emotions related to vulnerability formed part of effective coping repertoires among adults who were forcibly recruited as children into the Ugandan civil war. These strategies were found to reduce distress among loved ones and victims and prevent stigmatization and retaliatory responses once they returned to their communities.
Overall, our results have potential implications for clinical practice. Empirically supported treatments for PTSD focus on identifying and modifying idiosyncratic maladaptive appraisals of trauma and its sequelae. 8 These interventions do not explicitly target appraisals related to problem-solving ability. However, feelings of helplessness and powerlessness represent core emotional responses to trauma and are elicited by appraisals of not being able to act or respond in an adaptive way (i.e., not being able to effectively solve a problem) and a loss of a sense of PC. 27 Hence, a complementary focus of interventions can involve assessing problem-solving appraisals and developing and increasing adaptive or positive cognitions pertaining to PC and confidence in problem-solving ability. Therefore, with PC emerging as a salient factor, clinicians could potentially target specific appraisals that enhance perceptions of control. This could possibly form part of a broader process of rebuilding the individual's worldview following exposure to trauma. The PSI can also be used to monitor changes in appraisals of problem-solving ability, PC, and PSC to determine whether an intervention produces changes in symptomology. Although AAS did not emerge as a significant predictor of psychological distress in the present study, it is well established that cognitive and behavioral avoidance maintain symptoms of PTSD. Hence, one potential use of the PSI can, for example, be to determine if the individual is strongly avoidant (i.e., AAS) and how this could potentially maintain PTSD symptomology. Interventions to enhance their problem-solving appraisals can be monitored to determine if they lead to changes in PTSD symptomology by motivating the individual to approach rather than avoid the problem. This type of information can aid in tailoring interventions and thereby improving treatment outcomes.
This study has several methodological limitations, including its cross-sectional research design, which precluded the examination of the temporal associations between the study variables, and the use of self-report instruments, which are prone to selection and social desirability biases. Longitudinal research and the use of structured interviews to assess study variables may reduce bias and confirm the results. Additionally, the sample was recruited from a single site and predominantly consisted of women. Therefore, a larger and more representative sample is recommended to corroborate our findings.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the South African Medical Research Council (grant number: SIR grant)
ORCID iD: Tyrone B. Pretorius https://orcid.org/0000-0002-6325-6623
References
- 1.Lazarus RS, Folkman S. Stress, appraisal, and coping. Springer; 1984. [Google Scholar]
- 2.Gómez de La Cuesta G, Schweizer S, Diehle J, Young J, Meiser-Stedman R. The relationship between maladaptive appraisals and posttraumatic stress disorder: a meta-analysis. Eur J Psychotraumatol. 2019;10(1):1620084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hitchcock C, Ellis AA, Williamson P, Nixon RDV. The prospective role of cognitive appraisals and social support in predicting children’s posttraumatic stress. J Abnorm Child Psychol. 2015;43(8):1485–1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mehu M, Scherer KR. The appraisal bias model of cognitive vulnerability to depression. Emot Rev . 2015;7(3):272–279. [Google Scholar]
- 5.Stapinski LA, Abbott MJ, Rapee RM. Evaluating the cognitive avoidance model of generalised anxiety disorder: impact of worry on threat appraisal, perceived control and anxious arousal. Behav Res Ther. 2010;48(10):1032–1040. [DOI] [PubMed] [Google Scholar]
- 6.Taylor PJ, Wood AM, Gooding P, Tarrier N. Appraisals and suicidality: the mediating role of defeat and entrapment. Arch Suicide Res. 2010;14(3):236–247. [DOI] [PubMed] [Google Scholar]
- 7.Maria P, Gooding P, Taylor P, Tarrier N. Negative self-appraisals and suicidal behavior among trauma victims experiencing PTSD symptoms: the mediating role of defeat and entrapment. Depress Anxiety . 2012;29(3):187–194. [DOI] [PubMed] [Google Scholar]
- 8.Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behav Res Ther . 2000;38(4):319–345. [DOI] [PubMed] [Google Scholar]
- 9.Halligan SL, Michael T, Clark DM, Ehlers A. Posttraumatic stress disorder following assault: the role of cognitive processing, trauma memory, and appraisals. J Consult Clin Psychol . 2003;71(3):419–431. [DOI] [PubMed] [Google Scholar]
- 10.Fedroff IC, Taylor S, Asmundson GJG, Koch WJ. Cognitive factors in traumatic stress reactions: predicting PTSD symptoms from anxiety sensitivity and beliefs about harmful events. Behav Cogn Psychother . 2000;28(1):5–15. [Google Scholar]
- 11.Sherrer MV. The role of cognitive appraisal in adaptation to traumatic stress in adults with serious mental illness: a critical review. Trauma Violence Abuse. 2011;12(3):151–167. [DOI] [PubMed] [Google Scholar]
- 12.Beck AT, Emery G, Greenberg RL. Anxiety disorders and phobias: a cognitive perspective . Basic Books; 1985. [Google Scholar]
- 13.Shahrour G, Dardas LA. Acute stress disorder, coping self-efficacy and subsequent psychological distress among nurses amid COVID-19. J Nurs Manag . 2020;28(7):1686–1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Trompeter N, Bussey K, Fitzpatrick S. Cyber victimization and internalizing difficulties: the mediating roles of coping self-efficacy and emotion dysregulation. J Abnorm Child Psychol . 2018;46(5):1129–1139. [DOI] [PubMed] [Google Scholar]
- 15.Luberto CM, Cotton S, McLeish AC, Mingione CJ, O’Bryan EM. Mindfulness skills and emotion regulation: the mediating role of coping self-efficacy. Mindfulness (N Y). 2014;5(4):373–380. [Google Scholar]
- 16.Heppner PP, Heppner MJ, Wang Y-W, Lee D-G. Creating a positive life: the role of problem-solving appraisal. In: Gallagher MW, Lopez SJ, eds. Positive psychological assessment: a handbook of models and measures . American Psychological Association; 2019: 111–124. [Google Scholar]
- 17.Chu C, Walker KL, Stanley IH, et al. Perceived problem-solving deficits and suicidal ideation: evidence for the explanatory roles of thwarted belongingness and perceived burdensomeness in five samples. J Pers Soc Psychol . 2018;115(1):137–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gabrielian S, Bromley E, Hamilton AB, et al. Problem solving skills and deficits among homeless veterans with serious mental illness. Am J Orthopsychiatry . 2019;89(2):287–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Elliott TR, Godshall FJ, Herrick SM, Witty TE, Spruell M. Problem-solving appraisal and psychological adjustment following spinal cord injury. Cognit Ther Res . 1991;15(5):387–398. [DOI] [PubMed] [Google Scholar]
- 20.Kerns RD, Rosenberg R, Otis JD. Self-appraised problem solving and pain-relevant social support as predictors of the experience of chronic pain. Ann Behav Med . 2002;24(2):100–105. [DOI] [PubMed] [Google Scholar]
- 21.Dixon WA, Heppner PP, Anderson WP. Problem-solving appraisal, stress, hopelessness, and suicide ideation in a college population. J Couns Psychol . 1991;38(1):51–56. [Google Scholar]
- 22.Artime TM, Buchholz KR, Jakupcak M. Mental health symptoms and treatment utilization among trauma-exposed college students. Psychol Trauma. 2019;11(3):274–282. [DOI] [PubMed] [Google Scholar]
- 23.Anders SL, Frazier PA, Shallcross SL. Prevalence and effects of life event exposure among undergraduate and community college students. J Couns Psychol . 2012;59(3):449–457. [DOI] [PubMed] [Google Scholar]
- 24.Kagee A, McGowan TC. Exposure to traumatic events and symptoms of post-traumatic stress among South African university students. S Afr J Psychol . 2013;43(3):327–339. [Google Scholar]
- 25.Padmanabhanunni A. Trauma nation: exposure to traumatic events among South African university students. J Community Psychol . 2020; 48(6):1853–1862. [DOI] [PubMed] [Google Scholar]
- 26.Bryant RA. Post-traumatic stress disorder: a state-of-the-art review of evidence and challenges. World Psychiatry . 2019;18(3):259–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Littlewood DL, Gooding PA, Panagioti M, Kyle SD. Nightmares and suicide in posttraumatic stress disorder: the mediating role of defeat, entrapment, and hopelessness. J Clin Sleep Med . 2016;12(3):393–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cohen S. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, eds. The social psychology of health . Sage Publications; 1988: 31–67. [Google Scholar]
- 29.Heppner P. The problem solving inventory. Consulting Psychologists Press; 1988. [Google Scholar]
- 30.Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress . 2015;28(6):489–498. [DOI] [PubMed] [Google Scholar]
- 31.Heppner PP, Pretorius TB, Wei M, Lee D-g, Wang Y-W. Examining the generalizability of problem-solving appraisal in black South Africans. J Couns Psychol . 2002;49(4):484–498. [Google Scholar]
- 32.Pretorius TB. The family environment of students self-appraised as effective and ineffective problem solvers. Psychol Rep . 1996;79(3):915–921. [Google Scholar]
- 33.Pretorius TB, Diedricks M. Problem-solving appraisal, social support and stress-depression relationship. S Afr J Psychol . 1994;24(2):86–90. [Google Scholar]
- 34.Padmanabhanunni A, Wiid C. From fear to fortitude: differential vulnerability to PTSD among South African university students. Traumatology (Tallahassee, Fla). 2022;28(1):167–174. [Google Scholar]
- 35.Hayes AF, Coutts JJ. Use omega rather than Cronbach’s alpha for estimating reliability. But…. Commun Methods Meas . 2020;14(1):1–24. [Google Scholar]
- 36.Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. Guilford Publications; 2017. [Google Scholar]
- 37.Brown AD, Kouri NA, Rahman N, Joscelyne A, Bryant RA, Charles RM. Enhancing self-efficacy improves episodic future thinking and social-decision making in combat veterans with posttraumatic stress disorder. Psychiatry Res . 2016;242:19–25. [DOI] [PubMed] [Google Scholar]
- 38.Fredrickson BL. Cultivating positive emotions to optimize health and well-being. Prev Treat. 2000;3(1):1a. [Google Scholar]
- 39.Pagnini F, Bercovitz K, Langer E. Perceived control and mindfulness: implications for clinical practice. J Psychother Integr. 2016;26(2):91–102. [Google Scholar]
- 40.Brooks M, Graham-Kevan N, Lowe M, Robinson S. Rumination, event centrality, and perceived control as predictors of post-traumatic growth and distress: the cognitive growth and stress model. Br J Clin Psychol . 2017;56(3):286–302. [DOI] [PubMed] [Google Scholar]
- 41.Bernardi J, Engelbrecht A, Jobson L. The impact of culture on cognitive appraisals: implications for the development, maintenance, and treatment of posttraumatic stress disorder. Clin Psychol (Aust Psychol Soc). 2019;23(2):91–102. [Google Scholar]
- 42.Gallagher MW, Bentley KH, Barlow DH. Perceived control and vulnerability to anxiety disorders: a meta-analytic review. Cognit Ther Res . 2014;38(6):571–584. [Google Scholar]
- 43.Thomassen ÅG, Hystad SW, Johnsen BH, Johnsen GE, Bartone PT. The effect of hardiness on PTSD symptoms: a prospective mediational approach. Mil Psychol . 2018;30(2):142–151. [Google Scholar]
- 44.Sheerin CM, Chowdhury N, Lind MJ, et al. Relation between coping and posttrauma cognitions on PTSD in a combat-trauma population. Mil Psychol . 2018;30(2):98–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Harnisch H, Montgomery E. “What kept me going”: a qualitative study of avoidant responses to war-related adversity and perpetration of violence by former forcibly recruited children and youth in the Acholi region of northern Uganda. Soc Sci Med (1982). 2017;188:100–108. [DOI] [PubMed] [Google Scholar]