Ending hunger in the United States by 2030 “is a goal within our reach,” said President Joseph R Biden on 28 September, 2022, at a White House Conference on Hunger, Nutrition, and Health [1,2]. The historic gathering, 50 y after the 1972 conference convened by then President Richard Nixon, was a call to action for a coordinated strategy to drive a transformative change in the United States to end hunger, improve nutrition and physical activity, and close the disparities surrounding them. The White House staff and federal agencies that planned the conference, including the NIH, have continued to meet, reflect on, and discuss whole-of-society and whole-of-government approaches to these challenges.
The centrality of nutrition in our health and lives is well-known biologically, culturally, and economically. Notably, one of the White House Conference panels was “Food is Medicine: Bringing nutrition out of the healthcare shadows." Food is Medicine is a key element within the National Strategy on Hunger, Nutrition, and Health, which envisions complete integration of nutrition and health care [3]. Food is Medicine is an umbrella term for programs that respond to the critical link between diet and health involving (1) the provision of Food is Medicine services (medically tailored meals, medically tailored groceries, produce prescriptions, teaching kitchens, etc.), and (2) a nexus to the healthcare system hopefully deploying other nutrition or lifestyle medicine care to its communities. The nexus to the healthcare system recognizes healthcare providers as a trusted source of information and is a valuable opportunity not to be missed. Although only a few people report receiving dietary guidance from their healthcare providers, 78% of those that do receive such advice adjust their dietary habits [4].
Food is Medicine is a Growing Opportunity for System-Level Health Improvement
Food is Medicine is an evidence-based solution for addressing food insecurity and the many diet-related chronic diseases affecting millions in the United States and people worldwide. Food is Medicine interventions have been shown to reduce food insecurity, which is an independent risk factor for morbidity, medication compliance, depression, and mortality in a number of disorders [4]. Evidence is also mounting on how Food is Medicine strategies are associated not only with meaningful improvements in food security but also with health biomarkers (e.g., BMI, cardiometabolic parameters, and HbA1c), insurance costs, and health quality indicators (e.g., hospital readmissions for the same diagnosis) [4]. Consequently, these services are increasingly being covered by private medical insurance and federal payors through Medicare Advantage and Medicaid (via waiver programs). Now is the time to extend the research base on this topic so that we can critically assess the evidence to better integrate it into healthcare through evidence-backed policies.
Fully realizing the promise of Food is Medicine goes beyond delivery of interventions; it also requires an anchor point within the healthcare system that deploys community-based care related to nutrition, obesity, and lifestyle medicine. Doing so builds on strong community connections and existing trust between individuals and their healthcare providers. Sustainable clinical-community partnerships could act as an effective bridge between healthcare interactions and an individual’s dietary and lifestyle behaviors.
NIH Food is Medicine Networks or Centers of Excellence
Multiple sectors are needed to fully actualize a national Food is Medicine strategy, but the first step is to obtain evidence gained through rigorous community-involved research. As articulated by the National Strategy on Hunger, Nutrition, and Health [2], a whole-of-government approach that draws expertise and innovation from multiple agencies is needed to build and implement an evidence base that integrates research findings geographically, economically, and socio-culturally. To that end, 12 federal agencies that assisted in planning the White House Conference are participating in a Food is Medicine Request for Information (RFI; NOT-OD-23-107), which was released on 11 April, 2023 [5]. This RFI asks for input on “Food is Medicine” research opportunities, education and training needs, community outreach and engagement, and insurance coverage for “Food is Medicine” services and related activities (e.g., teaching kitchens).
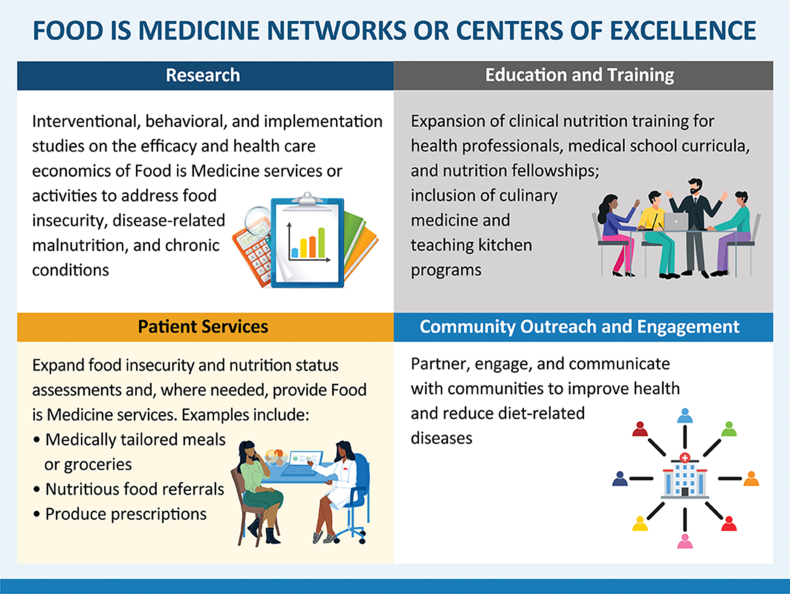
The NIH Office of Nutrition Research has also received concept approval for an innovative initiative: comprehensive Food is Medicine Networks or Centers of Excellence (Figure 1). The intent of these Networks or Centers is ambitious. They would not only critically assess strategies for the integration of Food is Medicine into United States healthcare but also serve as idea incubators that conceive and test novel approaches to ensure that nutrition and social sciences are optimally utilized for the promotion of health in our society. Ideally, they would serve as catalysts, fundamentally transforming attention to nutrition in health care and becoming the nexus in their communities to rectify social barriers that are driving diet-related diseases.
FIGURE 1.
Infographic showing the 4 domains of a comprehensive proposed concept for Food is Medicine Networks or Centers of Excellence to address diet-related diseases, disease-related malnutrition, and food insecurity and to increase nutrition training across health professions and stages (e.g., undergraduate, graduate training including fellowship training, continuing medical education, and other ongoing professional staff training).
A wide-ranging set of research questions is ready for investigation (Table 1). In addition to conducting research analogous to the National Cancer Institute Comprehensive Cancer Centers, these Food is Medicine Networks or Centers of Excellence also aim to impact patient care, training, and education, along with community outreach and engagement (Figure 1). Notably, the initiative aims to increase clinical nutrition, lifestyle, and obesity medicine in health professional education, including the expansion of fellowship programs. Increasing nutrition education and training in medical schools is a popular, bipartisan issue under consideration by the Accreditation Council for Graduate Medical Education, the Association of American Medical Colleges, and the American Association of Colleges of Osteopathic Medicine, which recently joined together for a Summit on Medical Education in Nutrition [6]. The initiative also includes community outreach and engagement to ensure representative diversity of research participants, to engage the community in research design, and to form collaborations of the government, organizations, and private sector groups that are already serving and fulfilling the food security, nutrition disparities, and public health niches in their communities. Planning this initiative will be informed by the above-mentioned collaborative RFI.
TABLE 1.
Examples of research areas for advancing Food is Medicine
|
|
|
|
|
|
|
|
|
|
|
Looking Ahead
Imagine a world where greater attention is paid to the power of nutrition in healthcare and a world without hunger and food insecurity. It is a world in which all individuals, families, and communities have ready access to enough affordable, nutritious food to sustain a happy and healthy life. Health conditions linked to poor diet are associated with preventable causes of death in the United States and are major drivers of healthcare costs, estimated to be in the hundreds of billions of dollars annually [7]. We know that food and nutrition insecurity, lack of access to a healthy diet, and disease-related malnutrition are harmful to health, but we also know that these problems and their consequences are preventable. Rigorous research can turn knowledge into workable strategies and convene partners across public and private sectors to develop a roadmap for change.
Harnessing the power of research to end hunger and prevent diet-related disease is also tightly linked to achieving health equity—a key goal of the current administration and NIH. The future is now if we invest in Food is Medicine and nutrition research to inform policy to develop and disseminate durable, evidence-based solutions for ending hunger and addressing chronic diet-related diseases as soon as possible using science-based tools and resources. As mentioned earlier, federal agencies have released an RFI that seeks your input on gaps and opportunities for Food is Medicine research, provision and coverage of Food is Medicine services and activities, education and training, and community outreach and engagement [5]. If you have experience or thoughts about Food is Medicine, this RFI is your opportunity to provide input.
Acknowledgments
I thank Alison F Davis and Robert Eisinger for their assistance in the preparation and review of the manuscript. I also recognize the efforts of the Strategic Plan for NIH Nutrition Research Implementation Working Groups. These are cochaired by Tanya Agurs-Collins, Jill Reedy, and April Oh (National Cancer Institute); Charlotte Pratt and Alison Brown (National Heart, Lung, and Blood Institute); Padma Maruvada and Mary Evans (National Institute of Diabetes and Digestive and Kidney Diseases); Andrew Bremer and Kimberlea Gibbs (Eunice Kennedy Shriver National Institute of Child Health and Human Development); Holly Nicastro and Roberto Flores (Office of Nutrition Research); and Nancy Potischman (Office of Dietary Supplements), along with Office of Nutrition staff who have continually provided leadership on this topic, nutrition research, food insecurity, nutrition disparities, and implementation science.
Author contributions
The sole author was responsible for all aspects of this manuscript.
Conflicts of interest
CJL is a paid employee of the NIH and has no other financial conflicts of interest.
References
- 1.Office of Disease Prevention and Health Promotion . United States Department of Health and Human Services. [Internet]; 2022. Ending hunger and reducing diet-related diseases and disparities.https://health.gov/our-work/nutrition-physical-activity/white-house-conference-hunger-nutrition-and-health [updated 24 March, 2023; cited 31 March, 2023]. Available from: [Google Scholar]
- 2.Psota T., Maniscalco S., Kijek M., Ohlhorst S.D. Driving transformative change to end hunger and reduce diet-related diseases and disparities: the White House Conference on Hunger, Nutrition, and Health. Am. J. Clin. Nutr. 2023;117(4):649–658. doi: 10.1016/j.ajcnut.2023.01.013. [DOI] [PubMed] [Google Scholar]
- 3.Biden-Harris Administration National Strategy on Hunger . 2022. Nutrition, and Health. The White House Domestic Policy Council.https://www.whitehouse.gov/wp-content/uploads/2022/09/White-House-National-Strategy-on-Hunger-Nutrition-and-Health-FINAL.pdf [Internet] [cited 31 March, 2023]. Available from: [Google Scholar]
- 4.Downer S., Clippinger J., Kummer C., Hager K. The Aspen Institute; Washington, DC: 2022. Food is Medicine Research Action Plan.https://www.aspeninstitute.org/programs/food-and-society-program/food-is-medicine-project/ [Internet] [cited 31 March, 2023] Available from: [Google Scholar]
- 5.Request for Information (RFI) National Institutes of Health; 2023. Food is Medicine Research Opportunities.https://grants.nih.gov/grants/guide/notice-files/NOT-OD-23-107.html [Internet] [cited April 18, 2023]. Available from: [Google Scholar]
- 6.ACGME hosts summit on medical education in nutrition. Accreditation Council for Graduate Medical Education, [Internet]; 2023. https://www.acgme.org/newsroom/2023/3/acgme-hosts-summit-on-medical-education-in-nutrition/ [cited 31 March, 2023]. Available from: [Google Scholar]
- 7.O’Neil Hayes T., Asres R. American Action Forum. [Internet]; 2023. The economic costs of poor nutrition.https://www.americanactionforum.org/research/the-economic-costs-of-poor-nutrition/#_edn1 [cited 31 March, 2023]. Available from: [Google Scholar]