Abstract
Trichosporon spp. endocarditis is a severe and hard-to-treat infection. Immunosuppressed subjects and carriers of prosthetic valves or intracardiac devices are at risk. This article presents the case of an immunocompetent 74-year-old man affected by endocarditis of the prosthetic aortic valve. After Bentall surgery, cultures of the removed valve demonstrated Trichosporon ashaii as the etiological agent. The patient was treated with amphotericin B at first and subsequently with fluconazole. Given the fragility of the patient and the aggressiveness of the pathogen, life-long prophylactic therapy with fluconazole was prescribed. After 5 years follow-up, no drug-related toxicities were reported and the patient never showed any signs of recurrence. The review of the literature illustrates that Trichosporon spp. endocarditis may present even many years after heart surgery, and it is often associated with massive valve vegetations, severe embolic complications, and unfavorable outcome. Due to the absence of international guidelines, there is no unanimous therapeutic approach, but amphotericin B and azoles are usually prescribed. Additionally, a prompt surgical intervention seems to be of paramount importance. When dealing with a life-threatening disease, such as mycotic endocarditis of prosthetic valves, it is essential to consider and treat even rare etiological agents such as Trichosporon spp.
Keywords: Trichosporon, asahii, azoles, endocarditis, prosthetic valve
1. Introduction
Invasive mycosis caused by non-Candida yeasts such as trichosporonosis are rare opportunistic infections that may lead to life-threatening disease in immunodeficient individuals [1,2,3,4]. Trichosporonosis refers to invasive human infection by Trichosporon spp., which is a large heterogeneous genus of basidiomycetous yeasts, producing arthroconidia [5]. Trichosporon spp. is ubiquitous in soil, decomposing wood, bird droppings, bats, cattle, food, and water. In rare cases, it can be present among the colonizing flora of the human body, reportedly being isolated from the pharynx, gastrointestinal tract, vagina, skin, and nails [1,6,7,8]. Early descriptions of the pathogen date back to 1890 by Hermann Beigel, who identified Trichosporon in infected mustache hair, but several classifications have since been proposed [5]. In 1992, the first taxonomy review was completed, and more species were identified and characterized based on molecular analysis. Several species were recognized as formerly T. beigelii: T. asahii, T. mucoides, T. inkin, T. ovoides, and T. steroids [9,10,11]. Nowadays, the genus includes at least 50 species, 16 of which might have clinical relevance [6,12]. The most common species reported in deep-seated disseminated infections is Trichosporon asahii, followed by T. mucoides: together, they are responsible for the vast majority of human trichosporonosis cases. T. ovoides, T. inkin, T. asteroides, and T. cutaneum are correlated with hair infection and superficial skin lesions [5,13]. The phenotypical identification of Trichosporon is based on its ability to produce arthroconidia. However, since Geotrichum shares this microbiological feature, when arthroconidia are observed, a urease test is recommended to discriminate Trichosporon upon its ability to hydrolyze urea. Phenotypic identification is useful for Trichosporon spp. screening, but classical yeast identification methods present limited accuracy and reproducibility. The implementation of new identification methods, such as matrix-assisted laser desorption/ionization–time of flight (MALDI-TOF) analysis, may be useful in the etiological diagnosis. However, only molecular analysis, mostly PCR-based methods, and flow cytometry assays allow the definitive recognition of Trichosporon isolates at the species level. The detection of 1,3--D-glucan (BDG) is reported in trichosporonosis, but no data are available to define the clinical sensitivity and specificity of this test. Moreover, it is well known that cross-reactions with C. neoformans antigens may occur during trichosporonosis [6]. Historically, Trichosporon spp. was considered responsible for a distal infection of the hair shaft called white piedra, but was later also associated with invasive infections [1,14,15]. Risk factors for Trichosporon spp. invasive infection are neutropenia due to myeloablative chemotherapy, bone marrow or solid organ transplantation, diabetes mellitus, HIV infection, end-stage chronic kidney disease, the positioning of invasive medical devices, extensive burns, prior prolonged antibiotic or glucocorticoid treatment, and previous heart valve surgery. The main pathogenetic hypothesis is that Trichosporon spp. penetrates through the intestinal tract, upper respiratory tract, or a venous catheter. This might explain why chemotherapy or prolonged antimicrobial therapy, which are known to be involved in damaging the digestive tract mucosa and causing major disruption of the intestinal flora, respectively, seem to be etiologically related to the onset of trichosporonosis [15,16,17,18]. Invasive Trichosporon spp. infections are rarely confined to a single organ. Nonetheless, Trichosporon spp. infective endocarditis seems to represent a stand-alone clinical entity, as it is not limited to severely immunocompromised subjects. In fact, the presence of a prosthetic valve or intracardiac device constitutes a major independent risk factor, even many years after cardiac surgery in immunocompetent subjects [15,19]. To the best of our knowledge, no endocarditis on native valves has been reported in the literature in the last 20 years.
We hereby present a intriguing case of Trichosporon ashaii endocarditis in an immunocompetent patient who underwent multiple heart surgeries and was later prescribed with life-long medical therapy. Our aim was to highlight the potential aggressiveness of the yeast and the challenges that it may present to the infectious disease specialist.
2. Case Report
Patient history: We present the case of a 75-year-old Italian male who was referred to our clinic in May 2018. Upon reviewing his medical records, it was discovered that at the age of 39, in 1981, the patient underwent aortic valve replacement surgery. The procedure involved implanting a mechanical valve due to aortic stenosis, suspected to have resulted from post-rheumatic causes. He also had a history of chronic obstructive pulmonary disease (COPD), chronic heart failure, type 2 diabetes mellitus (DM), and obstructive sleep apnea syndrome (OSAS). He reported allergy to amoxicillin. After the surgery and up until 2017, neither post-operative nor long-term complications had occurred. In 2017, a transthoracic two-dimensional echography was performed as a preoperative test before an elective hip replacement surgery. The exam showed a large (5.7) aortic aneurysm and surgical correction of the vascular defect was recommended. The patient underwent a Bentall procedure, consisting of a composite graft replacement of the aortic valve, aortic root, and ascending aorta, with re-implantation of the coronary arteries into the graft. On day 7 after surgery, the patient presented a second-degree atrioventricular Luciani–Wenckebach block, associated with episodes of atrioventricular dissociation. A pacemaker (PM) was therefore implanted. The patient was transferred to the Cardiological Rehabilitation Department. At that time, there was no evidence of leukocytosis (WBC 6.7 × 103/uL, reference range 4 to 10 × 103/uL) or increased inflammatory markers (CRP 2.38 mg/dL, reference range 0 to 0.5 mg/dL).
Clinical presentation: Four months after the cardiac surgery, the man presented to the Emergency Department of our hospital (day 0) with epigastric pain, fever, and diaphoresis.
Investigations: Computed tomography (CT) of the chest, performed to exclude pulmonary embolism, showed two hypodense splenic lesions suggestive of septic embolization. Transesophageal echocardiography (TEE) was performed the day after the admission and revealed a posterior and a medial abscess starting from the valve plane with a 4 cm cranial extension and several floating vegetations attached to the biological aortic valve. Once the suspicion of infective endocarditis was confirmed, a CT scan of the brain and fundus oculi examination were prescribed to complete the diagnostic work-up; these excluded cerebral or retinal septic embolization. On day 24, the patient, who was still febrile, was transferred to another hospital. There, he underwent thoracic aortic vascular prosthesis replacement using a bovine pericardial patch from which a tube graft was formed and then sutured with two end-to-end anastomoses. The infected appositions on the prosthetic cups were removed by performing accurate debridement of the previously implanted prosthetic valve. Lastly, a single coronary artery bypass was performed with an inverted autologous great saphenous vein tract to the anterior descending artery. The entire procedure was performed in deep hypothermia. Fifty-two days after hospital admission, the patient was discharged and transferred to a Cardiologic Rehabilitation Institute. One week later, fever started again, and the patient was transferred back to the Cardiothoracic Department of the previous hospital. TEE showed persisting vegetations within the vascular prosthetic lumen and an increase periaortic thickening. Seven weeks after the previous aortic replacement, a new surgical treatment was performed by a second Bentall procedure. Throughout the hospital stay, the PM was never removed, and it is still in place.
Diagnosis: From intraoperative samples collected during the last surgical intervention, Trichosporon asahii was finally isolated. Identification of the pathogen was made using conventional cultures. Antifungal susceptibility testing demonstrated that the isolated strain was susceptible to fluconazole (MIC 0.250 uL/mL); no other EUCAST breakpoints were established at the time. Periodically collected blood cultures consistently showed no growth.
Treatment: Empirical treatment with vancomycin, gentamycin, and rifampin for prosthetic valve endocarditis was started three days after hospital admission. On hospital day 17, the patient was still febrile, so gentamycin was suspended, and levofloxacin and cefepime were introduced. One week later, considering the lack of clinical improvement, the therapy was modified again: vancomycin, levofloxacin, and cefepime were suspended and meropenem and daptomycin, along with ongoing rifampin, were started. After the first surgical intervention, all ongoing therapy was suspended and switched to daptomycin, ceftriaxone, and levofloxacin. Then, before the second surgical intervention, treatment was modified again to levofloxacin, meropenem, daptomycin, and anidulafungin. As soon as Trichosporon asahii infection was diagnosed, intravenous amphotericin B was introduced, and the ongoing antibiotic therapy was suspended a few days later. Ten days later, the antimicrobial treatment was simplified to fluconazole (600 mg every 24 h). The patient was discharged seven weeks after the first hospital admission.
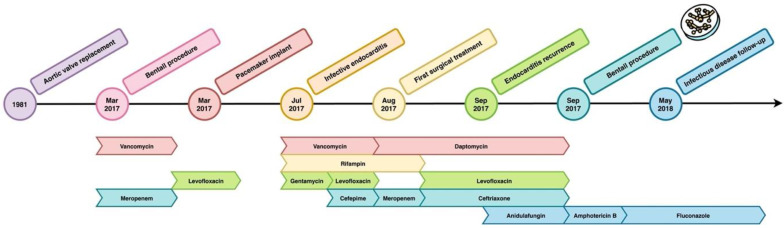
Follow-up: During the scheduled follow-up, he underwent imaging controls with multiple FDG-PET/CT (18F-fluorodeoxyglucose positron emission tomography, contrast-enhanced computed tomography), which repeatedly showed conspicuous hyperaccumulations in the ascending aorta up to the aortic valve. Blood parameters were monitored every two weeks and no significant changes were found in the first eight months: blood count was stationary; C-reactive protein (CRP) was always less than 10 mg/dL (reference range 0 to 5 mg per liter); aspartate aminotransferase and alanine aminotransferase results were in range in all measurements; and the blood level of creatinine was stable. Fluconazole was well tolerated and discontinued after 12 months. During the months following the end of the therapy, FDG-PET/CT remained unchanged. Due to anamnestic COPD, the patient required several prolonged steroid treatments because of frequent flare-ups. CT scan of the chest showed lung densities in the middle lobe surrounded by ground glass areas. Blood tests showed increased CRP (29 mg/L in a first episode and 19.6 mg/L in the second event; reference range, 0 to 5 mg/L). Considering the higher risk of recurrence of complicated fungal infection in immunocompromised subjects, the patient’s frailty, and his frequent need for steroid treatment, we decided to resume antifungal therapy, and fluconazole 100 mg daily was prescribed as life-long suppressive therapy. Approximately one year after the reintroduction of therapy, increased bilirubin (1.75 mg/dL; reference range, 0.2 to 1.2 mg per deciliter) and gamma-glutamyl transpeptidase (195 U/L; reference range, 0 to 50 U/L) were noted. On suspicion of liver toxicity, we decided to halve the dosage of fluconazole (50 mg every 24 h). In the following years, the patient went through a progressive normalization of cholestasis indices. The semiannual TTE follow-up showed substantial stability. Ejection fraction was 30%. Mitral valve revealed fibro-calcification. Doppler study revealed mild-to-moderate mitral regurgitation. Aortic biologic prosthesis showed normal opening, no obstruction, no evident pathological regurgitation, and no significant stenosis. At the last outpatient evaluation, five years after the start of suppressive therapy, the patient was found in good general condition and reported subjective well-being. On physical examination, vesicular breath sounds were reduced in left pulmonary base with no added pathological sounds. The cardiac examination was normal, except for a grade 3 systolic murmur. The remainder of the examination was normal. A graphic representation of the timeline of the clinical course of the patient is shown in Figure 1.
Figure 1.
Timeline of the clinical history of the patient and subsequent antibiotic molecule administrated. The little Petri dish indicates the isolation of T. asahii on valve samples.
3. Literature Review
Advanced research on PubMed for “(trichosporon) AND (endocarditis)”, filtering the last twenty years (from January 2003 to April 2023), generated eight results, all of which were case reports. One of them was inherent to Wickerhamomyces anomalous bacteriemia [20]; therefore, we only considered seven research papers in our analysis, in addition to our case report. The main clinical information concerning the papers is summarized in Table 1.
Table 1.
Summary of cases of Trichosporon asahii endocarditis from January 2003 to April 2023. The present case is included (number 8). M: male, F: female, IV: intravenous, HTN: hypertension, FU: follow-up, mth: month, NA: not applicable.
| Age, Sex, Country | Comorbidities and Previous Surgery | Cultures and Pathogen | Site of Infection | Induction Therapy | Maintenance Therapy | Cardiac Surgery | Medical Suppression | Clinical Outcome | Follow-Up | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 [21] | 52, M, Spain | Biological valve replacement | Blood cultures: T. inkin post-mortem | Vegetation of the prosthetic aortic valve | None | None | None | None | Exitus 30 h after hospital admission | NA |
| 2 [16] | 58, M, Japan | HTN | Blood cultures: S. oralis later T. asahii | Endocarditis of prosthetic mitral valve and aortic valve cusp | IV fluconazole 400 mg/day | Fluconazole 200 mg q24h | Aortic and mitral valve replacement | None | Recovery | NA |
| 3 [14] | 57, F, India | HTN, DM, COPD, PM implant |
Blood cultures: Trichosporon spp. | PM infection all valves were normal | IV voriconazole 200 mg q12h | Oral voriconazole 200 mg q12h | None | Voriconazole 200 mg q12h | Recovery | No recurrence, increased size of vegetation |
| 4 [22] | 20, M, Texas, USA | Biological aortic valve replacement | Blood cultures: negative Valve cultures: T. asahii |
Large vegetations on the anterior wall of the aorta | Amphotericin B and ketoconazole for 2 weeks | Voriconazole | Valve replacement, patching of the aorta’s wall |
Voriconazole 400 mg q8h for 6 months, q12h for 6 months, qd for 6 months | Complete recovery, resolution of hemiplegia | Normal echocardiogram at 5 years FU |
| 5 [15] | 66, M, Republic of Korea | Aortic valve replacement and mitral annuloplasty | Blood cultures and valve cultures: T. mucoides |
Endocarditis of the prosthetic aortic and mitral valves | IV voriconazole and amphotericin B for 22 days | Voriconazole for 3 months | Valve replacement, removal of the prosthetic ring and pannus | None | Recovery | No evidence of relapse at 18 months FU |
| 6 [19] | 57, M, Portugal | Mitral valve replacement | Blood cultures: negative Valve cultures: T. beigelii |
Endocarditis of prosthetic biological valve | Amphotericin B | Voriconazole | Valve replacement | None | Exitus 13 days after surgery | NA |
| 7 [23] | 63, M, Canada | DM, bioprosthetic aortic root and valve | Blood cultures: T. mucoides |
Endocarditis of prosthetic aortic valve and valve abscess |
Amphotericin B q24h for 6 days, IV voriconazole q12h for 2 weeks | Voriconazole 300 mg q12h and terbinafine 250 mg q24h | None | Voriconazole | Recovery | No recurrence but increased valve abscess at 12 months FU |
| 8 | 75, M, Italy | COPD, DM, OSAS Bioprosthetic aortic root and valve |
Blood cultures: negative Valve cultures: T. asahii |
Abscess of bioprosthetic aortic valve and several vegetations | Amphotericin B for 10 days | Fluconazole 600 mg q24h | Bioprosthetic valve replacement | Fluconazole 400 mg, later reduced to 100 mg, later reduced to 50 mg | Complete recovery | No recurrences, no valve vegetations at 5 years FU |
Our search showed that trichosporonosis patients are mostly men (only one woman was reported with the disease), with a median age of 56.00 16.16 years. Trichosporon endocarditis developed after a median of 5.60 4.56 years from heart surgery. Surprisingly, even if Trichosporon spp. is a known opportunistic pathogen, all patients were immunocompetent. A possible explanation is that these cases are more likely to be published on account of their singularity. Alternatively, it may be speculated that previous heart surgery is such a strong risk factor that Trichosporon endocarditis can occur in immunocompetent subjects. Clinical presentation was usually subacute with low-grade fever, leukocytosis, and CRP elevation. Eosinophilia was reported by two authors. A previously unknown cardiac murmur was described in 4/8 cases; microvascular damage signs, such as conjunctival hemorrhage, petechial eruption, or Osler nodules were present in 4/8 patients; and hemiplegia was described in 1 case. Interestingly, a correlation to onychomycosis from Trichosporon mucoides is pointed out in one case: this was the only fungal-related clinical sign at time of hospital admittance. All the patients had a previous heart surgery, mostly because of valvopathies, and one PM implant. In all cases, the left chambers of the heart were implicated, with the only exception of the PM infection, which was positioned in the right chambers. Four cases of endocarditis involved the aortic valve (in one case also the wall of the ascending aorta presented a vegetation), one involved the mitral valve, and in two cases, vegetations on both the left valves were documented. The most impressive feature of these vegetations was their very large size (up to 2.54 × 2.36 cm). This is probably the reason why most of the echocardiographic diagnoses were made by a transthoracic echocardiography (TTE in 4 cases, TEE in 3 cases, unspecified in 1 case). The large size of vegetations, often described as mobile and irregular, may also explain the high incidence of severe complications reported. In detail, embolic complications, both splanchnic and encephalic were demonstrated in 5/8 patients, and hemiplegia/hemiparesis were described in 2 cases, vasculitis-like complications were demonstrated in 2/8 cases, and heart failure occurred in 3/8 of the patients, with a rapid fatal evolution in 2 of them.
Trichosporon spp. was found in blood cultures in 5/8 patients, and in valve cultures in the 3/8 cases with negative blood cultures. It was the only proven etiologic agent in all but one case, in whom a T. asahii fungemia complicated a previously documented endocarditis of prosthetic valve from S. oralis. In one case, the cultural diagnosis was confirmed by a histopathological exam. An antigenic test was performed in two patients, both with positive results (BDG and galactomannan in one case and BDG only in the other one).
Patients presented with signs of endocarditis, but no specific risk factor or clinical sign suggestive for a mycotic etiology; therefore, most patients initially received empirical antibacterial therapies (most frequently the combination of vancomycin, gentamycin, and rifampin). In one single case, caspofungin was initiated for suspected candidemia.
Different approaches to treatment of trichosporonosis were adopted due to the lack of international guidelines and the very large time window considered. Liposomal amphotericin B was prescribed as monotherapy in two cases, and in 3/8 cases in combination with azoles (1 ketoconazole, 2 voriconazole). In additionally, 2 patients were treated with azole monotherapy (1 fluconazole, 1 voriconazole). After a variable amount of time, they were all switched to a maintenance therapy with azoles. Five patients underwent a surgical source control of infection, while life-long voriconazole suppressive therapy was prescribed to the other three. The difference between these two treatment strategies was evaluated based on the clinical outcome. Both groups presented a fatality, while the others had a clinical resolution with no recurrences. However, 2/3 patients in the suppressive therapy group presented increased size of vegetations at follow-up echocardiograms.
4. Discussion
The etiologic agents most frequently isolated in mycotic endocarditis are Candida spp. and Aspergillus spp. [24], but there is increasing clinical interest in rare yeast etiologies. The incidence of trichosporonosis in deep mycosis patients is about 5% [17]. Trichosporonosis is commonly found in immunocompromised patients, and the associated outcome is usually poorer than other similar yeast-like invasive infections, as mortality ranges from 30 to 90% [1,6]. Emboli complications have been reported to occur in 75% of the cases, and mortality has been reported up to 83% [15,16]. In some cases, the exitus may occur before starting treatment or even before diagnosis [21]. Known high-risk patients for Trichosporon spp. deep-seated infections include those who underwent bone marrow or solid organ transplantation, burn victims, receivers of prosthetic heart valves or intracardiac device placement, HIV-infected subjects, those undergoing peritoneal dialysis, and intravenous drug users [16,25]. Some authors reported the genus Trichosporon to be the second most common agent of disseminated yeast infections after the genus Candida, in patients affected by a malignant hematopathy [6,26,27,28]. In these patients, the outcome is usually worse. However, there are some exceptions; for example, invasive infections due to T. mucoides, including fungemia, peritonitis, brain abscess, and prosthetic valve endocarditis, have been reported in both immunosuppressed and immunocompetent hosts [1,15,29,30,31,32]. The diagnosis of trichosporonosis includes various tools that can often be used in combination. When Trichosporon mycelial threads or conidia are observed in a biopsy specimen, they must be considered as definitely diagnostic. However, it is not advisable to rely on a histopathological diagnosis because adequate samples might not be available, and it usually takes a long time to get the results. Therefore, blood cultures, or any culture of otherwise sterile samples (such as cerebrospinal fluid, endothelial tissues) are the only established microbiologic diagnostic tool [1,6]. However, blood cultures have low sensitivity, resulting in false-negative results in systemic trichosporonosis [14,16,33]. Whereas the diagnostic role of histopathological exam, or positive blood cultures is well defined, the usefulness of antigenic tests is not. For example, both galactomannan and BDG elevation could be correlated to the presence of Trichosporon spp. However, since their specificity is very low, they could play a better role as screening markers for mycotic infections in general, rather than trichosporonosis [1,16]. Moreover, a cross-reactivity with glucuronoxylomannan antigen, which is known as the Cryptococcus capsular antigen, has been described [34]. As an indirect diagnostic tool, eosinophilia may be associated with trichosporonosis. In rare cases, eosinophils may reach even very high values and even lead to acute eosinophilic pneumonia. When an elevated eosinophil count is reported at diagnosis, it can be later used as a marker of response to treatment [23]. The clinical presentation of Trichosporon spp. endocarditis is comparable to any other infective endocarditis. It is recommended to follow the revised Duke’s criteria to risk stratify patients into three categories of definite, possible, and rejected diagnosis [35]. Regarding our case, it was correctly considered as a definite infective endocarditis according to Duke’s criteria. The physiopathology of Trichosporon spp. endocarditis seems to be strictly dependent on the presence of a prosthetic valve or intracardiac implant [1,6]. In some cases, the pathogen reaches the heart valves after contamination of a percutaneously inserted intravascular catheter via colonized skin [36]. This is probably how our patient acquired Trichosporon asahii, right after the heart surgery. However, the trichosporonosis clinical course is peculiar, and the infection timing may also be prolonged as Trichosporon spp. is not necessarily a hospital-acquired pathogen. As our literature research underlines, Trichosporon spp. endocarditis may present even after eleven years from the implant of a prosthetic valve [14,15,16,19,21,22,23]. An underlying gastrointestinal colonization and further translocation throughout the gut seems to be the most probable explanation to this kind of late-onset deep-seated infection [37,38].
The optimal treatment of trichosporonosis is not established yet due to the rarity of the infection. According to the global guideline for the diagnosis and management of rare yeast infections, posaconazole or voriconazole are considered as first-line treatments, and fluconazole may be acceptable as an alternative first choice. Amphotericin B is only contemplated as a second-line treatment. Echinocandins should be avoided [1] as all Trichosporon genera had been found to be intrinsically resistant to these drugs in vitro [6,39]. In our case, amphotericin B was chosen for induction therapy and a good outcome was obtained, as in other case reports [19,23]. A combination therapy with 5-fluorocytosine and amphotericin B has also been associated with good clinical response in one case report [29]. Moreover, combination therapy with 5-fluorocytosine and amphotericin B has been associated with good clinical response in one case report [29]. Nevertheless, in other studies, amphotericin B has been correlated to poor clinical outcome, and therefore it may not be a good option as a monotherapy [40,41]. Azoles, and especially the newer triazoles, may be a good therapeutic strategy both as monotherapy and combination therapy. Fluconazole, posaconazole, voriconazole, and ravuconazole have been described to be efficacious; in particular, voriconazole presented the strongest activity in vitro, even better than liposomal amphotericin B [1,14,15,30,42,43]. The use of terbinafine, which is usually involved in the treatment of dermatophyte infections, has been reported in one case report in association with voriconazole [23]. The rationale of these association is that in vitro a synergistic combination has been reported with azoles, echinocandins, or polyenes. However, evidence suggests an emerging resistance to azole treatment because of the formation of biofilms; this hypothesis is particularly concerning for patients with cardiac devices or mechanical prosthetic valves [44]. Therapeutic failure has been described, mostly in immunocompromised patients, for all cited antimycotic regimens.
In general, when fungal endocarditis is diagnosed, pharmacological therapy is not sufficient: a valve replacement should be considered mandatory [15,23,35]. The 2009 IDSA guidelines for Candida endocarditis treatment recommend fluconazole as step-down therapy for patients undergoing valve replacement surgery, and indefinite fluconazole suppression therapy for patients unable to undergo valve replacement surgery [45]. The American Heart Association guidelines recommend valve surgery in addition to parenteral antifungal therapy, followed by life-long therapy with azoles [35]. Boland et al. [46] described their 40-year experience (1970–2008) at the Mayo Clinic with fungal endocarditis. They collected twenty-one cases of culture-proven prosthetic valve fungal endocarditis. Among the seven long-term survivors (follow-up range, 22–129 months; mean, 70 months; median, 72 months), four received chronic (>6 months) suppressive treatment after initial treatment with valve replacement and parenteral antifungal therapy. Given the limited experience on Trichosporon spp. endocarditis, there are no official recommendations regarding long-term suppressive therapy and, nowadays, the prescription of long-life suppressive therapy after the valve surgical replacement is controversial. In fact, considering the ability of Trichosporon spp. strains to form biofilms on implanted devices, azoles or even the newer triazoles might not represent the optimal molecules for suppressive therapy after cardiac surgery because of their poor penetration of biofilms [44,47,48,49]. However, since an endogenous dissemination model of Trichosporon spp. have been theorized, at least in immunocompromised or at-risk patients, this therapeutic approach may be useful in preventing recurrencies of trichosporonosis in previously affected patients [6,50]. In our case, the fluconazole prescription was always well-tolerated and possibly contributed to our patient remaining relapse-free.
5. Conclusions
Clinicians should be aware of the existence of rare causes of fungal endocarditis or endovascular infections such as Trichosporon spp. in immunocompromised and immunocompetent patients with recent heart surgery. Consideration of all possible causative agents of infective endocarditis is essential to prescribe an appropriate empirical therapy. Considering the high mortality rate of Trichosporon spp. invasive infections, this yeast should be considered when treating a prosthetic valve infection with negative blood cultures, irrespective of the time elapsed since surgery. The combination of voriconazole plus amphotericin B, along with prompt surgical intervention, may be effective for the acute treatment of Trichosporon endocarditis. Considering the high mortality and morbidity risk in case of fungal endocarditis recurrencies, long-term suppressive therapy with azoles should be considered in patients who have undergone surgical treatment and are considered at high risk of infection relapse.
Author Contributions
Conceptualization, L.S., B.F., A.M. (Alice Mulè); data curation, A.L., F.R., A.S., writing—original draft preparation, A.M. (Alice Mulè), A.L., F.R., A.S.; writing—review and editing, B.F., S.A., S.L., E.C., P.L., E.V.H., B.S.; supervision, L.S., F.C., A.M. (Alberto Matteelli). All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki.
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Chen S.C.-A., Perfect J., Colombo A.L., Cornely O.A., Groll A.H., Seidel D., Albus K., de Almedia J.N., Garcia-Effron G., Gilroy N., et al. Global Guideline for the Diagnosis and Management of Rare Yeast Infections: An Initiative of the ECMM in Cooperation with ISHAM and ASM. Lancet Infect. Dis. 2021;21:e375–e386. doi: 10.1016/S1473-3099(21)00203-6. [DOI] [PubMed] [Google Scholar]
- 2.Gross J.W., Kan V.L. Trichosporon Asahii Infection in an Advanced AIDS Patient and Literature Review. AIDS. 2008;22:793–795. doi: 10.1097/QAD.0b013e3282f51ecc. [DOI] [PubMed] [Google Scholar]
- 3.Bayramoglu G., Sonmez M., Tosun I., Aydin K., Aydin F. Breakthrough Trichosporon Asahii Fungemia in Neutropenic Patient with Acute Leukemia While Receiving Caspofungin. Infection. 2008;36:68–70. doi: 10.1007/s15010-007-6278-6. [DOI] [PubMed] [Google Scholar]
- 4.Biasoli M.S., Carlson D., Chiganer G.J., Parodi R., Greca A., Tosello M.E., Luque A.G., Montero A. Systemic Infection Caused by Trichosporon Asahii in a Patient with Liver Transplant. Med. Mycol. 2008;46:719–723. doi: 10.1080/13693780802232928. [DOI] [PubMed] [Google Scholar]
- 5.Takashima M., Sugita T. Taxonomy of Pathogenic Yeasts Candida, Cryptococcus, Malassezia, and Trichosporon. Med. Mycol. J. 2022;63:119–132. doi: 10.3314/mmj.22.004. [DOI] [PubMed] [Google Scholar]
- 6.Colombo A.L., Padovan A.C.B., Chaves G.M. Current Knowledge of Trichosporon spp. and Trichosporonosis. Clin. Microbiol. Rev. 2011;24:682–700. doi: 10.1128/CMR.00003-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chagas-Neto T.C., Chaves G.M., Colombo A.L. Update on the Genus Trichosporon. Mycopathologia. 2008;166:121–132. doi: 10.1007/s11046-008-9136-x. [DOI] [PubMed] [Google Scholar]
- 8.Walsh T.J. Trichosporonosis. Infect. Dis. Clin. N. Am. 1989;3:43–52. doi: 10.1016/S0891-5520(20)30245-2. [DOI] [PubMed] [Google Scholar]
- 9.Sugita T., Nishikawa A., Shinoda T., Kume H. Taxonomic Position of Deep-Seated, Mucosa-Associated, and Superficial Isolates of Trichosporon Cutaneum from Trichosporonosis Patients. J. Clin. Microbiol. 1995;33:1368–1370. doi: 10.1128/jcm.33.5.1368-1370.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ruan S.-Y., Chien J.-Y., Hsueh P.-R. Invasive Trichosporonosis Caused by Trichosporon asahii and Other Unusual Trichosporon Species at a Medical Center in Taiwan. Clin. Infect. Dis. 2009;49:e11–e17. doi: 10.1086/599614. [DOI] [PubMed] [Google Scholar]
- 11.Guého E., de Hoog G.S., Smith M.T. Neotypification of the Genus Trichosporon. Antonie Van. Leeuwenhoek. 1992;61:285–288. doi: 10.1007/BF00713937. [DOI] [PubMed] [Google Scholar]
- 12.Pagnocca F.C., Legaspe M.F.C., Rodrigues A., Ruivo C.C.C., Nagamoto N.S., Bacci M., Forti L.C. Yeasts Isolated from a Fungus-Growing Ant Nest, Including the Description of Trichosporon chiarellii sp. nov., an Anamorphic Basidiomycetous Yeast. Int. J. Syst. Evol. Microbiol. 2010;60:1454–1459. doi: 10.1099/ijs.0.015727-0. [DOI] [PubMed] [Google Scholar]
- 13.Hickey P.W., Sutton D.A., Fothergill A.W., Rinaldi M.G., Wickes B.L., Schmidt H.J., Walsh T.J. Trichosporon mycotoxinivorans, a Novel Respiratory Pathogen in Patients with Cystic Fibrosis. J. Clin. Microbiol. 2009;47:3091–3097. doi: 10.1128/JCM.00460-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rath P.C., Purohit B.V., Agrawal B., Reddy K., Nutankavala L., Narreddy S., Reddy M., Abu Salim M. Pacemaker Lead Endocarditis Due to Trichosporon Species. J. Assoc. Physicians India. 2015;63:66–68. [PubMed] [Google Scholar]
- 15.Oh T.H., Shin S.U., Kim S.S., Kim S.E., Kim U.J., Kang S.-J., Jang H.-C., Jung S.I., Shin J.-H., Park K.-H. Prosthetic Valve Endocarditis by Trichosporon mucoides: A Case Report and Review of Literature. Medicine. 2020;99:e22584. doi: 10.1097/MD.0000000000022584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Izumi K., Hisata Y., Hazama S. A Rare Case of Infective Endocarditis Complicated by Trichosporon asahii Fungemia Treated by Surgery. Ann. Thorac. Cardiovasc. Surg. 2009;15:350–353. [PubMed] [Google Scholar]
- 17.Tokimatsu I., Kushima H., Hashinaga K., Umeki K., Ohama M., Ishii H., Kishi K., Hiramatsu K., Kadota J.-I. The Prophylactic Effectiveness of Various Antifungal Agents against the Progression of Trichosporonosis Fungemia to Disseminated Disease in a Neutropenic Mouse Model. Int. J. Antimicrob. Agents. 2007;29:84–88. doi: 10.1016/j.ijantimicag.2006.09.013. [DOI] [PubMed] [Google Scholar]
- 18.Ye X., Wang A., Lin W., Xu Y., Dong X., Zhou Y., Tian K., Xu X. The Role of Intestinal Flora in Anti-Tumor Antibiotic Therapy. Front. Biosci. 2022;27:281. doi: 10.31083/j.fbl2710281. [DOI] [PubMed] [Google Scholar]
- 19.Couto R., Couto G., Abrahão I., Compagnoni I., Carnio T., Tolentino J. Endocarditis Due to Trichosporon beigelii 11 Years after Mitral Valve Replacement. Rev. Port. De Cardiol. 2021;40:305.e1–305.e3. doi: 10.1016/j.repce.2018.04.014. [DOI] [PubMed] [Google Scholar]
- 20.Mehta V., Mohanty A., Meena S., Rahul J.S., Uttam Kumar N., Chattopadhyay D., Bakliwal A., Choudhary R., Gupta P. Wickerhamomyces Anomalous: A Rare Cause of Fungemia Causing Febrile Neutropenia in Acute Lymphoblastic Leukemia. Case Rep. Infect. Dis. 2020;2020:8847853. doi: 10.1155/2020/8847853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ramos J.M., Cuenca-Estrella M., Gutierrez F., Elia M., Rodriguez-Tudela J.L. Clinical Case of Endocarditis Due to Trichosporon Inkin and Antifungal Susceptibility Profile of the Organism. J. Clin. Microbiol. 2004;42:2341–2344. doi: 10.1128/JCM.42.5.2341-2344.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Paniagua L.M., Sudhakar D., Perez L.E., Miranda D., Urena P., Gregoric I., Kar B., Jneid H., Ramirez J., Paniagua D. Prosthetic Valve Endocarditis from Trichosporon asahii in an Immunocompetent Patient. JACC Case Rep. 2020;2:693–696. doi: 10.1016/j.jaccas.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tse C., Boodman C., Wuerz T. Trichosporon Mucoides Prosthetic Valve Endocarditis Managed with Antifungal Suppression Therapy. Med. Mycol. Case Rep. 2022;36:10–12. doi: 10.1016/j.mmcr.2022.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tattevin P., Revest M., Lefort A., Michelet C., Lortholary O. Fungal Endocarditis: Current Challenges. Int. J. Antimicrob. Agents. 2014;44:290–294. doi: 10.1016/j.ijantimicag.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 25.Ghiasian S.A., Maghsood A.H., Mirhendi S.H. Disseminated, Fatal Trichosporon asahii Infection in a Bone Marrow Transplant Recipient. J. Microbiol. Immunol. Infect. 2006;39:426–429. [PubMed] [Google Scholar]
- 26.Fleming R.V., Walsh T.J., Anaissie E.J. Emerging and Less Common Fungal Pathogens. Infect. Dis. Clin. N. Am. 2002;16:915–933. doi: 10.1016/S0891-5520(02)00041-7. [DOI] [PubMed] [Google Scholar]
- 27.Krcmery V., Mateicka F., Kunová A., Spánik S., Gyarfás J., Sycová Z., Trupl J. Hematogenous Trichosporonosis in Cancer Patients: Report of 12 Cases Including 5 during Prophylaxis with Itraconazol. Support. Care Cancer. 1999;7:39–43. doi: 10.1007/s005200050221. [DOI] [PubMed] [Google Scholar]
- 28.Walsh T.J., Groll A., Hiemenz J., Fleming R., Roilides E., Anaissie E. Infections Due to Emerging and Uncommon Medically Important Fungal Pathogens. Clin. Microbiol. Infect. 2004;10((Suppl. 1)):48–66. doi: 10.1111/j.1470-9465.2004.00839.x. [DOI] [PubMed] [Google Scholar]
- 29.Kendirli T., Ciftçi E., Ince E., Oncel S., Dalgiç N., Güriz H., Unal E., Dogru U. Successful Treatment of Trichosporon Mucoides Infection with Lipid Complex Amphotericin B and 5-Fluorocytosine. Mycoses. 2006;49:251–253. doi: 10.1111/j.1439-0507.2006.01223.x. [DOI] [PubMed] [Google Scholar]
- 30.Padhi S., Dash M., Pattanaik S., Sahu S. Fungemia Due to Trichosporon mucoides in a Diabetes Mellitus Patient: A Rare Case Report. Indian. J. Med. Microbiol. 2014;32:72–74. doi: 10.4103/0255-0857.124324. [DOI] [PubMed] [Google Scholar]
- 31.Lopes J.O., Alves S.H., Klock C., Oliveira L.T., Dal Forno N.R. Trichosporon Inkin Peritonitis during Continuous Ambulatory Peritoneal Dialysis with Bibliography Review. Mycopathologia. 1997;139:15–18. doi: 10.1023/A:1006870017725. [DOI] [PubMed] [Google Scholar]
- 32.Watson K.C., Kallichurum S. Brain Abscess Due to Trichosporon Cutaneum. J. Med. Microbiol. 1970;3:191–193. doi: 10.1099/00222615-3-1-191. [DOI] [PubMed] [Google Scholar]
- 33.Reyes C.V., Stanley M.M., Rippon J.W. Trichosporon beigelii Endocarditis as a Complication of Peritoneovenous Shunt. Hum. Pathol. 1985;16:857–859. doi: 10.1016/S0046-8177(85)80262-8. [DOI] [PubMed] [Google Scholar]
- 34.McManus E.J., Jones J.M. Detection of a Trichosporon beigelii Antigen Cross-Reactive with Cryptococcus Neoformans Capsular Polysaccharide in Serum from a Patient with Disseminated Trichosporon Infection. J. Clin. Microbiol. 1985;21:681–685. doi: 10.1128/jcm.21.5.681-685.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Baddour L.M., Wilson W.R., Bayer A.S., Fowler V.G., Tleyjeh I.M., Rybak M.J., Barsic B., Lockhart P.B., Gewitz M.H., Levison M.E., et al. Infective Endocarditis in Adults: Diagnosis, Antimicrobial Therapy, and Management of Complications: A Scientific Statement for Healthcare Professionals from the American Heart Association. Circulation. 2015;132:1435–1486. doi: 10.1161/CIR.0000000000000296. [DOI] [PubMed] [Google Scholar]
- 36.Kontoyiannis D.P., Torres H.A., Chagua M., Hachem R., Tarrand J.J., Bodey G.P., Raad I.I. Trichosporonosis in a Tertiary Care Cancer Center: Risk Factors, Changing Spectrum and Determinants of Outcome. Scand. J. Infect. Dis. 2004;36:564–569. doi: 10.1080/00365540410017563. [DOI] [PubMed] [Google Scholar]
- 37.Nucci M., Anaissie E. Revisiting the Source of Candidemia: Skin or Gut? Clin. Infect. Dis. 2001;33:1959–1967. doi: 10.1086/323759. [DOI] [PubMed] [Google Scholar]
- 38.Colombo A.L., Branchini M.L., Geiger D., Schimidt A.L., Pignatari A.C., Fischman O. Gastrointestinal Translocation as a Possible Source of Candidemia in an AIDS Patient. Rev. Inst. Med. Trop. Sao Paulo. 1996;38:197–200. doi: 10.1590/S0036-46651996000300006. [DOI] [PubMed] [Google Scholar]
- 39.Serena C., Pastor F.J., Gilgado F., Mayayo E., Guarro J. Efficacy of Micafungin in Combination with Other Drugs in a Murine Model of Disseminated Trichosporonosis. Antimicrob. Agents Chemother. 2005;49:497–502. doi: 10.1128/AAC.49.2.497-502.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Singh S., Capoor M.R., Varshney S., Gupta D.K., Verma P.K., Ramesh V. Epidemiology and Antifungal Susceptibility of Infections Caused by Trichosporon Species: An Emerging Non-Candida and Non-Cryptococcus Yeast Worldwide. Indian. J. Med. Microbiol. 2019;37:536–541. doi: 10.4103/ijmm.IJMM_19_146. [DOI] [PubMed] [Google Scholar]
- 41.Girmenia C., Pagano L., Martino B., D’Antonio D., Fanci R., Specchia G., Melillo L., Buelli M., Pizzarelli G., Venditti M., et al. Invasive Infections Caused by Trichosporon Species and Geotrichum Capitatum in Patients with Hematological Malignancies: A Retrospective Multicenter Study from Italy and Review of the Literature. J. Clin. Microbiol. 2005;43:1818–1828. doi: 10.1128/JCM.43.4.1818-1828.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lacasse A., Cleveland K.O. Trichosporon mucoides Fungemia in a Liver Transplant Recipient: Case Report and Review. Transpl. Infect. Dis. 2009;11:155–159. doi: 10.1111/j.1399-3062.2008.00355.x. [DOI] [PubMed] [Google Scholar]
- 43.Francisco E.C., de Almeida Junior J.N., de Queiroz Telles F., Aquino V.R., Mendes A.V.A., de Andrade Barberino M.G.M., de Tarso O Castro P., Guimarães T., Hahn R.C., Padovan A.C.B., et al. Species Distribution and Antifungal Susceptibility of 358 Trichosporon Clinical Isolates Collected in 24 Medical Centres. Clin. Microbiol. Infect. 2019;25:909.e1–909.e5. doi: 10.1016/j.cmi.2019.03.026. [DOI] [PubMed] [Google Scholar]
- 44.Iturrieta-González I.A., Padovan A.C.B., Bizerra F.C., Hahn R.C., Colombo A.L. Multiple Species of Trichosporon Produce Biofilms Highly Resistant to Triazoles and Amphotericin B. PLoS ONE. 2014;9:e109553. doi: 10.1371/journal.pone.0109553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Baddley J.W., Benjamin D.K., Patel M., Miró J., Athan E., Barsic B., Bouza E., Clara L., Elliott T., Kanafani Z., et al. Candida Infective Endocarditis. Eur. J. Clin. Microbiol. Infect. Dis. 2008;27:519–529. doi: 10.1007/s10096-008-0466-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Boland J.M., Chung H.H., Robberts F.J.L., Wilson W.R., Steckelberg J.M., Baddour L.M., Miller D. V Fungal Prosthetic Valve Endocarditis: Mayo Clinic Experience with a Clinicopathological Analysis. Mycoses. 2011;54:354–360. doi: 10.1111/j.1439-0507.2010.01884.x. [DOI] [PubMed] [Google Scholar]
- 47.Dağ A., Cerikçioğlu N. Investigation of Some Virulence Factors of Trichosporon asahii Strains Isolated from the Clinical Samples of Hospitalized Patients. Mikrobiyol. Bul. 2006;40:225–235. [PubMed] [Google Scholar]
- 48.Di Bonaventura G., Pompilio A., Picciani C., Iezzi M., D’Antonio D., Piccolomini R. Biofilm Formation by the Emerging Fungal Pathogen Trichosporon asahii: Development, Architecture, and Antifungal Resistance. Antimicrob. Agents Chemother. 2006;50:3269–3276. doi: 10.1128/AAC.00556-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sun W., Su J., Xu S., Yan D. Trichosporon asahii Causing Nosocomial Urinary Tract Infections in Intensive Care Unit Patients: Genotypes, Virulence Factors and Antifungal Susceptibility Testing. J. Med. Microbiol. 2012;61:1750–1757. doi: 10.1099/jmm.0.049817-0. [DOI] [PubMed] [Google Scholar]
- 50.Walsh T.J., Lee J.W., Melcher G.P., Navarro E., Bacher J., Callender D., Reed K.D., Wu T., Lopez-Berestein G., Pizzo P.A. Experimental Trichosporon Infection in Persistently Granulocytopenic Rabbits: Implications for Pathogenesis, Diagnosis, and Treatment of an Emerging Opportunistic Mycosis. J. Infect. Dis. 1992;166:121–133. doi: 10.1093/infdis/166.1.121. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.